Abstract
Background
Personal health records (PHRs) are web based tools that help people to access and manage their personalized medical information. Although needs for PHR are increasing, current serviced PHRs are unsatisfactory and researches on them remain limited. The purpose of this study is to show the process of developing Seoul National University Bundang Hospital (SNUBH)'s own PHR system and to analyze consumer's use pattern after providing PHR service.
Methods
Task force team was organized to decide service range and set the program. They made the system available on both mobile application and internet web page. The study enrolled PHR consumers who assessed PHR system between June 2013 and June 2014. We analyzed the total number of users on a monthly basis and the using pattern according to each component.
Results
The PHR service named Health4U has been provided from June 2013. Every patient who visited SNUBH could register Health4U service and view their medical data. The PHR user has been increasing, especially they tend to approach via one way of either web page or mobile application. The most frequently used service is to check laboratory test result.
Conclusion
For paradigm shift toward patient-centered care, there is a growing interest in PHR. This study about experience of establishing and servicing the Health4U would contribute to development of interconnected PHR.
Keywords: Personal Health Records, Electronic Health Records, Patient-Centered Care
INTRODUCTION
Contemporarily, the development of information technology, including the Internet, allows people to easily obtain and share specialized information. Consumers can access information from anywhere and at any time, and produce and distribute their information through computers or mobile devices. O'Reilly1) called such change 'Web 2.0,' which can be summarized into three words: participation, sharing, and openness a paradigm shift from a producer-centric approach to a consumer-centric approach has also affected the medical field, leading to a paradigm shift to a patient-centric medicine.2) At the same time, the importance of personal health records (PHR) are also emerging.3)
PHR refers to an individual's lifelong health record, and combines medical information provided by various medical institutions. The PHR is comprehensive because it also includes the medical record made by the individual and the necessary tools to for record management. This record improves patients' accessibility to medical information and enhances communication and relationships with medical teams. Consequently, the patient can actively participate in his or her treatment, increasing treatment compliance and enhancing treatment efficiency and quality.4)
With the introduction of PHR, it is expected that the hospital-centric paradigm will shift to the patient-centric paradigm.5) In the existing hospital setting, patients' medical records are primarily kept in the hospital they visit most frequently and are predominantly managed by the hospital. However, once a PHR is established, treatment quality can be improved because all hospitals can access the patient's PHR and share relevant medical information. This type of PHR is called the interconnected PHR, and prior versions of the PHR include the stand-alone PHR and electronic medical record (EMR)-tethered PHR. In the stand-alone PHR, patients' medical information can be stored in a smart card, USB, or CD. This system is less costly and allows patients the most control in the management of their medical information. However, a drawback is that it records medical information based on records created by patients. Since it is connected with a hospital's EMR, an EMR-tethered PHR has additional features, including booking appointments and checking prescriptions and exam information. In this type of PHR, information generated when a patient visits a hospital is automatically delivered to the PHR. Here, the drawback is that patients' play a decreased role in controlling their medical information. However, this drawback can be mitigated and patient control increased when a patient health record book feature is added to an EMR-tethered PHR. In addition, this is the system that immediately precedes the interconnected PHR in effectiveness, because medical records are accurate and easily accessible to both physicians and patients.
Currently in the US, more than 70 web-based PHRs are being utilized and some hospitals provide their own PHR service based on EMR information. Since most medical consumers desire access to a PHR, an increasing number of hospitals intend to provide the PHR service.6) As a pilot service, a number of hospitals began providing medical information (e.g., outpatient/medication results, hospitalization information, diagnostic or imaging exams) on USB or CD rather than in paper form. However, the service is in an elementary level, and it is difficult to provide it when the PHR is not linked to the EMR.3)
The Seoul National Bundang Hospital (SNUBH) was the first hospital outside of the US to obtain Healthcare Information and Management Systems Society state 7, the highest certification stage for hospital information systems.7) Specifically, SNUBH developed an EMR-tethered PHR that expanded the scope of their existing services. This service is named Health4U, and started providing the service in June 2013.8)
In this study, we introduced the development process of Health4U and used information accumulated over a 1-year period to analyze the behavior of medical consumers who accessed Health4U. An EMR-tethered PHR is an intermediate stage of an interconnected PHR, which is the ultimate PHR designation. By analyzing 1 year of experience operating the EMR-tethered PHR, we attempted to provide supporting information for the introduction of an EMR-tethered PHR in other medical institutions, public organizations and insurance companies, or to establish a regional or national interconnected PHR.
