Abstract
Background and Aims:
Both inhalational and intravenous anaesthetic agents are being used for neuroanaesthesia. Clinical trials comparing “propofol and sevoflurane” and “desflurane and sevoflurane” have been published. However, the comparison of all the three anaesthetics in neurosurgical patients has not been done. A randomised clinical study was carried out comparing propofol, sevoflurane and desflurane to find the ideal neuroanaesthetic agent.
Methods:
A total of 75 adult patients undergoing elective craniotomy for supratentorial tumours were included in the study. The patients were induced with morphine 0.1 mg/kg and thiopentone 4-6 mg/kg. Neuromuscular blockade was facilitated with vecuronium. The patients were randomised to receive propofol, sevoflurane or desflurane along with nitrous oxide in oxygen for maintenance of anaesthesia. The neuromuscular blockade was reversed following the surgery once the patients opened eyes or responded to verbal commands. The three anaesthetics were compared for their effects on haemodynamics, brain relaxation and emergence characteristics.
Results:
The mean arterial blood pressure during anaesthesia was comparable among the groups. The patients receiving sevoflurane had faster heart rates intraoperatively when compared to desflurane (P < 0.05). The brain relaxation scores at various intraoperative time frames were comparable among the three groups (P > 0.05). The time to response to verbal commands were significantly prolonged with use of sevoflurane (8.0 ± 2.9 min) when compared to propofol (5.3 ± 2.9 min) and desflurane (5.2 ± 2.6 min) (P = 0.003). However, the time to emergence and the number of patients who had early emergence (<15 min) were comparable among the groups (P > 0.05). The quality of emergence (coughing and emergence agitation), as well as postoperative complications, were also comparable among the three groups.
Conclusions:
All the three anaesthetic agents-propofol, sevoflurane and desflurane appear comparable and acceptable with regard to their clinical profile during anaesthesia in patients undergoing elective supratentorial surgeries.
Keywords: Anaesthetics: Propofol, sevoflurane and desflurane, Anaesthesia: Neuroanaesthesia, Surgery: Neurosurgery
INTRODUCTION
Anaesthesia for neurosurgical patients is a challenge. Continuous research in neuroanaesthesia over the last three decades has been dedicated towards understanding of anaesthetic agents, which have favourable cerebral physiology with minimal adverse effects.[1,2] The important goals of anaesthesia in neurosurgical patients are maintenance of haemodynamic stability, producing a slack brain and facilitating early emergence.[3,4] In this regard, nearly every anaesthetic agent has been used and the choice of anaesthetic agent, such as intravenous or volatile agent, has been considered an area of significant debate in neuroanaesthesia for last one and half decades at least.[1]
The three agents, which are very popular in the present scenario for use in the neurosurgical patients are propofol, sevoflurane and desflurane. Nevertheless, there is only an isolated study comparing sevoflurane and desflurane in neurosurgical patients with paucity of data comparing propofol, sevoflurane and desflurane in patients undergoing neurosurgery.[5] The present preliminary study was carried out to assess and compare the effects of propofol, sevoflurane and desflurane on haemodynamics, intraoperative brain relaxation and emergence characteristics in patients undergoing elective supratentorial tumour surgery.
METHODS
Patients of American Society of Anaesthesiologists physical status I and II, age ranging from 20 to 60 years of either sex with preoperative Glasgow coma score of 15 were included in the study. Approval was obtained from the Institutional Ethics and Research Committee. Signed informed consent was taken from all the patients. The tumour characteristics (type, size, mass effect and midline shift) were noted from the preoperative computed tomographic and magnetic resonance imaging scans. Randomisation to one of the three equally distributed groups was by computer generated random numbers and allocation to each group was done after picking from sequentially numbered opaque sealed envelopes. The three groups were group P (propofol), group S (sevoflurane) and group D (desflurane). Patients with ischaemic and/or congestive heart disease, hypertension, diabetes mellitus, chronic obstructive pulmonary disease, hepatic and renal dysfunction were excluded from the study. The surgery was performed by the experienced neurosurgeons of the institute who were unaware of the anaesthetic technique. The patients who had surgery related complications like vascular injury, massive intraoperative bleeding or injury to vital structures necessitating elective postoperative mechanical ventilation were excluded from the study.
