Abstract
Endoscopic ultrasonography (EUS) is a useful modality for imaging of the blood vessels of the mediastinum and abdomen. The aorta acts as an important home base during EUS imaging. The aorta and its branches are accessible by standard angiographic methods, but endosonography also provides a unique opportunity to evaluate the aorta and its branches. This article describes the techniques of imaging of different part of the aorta by EUS.
Keywords: Aorta, blood vessel, branch, endoscopic ultrasound, imaging
INTRODUCTION
Endoscopic ultrasonography (EUS) is a useful modality for imaging of the blood vessels of the mediastinum and abdomen. The important vessels in EUS imaging include the aorta and its branches (the great vessels of neck, mesenteric arteries), superior and inferior vena cava, azygos vein (AV) and vessels related to portal venous system.[1,2,3,4,5,6] Computed tomography scan or magnetic resonance imaging are the usual methods for detection of abnormalities in aortic disease.[7,8,9,10,11,12,13] Aorta acts as an important home base during EUS imaging. EUS imaging also provides a unique opportunity to evaluate the aorta and its branches as well as certain congenital aortic anomalies.[14,15] Conventional abdominal sonography can evaluate the abdominal aorta or its branches, but it is usually difficult to evaluate the thoracic part of the aorta.[16] The evaluation of the aorta and its branches may be helpful in the assessment of diseases primarily involving the aorta or its branches, for assessment of invasion of the thoracic aorta in mediastinum and evaluation and staging of pancreaticobiliary malignancies. The aorta and its branches are accessible by standard angiographic methods, but endosonography guided access can provide an alternative method for diagnostic and therapeutic interventions. This article describes the techniques of imaging of different part of the aorta by EUS.
EXTENT OF IMAGING
The imaging of most of the aorta can be done from its origin from the heart to the point of bifurcation at the L-4 vertebra from the following positions [Table 1, Figure 1].
Table 1.
Different parts of aorta and the position of imaging
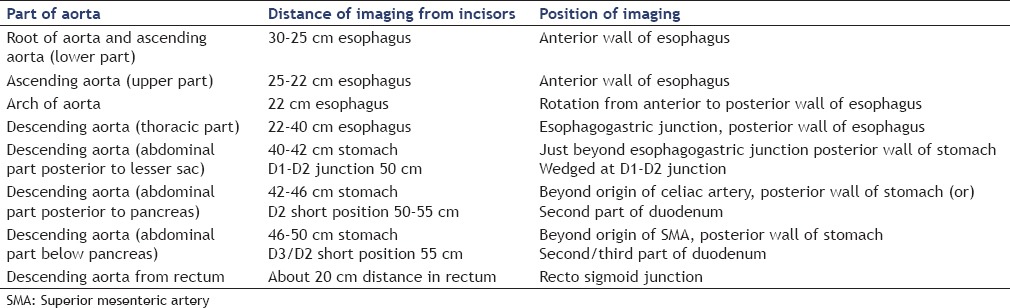
Figure 1.
Imaging of aorta can be done from various positions in mediastinum, stomach, and duodenum. The bifurcation of aorta can be also visualized by rectal ultrasound
IMAGING OF AORTIC ROOT AND LOWER PART OF ASCENDING AORTA
Anatomical landmark
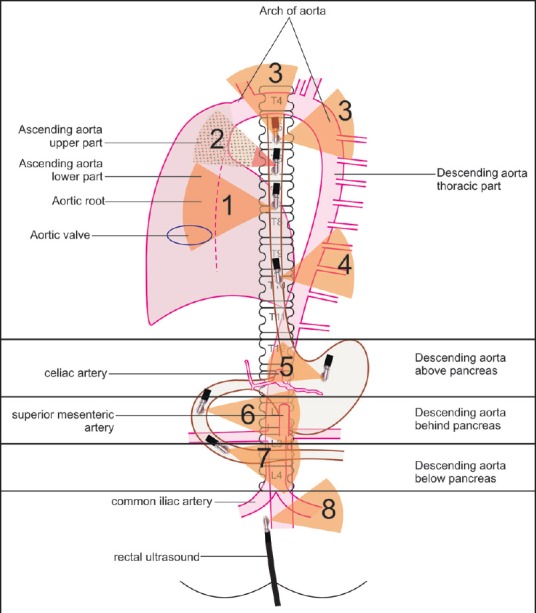
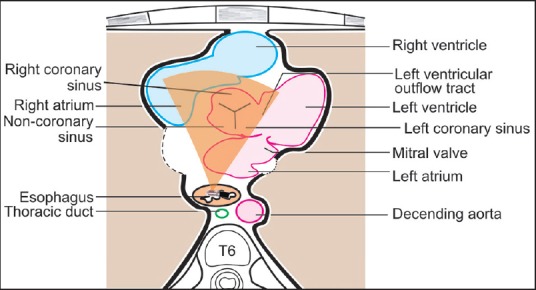
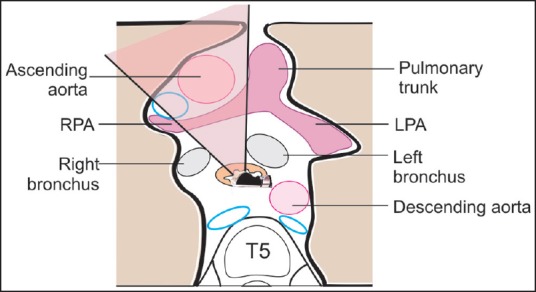
The aortic root has a diameter of 2.4-4.7 cm (its diameter is more in males than females) and lies at the base of the left ventricle posterior to the right ventricular outflow tract. The aortic annulus, which lies at the base of the aortic root, provides attachment to three semilunar cusps (one anterior and two posterior)[7,9,10,12] [Figure 2a]. Distal to the attachment of the cusps the aorta is wide and presents three dilatations which are called the aortic sinuses of Valsalva, (right coronary — anterior, left coronary — left posterior and noncoronary — right posterior) [Figure 2b]. From the aortic root, the ascending aorta passes upwards, forwards and to the right to continue as the arch at the level of upper border of the right second costal cartilage (sternal angle, lower border of the T4 vertebra). It ascends anterior to the left atrium, right pulmonary artery and right principal bronchus, and posterior to the right ventricular outflow tract and beginning of the pulmonary trunk [Figure 3, Video 1].
Figure 2a.