METHODS
1. Personal Health Records Development Process
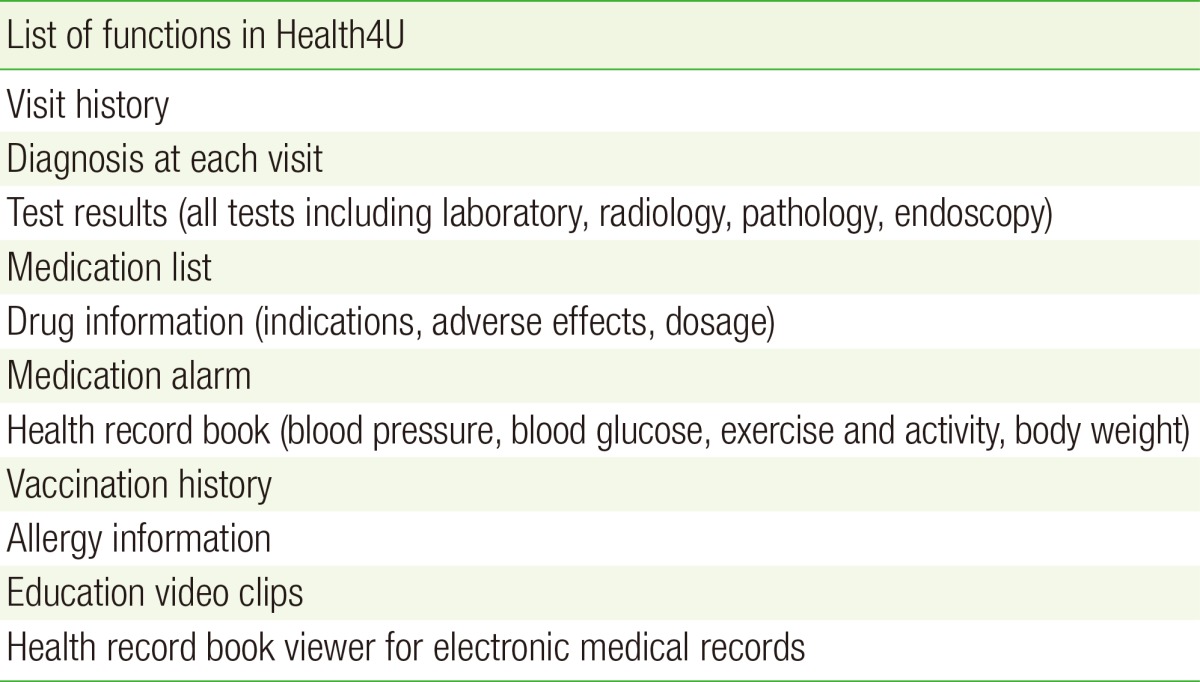
A task force team consisting of 8 physicians, 3 nurses, and 3 developers was formed to develop the PHR system. In order to select feasible features and determine the scope of patient medical information to be provided, a period of approximately 1 year (August 2011 to July 2012) was spent determining the scope of the PHR service and operation policies (Table 1). Subsequently, approximately 10 months (August 2012 to June 2013) were spent designing a user interface and developing PHR applications for iOS and Android, as well as the PHR for the website.
Table 1. Task force team requests for personal health record development during the planning period.
