Abstract
Objective
This study examined a multivariate model of the relationship between caregiver strain and adolescent diabetes illness outcomes in a sample of caregivers of adolescents in chronically poor metabolic control (Hba1c ≥ 8.0% at enrollment and for previous 12 months). Caregiver mental health symptoms were hypothesized to mediate the relationship between caregiver strain and adolescent illness management behavior and metabolic control. Caregivers’ perceptions of social support and their level of responsibility for diabetes care tasks were hypothesized to be directly related to caregiver strain and indirectly to caregiver mental health symptoms.
Method
One hundred forty-six caregiver-adolescent dyads completed baseline measures of caregiver strain, responsibility for diabetes care, social support, mental health symptoms, and illness management behavior. Adolescent metabolic control was also assessed.
Results
Findings from structural equation modeling suggested that caregiver strain was directly and positively associated with caregiver mental health symptoms which mediated the relationship to adolescent diabetes management behavior and metabolic control. Caregivers’ responsibility for diabetes care tasks was directly related to caregiver strain and indirectly to caregiver mental health, but caregiver perceptions of social support was not.
Conclusions
These findings suggest that caregiver strain is an important dimension of the caregiving context of diabetes. Clinicians and researchers should consider how caregiving strain, responsibility for illness management, and mental health symptoms might be impacting children’s diabetes care behavior and diabetes health when working with and designing interventions for adolescents with diabetes.
Insulin-dependent diabetes (IDDM) is a chronic metabolic disorder that affects roughly 3.2 out of every 1,000 children under the age of eighteen in the United States and 5.6 of every 1,000 children age twelve to seventeen1. Effective diabetes management requires a complex and demanding daily regimen of blood glucose monitoring, insulin administration, dietary regulation, and regular exercise that requires daily motivation and self-control on the part of the child2 and support and guidance from the family3. Declines in diabetes management and metabolic control during adolescence due to both biological4,5 and behavioral mechanisms6,7,8,9 are well documented. Addressing declines in illness management during adolescence is critical due to the fact that illness management is strongly associated with poor metabolic control10,11,12 which, in turn, is predictive of poor metabolic control in adulthood13,14,15 and is linked to negative consequences including the onset of diabetes complications16 and increased health care costs17.
Because the majority of diabetes care occurs in the home, the primary responsibility for effective management falls on the family and places increased demands on caregivers3,18. Caregiver strain is one of the many negative consequences of these increased caregiving demands, however, the implications of such strain for children’s diabetes management has not been examined. Often referred to as “burden of care” or “family impact”19, caregiver strain differs from general psychological stress by referring to the specific “demands, responsibilities, difficulties, and negative psychic consequences of caring for relatives with special needs”20. Primarily studied in the caregivers of children with severe emotional disturbance20,21,22,23,24, caregiving strain has also been studied in several pediatric chronic illness populations including hemophilia25, Joubert syndrome26, cerebral palsy27, Tourette’s disorder28,29, developmental disabilities30,31, traumatic brain injury32, and, recently, diabetes33,34,35. These studies suggest that caregiver strain is also associated with child age24, caregiver age35, single- versus two-parent families25, and family income24,35.
Research examining the consequences of caregiver strain has focused nearly exclusively on caregivers’ own outcomes, primarily the relationship between caregiver strain and caregiver mental health symptoms. The findings from this literature are mixed. Several studies offer only correlational support for the caregiver strain-mental health relationship26,29,32. Of those testing directional relationships, some have found support for the hypothesis that mental health symptoms predict strain25,36 while others suggest that strain predicts mental health27,37,38. Brannan and Heflinger22 tested these two alternative models of caregiver strain and mental health and found a significant relationship when caregiver strain was hypothesized to predict caregiver mental health. In contrast, when caregiver mental health was hypothesized to predict strain the relationship was nonsignificant. Therefore, in the present study, we test a model consistent with these findings.
Caregiver stain has also been linked to several child-level variables including child mental health37,39,40, outpatient service utilization21,41,42, and, most recently, metabolic control in children with diabetes. Of the three studies that have examined caregiver strain and metabolic control, two linked lower levels of caregiver strain to better metabolic control33,34 while the third was unable to link strain and metabolic control40. All three examined caregiving strain in primarily white (≥ 87%), two-parent (≥ 76%), middle-class families caring for children with adequate metabolic control (8.4 ≤ mean HbA1c ≤ 8.8). This study extends the literature by examining caregiver strain, adolescent illness management behavior, and metabolic control in a sample of adolescents with poorly controlled diabetes, a group where caregiver strain might be particularly high.
Few studies have examined factors that buffer caregiver strain. The stress prevention model of social support suggests that social support tempers the impact of stressful events43. For caregivers of children with diabetes, social support may alleviate caregiver strain through the provision of instrumental (i.e., assisting with specific caregiving tasks) and emotional support. The social support-caregiver strain relationship has been empirically supported in studies of caregivers of children with Tourette’s disorder28, developmental disabilities31, and those at risk for ADHD42 as well as in the broader caregiver strain literature38,44.
While social support may decrease caregiver strain, caregivers with greater responsibility for daily diabetes care might experience higher levels of caregiving strain. For example, the number of caregiving tasks was associated with strain in a study of caregivers of elderly family members35. No studies of pediatric caregivers have examined caregiver responsibility and strain, but several have documented the problem of premature transfer of responsibility from caregiver to adolescent45,46. One explanation for this phenomenon may be that caregivers increase adolescents’ diabetes care responsibilities prematurely due to the strain associated with being responsible for the child’s diabetes care. Thus, this study will examine whether social support buffers strain while increased caregiver responsibility for diabetes care potentiates strain.
The working hypotheses guiding this investigation were (1) caregiver strain is negatively related to caregiver mental health symptoms and indirectly negatively related to adolescent illness management behavior and, through illness management behavior, metabolic control, (2) caregiver perceptions of social support are negatively related to caregiver strain directly and caregiver mental health symptoms indirectly, (3) caregiver responsibility is positively related to caregiver strain directly and caregiver mental health symptoms indirectly. Covariates of study variables were examined based on associations previously identified in literature; diabetes type was also included as a covariate to control for the differences in disease type.
