Abstract
Innovative treatments like yoga for men’s smoking cessation (SC) are lacking. To examine the feasibility and acceptability of yoga for men’s SC. We randomly assigned eligible men (smoker, ≥5 cigarettes/day, age 18–65) to receive cognitive behavioral therapy for SC, plus a yoga or wellness program. Measures included feasibility (recruitment, class attendance) and acceptability (customer satisfaction). We enrolled 38 of 49 eligible men of 167 screened in response to ads (mean age 39.9 years, ±13.7) who smoked on average 18.6 cigarettes/day (±8.3). Wellness (75.8 %) versus yoga (56 %) men attended more SC classes, p < 0.01. Sixty percent attended ≥1 yoga class. Men reported greater satisfaction with in-house versus community yoga classes. Wellness appears to be the preferred intervention; results indicated that it may be more feasible and showed increased attendance at smoking classes. To be fully feasible, yoga + SC may need to be a unified program offering all classes tailored for men and in the same location.
Keywords: Smoking cessation, Tobacco use cessation, Yoga, Exercise, Affect, Mind-body therapies
INTRODUCTION
Five times more men than women smoke worldwide [1]. In the USA in particular, where smoking is the leading preventable cause of death [2] and smoking prevalence has decreased by over 50 % since 1965, there are still significantly more men (21.5 %) than women (16.5 %) smokers [3]. The 2001 Surgeon General’s report on women and smoking highlighted several urgent action items [4]. One of these action items was to “encourage the reporting of gender-specific results from studies of influences on smoking behavior, smoking prevention, and cessation interventions.” Since 2001, researchers have made considerable progress toward increasing the evidence base and understanding of tobacco use and smoking cessation among women, although more research is still needed. However, given the continued significantly greater number of men who smoke and in some cases, higher rates of associated co-morbidities, it is imperative that the smoking cessation evidence base for men also continues to be current.
Both men and women smokers have a 3-fold increased risk of death from heart disease and a 10-fold increased risk of death due to chronic obstructive pulmonary disease (COPD) or emphysema [5]. However, across all leading mortality-related conditions, significantly more men than women die from these diseases. Men have a 22-fold increased risk of death from lung cancer when compared to nonsmokers of either gender. This is nearly double the 12-fold increased risk of death among women who smoke. Eighty to 90 % of all deaths from COPD and 90 % of all lung cancer deaths are the result of smoking [5]. And, while COPD death rates are higher for women (65,000) and rates of hospitalization and death have continued to decline among men in recent years, there is still a sizeable proportion of men who are dying from COPD (60,000) [6].
Over two thirds of men who smoke are interested in quitting smoking, and over half have reported a failed quit attempt in the past year [7]. Negative affect, stress, and cigarette cravings frequently hinder smoking cessation attempts [8]. Treatments that address these symptoms by providing smokers with methods for coping with stress improve men’s ability to quit and remain quit [9]. However, much of the research on gender differences in smoking cessation treatments has focused on the efficacy of the nicotine replacement therapy, for which the vast majority of these trials found no differences by gender, whether or not behavioral counseling was provided [10]. A review of the literature by Okoli et al. [11] showed that there are relatively few large treatment trials conducted on men’s smoking cessation. Findings from these large trials have generally shown moderate efficacy of programs typically involving a combination of behavioral counseling and medication. They were able to identify only five men’s smoking cessation studies conducted in the USA and only two since 2000 [11]. One of these later trials, Kalman et al. [12], found no significant differences in smoking abstinence among men admitted to a 21-day in-patient alcohol treatment facility (N = 36) and randomized to two conditions, 8 weeks of nicotine patch and three sessions of smoking cessation counseling delivered either concurrent with substance abuse treatment or 6 weeks delayed. The other more recent men’s smoking cessation trial [13] retrospectively analyzed the impact of mental illness on posttreatment quit rates among a largely alcohol- and/or cocaine-dependent sample of men (N = 231) attending a clinic-based 6–12-week behavioral quit smoking program in combination with prescribed bupropion and/or nicotine replacement therapy. At end of treatment 36 % of men were quit, with men diagnosed with alcohol dependence and/or schizophrenia having worse quit rates. It is notable that both of these later studies focused on substance abusers or those with mental illness [12, 13], highlighting a continuing need for research in the general population of men who smoke. In many countries, initiating smoking marks the transition to manhood and is deeply embedded in men’s everyday social relations [14]. These gender-specific issues, combined with the paucity of current smoking-cessation research in men, suggest that there is great need for programmatic tobacco cessation research specifically targeting men.
Western aerobic exercise such as brisk walking, bicycling, or treadmill use reduces cigarette cravings and nicotine withdrawal symptoms and has been shown to have a positive effect on mood and negative affect [15]. Our research with women has demonstrated that aerobic exercise coupled with CBT produces higher quit rates at posttreatment (30.6 vs. 21.8 %) and 6-month follow-up (24.6 vs. 13.6 %) than CBT without exercise [16]. Unfortunately, studies of exercise as a complementary treatment to smoking cessation have either focused exclusively on women, or have enrolled men and women, but have not reported gender-specific outcomes [17].
Yoga is an alternative to western aerobic exercise that has shown promise in our previous preliminary investigation of yoga (vinyasa) as a complementary treatment for smoking cessation among women. That pilot trial demonstrated a large effect size for smoking cessation for the group that received the yoga intervention (odds ratio = 4.56) [18]. While yoga’s growing popularity among women in the USA has been documented [19, 20], we were unable to identify any research showing trends for men’s yoga practice in the USA. It is likely, however, that there are more men practicing yoga than is believed, given the growing popularity of yoga in general [19, 20]. Further, yoga may have many benefits specifically for men, including enhancements to male reproductive health [21, 22]. In fact, many of the common poses in yoga were actually developed for young boys. Yoga schools and colleges in India, where yoga originated over 7,000 years ago, were established in the nineteenth century exclusively for boys to offer them a full education in physical health. As a form of exercise, yoga shares many of the same properties as aerobic exercise, and several studies have demonstrated that yoga produces positive effects similar to aerobic exercise including improved cardiorespiratory function, weight and body composition [23, 24], reduced stress, enhanced mood [25, 26], and overall well-being [27], and improved self-efficacy [28].
We identified four other studies that examined yoga and smoking in addition to our previous trial among women [18]. All of these studies included men and women and did not report outcomes by gender. Two studies, one investigating hatha yoga [29] and the other investigating yogic breathing exercises [30], found positive effects of yoga on cravings and mood following a period of brief smoking abstinence (e.g., 1 or 12 h) but did not focus on smoking cessation. The other two studies recruited specific clinical populations: rhythmic breathing (Sudarshan kriya and pranayama) as part of a quit smoking program for patients with cancer [31] and hatha yoga for patients quitting smoking in a drug rehabilitation program [32]. Both studies reported that a significant number of participants increased motivation to quit; however, actual quitting outcomes were not measured. None of these studies examined the feasibility of yoga for smoking cessation for men specifically. The objective of the present study (QuitStrong) was to examine feasibility and acceptability of a brief smoking cessation plus yoga intervention for a nonclinical sample of men.
