Abstract
Introduction
Free fat dermis graft is a good interpositional material for TMJ gap arthroplasty. Analysing the fate of the graft by magnetic resonance imaging (MRI) images helps in excellent visualization of both bony and soft tissue anatomy of the operated TMJ joint as well as in assessing the changes in dermis graft which was previously placed.
Purpose of this Study
To investigate the radiological fate of the dermis-fat graft within the TMJ using MRI.
Materials and Methods
Five joints of five patients who had dermis-fat grafts placed in their TMJ following gap arthroplasty were recruited for this study. Each patient had undergone TMJ gap arthroplasty with immediate dermis-fat graft placement. All the patients are then subjected to MRI.
Results
Fat graft was identified in close proximity to the mandibular condyle in all cases, with only three joints demonstrating fat covering the entire articular surface of the mandibular condyle. In the remaining joints the interpositional material found in the MRI defined joint space with mainly grey appearance, suggesting tissue change to other than fat, i.e. scar or granulation tissue.
Conclusion
When free fat dermis graft is placed as interpositional material the graft occupied the entire TM joint and prevented it from recurrent ankylosis. The graft placed aids in normal functioning of the temperomandibular joint without any complications.
Keywords: Temporomandibular joint, Ankylosis, Temporomandibular joint gap arthroplasty, MRI, Dermis-fat graft
Introduction
Current knowledge of TMJ pathologies largely depend on both the clinical presentations and available routine radio investigation. With the advent of MR imaging, the understanding of the osseous component of articulations has been furthered and the soft tissues in and about the articulation have also moved firmly into the spotlight in the new era. The distinct advantage of MR imaging and MR arthrography (MRA) [6] is that they allow for excellent visualization of both bony and soft tissue anatomy using a technique that is only minimally invasive.
Temporomandibular joint bony ankylosis is one of the rather uncommon pathologic conditions seen by the oral and maxillofacial surgeon. Ankylosis is a Greek word meaning “stiff joint”. There are various modalities of treatment for ankylosis of temporomandibular joint and temporomandibular joint gap arthroplasty has been used as a surgical treatment for many years with good outcomes. Unfortunately, TMJ gap arthroplasty results in significant regressive remodelling of the mandibular condyle. Attempts to help reduce this effect have been made with the use of interpositional grafts, but have met with little success, with alloplastic and various autogenous grafts failing to live up to expectations.
Free fat dermis graft is one such interpostioning material which is presently in research and clinical use as an interpositional material.
As early as 1914, Murphy [1] described the transplantation of autogenous free fat grafts into joints. In 1925, Lexer [1] reported that multiple small fat grafts do not survive as well as a single large fat graft when he found that the volume of the original graft can shrink to two-third of its original volume after 1 year. The shrinkage of free fat grafts was confirmed by Peer [1] who also found that after 1 year, free fat grafts lose, on average, 45 % of their original volume following transplantation.
The dermis-fat graft has previously been reported for use as an interpositional material following gap arthroplasty in the management of TMJ internal derangement. Dimitroulis [2] had been using the dermis-fat graft as interpositional material following TMJ gap arthroplasty for severe TMJ discectomy for over 5 years. While the clinical outcomes appear favourable for the use of this material in the TMJ, the fate of the dermis-fat graft within a functional joint space has never been determined and published with good result. The purpose of this study is to investigate the radiological fate of the dermis-fat graft within the TMJ using magnetic resonance imaging (MRI) (Figs. 1, 2, 3).
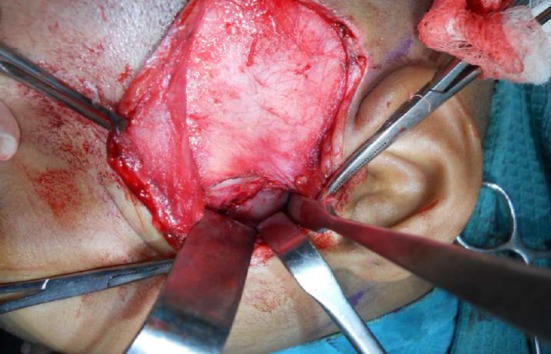
Fig. 1.

Free fat dermis graft
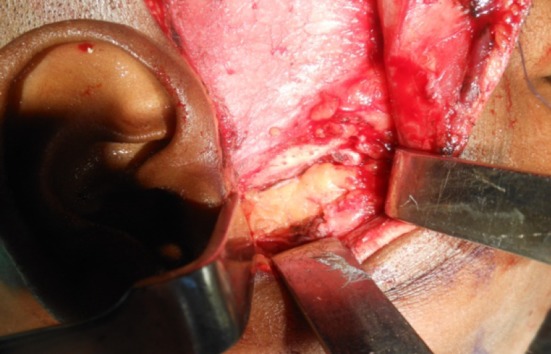
Fig. 2.