Method
Participants
Participants were 146 caregiver-adolescent dyads participating in a larger intervention trial targeting diabetes illness management in adolescents with chronically poor metabolic control. To be eligible for the study, adolescents had to be 1) between 10 and 17 years of age, 2) diagnosed for at least one year with type 1 or 2 diabetes requiring insulin management, 3) have a current and a mean HbA1c during the year prior to study entry of 8.0% or higher, 4) have no known developmental delay or other chronic medical condition, 5) reside in a home-like setting, and 6) written and verbal English fluency. Five hundred thirteen families were screened for participation, of which 238 were ineligible and 36 could not be contacted. Fifty-two of the remaining 239 refused to participate and 10 withdrew prior to randomization resulting in a 26% refusal rate. One hundred forty-six adolescents and their families comprised the final sample. Data for the present study were drawn from the baseline data collection prior to randomization to treatment condition. The primary caregiver of the child, defined by the family as the person who most often helps the child with his/her diabetes care, completed the parent measures.
Adolescents were 14.2 (SD = 2.3) years old on average and just over half were female (56.2%, n = 82). Three-quarters were African American (77.4%, n = 113), a fifth were White (19.9%, n = 29), and the remaining 2.8% endorsed the bi-racial or other categories (n = 4). The majority of adolescents had been diagnosed with type 1 diabetes (89.7%, n = 131) and, at the time of study entry, adolescents had been living with diabetes for an average of 4.7 (SD = 3.0) years. Two-thirds were on intensive insulin regimens (injected insulin: 56.8%, n = 83; insulin infusion pump: 13.0%, n = 19) while a third were on a conventional mixed injection regimen (26.7%, n = 39). The mean HbA1c level was 11.7% (SD = 2.5%).
Caregivers were 41.4 (SD = 7.9) years old on average. The majority were biological mothers (84.9%, n = 124), 8.2% (n = 12) were biological fathers, and the remaining caregivers were three adoptive mothers, three female legal guardians, three other female caregivers, and one step-father. More than half of the caregivers were single parents (58.9%, n = 86). The median family income was between $30,000 and $39,999 per year with families reporting incomes from less than $10,000 to greater than $100,000 per year. Overall, the demographics of the sample were representative of the diverse population served by the clinic where subjects were recruited.
Procedure
Families were recruited from a university-affiliated diabetes clinic in a children’s hospital located in a large Midwestern city. The diabetes clinic staff approached eligible families during routine diabetes clinic visits or during inpatient admissions. Interested families signed releases of information that were relayed to the research staff. The diabetes clinic staff mailed letters of introduction to all eligible families not able to be contacted in person. Disinterested families could opt out while the research staff followed up with the remaining families to assess their interest in participation. The research protocol was approved by the university’s Human Investigations Committee as well as the hospital’s research review board. All caregivers provided informed consent and adolescents informed assent. Data collection occurred during an in-home visit by a trained research assistant. Participants received $50 for completing the baseline assessment.
Measures
Caregiver Strain
The Caregiver Strain Questionnaire (CGSQ)20 assesses three dimensions of caregiver strain. Objective strain (CGSQ-OBJ; 11 items) refers to the extent to which caregivers perceive observable negative events for their family related to their child’s illness such as disrupted family routines and loss of personal time. Subjective internalized strain (CGSQ-INT; 6 items) is the degree of inwardly directed negative feelings such as worry, guilt, and feeling tired. Subjective externalized strain (CGSQ-EXT; 4 items) captures the experience of negative feelings directed toward the child including anger, resentment, or embarrassment. Caregivers consider the past six months using a five-point Likert scale ranging from 1, not at all, to 5, very much a problem. Previous research has confirmed the factor structure of the measure and the internal consistency of the scales, objective = .92, internalized strain = .86, and externalized strain = .7420. In this study, the internal consistency was 0.86 for objective strain, 0.79 for subjective internalized strain, and 0.57 for subjective externalized strain.
Caregiver Mental Health Symptoms
The Brief Symptom Inventory 18 (BSI-18)47 is an abbreviated measure of psychological status in persons over 18 years of age. The BSI 18 measures three primary symptom dimensions: somatization (BSI-SOM), depression (BSI-DEP), and anxiety (BSI-ANX). Higher scores on the BSI 18 indicate more symptoms. Internal consistency for the current sample was 0.81 for the somatization scale, 0.82 for depression, and 0.72 for anxiety.
Social Support
The Diabetes Social Support Questionnaire-Parent (DSSQ-Parent) is an investigator-developed measure of diabetes-specific social support adapted from the Diabetes Social Support Questionnaire-Friends48 that captures caregivers’ perceptions of social support received from the person in their support network who supports them the most with diabetes care. Items cover five areas of diabetes care: insulin administration (2 items), blood glucose testing (5 items), exercise (4 items), and emotional support (3 items). Each item is presented using a two-part Likert scale format; the first part asks “How often does your support person…” do each supportive behavior, 0, never, 1, less than two times a month, 2, twice a month, 3, once a week, 4, several times a week, or 5, at least once a day. The caregiver then rates the supportiveness of each behavior, “How supportive (helpful) is this to you?”, with a 3-point Likert scale, 0, not at all, 1, somewhat, or 2, very. The frequency of each behavior is multiplied by its supportiveness to calculate an individualized item score49. Mean individualized scores can range from 0 to 10 with higher scores reflecting greater perceived support. In this study, Cronbach’s alpha was .91 indicating good internal consistency. The DSSQ-Parent demonstrates some evidence of discriminant validity as it correlated at a low level with youth ratings of family support (r = .24, p ≤ .01) and caregiver ratings of health care provider support (r = .18, p ≤ .05)50.
Caregiver Responsibility
The Diabetes Family Responsibility Questionnaire (DFRQ)51 assesses responsibility for diabetes management behavior. Caregivers indicate whether they are primarily responsible for 20 discrete diabetes care tasks, they share the tasks with their child, or whether the child is primarily responsible. A caregiver responsibility summary score is constructed by tallying the number of tasks for which caregivers report primary responsibility52. Scores ranged from 0 to 20 where higher scores indicate greater caregiver responsibility. Cronbach’s alpha was .81.