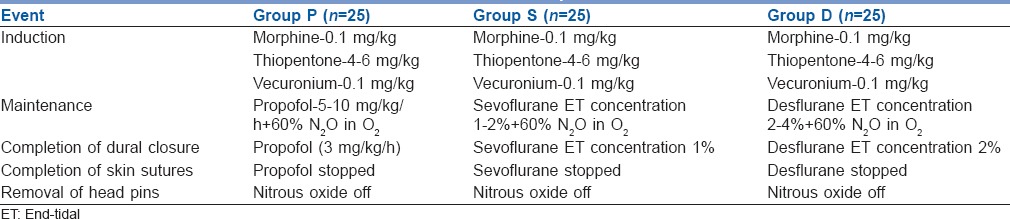
The preoperative anticonvulsants and steroids were continued until the morning of the surgery. Oral diazepam 10 mg was administered to all the patients the night before surgery. Preinduction monitoring (Datex-Ohmeda S/5 Avance©, Madison, WI, USA) consisted of 5-lead electrocardiography, heart rate (HR), arterial (radial) blood pressure and pulse oximetry. The mean of the three recordings of HR and mean arterial pressure (MABP) were registered as the baseline HR and MABP. Prior to induction, the patients were randomised in one of the three study groups. Induction was achieved with morphine 0.1 mg/kg, followed by thiopentone 4–6 mg/kg. Tracheal intubation was facilitated with vecuronium 0.1 mg/kg. Thiopentone 2 mg/kg was administered just before the four pin head holder was applied to suppress the pin response. Additional postinduction monitoring consisted of end-tidal carbon dioxide, nasopharyngeal temperature and neuromuscular monitoring. Ventilation was adjusted so as to achieve an end-tidal carbon dioxide concentration of around 30–35 mm Hg. Anaesthesia was maintained immediately after induction with either propofol (group P), sevoflurane (group S) or desflurane (group D) depending upon the randomised study group. The anaesthesia protocol was based on the current practice at our institution [Table 1]. Intermittent vecuronium was administered till the beginning of skin closure according to the need to maintain a maximum of single twitch on neurostimulation.
Table 1.
Anaesthesia protocol
At the beginning of skin incision, the patients were given mannitol 1 g/kg. The intraoperative brain relaxation was assessed by the surgeon at the following times (a) following raising of the bone flap, (b) following dural reflection, (c) during tumour excision, (d) following dural closure. The grading was done at each time point as (I) satisfied (II) not satisfied but can manage and (III) not satisfied, and intervention is required. Similarly at the time of raising the bone flap, a blinded anaesthesiologist also looked into the slackness of brain and graded it as (I) within the margin of the inner table of the skull, (II) within the margin of the outer table of the skull, and (III) outside the margin of the outer table of the skull.
Normal body temperature was maintained using a forced-air warming blanket. During the dural closure diclofenac, 2 mg/kg was given as an infusion along with injection ondansetron 4 mg intravenously. Following the completion of the surgery the patients were ventilated with high flow oxygen at 10 l/min. Once patients opened eyes or responded to verbal commands, the residual neuromuscular blockade was reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg. The trachea was extubated after (a) adequate reversal of neuromuscular blockade, (b) return of spontaneous respiration, (c) maintenance of adequate oxygen saturation on the pulse oximeter and (d) when the patient followed commands.[6] Thereafter the patients were moved to the Postanaesthesia Care Unit. The patients who had delayed emergence and could not be extubated were shifted to neurosurgical intensive care unit for ventilatory support. Intraoperative use of IV fluids, blood loss and urine output were recorded. The study period extended from the 15 min in preinduction period up to 1 h following extubation.
Heart rate and mean arterial blood pressure were recorded at the following time periods: preinduction, postintubation, during pin application, incision and thence every ½ hourly till dural closure. Subsequently, they were recorded during skin closure, pin removal, prior to and during extubation. In the postextubation period, the recordings were done every minute for the first 5 min and thence every 15 min till 1 h following extubation. Hypertension (defined as an increase of MABP >20% of the baseline value and sustained for >1 min) were treated with bolus of esmolol 1 mg/kg and thereafter 0.5 mg/kg. Hypotension (defined as a decrease in MABP <70 mm Hg for >1 min) was managed with increased rate of infusion of crystalloids. If this was not effective, a vasopressor (mephentermine) was used.