Intra operative, before placing the graft
Fig. 3.
Fat placement as interpositional gap arthroplasty
Materials and Methods
Five patients who had dermis-fat grafts placed in their TMJ following gap arthroplasty were recruited for this study. Each patient had undergone TMJ gap arthroplasty with immediate dermis-fat graft placement within the resultant joint space. The dermis-fat graft was procured from the lower abdomen through an elliptical incision that was closed primarily. The covering epidermis was removed freehand by sharp dissection with a No. 15 scalpel blade and discarded. The dermis-fat graft was trimmed and passively placed into the joint cavity to fill the whole space, and the surrounding capsule sutured to hold the graft in place. The five patients of age group from 4 to 40 years were divided into 2 groups of 2 and 3 according to the time lapse between the TMJ surgery and the MRI investigation: 0–6 months, 5–6 years (Table 1).
Table 1.
Summary of results
| Name | Age/sex | Diagnosis | Treatment done | Treatment done before | MRI findings | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| TMJ appears | Signals | Graft placed | Disk space | Graft seen | Operated space occupied | |||||
| Rajammal | 37/F | Ankylosis of left TMJ | Release of ankylotic mass and placing free fat dermis graft as an interpositional material of gap arthroplasty | 5 years | Wider | High signal areas, low signals areas in mid portion | Diffuse manner | Superiorly anteriorly posteriorly of ressected mandible | 2/3rd of the operated joint | |
| Rajeswari | 29/F | Ankylosis of left TMJ | Release of ankylotic mass and placing free fat dermis graft as an interpositional material of gap arthroplasty | 5 years | Wider larger | High signal areas, low signals areas in mid portion | Regular manner | Superiorly anteriorly posteriorly of ressected mandible | 2/3rd of the operated joint | |
| Shanthi | 28/F | Ankylosis of right TMJ | Release of ankylotic mass and placing free fat dermis graft as an interpositional material of gap arthroplasty | 6 months | Wider | Iso-high signal | Regular manner | Well outlined, anteriorly and superiorly graft placed | Superiorly anteriorly posteriorly of ressected mandible | Almost entire joint |
| Pradeepa | 4/F | Ankylosis of left TMJ | Release of ankylotic mass and placing free fat dermis graft as an interpositional material of gap arthroplasty | 6 months | Wider larger | Iso-high signal | Regular manner | Anteriorly posteriorly and superiorly graft placed | Anteriorly posteriorly of ressected mandible | Almost entire joint |
| Chandra Kupta | 38/M | Ankylosis of left TMJ | Release of ankylotic mass and placing free fat dermis graft as an interpositional material of gap arthroplasty | 6 months | Wider | Iso-high signal | Regular manner | Well outlined, anteriorly and superiorly graft placed | Superiorly anteriorly posteriorly of ressected mandible | Almost entire joint |
The patients recruited for this study were randomly selected from a larger pool of patients who were similarly treated by the same clinician for severe TMJ ankylosis (Figs. 4, 5, 6, 7).
Fig. 4.

Pre operative
Fig. 5.

Pre operative CT of TMJ
Fig. 6.

Preoperative 3D CT
Fig. 7.

Post operative mouth opening after the free fat dermis graft placed
All five patients who participated in the study were asymptomatic with good joint function at the time of the MRI investigation. Written consent from each patient was obtained. All patients underwent a standard safety screening process to identify any contraindications, such as the presence of cardiac pacemakers, steel mini-plate in the maxilla and genium were removed before their MRI examination.
All patients were scanned on a 1.5-T Philips Intra MR system using the standard 12-channel head coil. Patients were positioned comfortably and asked to keep their mouth closed for all but the last sequence, at which time a bite block was used to keep their mouths open as wide as comfortably possible.
After appropriate localizers [1] to identify the TMJ, the following sequences were acquired:
- Closed mouth:
- Sagittal T1 & proton density (PD) turbo spin echo (TSE),
- Axial T2 & T1 TSE,
- Coronal T1 & PD fat-saturated TSE,
-
2.Open mouth:
- Sagittal PD TSE.