Illness Management
Two self-report and one objective measure of illness management were collected to capture the multifaceted nature of this behavior53. The Diabetes Management Scale (DMS)54 measures a broad range of diabetes management behaviors, including insulin management, dietary management, blood glucose monitoring, and symptom response. Adolescents (DMS-A) rated their own diabetes management behavior and caregivers (DMS-CG) completed a parallel form assessing their child’s behavior. The original DMS was developed before the widespread use of intensive insulin regimens and, hence, a subset of items are not appropriate for adolescents on intensive insulin regimens (71.6%, n = 101). Therefore, adolescents (and their caregivers) prescribed traditional mixed injection regimens responded to 18 questions and those on intensive insulin regimens responded to 10 items. Regardless of insulin regimen, respondents indicate “What percent of the time do you/your child (e.g., take your/his/her insulin)” using a 0–100% scale. The mean of all items is calculated to derive an overall diabetes management summary score. The original instrument demonstrated adequate reliability and validity55,56. Internal consistency in the current sample was 0.60 for adolescents on traditional insulin regimens, 0.63 for adolescents on intensive insulin, 0.81 for caregiver reports of adolescents on traditional insulin regimens, and 0.71 for caregiver reports of adolescents on intensive insulin. An objective measure of illness management was the frequency of blood glucose monitoring (BGM). Glucose meter data were downloaded and an average daily testing frequency was calculated for the fourteen-day period immediately preceding data collection. Blood glucose monitoring is the behavior most closely linked to metabolic control in pediatric populations57.
Metabolic Control
Metabolic control was assessed using hemoglobin A1c (HbA1c), an indirect and retrospective measure of average blood glucose over the previous two to three months. Values were obtained using the FDA-approved Accubase A1c test kit58. The test uses a capillary tube blood collection method instead of venipuncture making it appropriate for home-based data collection by non-phlebotomists. The blood sample is analyzed using high performance liquid chromatography (HPLC). HbA1c obtained by the Accubase test is comparable to HbA1c obtained from venous whole blood as established in several studies, including a pediatric sample, r = .98758.
Statistical Analyses
Questionnaire-level data were missing on only one measure, blood glucose monitoring (2.8%, n = 4). These data were estimated using full-information maximum likelihood estimation in Amos, 19.059, the statistical software package used to implement the multivariate analyses. All descriptive and bivariate analyses were conducted with SPSS Statistics60.
The study hypotheses were tested using structural equation modeling (SEM) which permits the simultaneous examination of multiple relationships in a single analytical model. SEM was implemented with Amos 19.059 using a one-step modeling procedure61. The following benchmarks were used to evaluate the SEM model62,63,64: that the likelihood ratio Χ2 test of model fit was nonsignificant, the ratio of the Χ2 to df ≤ 2, the comparative fit index (CFI) was > .95, and the root mean square error of approximation (RMSEA) was ≤ .08. The adequacy of the measurement model was then assessed by evaluating the factor loadings of each observed indicator variable on its latent construct. Factor loadings were determined adequate if they were at least .30 and statistically significant. Finally, the standardized parameter estimates of the structural model were assessed. The alpha level was set at .05 for all analyses.
Results
Descriptive and Bivariate Statistics
Table 1 presents the results of the descriptive and bivariate statistics. Higher levels of caregiver strain were related to greater caregiver mental health symptoms across both measures’ subscales with one exception; externalized strain was unrelated to symptoms of anxiety. Greater caregiver strain (objective, r = −.282, p ≤ .001; internalized, r = −.342, p ≤ .001; externalized, r = −.302, p ≤ .001) was related to poorer caregiver-reported illness management behavior; greater objective (r = −.185, p ≤ .05) and internalized strain (r = −.281, p ≤ .001) were related to poorer adolescent-reported illness management behavior, and greater internalized strain was related to a lower frequency of blood glucose monitoring (r = −.213, p ≤ .05). Caregiver strain was unrelated to metabolic control. Greater objective (r = .218, p ≤ .01) and internalized subjective caregiver strain (r = .226, p ≤ .01) was related to greater caregiver responsibility for diabetes care tasks. Greater internalized (r = −.217, p ≤ .01) and externalized subjective caregiver strain (r = −.189, p ≤ .05) was associated with lower levels of support.
Table 1.