2. Health4U Structure and Components
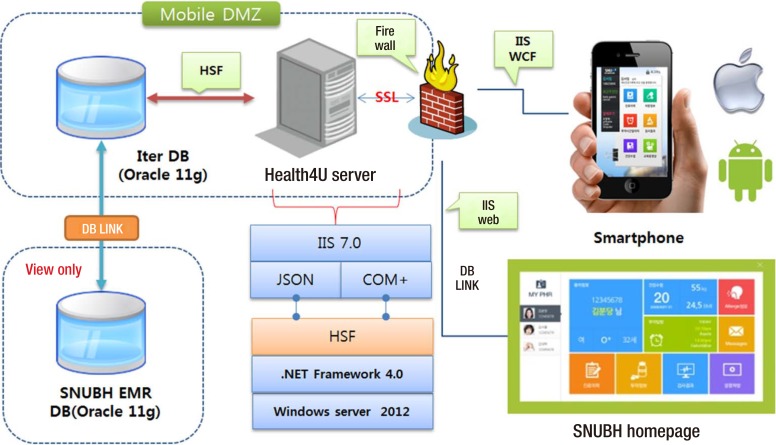
The mobile application for Health4U was made for iOS and Android platforms and was developed in the form of a hybrid application with the combination of native and web applications. The PHR service server consists of the Windows 2012 Server, Net Framework 4.0, and Microsoft Internet Information Service (IIS). The Health4U mobile application communicates with the Health4U server through the Windows Communication Foundation service provided by IIS 7.0, in which Simple Object Access Protocol is used as a communication protocol. The Health4U service offered on the SNUBH website communicates with the Health4U server through the IIS 7.0 web service. The Health4U server accesses the SNUBH EMR database (DB) via the Iter DB using the Healthcare Software Framework. SNUBH EMR DB and Iter DB are linked together with DB LINK (Figure 1).
Figure 1. System architecture of Health4U. Mobile DMZ, Mobile Demilitarized Zone; JSON, JavaScript Object Notation; COM+, Component Object Model; HSF, Healthcare Service Framework; IIS, Internet Information Services; WCF, Windows Communication Foundation; SNUBH EMR DB (Oracle 11 g), Seoul National University Bundang Hospotal Electronic Medical Record DataBase (Oracle 11 g); DB, database.
3. Materials and Statistical Analysis
Using the data extracted from the Health4U DB and Development Milestone Release DB, we analyzed the login data from June 2013 to June 2014. Subjects included 6,555 male and 5,298 females of all ages who accessed Health4U through either the mobile application or the website. The specific services included in analysis were the number of searches for treatment history, prescription information, medication reminders, exam results, health record book, as well as the number of health record books. Users who accessed Health4U 3 or more times were counted to represent the number of searches by service items and the annual trend was evaluated by analyzing the number of monthly users. This study was approved by the institutional review board of the Seoul National University Bundang Hospital (IRB No: B-1504-294-107).
RESULTS
Beginning in June 2013, SNUBH patients could search their personal medical information using PC web browsers or the mobile Health4U application (Figure 2).
Figure 2. Screenshot from Health4U main webpage. The webpage includes information about visit history, health record book, laboratory test results, medication information, medication alarms, vaccination history, and education video clips. PHR, personal health record.
Service items that could be accessed using searches on Health4U included information such as exam results, treatment history, prescription information, medication reminders, a health record book, allergy information, vaccinations, and educational videos. All hospital patients could access information about all exams, medications, and sample test results. To prevent the patient from arbitrarily interpreting test results, disclosure of sample test results were only made after the patient received hospital treatment. The results were available for hospitalized or emergency patients the day after the tests had been conducted. Like other PHRs or health management applications, Health 4U offered a diary feature (health record book) to record factors such as blood pressure, blood sugar, amount of exercise, and body weight. In turn, medical teams could access this feature via EMR, facilitating two-way communication between patients and physicians.
1. Use Status
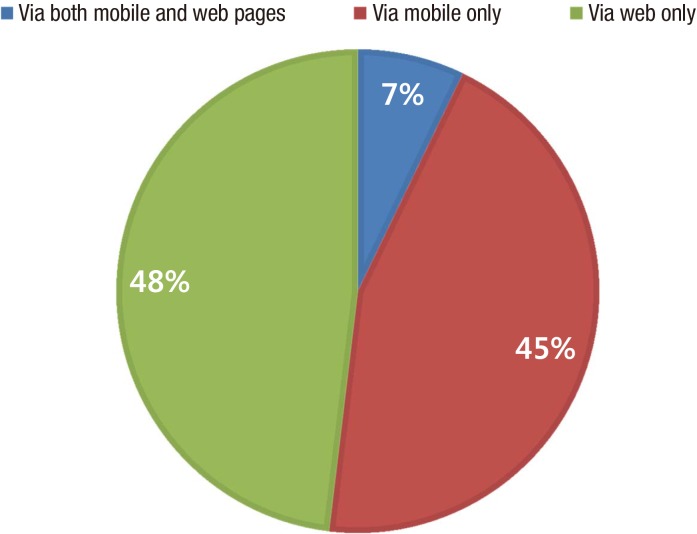
A total of 11,853 users accessed Health4U between June 2013 and June 2014. Of these users, 849 accessed information using both mobile and website methods, 5,303 only used mobile applications, and 5,701 only used the website, respectively (Figure 3).