The aortic valve is seen during imaging from esophagus through the left atrium. The right coronary sinus is the one which is away from the left atrium towards the base of pulmonary trunk and the left coronary sinus faces the left ventricle
Figure 2b.
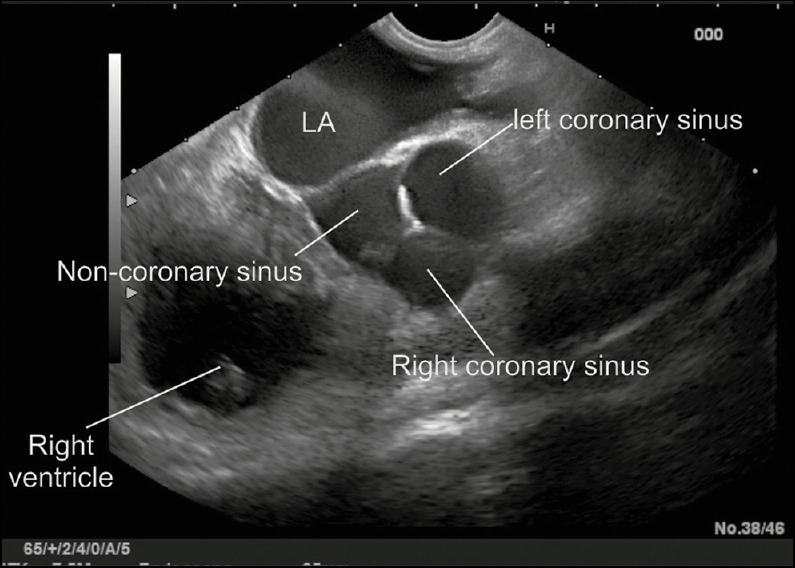
The origin of aorta from the left ventricle can be seen at about 30 cm distance in esophagus. Slight clock-wise and anti-clockwise rotation reveals the three sinuses just above the aortic valve
Figure 3.
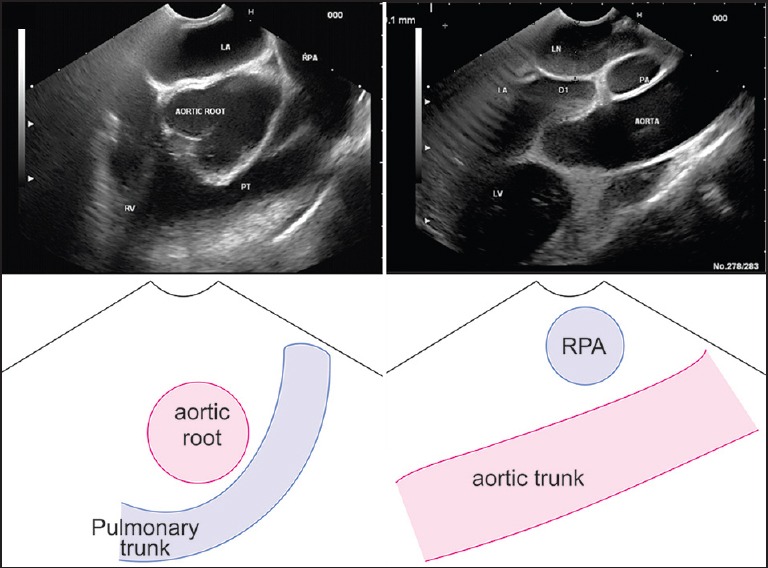
Ascending aorta is 5 cm long and 3 cm wide and lies in the middle mediastinum within the fibrous pericardium along with the pulmonary trunk. The relation of the ascending aorta and the right pulmonary artery on endoscopic ultrasonography in this position follow a simple observation “if you see one in long axis you will see the other in short axis”. If the aorta is seen in a long axis, the pulmonary artery is seen in a rounded axis and vice versa. In this figure a lymph node of subcarinal area is also seen
Technique of imaging
Identify the left atrium and right pulmonary artery.
The left atrium is identified as the largest pulsatile chamber at about 30 cm in the anterior wall of the esophagus.
The right pulmonary artery is seen above the left atrium.
Identify the root of the aorta.
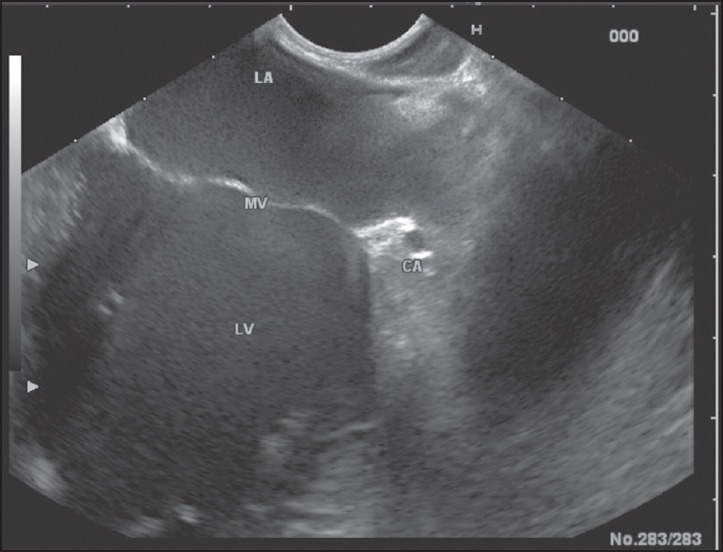
The root of aorta is identified anteriorly to the upper part of the left atrium or right pulmonary artery [Figure 4].
Rotation of the scope is able to identify the individual leaflets of the aortic valve. The origin of both coronary arteries can be visualized in this position.
Trace the ascending aorta from the aortic valve.
The ascending aorta is identified as a long tubular structure going up for a distance of about 5 cm from the aortic valve [Videos 2 and 3].
Figure 4.
The subcarinal window provides an opportunity and a window of imaging between the right and left bronchus. The imaging of base of aorta is possible through the left atrium and pulmonary artery
Imaging of the branches
The right coronary artery arises from the right (anterior) sinus of Valsalva and the left coronary artery arises from the left (left posterior) sinus of Valsalva [Figures 5 and 6, Video 4]. The left coronary artery is followed-up easily for a distance of about 1-2 cm from its origin on EUS [Figure 7].
Figure 5.