Descriptive Statistics and Correlation Matrix of Study Variables
| DFRQ | DSSQ-Parent | CGSQ-OBJ | CGSQ-EXT | CGSQ-INT | BSI-SOM | BSI-DEP | BSI-ANX | DMS-A | DMS-CG | BGM | HbA1c | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DSSQ-Parent | −.217** | |||||||||||
| CGSQ-OBJ | .219** | −.069 | ||||||||||
| CGSQ-EXT | .010 | −.189* | .248** | |||||||||
| CGSQ-INT | .226** | −.217** | .569*** | .281*** | ||||||||
| BSI-SOM | .106 | −.022 | .246** | .162* | .272*** | |||||||
| BSI-DEP | .087 | −.157 | .447*** | .284*** | .376*** | .543*** | ||||||
| BSI-ANX | .140 | −.091 | .354*** | .118 | .341*** | .607*** | .671*** | |||||
| DMS-A | −.063 | .206* | −.185* | −.075 | −.281*** | −.237** | −.261* | −.202* | ||||
| DMS-CG | .014 | .128 | −.282*** | −.302*** | −.342*** | −.260** | −.332*** | −.138 | .475*** | |||
| BGM | −.019 | .139 | −.040 | −.088 | −.213* | −.142 | −.155 | −.077 | .528*** | .369*** | ||
| HbA1c | −.104 | .006 | .020 | .103 | .083 | .002 | .072 | −.051 | −.347*** | −.221** | −.429*** | |
| Diabetes Typea | .010 | −.099 | −.118 | .186* | −.091 | .021 | −.141 | −.129 | −.131 | −.132 | −.305** | .126 |
| Adolescent Age | −.255** | −.210* | −.042 | .171* | .103 | .031 | .136 | −.016 | −.268** | −.341*** | −.403*** | .296*** |
| Caregiver Age | .013 | −.035 | .006 | .093 | .001 | −.105 | −.115 | −.155 | −.012 | .014 | −.036 | −.006 |
| Caregiver Raceb | .028 | −.101 | .117 | .079 | .123 | .025 | .079 | .180* | .131 | .000 | .292*** | −.309*** |
| Caregiver Marital Statusc | −.007 | .163* | −.147 | −.089 | −.143 | −.193* | −.187* | −.127 | .226** | .121 | .109 | −.128 |
| Family Income | −.001 | .050 | −.005 | .047 | −.003 | −.177* | −.129 | −.068 | .140 | .157 | .266** | −.257** |
| M | 6.10 | 3.46 | 1.66 | 1.34 | 2.91 | 3.21 | 3.16 | 2.53 | 67.61 | 67.59 | 2.33 | 11.67 |
| SD | 3.42 | 3.14 | 0 .63 | 0 .50 | .94 | 4.14 | 3.92 | 3.15 | 15.75 | 16.67 | 1.52 | 2.53 |
| α | .81 | .91 | .86 | .57 | .79 | .81 | .82 | .72 | .60a .63b |
.81a .71b |
Note: DFRQ = Diabetes Family Responsibility Questionnaire; DSSQ-Parent = Diabetes Social Support Questionnaire-Parent; CGSQ = Caregiver Strain Questionnaire: OBJ = Objective Strain Scale, INT = Internalized Strain Scale, EXT = Externalized Strain Scale; BSI = Brief Symptom Inventory: SOM = Somatization Scale, DEP = Depression Scale, ANX = Anxiety Scale; DMS = Diabetes Management Scale: A = Adolescent-Report, CG = Caregiver-Report; BGM = Blood Glucose Monitoring; HbA1c = Metabolic control
Diabetes type was dummy coded: 0 = Type 1, 1 = Type 2
Caregiver race dummy coded: 0 = African American, 1 = Other Races
Caregiver marital status was dummy coded: 0 = single-parent, 1 = two-parent
p ≤ .05,
p ≤ .01,
p ≤ .001
Associations among potential covariates known to be associated with study variables were also assessed; these results are presented in Table 1. Type 2 diabetes (dummy coded where 0 = Type 1, 1 = Type 2) was related to greater externalized caregiver strain (rpb = .186, p ≤ .05) and lower levels of blood glucose monitoring (rpb = −.305, p ≤ .001). Older adolescent age was related to less caregiver responsibility (r = −.255, p ≤ .01), less caregiver social support (r = −.210, p ≤ .05), greater externalized caregiver strain (r = .171, p ≤ .05), poorer illness management behavior across all three measures (adolescent-report, r = −.268, p ≤ .01; caregiver report, r = −.341, p ≤ .001; blood glucose monitoring, r = −.403, p ≤ .001), and poorer metabolic control (r = .296, p ≤ .001). Caregiver age was unrelated to study variables at the bivariate level, but caregiver African American race (dummy coded where 0 = African American, 1 = Other races) was significantly related to lower levels of anxiety symptoms (rpb = .180, p ≤ .05), lower levels of blood glucose monitoring (rpb = .292, p ≤ .001), and poorer metabolic control (rpb = −.309, p ≤ .001). Single parenting caregivers were more likely to have lower social support (rpb = .163, p ≤ .05), higher levels of somatic (rpb = −.193, p ≤ .05) and depression symptoms (rpb = −.187, p ≤ .05), and teens who reported poorer illness management (rpb = .226, p ≤ .01). Lower family income was associated with increased caregiver somatic symptoms (rpb = −.177, p ≤ .05), lower levels of blood glucose monitoring (rpb = .266, p ≤ .01), and poorer metabolic control (rpb = −.257, p ≤ .01).
Structural Equation Modeling
A structural equation model with three latent constructs (caregiver strain, caregiver mental health symptoms, and illness management behavior), each comprised of three indicators, was fit to the variance/covariance matrix using a maximum likelihood solution to model relationships between variables. The model had two exogenous variables (caregiver responsibility and social support) predicting four endogeneous variables (caregiver strain → caregiver mental health symptoms → illness management behavior → and metabolic control). Four covariates (diabetes type, adolescent age, caregiver marital status, and family income) were added to the model based on the empirical literature and the results of the bivariate analyses in Table 1.
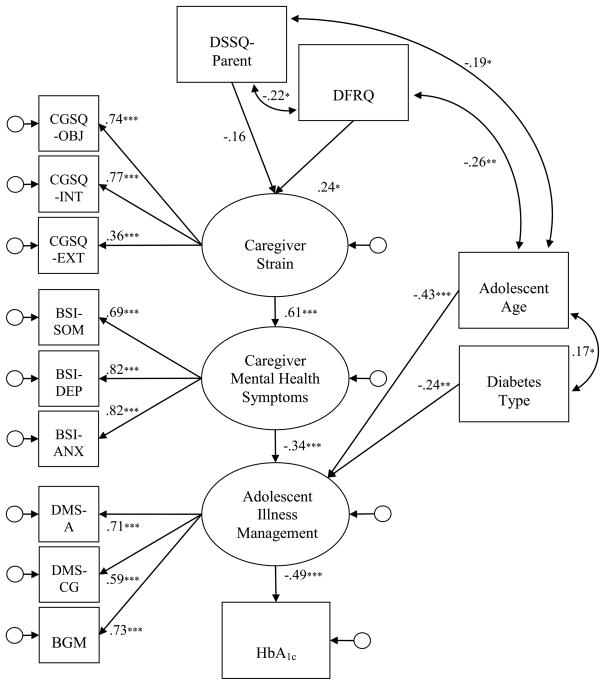
This model demonstrated adequate fit [X2(86, N = 146) = 126.485, p = .003; CFI = 0.919; RMSEA = 0.057] but there were several nonsignificant covariate pathways. Caregiver marital status and family income were not significantly related to any study variable in the model and, hence, were removed. The following nonsignificant covariances were also eliminated: adolescent age and caregiver strain, diabetes type and caregiver strain, and adolescent age and HbA1c. The model was retested and the fit of the revised model was adequate [X2(71, N = 146) = 114.740, p = .001; CFI = 0.909; RMSEA = 0.065]. Indicator factor loadings for all three latent constructs were all at least .3 and statistically significant. Figure 1 presents these results.
