Abstract
Hypertension (HTN) and CKD are closely associated with an intermingled cause and effect relationship. Blood pressure (BP) typically rises with declines in kidney function, and sustained elevations in BP hasten progression of kidney disease. This review addresses current management issues in HTN in patients with CKD including altered circadian rhythm of BP, timing of antihypertensive medication dosing, BP targets, diagnostic challenges in evaluating secondary forms of HTN, and the role of salt restriction in CKD. HTN in patients with CKD is often accompanied by a decrease in the kidney’s ability to remove salt. Addressing this salt sensitivity is critical for the management of HTN in CKD. In addition to the well-established use of an ACEI or angiotensin receptor blocker, dietary salt restriction and appropriate diuretic therapy make up the mainstay of HTN treatment in patients with CKD. Bedtime dosing of antihypertensive medications can restore nocturnal dips in BP, and future clinical practice guidelines may recommend bedtime dosing of 1 or more antihypertensive medications in patients with CKD.
Keywords: Resistant, Hypertension, Blood pressure, CKD, Salt
Introduction
CKD and hypertension (HTN) are closely associated with an overlapping and intermingled cause and effect relationship. Declines in kidney function are typically associated with rises in blood pressure (BP), and sustained elevations in BP hasten the progression of kidney function decline.1 This detrimental positive feedback interaction between kidney function and BP was observed in early experiments with animal models of kidney injury and later in clinical trials. In the Chronic Renal Insufficiency Cohort (CRIC), which consists of 3612 adults with CKD (majority moderate stage), the prevalence of self-reported HTN was 86% compared with 29% in the general population.2,3 Furthermore, the prevalence rate of HTN rises, and BP becomes more difficult to control with advancing CKD stage.4 Worsening of kidney function as a consequence of an elevated BP is evident by a direct relationship between relative risk of developing end-stage kidney disease (ESKD) and BP severity.5,6 In a large health screening registry, individuals with a baseline BP close to 180/100 mm Hg were approximately 15 times more likely to develop ESKD than individuals with a baseline BP close to 110/70 mm Hg.5
The interdependence between CKD and HTN complicates management of both diseases. This article addresses current issues in HTN in patients with CKD including altered circadian rhythm of BP and timing of antihypertensive medication dosing, BP targets, diagnostic challenges in evaluating secondary forms of HTN, and specialized management strategies of HTN in patients with CKD.
Defining BP Control by Ambulatory Monitoring in HTN
For groups where an office BP less than 140/90 mm Hg defines control, the overall 24-hour mean BP should be less than 130/80 mm Hg with a corresponding mean daytime BP less than 135/85 mm Hg and mean night-time BP less than 120/70 mm Hg.7 Blood pressure control using self-measured BPs at home is identical to mean daytime BP with ambulatory monitoring (<135/85 mm Hg).8 Individuals with an office BP less than 140/90 mm Hg yet who are not controlled by home BP monitoring or 24-hour ambulatory monitoring are classified as masked HTN or masked uncontrolled HTN if he/she is receiving antihypertensive medications.7 Table 1 summarizes definitions of common terms associated with HTN.
Table 1.
Definition of Terms Associated With Hypertension
| Hypertensive Term | Definition | Comments |
|---|---|---|
| Resistant hypertension | Uncontrolled BP despite maximal effective dosing of ≥3 medications of different classes, one ideally being a diuretic41 | Includes patients controlled on ≥4 medications |
| Apparent resistant hypertension | Meeting criteria for resistant HTN, yet unable to exclude pseudoresistance62 | Reported in observational studies |
| Pseudoresistance | Uncontrolled office BP while receiving ≥3 medications in the setting of medication nonadherence, improper BP measurement technique, and/or white coat HTN | Presumed to contribute to as much as 50% of resistant hypertension62 |
| White coat hypertension | Uncontrolled office BP with a controlled overall average BP by 24-hr ABPM (<130/80 mm Hg) or home BP < 135/85 mm Hg7 | |
| Masked uncontrolled hypertension | Controlled office BP (<140/90 mm Hg) with an elevated overall average BP by 24-hr ABPM (>130/80 mm Hg) or home BP > 135/85 mm Hg7 | Present in as many as 40%–70% of patients with CKD and HTN9,10 |
| Dipping | Fall in nocturnal systolic and diastolic BP of >10% of daytime values7 | |
| Nondipping and rising | No reduction or an increase in nocturnal systolic and/or diastolic BP7 | |
| Refractory hypertension | Uncontrolled BP despite maximal medical therapy (ie, ≥5 antihypertensive medications at maximal effective dosing and of different class) |
Abbreviations: ABPM, ambulatory blood pressure monitoring; BP, blood pressure; CV, cardiovascular; HTN, hypertension.