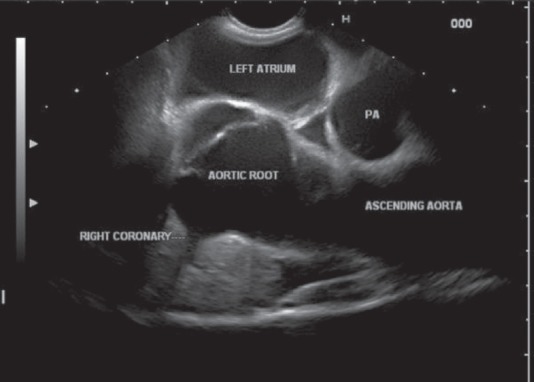
The origin of right coronary artery is seen from the anterior sinus
Figure 6.
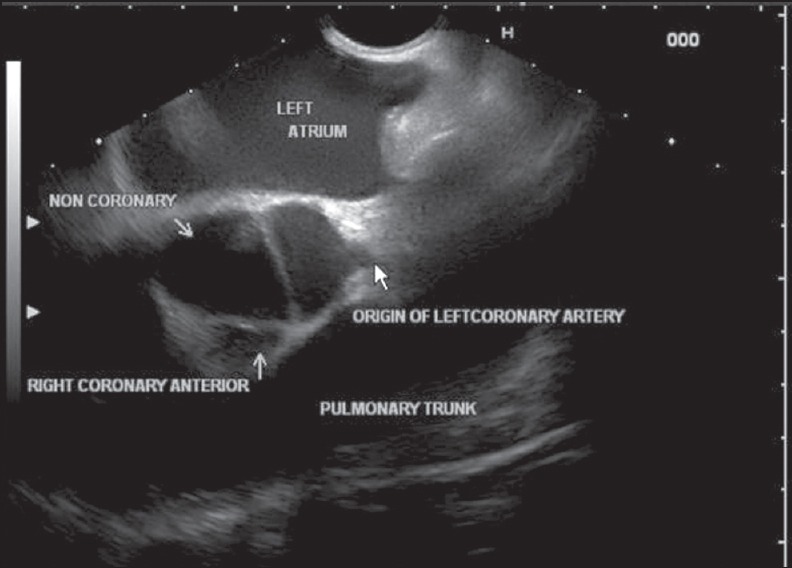
The origin of left coronary artery is seen from the left sinus
Figure 7.
It is usually possible to follow the course of the left coronary artery for some distance
ASCENDING AORTA, UPPER PART
This part lies at about 25-22 cm distance in the anterior wall of the esophagus. The imaging of the uppermost part of the ascending aorta, the origin of the brachiocephalic trunk (BCT) and some part of the arch of the aorta is not possible (blind area of imaging) as the trachea and part of the left bronchus comes to lie between the esophagus and ascending part of the aorta. This part of the aorta has no branches [Figure 8].
Figure 8.
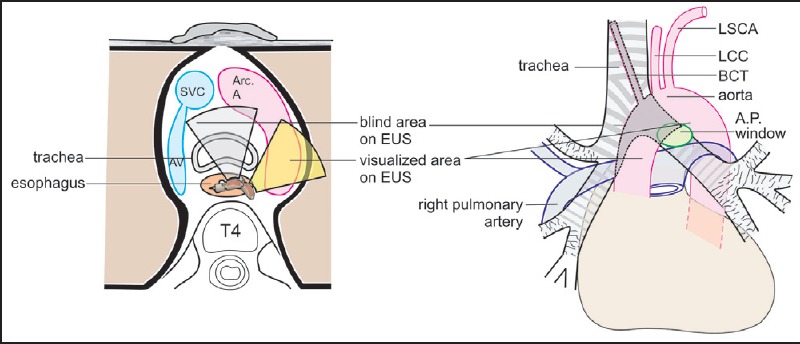
The shaded area shows the blind areas of imaging during endoscopic ultrasound. The upper part of ascending aorta, the brachiocephalic trunk and part of the arch of aorta lie in front of trachea and cannot be visualized by endoscopic ultrasonography. SVC = Superior vena cava, AV = Azygos vein, Arc. A = Arch of aorta, T4 = Fourth thoracic vertebra, LSCA = Left subclavian artery, LCC = Left common carotid artery, BCT = Brachiocephalic trunk, AP window = Aortopulmonary window
THE ARCH OF AORTA AT 22 CM DISTANCE IN THE ESOPHAGUS
Anatomical landmark
The aortic arch begins as a continuation of the ascending aorta at the level of the upper border of the right sternocostal joint. Its diameter ranges from 0.9 to 2.5 cm. It ascends slightly to the left across the anterior surface of the trachea, arches over the root of the left lung and then descends on the left side of the trachea and T4 vertebra to continue as the descending thoracic aorta [Figure 8]. The lower border of the arch forms an important boundary of the aortopulmonary (AP) window [Figure 9].
Figure 9.
The boundaries of aortopulmonary window includes the ascending aorta anteriorly, the esophagus and descending aorta posteriorly, the left lateral wall of the trachea and the left main bronchus medially, the left upper-lobe pleura laterally, the aortic arch superiorly, and the left pulmonary artery inferiorly
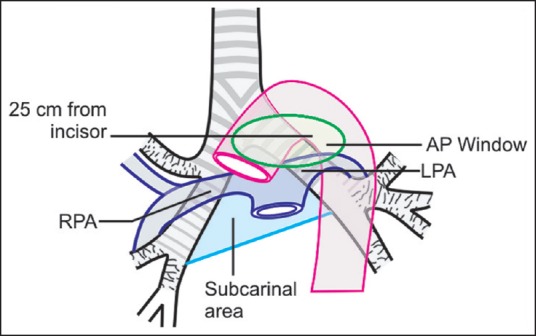
Technique of imaging of arch
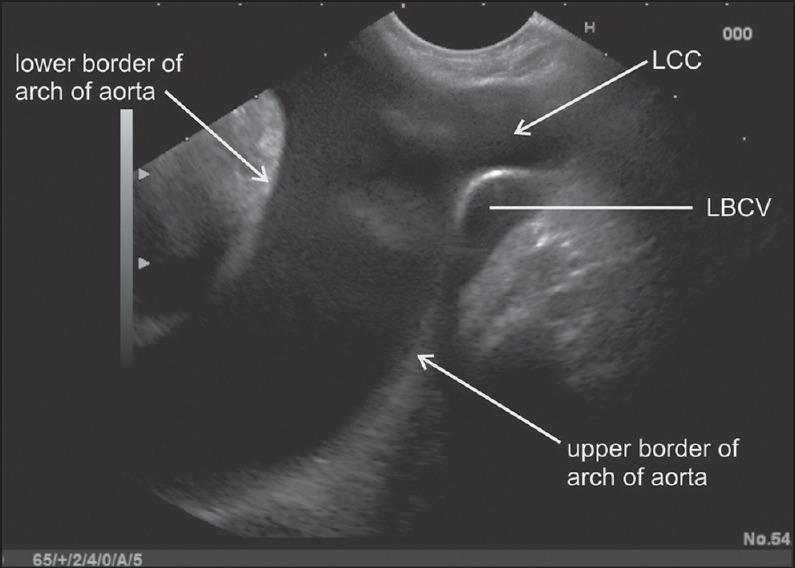
The beginning and ending of the arch are present at the same level of the sternal angle. Initially, the aorta is located in a rounded position at 22 cm distance and the upper and lower borders are identified [Figure 10].
