Abstract
Background.
In Asia, the role of primary care physicians (PCPs) in mental health delivery is not clearly defined and what happens to patients following a depressive episode remains poorly understood.
Objective.
To examine the 12-month naturalistic outcomes of depression in primary care and the impact of PCP identification.
Methods.
A cohort study was conducted. A total of 10179 adults were consecutively recruited from the waiting rooms of 59 PCPs across Hong Kong to complete a survey which screened for depression. Blinded doctors provided data on their diagnosis and management; 539 screened-positive and 3819 screened-negative subjects consented to telephone follow-up at 3, 6 and 12 months. Study instruments included Patient Health Questionnaire-9, Centre for Epidemiologic Studies Depression Scale 20 and Short-Form Health Survey Version 2.0 (SF-12v2) and self-reported mental health and primary care service use.
Results.
12-month remission rate was 60.31%. PCP detection had no association with remission. Identified patients had poorer health-related quality of life (HRQOL) at baseline but a faster rate of recovery in SF-12v2 mental component scores. PCP detection was associated with greater mental health service use at 12, 26 and 52 weeks, while GP consultation rates were only increased at 12 weeks.
Conclusions.
Over 1 year, ~60% of depressed patients experience symptom resolution, while 40% continue to suffer a chronic or remitting course of illness. Identification of depression by a PCP does not appear to affect remission of mood symptoms at 12 months, but is associated with a faster rate of recovery of HRQOL. PCP detection raises GP consultation rates temporarily however appears to enable more patients to access mental health services over 12 months.
Key words. Chinese, cohort study, depressive disorders, Hong Kong, primary care
Introduction
Depression has been identified as a global public health issue including in Hong Kong (1). A recent study conducted in Hong Kong’s primary care setting estimated the cross-sectional prevalence for moderate to severe depression [defined as Patient Health Questionnaire-9 (PHQ-9) score >9] as 10.9%, however of these, only 23.1% were diagnosed as having depression by the doctor (2).
Primary care is the entry point for most people into the health system and primary care physicians (PCPs) are ideally placed to provide care for patients with depression. In many Asian settings however, the role of the PCP is still poorly defined especially when related to mental health delivery, and patients can consult specialists without a referral. To date, few studies have examined the longitudinal outcomes and the factors affecting prognosis for primary care depression in Asian health care settings (3).
Hong Kong is a Special Administrative Region of the People’s Republic of China. Approximately 95% of the seven million people living in Hong Kong are of Chinese descent. Hong Kong has a developed capitalist economy, with a gross domestic product of US$301.6 billion of which ~5.5% is spent on health care and ~0.24% on mental health (4). It has a two-tiered mixed medical economy. Approximately 80% of primary care is delivered through a ‘fee-for-service’ private sector and 20% through government-funded General Out-Patient Clinics which are aimed at caring for the elderly and those with chronic diseases. There are currently no statutory post-graduate qualifications required for doctors to practice in primary care, and in private settings, any patient can seek the care of any doctor (5).
To promote evidence-based decision making, it is essential to have current knowledge on the natural course of a disease and the impact of care on outcomes in the setting where the health care is delivered. In terms of health services research, a study on primary care patients rather than on the general population is important as it provides information on people who already access the health care system and who would be efficient targets for interventions. To help fill the knowledge gap which currently exists for this setting, the aim of this study was to examine the naturalistic outcomes of patients with depressive symptoms and the impact of PCP detection.
The objectives of the study were:
1. To evaluate the 12-month outcomes of patients with screened-positive depression in terms of symptom severity, health-related quality of life (HRQOL) and service use;
2. To identify the factors affecting prognosis;
3. To compare the outcomes of depressed patients who have and have not been identified by the PCP.
Methods
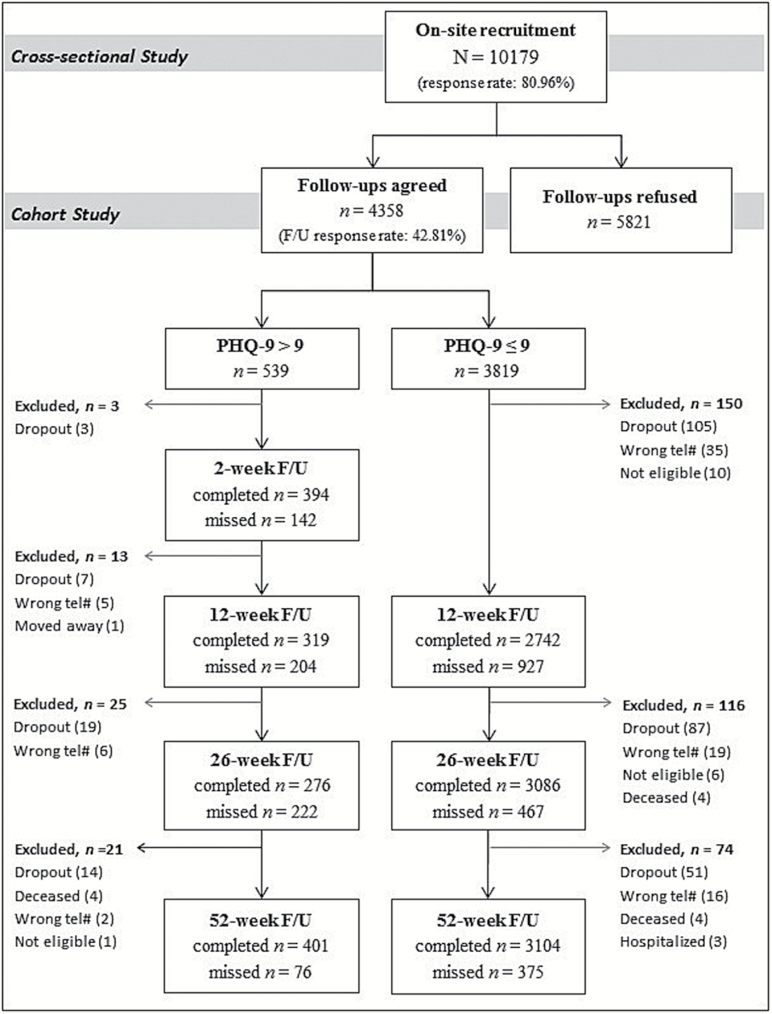
A cross-sectional followed by a longitudinal cohort study was conducted (Fig. 1). Baseline recruitment of subjects occurred between October 2010 and January 2012. Longitudinal data collection occurred between October 2010 and January 2013. The study protocol and preliminary findings of the cross-sectional study have been previously published (2,6). This paper focusses on the findings of the cohort study.