Masked uncontrolled HTN is more prevalent among individuals with CKD with rates ranging from 40% to 70%.9,10 The likelihood of having masked uncontrolled HTN rises in proportion to kidney dysfunction and the extent of proteinuria.11 Without an assessment of ambulatory or home BP, masked uncontrolled HTN will be missed, and this group of individuals is at a high risk for both cardiovascular events and initiation of dialysis. In a multicenter prospective study of 489 consecutive hypertensive patients with CKD, the group with masked uncontrolled HTN had a 3-fold higher risk for fatal and nonfatal cardiovascular events and a nearly 4-fold higher risk for dialysis initiation after a median of 5.2 years of follow-up, compared with the group controlled both at home and in the clinic. No increase in risk was seen in the group who was uncontrolled in the office yet controlled at home.12
Circadian Rhythm of BP in Patients With CKD
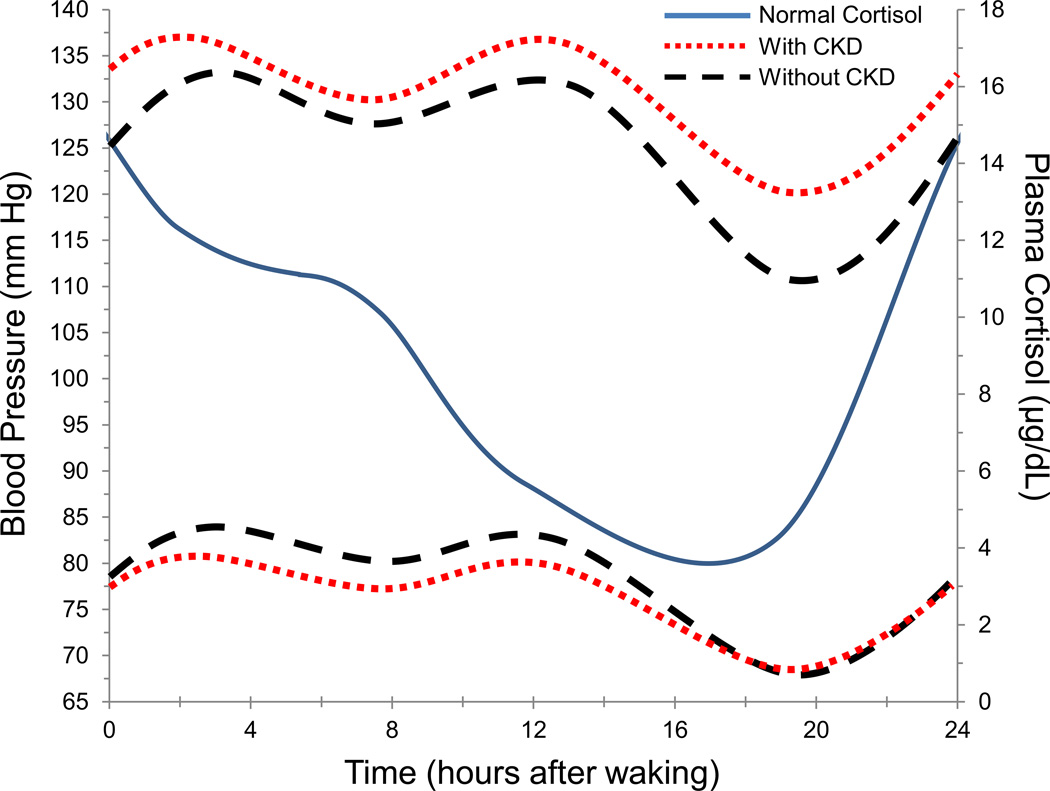
In healthy individuals, BP falls by 10% to 20% during sleep. A fall in nocturnal BP characterizes a normal circadian pattern of BP. Individuals whose BP fails to drop or, instead, rises at night are at an increased risk of death compared with dippers.13,14 In addition, mean nocturnal systolic BP predicts ESKD or death,15 and nondipping is associated with the severity of interstitial fibrosis and tubular atrophy by kidney biopsy.16 Therefore, the findings from Mojon and colleagues17,18 that dipping patterns are blunted in individuals with CKD (Fig 1) is concerning and particularly relevant for management of HTN in patients with CKD.
Figure 1.
Diurnal blood pressure in individuals with and without CKD plotted alongside normal diurnal variations in plasma cortisol levels.
Modified from Mojon et al.17
A cross-sectional analysis and small prospective study have shown an increased prevalence of nondipping among patients with CKD and HTN.9,19 Prevalence rates for nondipping were as high as 80% in a subgroup of the study participants of the African American Study of Kidney Disease and Hypertension (AASK) trial with baseline ambulatory BP monitoring.9 In 232 Veterans with CKD in stages ranging from 2 to 5, nondipping was detected more frequently in later stages of CKD (60% in Stage 2, 80% in Stage 3, and 72% in Stage 4).19
However, Mojon and others were the first to examine circadian BP patterns in patients with HTN and CKD on a large scale. The Hygia project, which is an ongoing prospective study aimed to assess ambulatory BP monitoring and HTN treatment time on cardiovascular risk, enrolls patients with HTN from primary care centers in northwest Spain. At the time of cross-sectional analysis by Mojon and colleagues, 10,271 hypertensive patients had been enrolled, of which 3227 had CKD defined by an estimated GFR less than 60 mL/min/1.73 m2 and/or urine albumin-to-creatinine ratio of 30 mg/g or more. In patients with CKD compared with those without CKD, ambulatory systolic BP was higher, particularly at night (mean asleep systolic BP 125.0 ± 17.9 vs 117.5 ± 13.1 mm Hg, P < .001), whereas overall diastolic BP was lower (mean 48-hour diastolic BP 74.8 ± 11.6 vs 76.9 ± 9.5 mm Hg, P < .001). The prevalence of nondipping was higher in patients with CKD (60.6% vs 43.2%, P < .001); however, the largest difference was seen in the riser pattern where mean asleep systolic BP greater than mean awake systolic BP occurred in 17.6% of patients with CKD vs 7.1% of patients without CKD.17 A comparison of the BP pattern between patients with and without CKD is displayed alongside a typical diurnal variation of plasma cortisol levels in Figure 1.
