Abstract
Background and Aims:
Insertion of laryngeal mask airway (LMA) requires adequate depth of anaesthesia, which provides jaw relaxation and suppression of upper airway reflexes. Propofol can provide these conditions especially when combined with narcotics. This study had been designed to find out the effect-site concentration (EC50) of propofol using target controlled infusion (TCI) when fentanyl or morphine is added as an adjuvant.
Methods:
Patients satisfying inclusion criteria were divided into fentanyl and morphine groups. Intravenous glycopyrrolate 0.2 mg was given 15 min before induction. Patients were given either intravenous fentanyl (1 μg/kg) or morphine (0.1 mg/kg) before propofol infusion depending on the group. Patients in either groups were induced by continuous infusion of propofol at an EC of 6 μg/mL by TCI with Schneider pharmacokinetic model. The LMA supreme of appropriate size was inserted 1 min after achieving target concentration. Patient movement at LMA insertion or within 1 min of insertion was classified as failure. For subsequent patients, the target EC was increased/decreased depending on previous patients' response. Dixons up and down method was used to determine the EC50. The EC50 is defined as the mean of crossover midpoints in each pair of failure to success.
Results:
The EC50 of propofol in the fentanyl group for LMA insertion was 5.95 ± 0.6 μg/ml and morphine group was 5.75 ± 0.8 μg/ml. No significant difference in insertion conditions was noticed between the two groups (P = 0.3).
Conclusion:
We conclude that there was no significant difference in propofol EC50 for insertion of LMA and insertion conditions were similar when fentanyl or morphine was used as an adjuvant drug.
Keywords: Effect-site concentration, laryngeal mask airway, propofol
INTRODUCTION
Propofol, an alkyl phenol compound is an intravenous anaesthetic agent used since early 1980s for induction and maintenance of anaesthesia in day care surgery.[1] It has the unique property of rapid induction with rapid and complete recovery from general anaesthesia. Propofol is considered as the superior induction agent for achieving the optimum laryngeal mask airway (LMA) insertion conditions compared with thiopentone and other intravenous induction agents.[2] The recommended intravenous bolus dose of propofol at 2.5 mg/kg could be associated with significant cardiovascular and respiratory depression.[3]
Several manual infusion regimens were put forth to reduce the dose requirement and ensure rapid emergence, but their use was limited by the inaccurate prediction of propofol plasma concentration (Cp). Target controlled infusion (TCI) is an intravenous drug delivery system where anaesthesiologists can set the target plasma or effect-site concentration (EC50 ) to achieve the desired clinical effect.[4] TCI involves computer control of an infusion pump thereby administering drug according to preprogrammed computerised pharmacokinetic model.[5] Some systems have the facility to plot and display the calculated effect-site concentration of propofol. Performance of these systems have been analysed for reliability.[6] The Schnider pharmacokinetic EC model is one such model used for TCI. This EC50 of propofol at which successful LMA insertion is possible in 50% of adults is referred to as EC50 for LMA.[7] Most commonly used opioids are fentanyl, remifentanil, alfentanil owing to their rapid onset and shorter duration of action.[8] However, little is known about optimal EC of propofol required for successful LMA insertion using morphine as adjuvant. We conducted this study to determine the EC of propofol for facilitation of LMA insertion using fentanyl or morphine as adjuvant opioids in South Indian population.
METHODS
This prospective randomised study was conducted at a teaching hospital in South India from January 2012 to June 2013 after approval from the institutional research and human ethics committee. After a thorough preoperative evaluation, patients with ASA physical status I-II and aged between 18 and 60 years scheduled for elective surgery under general anaesthesia were included in the study. Patients with cervical spine disease, Mallampati classification III or IV, a mouth opening of < 2.5 cm, patients with reactive airway disease and risk of aspiration and thyroid disease were excluded. Patients were advised a fasting period of at least 6 h. They were premedicated with tablet diazepam 10 mg and tablet ranitidine 150 mg orally on the night before surgery and the morning of surgery. In the preanaesthetic preparation room, an 18G venous cannula was secured, and Ringer's lactate solution administered at 10 ml/kg. Intravenous glycopyrrolate 0.2 mg/kg was administered intravenously 10–15 min before anaesthesia induction to reduce oral secretions.