A rotation of EUS scope at this level is able to demonstrate most of the arch and its borders. The outer border presents as a convexity facing anteriorly and to the left and the inner border presents as a concavity facing posteriorly to the right [Figure 11].
From a rounded position, the entire arch can be traced by clockwise and anticlockwise rotation [Figure 11].
Tracing of the upper border of the arch finds the origin of great vessels of the neck and tracing the lower border of the arch identifies the AP window [Figure 9].
Imaging of AP window is possible either by focusing on the arch and descending aorta (DA) or by focusing on the pulmonary arteries.
Figure 10.
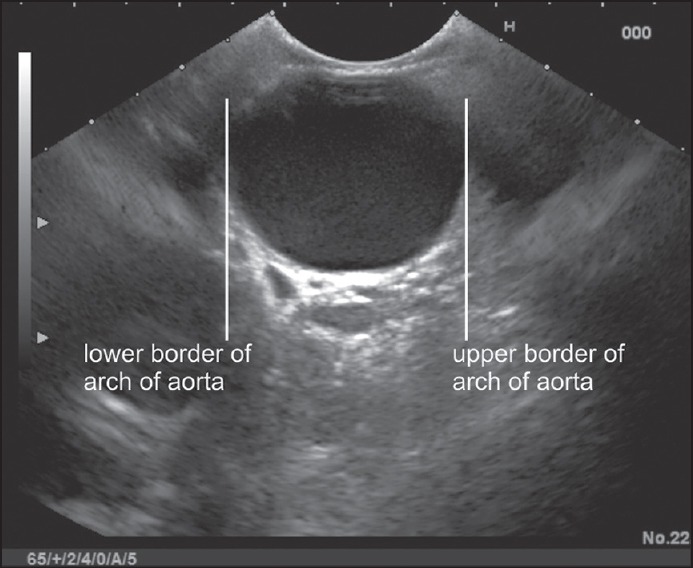
The upper and lower border of the arch of the aorta are located at the 22 cm distance as a rounded vascular structure
Figure 11.
Rotation of the scope follows the borders of the arch
Imaging of the aortopulmonary window with the descending aorta as the base
Follow the DA upward till it becomes the arch of the aorta.
Turn clockwise with a slight push to see the AP window [Figure 12 Video 5].
As an alternative method initially the arch of aorta is visualized.
Slight pushing up with anticlockwise torque is needed to see the AP window [Figure 13].
Figure 12.
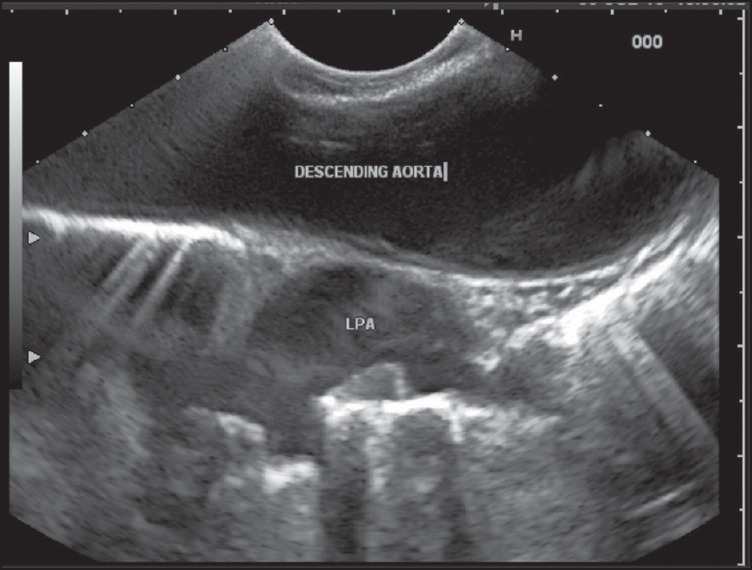
The descending aorta can be traced once the arch of the aorta is located by pushing down the scope on endoscopic ultrasonography. The left pulmonary artery lies very close to the outer border of descending aorta and can be often seen through the descending aorta. A tilting up of the probe in this position will demonstrate the aortopulmonary window
Figure 13.
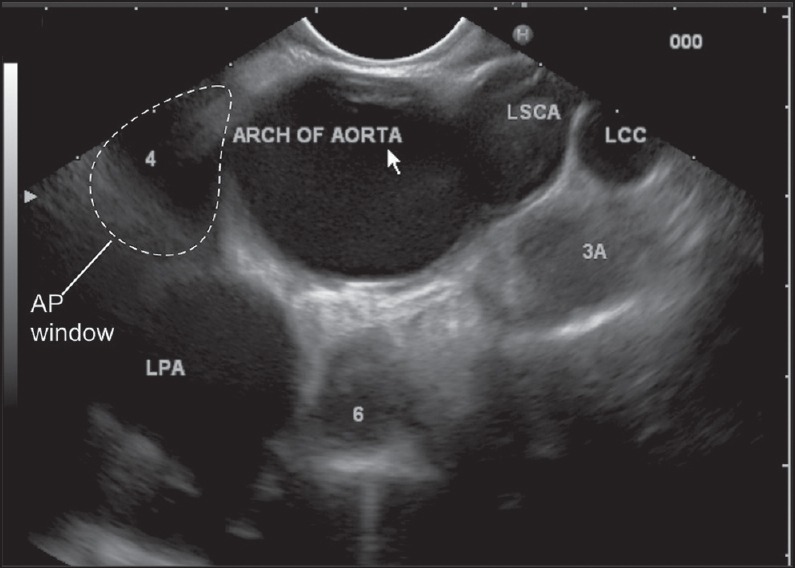
The arch of the aorta is identified as a rounded structure and the left pulmonary artery is seen through the arch of the aorta. Pushing the scope slightly and moving it up will show the aortopulmonary window. In this figure, the lymph nodes present at 3a, 4l and station 6 lymph nodes (IASLC classification) are also seen
Imaging of aortopulmonary window with the pulmonary artery as the base
Identify the left atrium.