Figure 1.
Patient recruitment flowchart.
Setting and subjects
Doctors working in primary care clinics across Hong Kong were invited to collaborate as part of a practice-based research network. PCPs were initially identified using the mailing list of the Hong Kong College of Family Physicians. Reflecting the delivery of primary care in Hong Kong, participants consisted of clinicians working in private practice, government-funded primary care clinics of the Hong Kong Hospital Authority, and non-profit, non-governmental organizations.
Details of our subject sampling and recruitment strategy have been previously reported (6). In summary, all consecutive, eligible patients presenting to the study doctor on one randomly allocated day each month over a 12-month recruitment period were approached in the waiting room to complete a baseline survey. Patients were excluded if they were <18 years, did not speak or understand English, Cantonese or Mandarin, had cognitive or communication difficulties, had previously been recruited to the study, or did not consult the doctor. A research assistant was present to administer the survey to those with poor literacy or eyesight and to answer any queries. Doctors (who were blinded to the depression screening scores) were asked to document the patient’s presenting problem, their opinion on whether the patient had depression and their management if they had identified the patient as being depressed. All respondents were invited to participate in the 12-month longitudinal follow-up. Those who consented by providing their name and contact details were interviewed by telephone at 12, 26 and 52 weeks (Fig. 1).
Study instruments
Questions on socio-demography and co-morbidity were adapted from previously performed primary care patient surveys and were asked at baseline (7).
At each follow-up time point (12, 26 and 52 weeks), patients’ self-reported health and mental health status, and recent service utilization were collected with the following instruments:
PHQ-9 is a nine item questionnaire used to screen, monitor, diagnose and measure the severity of depressive symptoms (8). The Chinese version has been validated among the Hong Kong general population (9). A PHQ-9 cut-off score >9 was used to define a positive screened case for depressive disorders (10).
Centre for Epidemiologic Studies Depression Scale (CES-D 20) is a 20-item scale for measuring the current levels of depressive symptoms (11). It has been translated into Chinese and been used locally in large population surveys (12). A PHQ-9 score <5 together with a CES-D 20 score <16 was used to define remission from depression.
Short-Form Health Survey Version 2.0 (SF-12v2) is a 12-item abbreviated version of the SF-36 Health Survey that assesses HRQOL (13). It generates two norm-based summary scores, the mental component score (MCS) and the physical component score (PCS). Each averages at 50 for the general population, with higher scores indicating better health. The SF-12v2 has been translated and validated for use in Hong Kong’s primary care (14).
Questions on health service use included whether respondents had consulted a psychiatrist in the last 3 months; whether they had received professional psychological counselling from a GP, psychologist and social worker in the past 3 months; and asked how many times they had seen a GP in the past month.
Ethics
This study received ethics approvals by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster as well as all relevant regional and intuitional review boards.
Data analysis
Using a PHQ-9 score <5 together with a CES-D 20 score <16 to define remission from depression, estimation of the remission from depression over a 12-month period was made on subjects who screened PHQ+ve at baseline with a 95% confidence interval (CI), taking into account the design of clustering by practice. Patient and doctor factors associated with remission were examined using a non-linear mixed effects model with logit link taking into account the within practice correlation.
Predictive significance of patient and doctor factors on the two SF-12v2 component scores at 12-month interval were examined by linear mixed effect model. The change of PHQ-9 score and the two SF-12v2 component scores among the initially screened PHQ-9 positive subjects who had and had not been identified with depression by study doctor at baseline were compared using mixed models for dealing with missing data. A 5% level of significance was used and all estimates accompanied by a 95% CI where appropriate.
Proportional differences in health service use between the patient subgroups that screened PHQ+ve and PHQ−ve, and in PHQ+ve subjects who were detected and not detected by the doctor were examined using chi-square tests of independence.
STATA version 12 was used to carry out the analyses.
