Abstract
An 85-year-old male patient with common bile duct stones and gallbladder stone was admitted to the hospital. Endoscopic ultrasound (EUS)-guided cholecystogastrostomy and the placement of a novel covered mental stent was performed after the endoscopic sphincter ectomy procedure. Two weeks later the stents were removed, and an endoscope was advanced into the gallbladder via the fistula, and cholecystolithotomy was performed. For weeks later gallbladder was assessed by abdominal ultrasound. EUS-guided cholecystogastrostomy with mental stent deployment was successfully performed. Two weeks after the procedure, the fistulas had formed, and the stent were removed. Endoscopic cholecystolithotomy was successfully performed through the fistula. The ultrasound exam of gallbladder 4 weeks later showed no stone remain and satisfactory function. The EUS-guided placement of a novel metal stent was a safe and simple approach to performing an endoscopic cholecystogastrostomy, which can subsequently allow procedures for treating biliary disease, including cholecystolithotomy.
Keywords: Cholecystogastrostomy, endoscopic ultrasound, gallbladder stones, metal stent
INTRODUCTION
Laparoscopic cholecystectomy has become the “gold standard” for the treatment of symptomatic gallstones.[1] However, innovative methods for treating gallstones are being introduced, such as scarless therapeutic procedures through a natural orifice, which include transgastric and transcolonic endoscopic cholecystectomies.[2,3,4,5] However, before clinical implementation of these procedures, modifications of the relevant instruments are still needed, and furthermore, a more convenient procedure is still desired.[6]
A recently developed metal stent, the lumen-apposing, fully coated stent, has been proven to be highly efficient for drainage of pancreatic fluid collections, especially for walled-off pancreatic necrosis.[7,8,9,10] Its efficiency in forming an anastomosis between 2 separate hollow organs has started to be verified clinically by such procedures as cholecystogastrostomy and gastroenterostomy. Here, we report a patient with symptomatic gallstones who underwent endoscopic transgastric cholecystolithotomy via a fistula formed around a lumen-apposing metal stent that had been deployed during a previous cholecystogastrostomy procedure.
CASE REPORT
An 85-year-old man presented to our hospital with acute abdominal pain. An initial endoscopic ultrasound (EUS) and magnetic resonance imaging scan revealed bile duct and gallbladder stones [Figure 1]. Conventional endoscopic sphincter ectomy (EST) was performed to remove the stones in the common bile duct. Because the patient was in poor condition and could not be a candidate for surgery like cholecystectomy, EUS-guided cholecystolithotomy was planned after successful EST.
Figure 1.
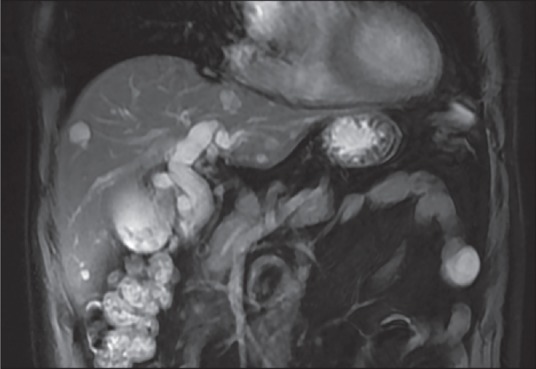
Magnetic resonance imaging showed bile duct and gallbladder stones
Cholecystogastrostomy
The patient provided informed consent for this procedure. A longitudinal echoendoscope (EG-3830-UT, Pentax Corporation, Japan) with a working channel of 3.8 mm was introduced into the stomach to scan for the gall bladder and mark the puncture point [Figure 2]. The contact zone (i.e., the region of the gastric wall representing the shortest distance between the gastric and gallbladder walls) was identified on the anterior wall of the antrum. Color Doppler was then used to identify interposing vessels in order to avoid them during puncture. An EchoTip Ultra EUS needle (19-G; Cook Medical Inc., USA) was introduced via the working channel of the echoendoscope, and the gallbladder was punctured under EUS guidance. A sample was aspirated to confirm that the punctured structure was gallbladder. Several loops of a guide wire (Tracer Metro Direct Wire Guide, 0.035 in/480 mm; Cook Medical Inc., USA) were inserted into the gallbladder, and the needle was removed. The path of the needle was dilated using a Cystotome (10-Fr, Outer Catheter, Cook Medical Inc., USA).