Pull back the scope till you start seeing the right pulmonary artery.
Continue slowly pulling back and once the tracheal rings start appearing on the cranial side, torque counter clockwise for about 90° and the AP window will be visualized [Figure 14].
As an alternative method initially the left pulmonary artery is visualized through the lower part of the arch of the aorta.
Clockwise rotation along with up tilt will reveal the AP window.
Figure 14.
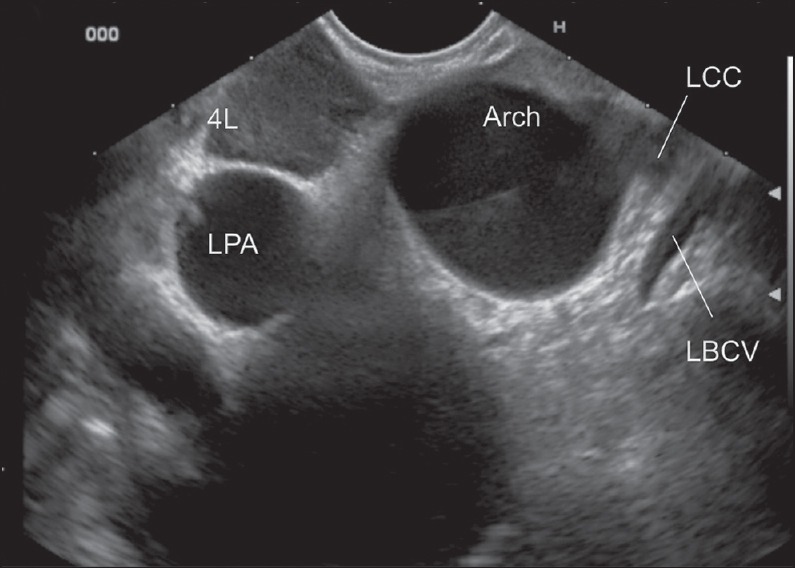
In this image the left common carotid artery is seen taking origin from the arch of the aorta. The lymph node lying below the arch of aorta belongs to station 4L
Imaging of branches
Three branches arise from the convexity of the arch, the BCT, left common carotid artery and left subclavian artery [Figures 15 and 16]. All the three arteries are crossed anteriorly by the left brachiocephalic vein and can be seen while tracing the upper border of the arch of the aorta. The BCT usually lies in the blind area of imaging. [Video 6]. The imaging of the bronchial arteries is possible in the AP window [Figure 17].
Figure 15.
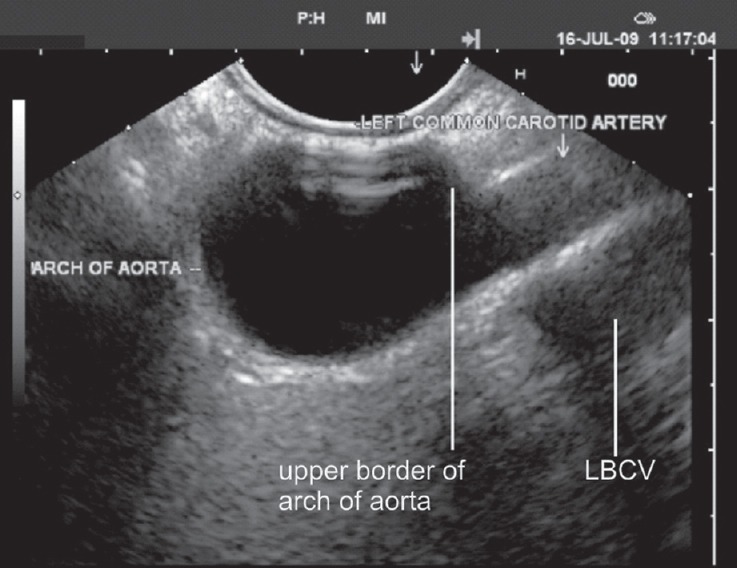
Clockwise rotation from the extreme left position (left lateral wall of the esophagus) shows the left common carotid artery. The left brachiocephalic vein crosses anterior to the left common carotid artery
Figure 16.
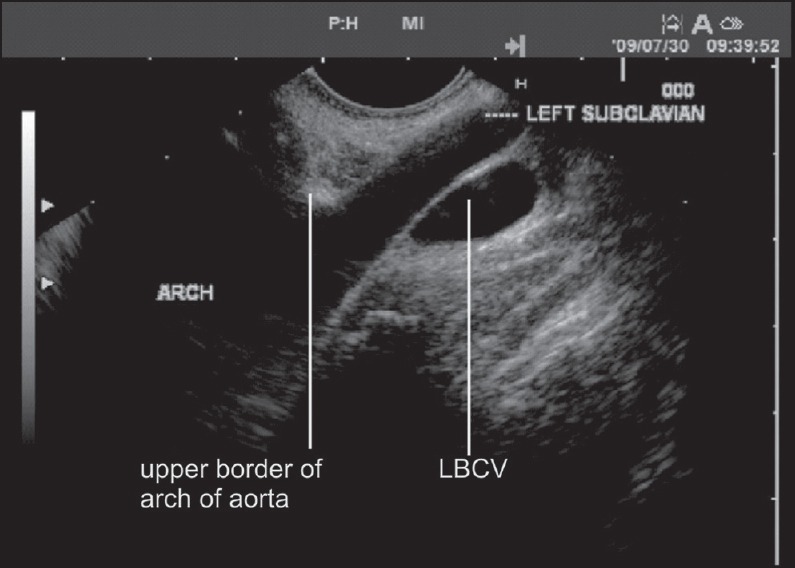
Clockwise rotation from along the left lateral wall of the esophagus shows the left subclavian artery. The left brachiocephalic vein crosses anterior to the artery
Figure 17.