In the operation theatre, standard monitoring using electrocardiogram, pulse oximetry, noninvasive blood pressure monitoring and end-tidal CO2 concentration were performed, and values recorded at regular intervals. The patients were randomised to one of the two groups by closed envelope technique. Group F received fentanyl 1 μg/kg 5 min before propofol infusion, and Group M received morphine 0.1 mg/kg 15 min before propofol infusion. The investigator was not blinded to the TCI pump as the patient's response determined the dose for the next patient. All patients were preoxygenated using 100% oxygen for 3 min. All patients received intravenous lignocaine 20 mg with venous occlusion for 2 min to relieve pain due to propofol infusion. To start with, patients in both the groups received propofol infusion at an EC of 6 μg/mL by TCI pump (Injectomat TIVA Angilia³, Fresenius Kabi, France) with Schnider pharmacokinetic model software. LMA was inserted 1 min after achieving equilibrium between plasma and EC50 [Figure 1].
Figure 1.

Target controlled infusion pump showing equilibration between plasma concentration and effect concentration. A: Plasma concentration, B: Effect-site concentration, C: Target effect-site concentration
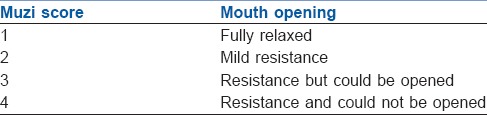
Anaesthesiologist involved in the study had the experience of inserting 50 LMA Supreme© before starting the study. The same anaesthesiologist had inserted LMA in all cases of study. The LMA of appropriate size according to body weight was used. The LMA cuff was deflated completely and lubricated. LMA was introduced through the midline of the mouth, sliding it smoothly along the hard palate with its tip pressed against the palate until resistance was felt while the free hand held the patient's mouth open. The finger was not introduced into the mouth. Patient movement at the time of LMA insertion or within 1 min of insertion was classified as a failure of insertion. “Movement” was defined as coughing, straining, bucking, laryngospasm or gross purposeful movement. Mouth opening was classified using Muzi score [Table 1].[9] Muzi score of >2 was defined as significant resistance. LMA insertion was attempted only once, and if patient movement was noticed, the further course of anaesthesia maintenance was decided by attending anaesthesiologist. Rescue measures for an apnoeic patient included gentle, positive pressure ventilation via bag and mask. Fall in systolic blood pressure <90 mmHg was treated with fluid bolus of 10 ml/kg and bradycardia with Injection atropine 0.6 mg IV.
Table 1.
Muzi score for jaw relaxation
To determine the EC50 modified Dixon's up- and down- method, was adopted.[10] The first patient received an EC of propofol at 6 μg/mL. The response of each patient determined the EC of propofol for the next patient. If the insertion of the LMA was successful, then the target EC was decreased by a step of 1 μg/ml in the next patient. If the insertion was a failure, then the target EC in the next patient was increased by 1 μg/ml. The EC of propofol for each patient was plotted sequentially to identify the negative-positive crossover. In modified Dixon's method, the first stage consisted of an up- and down- sequence of steps of 1 μg/mL until three changes of response type were observed. After the first three such “negative-positive” crossovers, the step change of dose was reduced by half to 0.5 μg/ml until next three such “negative-positive” crossovers was obtained.
The EC50 of propofol which enabled successful laryngeal mask insertion was determined by calculating the mean of midpoint dose of all independent pairs of crossover points obtained in the modified Dixons up and down graph. All data were recorded in Microsoft excel (Microsoft) chart, and statistical analysis was done by Statistical Package for Social Sciences (SPSS) software 19 version (IBM). Demographics were analysed using unpaired t-test for parametric data and Mann–Whitney test for nonparametric data. Haemodynamic data were analysed using one-way ANOVA to find statistical difference within and between the two groups.
