Abstract
Introduction
Orthognathic surgery involves making several osteotomies. Any osteotomies leads to varying degrees of post-operative swelling. The aim of this study was to evaluate the effectiveness of anti-edema drugs for the control of edema, using Digitizer 3D™ for measuring soft-tissue thickness, in patients who underwent bimaxillaryorthognathic surgery.
Materials and Methods
In this double-blinded, randomized, control trial, 24 patients (study group: 12 patients, control group: 12 patients) in whom bimaxillary orthognathic surgery was indicated, were included in this study. All swelling measurements were expressed as total 3-D area of the landmarks (cm2) in T0 pre-operative, T1 first day after surgery, T2 fourth day after surgery, T3 4 months after surgery. For each patient we compared, by adding left and right area, the increase of swelling between T1–T0, T2–T0 and T1–T3.
Results
The differences T0–T1 are highly significant (p < 0.01) between group 1 or study group (treated with Venoplant®) and group 2 (control group); the differences T0–T2 are significant (p < 0.05) between group 1 (treated with Venoplant®) and group 2 (control group). The differences T1–T3 are significant (p < 0.05) between group 1 (treated with Venoplant®) and group 2 (control group).
Discussion
The present study suggests that Venoplant® significantly decreases postoperative edema in orthognathic surgery, thus precluding long-term corticosteroid use.
Keywords: Orthognathic surgery, Edema, Anti-edema drugs, Digitizer 3-D
Introduction
Orthognathic surgery involves making several osteotomies in order to reposition the jaw in the right position. Any osteotomy, which involves the reflection of a full thickness mucoperiosteal flap, leads to varying degrees of post-operative swelling. An extensive swelling can compromise the surgical outcome as well as patient recovery and the airway [1].
Several methods have been developed to measure facial soft tissue thickness in cadavers and in live patients [2]. Traditionally, facial soft tissue measurements have been studied using the needle depth probing method on cadavers [3]. Several imaging-based methods for measuring living facial soft-tissue thickness have been reported [4–9].
In the present study a MakerBot® Digitizer 3D™ was used to assess accurate volume measurements.
In maxillofacial surgery, various methods are used to decrease postoperative swelling, including pressure dressings, ice packs, and placement of drains. Another reported method to decrease postoperative edema in orthognathic surgery is using the endoscopic approach for ramus osteotomy [10]. Medical management of swelling in orthognathic surgery is confined mainly to the use of steroids or non-steroidal anti-inflammatory drugs. The use of systemic enzyme therapy (SET) for edema control in orthognathic surgery is not well established in the literature [11].
We used in this study tablets containing active ingredients (Diosmin, Coumarin, Centella: Venoplant®) that promote a physiological improvement of microcirculation and trophism of capillary tone after traumatology.
The aim of this study was to evaluate the effectiveness of anti-edema drugs for the control of edema, using Digitizer 3D™ for measuring soft-tissue thickness, in patients who underwent bimaxillaryorthognathic surgery.
Materials and Methods
Patients
In this double-blinded, randomized, control trial, 24 patients (study group: 12 patients, control group: 12 patients) in whom bimaxillary orthognathic surgery was indicated, were included.
Before surgery each patient alternatively was randomly included in the study group (treated with Venoplant® and corticosteroid) or in the control group (treated with corticosteroid).
This study was in accordance with the ethical standards and all participants signed an informed consent agreement.
Inclusion criteria were as follows: patients selected had no preexisting medical conditions or medications that would influence their ability to undergo surgery or alter their wound healing after surgery.
All cases were diagnosed as skeletal Class III including mandibular prognathism and/or maxillary retrognathism on the basis of a lateral cephalogram analysis and the patients underwent orthognathic surgery.
The study group consisted of 9 men (average age 18–34 years) and 15 women (average age 19–27 years) with Class III malocclusion.
Control groups consisted of 3 men (average age 18–30 years) and 9 women (average age 20–27 years) and without drug assumption.
Tablets
Venoplant® tablets (Aesculapius, Brescia, Italy) contains Diosmin 300 mg, Coumarin in sweet clover tit. 25 %, triterpenes in Centella tit. 45 %.
Diosmin is a flavanoide used to improve the tone of venous vessels, reduce excessive microvascular permeability decrease the formation of edema.
Coumarin in sweet clover stimulates the action of proteolytic enzymes in macrophages, which are the main cause of edema.