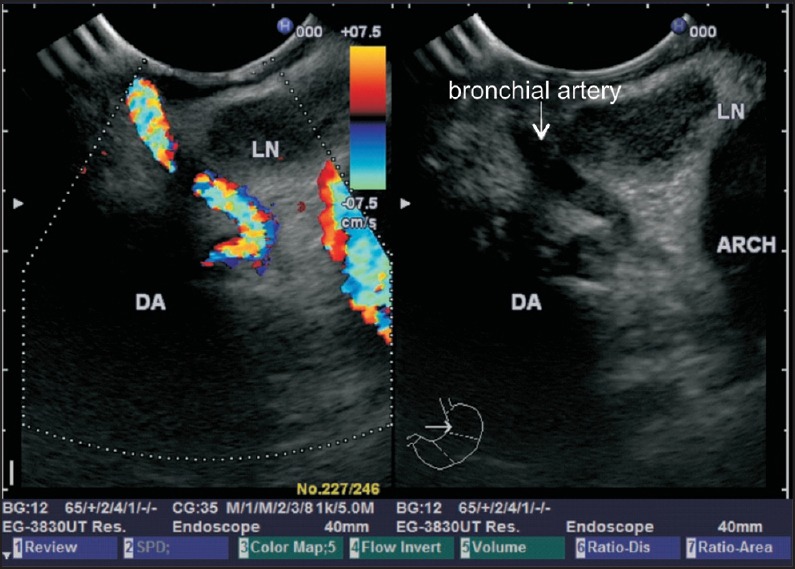
The aortopulmonary window is filled with fat and areolar tissue, lymph nodes and is traversed by the ligamentum arteriosum and left bronchial arteries. DA = Descending aorta
DESCENDING AORTA (THORACIC PART) 22-40 CM DISTANCE IN ESOPHAGUS
Anatomical landmark
The descending thoracic aorta extends from the level of lower border of the T4 vertebra to the aortic hiatus in the diaphragm in the midline at the level of lower border of the T12 vertebra where it continues as the abdominal aorta. It is about 16-18 cm in length and the diameter of its mid portion ranges from 1.6 to 3.7 cm. It lies in the posterior mediastinum, atfirst to the left of the vertebral column and then in front of the vertebral column. It descends successively posterior to the left pulmonary hilum and esophagus with which it is mutually spiralized to a limited extent and finally the diaphragm.
Technique of imaging
It is fairly easy to trace the DA by pushing along the posterior wall of the esophagus from the arch downwards [Figure 18].
Figure 18.
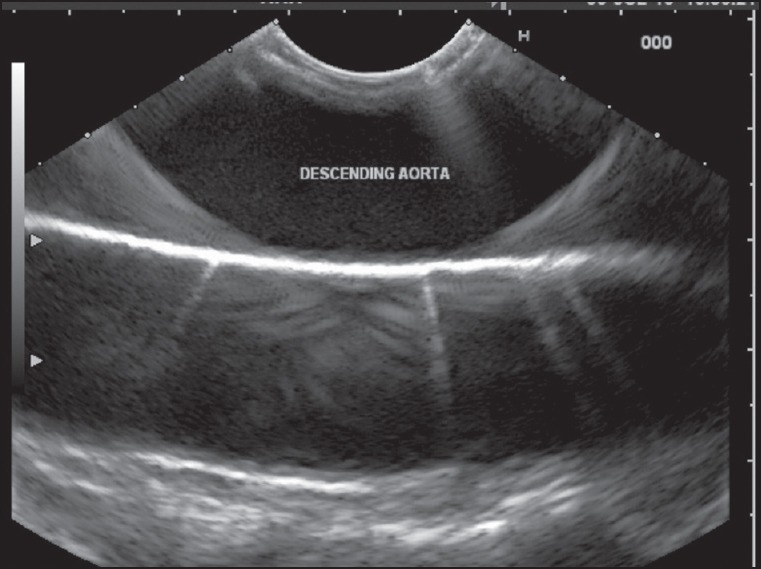
The outer border of descending aorta abuts against the left lung and makes a mirror image artificat because of the reflection of sound waves from the lung
Imaging of the branches
The origin of the intercostal arteries can be seen from the left and right borders of descending thoracic aorta on clockwise or anticlockwise rotation of the scope. The course of right intercostal arteries is more easily traced as they go across the spine after indenting the posterior border of the AV [Figure 19]. The left bronchial arteries can be sometimes traced in the AP window [Figure 17].
Figure 19.
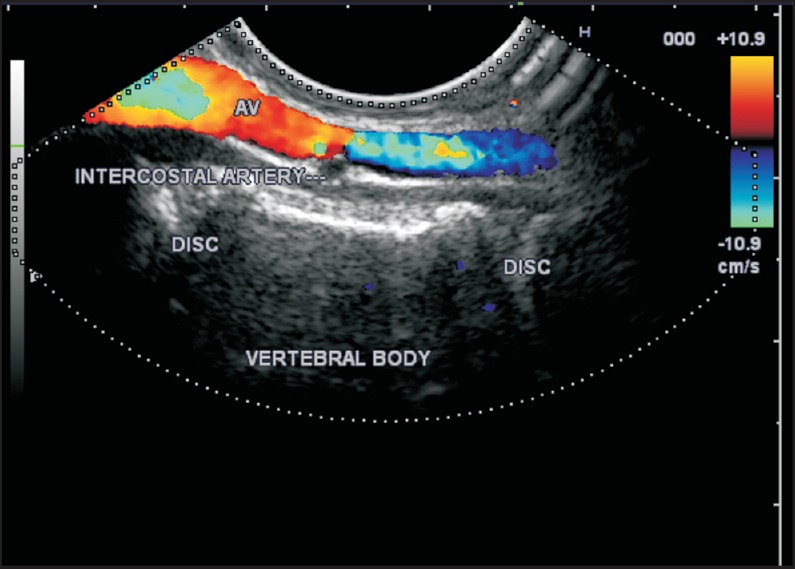
The posterior border of the azygos vein is indented at each vertebral level by the posterior intercostal arteries which can be traced to the descending aorta by a clockwise rotation. Alternatively when an anticlockwise sweep is made from the aorta to the azygos vein the posterior intercostal arteries can be traced going from behind the AV to merge into the lateral part of the descending aorta AV = Azygos vein
DESCENDING AORTA
The DA in the abdominal part can be divided into three parts [Figure 20]. The first part extends from the aortic hiatus to the upper border of the pancreas and lies posterior to the omental bursa and is related anteriorly to the origin of the first major branch of the abdominal aorta, the celiac artery at the T-12/L-1 vertebral level. The second part lies posterior to the pancreas and is related anteriorly to the origin of the superior mesenteric artery (SMA) at the L-1/L-2 vertebral level. The third part (can be referred to as the infra renal part) extends from the lower border of the pancreas to the aortic bifurcation and is related anteriorly to the origin of the inferior mesenteric artery at the L-3 vertebral level.