Figure 3. Users' methods of accessing Health4U.
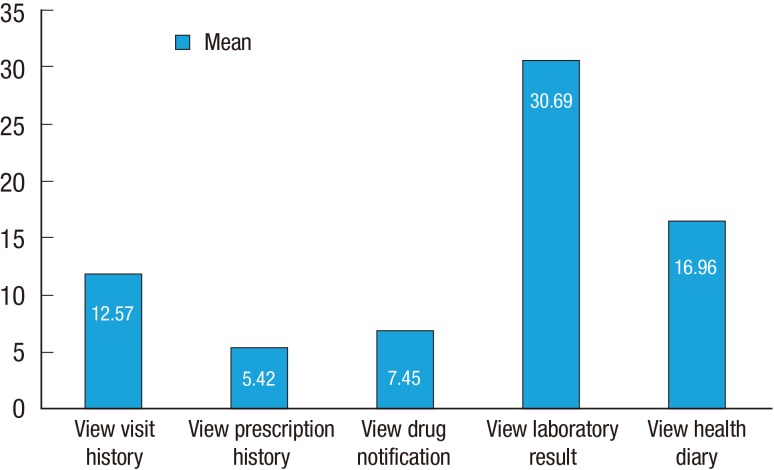
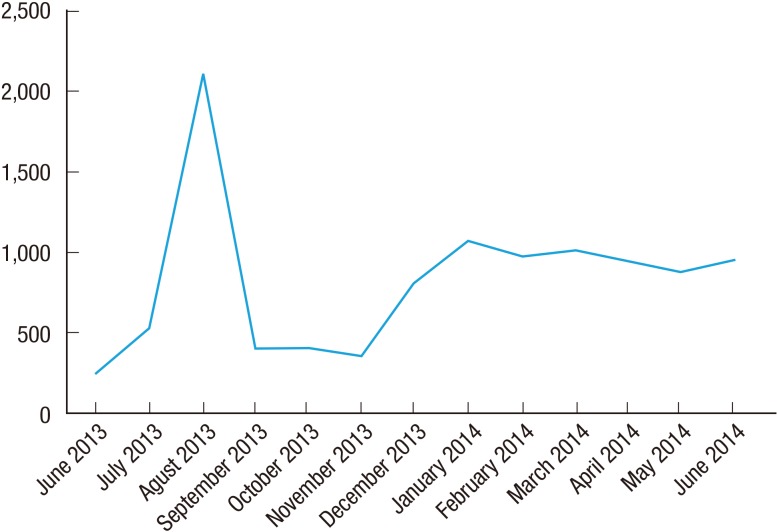
For those who used Health4U 3 or more times, the average numbers of access by service item were 30.69 for exam results, 16.96 for the health record book, 12.57 times for treatment history and diagnosis, 7.45 times for medication reminders, and 5.42 times for prescription information (Figure 4). Thus, patients most frequently searched for information about exam results (Figure 4). Analysis of monthly use of Health4U revealed a continuous increase in number of users following the initiation of the service (Figure 5).
Figure 4. Service item access patterns among users who used Health4U 3 or more times (mean).
Figure 5. Number of Health4U users between June 2013 and June 2014.
2. Health4U User Feedback
Following the launch of the Health4U service in June 2013, patients who used PHR over a period of 1 year made fewer than 100 complaints. Most complaints were about not providing the results of imaging, function and pathology exams, and laboratory tests. However, users made no complaints about a lack of medical records written by physicians. Users were also concerned about possible leaks of medical information if the server was hacked, while most complaints were about program errors.
DISCUSSION
Since PHR was introduced prior to 2000, it is not a new concept. One study reported that more than 86% of medical consumers feel the need for a PHR.6) However, to this point, the standalone PHR has dominated the field and only a small number of patients can access medical information. Consequently, there has been continued interest in an EMR-tethered PHR because it automatically enters medical information and is accessible to all patients. After building an entirely paperless EMR environment in the early 2000s, SNUBH developed and started the Health4U service as its own PHR. Since the number of PHR users has continuously increased, medical consumers' needs have been confirmed.