The axial and coronal sequences were orthogonal to the body axis and centred on the TMJs. The sagittal sequences were positioned perpendicular to the head of the mandibular condyle and parallel to the ramus. The total examination time was under 30 min and all patients tolerated the examination well. The MR images obtained were examined and interpreted by two experienced specialist musculoskeletal MRI radiologists.
The grafts were evaluated on the following criteria [1]:
Signal on T1 and T2/PD images;
Presence or absence of graft tissue within the joint space. The radiological joint space was determined as the 120-degree arc extending from the midbody of the condylar head to the glenoid fossa in the sagittal and coronal planes;
If present, nature of the tissue within the joint space as determined by the T1 signal characteristics;
Volume of the fat graft within or around the joint space as calculated from the maximum diameters in the 3 orthogonal planes.
Results
The presence of dermis could not be found out on the images obtained, which was probably due to the limitation of the imaging technology of MRI rather than absence of the dermis. While fat graft was identified in close proximity to the mandibular condyle in all cases, with only 3 joints demonstrating fat covering the entire articular surface of the mandibular condyle. In the remaining joints, the interpositional material found in the MRI study defined joint space as mainly of grey appearance, suggesting tissue change to other than fat, i.e. scar or granulation tissue (Figs. 8, 9). The result has been segregated into two groups; 6 months follow up results and 4 years follow up result.
Fig. 8.
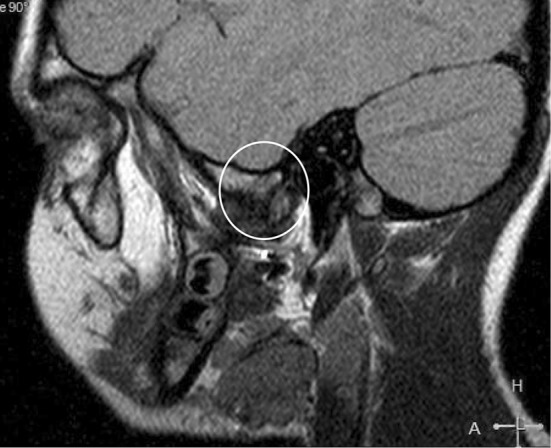
PD sagittal MR image of the TMJ (open mouth position) showing the presence of fat in the space vacated by the forward translation of the mandibular condyle in a patient who had a dermis-fat graft placed 6 months previously
Fig. 9.

PD sagittal MR image of the TMJ (closed mouth position) showing the presence of fat in the space vacated by the forward translation of the mandibular condyle in a patient who had a dermis-fat graft placed 5 years previously
Result Obtained by the End of 6 Months
TM Joint appears little wider and volume appears normal.
Iso to High Signal areas (free fat dermis graft) are noted within the graft replaced region.
Disc space is well outlined, both anteriorly and superiorly showing the free fat dermis graft being well placed.
Free fat graft is seen superiorly as well as anteriorly and posteriorly in the region of the ressected condyle of the mandible. Free fat graft occupies almost the entire joint space of operated joint except the disc space.
Result Obtained After 4 Years Follow up
TM Joint appears wider and volume appears larger.
High signal areas (free fat dermis graft) are noted within the graft replaced region with little low intense signal area in the middle portion.
Free fat graft seen in a diffuse manner.
Free fat graft is seen superiorly as well as anteriorly and posteriorly in the region of the ressected condyle of the mandible.
Free fat graft occupies almost 2/3rd of the space of operated joint.
Discussion
This study shows the MRI findings seen in the operated TMJ by the end of 6 months and 5 years. MRI is a potent additional tool for diagnosis if there is a second grade or more of synovial fluid. It can reduce arthroscopic interventions for diagnostic purposes.
From the investigation using MRI it was found that the grafted fat reduced in size to about 33 % of the original size after 1 year. While the signal intensity of the grafted fat was lower than that of normal subcutaneous fat tissue in the first 6 weeks following surgery, the intensity had recovered to normal status by 1 year after surgery. Ultimately, the MRI results showed that the grafted fat was alive.
MRI investigation suggests the survival of free fat dermis grafts implanted into bony cavities other than bone. The average size of the fat graft was found to be almost the same, whether free fat graft was implanted during less than 6 months ago or more than 4 years previously.
The presence of dermis was impossible to demonstrate based on the limited current MRI technology available. The most remarkable finding of this study was the survival of the dermis fat graft, which was seen in and around all the joints. The fat that was transplanted to the TMJ was not vascularised, and still the graft appeared to have survived in all cases. The fate of transplanted fat may be linked to adipose precursor cells which are distributed widely in connective tissues throughout the adult body [3]. Such cells in the surrounding connective tissue can proliferate and mature into fat cells depending on the micro-environment [3].