The time between anaesthetic (N2O) discontinuation and the response to verbal commands was recorded. Emergence time was defined as the time between N2O discontinuation and tracheal extubation, following, which the patient could be subjected to neurological examination. The time to response to verbal commands and emergence time were noted and compared among the three groups. The patients who could be extubated <15 min following cessation of anaesthesia were considered to have early emergence.[6] The patients who were not responsive and could be extubated >15 min following cessation of anaesthesia were categorised as delayed emergence. The patients who had >20% rise in MABP for more than a minute from the baseline values during emergence were considered to have emergence hypertension. Assessment for coughing was done following cessation of anaesthesia and prior to extubation as none, mild (single cough), moderate (more than one bout but unsustained [≤5 s] coughing), severe (sustained [≥5 s] bouts of coughing).[7] The reaction of the patient following extubation was categorised as agitated, calm or sedated. Agitated patients were those who required verbal, pharmacological or physical restraint. Those patients who were lying down comfortably and were cooperative were labelled as calm. Those patients who were responding to commands but were drowsy were labelled as sedated.
Postoperative complications such as pain, postoperative nausea and vomiting (PONV) and postoperative convulsions during 1st postoperative hour were noted. Pain was assessed using verbal rating scale of 0–10, 0 being no pain, 1–3 mild, 4–6 moderate, and 7 or more as severe pain. Rescue analgesic (score ≥5) consisted of diclofenac 1 mg/kg given as an infusion. Desaturation episodes (defined as the fall in oxygen saturation <95% on face mask with oxygen flow rate of 5–6 l/min) was noted. All the patients were interviewed on the second postoperative day for awareness during anaesthesia using the modified Brice interview.[8]
Sample size was estimated based on mean extubation time of 15.2 minutes with sevoflurane and 11.3 minutes with desflurane in a recent study.[5] To detect a 25% decrease in extubation time with standard deviation (S.D.) of 3.5, the calculated sample size was 17 per group at a power of 90% and confidence interval of 95% with an effect size of 1.1. To have adequate power of study despite possible dropouts and exclusion because of surgical reasons, the sample size was increased to 25 patients per group. The statistical analysis was carried out using Statistical Package for Social Sciences (SPSS Inc. 2013, version 22.0 for Windows, Armonk, NY, USA). Normally distributed data were presented as mean ± standard deviation. Categorised data were presented as frequency and/or percentage. The parametric data were compared among groups using One-way analysis of variance, whereas the posthoc analysis for the same data was performed using a Bonferroni correction. Nonparametric data were compared using Pearson's Chi-square or Kruskal-Wallis test. Categorical data were analysed with the Fisher's exact test. Post-hoc analysis for the nonparametric data were performed with Mann-Whitney test. A P < 0.05 was considered statistically significant.
RESULTS
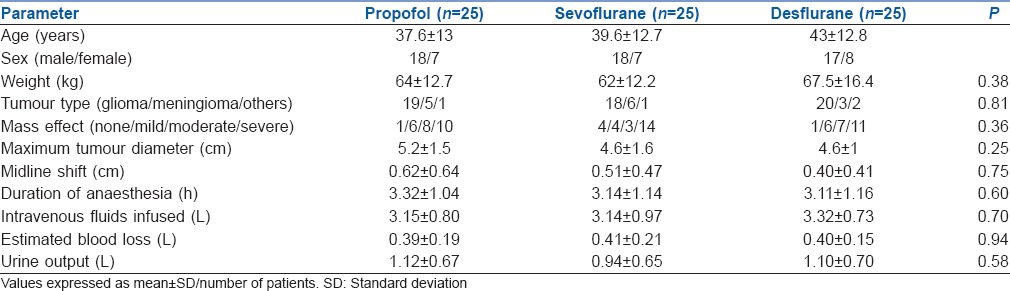
Seventy-five patients undergoing surgery for supratentorial tumour resection between December 2009 and February 2011 were enrolled in the study. The demographic profile was comparable among the three groups [Table 2]. The total duration of anaesthesia and intraoperative data were comparable in the three groups [Table 2].
Table 2.