Centella is a plant with substances that stimulate the connective tissue tropism and control microvascular permeability.
All patients in the 2 groups received corticosteroids for 2 days (betamethasone f 4 mg ev × 2/day 1, betamethasone f 4 mg ev/day 2). In addition, patients in the study group received Venoplant® (1 cpr/die × 4 days).
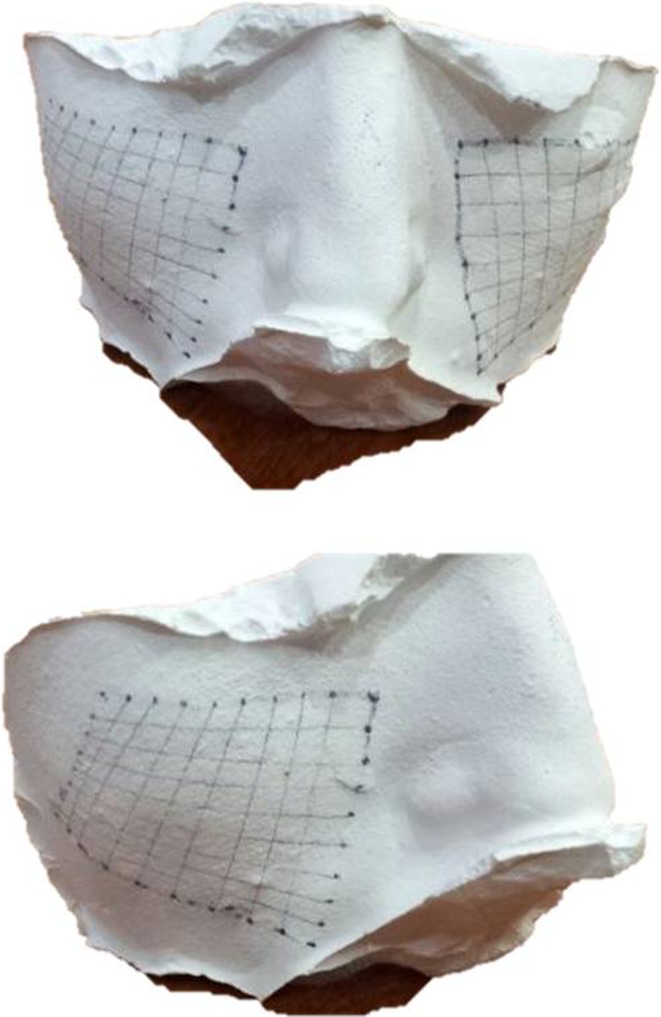
Selection of Landmarks
Bilaterally, in each patient the area between four lines: (1) the line passing through the tragus of the ear and the ipsilateral labial commissure; (2) the line passing through 1 cm below the eyelid with the open eye and the tragus ipsilateral; (3) the line perpendicular to the Frankfurt plane and passing through the tail of the eyebrow; (4) the line passing through the medial canthus and the ipsilateral labial commissure, was selected (Figs. 1, 2).
Fig. 1.

Area landmarks, frontal view
Fig. 2.

Area landmarks, lateral view
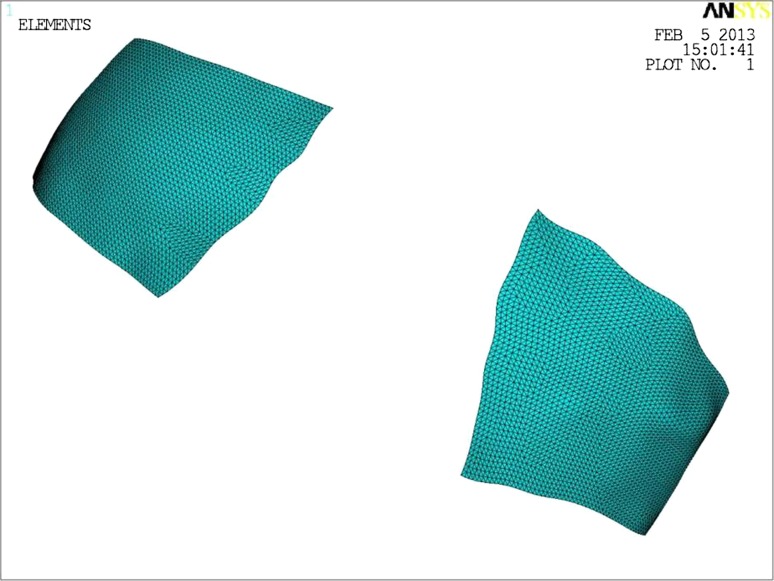
Measurements
Area After the selection of landmarks a silicone mask with VynilPolysiloxane Impression Material Putty (Express STD Putty, 3 M ESPE, Pioltello, Milan—Italy) for the area of interest was made, then we created a plaster cast to conform to the mask previously formed (Fig. 3). The mold was processed by the program Digitizer 3-D™ (MakerBot®) (Fig. 4) of Aerospace Engineering (S.U.N. University of Naples) for the precise measurement of the three-dimensional area (Fig. 5).