Figure 20.
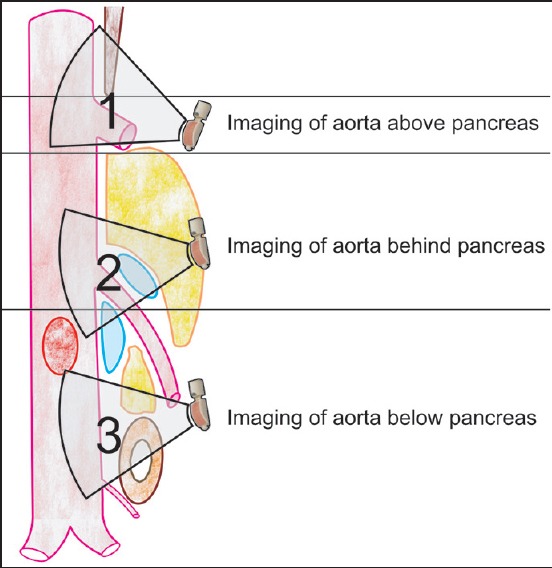
Descending aorta (abdominal part). As the descending aorta enters the abdomen the left crus comes between the aorta and esophagus. The descending aorta in abdominal part can be divided into three parts
DESCENDING AORTA (ABDOMINAL AORTA) (POSTERIOR TO LESSER SAC)
Anatomical landmark
The abdominal aorta begins at the aortic opening of the diaphragm in the midline, at the level of the lower border of the T-12 vertebra and ends at the level of the lower border of the L-4 vertebra, slightly to the left of the midline, by dividing into two common iliac arteries. Its average length is about 10 cm and the diameter (1.7-2.3 cm) decreases from above downwards because of the origin of the large branches.
Technique of imaging
There are three ways of locating the DA in abdomen:
Pushing the scope into the stomach follows down the thoracic aorta into the abdominal part. The thoracic aorta maintains a very close relationship to the esophagus but abdominal aorta goes away from the posterior wall of the stomach as the pancreas comes to lie between the aorta and stomach. The downward movement of the big wheel is usually required to follow the aorta. Following the thoracic aorta down and simultaneously moving the wheel down gives a sensation of climbing over a hill for an endosonographer akin to a car driver (in this case pancreas is the hill) [Figure 20].
The second way of imaging is by probing at the esophagogastric junction (40 cm) with the wheels of the scope in a neutral position and slight tipping up to maintain contact with the posterior wall of the stomach.
The third way of imaging is by finding the liver during probing at 40 cm and 180° rotation to either side will locate the aorta.
Imaging of branches
The imaging of DA from beyond the hiatus shows two vessels:
Celiac artery: The celiac artery is a short artery (length = 1.25 cm), which begins just below the median arcuate ligament where the left and right crura join and goes a little to the right side after taking origin from the aorta [Figures 21 and 22]. A counterclockwise rotation with slight torquing and simultaneously pushing down slightly locate the celiac artery. Torquing is required as the origin of the celiac artery is usually on one side of the aorta and without torquing the origin of the celiac artery may be missed. In general, more torquing than pushing is required and by torquing the trifurcation of artery into three, branches can be also identified [Figures 23 and 24, Video 7].
Left inferior phrenic artery: The left inferior phrenic artery is located just above the origin of the celiac artery. Usually an application of color Doppler over the anterior border of the aorta is required for locating the artery [Figure 25].
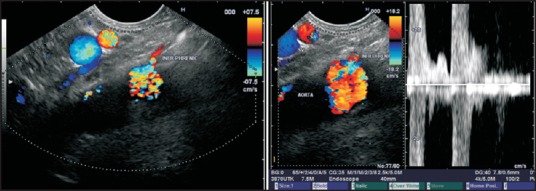
Figure 21.
The celiac artery is the first major artery, which takes origin from the anterior aspect of the descending aorta just below the diaphragmatic hiatus. The superior mesenteric artery (SMA) lies approximately 2 cm below the origin of celiac artery. The origin of celiac and superior mesenteric artery from the aorta may be considered as two barrels of a gun where the aorta is the gun where the upper barrel generally takes off at an angle slightly <90° and the SMA takes off at an angle of 30-45°. The posterior surface of body of pancreas rests between the two barrels formed by the celiac artery and SMA
Figure 22.
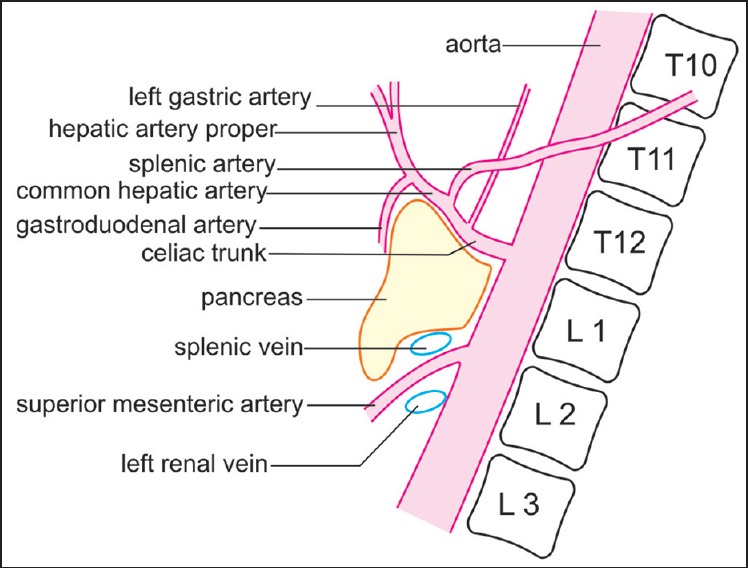
The celiac artery trifurcates into three branches, which are the hepatic artery, celiac artery and left gastric artery. The splenic artery and hepatic artery go in opposite directions and the left gastric artery take off is seen from the upper border. The common hepatic artery divides into the gastroduodenal artery and hepatic artery proper
Figure 23.