To date, Health4U has a number of features that differ from PHR services provided by other hospitals. First, Health4U is a universal service provided to all hospital patients. Second, it allows access form both computers (via the website) as well as through an exclusive application that enables users to conveniently use the service with all Android- and iOS-based smart devices. According to our study results about Health4U user mobile and web access patterns, most access the PHR using one of the two methods (i.e., either mobile or website), and there were similar ratios between those who used each method. In terms of information accessibility, this suggests, that it is essential to provide the PHR services in both forms. As of 2012, approximately 1 billion people worldwide use smartphones and this number is expected to increase to 2 billion in 2015.9) In addition, a study demonstrating that smartphone applications increase physical activity and contribute to weight loss indicates that mobile PHR use has a positive clinical effect.10) Third, patients can search for results from laboratory and other test types, and access medication information. Fourth, since Health4U is systematically linked with EMRs, medical teams can search the health information patients have entered, allowing for evaluation of patient compliance. Similarly, it enables continuous patient communication by establishing target numbers for reaching specific health goals. For instance, a study on patients with chronic pain reported that writing in a smartphone diary and medical team intervention using diary information prevented symptom aggravation and helped patients' rehabilitation.11) Finally, although Health4U also provides features similar to other PHRs that manage activity level, blood pressure, blood sugar, and weight, it also offers a feature enabling patients to compare hospital score tests with the numbers they personally enter. Consequently, this helps patients more effectively manage their own health.
According to previous studies, medical consumers have a high level of PHR satisfaction and assign it high value because they can search test results and more easily communicate with physicians about them.12) Regarding the number of access by service item for 3 times or more, the number of search for test results was the most with its average at 30.69. Furthermore, the finding that user complaints were most frequently related to the inaccessibility of results of imaging, function, and pathology tests suggests that medical consumers consider it important to check test results through a PHR.
Some test results were not provided owing to objections by physicians who received results and were in the process of determining the scope of medical information to be provided to patients. Specifically, they objected because the results of imaging, function, and pathology tests alone cannot provide sufficient information and frequently require determining a clinical correlation with clinical symptoms. Consequently, access to these results could cause patients' unnecessary anxiety and reduce PHR efficiency from excessive complaints. A study on medical teams' positions regarding PHRs reported similar concerns, reflected in their comment that "the results of blood tests provided without accumulated medical knowledge are likely to negatively affect the relationship between physicians and patients because there is a possibility of misinterpretation."13) Additionally, although treatment history can be searched, physicians' medical records are not provided in the PHR. In particular, information quality problems may arise if patients can read physicians' medical records at any time because physicians have recording limitations.13) However, in the current study, these concerns were not expressed during the 1-year period even though all sample test results were provided. This suggests that the service design that provided test results following treatment was effective. Furthermore, patients did not complain about a lack of physician medical records, indicating a low desire to access this information and were more interested in retrieving other forms of medical information from the PHR.
A previous study has already documented medical team's resistance to change and their negative response to patient evaluation and disclosure of evaluation results.14) However, the fundamental purpose of a PHR is to allow patients to easily access their health information and directly manage it.15) Thus, this implies that patients not only gain knowledge and interest in their health and illnesses, but also can subjectively participate in the medical decision-making process. This is the basis of patient-centric medicine and a form of "providing sufficient information," which is central in patient-centric medicine.16,17) Although medical teams may be concerned that providing patients with medical information causes unnecessary anxiety, patients' participation in the diagnostic process and treatment plan can actually improve patients' experience and reduce anxiety.18) Since the analysis of PHR usage by service item indicates that patients desire access to their medical information, and that the PHR can be a tool to facilitate this.19) Unless information asymmetry is solved, equality between physicians and patients is cannot be achieved.20) Thus, the use of a PHR is a valuable means of addressing the asymmetry of access to medical information by patients and physicians.
Lastly, medical institutions providing the PHR service linked with EMRs should build a system that fully protects medical information. For instance, in this study, subscribing membership was blocked at the onset for a patient who expressed privacy concerns.
The limitation of this study was low representativeness and generalizability because subjects were all seeking medical services at a single hospital. Nevertheless, it has a number of strengths including the following: all hospital patients could participate, it was the first study of its kind in Korea, and it studied the rare topic of PHR service provision using both mobile and website medical information access.