Figure 2.

Cholecystogastrostomy (a) A 19-gauge needle puncture of the gallbladder; (b) The needle path was dilated with Cystotome; (c) Fluoroscopic image of the deployed stent; (d) Endoscopic view of the deployed stent
Under EUS guidance, the stent (10 mm/35 mm; Micro-Tech/Nan Jing Co., Ltd. China) was slowly deployed into the gallbladder until the flared distal end was completely open. Gentle traction was applied to pull the gallbladder wall close to the gastric wall. Then, under endoscopic surveillance, the remainder of the stent was deployed, keeping the proximal end in sight. EUS was used to confirm the position of the stent and rule out leakage. Postoperatively, the patient only complained of mild abdominal discomfort; no sign of peritonitis was observed, and he resumed a normal diet 24 h later. A computed tomography scan was performed to check the stent position [Figure 3].
Figure 3.

Computed tomography scan revealed a stent kept in position
Transgastric cholecystolithotomy
The patient underwent transgastric cholecystolithotomy 2 weeks after cholecystogastrostomy [Figure 4]. A standard gastrointestinal (GI) endoscope was used to determine that the stent remained in place. A 14-mm balloon was inserted through the stent and the track was dilated. The stent was removed using a foreign-body forceps. The endoscope was advanced into the gallbladder via the fistula formed by the stent. Stones were seen in the fundus and neck of the gallbladder. A stone basket was inserted into the gallbladder to retrieve the stones. First, the basket was opened, and then suction was applied to aspirate gas in the GI tract and gallbladder, and until the wall of the gallbladder was gathered around the basket and the stones could fall into the basket. The basket was withdrawn from the gallbladder, and the stones were discharged into the GI tract. After several deployments of the basket to remove stones, an endoscope was introduced into the gallbladder to check for remaining stones. The inside of the gallbladder was clearly visualized, and small residual stones were easily removed using a biopsy forceps. An endoscopic nasobiliary drainage (ENBD) tube was placed in the gallbladder after the stones were removed, and 24 h later, radiography performed via the ENBD tube showed that the gallbladder was free of residual stones. The patient was discharged after the ENBD was removed.
Figure 4.
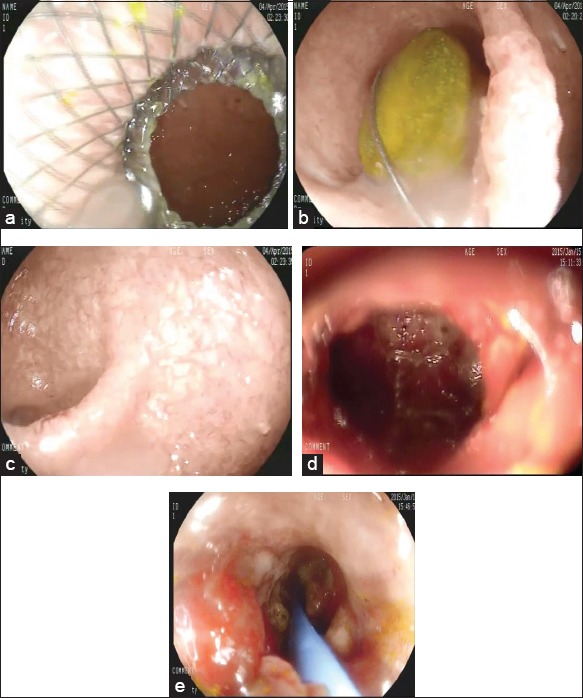
Gastric transmural cholecystolithotomy (a) Endoscopic view of the deployed stent; (b) Endoscopic gallbladder stone removing; (c) Gallbladder was emptied of stones; (d) A fistula was formed after stent removal; (e) An endoscopic nasobiliary drainage was kept in the gallbladder
Follow-up
Four weeks after transgastric cholecystolithotomy, the contractile response of the patient's gallbladder was assessed by abdominal ultrosonography. The size of the fasting gallbladder on ultrasound was 5.4 cm × 2.6 cm × 2.6 cm, and there were no residual stones or food. An ultraosonographic evaluation performed 60 min after the patient ate 2 fried eggs showed the size of the gallbladder to be 2.5 cm × 1.2 cm × 1.1 cm. The gallbladder ejection fraction was estimated to be 91%, which indicated satisfactory function.