Although the mechanisms underlying sleep-related increases in BP and elevated pulse pressure in patients with CKD and HTN are not known, impaired long-term balance of salt and water by the kidney is an attractive hypothesis. High salt intake diminishes night-time dipping of BP in salt-sensitive HTN.20 In a small clinical trial in patients with HTN and type 2 diabetes mellitus, the night-to-day ratio of mean BP by ambulatory monitoring correlated with 24-hour urine sodium excretion.21 An excess of total body salt likely also contributes to arterial stiffness, which is approximated by pulse pressure and known to be associated with worsened kidney function.22 Although it is difficult to disassociate BP-lowering effects on improvements in arterial stiffness with dietary restrictions of salt.23 The cause and effect relationship between total body salt and obstructive sleep apnea also remains undefined. However, the 2 are likely related given the high prevalence for both salt excess and obstructive sleep apnea in resistant HTN and CKD.24,25 Importantly, obstructive sleep apnea may contribute to nocturnal HTN and nondipping in individuals with CKD.
The Central Role of Salt in CKD and HTN
Experimental animal models have shown that HTN brought on by inducing kidney damage is associated with a decreased ability of the kidney to remove salt. For example, dogs with about 70% loss of kidney tissue develop HTN within a few days when dietary salt is increased, yet HTN disappears when the increased salt intake is stopped.26 When considering these experiments in combination with computer models of BP that identify salt and water balance in the kidney as the central long-term regulator of BP, one can reasonably attribute a large portion of HTN in CKD to an impaired salt excretion that is exacerbated by excess salt intake.27 Many conditions associated with CKD can impair salt excretion, including reduced renal mass, sympathetic nervous system activation, reninangiotensin-aldosterone imbalance, altered sodium chloride handling in the distal nephron, endothelial dysfunction, or some combination of the earlier mentioned conditions.
High dietary salt intake not only exacerbates HTN in patients with CKD but also has the potential to directly worsen kidney function. Rats receiving a high salt diet show sustained increases in kidney levels of transforming growth factor-β, polypeptides associated with kidney fibrosis.28 High salt diet blunts kidney autoregulation, which exposes the glomerulus to higher filtration pressures.29 Over time, the high glomerular filtration pressure leads to glomerular sclerosis and nephron loss. There are few clinical trials investigating salt intake on kidney outcomes. However, a recent systematic review found worsened kidney function, defined as a decline in creatinine clearance, doubling of serum creatinine, or progression to ESKD, associated with high sodium intake in all 4 cohort studies that compared a low and high sodium intake.30 The associated worsening of both HTN and CKD in the setting of high salt intake highlights the importance of salt restriction in the management of HTN in patients with CKD.
Blood Pressure Target in CKD
Starting in 2011, there have been 8 clinical practice guidelines published that address the treatment of HTN.31–37 Although opinions differ in areas lacking large randomized controlled trials, consensus exists in setting a goal BP of less than 140/90 mm Hg for the majority of individuals. The panel members appointed to the Eighth Joint National Committee restricted their analysis solely to long-term randomized controlled trials with hard outcomes in study populations of adults with HTN.35 Results from this analysis did not find sufficient evidence to recommend a lower BP goal less than 140/90 mm Hg in either patients with CKD or diabetes mellitus. The Kidney Disease Improving Global Outcomes BP work group expanded their pool of evidence beyond long-term randomized controlled trials in HTN to include meta-analyses, systematic reviews, and selected randomized controlled trials with outcomes related to kidney disease progression.34 Review of this evidence base supported a lower BP goal of less than 130/80 mm Hg for individuals with CKD and moderate-to-severe albuminuria (eg, urine albumin-to-creatinine ratio > 30 mg/g) either with or without diabetes mellitus. However, this recommendation was based on an evidence level equivalent to expert opinion. As summarized in the National Kidney Foundation–Kidney Disease Outcomes Quality Initiative commentary of the Kidney Disease Improving Global Outcomes guidelines and succinctly stated in a systematic review, the available evidence is inconclusive but does not prove that a BP target of less than 130/80 mm Hg improves clinical outcomes more than a target of less than 140/90 mm Hg in adults with CKD.38,39
The guidelines focus on setting a BP threshold for treatment, yet harm may exist with overtreatment of HTN in patients with CKD. In a cohort of over 650,000 Veteran Americans with CKD, extremes of both high and low BPs were associated with increased morality, with the highest mortality for patients with high pulse pressures. The authors conclude that it may not be advantageous to achieve an ideal systolic BP (<130 mm Hg) in patients who have existing low diastolic BP (<70 mm Hg).40
Screening for Secondary Causes of HTN in Patients With CKD
CKD alone can lead to antihypertensive medication resistance; however, patients who remain uncontrolled on ideal doses of 3 different medication classes, including a diuretic, should undergo an evaluation for a separate secondary cause of HTN.41 The recommended screening methods presented in the American Heart Association’s scientific statement on resistant HTN in 2008 require minor modifications when applied to the CKD population, outlined in Table 2.