Fig. 3.
The mold of the area
Fig. 4.
Digitizer 3-D™
Fig. 5.
The mold was processed by the program Digitizer 3-D™
Pain Pain scores were assessed using a 10 level visual analogue scale (VAS) of 100 mm, representing all pain sensations from none to maximum; where 0 indicates no pain, 5 moderate pain and 10 worst pain possible. Patients were asked to place a mark along the line that corresponded to the amount of pain they were experiencing.
Trismus Maximal mouth opening was recorded measuring the maximum inter-incisal distance using calipers.
All measurements were performed at four specific time points: T0 pre-operative, T1 directly one day after surgery, T2 fourth day after surgery.
All measurements for area were performed at four specific time points: T0 pre-operative, T1 directly one day after surgery, T2 four day after surgery, T3 4 months after surgery.
All measurements were recorded by a single operator (U.T.) and supervised by a single engineer (A.S.).
Surgical Technique
All patients underwent bimaxillaryorthognathic surgery (Le Fort I osteotomy plus bilateral sagittal split osteotomy plus genioplasty). The duration of surgery and the cheek retraction time were recorded for all patients. As a part of the routine premedication protocol, 1 dose of dexamethasone 6 mg was injected in all patients 30 min before surgery. A dose of dexamethasone 4 mg was repeated after 3 and 6 h in the same day of surgery, dexamethasone 4 mg was repeated first day after surgery, dexamethasone 2 mg was repeated 2 days after surgery. One tablet/die of Venoplant® was assumed 1 day before surgery and 4 days after surgery only by the patients of the study group. No surgical drains were placed and ice packs were given to all patients.
Results
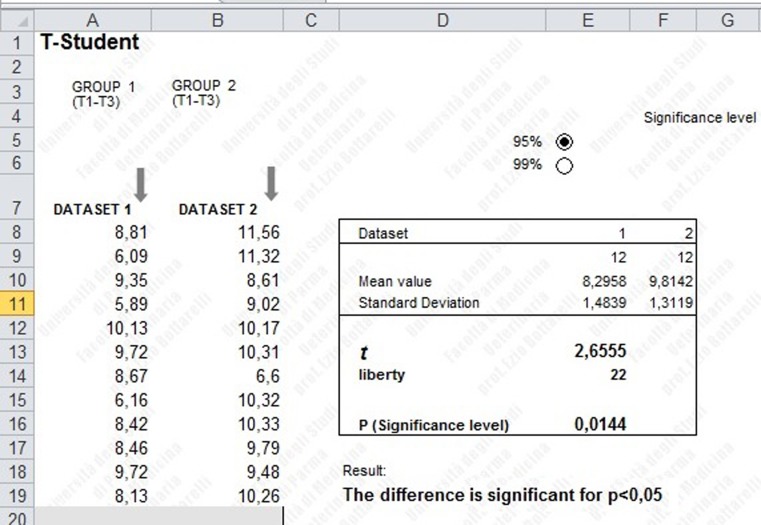
The data were analyzed and compared using the T Student test (Table 1, Fig. 6).
Table 1.