Figure 1.
Final model of caregiver responsibility, social support, strain, and mental health symptoms on adolescents’ illness management behavior and health status (standardized regression weights). Model fit indices: X2(71, N = 146) = 114.740, p = .001; CFI = 0.909; RMSEA = 0.065. Note: DFRQ = Diabetes Family Responsibility Questionnaire; DSSQ-Parent = Diabetes Social Support Questionnaire-Parent; CGSQ = Caregiver Strain Questionnaire: OBJ = Objective Strain Scale, INT = Internalized Strain Scale, EXT = Externalized Strain Scale; BSI = Brief Symptom Inventory: SOM = Somatization Scale, DEP = Depression Scale, ANX = Anxiety Scale; DMS = Diabetes Management Scale: A = Adolescent-Report, CG = Caregiver-Report; BGM = Blood Glucose Monitoring; HbA1c = Metabolic control
*p ≤ .05, **p ≤ .01, ***p ≤ .001
Counter to study hypotheses, social support was not significantly related to caregiver strain. All other hypothesized pathways were significant. Sobel’s test of indirect effects provided further support for the study hypotheses. Caregiver strain mediated the relationship between caregiver responsibility for illness management and caregiver mental health symptoms (2.284, p < .012). Caregiver mental health symptoms mediated the relationship between caregiver strain and adolescent illness management behavior (−2.944, p < .002). Adolescent illness management behavior mediated the relationship between caregiver mental health symptoms and HbA1c (2.904, p < .002). The final model explained 39% of the variance in caregiver mental health symptoms, 7% of the variance in illness management, and 24% of the variance in adolescent metabolic control.
Discussion
Research on the strain caregivers experience while caring for a chronically ill child has focused primarily on caregivers’ own health outcomes. Two of the three studies that have examined caregiver strain among the caregivers of children with diabetes have linked caregiver strain to children’s metabolic control33,34; however, all three studies targeted primarily white, two-parent, middle-class families caring for a child with diabetes in average metabolic control. Hence, this study is the first to link caregiver strain to adolescents’ diabetes management behavior in a sample of ethnically diverse, single parent, low income families caring for a child with poorly controlled diabetes.
The findings from the multivariate analyses partially supported the study hypotheses. First, caregiver strain was directly and positively associated with caregiver mental health symptoms. This is a strong and consistent finding in the caregiver strain literature25,26,27,29,32,36,37,38. Caregiver mental health symptoms mediated the relationship between caregiver strain and adolescent diabetes management behavior, which, in turn, was associated with adolescent metabolic control.
Two correlates of caregiver strain were hypothesized: caregiver responsibility for diabetes management tasks and social support provided to the caregiver. As the number of diabetes management tasks caregivers were responsible for increased, so did their reports of caregiver strain. This finding is consistent with at least one study of caregiver strain in the adult literature35 and represents the first in the pediatric literature to directly associate caregiver responsibility for chronic illness tasks to caregiver strain. The strain caregivers experience when they are primarily responsible for their children’s diabetes care tasks might lead them to transfer care tasks to their adolescents before the adolescents are fully ready and capable of accepting responsibility for their diabetes care, especially among caregivers of children with a history of chronic poor illness management behavior. However, further research is needed to understand how responsibility for diabetes care tasks impacts caregiver strain.
Counter to the hypotheses and despite a bivariate relationship, social support was unrelated to caregiver strain in the multivariate model. This finding is inconsistent with previously published research that has linked social support and caregiver strain in both the pediatric28,31 and adult literature38,44. This finding might be partly explained by the study sample. The caregivers in this study were largely low income, single parents of adolescents with chronically, poorly controlled diabetes targeted for treatment intervention. Caregivers reported a low level of social support on average (M = 3.46, SD = 3.14, out of a possible range of 0 – 10) and one-third reported no support for their child’s diabetes care50. Low levels of social support may be more common among caregivers of children with poor diabetes control; hence, a more diverse sample of caregivers reporting a greater range of social support is needed to examine the relationship between social support and caregiver strain among caregivers of adolescents with diabetes. It may also be that the type of social support is important. This study examined diabetes-specific instrumental social support primarily; only three items assessed emotional support. Thompson and colleagues44 found social support in the form of social participation, i.e., engaging in fun and recreational social activities, was more strongly related to caregiver strain than instrumental, such as material aid or physical assistance, or emotional support among caregivers of the elderly. Alternatively, non-supportive behaviors (e.g., behaviors that are actively detrimental to the child’s care) might be more important than supportive behaviors in the context of caregiver strain. In a study of caregivers of children with a number of chronic illnesses, caregivers reported non-supportive behaviors from extended family members to be a significant source of distress that often outweighs any positive benefit of support behavior from the same or other family members65. Further research is needed to examine the impact of both supportive and non-supportive behaviors on caregiver strain and diabetes outcomes.
Despite a bivariate association with study variables marital status and family income were unrelated in the multivariate model. Similarly, adolescent age was unrelated to caregiver strain and metabolic control but remained significantly associated with adolescent illness management behavior. These findings are counter to previous research suggesting that single-parenting caregivers66 and lower income families67 are more vulnerable to parenting stresses including caregiver strain35 than their two-parenting, higher income counterparts. However, it also provides increased confidence in the study findings by suggesting that caregivers with greater responsibility for diabetes care tasks experience higher levels of caregiver strain regardless of whether it is from a spouse residing in the home or from other sources such as extended family members or friends.
Study limitations include the nature, size, and representativeness of the sample. Participants in this study were 146 caregiver-adolescent (between 10 and 17 years) dyads recruited for an intervention study to treat poorly controlled diabetes. Although parenting a child with very poor diabetes control could potentially increase caregivers’ diabetes-related strain, the caregivers in this study reported strain at levels consistent with those reported in previous studies of caregivers of children with diabetes in average control33,34,40. Nonetheless, this sample size is relatively small for testing a structural model with three latent constructs. Replication of the results with larger, more diverse samples is needed in order to confidently generalize the findings to the broader population of caregivers of adolescents with diabetes.