Results
Participants and recruitment rates
A total of 10179 subjects were recruited at baseline (response rate of 81%). Of these, 4358 consented to participate in the longitudinal study (response rate of 42.8%). Demographic characteristics of the baseline subjects, cohort participants and the general population (from the Hong Kong 2011 Census) are shown in Table 1. A flowchart of subject recruitment and participation is shown in Figure 1.
Table 1.
Demographic characteristics of the cohort subjects and the Hong Kong general population
| Patient participants | Baseline sample (N = 10179) | Follow-up cohort (N = 4358) | HK 2011 Census (age ≥18 years) |
|---|---|---|---|
| Gender (n, %) | |||
| Male | 4142 (40.7%) | 1803 (41.4%) | 46.7% |
| Female | 5763 (56.6%) | 2529 (58.0%) | 53.3% |
| Not indicated | 274 (2.7%) | 26 (0.6%) | – |
| Age in year (mean ± SD) | 49.0±18.1 | 49.6±17.1 | 46.58±17.4 |
| Age group (n, %) | |||
| 18–24 years | 689 (6.8%) | 269 (6.2%) | 10.5% |
| 25–34 years | 1874 (18.4%) | 746 (17.1%) | 18.1% |
| 35–44 years | 1719 (16.9%) | 741 (17.0%) | 18.9% |
| 45–54 years | 1777 (17.5%) | 817 (18.7%) | 21.5% |
| 55–64 years | 1602 (15.7%) | 834 (19.1%) | 15.4% |
| 65+ years | 2071 (20.3%) | 888 (20.4%) | 15.7% |
| Not indicated | 447 (4.4%) | 63 (1.4%) | – |
| Ethnicity (n, %) | |||
| Chinese | 9744 (95.7%) | 4216 (96.7%) | 93.6% |
| Non-Chinese | 394 (3.9%) | 140 (3.2%) | 6.4% |
| Not indicated | 41 (0.4%) | 2 (0.1%) | – |
| Household monthly income (n, %) | |||
| ≤HK$5000 | 1243 (12.2%) | 560 (12.8%) | 11.1% |
| HK$5001–HK$10000 | 761 (7.5%) | 356 (8.2%) | 12.7% |
| HK$10001–HK$20000 | 1815 (17.8%) | 826 (19.0%) | 23.8% |
| HK$20001–HK$30000 | 1533 (15.1%) | 705 (16.2%) | 17.6% |
| HK$30001–HK$40000 | 1073 (10.5%) | 515 (11.8%) | 11.4% |
| >HK$40000 | 2159 (21.2%) | 994 (22.8%) | 23.5% |
| Not indicated | 1595 (15.7%) | 402 (9.2%) | – |
| Marital status (n, %) | |||
| Single | 2699 (26.5%) | 1080 (24.8%) | 28.8% |
| Married | 6059 (59.5%) | 2771 (63.6%) | 60.1% |
| Widowed | 773 (7.6%) | 330 (7.6%) | 6.5% |
| Separated/divorced | 326 (3.2%) | 163 (3.7%) | 4.6% |
| Not indicated | 322 (3.2%) | 14 (0.3%) | – |
| Education level (n, %) | |||
| No formal schooling | 775 (7.6%) | 274 (6.3%) | 6.4% |
| Primary | 1629 (16.0%) | 800 (18.4%) | 23.1% |
| Secondary | 4127 (40.5%) | 1864 (42.8%) | 46.8% |
| Tertiary | 3325 (32.7%) | 1404 (32.2%) | 23.8% |
| Not indicated | 323 (3.2%) | 16 (0.4%) | – |
| District of residence (n, %) | |||
| Hong Kong Island | 4085 (40.1%) | 1873 (43.0%) | 18.0% |
| Kowloon | 2243 (22.0%) | 1034 (23.7%) | 29.8% |
| New Territories | 3473 (34.1%) | 1431 (32.8%) | 52.2% |
| Not indicated | 378 (3.7%) | 20 (0.5%) | – |
Distributions of household monthly income and education level of the HK 2011 Census results reported above may not be exact due to the use of different classification groupings.
Remission rate and prognostic factors for depression
Among patients who screened PHQ+ve at baseline, the 12-month remission rate was 60.31% (95% CI: 54.08–66.53%). Both univariable and multivariable of non-linear mixed effects analysis was conducted to examine factors associated with remission. The result of multivariable model (Table 2) showed that having ≥2 co-morbidities was associated with the lowest likelihood of remission while being retired, was the only factor associated with an increased likelihood of remission. Baseline PHQ-9 score and doctor detection did not have any significant association with remission in both univariable and multivariable models. The lack of association between doctor detection and remission outcome within each PHQ-9 severity level were further confirmed with chi-square tests, all P values >0.2. There were no significant doctor factors associated with remission in the multivariable analysis.
Table 2.