METHODS
Design
QuitStrong is a pilot randomized controlled clinical trial (RCT) of a smoking cessation intervention that primarily aimed to test the feasibility of CBT plus yoga and to compare smoking outcomes for CBT plus yoga to a CBT plus a wellness program (Wellness). QuitStrong was a supplement to a larger trial comparing these treatments among women. We provided individual smoking cessation sessions and initially offered vouchers to yoga classes in the community (vs. using a cohort/group-based treatment design) based on the notion that recruiting men for yoga would be a slower process, given that yoga is largely practiced by women in the USA currently [19, 20, 33]. A wellness program was provided as a standard contact-control condition for comparison of recruitment, retention, and smoking outcomes for yoga + CBT participants.
Participant recruitment
Men were recruited through advertisements on the radio and in local newspapers, flyers inserted in local papers and posted at local venues (e.g., pharmacies, supermarkets), and brief descriptions of the study listed in the guides published by local yoga studios. Advertisements invited men smokers to join a quit-smoking research program combined with either a men’s health and wellness program or a yoga program. To be eligible for the study, callers needed to be healthy male smokers, ages 18–65, who self-reported smoking five or more cigarettes a day in the past year. Exclusion criteria were as follows: female gender, hypertension, current or recent history of medication use for major depression, participation in yoga classes within the past year, current or greater than 1 year of prior experience with mind/body therapies, or currently participating in regular exercise (defined as ≥75 min of vigorous or ≥150 min of moderate intensity activity per week). This criterion was changed during study recruitment to >180 min of moderate intensity exercise because too many potential participants were being excluded at the lower level. All advertisements contained a study phone number staffed by a research assistant who screened participants for eligibility. Callers were also screened for safe participation in exercise using the Physical Activity Readiness Questionnaire (PAR-Q) [34], a seven-item measure designed to identify individuals for whom physical activity would be inappropriate. Signed physician permission was required for study participation if potential participants endorsed one or more items on the PAR-Q. The Miriam Hospital Institutional Review Board approved study procedures and materials (#202407).
Procedures
Participants were randomly assigned to either CBT plus Yoga (Yoga) or CBT plus Contact Control (Wellness), following attendance at an orientation session where the study procedures were described. We obtained written consent from eligible men who continued to be interested in the study. Randomization was stratified by high versus low nicotine dependence using the Fagerstrom Nicotine Dependence Scale (see “Measures”) [35], to ensure even distribution across study conditions of highly nicotine-dependent men (score 7 and above). Participants in both the yoga and wellness conditions attended weekly 30-min individual sessions with a doctoral-level counselor as part of an 8-week CBT program for smoking cessation, which was based on our previous research [18] and that of others [36–38]. This program applied social cognitive theory [39] to smoking cessation, including self-monitoring stimulus control, coping with high-risk situations, stress management, and relaxation skills. A manual was used to deliver treatment and to ensure consistency of program delivery. The smoking cessation manual included topics such as setting a quit date, managing cravings, coping with triggers, and relapse prevention. Participants were not provided with smoking cessation medications by the study but were allowed to use them. We tracked participant medication usage at weekly sessions.
The yoga program included two 60–90-min beginner level vinyasa yoga classes per week administered over 8 weeks. Vinyasa yoga is characterized by a flow style of continuous movement through postures [40] and is considered to be one of the more vigorous intensity styles of yoga compared to others [41], such as Iyengar, which emphasizes correct postural alignment through the use of props, or Kripalu, which involves asanas, pranayama, and meditation in a nonstandardized sequence [42]. Men were initially given vouchers to attend yoga classes at community studios. The study team screened for beginner level vinyasa yoga classes and studios offering these classes in the local community. We provided study participants a list of these prescreened studios that they could choose to attend, along with the appropriate classes available at each facility. We collected redeemed vouchers from instructors at community studios to verify attendance. Costs of attending were covered by the study. Because of low attendance rates at these studios, halfway through the study (approximately 50 % of participants had enrolled), we arranged for vinyasa yoga classes to be delivered at our facilities (same location as the smoking classes). These in-house yoga sessions were designed to ensure that the level of difficulty of the practice was controlled and was appropriate for the study population of sedentary men who were trying to quit smoking and were new to yoga. In collaboration with the study team, the yoga instructor selected a pattern of postures (asanas) for beginners and taught this pattern consistently for each class. For example, advanced asanas such as crow pose, reverse triangle, wheel, and most arm balances (headstand, dolphin) were excluded from classes, given that they are considered inappropriate for beginners. In addition, modifications were always suggested as a variation in a sequence.
Each class consisted of the following elements (Table 1): (1) 10–15 min of pranayama (breathing exercises) and seated meditation along with grounding/centering exercises [43]; (2) followed by 40–60 min of dynamically linked asanas (e.g., sun salutations, standing postures, and seated postures); and (3) each class concluded with 10–15 min of slower, closing restorative asanas, including Savasana, and a final seated meditation. Teachers described and demonstrated postures and provided encouragement and positive affirmations. Experienced and certified yoga instructors taught all courses. All yoga instructors were registered with the National Yoga Alliance (yogaalliance.com), the national accrediting body of yoga teachers.
Table 1.
Elements of vinyasa yoga classes for QuitStrong
| 1. Pranayama (breathing practices) | Classes begin with active exhalations and very brief breath retentions. |
| 2. Seated meditation | Brief guided meditation that directs participants to focus on breath and body awareness as well as instilling feelings of well-being and acceptance. |
| 3. Grounding/centering | Focuses awareness and supports safety and guidance in the class [43]. Also prepares students psychologically, spiritually, and physically to grow in the practice shifting from usual to heightened awareness. The belief amongst yoga practitioners is that when a person is disconnected from his/her physical, emotional, or natural being, he becomes compromised such that his ability to grow is reduced, and this compromised state likely manifests behaviorally or psychologically/emotionally as anxiety or stress in the body. |
| 4. Sun salutations | Participants guided through a series of flowing yoga postures to warm the body and to prepare them for standing postures. Sequences are beginner level but aerobically challenging. |
| 5. Standing postures | Participants instructed in a series of standing postures linked together with the breath. |
| 6. Seated postures | Participants guided through seated postures involving abdominal exercises, forward bends, backbends, and twists. |
| 7. Inversions | Participants instructed in basic inversion poses such as shoulder stand and legs-up-the-wall pose. Poses are designed to cool the body after the vigorous poses and prepare the body for relaxation. |
| 8. Savasana (relaxation) | Participants have 5–10 min of supine-guided relaxation to provide closure. |
The wellness program consisted of a brief discussion with the smoking counselor, consisting of handouts, books, and videos focused on various health and lifestyle topics (e.g., healthy eating, cancer and cardiovascular disease prevention). These materials were delivered to participants following each of the 30-min weekly smoking classes. Counselors highlighted the main points of the wellness materials for the week and provided discussion on each topic and an opportunity to answer participant questions.
Measures
Feasibility (primary outcome) was defined based on three factors comparing yoga versus wellness participants: (1) recruitment (no. of calls received in response to advertising), (2) adherence to treatment (% classes attended), and (3) participant retention at key time points (number of enrolled men who completed treatment, 3- and 6-month follow-up). We measured study retention by tracking the number of missed sessions during treatment, number of required treatment makeup sessions (smoking, yoga and wellness), and the number of participants who dropped out of treatment. At the conclusion of treatment, smoking counselors asked men who participated in the yoga condition open-ended questions to gauge study acceptability and participant satisfaction with the program, including their feelings about the yoga class. These feasibility and acceptability measures were used to inform the refinement of the study protocol, including the yoga intervention, for a future trial.