Table 2.
Special Conditions Arising in the Evaluation of Secondary Causes of Hypertension in Patients With CKD
| Secondary Cause | CKD-Specific Comment |
|---|---|
| Pheochromocytoma | Plasma-free metanephrines (normetanephrine and metanephrine) levels may be falsely high in advanced CKD. In patients with CKD Stage 5, plasma catecholamines (epinephrine and norepinephrine) may be a more appropriate screening test for pheochromocytoma. |
| Primary aldosteronism | MR imaging of the abdomen can replace the CT with contrast of the abdomen that is recommend as follow-up for positive biochemical testing for primary aldosteronism (eg, 24-hr urine aldosterone >12 µg with a suppressed plasma renin activity in the setting of high dietary sodium intake) if iodinated contrast cannot be given. |
| RVH | Following the results of the CORAL trial,44 screening for atherosclerotic-related kidney artery stenosis is no longer recommended. However, in patients in whom FMD is suspected, an MR angiogram of the kidney should be performed. |
| Nephritic GN | Urinalysis with microscopy may be an early sign of GN in patients with both worsening hypertension and rising serum creatinine. |
Abbreviations: CT, computed tomography; FMD, fibromuscular dysplasia; GN, glomerulonephritis; MR, magnetic resonance; RVH, renovascular hypertension.
Screening for Renal Artery Stenosis: The Effects of CORAL
Revascularization (eg, angioplasty or stenting) for atherosclerotis-related renal artery stenosis (RAS) was looked on unfavorably after the high rates of serious complications and lack of overall efficacy in either improvement in kidney function or reduction in BP seen in the Angioplasty and Stenting for Renal Artery Lesions (ASTRAL) and Prevention of Progression of Renal Dysfunction Caused by Atherosclerotic Ostial Stenosis of the Renal Artery (STAR) trials.42,43 However, it was argued that individuals with severe atherosclerotic-related RAS could still benefit from revascularization. The Cardiovascular Outcomes in Renal Atherosclerotic Lesions (CORAL) trial addressed this possibility. Patients with CKD Stage 3 or more or HTN requiring 2 or more antihypertensive medications and more than 60% RAS by angiography did not benefit from revascularization in addition to medical therapy with candesartan ± hydrochlorothiazide and the combination amlodipine-atorvastatin. Specifically, no difference was detected in a composite end point of cardiovascular and kidney events over a median of 43 months of follow-up, and the most common complication, kidney artery dissection, occurred in 11 of 495 participants.44
Importantly, ASTRAL, STAR, and CORAL all assessed revascularization in atherosclerotic-related RAS but not RAS because of fibromuscular dysplasia (FMD). Young women presenting with severe HTN and a family history of HTN at an early age or with an abdominal bruit on physical examination will benefit from RAS detection and angioplasty (not stenting) of FMD-related kidney artery narrowings. For patients in whom atherosclerotic disease is suspected, an RAS assessment by kidney duplex ultrasonography is still clinically helpful. In addition to obtaining structural imaging of the kidneys, a diagnosis of RAS provides a target for medical therapy and closure in the cause of HTN. Therefore, the primary change in screening recommendations for RAS in resistant HTN after CORAL may be to no longer pursue angiography or contrast-containing imaging in older patients where the likelihood of FMD-related RAS is very small.
It must also be noted that no trial has assessed the efficacy of kidney artery revascularization in high-risk clinical presentations like acute HTN associated with flash pulmonary edema. Kidney artery stenting and/or angioplasty may be indicated in these acute presentations.
HTN Management in Patients With CKD
Salt Restriction
The available evidence supports a large component of salt sensitivity to HTN in patients with CKD. Therefore, educating patients with CKD on a low salt diet is critical to achieving BP control while maintaining a simple BP medication regimen. In a double-masked placebo-controlled crossover trial, 20 hypertensive adults with Stage 3 to 4 CKD were randomized to a low sodium diet by dietary education plus 120 mmol of sodium or a low sodium diet plus matched placebo capsules. Participants received each diet with capsules for 2 weeks with a 1-week washout period in between. Mean 24-hour urinary sodium excretions were 168 mmol (95% confidence interval [CI], 146–219) and 75 mmol (95% CI, 58–112) for the high and low salt interventions, respectively. Mean BP by 24-hour ambulatory monitoring was lower by 9.7/3.9 mm Hg (95% CI, 4.5–14.8/1.3–6.4) in the low salt intervention.45
A modest dietary sodium restriction can enhance the effects of antihypertensive medications like angiotensin-converting enzyme inhibitors or angiotensin receptor blockers when treating HTN in CKD. In a small randomized trial, 52 patients with nondiabetic nephropathy receiving lisinopril 40 mg daily were randomized to valsartan 320 mg daily or placebo combined with consecutively a low sodium (target 50 mmol/d) or a regular sodium (target 200 mmol/d) diet in a crossover design for four 6-week periods. Mean urinary sodium excretion was 106 and 184 mmol/d in the low and regular sodium interventions. This difference in dietary sodium intake resulted in a larger BP reduction (7% vs 2% reduction, P = .003) compared with the addition of the angiotensin receptor blocker to lisinopril 40 mg daily.46
Importantly, low dietary salt intake also augments the antiproteinuric effect of diuretics and renin-angiotensin-aldosterone blocking drugs. In 34 proteinuric patients with diabetes mellitus, reductions in mean baseline proteinuria were increased from 30% to 55% with the addition of a low salt diet to losartan monotherapy. The combination of a low salt diet and hydrochlorothiazide reduced proteinuria by 70% from baseline.47 Conversely, a high salt diet offsets the efficacy of diuretics and renin-angiotensin-aldosterone blockers to both reduce BP and proteinuria.