Factors associated with remission and HRQOL at 12 months in the PHQ-9 positive cohort, the multivariable linear mixed effects models
| Remission (patient N = 322, doctor N = 54) | SF-12v2 PCS (patient N = 305, doctor N = 54) | SF-12v2 MCS (patient N = 305, doctor N = 54) | |
|---|---|---|---|
| Odds ratio (95% CI) | Coefficient (95% CI) | Coefficient (95% C.I.) | |
| Fixed effects | |||
| Intercept | 2.84 (0.34, 23.50) | 56.24* (48.37, 64.12) | 54.91* (45.20, 64.62) |
| Level 1: effects on patient factors | |||
| Gender (Male) | |||
| Female | 0.77 (0.42, 1.41) | −0.83 (−3.10, 1.44) | 1.02 (−1.78, 3.82) |
| Age | 0.98 (0.95, 1.00) | −0.10 (−0.20, 0.00) | 0.02 (−0.10, 0.14) |
| Ethnicity (Chinese) | |||
| Non-Chinese | 1.22 (0.21, 7.01) | 4.29 (−4.15, 12.74) | −6.54 (−16.95, 3.87) |
| Marital status (Married) | |||
| All others | 0.80 (0.45, 1.42) | −1.84 (−3.96, 0.28) | −1.26 (−3.87, 1.35) |
| Household monthly income (>HK$30000) | |||
| ≤HK$30000 | 1.58 (0.83, 3.00) | −1.33 (−3.76, 1.10) | 0.92 (−2.08, 3.92) |
| Education level (Secondary or tertiary education) | |||
| No formal or primary education | 0.98 (0.46, 2.07) | −1.87 (−4.58, 0.83) | 0.98 (−2.36, 4.31) |
| Working status (Employed) | |||
| Unemployed | 0.26 (0.04, 1.62) | −3.44 (−8.79, 1.91) | −5.54 (−12.13, 1.06) |
| Retired | 3.40* (1.29, 9.00) | −2.54 (−6.15, 1.08) | 5.98* (1.52, 10.43) |
| House-maker | 0.79 (0.33, 1.85) | −1.01 (−4.11, 2.10) | −2.40 (−6.22, 1.43) |
| Student | 1.15 (0.29, 4.59) | 1.12 (−3.77, 6.01) | −1.19 (−7.21, 4.84) |
| Smoking (Non-smoker) | |||
| Smoker | 0.63 (0.29, 1.37) | 1.14 (−1.69, 3.96) | −2.73 (−6.22, 0.76) |
| Drinking (Non-drinker) | |||
| Drinker | 1.46 (0.65, 3.28) | −1.15 (−4.14, 1.84) | 1.51 (−2.18, 5.20) |
| Exercise (With exercise) | |||
| No exercise | 1.24 (0.71, 2.15) | −2.55* (−4.57, −0.53) | 2.35 (−0.14, 4.85) |
| Number of co-morbidity (0) | |||
| 1 | 0.52 (0.27, 1.02) | −2.85* (−5.45, −0.24) | −0.53 (−3.74, 2.69) |
| ≥2 | 0.31* (0.15, 0.64) | −3.44* (−6.15, −0.73) | −3.50* (−6.84, −0.16) |
| Family history of mental illness (No) | |||
| Yes | 0.88 (0.44, 1.78) | 0.98 (−1.62, 3.58) | 2.22 (−0.99, 5.42) |
| Seen a western doctor in past 4 weeks (No) | |||
| Once or twice | 1.01 (0.59, 1.73) | −1.94 (−3.98, 0.10) | −1.95 (−4.47, 0.57) |
| More than twice | 0.48 (0.20, 1.12) | −9.57* (−12.63, −6.51) | −4.88* (−8.65, −1.11) |
| Seen a TCM practitioner in past 4 weeks (No) | |||
| Yes | 0.48* (0.24, 0.96) | −3.39* (−5.96, −0.83) | −2.65 (−5.81, 0.51) |
| District of residence (Hong Kong) | |||
| Kowloon | 0.91 (0.31, 2.70) | −0.65 (−4.80, 3.51) | 0.23 (−4.90, 5.36) |
| New Territories | 0.53 (0.19, 1.48) | −1.02 (−5.08, 3.04) | −1.58 (−6.59, 3.43) |
| Diagnosis of depression by doctor at baseline (No) | |||
| Yes | 0.90 (0.47, 1.72) | 0.62 (−1.75, 2.99) | −0.61 (−3.53, 2.32) |
| Take psychotropic drugs in the past 1 year (No) | |||
| Yes | 0.70 (0.39, 1.24) | 0.77 (−1.38, 2.93) | −3.89* (−6.54, −1.23) |
| PHQ-9 score at baseline | 1.00 (0.93, 1.08) | −0.24 (−0.51, 0.03) | −0.30 (−0.63, 0.04) |
| Level 2: effects on doctor factors | |||
| Gender (Male) | |||
| Female | 0.71 (0.35, 1.43) | 0.30 (−2.33, 2.93) | −1.55 (−4.80, 1.69) |
| Age | 1.00 (0.97, 1.03) | 0.04 (−0.07, 0.16) | −0.01 (−0.15, 0.12) |
| District of practice (Hong Kong) | |||
| Kowloon | 0.96 (0.31, 2.94) | 0.65 (−3.65, 4.94) | −2.18 (−7.47, 3.12) |
| New Territories | 1.43 (0.47, 4.28) | −1.12 (−5.41, 3.17) | 1.20 (−4.08, 6.49) |
| Previous education and training (None) | |||
| Family Medicine training | 1.70 (0.74, 3.90) | 4.83* (1.67, 7.99) | 2.10 (−1.80, 6.00) |
| Diploma in Psychological Medicine | 0.98 (0.40, 2.40) | 1.96 (−1.40, 5.33) | −0.91 (−5.06, 3.24) |
| Both of the above | 1.97 (0.57, 6.75) | 4.68* (0.19, 9.16) | 3.17 (−2.36, 8.70) |
| System setting (Public) | |||
| Private | 2.33 (0.95, 5.71) | 4.29* (0.87, 7.72) | 3.00 (−1.23, 7.22) |
| Error variance | |||
| Intercept | Not applicable | 0.00 (0.00) | 0.00 (0.00) |
| Intercept (doctor), variance, standard error | 0.00 (0.00) | 64.54 (5.23) | 98.14 (7.95) |
| Goodness-of-fit | |||
| Akaike Information Criterion (AIC) | 448.13 | 2206.55 | 2334.41 |
| Bayesian Information Criterion (BIC) | 576.47 | 2336.76 | 2464.62 |
Estimated with linear mixed effects models. The reference category of each patient and doctor factor was bracketed. For remission model, doctor intraclass correlation coefficient (ICC) = 4.49%. For SF-12v2 PCS model, doctor ICC = 13.17%. For SF-12v2 MCS model, doctor ICC = 0.00%.