Assessments included measures of demographics (e.g., race, income, and education), smoking history and dependence (Fagerstrom Test of Nicotine Dependence (FTND)) [35, 44], smoking rate and self-reported medication usage (e.g., NRT), and withdrawal symptoms. The main outcome for analysis was a 7-day point prevalence abstinence measured at 8 weeks (end-of-treatment) and 3- and 6-month posttreatment. Participants completed smoking rate questions to measure continuous abstinence and 7-day point prevalence at weekly smoking cessation classes and follow-up assessments. They provided breath samples for carbon monoxide (CO) testing to objectively verify quit status. Verification was by self-report and CO breath sample (CO cutoff =8 parts per million) for participants using NRT [45]. Self-report was always overridden by objective verification in the conservative direction (i.e., smoking) [46]. We used the 17-item Withdrawal Symptom Scale to assess smoking withdrawal [47].
We measured cognitive factors shown to be predictive of smoking abstinence in previous research, including motivation to quit (stages of change) [48], self-efficacy for achieving smoking cessation, and the participant’s confidence in his ability to abstain from smoking in high-risk situations (Smoking Self-Efficacy Questionnaire (SEQ)) [49] and situational temptations to smoke (Smoking Situations Temptations Inventory (SST)) [50]. We also assessed for depression (CES-D) [51, 52], anxiety (STAIT) [53], mindfulness (Freiburg Mindfulness Inventory (FMI)) [54], and physical self worth, attractiveness, physical strength, and condition (Physical Self Perception Profile Scale (PSPP)) [55]. Participants also reported frequency and duration of their participation in weekly exercise and concerns regarding postcessation weight gain (Smoking Situations Questionnaire (SSQ)) [56].
Analyses
Baseline demographic, smoking, and other psychosocial variables were examined for group differences at baseline using chi-square tests or analysis of variance (ANOVA) depending on the variable characteristics. All descriptive, analysis of covariance (ANCOVA) analyses, general estimating equations (GEE), logistic regression, and longitudinal linear mixed model analyses were conducted using SAS 9.3 (©SAS Institute Inc., Cary, NC, 2002–2010, www.sas.com).
Primary analyses
The primary outcomes were study feasibility and acceptability, and 7-day point prevalence abstinence (PPA) measured at 8 weeks (end-of-treatment), 3- and 6-month follow-up. CO-validated 7-day PPA was examined across treatment group and time (week 8 and 3- and 6-month follow-up) using the intention-to-treat principle within the GEE approach [57]. The GEE model was fit with an autoregressive working correlation structure.
Secondary analyses
Longitudinal mixed model analyses using baseline values as covariates, and traditional ANCOVAs, were both used, depending on the number of assessments, to examine the differences in the effects of CBT + Yoga versus CBT + Wellness on psychosocial variables previously found to be, or potentially, related to smoking cessation, and/or posited to be potential mediating variables in the smoking cessation process. The mixed models were fit with an autoregressive covariance structure. All participant data was included in the longitudinal mixed analyses using the Proc MIXED procedure in SAS 9.3, which accommodates missing values under the assumption of missing at random to allow maximum use of the available data from each time point.
RESULTS
Eligibility and recruitment
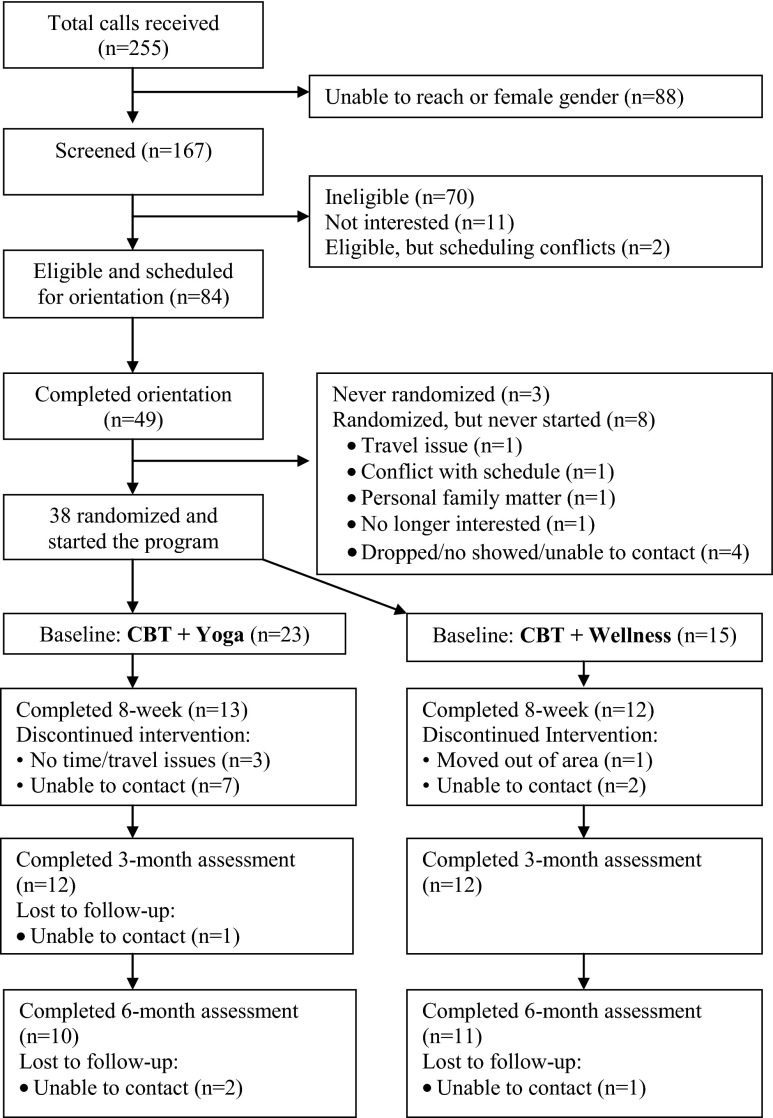
We received 255 calls in response to our advertisements; of these callers, 167 men could be reached and completed telephone screening (Fig. 1). Eighty-four of screened callers were eligible and scheduled for orientation. Forty-nine of eligible participants attended orientation. A final sample of 38 men was randomized and started treatment (n = 23 yoga; n = 15 wellness).
Fig. 1.
QuitStrong randomized feasibility pilot consort diagram
Eighty-three individuals screened ineligible. Reasons for ineligibility were medical conditions (54 %), current participation in regular exercise (10 %), schedule conflicts, or smoking less than five cigarettes daily (9 %). Other reasons for ineligibility were, age older than 65 (6 %), current use of NRT, current enrollment in another quit smoking program, BMI >40 (5 %), and current yoga practice (2 %).
Baseline demographic, psychosocial, and health characteristics
Most participants were Caucasian (94.6 %). The mean age of the sample was 39.9 years (SD = 13.7). A majority (57.9 %) of men had completed some college; 36.8 % were married or living with significant other; and 71.1 % were employed. Of the participants who answered the question about annual household income (n = 32), 37.5 % reported an income of < $30,000. There were no significant treatment group differences across demographic variables (Table 2).
Table 2.