This study is also limited by the use of cross-sectional data that preclude making causal inferences. Although the model of caregiver strain developed in this study was derived from the empirical caregiver strain literature22, alternative models of the relationships among study variables are plausible. For example, future studies could test alternative models in which caregiver mental health symptoms predict caregiver strain. Researchers could also consider testing models where the relationship between caregiver strain and adolescent diabetes outcomes, both illness management behavior and metabolic control, are partially mediated. However, disentangling the complex relationship between these variables requires prospective longitudinal research designs with an adequately sized sample.
Despite these limitations, this research informs our understanding of the caregiving context of diabetes. This study suggests that greater illness management responsibility is linked to greater caregiving strain, and though caregiver strain, greater mental health symptoms among caregivers of adolescents with diabetes. Understanding these linkages provides clinicians and researchers with critical intervention points. The strain and distress associated with having primary responsibility for diabetes care tasks might be one reason underlying the premature transfer of responsibility from caregiver to adolescents so often noted. Clinicians working with adolescents with diabetes should be cognizant of this relationship and assist caregivers in identifying strategies to ensure that diabetes care tasks are completed that also minimize the strain and distress caregivers may experience as a consequence of bearing this responsibility. Future research examining these relationships with research designs that enable the formal testing of causal relationships would advance the field as well as improve the quality of life of both caregivers and children living with chronic illness.
Acknowledgments
This project was supported grant #R01 DK59067 from the National Institute of Diabetes, Digestive and Kidney Diseases.
Footnotes
Conflicts of Interest
None of the authors have conflicts of interest related to the work described in the manuscript.
Contributor Information
April Idalski Carcone, Pediatric Prevention Research Center, Carman and Ann Adams Department of Pediatrics, Wayne State University, Detroit, Michigan
Deborah A. Ellis, Pediatric Prevention Research Center, Carman and Ann Adams Department of Pediatrics, Wayne State University, Detroit, Michigan
Sylvie Naar-King, Pediatric Prevention Research Center, Carman and Ann Adams Department of Pediatrics, Wayne State University, Detroit, Michigan
References
- 1.Lee JM, Herman WH, McPheeters ML, et al. An epidemiologic profile of children with diabetes in the U.S. Diabetes Care. 2006;29:420. doi: 10.2337/diacare.29.02.06.dc05-2182. [DOI] [PubMed] [Google Scholar]
- 2.Dovey-Pearce G, Doherty Y, May C. The influence of diabetes upon adolescent and young adult development: A qualitative study. British Journal of Health Psychology. 2007;12:75. doi: 10.1348/135910706X98317. [DOI] [PubMed] [Google Scholar]
- 3.Wysocki T, Greco P. Social support and diabetes management in childhood and adolescence: Influence of parents and friends. Current Diabetes Reports. 2006;6:117. doi: 10.1007/s11892-006-0022-y. [DOI] [PubMed] [Google Scholar]
- 4.Amiel S, Sherwin R, Simonson D, et al. Impaired insulin action in puberty. A contributing factor to poor glycemic control in adolescents with diabetes. N Eng J Med. 1986;315:215. doi: 10.1056/NEJM198607243150402. [DOI] [PubMed] [Google Scholar]
- 5.Moran A, Jacobs DRJ, Steinberger J, et al. Insulin resistance during puberty: Results from clamp studies in 357 children. Diabetes. 1999;48:2039. doi: 10.2337/diabetes.48.10.2039. [DOI] [PubMed] [Google Scholar]
- 6.Johnson SB. Adherence behaviors and health status in childhood diabetes. In: Holmes CS, editor. Neuropsychological and behavioral aspects of diabetes. New York, NY: Springer-Verlag; 1990. p. 30. Vol ch ed. [Google Scholar]
- 7.Thomas AM, Peterson L, Goldstein D. Problem Solving and Diabetes Regimen Adherence by Children and Adolescents with IDDM in Social Pressure Situations: A Reflection of Normal Development. Journal of Pediatric Psychology. 1997;22:541. doi: 10.1093/jpepsy/22.4.541. [DOI] [PubMed] [Google Scholar]
- 8.Weissberg-Benchell J, Glasgow AM, Tynan WD, et al. Adolescent Diabetes Management and Mismanagement. Diabetes Care. 1995;18:77. doi: 10.2337/diacare.18.1.77. [DOI] [PubMed] [Google Scholar]
- 9.Johnson SB, Perwien AR, Silverstein JH. Response to hypo- and hyperglycemia in adolescents with type I diabetes. Journal of Pediatric Psychology. 2000;25:171. doi: 10.1093/jpepsy/25.3.171. [DOI] [PubMed] [Google Scholar]
- 10.Morris AD, Boyle DI, McMahon AD, et al. Adherence to insulin treatment, glycemic control, and ketoacidosis in insulin-dependent diabetes mellitus. The Lancet. 1997;350:1505. doi: 10.1016/s0140-6736(97)06234-x. [DOI] [PubMed] [Google Scholar]
- 11.Haller M, Stalvey M, Silverstein J. Predictors of control of diabetes: Monitoring may be the key. The Journal of Pediatrics. 2004;144:660. doi: 10.1016/j.jpeds.2003.12.042. [DOI] [PubMed] [Google Scholar]
- 12.Levine BS, Anderson BJ, Butler DA, et al. Predictors of glycemic control and short-term adverse outcomes in youth with type 1 diabetes. Journal of Pediatrics. 2001;139:197. doi: 10.1067/mpd.2001.116283. [DOI] [PubMed] [Google Scholar]
- 13.Forsander G, Persson B, Sundelin J, et al. Metabolic control in children with insulin-dependent diabetes mellitus 5 y after diagnosis. Early detection of patients at risk for poor metabolic control. Acta Paediatr. 1998;87:857. doi: 10.1080/080352598750013635. [DOI] [PubMed] [Google Scholar]