In conclusion, active use of a PHR is expected to have a positive effect on treatment results because it allows patients to have increased management of their health and illnesses. Additionally, it can facilitate effective communication with physicians in sessions that typically are limited in time. A further study is needed with regard to the actual treatment effects of the PHR. Furthermore, in order to forecast future changes in medicine due to an increased use of a PHR, a study about how current PHR use has changed patients' medical use is required. Development focused on patient-centric medicine is essential in terms of free communication and information access. Consequently, a true PHR service should be in place, where medical information from all hospitals is combined and accessible. Thus, this study of the SNUBH PHR Health4U service is expected to contribute to the development and expansion future PHR services.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.O'Reilly T. What is Web 2.0: design patterns and business models for the next generation of software. Commun Strateg. 2007;65:17–37. [Google Scholar]
- 2.Spallek H, O'Donnell J, Clayton M, Anderson P, Krueger A. Paradigm shift or annoying distraction: emerging implications of web 2.0 for clinical practice. Appl Clin Inform. 2010;1:96–115. doi: 10.4338/ACI-2010-01-CR-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shin SY, Chung CK. A future of medical information system: establishment of hospital-oriented personal health record. J Korean Med Assoc. 2009;52:1115–1121. [Google Scholar]
- 4.Grossman JM, Zayas-Caban T, Kemper N. Information gap: can health insurer personal health records meet patients' and physicians' needs? Health Aff (Millwood) 2009;28:377–389. doi: 10.1377/hlthaff.28.2.377. [DOI] [PubMed] [Google Scholar]
- 5.Anderson RM, Funnell MM. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ Couns. 2005;57:153–157. doi: 10.1016/j.pec.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Kim JH, Kwak M, Kim EJ, Kwon CI, Kim Y. A survey of health consumers' attitude of personnel health management service using PHR. J Korean Soc Med Inform. 2008;14:329–343. [Google Scholar]
- 7.Healthcare Information and Management System Society Analytics. Stage 7 hospitals [Internet] Chicago: HIMSS Analytics Asia Pacific; c2014. [cited 2014 Aug 1]. Available from: http://www.himssanalyticsasia.org/emradoptionmodel-stage7hospitals.asp. [Google Scholar]
- 8.Google Inc. Google play: Health4U, Seoul National University Bundang Hospital [Internet] Mountain View (CA): Mountain View (CA); c2014. [cited 2014 Aug 1]. Available from: https://play.google.com/store/apps/details?id=com.neozen.snubh_phr&&hl=ko. [Google Scholar]
- 9.Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67. doi: 10.1186/1472-6947-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28:320–329. doi: 10.1097/JCN.0b013e318250a3e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kristjansdottir OB, Fors EA, Eide E, Finset A, Stensrud TL, van Dulmen S, et al. A smartphone-based intervention with diaries and therapist-feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain: randomized controlled trial. J Med Internet Res. 2013;15:e5. doi: 10.2196/jmir.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13:121–126. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yau GL, Williams AS, Brown JB. Family physicians' perspectives on personal health records: qualitative study. Can Fam Physician. 2011;57:e178–e184. [PMC free article] [PubMed] [Google Scholar]
- 14.Gillespie R, Florin D, Gillam S. How is patient-centred care understood by the clinical, managerial and lay stakeholders responsible for promoting this agenda? Health Expect. 2004;7:142–148. doi: 10.1111/j.1369-7625.2004.00264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc. 2008;15:1–7. doi: 10.1197/jamia.M2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stewart M. Patient-centered medicine: transforming the clinical method. London: Radcliffe Publishing; 2003. [Google Scholar]
- 17.Detmer D, Bloomrosen M, Raymond B, Tang P. Integrated personal health records: transformative tools for consumer-centric care. BMC Med Inform Decis Mak. 2008;8:45. doi: 10.1186/1472-6947-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 19.Nazi KM, Hogan TP, Wagner TH, McInnes DK, Smith BM, Haggstrom D, et al. Embracing a health services research perspective on personal health records: lessons learned from the VA My HealtheVet system. J Gen Intern Med. 2010;25:62–67. doi: 10.1007/s11606-009-1114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laine C, Davidoff F. Patient-centered medicine: a professional evolution. JAMA. 1996;275:152–156. [PubMed] [Google Scholar]