Demographics and intraoperative data
The HRs were significantly different among the three groups during various time points of the study [Figure 1]. Post-hoc analysis shows that patients of sevoflurane group had significantly higher HRs when compared to desflurane during the intraoperative period. Similar significant difference was seen with sevoflurane use when compared to propofol during emergence [Figure 1]. The MABP values were similar among the three groups at various time frames [Figure 2]. The patients in the sevoflurane group witnessed significantly lower MABP at some time points when compared to propofol [Figure 2].
Figure 1.
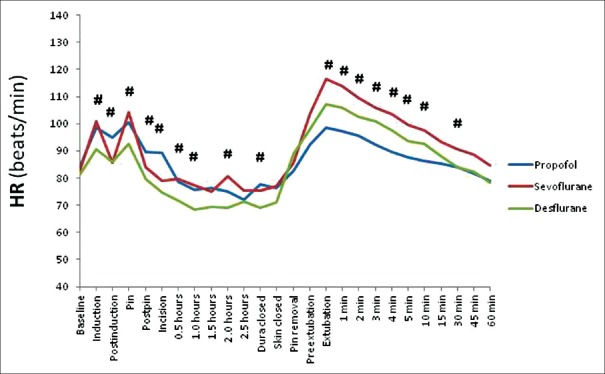
Data of heart rate at different stages of study period. *P < 0.05, comparing three groups at various time points
Figure 2.
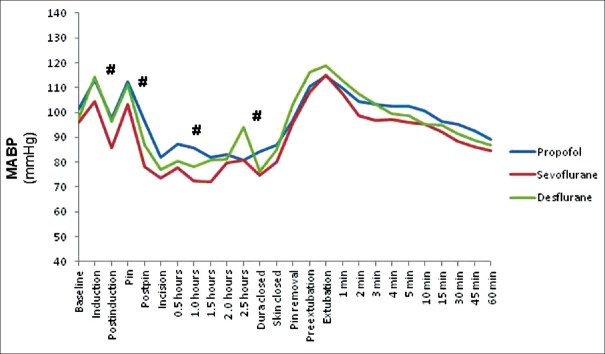
Data of mean arterial blood pressure at different stages of study period. *P < 0.05, comparing three groups at various time points
The brain relaxation scores were comparable among the three groups at various time points [Table 3].
Table 3.
Intraoperative brain relaxation scores

Six patients in the propofol, four in sevoflurane and three in desflurane groups were not extubated as they were unresponsive following surgery and were considered to have delayed emergence. Consequently, the data regarding emergence characteristics and postoperative complications have been analysed for 19 patients in the propofol, 21 patients in sevoflurane and 22 patients in the desflurane group [Table 4]. The time to response to verbal commands were significantly prolonged with use of sevoflurane (8.0 ± 2.9 min) when compared to propofol (5.3 ± 2.9 min) and desflurane (5.2 ± 2.6 min) (P = 0.003). Post-hoc analysis did not show any significant difference between propofol and desflurane group. However, the time to emergence was comparable among the groups [Table 4]. Similarly, the number of patients who had early (<15 min) emergence was similar among the three groups [Table 4]. Three-fourths of the patients had moderate coughing following cessation of anaesthesia irrespective of the status of emergence [Table 4]. Majority of the patients (84%) were calm following tracheal extubation [Table 4].
Table 4.
Emergence and postoperative characteristics
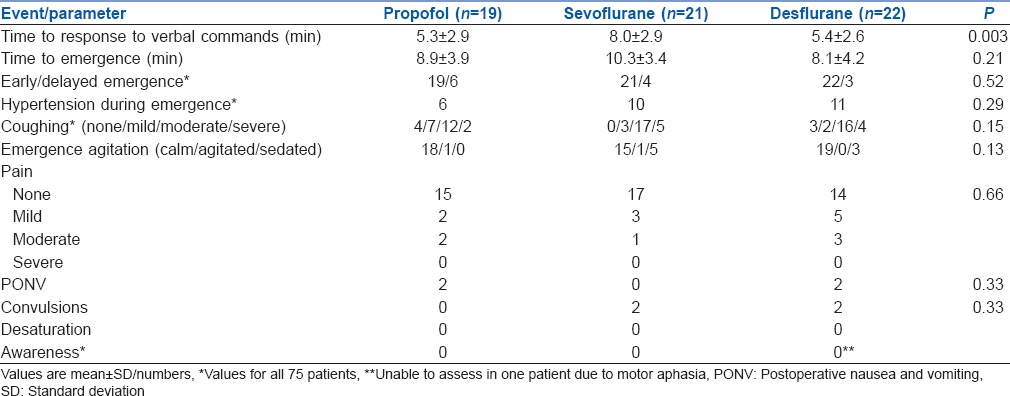
The incidence of postoperative complications was comparable among the three groups [Table 4]. Two patients in the propofol group and two in the desflurane group had PONV. Postoperative convulsions were observed in two patients in the sevoflurane group and two patients in the desflurane group. None of the patients in the three groups had any incidence of awareness under anaesthesia [Table 4].