- 14.Seiffge-Krenke I, Stemmler M. Coping with everyday stress and links to medical and psychosocial adaptation in diabetic adolescents. Journal of Adolescent Health. 2003;33:180. doi: 10.1016/s1054-139x(02)00707-3. [DOI] [PubMed] [Google Scholar]
- 15.Wysocki T, Hough BS, Ward KM, et al. Diabetes mellitus in the transition to adulthood: Adjustment, self-care, and health status. Journal of Development and Behavioral Pediatrics. 1992;13:194. [PubMed] [Google Scholar]
- 16.Diabetes Control & Complications Trial Research Group. Effect of intensive treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes control and complications trial. Journal of Pediatrics. 1994;125:177. doi: 10.1016/s0022-3476(94)70190-3. [DOI] [PubMed] [Google Scholar]
- 17.Delamater AM, Albrecht DR, Postellon DC, et al. Racial differences in metabolic control of children and adolescents with type 1 diabetes mellitus. Diabetes Care. 1991;14:20. doi: 10.2337/diacare.14.1.20. [DOI] [PubMed] [Google Scholar]
- 18.Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28:186. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 19.McCabe KM, Yeh M, Lau A, et al. Racial/ethnic differences in caregiver strain and perceived social support among parents of youth with emotional and behavioral problems. Mental Health Services Research. 2003;5:137. doi: 10.1023/a:1024439317884. [DOI] [PubMed] [Google Scholar]
- 20.Brannan AM, Heflinger CA, Bickman L. The Caregiver Strain Questionnaire: Measuring the impact on the family of living with a child with serious emotional disturbance. Journal of Emotional and Behavioral Disorders. 1997;5:212. [Google Scholar]
- 21.Brannan AM. The role of caregiver strain and other family variables in determining children’s use of mental health services. Journal of Emotional and Behavioral Disorders. 2003;11:77. [Google Scholar]
- 22.Brannan AM, Heflinger CA. Distinguishing caregiver strain from psychological distress: Modeling the relationships among child, family, and caregiver variables. Journal of Child and Family Studies. 2001;10:405. [Google Scholar]
- 23.Kang EJ, Brannan AM, Heflinger CA. Racial differences in reports of caregiver strain among caregivers of children with emotional and behavioral problems. Journal of Child and Family Studies. 2005;14:43. [Google Scholar]
- 24.Heflinger CA, Taylor-Richardson KD. Caregiver Strain in Families of Children with Serious Emotional Disturbance: Does Relationship to Child Make a Difference? Journal of Family Social Work. 2004;8:27. [Google Scholar]
- 25.Varekamp I, Suurmeijer P, Rosendaal F, et al. Family burden in families with a hemophilic child. Family Systems Medicine. 1990;8:291. [Google Scholar]
- 26.Luescher JL, Dede DE, Gitten JC, et al. Parental Burden, Coping, and Family Functioning in Primary Caregivers of Children With Joubert Syndrome. Journal of Child Neurology. 1999;14:642. doi: 10.1177/088307389901401004. [DOI] [PubMed] [Google Scholar]
- 27.Raina P, O’Donnell M, Rosenbaum P, et al. The Health and Well-Being of Caregivers of Children With Cerebral Palsy. Pediatrics. 2005;115:e626. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- 28.Schoeder CE, Remer R. Perceived social support and caregiver strain in caregivers of children with Tourette’s Disorder. Journal of Child and Family Studies. 2007;16:888. [Google Scholar]
- 29.Cooper C. Psychological morbidity and caregiver burden in parents of children with Tourette’s disorder and psychiatric comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1370. doi: 10.1097/01.CHI.0000085751.71002.48. [DOI] [PubMed] [Google Scholar]
- 30.Serr J, Mandleco BL, Roper SO. Linkages between Depression and Caregiver Burden in Parents Raising Children with Disabilities. 2007. [Google Scholar]
- 31.Oh H, Lee E-KO. Caregiver Burden and Social Support among Mothers Raising Children with Developmental Disabilities in South Korea. International Journal of Disability, Development and Education. 2009;56:149. [Google Scholar]
- 32.Wade SL, Taylor HG, Drotar D, et al. Family Burden and Adaptation During the Initial Year After Traumatic Brain Injury in Children. Pediatrics. 1998;102:110. doi: 10.1542/peds.102.1.110. [DOI] [PubMed] [Google Scholar]
- 33.Cunningham NR, Vesco AT, Dolan LM, et al. From Caregiver Psychological Distress to Adolescent Glycemic Control: The Mediating Role of Perceived Burden around Diabetes Management. Journal of Pediatric Psychology. 2011;36:196. doi: 10.1093/jpepsy/jsq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Butler DA, Zuehlke JB, Tovar A, et al. The impact of modifiable family factors on glycemic control among youth with type 1 diabetes. Pediatric Diabetes. 2008;9:373. doi: 10.1111/j.1399-5448.2008.00370.x. [DOI] [PubMed] [Google Scholar]
- 35.Montgomery RJV, Gonyea JG, Hooyman NR. Caregiving and the Experience of Subjective and Objective Burden. Family Relations. 1985;34:19. [Google Scholar]
- 36.Calderón C, Gómez-López L, Martínez-Costa C, et al. Feeling of Burden, Psychological Distress, and Anxiety among Primary Caregivers of Children with Home Enteral Nutrition. Journal of Pediatric Psychology. 2011;36:188. doi: 10.1093/jpepsy/jsq069. [DOI] [PubMed] [Google Scholar]
- 37.Sales E, Greeno C, Shear MK, et al. Maternal Caregiving Strain as a Mediator in the Relationship between Child and Mother Mental Health Problems. Social Work Research. 2004;28:211. [Google Scholar]
- 38.Baillie V, Norbeck JS. Stress, social support, and psychological distress of family caregivers of the elderly. Nursing Research. 1988;37:217. [PubMed] [Google Scholar]