Concerns have been raised about potential risks from overly restricting dietary sodium. In the Institute of Medicine’s salt intake report, the committee found that studies linking health outcomes to dietary sodium intake were highly variable in methodologic quality, which limited their conclusions. For the general US population, higher levels of sodium intake were associated with higher risk of cardiovascular disease; however, the evidence was insufficient to recommend restricting daily sodium intake further than 2.3 g/d. The committee did identify a subgroup at risk for adverse events from a low sodium diet (eg, individuals with heart failure with a reduced ejection fraction and receiving aggressive therapeutic regimens); however, this does not apply to most individuals with HTN and CKD, who are at risk for salt-sensitive HTN.48,49
Diuretic Use in Advanced CKD
In general, as GFR falls, higher doses of diuretics are needed to achieve a natriuretic response. Diuretic dosing can be particularly challenging in late stages of CKD when the risk of over diuresis and its associated hastening of progression to dialysis outweighs the benefit of improved BP control. This is further complicated in patients with hypoalbuminemia as less protein-bound loop diuretic is available for tubular secretion. Furthermore, the short-acting effect of many loop diuretics hinders their efficacy in long-term BP control. For all these reasons, clinicians have reconsidered the use of thiazide diuretics as an alternative or additional medication to the use of loop diuretics in advanced CKD (estimated GFR < 30 mL/min/1.73 m2) where they traditionally have been thought to be ineffective.50
In 2012, Dussol and colleagues performed a double-masked, randomized, crossover trial of furosemide and hydrochlorothiazide in 23 patients with CKD stages 4 and 5. After 3 months of treatment, hydrochlorothiazide at 25 mg dosing reduced mean supine BP by the same extent as furosemide 60 mg (from 101 mm Hg to 94 and 93 mm Hg, respectively; P < .05). Combination of the 2 study medications decreased mean supine BP more effectively to 86 mm Hg (P < .01).51 This prospective trial and other observational studies provide some evidence for efficacy of thiazide diuretics, often in combination with a loop diuretic, in advanced CKD.50 Chlorthalidone, the long-acting thiazide used in many of the large clinical trials of HTN, has twice the potency of hydrochlorothiazide at similar doses and may hold some efficacy in advanced CKD.52
The combination of a thiazide and a loop diuretic may be most effective in patients with excess volume.
Night-time Antihypertensive Medication Dosing
Multiple clinical trials have shown an improvement in nocturnal dipping of BP by dosing at least 1 antihypertensive medication at bedtime,53–55 and night-time medication dosing has been associated with reduced cardiovascular risk.56,57 In a prospective, open-label trial, Hermida and others randomized 661 individuals with HTN and CKD to all morning dosing of antihypertensive medications or at least 1 at bedtime. Ambulatory BP monitoring for 48 hours was performed at baseline and at least annually. After a median of 5.4 years of follow-up, patients with at least 1 medication dosed at bedtime had an adjusted risk for a composite outcome of cardiovascular death, myocardial infarction, and stroke of approximately one-third than that of patients who took all their antihypertensive medications in the morning (adjusted hazard ratio, 0.28; 95% CI, 0.13–0.61).56 In addition, bedtime dosing was associated with improved ambulatory BP control (56% vs 45%, P = .003). Based on results from similar trials in patients with diabetes mellitus, the American Diabetes Association included a level A recommendation to administer 1 or more antihypertensive medications at bedtime in the 2013 guidelines for the care of diabetes mellitus.31 Similar recommendations have yet to reach other guideline-producing groups, but given both the impaired circadian pattern of BP in patients with CKD and the increased cardiovascular risk associated with CKD, future guidelines involving HTN management in patients with CKD will likely include recommendations for bedtime medication dosing.
Mineralocorticoid Antagonist Use in CKD
Impressive reductions in BP for individuals receiving 3 or more antihypertensive medications have made mineralocorticoid antagonists an important fourth-line BP agent in the treatment of resistant HTN.41,58,59 Patients in later stages of CKD are likely to meet the classification of resistant HTN; however, risks of hyperkalemia and acute kidney injury have limited mineralocorticoid antagonist use in advanced CKD. In patients with resistant HTN and CKD Stage 3, mineralocorticoid antagonists raised serum potassium levels by an average of 0.4 mEq/L and serum creatinine concentrations increased from a mean of 1.5 to 1.8 mg/dL.60 In proteinuric CKD and HTN, spironolactone effectively reduces both BP and urine protein levels.61 However, caution is advised with starting spironolactone in patients who have a baseline serum potassium greater than 4.6 mEq/L. Spironolactone is contraindicated in patients with acute kidney injury and creatinine clearances less than 10 mL/min. Eplerenone, a more selective mineralocorticoid antagonist, is contraindicated for use when creatinine clearance falls less than 30 mL/min. Finerenone, which binds the mineralocorticoid receptor with a higher affinity than eplerenone, is currently undergoing clinical trials for Federal Drug Administration approval in the treatment of heart failure and proteinuric diabetic nephropathy.