DISCUSSION
The quest for an ideal anaesthetic agent, which subserves the neuroanaesthetic goals has now ushered us into an era whereby propofol, sevoflurane and desflurane have gained popularity. All the three anaesthetic agents in our study appear to subserve the objectives of maintaining haemodynamic stability, providing adequate brain conditions and facilitating early emergence. Considering the observations of our preliminary study, it is reasonable to interpret that propofol; sevoflurane as well as desflurane appear acceptable for use in practice of neuroanaesthesia.
Maintenance of stable haemodynamics is an important part of the neuroanaesthesia practice. Unacceptable hypotension can jeopardise the cerebral perfusion pressure. Similarly, perioperative hypertension is associated with intracranial hypertension, which may result in intracranial haemorrhage and aggravation of brain oedema.[9] Propofol, sevoflurane and desflurane produce dose-dependent decrease of systemic vascular resistance.[10] Propofol causes additional reduction of cardiac output.[11] Sevoflurane and desflurane may theoretically have an advantage of better haemodynamic control than propofol. However, our patients had similar haemodynamic profile with the use of three agents at most of the observations during the study period. Sevoflurane was associated with statistically lower MABP when compared to propofol at some points, which do not appear to have much clinical implication. Our results are similar to a recently conducted trial whereby sevoflurane use was associated with significantly lower blood pressure when compared to propofol.[12] However, other authors did not observe any significant increase in the percentage of patients who had changes in blood pressure with the use of sevoflurane when compared to propofol.[13] The haemodynamics were comparable among sevoflurane and desflurane groups in our study, which are similar to those reported in another study.[5] Sevoflurane had a greater influence on the HR in our study, which is analogous to a multicentre trial whereby sevoflurane use was associated with significant higher HR when compared to propofol.[12] Nevertheless, the MABP and HRs were within acceptable limits and did not demonstrate much clinical concern.
A slack brain facilitates a good surgical field and minimises the need for brain retraction.[14] Brain retraction pressure has been related to the occurrence of regional cerebral dysfunction.[15] Propofol is associated with dose-dependent reduction of cerebral blood flow (CBF) and cerebral metabolic rate (CMR) which results in a decrease of intracranial pressure (ICP).[16] Sevoflurane and desflurane causes reduction of CMR.[16] However, desflurane has more pronounced effect on increasing CBF and ICP than sevoflurane.[16] This should result in better brain relaxation with propofol and more brain swelling with desflurane anaesthesia. Our study demonstrates that the use of propofol, sevoflurane and desflurane have similar and acceptable effects on the brain relaxation scores at various stages of surgery. Similarly, no difference was found in the various studies conducted previously with the use of similar anaesthetic agents.[3,5,13,17] A recent meta-analysis shows that propofol-based anaesthesia is associated with lower initial ICP when compared to the volatile agent maintained anaesthesia.[18] However, this did not translate into better brain relaxation scores with use of propofol in comparison to volatile agent based anaesthesia.[18] One of the largest trial comparing three different anaesthetic techniques (propofol/fentanyl, isoflurane/nitrous oxide and fentanyl/nitrous oxide) could not demonstrate the superiority of one anaesthetic over the other with regards to either reduction of ICP or improved brain relaxation scores in patients undergoing elective supratentorial craniotomy.[2]
The emphasis in present clinical practice is to facilitate early awakening along with improved quality of emergence.[6,19] Early awakening allows for a timely detection of a neurological complication and reintervention if necessary. Emergence time in our study was the time from switching off of N2 O to extubation following which the patient can be subjected to neurological examination. The emergence time, which should be considered reasonable to facilitate early neurological evaluation has been suggested as 15 min.[6] Desflurane has the advantage of fast offset and recovery due to its low blood gas partition coefficient as compared to sevoflurane.[10] Recovery from propofol is rapid due to its short context-sensitive half-time and the decline in blood concentration required for awakening is somewhat <50% of that required for anaesthesia.