Area measurements
| Group 1 (cm2): study group | Group 2 (cm2): control group | |||
|---|---|---|---|---|
| Right area | Left area | Right area | Left area | |
| Pt 1 pre | 21.26 | 20.18 | 23.60 | 23.46 |
| 1 day-post | 26.17 | 25.43 | 29.72 | 29.70 |
| 4 day-post | 24.60 | 23.90 | 29.01 | 29.12 |
| 4 months-post | 21.47 | 21.32 | 23.98 | 23.88 |
| Pt 2 pre | 16.01 | 15.58 | 17.80 | 16.93 |
| 1 day-post | 20.90 | 20.50 | 23.12 | 23.03 |
| 4 day-post | 20.73 | 20.22 | 22.67 | 22.51 |
| 4 months-post | 17.89 | 17.42 | 17.80 | 17.03 |
| Pt 3 pre | 23.28 | 23.70 | 16.30 | 17.12 |
| 1 day-post | 28.97 | 29.12 | 22.18 | 22.91 |
| 4 day-post | 28.00 | 28.50 | 21.76 | 21.89 |
| 4 months-post | 24.21 | 24.53 | 18.12 | 18.36 |
| Pt 4 pre | 17.18 | 18.12 | 19.41 | 19.28 |
| 1 day-post | 21.24 | 21.90 | 24.47 | 24.33 |
| 4 day-post | 19.83 | 20.12 | 23.65 | 23.61 |
| 4 months-post | 18.54 | 18.71 | 20.00 | 19.78 |
| Pt 5 pre | 19.91 | 18.06 | 24.12 | 23.89 |
| 1 day-post | 25.12 | 25.06 | 30.21 | 30.11 |
| 4 day-post | 23.86 | 23.83 | 29.33 | 29.18 |
| 4 months-post | 20.18 | 19.87 | 25.14 | 25.01 |
| Pt 6 pre | 16.25 | 16.17 | 21.78 | 22.14 |
| 1 day-post | 22.03 | 21.62 | 27.12 | 27.49 |
| 4 day-post | 20.98 | 20.50 | 26.88 | 27.01 |
| 4 months-post | 17.00 | 16.93 | 22.12 | 22.18 |
| Pt 7 pre | 23.12 | 23.45 | 16.15 | 16.77 |
| 1 day-post | 27.58 | 28.04 | 21.38 | 21.53 |
| 4 day-post | 26.02 | 26.85 | 18.82 | 18.84 |
| 4 months-post | 23.39 | 23.56 | 17.89 | 18.42 |
| Pt 8 pre | 21.09 | 20.98 | 16.72 | 17.04 |
| 1 day-post | 26.15 | 26.24 | 22.18 | 22.81 |
| 4 day-post | 25.33 | 25.31 | 21.87 | 22.13 |
| 4 months-post | 23.21 | 23.02 | 17.28 | 17.39 |
| Pt 9 pre | 17.21 | 17.67 | 21.82 | 21.53 |
| 1 day-post | 21.89 | 22.05 | 26.99 | 26.93 |
| 4 day-post | 21.02 | 21.63 | 26.08 | 26.06 |
| 4 months-post | 17.69 | 17.83 | 21.84 | 21.75 |
| Pt 10 pre | 23.00 | 23.17 | 23.71 | 24.02 |
| 1 day-post | 28.37 | 28.42 | 29.55 | 30.01 |
| 4 day-post | 26.80 | 26.83 | 28.43 | 28.58 |
| 4 months-post | 24.02 | 24.31 | 24.78 | 24.99 |
| Pt 11 pre | 24.36 | 24.12 | 16.44 | 16.12 |
| 1 day-post | 29.85 | 29.88 | 21.56 | 21.69 |
| 4 day-post | 29.12 | 29.22 | 20.84 | 20.86 |
| 4 months-post | 25.01 | 25.00 | 16.98 | 16.79 |
| Pt 12 pre | 21.76 | 22.32 | 18.30 | 17.91 |
| 1 day-post | 27.12 | 26.80 | 24.12 | 23.88 |
| 4 day-post | 25.15 | 25.03 | 23.56 | 23.06 |
| 4 months-post | 22.65 | 23.14 | 18.90 | 18.84 |
Fig. 6.
T-Student analysis by Excel (Microsoft®)
Area All swelling measurements were expressed as total 3-D area of the landmarks (cm2) in T0 pre-operative, T1 first day after surgery, T2 fourth day after surgery, T3 4 months after surgery. For each patient we compared, by adding left and right area, the increase of swelling between T1–T0 and T2–T0 and the differences of the swelling at the peak time and original with the cheek forms four months after the operation. All the differences had a Gaussian distribution. The differences T0–T1 are highly significant (p < 0.01) between group 1 or study group (treated with Venoplant®) and group 2 (control group); the differences T0–T2 are significant (p < 0.05) between group 1 (treated with Venoplant®) and group 2 (control group); the differences T1–T3 are significant (p < 0.05) between group 1 (treated with Venoplant®) and group 2 (control group) (Table 2).
Table 2.