When a miniscule piece of non-vascularised fat was included in the sealed chamber, new fat formed and filled the space. The presence of transplanted fat grafts within a connective tissue environment stimulates endogenous precursor cells to proliferate and differentiate to form more adipose tissue [4].
MRI finding showed that the signal intensity of the dermis fat graft diminishes over the first 6 weeks but then strengthens, which may suggest that the grafted dermis fat tissue disappears and is gradually replaced by new adipose tissue laid down by the stimulated adipose precursor cells found in the connective tissues surrounding the TMJ [5].
Intermittent compressive forces of the joint may act as a negative influence on the growth and maintenance joint of fat tissue within the joint space itself [1].
Only 2 out of the 5 examined TM joints demonstrated any evidence of fat within the actual joint space. For the purpose of this investigation, the radiological joint space was determined as the 120-degree arc that extended from the mid body of the condylar head to the glenoid fossa in the sagittal and coronal planes [1].
The grey inter-positional material was detected in 2 TMJ joints, and the radiological opinion was that it could represent fibrotic scar or granulation tissue.
Conclusion
The present MRI study was designed to evaluate the fate of the free fat dermis graft placed as interpositional material in TMJ gap arthroplasty and its characteristic changes on these images obtained could be correlated as:-
Free fat dermis graft was present in similar quantities surrounding all joints whether it is newly operated or 5 years back.
The presence of dermis was impossible to demonstrate based on the current MRI technology available. The most remarkable finding of this study was the survival of the fat graft, which was evident in the MRI images and around all the joints. The fat that was transplanted to the TMJ was not vascularised but still it appeared to have survived in all cases.
It is speculated that the fat graft itself may be replaced by adipogenesis from the surrounding connective tissue bed, which may help explain the consistent finding of fat surrounding all TMJs that were scanned with MRI. Intermittent compressive forces within the temporo-mandibular joint space may act as a negative impact on growth and maintenance of fat tissue within the joint itself which was transplanted.
The grey interpositional material was detected in 2 TMJ joints, and the radiological opinion was that it could represent fibrotic scar or granulation tissue.
When free fat dermis graft is placed as interpositional material of gap arthroplasty the graft occupied the entire TM joint and prevented from recurrent ankylosis. The graft placed was helpful in normal to functioning of the temperomandibular joint.
Conflict of interest
None.
Contributor Information
A. Thangavelu, Phone: 09443244213, Email: omfsvat@hotmail.com
S. Thiruneelakandan, Email: thiruneel@hotmail.com
C. Hari Prasath, Email: Hcprasath@yahoo.co.in.
Dhruba Chatterjee, Email: dhruba.chatterjee@gmail.com.
References
- 1.Dimitroulis G, Trost N, Morrison W. The radiological fate of dermis-fat grafts in the human temporomandibular joint using magnetic resonance imaging. Int J Oral Maxillofac Surg. 2008;37:249–254. doi: 10.1016/j.ijom.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 2.Dimitroulis G. The use of dermis grafts after discectomy for internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 2005;63:173–178. doi: 10.1016/j.joms.2004.06.051. [DOI] [PubMed] [Google Scholar]
- 3.Kawaguchi N, Toriyama K, Nicodemou-Lena E, Inou K, Torii S, Kitagawa Y. De novo adipogenesis in mice at the site of injection of basement membrane and basic fibroblast growth factor. Proc Natl Acad Sci USA. 1998;95:1062–1066. doi: 10.1073/pnas.95.3.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly JL, Findlay MW, Knight KR, Penington A, Thompson EW, Messina A, Morrison WA. Contact with existing adipose tissue is inductive for adipogenesis in matrigel. Tissue Eng. 2006;12:2041–2047. doi: 10.1089/ten.2006.12.2041. [DOI] [PubMed] [Google Scholar]
- 5.Kanamori M, Kawaguchi Y, Ohmori K, Kimura T, Md HT, Matsui H. The fate of autogenous free-fat grafts after posterior lumbar surgery: part 1. A postoperative serial magnetic resonance imaging study. Spine. 2001;26:2258–2263. doi: 10.1097/00007632-200110150-00018. [DOI] [PubMed] [Google Scholar]
- 6.Wessely MA, Young MF. Magnetic resonance imaging of the temporomandibular joint. Clin Chiropr. 2008;11:37–44. doi: 10.1016/j.clch.2008.02.002. [DOI] [Google Scholar]