Conclusion
In some forms of CKD, HTN may be the earliest sign of kidney dysfunction (eg, polycystic disease) and appropriate HTN management reduces both cardiovascular and kidney outcomes. Impaired dipping of BP during sleep, salt-sensitive HTN in animal models of kidney injury, and exaggerated BP responses to restrictions in dietary salt all highlight the importance of salt in patients with CKD and HTN. In addition to the well-established use of an ACEI or angiotensin receptor blocker, dietary salt restriction and appropriate diuretic therapy make up the mainstay of HTN treatment in patients with CKD. Lastly, future clinical practice guidelines may recommend bedtime dosing of 1 or more antihypertensive medications in patients with CKD.
CLINICAL SUMMARY.
Ambulatory BP monitoring is needed to detect masked HTN and non-dipping, which are common in CKD.
ACEIs or ARBs, appropriate diuretic therapy, and dietary salt restriction make up the foundation for the treatment of HTN in CKD.
Bedtime dosing of at least one antihypertensive medication improves BP control in patients with CKD.
Acknowledgments
Support: This review was supported by the Department of Medicine, University of Alabama at Birmingham Walter B. Frommeyer, Jr. Award (to E.J.).
Footnotes
This article has been seen and approved by all authors and that it is not under consideration for publication elsewhere in a similar form, in any language.
Financial Disclosure: The authors declare that they have no relevant financial interests.
References
- 1.Bakris GL, Williams M, Dworkin L, et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis. 2000;36(3):646–661. doi: 10.1053/ajkd.2000.16225. [DOI] [PubMed] [Google Scholar]
- 2.Lash JP, Go AS, Appel LJ, et al. Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol. 2009;4(8):1302–1311. doi: 10.2215/CJN.00070109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 4.Cai G, Zheng Y, Sun X, Chen X. Prevalence, awareness, treatment, and control of hypertension in elderly adults with chronic kidney disease: results from the survey of Prevalence, Awareness, and Treatment Rates in Chronic Kidney Disease Patients With Hypertension in China. J Am Geriatr Soc. 2013;61(12):2160–2167. doi: 10.1111/jgs.12551. [DOI] [PubMed] [Google Scholar]
- 5.Tozawa M, Iseki K, Iseki C, Kinjo K, Ikemiya Y, Takishita S. Blood pressure predicts risk of developing end-stage renal disease in men and women. Hypertension. 2003;41(6):1341–1345. doi: 10.1161/01.HYP.0000069699.92349.8C. [DOI] [PubMed] [Google Scholar]
- 6.Klag MJ, Whelton PK, Randall BL, et al. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334(1):13–18. doi: 10.1056/NEJM199601043340103. [DOI] [PubMed] [Google Scholar]
- 7.Parati G, Stergiou G, O’Brien E, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32(7):1359–1366. doi: 10.1097/HJH.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 8.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34(28):2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 9.Pogue V, Rahman M, Lipkowitz M, et al. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension. 2009;53(1):20–27. doi: 10.1161/HYPERTENSIONAHA.108.115154. [DOI] [PubMed] [Google Scholar]
- 10.Bangash F, Agarwal R. Masked hypertension and white-coat hypertension in chronic kidney disease: a meta-analysis. Clin J Am Soc Nephrol. 2009;4(3):656–664. doi: 10.2215/CJN.05391008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cha RH, Kim S, Ae Yoon S, et al. Association between blood pressure and target organ damage in patients with chronic kidney disease and hypertension: results of the APrODiTe study. Hypertens Res. 2014;37(2):172–178. doi: 10.1038/hr.2013.127. [DOI] [PubMed] [Google Scholar]
- 12.Minutolo R, Gabbai FB, Agarwal R, et al. Assessment of achieved clinic and ambulatory blood pressure recordings and outcomes during treatment in hypertensive patients with CKD: a multicenter prospective cohort study. Am J Kidney Dis. 2014;64(5):744–752. doi: 10.1053/j.ajkd.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 13.Boggia J, Li Y, Thijs L, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370(9594):1219–1229. doi: 10.1016/S0140-6736(07)61538-4. [DOI] [PubMed] [Google Scholar]
- 14.Liu M, Takahashi H, Morita Y, et al. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction in haemodialysis patients. Nephrol Dial Transplant. 2003;18(3):563–569. doi: 10.1093/ndt/18.3.563. [DOI] [PubMed] [Google Scholar]
- 15.Minutolo R, Agarwal R, Borrelli S, et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med. 2011;171(12):1090–1098. doi: 10.1001/archinternmed.2011.230. [DOI] [PubMed] [Google Scholar]
- 16.Haruhara K, Tsuboi N, Koike K, et al. Renal histopathological findings in relation to ambulatory blood pressure in chronic kidney disease patients. Hypertens Res. 2014 doi: 10.1038/hr.2014.140. [e-pub ahead of print, 2014 Sep 18.]. http://dx.doi.org/10.1038/hr.2014.140. [DOI] [PubMed] [Google Scholar]