RESULTS
The study was completed with 41 patients as the required “negative-positive” crossovers were achieved. The demographic profile was comparable with no statistically significant difference between the groups [Table 2].
Table 2.
Demographic data for fentanyl and morphine groups

In fentanyl group the 3 pairs of failure to success was reached in nine patients while using 1 μg/ml steps and further 10 patients for steps of 0.5 μg/ml [Figure 2]. EC50 was calculated from the mean of midpoint dose of all independent failure to success pairs after obtaining crossover points. The EC50 for propofol was found to be 5.95 ± 0.6 μg/ml with fentanyl 1 μg/kg as adjuvant. In morphine group the 4 pairs of failure to success was reached in 14 patients while using 1 μg/ml steps and further eight patients for steps of 0.5 μg/ml [Figure 3]. The EC50 for propofol was found to be 5.75 ± 0.8 μg/ml. No significant difference in insertion conditions was noticed between the two groups (P = 0.3).
Figure 2.
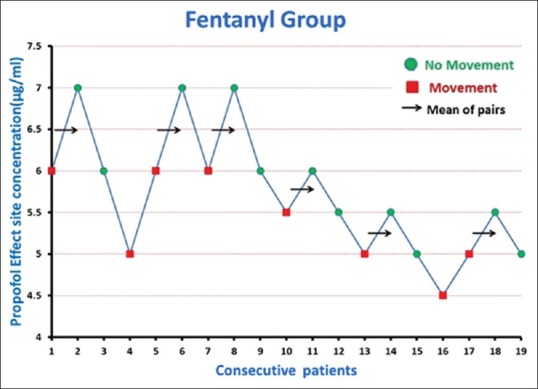
Effect-site concentration of propofol plotted in consecutive patients to identify the negative-positive crossovers in the fentanyl group
Figure 3.
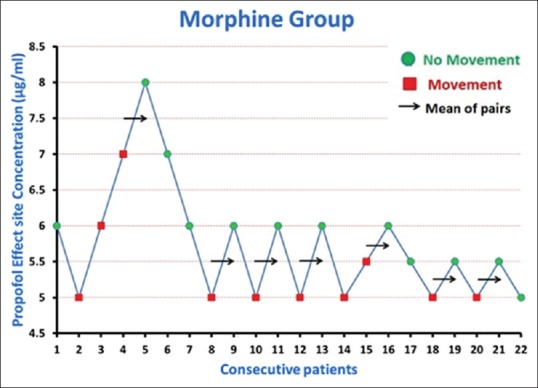
Effect-site concentration of propofol plotted in consecutive patients to identify the negative-positive crossovers in the morphine group
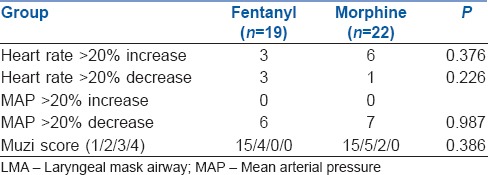
The 20% change in either direction, in heart rate and mean arterial pressure from the baseline to the time after LMA insertion and the mouth opening condition according to Muzi score are shown in Table 3.
Table 3.
Haemodynamic changes and Muzi grading during LMA insertion for fentanyl and morphine groups
DISCUSSION
Propofol has been widely used for LMA insertion because it provides greater inhibitory effect on pharyngeal and laryngeal reactivity than other commonly used intravenous induction agents like thiopentone.[9] Induction with propofol alone requires a high plasma target concentration of 7–9 μg/ml, which results in cardiovascular or respiratory depression.[9] The target EC50 of propofol to insert a LMA was recently reported as 7.3 ± 0.2 μg/ml.[11] The addition of opioids such as fentanyl, remifentanil, alfentanil during induction reduces the amount of propofol required and provides better haemodynamic stability.[2] However, little is known about optimal EC50 of propofol for LMA insertion using morphine as adjuvant. Most of the studies were conducted using plasma target concentration for propofol infusion.[2,3,12,13] In our study, we decided to use EC50 to infuse propofol and estimate the EC50 value of propofol for successful LMA insertion with fentanyl and morphine as adjuvants.