Baseline characteristics of QuitStrong study participants
| Wellness (n = 15) | Yoga (n = 23) | All (n = 38) | p value | |
|---|---|---|---|---|
| Age, mean (SD) | 35.3 (14.0) | 42.9 (12.9) | 39.9 (13.7) | 0.095 |
| Education, % | 0.292 | |||
| Less than high school High school Some college College Graduate |
13.3 46.7 6.7 33.3 |
8.7 21.7 21.7 47.8 |
10.5 31.6 15.8 42.1 |
|
| Race, % | 0.323 | |||
| White Black or African American-Asian |
92.9 0 7 1 |
95.7 4.3 0 |
94.6 2.7 2.7 |
|
| Household income, % | 0.398 | |||
| Under $10,000 $10,000–$29,999 $30,000–$50,000 Over $50,000 |
25.0 25.0 25.0 25.0 |
5.0 25.0 30.0 40.0 |
12.5 25.0 28.1 34.4 |
|
| Employed, % | 53.3 | 82.6 | 71.1 | 0.052 |
| Marital status, % | 0.799 | |||
| Single (never married) Single living with significant other Married Divorced Separated |
33.3 20.0 26.7 13.3 6.7 |
34.8 17.4 13.0 21.7 13.0 |
34.2 18.4 18.4 18.4 10.5 |
|
| Minutes per week exercise, mean (SD) | 51.3 (75.7) | 75.7 (150.5) | 66.13 (125.6) | 0.567 |
| Cigarette per day, mean (SD) Range |
15.3 (4.4) 10–20 |
20.8 (9.6) 7–40 |
18.6 (8.3) 7–40 |
0.024* |
| CO level, mean (SD) | 15.3 (11.1) | 24.4 (19.2) | 20.8 (16.9) | 0.103 |
| FTND score, mean (SD) | 4.3 (2.3) | 5.1 (2.4) | 4.8 (2.4) | 0.305 |
| Stage of change for smoking, % | 0.832 | |||
| Contemplation Preparation |
40 60 |
43.5 56.5 |
42.1 57.9 |
|
| Confidence to quit, mean (SD) | 4.2 (1.4) | 4.7 (1.3) | 4.5 (1.3) | 0.219 |
| Age when started smoking, mean (SD) | 15.9 (2.4) | 16.1 (4.4) | 16.0 (3.7) | 0.831 |
| Times made serious attempt, mean (SD) | 3.4 (3.0) | 3.8 (3.6) | 3.6 (3.3) | 0.705 |
| Withdrawal symptoms, mean (SD) | 36.4 (8.1) | 33.9 (10.2) | 34.9 (9.4) | 0.429 |
| Smoking Situations Questionnaire (SSQ), mean (SD) | 1.9 (0.8) | 1.8 (0.8) | 1.8 (0.8) | 0.627 |
| Smoking Self-Efficacy Questionnaire (SEQ), mean (SD) | ||||
| Overall Internal stimuli External stimuli |
2.7 (0.8) 2.7 (0.8) 2.8 (0.9) |
2.5 (0.7) 2.4 (0.9) 2.6 (0.8) |
2.6 (0.8) 2.5 (0.9) 2.6 (0.8) |
0.283 0.252 0.426 |
| Smoking Situations Temptations, mean (SD) | ||||
| Total Habit Social Mood |
30.4 (4.5) 9.4 (2.0) 9.9 (2.7) 11.1 (1.5) |
30.6 (6.9) 9.5 (3.1) 10.3 (2.4) 10.8 (3.4) |
30.5 (6.0) 9.5 (2.7) 10.1 (2.5) 10.9 (2.8) |
0.935 0.894 0.641 0.665 |
| CESD-10, mean, SD | 8.1 (4.0) | 7.0 (4.9) | 7.4 (4.6) | 0.490 |
| STAIT total score, mean, SD | 42.5 (6.8) | 35.8 (9.5) | 38.4 (9.1) | 0.023* |
| PSPP, mean (SD) | ||||
| Total Physical self-worth subscale Attractiveness subscale Physical strength subscale Physical condition subscale |
58.3 (9.7) 15.5 (3.4) 14.5 (3.6) 14.7 (3.6) 13.5 (3.1) |
61.6 (15.3) 15.9 (4.3) 15.7 (5.2) 15.8 (3.9) 14.1 (4.0) |
60.3 (13.3) 15.8 (3.9) 15.2 (4.6) 15.4 (3.8) 13.9 (3.6) |
0.421 0.776 0.458 0.361 0.626 |
| FMI-14 item score, mean (SD) | 36.8 (5.5) | 38.5 (7.2) | 37.8 (6.6) | 0.437 |
p values pertain to tests of statistical significance comparing yoga versus wellness conditions across each variable
Among the psychosocial variables (Table 2), the only significant baseline treatment group difference was for the STAIT score, with the wellness group (M = 42.5, SD = 6.8) exhibiting significantly higher anxiety scores than the yoga group (M = 35.8, SD = 9.5), p = 0.023.
Smoking history and readiness to quit
Baseline smoking patterns and history information are listed in Table 2. Men smoked on average 18.6 cigarettes per day (SD = 8.3), with the yoga group smoking at a higher rate (M = 20.8, SD = 9.6) than the wellness group (M = 15.3, SD = 4.4), p = 0.024. Forty-two percent of participants were in the contemplation stage (planned to quit in next 6 months), and 58 % were in preparation stage of change (planned to quit in next 30 days and had ≥1 quit attempt within the past year). On average, men reported the age of 16 years as when they began smoking, and they averaged 3.6 lifetime quit attempts. Mean reported confidence to quit was 4.5 (SD = 1.3; 7-point scale).
Feasibility: program adherence and participant retention
Treatment session attendance
Overall, men attended 63.5 % of CBT for smoking cessation sessions that were delivered once a week for 8 weeks. There was a significant difference (p < 0.001) in the percentage attendance of total possible smoking cessation sessions for men in the yoga group (56 %) versus men in the wellness group (75.8 %). Within the yoga condition, there was no significant difference (p = 0.41) between the community yoga participants’ attendance in smoking classes (58.3 %) versus the in-house yoga participants’ attendance (52.3 %).
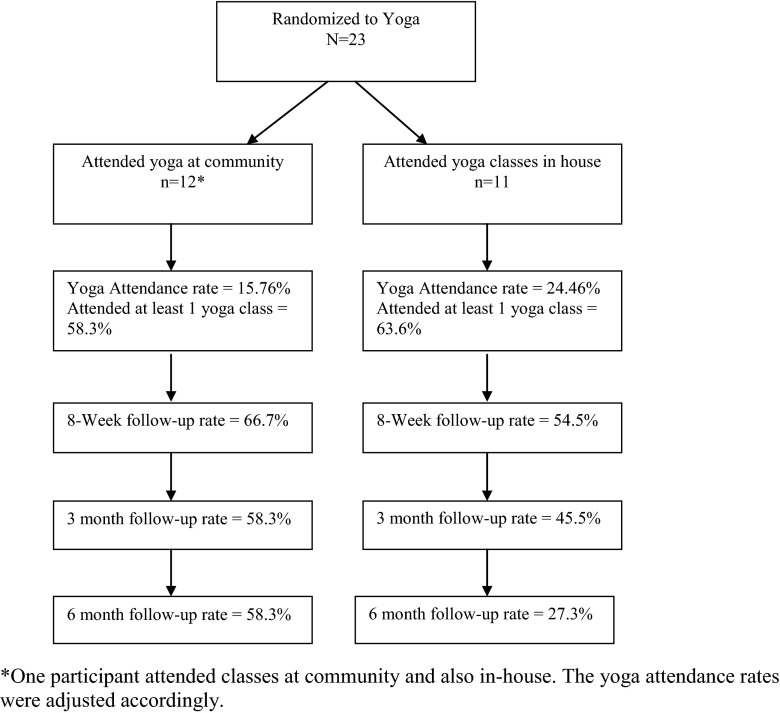
Men randomized to yoga attended 20.1 % of the 16 total yoga classes available across 8 weeks. Figure 2 shows yoga class and follow-up attendance by community versus in-house attendees. Men who attended in-house sessions attended significantly more of available sessions (24.5 %) than those who attended classes in the community (15.8 %), p = 0.037. Overall, 60.8 % of men attended at least one yoga class, and we observed no significant difference (p = 0.80) for those who attended at least one session of the community classes (58.3 %) versus the in-house classes (63.6 %).