[20] Though the time to response to verbal commands was significantly higher in the sevoflurane group when compared to the other two agents, there was no difference in the time to emergence among the three groups. Similarly, the number of patients who had early to those who had delayed emergence were comparable in the three groups. In one study, the time to extubation was shorter in the sevoflurane group when compared to propofol group.[11] In contradiction, other authors did not observe any difference in extubation times following use of propofol or sevoflurane.[3] When desflurane was compared to sevoflurane, the extubation time and recovery time were faster with desflurane.[5] The time to response to verbal commands was shorter with desflurane when compared to sevoflurane in our study. However, we did not observe any significant difference in the time to emergence among the three groups. Most of the trials have demonstrated acceptable emergence with all the three anaesthetic agents if clinical criteria of early emergence (≤15 min) is considered.[3,5,13,17]
Smooth emergence entails prevention of emergence hypertension and the patients experiencing minimum coughing during emergence. Moreover, the patients should remain calm and free of pain as well as PONV. The incidence of emergence hypertension in our study was comparable among the groups, which is similar to an observation in a study with the use of propofol and isoflurane.[6] The use of low dose fentanyl infusion during craniotomy closure has been demonstrated to be useful in limiting the emergence hypertension.[6] Coughing was observed in the majority of the patients with 72% of the patients experiencing a moderate degree of coughing. Coughing can be deleterious as it can lead to Valsalva effects, causing an increase in ICP.[21] None of the three agents had any favourable profile as far as coughing during emergence was concerned. One study reported decreased coughing scores with the use of propofol when compared to sevoflurane in patients undergoing cervical spine surgery.[22] The residual concentration of remifentanil at the end of surgery was higher in the propofol group in their study, which could have resulted in lower coughing scores in the propofol group. The effect of propofol, sevoflurane and desflurane were similar in the patients with regards to emergence agitation and immediate postoperative pain.
Neurosurgical population are at higher risk for PONV.[23] Two patients in the propofol group and two in the desflurane group had PONV. Propofol is widely believed to be associated with decreased incidence of PONV when compared to inhalational agents. However, our study did not observe any significant difference among the three groups. Convulsions following craniotomy can affect the postoperative outcome of the patients. Though the incidence of immediate postoperative convulsions following craniotomy has been reported to be 3%, the incidence of early postoperative convulsions was 6% in our study.[24] There is no strong clinical evidence to support use of one anaesthetic agent over the other in terms of anticonvulsive effects.[25] The results of our study are similar to previously published studies, which did not demonstrate any significant difference in the incidence of early postoperative convulsions with use of different anaesthetic agents.[3,13]
The present study has limitations of its own. The effects of three anaesthetic agents on brain physiology and brain conditions were majorly subjective. Though the satisfaction of the operating surgeon is important, monitoring of ICP during first burr hole in the skull would have been ideal. Another drawback was that it was not possible to double-blind this study, which could be a potential source of bias. The study compared three anaesthetic agents based on the institutional protocol. Though the depth of anaesthesia was monitored using end-tidal concentrations for sevoflurane and desflurane groups, the study could not monitor the anaesthetic depths for propofol group. The present study is a preliminary trial. The results of the present study need to be corroborated by conducting a large multicentric randomised clinical trials. Moreover, it will be important to study cost effectiveness of anaesthetic agents as inhalational anaesthesia has been associated with reduced costs when compared to propofol.[26]
CONCLUSION
All the three anaesthetic agents had comparable effects on haemodynamics, brain relaxation scores and emergence characteristics. The results of our preliminary study suggest that propofol, sevoflurane and desflurane appear to be similar and acceptable for neuroanaesthesia in patients undergoing elective supratentorial tumour surgery.
ACKNOWLEDGEMENT
We are grateful to the residents of the Departments of Anaesthesia and Neurosurgery for their help in conducting this study. We kindly acknowledge Mrs. Kusum Chopra for statistical assistance.