*Statistically significant, P value <0.05.
Patient and doctor factors associated with HRQOL
Univariable and multivariable of linear mixed effects analyses were performed for the two SF-12v2 component scores by including patient factors as level 1 covariates and doctor factors as level 2 covariates. In the multivariable model (Table 2), lower (worse) 12-month SF-12v2 PCS were observed in those with no exercise habit; those with at least one co-morbidity; those who had seen a western doctor more than twice in the past 4 weeks; and those who had seen a Traditional Chinese Medicine (TCM) practitioner in the past 4 weeks. Conversely, higher (better) 12-month SF-12v2 PCS scores were observed in those who had attended a doctor with training in Family Medicine; or who worked in a private setting. Lower (worse) 12-month SF-12v2 MCS were observed in those with ≥2 co-morbidities; in those who had consulted a western doctor more than twice in the previous 4 weeks; and in those who had reported to have taken psychotropic medications in the past 12 months. Better 12-month SF-12v2 MCS scores were observed in those who were retired in both univariable and multivariable analyses.
Change in depressive symptoms and HRQOL scores over 12 months
Mean PHQ-9 and SF-12v2 component scores at each follow-up time point and changes in scores stratified by detection status are shown in Table 3. Without controlling for potential confounding effects, subjects who received a diagnosis of depression by the study doctor had significantly lower MCS at baseline and higher PHQ-9 scores at baseline, 3 and 6 months; however, there was no significant difference in mean PHQ-9 or mean PCS and MCS between detected and undetected groups at 12 months.
Table 3.
Comparison of PHQ-9 and SF-12v2 component scores by detection status in the PHQ-9 positive cohort
| Doctor detection (−ve) | Doctor detection (+ve) | P value | |
|---|---|---|---|
| Raw scores at each time point | |||
| PHQ-9 score (mean ± SD) | |||
| At baseline | 13.3±3.2 | 14.9±4.1 | <0.001* |
| At 12 weeks | 6.4±4.5 | 8.1±5.5 | 0.007* |
| At 26 weeks | 5.8±4.6 | 7.3±6.3 | 0.029* |
| At 52 weeks | 5.2±4.8 | 6.1±5.6 | 0.113 |
| SF-12v2 PCS (mean ± SD) | |||
| At baseline | 42.8±11.8 | 41.9±12.2 | 0.500 |
| At 12 weeks | 43.2±12.2 | 42.0±12.4 | 0.505 |
| At 26 weeks | 46.4±10.8 | 45.5±11.1 | 0.559 |
| At 52 weeks | 47.6±10.2 | 45.8±11.9 | 0.139 |
| SF-12v2 MCS (mean ± SD) | |||
| At baseline | 40.0±11.8 | 31.8±12.3 | <0.001* |
| At 12 weeks | 48.0±10.6 | 45.5±12.3 | 0.093 |
| At 26 weeks | 49.3±11.3 | 46.9±14.0 | 0.156 |
| At 52 weeks | 50.8±11.0 | 49.5±11.9 | 0.325 |
| Difference in scores between baseline and each subsequent follow-up time point | |||
| PHQ-9 score (mean ± SD) | |||
| Between baseline and 12 weeks | −7.0±5.0 | −7.2±6.3 | 0.785 |
| Between baseline and 26 weeks | −7.3±4.6 | −7.4±7.1 | 0.894 |
| Between baseline and 52 weeks | −8.1±5.5 | −8.8±6.6 | 0.313 |
| SF-12v2 PCS (mean ± SD) | |||
| Between baseline and 12 weeks | 0.8±12.2 | 0.6±12.8 | 0.904 |
| Between baseline and 26 weeks | 3.3±11.2 | 4.4±13.7 | 0.501 |
| Between baseline and 52 weeks | 5.3±11.1 | 3.8±12.8 | 0.270 |
| SF-12v2 MCS (mean ± SD) | |||
| Between baseline and 12 weeks | 6.9±12.2 | 14.7±13.5 | <0.001* |
| Between baseline and 26 weeks | 10.0±13.2 | 15.3±14.5 | 0.005* |
| Between baseline and 52 weeks | 10.7±13.4 | 16.8±14.7 | <0.001* |
*Significant difference (P < 0.05) between groups by independent t-test.