Statistical analysis by T Student
| Mean value | SD | p value | |||
|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 1 | Group 2 | ||
| Area T1-T0 | 10.0267 | 11.2217 | 1.1908 | 0.8066 | p < 0.01 |
| 99 % | |||||
| Area T2-T0 | 7.9775 | 9.4492 | 1.7023 | 1.6698 | p < 0.05 |
| 95 % | |||||
| Area T1-T3 | 8.2958 | 9.8142 | 1.4839 | 1.3119 | p < 0.05 |
| 95 % | |||||
In group 1 (study group) the mean value of the difference between the total/bilateral area 1 day after surgery (T1) and before surgery (T0) was 10.0267 cm2, in group 2 (control group) the mean value of the difference between the total/bilateral area 1 day after surgery (T1) and before surgery (T0) was 11.2217 cm2; in group 1 (study group) the mean value of the difference between the total/bilateral area 4 days after surgery (T2) and before surgery (T0) was 7.9775 cm2, in group 2 (control group) the mean value of the difference between the total/bilateral area 4 days after surgery (T2) and before surgery (T0) was 9.4492 cm2; in group 1 (study group) the mean value of the difference between the total/bilateral area 1 day after surgery (T1) and four months after surgery (T3) was 8.2958 cm2, in group 2 (control group) the mean value of the difference between the total/bilateral area 1 day after surgery (T1) and 4 months after surgery (T3) was 9.8142 cm2.
Pain Comparing the study group and the control group results for pain scores assessed using a 10 level visual analogue scale (VAS) were not significant (p > 0.20) because the main value of VAS in study group was 7,2 at T1 and 6,8 at T2, VAS in control group was 7,3 at T1and 6,7 at T2.
Trismus Mouth opening values did not differ significantly in both groups and the values were not significant (p > 0.20) because the main value of mouth opening in study group was 2,9 cm at T1 and 3,1 cm at T2, mouth opening in control group was 3 cm at T1 and 3,1 at T2.
Discussion
Some clinical trials have advocated the use of steroids for edema control in orthognathic surgery [12]. In contrast, a longer use of steroids is associated with multiple problems, such as skin changes, increased serum glucose, adrenal suppression, disturbed wound healing, and impaired immunity [1].
Various non-medical methods also have been used for edema control, each with limitations. The pressure dressing has limited application because of the complex anatomy of the maxillofacial region. Also, excessive pressure in the lower third of face and neck may cause severe discomfort and can compress the airway in some patients. The placement of extraoral drains in such aesthetic procedures is not justified because of residual scar formation. Moreover, intraoral drains are not well tolerated by most patients. The use of ice bags to control edema after a maxillofacial procedure also has limited application [13].
Various methods have been suggested in the literature to measure the amount of tissue edema. Methods for measuring and quantifying such a 3-dimensional phenomenon include 3-dimensional laser scanning and magnetic resonance imaging [14, 15].
In the present study we used Digitizer 3-D™ under standardized conditions for the measurement of the area representative of the entire swelling. It is a simple, safe and accurate method. It is not widely available but we choose it for this study because this method is very accurate and we needed the precise measurement of the area.
There are various parameters that significantly influence the amount of soft-tissue swelling in orthognathic surgery. To decrease the influence of variables, such as type of surgery, extent of dissection, and duration of tissue manipulation, on the extent of swelling, these variables were standardized in the 2 groups. Hence, all patients included in the study underwent bimaxillaryorthognathic surgery (Le Fort I osteotomy plus bilateral sagittal split osteotomy plus genioplasty). All surgeries were performed under similar surgical and anesthesia conditions such that the technique, time, and tissue manipulation during surgeries were standardized. Also, all patients were mobilized to a sitting position within 24 h.
All patients in the 2 groups received corticosteroids. In addition, patients in the study group received a 4-day course of Venoplant®. In this study, the authors noted a significant difference in volume between the 2 groups. Thus, a direct correlation was observed between the use of Venoplant® and the decrease in postoperative swelling. In literature the edema of midface is lower than the edema of the mandibular region after orthognathic surgery [11].
However, there are no clinical trials that suggest the possible benefit of this therapy in maxillofacial surgery, in particular orthognathic surgery. The use of Venoplant® is correlated, for the midface region, to a minor post-operatory edema and a faster decrease of edema in the 4 days following the surgery.