Fig. 2.
Attendance and retention rates of community versus in-house yoga classes. One participant attended classes at community and also in-house. The yoga attendance rates were adjusted accordingly
Men in the wellness group received a brief discussion and handout materials about wellness immediately after the smoking session meeting, and consequently, the attendance rate for total wellness sessions is equal to that of their attendance for total smoking cessation sessions (75.8 %). This percentage is significantly greater (p < 0.001) than the rate of attendance (20.1 %) for total yoga sessions.
Follow-up attendance
A total of 25 men completed treatment, 8-week follow-up (n = 13 yoga; n = 12 wellness). Twenty-four men completed the 3-month follow-up (n = 12 yoga; n = 12 wellness), and 21 men completed the 6-month follow-up (n = 10 yoga; n = 11 wellness). Although a greater percentage of men in the yoga group were lost to attrition, the chi-square tests indicated that the group differences were not significant, with p = 0.14, 0.08 at 0.07 at 8 weeks, 3 and 6 months, respectively. Follow-up rates for yoga by community versus in-house are shown in Fig. 2 and were as follows: week 8 (66.7 vs. 54.5 %), 3 months (58.3 vs. 45.5 %), and 6 months (58.3 vs. 27.3 %). Chi-square tests indicated that these differences were also not significantly different between groups with p = 0.55, 0.54, and 0.13 at 8 weeks and 3- and 6-month follow-up, respectively.
We also examined attrition based on initial stage of change within each treatment group at each follow-up (Table 3). For participants who started in the contemplation stage, the proportion missing was similar within treatment groups at each assessment. However, for participants who started in the preparation stage, there was differential group attrition with only one participant in wellness missing at 6 months, while the number missing in the yoga group steadily increased from 5 to 7 to 8, at the 8-week, 3-month, and 6-month assessments, respectively, p = 0.02.
Table 3.
Baseline stage of change and attrition rates over time based on baseline stage
| Contemplation stage | Preparation stage | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 8 weeks missing, % (n) | 3 months missing, % (n) | 6 months missing, % (n) | Baseline | 8 weeks missing, % (n) | 3 months missing, % (n) | 6 months missing, % (n) | |
| In-house yoga | 6 | 50 (3) | 50 (3) | 66.7 (4) | 5 | 40 (2) | 60 (3) | 80 (4) |
| Community yoga | 4 | 25 (1) | 25 (1) | 25 (1) | 8 | 37.5 (3) | 50 (4) | 50 (4) |
| Wellness | 6 | 50 (3) | 33.3 (2) | 50 (3) | 9 | 0 | 0 | 11.1 (n) |
Missing % and n are based on n of original baseline staging
Acceptability: men’s reporting on yoga classes from open-ended questions
At the end of treatment, smoking counselors asked a random selection of men in the yoga condition at their 8-week smoking cessation session, open-ended questions regarding their perspectives on the yoga classes to better understand factors related to attendance. There were nine total responders to these questions: four men who had attended community classes, four men who had attended in-house classes, and one who began treatment, taking classes in the community but switched to in-house classes when we began offering these instead of studio vouchers halfway through the study. Four themes emerged across community versus in-house yoga, including feelings about attending classes with women, previous yoga experience, individual attention, and degree of challenge.
Community classes and observations regarding taking classes with women
Two participants directly commented on attending classes with women. One participant reported that he felt uncomfortable going to yoga class given that the classes were mostly older women. This participant reported that he practiced yoga at home and sometimes used video. Another participant reported that he liked being in a class of all women. However, both of these men attended only one yoga class.
Previous experience with yoga
Only men who had attended more than one yoga class at a community studio reported that they had done yoga in the past. One participant who took six classes in the community reported that he did not usually attend his assigned studio but instead attended a studio closer to his home. The other participant had taken nine classes and stated that he had previously attended yoga with a friend.
Preferences for individual attention and modifications
Men who attended in-house classes overall had positive experiences, and all five of them commented that they liked the individual level attention. One participant who completed community classes then switched to in-house classes responded that he liked the [in-house] yoga instructor’s class better than community classes, as the in-house instructor’s class better addressed his needs as a beginner. He stated that community classes did not always take into consideration that he was a beginner even though he was taking a beginner level class. One man enjoyed that the teacher had modified poses to help him with his back problems. Another man who also attended seven classes said that he would not change a thing about his first class. He enjoyed the pace, atmosphere, and personal instruction that each participant received as the facilitator moved around the room.
Yoga practice and degree of challenge
Three men who attended in-house classes commented on the level of challenged offered by yoga. Overall, they felt yoga was appropriately challenging for them. One participant who attended 15 in-house sessions stated that he liked the yoga and initially he felt that he wanted [the classes] to be more challenging, at a higher intensity and difficulty level. However, by the end of treatment, he reported feeling very challenged. He had started doing home practice and said that he was very interested in continuing to do yoga. Another participant who was only able to attend yoga once a week also found yoga to be challenging. Another participant stated that he found yoga to be challenging, but he liked the individual level attention. The participant who attended both community and in-house classes reported that he liked the pace, the intensity, and difficulty level of the in-house classes.
Smoking outcomes and treatment effects
A 2 (treatment groups) × 3 (time points) GEE longitudinal analysis examined the effects of the yoga versus wellness interventions for differences in 7-day point prevalence abstinence. There was a significant main effect for group (p = 0.042) with higher odds of 7-day point prevalence abstinence for the wellness group compared to the yoga group (OR = 3.73, 95 % CI = 1.07, 12.97). There were no significant effects for time (p = 0.958) or the group × time interaction (p = 0.246). While the overall group effect was significant, secondary analyses comparing group contrast estimates at each time point found the group effect to be primarily driven by the differences between the two interventions at week 8 (p = 0.014, OR = 9.19, 95 % CI = 1.57, 53.93), with no significant differences at month 3 (p = 0.265, OR = 2.38, 95 % CI = 0.52, 10.8), or month 6 (p = 0.265, OR = 2.38, 95 % CI = 0.52, 10.8). We also evaluated for treatment group differences in 24-h point prevalence using a 2 (treatment groups) × 3 (time points) GEE longitudinal analysis and found similar results with a significant overall group effect (p = 0.016), but no significant time (p = 0.774) or group × time interaction (p = 0.341).
Secondary longitudinal analyses
Longitudinal linear mixed model analysis over three time points (8 weeks, 3 months, and 6 months) examined group, time, and group-by-time interactions, using baseline values as covariates, for the CESD, STAIT, and PSPP total score, the four PSPP subscales (self-worth, attractiveness, physical condition, physical strength), and FMI and found no significant group or group-by-time interactions. Significant effects for time were found for FMI (p = 0.004) and the PSPP attractiveness subscale (p = 0.027). Longitudinal linear mixed model analysis over two available time points (3 and 6 months) examined group, time, and group-by-time interactions, using baseline values as covariates, for smoking cessation confidence, total symptoms, SEQ overall score, the SEQ internal stimuli score, the SEQ external stimuli score, and the number of minutes per week of exercise and found no significant group or group-by-time interactions. A significant effect for time (p = 0.006) was found for smoking cessation confidence. ANCOVAs using the baseline score as a covariate also examined for group effects of the SST overall score, as well the three SST subscales (social, mood, and habit) and found no significant group differences at the 8-week immediate posttreatment assessment.