Between baseline and 12 months, PCS improved by 10% while MCS improved by 30% across the entire PHQ+ve cohort. The amount of improvement in PHQ-9 and SF-12v2 PCS was not significantly different between detected and undetected groups; however, the amount of improvement in SF-12v2 MCS was significantly better in those who had been identified by the doctor.
Health service utilization patterns
A comparison of self-reported mental health services uptake and GP consultations rates stratified by PHQ and detection status are shown in Table 4. Within the PHQ+ve cohort, doctor detection was associated with significantly higher rates of mental health service use across all time points, while GP consultation rates were only raised at 12 weeks but not at 26 or 52 weeks. At each time point as well as cumulatively over 12 months more patients reported receiving mental health services from a psychiatrist than from a GP.
Table 4.
Mental health service uptake and GP utilization rates stratified by PHQ-9 and doctor identification status at baseline
| Self-reported health service use | 12-week follow-up | 26-week follow-up | 52-week follow-up | Cumulative service uptake/use over 12 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | P value | n (%) | n (%) | P value | n (%) | n (%) | P value | n (%) | n (%) | P value | |
| 1) Among the entire longitudinal cohort | PHQ+ve | PHQ−ve | PHQ+ve | PHQ−ve | PHQ+ve | PHQ−ve | PHQ+ve | PHQ−ve | ||||
| Consulted a psychiatrist or psychiatric clinic in last 3 months | 40 (13.3%) | 73 (2.7%) | <0.001* | 44 (16.2%) | 90 (3.0%) | <0.001* | 77 (19.7%) | 116 (3.8%) | <0.001* | 97 (21.7%) | 178 (5.2%) | <0.001* |
| Received professional psychological treatment or counselling from GP in last 3 months | 31 (10.3%) | 34 (1.3%) | <0.001* | 17 (6.3%) | 18 (0.6%) | <0.001* | 13 (3.3%) | 14 (0.5%) | <0.001* | 52 (11.6%) | 60 (1.8%) | <0.001* |
| Received professional psychological treatment or counselling from psychologist in last 3 months | 5 (1.7%) | 12 (0.4%) | 0.022* | 6 (2.2%) | 11 (0.4%) | 0.002* | 10 (2.6%) | 14 (0.5%) | <0.001* | 16 (3.6%) | 30 (0.9%) | <0.001* |
| Received professional psychological treatment or counselling from social worker in last 3 months | 11 (3.6%) | 11 (0.4%) | <0.001* | 8 (3.0%) | 14 (0.5%) | <0.001* | 6 (1.5%) | 12 (0.4%) | 0.012* | 18 (4.0%) | 32 (0.9%) | <0.001* |
| Received professional psychological treatment or counselling from other people in last 3 months | 4 (1.3%) | 9 (0.3%) | 0.035* | 1 (0.4%) | 11 (0.4%) | 1.000 | 6 (1.5%) | 5 (0.2%) | 0.001* | 9 (2.0%) | 24 (0.7%) | 0.011* |
| Mean number GP consultations in past 4 weeks, mean (SD) | 1.063 (1.439) | 0.947 (1.287) | 0.142 | 0.944 (1.307) | 0.874 (1.301) | 0.396 | 1.124 (1.646) | 0.926 (1.325) | 0.023* | 1.076 (1.205) | 0.919 (1.017) | 0.008* |
| 2) Among the PHQ+ve longitudinal cohort | Detected | Not detected | Detected | Not detected | Detected | Not detected | Detected | Not detected | ||||
| Consulted a psychiatrist or psychiatric clinic in last 3 months | 18 (25.0%) | 21 (9.3%) | <0.001* | 27 (35.5%) | 16 (8.3%) | <0.001* | 42 (40.4%) | 34 (12.0%) | <0.001* | 54 (45.0%) | 42 (13.0%) | <0.001* |
| Received professional psychological treatment or counselling from GP in last 3 months | 15 (20.5%) | 15 (6.6%) | <0.001* | 12 (16.2%) | 3 (1.6%) | <0.001* | 6 (5.8%) | 7 (2.5%) | 0.120 | 29 (24.2%) | 21 (6.4%) | <0.001* |
| Received professional psychological treatment or counselling from psychologist in last 3 months | 3 (4.1%) | 2 (0.9%) | 0.095 | 2 (2.7%) | 3 (1.6%) | 0.622 | 6 (5.8%) | 4 (1.4%) | 0.026* | 8 (6.7%) | 7 (2.1%) | 0.033* |
| Received professional psychological treatment or counselling from social worker in last 3 months | 5 (6.8%) | 6 (2.6%) | 0.144 | 4 (5.3%) | 4 (2.1%) | 0.226 | 4 (3.9%) | 2 (0.7%) | 0.045* | 9 (7.5%) | 9 (2.8%) | 0.031* |
| Received professional psychological treatment or counselling from other people in last 3 months | 2 (2.8%) | 2 (0.9%) | 0.246 | 0 (0.0%) | 1 (0.5%) | 1.000 | 2 (1.9%) | 4 (1.4%) | 0.660 | 3 (2.5%) | 6 (1.8%) | 0.707 |
| Mean number GP consultations in past 4 weeks, mean (SD) | 1.452 (2.069) | 0.927 (1.146) | 0.042* | 1.074 (1.399) | 0.866 (1.272) | 0.293 | 1.409 (2.062) | 1.014 (1.443) | 0.074 | 1.290 (1.543) | 0.984 (1.027) | 0.046* |
Displayed above are counts and percentages of ‘Yes’ respondents among each group. Corresponding values of ‘No’ respondents are omitted. Patients were stratified according to their PHQ-9 screening outcome at baseline, and whether they were detected or not detected with depressive disorder by study doctor at baseline. Cumulative service use for mental health service uptake refers to having reported the particular mental health service use at least once during the 12-month follow-up period. Cumulative service use for GP consultations refers to average number of GP consultations in the past 4 weeks over the three follow-up time points.