- 17.Mojon A, Ayala DE, Pineiro L, et al. Comparison of ambulatory blood pressure parameters of hypertensive patients with and without chronic kidney disease. Chronobiol Int. 2013;30(1–2):145–158. doi: 10.3109/07420528.2012.703083. [DOI] [PubMed] [Google Scholar]
- 18.Hermida RC, Smolensky MH, Ayala DE, et al. Abnormalities in chronic kidney disease of ambulatory blood pressure 24 h patterning and normalization by bedtime hypertension chronotherapy. Nephrol Dial Transplant. 2014;29(6):1160–1167. doi: 10.1093/ndt/gft285. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal R, Andersen MJ. Correlates of systolic hypertension in patients with chronic kidney disease. Hypertension. 2005;46(3):514–520. doi: 10.1161/01.HYP.0000178102.85718.66. [DOI] [PubMed] [Google Scholar]
- 20.Higashi Y, Oshima T, Ozono R, et al. Nocturnal decline in blood pressure is attenuated by NaCl loading in salt-sensitive patients with essential hypertension: noninvasive 24-hour ambulatory blood pressure monitoring. Hypertension. 1997;30(2 Pt 1):163–167. doi: 10.1161/01.hyp.30.2.163. [DOI] [PubMed] [Google Scholar]
- 21.Uzu T, Sakaguchi M, Yokomaku Y, et al. Effects of high sodium intake and diuretics on the circadian rhythm of blood pressure in type 2 diabetic patients treated with an angiotensin II receptor blocker. Clin Exp Nephrol. 2009;13(4):300–306. doi: 10.1007/s10157-009-0157-7. [DOI] [PubMed] [Google Scholar]
- 22.Townsend RR, Wimmer NJ, Chirinos JA, et al. Aortic PWV in chronic kidney disease: a CRIC ancillary study. Am J Hypertens. 2010;23(3):282–289. doi: 10.1038/ajh.2009.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gates PE, Tanaka H, Hiatt WR, Seals DR. Dietary sodium restriction rapidly improves large elastic artery compliance in older adults with systolic hypertension. Hypertension. 2004;44(1):35–41. doi: 10.1161/01.HYP.0000132767.74476.64. [DOI] [PubMed] [Google Scholar]
- 24.Logan AG, Perlikowski SM, Mente A, et al. High prevalence of unrecognized sleep apnoea in drug-resistant hypertension. J Hypertens. 2001;19(12):2271–2277. doi: 10.1097/00004872-200112000-00022. [DOI] [PubMed] [Google Scholar]
- 25.Sakaguchi Y, Shoji T, Kawabata H, et al. High prevalence of obstructive sleep apnea and its association with renal function among non-dialysis chronic kidney disease patients in Japan: a cross-sectional study. Clin J Am Soc Nephrol. 2011;6(5):995–1000. doi: 10.2215/CJN.08670910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Langstan JB, Guyton AC, Douglas BH, Dorsett PE, Russel A, McCaa RE. Effect of changes in salt intake on arterial pressure and renal function in partially nephrectomized dogs. Circ Res. 1963;12:508–513. [Google Scholar]
- 27.Guyton AC. Blood pressure control—special role of the kidneys and body fluids. Science. 1991;252(5014):1813–1816. doi: 10.1126/science.2063193. [DOI] [PubMed] [Google Scholar]
- 28.Ying WZ, Sanders PW. Dietary salt modulates renal production of transforming growth factor-beta in rats. Am J Physiol. 1998;274(4 Pt 2):F635–F641. doi: 10.1152/ajprenal.1998.274.4.F635. [DOI] [PubMed] [Google Scholar]
- 29.Fellner RC, Cook AK, O’Connor PM, Zhang S, Pollock DM, Inscho EW. High-salt diet blunts renal autoregulation by a reactive oxygen species-dependent mechanism. Am J Physiol Renal Physiol. 2014;307(1):F33–F40. doi: 10.1152/ajprenal.00040.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smyth A, O’Donnell MJ, Yusuf S, et al. Sodium intake and renal outcomes: a systematic review. Am J Hypertens. 2014;27(10):1277–1284. doi: 10.1093/ajh/hpt294. [DOI] [PubMed] [Google Scholar]
- 31.American Diabetes Associations. Standards of medical care in diabetes— 2013. Diabetes Care. 2013;36(suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2013;31(10):1925–1938. doi: 10.1097/HJH.0b013e328364ca4c. [DOI] [PubMed] [Google Scholar]
- 33.Go AS, Bauman MA, Coleman King SM, et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014;63(4):878–885. doi: 10.1161/HYP.0000000000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Group KDIGOKBPW. Clinical practice guideline for the evaluation and management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012;2(5):337–414. [Google Scholar]
- 35.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 36.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. doi: 10.1136/bmj.d4891. [DOI] [PubMed] [Google Scholar]
- 37.Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich) 2014;16(1):14–26. doi: 10.1111/jch.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taler SJ, Agarwal R, Bakris GL, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for management of blood pressure in CKD. Am J Kidney Dis. 2013;62(2):201–213. doi: 10.1053/j.ajkd.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Upadhyay A, Earley A, Haynes SM, Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Ann Intern Med. 2011;154(8):541–548. doi: 10.7326/0003-4819-154-8-201104190-00335. [DOI] [PubMed] [Google Scholar]