Footnotes
Source of Support: Institutional Resources.
Conflict of Interest: None declared
REFERENCES
- 1.Engelhard K, Werner C. Inhalational or intravenous anesthetics for craniotomies. Pro inhalational? Curr Opin Anaesthesiol. 2006;19:504–8. doi: 10.1097/01.aco.0000245275.76916.87. [DOI] [PubMed] [Google Scholar]
- 2.Todd MM, Warner DS, Sokoll MD, Maktabi MA, Hindman BJ, Scamman FL, et al. A prospective, comparative trial of three anesthetics for elective supratentorial craniotomy. Propofol/fentanyl, isoflurane/nitrous oxide, and fentanyl/nitrous oxide. Anesthesiology. 1993;78:1005–20. doi: 10.1097/00000542-199306000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Magni G, Baisi F, La Rosa I, Imperiale C, Fabbrini V, Pennacchiotti ML, et al. No difference in emergence time and early cognitive function between sevoflurane-fentanyl and propofol-remifentanil in patients undergoing craniotomy for supratentorial intracranial surgery. J Neurosurg Anesthesiol. 2005;17:134–8. doi: 10.1097/01.ana.0000167447.33969.16. [DOI] [PubMed] [Google Scholar]
- 4.Bruder N, Ravussin P. Recovery from anesthesia and postoperative extubation of neurosurgical patients: A review. J Neurosurg Anesthesiol. 1999;11:282–93. doi: 10.1097/00008506-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Magni G, Rosa IL, Melillo G, Savio A, Rosa G. A comparison between sevoflurane and desflurane anesthesia in patients undergoing craniotomy for supratentorial intracranial surgery. Anesth Analg. 2009;109:567–71. doi: 10.1213/ane.0b013e3181ac1265. [DOI] [PubMed] [Google Scholar]
- 6.Bhagat H, Dash HH, Bithal PK, Chouhan RS, Pandia MP. Planning for early emergence in neurosurgical patients: A randomized prospective trial of low-dose anesthetics. Anesth Analg. 2008;107:1348–55. doi: 10.1213/ane.0b013e31817f9476. [DOI] [PubMed] [Google Scholar]
- 7.Aouad MT, Al-Alami AA, Nasr VG, Souki FG, Zbeidy RA, Siddik-Sayyid SM. The effect of low-dose remifentanil on responses to the endotracheal tube during emergence from general anesthesia. Anesth Analg. 2009;108:1157–60. doi: 10.1213/ane.0b013e31819b03d8. [DOI] [PubMed] [Google Scholar]
- 8.Enlund M, Hassan HG. Intraoperative awareness: Detected by the structured Brice interview? Acta Anaesthesiol Scand. 2002;46:345–9. doi: 10.1034/j.1399-6576.2002.460402.x. [DOI] [PubMed] [Google Scholar]
- 9.Basali A, Mascha EJ, Kalfas I, Schubert A. Relation between perioperative hypertension and intracranial hemorrhage after craniotomy. Anesthesiology. 2000;93:48–54. doi: 10.1097/00000542-200007000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Stoelting RK, Hillier SC, editors. Pharmacology and Physiology in Anaesthetic Practice. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2006. Inhaled anaesthetics; pp. 42–86. [Google Scholar]
- 11.Stoelting RK, Hillier SC, editors. Pharmacology and Physiology in Anaesthetic Practice. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2006. Nonbarbiturate intravenous anaesthetic drugs; pp. 155–78. [Google Scholar]
- 12.Citerio G, Pesenti A, Latini R, Masson S, Barlera S, Gaspari F, et al. A multicentre, randomised, open-label, controlled trial evaluating equivalence of inhalational and intravenous anaesthesia during elective craniotomy. Eur J Anaesthesiol. 2012;29:371–9. doi: 10.1097/EJA.0b013e32835422db. [DOI] [PubMed] [Google Scholar]