*Significant difference (P < 0.05) between groups by chi-square test or Fisher exact test, as appropriate.
Discussion
To date, there has been no similar wide-scale longitudinal study on depression in the Hong Kong adult primary care population and the findings of this study contributes to the knowledge base of what happens to primary care patients in Asian settings following a depressive episode.
Symptom resolution and factors affecting remission
A 2014 meta-analysis of remission rates from untreated major depression in adult primary care patients estimated that around a quarter of cases remit within 3 months, a third within 6 months and half within 12 months (15). This was consistent with our study’s estimate for 12-month naturalistic observation of remission which included both treated and untreated cases. Although 60% of subjects reported symptom remission, around 40% appear to suffer a chronic or remitting course of illness with persistence of symptoms at 12 months. At greatest risk of poor prognosis are depressed patients with multiple physical co-morbidities. Similarly, an Australian study examining the association between chronic illness, multi-morbidity and depressive symptoms in primary care identified a clear dose–response relationship between the number of chronic physical problems and depressive symptoms, probably mediated via the patient’s HRQOL (16).
In many studies, higher baseline depression severity is a predictor for lower rates of remission at 12 months; however, this was not observed in our study (17,18). It appears that the trajectory course of depressive illness may differ in our setting to those in Western health care settings. This may be due to differences in detection or treatment rates, or possibly to social or health system factors, and requires further exploration.
Of note, retirement appeared to be the only protective patient factor associated with better prognosis, possibly reflecting the stressful nature of Hong Kong’s working environment.
Health service use
Mental health service uptake rates were increased over 12 months in patients who screened PHQ+ve with identified cases having significantly higher uptake rates than those who were not identified. PCP detection only raised GP consultation rates temporarily and there was no significant difference in GP consultation rates between detected and undetected cases at 6 or 12 months. Chinese have been identified as chronic under-users of mental health services (19), and GP detection appears to enable more patients to access mental health care, possibly by helping to overcome some of the personal or social stigmas associated with mental health interventions or by providing a practical means to access care for those seeking help for their mood disturbance. The high rate of psychiatric service use probably reflects the poorly defined role of primary care in delivering mental health services in our setting, as well as patient’s personal help-seeking preferences (20).
Impact of doctor detection
Although doctor identification did not have any association with 12-month remission rates, mean PHQ-9 scores, change in PHQ-9 scores or mean HRQOL PCS over 12 months, the amount of improvement to HRQOL MCS was significantly better in those who had their depression diagnosed by the doctor with the greatest impact occurring within the first 3 months. It appears that doctors are better at detecting those with poorer mental HRQOL and are more effective at facilitating recovery of patient’s functional status than improvement of their mood symptoms.
Although doctor factors did not have any significant association with prognosis, there were still some interesting findings noted. Firstly, patients who screened positive for depression were more likely to consult a younger doctor; however, doctors who were older were more likely to identify a patient as being depressed. Secondly, screened-negative patients who attended doctors in the public sector (who were all Family Medicine trained doctors) or doctors with training in both Family Medicine and Psychological Medicine had a lower risk of developing depression over the year. Similarly, HRQOL physical component scores were better at 12 months in those who had attended a doctor in the public sector or who had training in Family Medicine. It is difficult to prove a causal effect, but it appears attending a doctor with training in Family Medicine or with further training in psychological medicine, has protective benefits on mental well-being.
Strengths and limitations
One of the major strengths of this study was our success in recruiting a large number of PCPs to collaborate in this study. There are many service delivery options for patients seeking primary care in Hong Kong and our wide sampling of practice types captures this diversity. Despite this, there were limitations to our sampling strategy.
While we recruited subjects from all three regions of Hong Kong, ~40% were recruited from Hong Kong Island. Although the three regions differ in terms of geographic size, population number and socio-economy, a previous study of Hong Kong’s primary care found the morbidity patterns to be quite similar territory wide (7).
The cohort sample was self-selected which incurs a risk of self-selection bias.
Screening for depression was based on a subjective self-reported instrument and was not confirmed by a clinical diagnostic interview which would be the gold standard for diagnosis of depression. This study therefore reports the associations between patients with depressive symptoms as measured by the PHQ-9 and their longitudinal outcomes, and our findings may not be applicable to subjects with depressive symptoms measured or identified by other methods.
Finally, even though detection by PCP appears to have no association with remission rates or HRQOL in our study population, there may still be other benefits of PCP detection which this study did not measure.