We examined change in smoking status based on initial stage of change at each follow-up. At the 8-week assessment, seven of the nonsmokers had started in the preparation stage versus two in the contemplation stage. However, this ratio changed at both the 3- and 6-month assessments, with five nonsmokers having started in preparation versus four in contemplation. There was no significant difference between nonsmokers and the stage of change they started in at 8 weeks (p = 0.17), 3-months (p = 0.87), or 6-months (p = 0.87).
DISCUSSION
We screened over 160 men of 255 callers who expressed interest in participating in this innovative research. Our final enrolled and randomized sample of men characteristically was similar to the women’s study: largely middle-income, employed Caucasian adults who were heavy smokers with reasonably moderate levels of confidence in their ability to quit. We found that at baseline, over 40 % of men expressed readiness to quit in the next 6 months (contemplation stage of change) and almost 60 % were ready to quit in the next 30 days (preparation stage of change). They also reported a very recent quit attempt (in the past year), with an average of almost four lifetime quit attempts. Over 60 % of men attended at least one yoga class, and more men attended in-house classes versus community classes. Additionally, men given the in-house program found yoga to be adequately challenging, and they overwhelmingly endorsed receiving individual attention and modifications in these classes. All of these findings suggest that, like the women in our first pilot study, men similarly have at least an initial interest in yoga for smoking cessation and can be recruited to participate in yoga for smoking cessation research. Therefore, at the very least, this study established recruitment feasibility for men and yoga plus smoking cessation research/programs. Further, it appears that, to a large extent, we captured the right audience of men for participation in a yoga-for-smoking-cessation study: Men who were very ready to quit and who had tried unsuccessfully using other methods.
There were, however, two other factors defined a priori to ascertain feasibility of yoga for smoking cessation, in addition to recruitment: (1) class attendance and (2) retention at end of treatment and follow-up. As attendance at smoking cessation classes (56 vs. 75.8 %) as well as abstinence from smoking was greater for those in the wellness group, we recognize that wellness appears to be the preferred augmentation for this population. However, it should be noted that the wellness program consisted of handouts and a brief discussion with the smoking counselor; therefore, participant burden was much lower than for yoga participants who had to attend in addition to sessions with the smoking counselor, at first, classes in the community and later, classes in-house. It is unclear whether wellness would continue to show higher rates of class attendance if participant burden were similar. Also, the lack of significant findings for the effects of yoga on smoking cessation in men in this study should be viewed with caution. All of these findings may be related to problems with our study design including obstacles to retention rather than a true reflection of yoga’s versus wellness’s efficacy for smoking cessation. In short, in terms of treatment adherence and retention feasibility, our initial design of yoga in the community compared to wellness handouts with brief discussion was not feasible, as demonstrated by the overall poor class attendance, where yoga participants only attended 20 % of all yoga classes. Class attendance was somewhat higher for in-house attendees, but this finding is somewhat muted given the lack of difference in first session attendance for the two yoga groups. Further, there was a trend toward greater numbers of yoga versus wellness participants being lost to follow-up, albeit not significant. Overall, these design issues notwithstanding wellness still may be the preferable intervention both because it appears to be more feasible and because it significantly heightened attendance at smoking classes.
The study design issues and how they inform future trials are in keeping with the purpose of this pilot study, which was to test for feasibility. As our own women’s pilot study was the only available research to which we could refer, our design of QuitStrong was largely exploratory. For this men’s study, we modified the women’s study design to initially allow men the freedom to choose their yoga classes from among those offered in the community. Our rationale was that men would be more interested in choosing a “yoga” study, if we “built in” more autonomy and control by allowing them to choose the classes they would attend. While the smoking classes were relatively better attended, we found poor attendance for yoga classes overall, particularly after the first class. Notwithstanding, significantly more men attended in-house classes. Responses to open-ended questions provide support for why this was the case, in particular, the reports by participants that they found attending community yoga classes uncomfortable. This discomfort was multifaceted. Quite often, community yoga classes are largely made up of women who have experience with yoga, are familiar with the postures, and are physically fit [19]. Indeed, both of the men who expressed preferences about attending classes with women only attended one yoga class, and this happened despite one man stating that he liked attending classes with women. Further, yoga instructors believe that bonding and support are important for yoga practice. Quite often, people feel supported when they can identify with others in a group. This does not appear to have been generally the case for the men smokers in QuitStrong attending community yoga versus in-house classes, as one participant who attended both community and in-house classes noted that he did not readily feel supported as a beginning yoga practitioner, even though he was attending beginner level yoga classes. These factors certainly affected class participation, enthusiasm, and ultimately retention and treatment findings in the yoga group, given the small final sample of men in the yoga arm of the study at follow-ups over time. This is also evidenced by the differentially higher dropout rate over time for men in the preparation stage of change who participated in the yoga versus wellness program, but no group differential dropout rate for contemplators. One would expect that if attrition was solely a factor of participant burden in the yoga arm given the greater study participation requirements and which might be suggested by our finding that significantly higher numbers of smoking classes were attended by men in wellness versus yoga, then we would expect to see similarly high group differential dropout for contemplators. With attrition largely affecting preparers in yoga, this is supportive of the idea that men were definitely interested in the yoga program, but the community-based yoga classes for men smokers trying to quit, with little to no yoga experience, were not a good fit. And, by the time that we made the change to in-house classes, very few men remained in the yoga arm of the study, too few to realistically analyze group differences across those who attended classes in the community versus in-house across stage of change.
In response to observing low yoga class attendance, we moved yoga sessions in-house, reverting to the design format we had used in the women’s study. Even though there had been significant attrition in yoga by this point, the feasibility goal and exploratory nature of the study meant that it would be necessary to adjust that which was not working in order to still inform future research with potentially testable solutions. Accordingly, in-house yoga classes consisted entirely of men who smoked, who were yoga beginners, and who had an immediate basis for bonding and social support. We are optimistic that this approach will serve as a good strategy for future investigations, given the feedback we received from men who had taken classes in the community versus in-house. In short, tailored group yoga classes for men smokers would provide the “we’re all in this together” type of peer and social support to which many of the men in the yoga condition of QuitStrong seemed to allude. Offering these tailored classes at the same site as smoking classes, as was the case when we switched yoga classes in-house, provides a more holistic presentation of a yoga and smoking cessation program and may be more feasible and acceptable for future yoga and smoking programs and research trials. This design is also in keeping with our positive experiences in the women’s study. Further, we have already incorporated all of these elements into our current large-scale efficacy trial (anticipated n = 300) designed to test yoga for smoking cessation that includes at this point at least 50 % men.
The higher mindfulness and feelings of attractiveness and confidence in ability to quit for men posttreatment compared to baseline are interesting; albeit results should be interpreted cautiously given the sample size and attrition. Overall, these findings suggest that our study may have been helpful in positively shaping men’s self-concepts. This is encouraging as it is well established that self-efficacy is a theoretical mediator for smoking cessation [58].