- 13.Lauta E, Abbinante C, Gaudio AD, Aloj F, Fanelli M, de Vivo P, et al. Emergence times are similar with sevoflurane and total intravenous anaesthesia: Results of a multicentric RCT of patients scheduled for elective supratentorial craniotomy. J Neurosurg Anesthesiol. 2010;22:110–8. doi: 10.1097/ANA.0b013e3181c959da. [DOI] [PubMed] [Google Scholar]
- 14.Bruder N, Ravussin PA. Supratentorial masses: Anaesthetic considerations. In: Cottrell JE, Young WL, editors. Cottrell and Young's Neuroanaesthesia. 5th ed. Philadephia: Elsevier; 2010. pp. 184–202. [Google Scholar]
- 15.Herrick IA, Gelb AW, Manninen PH, Reichman H, Lownie S. Effects of fentanyl, sufentanil, and alfentanil on brain retractor pressure. Anesth Analg. 1991;72:359–63. doi: 10.1213/00000539-199103000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Sakabe T, Matsumoto M. Effects of anaesthetic agents and other drugs on cerebral blood flow, metabolism and intracranial pressure. In: Cottrell JE, Young WL, editors. Cottrell and Young's Neuroanaesthesia. 5th ed. Philadelphia: Elseviers; 2010. pp. 78–94. [Google Scholar]
- 17.Sneyd JR, Andrews CJ, Tsubokawa T. Comparison of propofol/remifentanil and sevoflurane/remifentanil for maintenance of anaesthesia for elective intracranial surgery. Br J Anaesth. 2005;94:778–83. doi: 10.1093/bja/aei141. [DOI] [PubMed] [Google Scholar]
- 18.Chui J, Mariappan R, Mehta J, Manninen P, Venkatraghavan L. Comparison of propofol and volatile agents for maintenance of anesthesia during elective craniotomy procedures: Systematic review and meta-analysis. Can J Anaesth. 2014;61:347–56. doi: 10.1007/s12630-014-0118-9. [DOI] [PubMed] [Google Scholar]
- 19.Lin BF, Ju DT, Cherng CH, Hung NK, Yeh CC, Chan SM, et al. Comparison between intraoperative fentanyl and tramadol to improve quality of emergence. J Neurosurg Anesthesiol. 2012;24:127–32. doi: 10.1097/ANA.0b013e31823c4a24. [DOI] [PubMed] [Google Scholar]
- 20.Reves JG, Glass PS, Lubarsky DA, McEvoy MD, Martinez-Ruiz R. Intravenous anaesthetics. In: Miller RD, editor. Miller's Anaesthesia. 7th ed. Philadelphia: Elsevier's; 2010. pp. 719–68. [Google Scholar]
- 21.Prabhakar H, Bithal PK, Suri A, Rath GP, Dash HH. Intracranial pressure changes during Valsalva manoeuvre in patients undergoing a neuroendoscopic procedure. Minim Invasive Neurosurg. 2007;50:98–101. doi: 10.1055/s-2007-982505. [DOI] [PubMed] [Google Scholar]
- 22.Hans P, Marechal H, Bonhomme V. Effect of propofol and sevoflurane on coughing in smokers and non-smokers awakening from general anaesthesia at the end of a cervical spine surgery. Br J Anaesth. 2008;101:731–7. doi: 10.1093/bja/aen271. [DOI] [PubMed] [Google Scholar]
- 23.Latz B, Mordhorst C, Kerz T, Schmidt A, Schneider A, Wisser G, et al. Postoperative nausea and vomiting in patients after craniotomy: Incidence and risk factors. J Neurosurg. 2011;114:491–6. doi: 10.3171/2010.9.JNS10151. [DOI] [PubMed] [Google Scholar]
- 24.Manaka S, Ishijima B, Mayanagi Y. Postoperative seizures: Epidemiology, pathology, and prophylaxis. Neurol Med Chir (Tokyo) 2003;43:589–600. doi: 10.2176/nmc.43.589. [DOI] [PubMed] [Google Scholar]
- 25.Perks A, Cheema S, Mohanraj R. Anaesthesia and epilepsy. Br J Anaesth. 2012;108:562–71. doi: 10.1093/bja/aes027. [DOI] [PubMed] [Google Scholar]
- 26.Dolk A, Cannerfelt R, Anderson RE, Jakobsson J. Inhalation anaesthesia is cost-effective for ambulatory surgery: A clinical comparison with propofol during elective knee arthroscopy. Eur J Anaesthesiol. 2002;19:88–92. doi: 10.1017/s0265021502000157. [DOI] [PubMed] [Google Scholar]