Conclusions
In our setting, most primary care patients who screen positive for depression have mild and mostly self-limiting symptoms with impaired HRQOL. Over a 12-month period, while ~60% will experience remission and return to normal levels of HRQOL, 40% appear to have a chronic or remitting course of depressive symptomatology. Identification of depression by a doctor does not affect prognosis at 12 months, but is associated with a faster rate of recovery of HRQOL. PCP identification of depression is associated with better uptake rates for mental health services, but in this setting, it appears that more patients receive mental health treatments from a psychiatrist than a GP. This study provided estimates for remission and the factors influencing remission and HRQOL; however, longer duration studies are needed to establish reliable data on chronicity, relapse rates and factors associated with relapse. A closer examination of the trajectory paths for depression in this setting is needed to understand why patients with more severe symptoms do not have worse outcomes.
Declaration
Funding: this study was funded by the Hong Kong Food and Health Bureau’s Commissioned Research on Mental Health Policy and Service grant reference no. SMH-27.
Ethical approval: this study received approvals by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster, the Research Committee of Evangel Hospital, the Research Committee of Hong Kong Sanatorium and Hospital, the Research Committee of Matilda International Hospital, the Research Ethics Committee for Hong Kong Hospital Authority Kowloon East Cluster and Kowloon Central Cluster, and the Joint Chinese University of Hong Kong and Hong Kong Hospital Authority New Territories East Cluster Clinical Ethics Review Committee.
Conflict of interest: none.
Acknowledgements
The authors wish to acknowledge the contributions of Prof. Jane Gunn (University of Melbourne) and Prof. Walter Rosser (Queens University, Ontario) who helped as external advisors during the planning and drafting stages of the protocol. We also wish to acknowledge all the doctors of our Primary Care Research Network for their contribution to this study.
References
- 1. Murray CJ, Lopez AD. (eds.). The Global Burden of Disease: A Comprehensive Assessment of Morbidity and Disability From Disease, Injuries and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press, 1996. [Google Scholar]
- 2. Chin WY, Chan KT, Lam CL, et al. Detection and management of depression in adult primary care patients in Hong Kong: a cross-sectional survey conducted by a primary care practice-based research network. BMC Fam Pract 2014; 15: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chiu E. Epidemiology of depression in the Asia Pacific region. Australas Psychiatry 2004; 12 (suppl): S4–10. [DOI] [PubMed] [Google Scholar]
- 4. Cheung E, Lam L, Hung S. Hong Kong. In: Ghodse H. (ed). International Perspectives on Mental Health. London: RCPsych Publications, 2011. [Google Scholar]
- 5. Wun YT, Lam TP, Lam KF, Goldberg D, Li DK, Yip KC. How do patients choose their doctors for primary care in a free market? J Eval Clin Pract 2010; 16: 1215–20. [DOI] [PubMed] [Google Scholar]
- 6. Chin WY, Lam CL, Wong SY, et al. The epidemiology and natural history of depressive disorders in Hong Kong’s primary care. BMC Fam Pract 2011; 12: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lo YYC, Lam CLK, Mercer SW, et al. Morbidity and Management Patterns of Community-Based Primary Health Care Services in Hong Kong. Hong Kong: University of Hong Kong, 2009. [PubMed] [Google Scholar]
- 8. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999; 282: 1737–44. [DOI] [PubMed] [Google Scholar]
- 9. Yu X, Tam WW, Wong PT, Lam TH, Stewart SM. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry 2012; 53: 95–102. [DOI] [PubMed] [Google Scholar]
- 10. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Radolff LS. The CES-D Scale: a self report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401. [Google Scholar]
- 12. Hong Kong Department of Health. Hong Kong University Department of Community Medicine. 2003–2004 Hong Kong Population Health Survey http://www.chp.gov.hk/files/pdf/full_report_on_population_health_survey_2003_2004_en_20051024.pdf (accessed on 10 October 2014).
- 13. Ware JE, Jr, Kosinski M, Turner-Bowker DM, Gandek B. How to Score Version 2 of the SF-12 Health Survey. Lincoln, RI: QualityMetric Incorporated, 2002. [Google Scholar]
- 14. Lam CLK, Wong CKH, Lam ETP, Lo YYC, Huang WW. Population norm of Chinese (HK) SF-12 health survey_version 2 of Chinese adults in Hong Kong. Hong Kong Practitioner 2010; 32: 77–86. [Google Scholar]
- 15. Whiteford HA, Harris MG, McKeon G, et al. Estimating remission from untreated major depression: a systematic review and meta-analysis. Psychol Med 2013; 43: 1569–85. [DOI] [PubMed] [Google Scholar]
- 16. Gunn JM, Ayton DR, Densley K, et al. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatr Epidemiol 2012; 47: 175–84. [DOI] [PubMed] [Google Scholar]
- 17. Lamers F, Beekman AT, de Jonge P, Smit JH, Nolen WA, Penninx BW. One-year severity of depressive symptoms: results from the NESDA study. Psychiatry Res 2011; 190: 226–31. [DOI] [PubMed] [Google Scholar]
- 18. Stegenga BT, Kamphuis MH, King M, Nazareth I, Geerlings MI. The natural course and outcome of major depressive disorder in primary care: the PREDICT-NL study. Soc Psychiatry Psychiatr Epidemiol 2012; 47: 87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kung WW. Cultural and practical barriers to seeking mental health treatment for Chinese Americans. J Community Psychol 2004; 32: 27–43. [Google Scholar]
- 20. Wun YT, Lam TP, Goldberg D, Lam KF, Li KT, Yip KC. Reasons for preferring a primary care physician for care if depressed. Fam Med 2011; 43: 344–50. [PubMed] [Google Scholar]