Limitations
Given the numbers of missed session across study arms and classes, it is likely that other issues in addition to those related to yoga classes affected men’s study participation and outcomes (e.g., eligibility criteria, wellness program design) for which we have made protocol modifications to improve feasibility and acceptability of a future trial (e.g., broader medical inclusion criteria, group-based CBT for smoking cessation, more interactive wellness program using a wellness counselor). However, the lack of yoga and smoking cessation research in general, coupled with the differential dropout rate in the yoga arm of QuitStrong, speaks to the priority of understanding the feasibility aspects of yoga, which has shown promise as a smoking cessation therapy.
CONCLUSIONS
Exercise has been shown to be an effective adjunct to smoking cessation therapy. There is sufficient research to suggest that yoga may have properties that will make it as, or even more, effective. Our preliminary research on yoga for smoking cessation was the first of its kind and focused on women. The purpose of the current study was to gain an initial understanding of yoga as a complementary treatment for smoking cessation among men. Prior to our work, smoking research employing yoga had examined only brief smoking abstinence (<12-h quit period) versus actual smoking cessation, or these studies were based on clinical samples, such as cancer patients or adults participating in a drug rehabilitation program [29–31]. Thus, as was our work among women, this research is unique, given that no other yoga studies have focused exclusively on designing and understanding yoga for men’s smoking cessation. This study showed that men were initially interested in smoking cessation programs that include yoga. However, future studies should integrate therapies such that the smoking cessation and yoga programs are perceived as a whole, rather than relying on yoga classes offered in the community that are not tailored for smokers. These yoga + smoking cessation programs need to be also designed to accommodate them as beginning level yoga practitioners who are smokers trying to quit and who are also likely to have significantly more comorbidities than those typically in yoga classes, as indicated by our exclusion of almost 55 % of men for medical/health reasons. Additionally, future trials need to carefully design the comparison arm (e.g., wellness) to ensure for appropriate equivalency in terms of participant burden and involvement to be able to solidly compare outcomes. In the mean time, our findings suggest that wellness may be the preferable and more feasible intervention program.
Acknowledgments
Funding was provided by the National Institutes of Health, National Center for Complementary, and Alternative Medicine (NCCAM #R21AT003669 to BB). The funding agency played no role in the design, conduct, or analysis of the study nor in the interpretation and reporting of the study findings. The researchers were independent from the funder. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
Ronnesia B. Gaskins, Ernestine Jennings, Herpreet Thind, Joseph Fava, Santina Horowitz, Ryan Lantini, Bruce M. Becker, and Beth C. Bock declare that they have no conflict of interest.
Adherence to ethical standards
All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Trial registration
ClinicalTrials NCT02055326
Footnotes
Implications
Practice: Yoga for smoking cessation programs would likely resonate better with men participants if both yoga and smoking cessation elements are offered in one physical location as a unified program tailored for men smokers trying to quit.
Policy: Given that the best quit smoking programs produce less than 50 % abstinence rates, new approaches, including Complementary and Alternative Medicine Therapies such as yoga, need to be considered.
Research: More research is needed to better understand gender differences in yoga practice as they may be related to health behaviors such as smoking cessation.
Contributor Information
Ronnesia B. Gaskins, Email: ronnesia_gaskins@brown.edu.
Ernestine G. Jennings, Email: Ernestine_Jennings@brown.edu.
Herpreet Thind, Email: Herpreet_Thind@brown.edu.
Joseph L. Fava, Email: jfava@lifespan.org.
Santina Horowitz, Email: shorowitz@lifespan.org.
Ryan Lantini, Email: rlantini@lifespan.org.
Bruce M. Becker, Email: bbecker@lifespan.org.
Beth C. Bock, Email: Beth_Bock@Brown.edu.
References
- 1.Guindon GE, Boisclair D. Past, current and future trends in tobacco use: HNP discussion paper. The World Bank: Washington; 2003. [Google Scholar]
- 2.CDC Smoking attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR. 2008;57:1226–1228. [PubMed] [Google Scholar]
- 3.CDC Vital signs: current cigarette smoking among adults aged >18 years—United States, 2005–2010. MMWR. 2011;60(33):1207–1212. [PubMed] [Google Scholar]
- 4.USDHHS. Surgeon general’s report—women and smoking. U.S. Department of Health and Human Services;2001.
- 5.USDHHS. The health consequences of smoking: a report of the Surgeon General. Atlanta, US: U.S. Department of Health and Human Services;2004.
- 6.Akinbami LJ, Liu X. Chronic obstructive pulmonary disease among adults aged 18 and over in the United States, 1998–2009. NCHS data brief, no 63. Hyattsville, MD.: National Center for Health Statistics.;2011. [PubMed]
- 7.CDC Quitting smoking among adults—United States, 2001–2010. MMWR. 2011;60(44):1513–1519. [PubMed] [Google Scholar]
- 8.Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129(2):270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 9.Shadel WG, Mermelstein RJ. Cigarette smoking under stress: the role of coping expectancies among smokers in a clinic-based smoking cessation program. Health Psychol. 1993;12(6):443–450. doi: 10.1037/0278-6133.12.6.443. [DOI] [PubMed] [Google Scholar]
- 10.Perkins KA, Scott J. Sex differences in long-term smoking cessation rates due to nicotine patch. Nicotine Tob Res. 2008;10(7):1245–1250. doi: 10.1080/14622200802097506. [DOI] [PubMed] [Google Scholar]
- 11.Okoli C, Torchalla I, Oliffe JL, Bottorff JL. Men's smoking cessation interventions: a brief review. J Men’s Health. 2011;8(2):100–108. doi: 10.1016/j.jomh.2011.03.003. [DOI] [Google Scholar]
- 12.Kalman D, Hayes K, Colby SM, Eaton CA, Rohsenow DJ, Monti PM. Concurrent versus delayed smoking cessation treatment for persons in early alcohol recovery. A pilot study. J Subst Abuse Treat Apr. 2001;20(3):233–238. doi: 10.1016/S0740-5472(00)00174-4. [DOI] [PubMed] [Google Scholar]
- 13.Gershon Grand RB, Hwang S, Han J, George T, Brody AL. Short-term naturalistic treatment outcomes in cigarette smokers with substance abuse and/or mental illness. J Clin Psychiatry. 2007;68(6):892–898. doi: 10.4088/JCP.v68n0611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO. Gender, Health and Tobacco. Geneva, Switzerland: Department of Gender and Women's Health, World Health Organization;2003.