DISCUSSION
Choledocholithiasis is a common problem that has been treated by surgery for nearly 300 years. A major evolutionary step in the treatment of choledocholithiasis was the transition from laparotomy to laparoscopy, which remains the standard treatment for gallstones. Long-term follow-up studies have found that cholecystectomy is associated with increased incidence of dyspepsia, calculus of the common bile duct, and colon carcinoma. There are also serious complications associated with the procedure, including hemorrhage, bile duct injury, bile leakage, and abdominal infection.
Transgastric gallbladder entry through a cholecystogastric fistula formed as a complication from gallbladder surgery was first described in a case report by Chen et al.;[11] however, the cholecystoenterostomy may also be a complication of gallstone disease rather than a result of medical intervention. In a previous animal study, we evaluated EUS-assisted transmural cholecystolithotomy performed 4 weeks after a cholecystogastrostomy procedure that placed a novel, fully covered metal stent.[12] Transmural cholecystogastrostomy using a lumen-apposing metal stent may not only be used to facilitate gallbladder drainage,[13,14,15,16] but it may also be a technically easy method for treating cholelithiasis. The high efficiency of anastomosis formation that we found in our study was a result of the lumen-apposing metal stent, which has 2 large, flared ends that firmly hold the gastric wall against the gallbladder wall. The flared ends had blunt edges to prevent further injury to the mucosa. The covered stents were also found to prevent bile leakage.
In our patient, transgastric cholelithiasis was performed 2 week after the initial cholecystogastrostomy procedure. A mature fistula had already formed by that time, which was safely dilated using a 14-mm balloon, and which remained intact during repeated entries of the endoscope until deposits and stones were completely removed from the gallbladder. During removal of the stones, we also found that the fistula allowed clear and complete visualization of the interior gallbladder. Similar transgastric cholelithiasis was also reported by Itoi et al.,[17] in which during the stone removing process the metal stent was still kept in place. In our study, we performed the transgastric cholelithiasis via the mature fistula without stent, which may be more convenient for the dilation process. Therefore, the cholecystogastrostomy procedure using the lumen-apposing stent might facilitate further research and development of novel examination and treatment methods for gallbladder disease. Gallbladder mucosal biopsies and polyp resections may be the next applications of this procedure.
Limitations
Reflux of gastric contents into the gallbladder through the stent may increase the risk of infection and stone formation. Therefore, the lumen-apposing metal stent should be further modified so that it has an antireflux function. In addition, the formation of the fistula needs further detailed study.
CONCLUSION
The EUS-guided placement of a novel metal stent was a safe and simple approach to performing an endoscopic cholecystogastrostomy, which can subsequently allow procedures for treating biliary disease, including cholecystolithotomy. Although we cannot conclude from this case that EUS-guided cholecystolithotomy will replace laparoscopic cholecystectomy to become the procedure of choice for gallstones, it has obvious advantages, especially for elderly and asthenic patients who cannot tolerate surgery. It is a minimally invasive, scarless procedure that preserves the gallbladder and its digestive functions.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (Grant No. 81470908).
Footnotes
Source of Support: This study was supported by the National Natural Science Foundation of China (Grant No. 81470908).
Conflict of Interest: None declared.