We achieved that the our values were statistically significant using a T-student analysis by Excel format (Microsoft®) that showed a lower pick increasement of the edema especially the day after surgery and a lower edema 4 days after surgery.
This therapy is usually well tolerated by patients. However, some patients may complain of odorless and colorless feces, a sensation of fullness, flatulence, and occasional episodes of nausea with much higher dosages. These complaints were not noted in the study group of patients.
The present study suggests that Venoplant® significantly decreases postoperative edema in orthognathic surgery, thus precluding long-term corticosteroid use.
Conflict of interest
All authors disclose any financial and personal relationships with other people or organisations that could inappropriately influence their work.
References
- 1.Cheginia S, Dhariwal DK. Review of evidence for the use of steroids in orthognathic surgery. Br J Oral Maxillofac Surg. 2012;50:97. doi: 10.1016/j.bjoms.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 2.Sahni D, Singh SG, Jit I, et al. Facial soft tissue thickness in Northwest Indian adults. Forensic Sci Int. 2008;179:137. doi: 10.1016/j.forsciint.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Suazo GIC, Cantın LM, Zavando MDA, et al. Comparisons in soft-tissue thicknesses on the human face in fresh and embalmed corpses using needle puncture method. Int J Morphol. 2008;26:165. [Google Scholar]
- 4.Kim DK, Ruprecht A, Wang G, et al. Accuracy of facial soft tissue thickness measurements in personal computer-based multiplanar reconstructed computed tomography images. Forensic Sci Int. 2005;155:28. doi: 10.1016/j.forsciint.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 5.George RM. The lateral craniographic method of facial reconstruction. J Forensic Sci. 1987;32:1305. [Google Scholar]
- 6.Phillips VM, Smuts NA. Facial reconstruction: utilization of computerized tomography to measure facial tissue thickness in a mixed racial population. Forensic Sci Int. 1996;83:51. doi: 10.1016/0379-0738(96)02010-5. [DOI] [PubMed] [Google Scholar]
- 7.El-Mehallawi IH, Soliman EM. Ultrasonic assessment of facial soft tissue thicknesses in adult Egyptians. Forensic SciInt. 2011;117:99. doi: 10.1016/S0379-0738(00)00453-9. [DOI] [PubMed] [Google Scholar]
- 8.Lam EW, Hannam AG, Wood WW, et al. Imaging orofacial tissues by magnetic resonance. Oral Surg Oral Pathol Oral Radiol Endod. 1989;68:2. doi: 10.1016/0030-4220(89)90106-0. [DOI] [PubMed] [Google Scholar]
- 9.FourieZ Damstra J, Gerrits PO, et al. Accuracy and reliability of facial soft tissue depth measurements using cone beam computer tomography. Forensic Sci Int. 2010;199:9. doi: 10.1016/j.forsciint.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Williams WB, Abukawa H, Shuster V et al (2003) A comparison of postoperative edema after intraoral vs. endoscopic mandibular ramus osteotomy. J Oral Maxillofac Surg 61(8 suppl.): 61a
- 11.Shetty W, Mohan A. A prospective, randomized, double-blind, placebo-controlled clinical trial comparing the efficacy of systemic enzyme therapy for edema control in orthognathic surgery using ultrasound scan to measure facial swelling. J Oral Maxillofac Surg. 2013;71:1261–1267. doi: 10.1016/j.joms.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 12.Weber CR, Griffin JM. Evaluation of dexamethasone for reducing postoperative oedema and inflammatory response after orthognathic surgery. J Oral Maxillofac Surg. 1994;52:35. doi: 10.1016/0278-2391(94)90010-8. [DOI] [PubMed] [Google Scholar]
- 13.Nusair YM. Local application of ice bags did not affect postoperative facial swelling after oral surgery in rabbits. Br J Oral Maxillofac Surg. 2007;45:48. doi: 10.1016/j.bjoms.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Harrison JA, Nixon MA, Fright WR, Snape L. Use of hand-held laser scanning in the assessment of facial swelling: a preliminary study. Br J Oral Maxillofac Surg. 2004;42:8. doi: 10.1016/S0266-4356(03)00192-X. [DOI] [PubMed] [Google Scholar]
- 15.Llewelyn J, Ryan M, Santosh C. The use of magnetic resonance imaging to assess swelling after the removal of third molar teeth. Br J Oral Maxillofac Surg. 1996;34:419. doi: 10.1016/S0266-4356(96)90099-6. [DOI] [PubMed] [Google Scholar]