- 39.Bussing R, Gary FA, Mason DM, et al. Child temperament, ADHD, and caregiver strain: Exploring relationships in an epidemiological sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:184. doi: 10.1097/00004583-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 40.Leishman JM. Individual and Family Predictors of the Caregiver Burden of Parents Rearing a Child with Diabetes. Brigham Young University; 2010. [Google Scholar]
- 41.Angold A, Messer SC, Stangl D, et al. Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health. 1998;88:75. doi: 10.2105/ajph.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bussing R, Zima BT, Gary FA, et al. Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:842. doi: 10.1097/01.CHI.0000046876.27264.BF. [DOI] [PubMed] [Google Scholar]
- 43.Barrera M. Distinctions between social support concepts, measures, and models. American Journal of Community Psychology. 1986;14:413. [Google Scholar]
- 44.Thompson EH, Futterman AM, Gallagher-Thompson D, et al. Social support and caregiving burden in family caregivers of frail elders. Journal of Gerontology. 1993;48:S245. doi: 10.1093/geronj/48.5.s245. [DOI] [PubMed] [Google Scholar]
- 45.Palmer DL, Berg CA, Wiebe DJ, et al. The role of autonomy and pubertal status in understanding age differences in maternal involvement in diabetes responsibility across adolescence. Journal of Pediatric Psychology. 2004;29:35. doi: 10.1093/jpepsy/jsh005. [DOI] [PubMed] [Google Scholar]
- 46.Wysocki T, Taylor A, Hough BS, et al. Deviation from developmentally appropriate self-care autonomy: Association with diabetes outcomes. Diabetes Care. 1996;19:119. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]
- 47.Derogatis LR. BSI 18 manual. Minneapolis, MN: Pearson; 2004. [Google Scholar]
- 48.Bearman KJ, La Greca AM. Assessing friend support of adolescents’ diabetes care: The Diabetes Social Support Questionnaire-Friends Version. Journal of Pediatric Psychology. 2002;27:417. doi: 10.1093/jpepsy/27.5.417. [DOI] [PubMed] [Google Scholar]
- 49.La Greca AM, Bearman KJ. The diabetes social support questionnaire-family version: Evaluating adolescents’ diabetes-specific support from family members. Journal of Pediatric Psychology. 2002;27:665. doi: 10.1093/jpepsy/27.8.665. [DOI] [PubMed] [Google Scholar]
- 50.Idalski Carcone A, Ellis DA, Weisz A, et al. Social Support for Diabetes Illness Management: Supporting Adolescents and Caregivers. Journal of Developmental and Behavioral Pediatrics. 2011;32 doi: 10.1097/DBP.0b013e31822c1a27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Anderson BJ, Auslander WF, Jung KC, et al. Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology. 1990;15:477. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- 52.Dashiff CJ. Self- and Dependent-Care Responsibility of Adolescents with IDDM and their Parents. Journal of Family Nursing. 2003;9:166. [Google Scholar]
- 53.Quittner AL, Modi AC, Lemanek KL, et al. Evidence-based assessment of adherence to medical treatments in pediatric psychology. Journal of Pediatric Psychology. 2008;33:916. doi: 10.1093/jpepsy/jsm064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Frey MA, Ellis DA, Naar-King S, et al. Diabetes management in adolescents in poor metabolic control. The Diabetes Educator. 2004;30:647. doi: 10.1177/014572170403000416. [DOI] [PubMed] [Google Scholar]
- 55.Frey MA, Denyes MJ. Health and illness self-care in adolescents with IDDM: A test of Orem’s theory. ANS Advances in Nursing Science. 1989;12:67. doi: 10.1097/00012272-198910000-00009. [DOI] [PubMed] [Google Scholar]
- 56.Schilling LS, Grey M, Knafl K. A review of measures of self-management of type 1 diabetes by youth and their parents. The Diabetes Educator. 2002;28:796. doi: 10.1177/014572170202800520. [DOI] [PubMed] [Google Scholar]
- 57.Levine B-S, Anderson BJ, Butler DA, et al. Predictors of glycemic control and short-term adverse outcomes in youth with type 1 diabetes. The Journal of Pediatrics. 2001;139:197. doi: 10.1067/mpd.2001.116283. [DOI] [PubMed] [Google Scholar]
- 58.Diabetes Technologies Inc. AccuBase A1c™ Test Kit. Thomasville, GA: Diabetes Technologies Inc; 2004. laboratory test kit. [Google Scholar]
- 59.Amos [computer program]. 19.0.0 19.0.0. Chicago, IL: 2010. [Google Scholar]
- 60.IBM SPSS Statistics [computer program]. 19.0.1 19.0.1. Chicago, IL: 2011. [Google Scholar]
- 61.Ratner PA, Bottorff JL, Johnson JL. Structural Equation Modeling. In: Brink PJ, Wood MJ, editors. Advanced design in nursing research. Thousand Oaks: Sage; 1998. Vol ch ed. [Google Scholar]
- 62.Kline RB. Principles and practice of structural equation modeling. New York: Guilford; 2005. [Google Scholar]
- 63.Arbuckle JL. Amos 18 User’s Guide. Crawfordville, FL: Amos Development Corporation; 2009. [Google Scholar]
- 64.Schreiber JB, Nora A, Stage FK, et al. Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research. 2006;99:323. [Google Scholar]
- 65.Patterson JM, Garwick AW, Bennett FC, et al. Social support in families of children with chronic conditions: Supportive and nonsupportive behaviors. Journal of Developmental and Behavioral Pediatrics. 1997;18:383. doi: 10.1097/00004703-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 66.Mullins LL, Wolfe-Christensen C, Chaney JM, et al. The Relationship Between Single-Parent Status and Parenting Capacities in Mothers of Youth with Chronic Health Conditions: The Mediating Role of Income. Journal of Pediatric Psychology. 2011;36:249. doi: 10.1093/jpepsy/jsq080. [DOI] [PubMed] [Google Scholar]
- 67.Canning RD, Harris ES, Kelleher KJ. Factors Predicting Distress Among Caregivers to Children with Chronic Medical Conditions. Journal of Pediatric Psychology. 1996;21:735. doi: 10.1093/jpepsy/21.5.735. [DOI] [PubMed] [Google Scholar]