REFERENCES
- 1.Fisichella PM, DeMeester SR, Hungness E, et al. Emerging techniques in minimally invasive surgery. Pros and Cons. J Gastrointest Surg. 2015 doi: 10.1007/s11605-015-2766-7. [Epub ahead of print: DOI 10.1007/s11605-015-2766-7] [DOI] [PubMed] [Google Scholar]
- 2.Strain M, Chisevescu D, Blaj S, et al. Thefirst NOTE (Natural Orifice Translumenal Endoscopic) cholecystectomy in Romania: An experimental model in pig. Chirurgia (Bucur) 2009;104:173–9. [PubMed] [Google Scholar]
- 3.Cuadrado-Garcia A, Noguera JF, Olea-Martinez JM, et al. Hybrid natural orifice transluminal endoscopic cholecystectomy: Prospective human series. Surg Endosc. 2011;25:19–22. doi: 10.1007/s00464-010-1121-z. [DOI] [PubMed] [Google Scholar]
- 4.Cho YB, Park CM, Chun HK, et al. Transvaginal endoscopic cholecystectomy using a simple magnetic traction system. Minim Invasive Ther Allied Technol. 2011;20:174–8. doi: 10.3109/13645706.2010.526911. [DOI] [PubMed] [Google Scholar]
- 5.Ogredici O, Linke GR, Lamm S, et al. Routine cholangiography during rigid-hybrid transvaginal natural orifice transluminal endoscopic cholecystectomy. Surg Endosc. 2014;28:910–7. doi: 10.1007/s00464-013-3246-3. [DOI] [PubMed] [Google Scholar]
- 6.Hall RC. Is natural orifice transluminal endoscopic cholecystectomy as safe as laparoscopic cholecystectomy? Arch Surg. 2008;143:604. doi: 10.1001/archsurg.143.6.604-a. [DOI] [PubMed] [Google Scholar]
- 7.Parra V, Kedia P, Zerbo S, et al. Drainage of infected pancreatic necrosis by using 2 lumen-apposing metal stents, a nasocystic drain, and hydrogen peroxide. Gastrointest Endosc. 2015;81:1261. doi: 10.1016/j.gie.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Wrobel PS, Kaplan J, Siddiqui AA. A new lumen-apposing metal stent for endoscopic transluminal drainage of peripancreatic fluid collections. Endosc Ultrasound. 2014;3:203–4. doi: 10.4103/2303-9027.144508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah RJ, Shah JN, Waxman I, et al. Safety and efficacy of endoscopic ultrasound-guided drainage of pancreatic fluid collections with lumen-apposing covered self-expanding metal stents. Clin Gastroenterol Hepatol. 2015;13:747–52. doi: 10.1016/j.cgh.2014.09.047. [DOI] [PubMed] [Google Scholar]
- 10.Walter D, Will U, Sanchez-Yague A, et al. A novel lumen-apposing metal stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections: A prospective cohort study. Endoscopy. 2015;47:63–7. doi: 10.1055/s-0034-1378113. [DOI] [PubMed] [Google Scholar]
- 11.Chen YY, Su PY, Shen WC. Gallbladder polyp treated with endoscopic polypectomy through a cholecystogastrostomy. Endoscopy. 2011;43(Suppl 2 UCTN):E88–9. doi: 10.1055/s-0030-1255983. [DOI] [PubMed] [Google Scholar]
- 12.Ge N, Wang Z, Sun S, et al. EUS assisted transmural cholecystogastrostomy fistula creation as a bridge for endoscopic internal gallbladder therapy using a novel fully covered metal stent. BMC Gastroenterol. 2014;14:164. doi: 10.1186/1471-230X-14-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de la Serna-Higuera C, Pérez-Miranda M, Gil-Simón P, et al. EUS-guided transenteric gallbladder drainage with a new fistula-forming, lumen-apposing metal stent. Gastrointest Endosc. 2013;77:303–8. doi: 10.1016/j.gie.2012.09.021. [DOI] [PubMed] [Google Scholar]
- 14.Itoi T, Binmoeller K, Itokawa F, et al. Endoscopic ultrasonography-guided cholecystogastrostomy using a lumen-apposing metal stent as an alternative to extrahepatic bile duct drainage in pancreatic cancer with duodenal invasion. Dig Endosc. 2013;25(Suppl 2):137–41. doi: 10.1111/den.12084. [DOI] [PubMed] [Google Scholar]
- 15.Widmer J, Alvarez P, Gaidhane M, et al. Endoscopic ultrasonography-guided cholecystogastrostomy in patients with unresectable pancreatic cancer using anti-migratory metal stents: A new approach. Dig Endosc. 2014;26:599–602. doi: 10.1111/den.12163. [DOI] [PubMed] [Google Scholar]
- 16.Saftoiu A, Vilmann P, Bhutani MS. Feasibility study of EUS-NOTES as a novel approach for peroral cholecysto-gastrostomy. Chirurgia (Bucur) 2013;108:62–9. [PubMed] [Google Scholar]
- 17.Itoi T, Itokawa F, Tsuchiya T, et al. Transgastric large gallstone extraction through a lumen-apposing metal stent in a patient with acute cholecystitis. Gastrointest Endosc. 2014;79:547. doi: 10.1016/j.gie.2013.12.010. [DOI] [PubMed] [Google Scholar]