- 15.Taylor AH, Ussher MH, Faulkner G. The acute effects of exercise on cigarette cravings, withdrawal symptoms, affect and smoking behaviour: a systematic review. Addict. 2007;102(4):534–543. doi: 10.1111/j.1360-0443.2006.01739.x. [DOI] [PubMed] [Google Scholar]
- 16.Marcus BH, Albrecht AE, King TK, et al. The efficacy of exercise as an aid for smoking cessation in women: a randomized controlled trial. Arch Intern Med. 1999;159(11):1229–1234. doi: 10.1001/archinte.159.11.1229. [DOI] [PubMed] [Google Scholar]
- 17.Roberts V, Maddison R, Simpson C, Bullen C, Prapavessis H. The acute effects of exercise on cigarette cravings, withdrawal symptoms, affect, and smoking behaviour: systematic review update and meta-analysis. Psychopharmacol (Berl) 2012;222(1):1–15. doi: 10.1007/s00213-012-2731-z. [DOI] [PubMed] [Google Scholar]
- 18.Bock BC, Fava JL, Gaskins R, et al. Yoga as a complementary treatment for smoking cessation in women. J Womens Health (Larchmt) 2012;21(2):240–248. doi: 10.1089/jwh.2011.2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birdee GS, Legedza AT, Saper RB, Bertisch SM, Eisenberg DM, Phillips RS. Characteristics of yoga users: results of a national survey. J Gen Intern Med. 2008;23(10):1653–1658. doi: 10.1007/s11606-008-0735-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross A, Friedmann E, Bevans M, Thomas S. National survey of yoga practitioners: mental and physical health benefits. Complement Ther Med. 2013;21(4):313–323. doi: 10.1016/j.ctim.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sengupta P, Chaudhuri P, Bhattacharya K. Male reproductive health and yoga. Int J Yoga. 2013;6(2):87–95. doi: 10.4103/0973-6131.113391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sengupta P. Health impacts of yoga and pranayama: a state-of-the-art review. Int J. Prev Med. 2012;3(7):444–458. [PMC free article] [PubMed] [Google Scholar]
- 23.Bijlani RL, Vempati RP, Yadav RK, et al. A brief but comprehensive lifestyle education program based on yoga reduces risk factors for cardiovascular disease and diabetes mellitus. J Altern Complement Med. 2005;11(2):267–274. doi: 10.1089/acm.2005.11.267. [DOI] [PubMed] [Google Scholar]
- 24.Yadav RK, Das S. Effect of yogic practice on pulmonary functions in young females. Indian J Physiol Pharmacol. 2001;45(4):493–496. [PubMed] [Google Scholar]
- 25.Bower JE, Woolery A, Sternlieb B, Garet D. Yoga for cancer patients and survivors. Cancer Control. 2005;12(3):165–171. doi: 10.1177/107327480501200304. [DOI] [PubMed] [Google Scholar]
- 26.Culos-Reed N, Carlson LE, Daroux LM, Hately-Aldous S. Discovering the physical and psychological benefits of yoga for cancer survivors. Int J Yoga Ther. 2004;14(1):45–52. [Google Scholar]
- 27.Malathi A, Damodaran A, Shah N, Patil N, Maratha S. Effect of yogic practices on subjective well being. Indian J Physiol Pharmacol. 2000;44(2):202–206. [PubMed] [Google Scholar]
- 28.Bussing A, Michalsen A, Khalsa SB, Telles S, Sherman KJ. Effects of yoga on mental and physical health: a short summary of reviews. Evid Based Complement Alternat Med. 2012;2012:165410. doi: 10.1155/2012/165410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elibero A, Janse Van Rensburg K, Drobes DJ. Acute effects of aerobic exercise and hatha yoga on craving to smoke. Nicotine Tob Res Nov. 2011;13(11):1140–1148. doi: 10.1093/ntr/ntr163. [DOI] [PubMed] [Google Scholar]
- 30.Shahab L, Sarkar BK, West R. The acute effects of yogic breathing exercises on craving and withdrawal symptoms in abstaining smokers. Psychopharmacol (Berl) 2013;225(4):875–882. doi: 10.1007/s00213-012-2876-9. [DOI] [PubMed] [Google Scholar]
- 31.Kochupillai V, Kumar P, Singh D, et al. Effect of rhythmic breathing (Sudarshan Kriya and Pranayam) on immune functions and tobacco addiction. Ann N Y Acad Sci. 2005;1056:242–252. doi: 10.1196/annals.1352.039. [DOI] [PubMed] [Google Scholar]
- 32.McIver S, O’Halloran P, McGartland M. The impact of Hatha yoga on smoking behavior. Altern Ther Health Med. 2004;10(2):22–23. [PubMed] [Google Scholar]
- 33.Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in use of complementary and alternative medicine by US adults: 1997–2002. Altern Ther Health Med. 2005;11(1):42–49. [PubMed] [Google Scholar]
- 34.Adams R. Revised Physical Activity Readiness Questionnaire. Can Fam Physician. Apr 1999;45:992, 995, 1004–1005. [PMC free article] [PubMed]
- 35.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 36.Perkins KA, Conklin CA, Levine MD. Cognitive-behavioral therapy for smoking cessation: a practical guidebook to the most effective treatments. New York: Routledge/Taylor & Francis; 2008. [Google Scholar]
- 37.Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service;2008.
- 38.Killen JD, Fortmann SP, Schatzberg AF, et al. Extended cognitive behavior therapy for cigarette smoking cessation. Addiction. 2008;103(8):1381–1390. doi: 10.1111/j.1360-0443.2008.02273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bandura A. The exercise of control. New York: W.H. Freemon; 1997. [Google Scholar]
- 40.Maehle G. Ashtanga yoga: practice and philosophy. Novato, CA: New World Library; 2011. [Google Scholar]
- 41.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 42.Faulds R. Seniors teachers at Kripalu Center for Yoga and Health. Kripalu yoga: a guide to practice on and off the mat. LLC: Random House; 2010. [Google Scholar]
- 43.Chandler K, Sahady J. Innerlight yoga teacher training manual 2005–2006. 2005. [Google Scholar]
- 44.Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addict Behav. 1994;19(1):33–39. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 45.West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction. 2005;100(3):299–303. doi: 10.1111/j.1360-0443.2004.00995.x. [DOI] [PubMed] [Google Scholar]
- 46.Ossip-Klein DJ, Bigelow G, Parker SR, Curry S, Hall S, Kirkland S. Classification and assessment of smoking behavior. Health Psychol. 1986;5(Suppl):3–11. doi: 10.1037/0278-6133.5.Suppl.3. [DOI] [PubMed] [Google Scholar]
- 47.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43(3):289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 48.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol Sep. 1992;47(9):1102–1114. doi: 10.1037/0003-066X.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 49.Etter JF, Bergman MM, Humair JP, Perneger TV. Development and validation of a scale measuring self-efficacy of current and former smokers. Addiction. 2000;95(6):901–913. doi: 10.1046/j.1360-0443.2000.9569017.x. [DOI] [PubMed] [Google Scholar]
- 50.Velicer WF, Diclemente CC, Rossi JS, Prochaska JO. Relapse situations and self-efficacy: an integrative model. Addict Behav. 1990;15(3):271–283. doi: 10.1016/0306-4603(90)90070-E. [DOI] [PubMed] [Google Scholar]
- 51.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 52.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 53.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press; 1983. [Google Scholar]
- 54.Walach H, Buchheld N, Buttenmüller V, Kleinknecht N, Schmidt S. Measuring mindfulness—the Freiburg Mindfulness Inventory (FMI) Pers Individ Differ. 2006;40(8):1543–1555. doi: 10.1016/j.paid.2005.11.025. [DOI] [Google Scholar]
- 55.Fox KR, Corbin CB. The Physical Self-Perception Profile: development and preliminary validation. J Sport Exerc Psychol. 1989;11:408–430. [Google Scholar]
- 56.Weekley CK, 3rd, Klesges RC, Reylea G. Smoking as a weight-control strategy and its relationship to smoking status. Addict Behav. 1992;17(3):259–271. doi: 10.1016/0306-4603(92)90031-P. [DOI] [PubMed] [Google Scholar]
- 57.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biom. 1986;42(1):121–130. doi: 10.2307/2531248. [DOI] [PubMed] [Google Scholar]
- 58.Schnoll RA, Martinez E, Tatum KL, et al. Increased self-efficacy to quit and perceived control over withdrawal symptoms predict smoking cessation following nicotine dependence treatment. Addict Behav. 2011;36(1–2):144–147. doi: 10.1016/j.addbeh.2010.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]