Various pharmacokinetic models were developed and incorporated in the TCI pump. The first-generation systems allowed the user to target the Cp. Later, the Keo value was incorporated allowing an estimate of the EC to be made and to be displayed as additional information.[5] In the present study, TCI using Schneider model was used in all patients. Sample size is not required in Dixon up- and down- method as the study will be terminated when the required up and downs are achieved.[10]
In our study, we used equipotent dose of fentanyl 1 μg/kg and morphine 0.1 mg/kg.[14] As peak effect of intravenous fentanyl is 5 min and intravenous morphine is 15 min, they were given at 5 or 15 min before propofol infusion as per the groups.[14] Opioids were given before propofol infusion to observe for any decrease in respiratory rate.
This study of 41 patients who underwent elective surgeries under general anaesthesia shows that the required EC of propofol at which successful LMA insertion is possible in 50% of adult with fentanyl 1 μg/kg was 5.95 ± 0.6 μg/ml and with morphine 0.1 mg/kg was 5.75 ± 0.8 μg/ml using modified Dixons up and down graph.
A study conducted by Kodaka et al.[8] estimated EC50 of propofol with saline (control group) and at different fentanyl concentration ranging from 0.5 μg/kg to 2 μg/kg. They found that EC50 LMA for the control, fentanyl 0.5, 1 and 2 μg kg-1 groups were 3.25, 2.06, 1.69 and 1.50 μg ml-1, respectively; those of all fentanyl groups were significantly lower than that of control. They suggested that pretreatment with fentanyl 0.5 μg/kg reduces required EC50 concentration of propofol with minimal respiratory depression. Similar study was done by Yumura et al.[15] suggested that EC50 of propofol for LMA insertion was decreased by supplementing 0.25 μg/kg fentanyl without haemodynamic or respiratory depression.
Laryngeal mask airway insertion was successful in six out of nine patients in the fentanyl group and eight out of ten in the morphine group with EC50 above 6 μg/ml in our study. Muzi score was used to assess the mouth opening for successful LMA insertion. We found that in the fentanyl group jaw was fully relaxed above EC50 of 5 μg/ml whereas in morphine group mild resistance was found to mouth opening even at 6 μg/ml. Kim et al.[7] used Muzi score for mouth opening as one of the criteria to decide the success or failure of LMA insertion in a study to determine the EC50 of remifentanil.
There was no statistical difference in heart rate at various intervals (after adjuvant, after propofol infusion, after LMA insertion) within the group compared to the baseline value. There was also no statistical difference in heart rate between two groups at various intervals. This could be due to administration of intravenous glycopyrrolate 0.2 mg to all patients 15 min before propofol induction.