- 40.Kovesdy CP, Bleyer AJ, Molnar MZ, et al. Blood pressure and mortality in U.S. veterans with chronic kidney disease: a cohort study. Ann Intern Med. 2013;159(4):233–242. doi: 10.7326/0003-4819-159-4-201308200-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403–1419. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 42.Bax L, Woittiez AJ, Kouwenberg HJ, et al. Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med. 2009;150(12):840–848. w150–w841. doi: 10.7326/0003-4819-150-12-200906160-00119. [DOI] [PubMed] [Google Scholar]
- 43.Wheatley K, Ives N, Gray R, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med. 2009;361(20):1953–1962. doi: 10.1056/NEJMoa0905368. [DOI] [PubMed] [Google Scholar]
- 44.Cooper CJ, Murphy TP, Cutlip DE, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014;370(1):13–22. doi: 10.1056/NEJMoa1310753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McMahon EJ, Bauer JD, Hawley CM, et al. A randomized trial of dietary sodium restriction in CKD. J Am Soc Nephrol. 2013;24(12):2096–2103. doi: 10.1681/ASN.2013030285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Slagman MC, Waanders F, Hemmelder MH, et al. Moderate dietary sodium restriction added to angiotensin converting enzyme inhibition compared with dual blockade in lowering proteinuria and blood pressure: randomised controlled trial. BMJ. 2011;343:d4366. doi: 10.1136/bmj.d4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vogt L, Waanders F, Boomsma F, de Zeeuw D, Navis G. Effects of dietary sodium and hydrochlorothiazide on the anti-proteinuric efficacy of losartan. J Am Soc Nephrol. 2008;19(5):999–1007. doi: 10.1681/ASN.2007060693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Institute of Medicine. Sodium Intake in Populations: Assessment of Evidence. Washington, DC: The National Academies Press; 2013. [Google Scholar]
- 49.Anderson CA, Ix JH. Sodium reduction in CKD: suggestively hazardous or intuitively advantageous? J Am Soc Nephrol. 2013;24(12):1931–1933. doi: 10.1681/ASN.2013090923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Agarwal R, Sinha AD. Thiazide diuretics in advanced chronic kidney disease. J Am Soc Hypertens. 2012;6(5):299–308. doi: 10.1016/j.jash.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 51.Dussol B, Moussi-Frances J, Morange S, Somma-Delpero C, Mundler O, Berland Y. A pilot study comparing furosemide and hydrochlorothiazide in patients with hypertension and stage 4 or 5 chronic kidney disease. J Clin Hypertens (Greenwich) 2012;14(1):32–37. doi: 10.1111/j.1751-7176.2011.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension. 2004;43(1):4–9. doi: 10.1161/01.HYP.0000103632.19915.0E. [DOI] [PubMed] [Google Scholar]
- 53.Crespo JJ, Pineiro L, Otero A, et al. Administration-time-dependent effects of hypertension treatment on ambulatory blood pressure in patients with chronic kidney disease. Chronobiol Int. 2013;30(1–2):159–175. doi: 10.3109/07420528.2012.701459. [DOI] [PubMed] [Google Scholar]
- 54.Hermida RC, Ayala DE. Chronotherapy with the angiotensin-converting enzyme inhibitor ramipril in essential hypertension: improved blood pressure control with bedtime dosing. Hypertension. 2009;54(1):40–46. doi: 10.1161/HYPERTENSIONAHA.109.130203. [DOI] [PubMed] [Google Scholar]
- 55.Hermida RC, Ayala DE, Mojon A, Fernandez JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010;27(8):1629–1651. doi: 10.3109/07420528.2010.510230. [DOI] [PubMed] [Google Scholar]
- 56.Hermida RC, Ayala DE, Mojon A, Fernandez JR. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J Am Soc Nephrol. 2011;22(12):2313–2321. doi: 10.1681/ASN.2011040361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hermida RC, Ayala DE, Mojon A, Fernandez JR. Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care. 2011;34(6):1270–1276. doi: 10.2337/dc11-0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chapman N, Dobson J, Wilson S, et al. Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension. 2007;49(4):839–845. doi: 10.1161/01.HYP.0000259805.18468.8c. [DOI] [PubMed] [Google Scholar]
- 59.Vaclavik J, Sedlak R, Plachy M, et al. Addition of spironolactone in patients with resistant arterial hypertension (ASPIRANT): a randomized, double-blind, placebo-controlled trial. Hypertension. 2011;57(6):1069–1075. doi: 10.1161/HYPERTENSIONAHA.111.169961. [DOI] [PubMed] [Google Scholar]
- 60.Pisoni R, Acelajado MC, Cartmill FR, et al. Long-term effects of aldosterone blockade in resistant hypertension associated with chronic kidney disease. J Hum Hypertens. 2012;26(8):502–506. doi: 10.1038/jhh.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shavit L, Lifschitz MD, Epstein M. Aldosterone blockade and the mineralocorticoid receptor in the management of chronic kidney disease: current concepts and emerging treatment paradigms. Kidney Int. 2012;81(10):955–968. doi: 10.1038/ki.2011.505. [DOI] [PubMed] [Google Scholar]
- 62.Judd E, Calhoun DA. Apparent and true resistant hypertension: definition, prevalence and outcomes. J Hum Hypertens. 2014;28(8):463–468. doi: 10.1038/jhh.2013.140. [DOI] [PMC free article] [PubMed] [Google Scholar]