A 20% fall in mean arterial pressure from baseline to the time after LMA insertion was observed in six patients in the fentanyl and seven patients in the morphine group. Rapid administration of propofol in Schneider pharmacokinetic model results in an early peak drug concentration in plasma, thus providing a larger gradient for propofol uptake into the effect-site and for drug redistribution to other body tissues. The fall in mean arterial pressure was related to higher peak blood concentration achieved immediately after propofol infusion using schneider pharmacokinetic model.[9]
CONCLUSION
The effect site concentration of propofol for LMA insertion in fentanyl group was found to be 5.95 ± 0.6 μg/kg and in morphine group to be 5.75 ± 0.8 μg/kg (Dixon's method). No significant difference in insertion conditions was noticed between the two groups (P = 0.3).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Fulton B, Goa KL. Propofol. A pharmacoeconomic appraisal of its use in day case surgery. Pharmacoeconomics. 1996;9:168–78. doi: 10.2165/00019053-199609020-00008. [DOI] [PubMed] [Google Scholar]
- 2.Park HJ, Kang HS. Comparison of propofol ED50 and insertion conditions of LMA between Fentanyl and Alfentanil Adjuvant Group. Korean J Anesthesiol. 2007;52:21. [Google Scholar]
- 3.Wong CM, Critchley LA, Lee A, Khaw KS, Ngan Kee WD. Fentanyl dose-response curves when inserting the LMA Classic laryngeal mask airway. Anaesthesia. 2007;62:654–60. doi: 10.1111/j.1365-2044.2007.05057.x. [DOI] [PubMed] [Google Scholar]
- 4.Guarracino F, Lapolla F, Cariello C, Danella A, Doroni L, Baldassarri R, et al. Target controlled infusion: TCI. Minerva Anestesiol. 2005;71:335–7. [PubMed] [Google Scholar]
- 5.Absalom AR, Mani V, De Smet T, Struys MM. Pharmacokinetic models for propofol - Defining and illuminating the devil in the detail. Br J Anaesth. 2009;103:26–37. doi: 10.1093/bja/aep143. [DOI] [PubMed] [Google Scholar]
- 6.Naidoo D. Target Controlled Infusion. 2011. [Last cited on 2013 Sep 28]. Available from: http://www.anaesthetics.ukzn.ac.za/Libraries/Documents2011/D_Naidoo_Target_Controlled_Infusion.sflb.ashx .
- 7.Kim MK, Lee JW, Jang DJ, Shin OY, Nam SB. Effect-site concentration of remifentanil for laryngeal mask airway insertion during target-controlled infusion of propofol. Anaesthesia. 2009;64:136–40. doi: 10.1111/j.1365-2044.2008.05707.x. [DOI] [PubMed] [Google Scholar]
- 8.Kodaka M, Okamoto Y, Handa F, Kawasaki J, Miyao H. Relation between fentanyl dose and predicted EC 50 of propofol for laryngeal mask insertion. Br J Anaesth. 2004;92:238–41. doi: 10.1093/bja/aeh033. [DOI] [PubMed] [Google Scholar]
- 9.Taylor IN, Kenny GN. Requirements for target-controlled infusion of propofol to insert the laryngeal mask airway. Anaesthesia. 1998;53:222–6. doi: 10.1046/j.1365-2044.1998.00316.x. [DOI] [PubMed] [Google Scholar]
- 10.Dixon WJ. Staircase bioassay: The up-and-down method. Neurosci Biobehav Rev. 1991;15:47–50. doi: 10.1016/s0149-7634(05)80090-9. [DOI] [PubMed] [Google Scholar]
- 11.Richebé P, Rivalan B, Baudouin L, Sesay M, Sztark F, Cros AM, et al. Comparison of the anaesthetic requirement with target-controlled infusion of propofol to insert the laryngeal tube vs. the laryngeal mask. Eur J Anaesthesiol. 2005;22:858–63. doi: 10.1017/S0265021505001456. [DOI] [PubMed] [Google Scholar]
- 12.Sivalingam P, Kandasamy R, Madhavan G, Dhakshinamoorthi P. Conditions for laryngeal mask insertion. A comparison of propofol versus sevoflurane with or without alfentanil. Anaesthesia. 1999;54:271–6. doi: 10.1046/j.1365-2044.1999.00663.x. [DOI] [PubMed] [Google Scholar]
- 13.Kazama T, Ikeda K, Morita K. Reduction by fentanyl of the Cp50 values of propofol and hemodynamic responses to various noxious stimuli. Anesthesiology. 1997;87:213–27. doi: 10.1097/00000542-199708000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Stoelting RK, Hillier SC, editors. Handbook of Pharmacology and Physiology in Anesthetic Practice. 2nd ed. USA: Lippincott Williams and Wilkins; 2006. pp. 82–117. [Google Scholar]
- 15.Yumura J, Koukita Y, Fukuda K, Kaneko Y, Ichinohe T. Low dose of fentanyl reduces predicted effect-site concentration of propofol for flexible laryngeal mask airway insertion. J Anesth. 2009;23:203–8. doi: 10.1007/s00540-008-0728-x. [DOI] [PubMed] [Google Scholar]