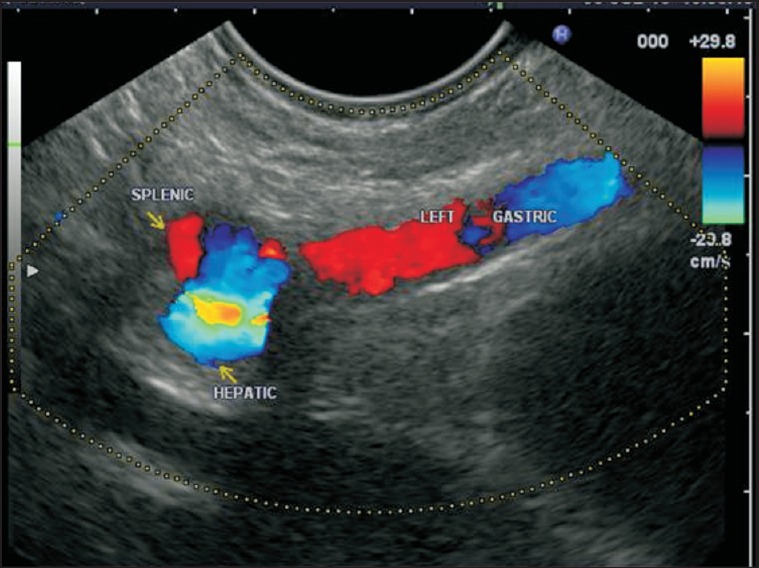
The trifurcation of the celiac artery into three branches is seen
Figure 24.
On linear endoscopic ultrasonography the trifurcation of the celiac artery into its three branches; the hepatic artery, celiac artery and left gastric artery is seen fairly regularly. The splenic artery and hepatic artery go in opposite directions and the left gastric artery take off is seen from the upper border
Figure 25.
The left inferior phrenic artery is a small artery which can be seen taking origin from the anterior surface of the aorta just above the origin of the celiac artery. Usually application of the color Doppler helps in identifying this artery
DESCENDING AORTA (POSTERIOR TO PANCREAS)
Anatomical landmark
The imaging of this part of the aorta can be done from just beyond the esophagogastric junction near the posterior wall of the stomach or from the second/third part of the duodenum. The abdominal aorta beyond the origin of the celiac artery to the origin of the SMA can be traced from the stomach as well as from the second/third part of the duodenum [Figure 26].
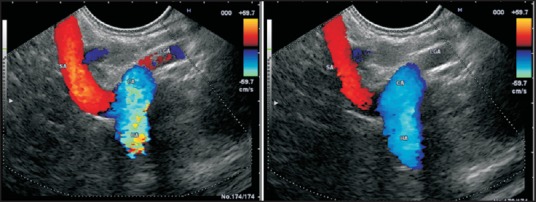
Figure 26.
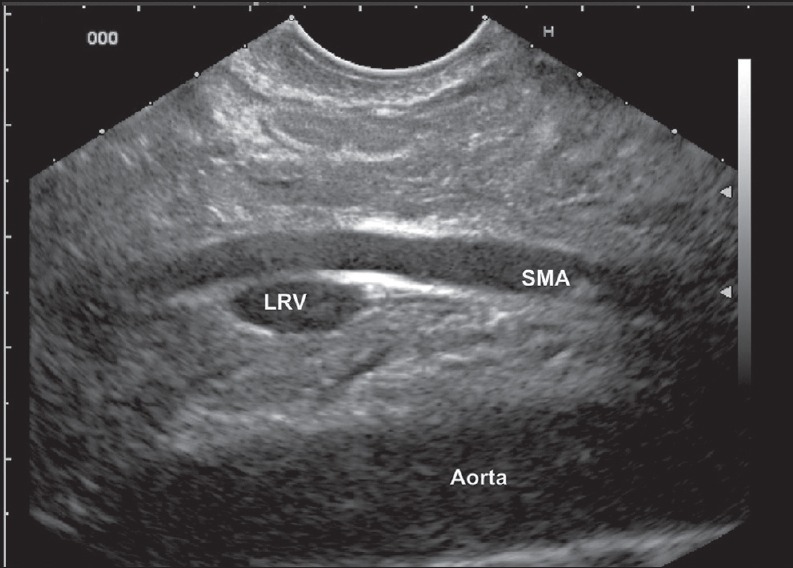
Imaging from the stomach shows the superior mesenteric artery. The left renal vein is seen in the angle between the aorta and superior mesenteric artery
Technique of imaging
Initially, the scope is negotiated into the third part of the duodenum.
Slow pull out is done in a neutral position of the knobs.
Slight clockwise and anticlockwise rotation helps in finding and following the SMA from below upwards up to the point of its origin from the aorta [Video 8].
As an alternative method, pushing the scope down after locating the celiac artery from the stomach is able to locate the origin of the SMA fairly regularly.
Imaging of branches
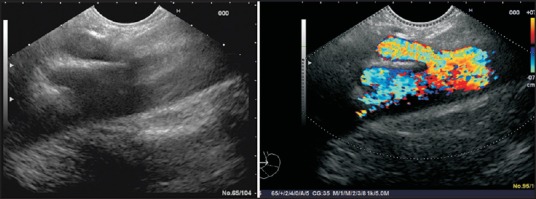
The superior mesenteric artery is identified by the presence of pancreatic tissue between the SMA and aorta in imaging from the stomach or duodenum. Slight clockwise and counterclockwise rotation at this level shows the origin of the right and left renal arteries also [Video 9 and Figure 27].
Figure 27.
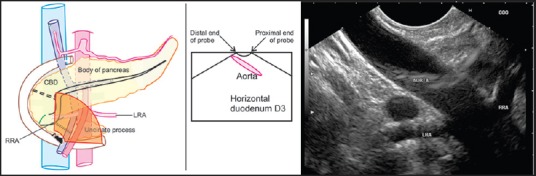
When the probe is placed near the horizontal part of duodenum the distal end of the probe comes close to the lower part of the aorta below the origin of the renal artery. In this position the proximal end of the probe is away from the aorta and the distal end of the probe is close to the aorta
DESCENDING AORTA BELOW PANCREAS
Anatomical landmark
The third part of aorta is crossed anteriorly by the third part of the duodenum and it is generally easier to image both the second and third parts of the abdominal aorta from second and third parts of the duodenum.
Technique of imaging
The scope is positioned in the duodenum and shortened in such a manner that the aorta may lie in one of the three positions.
The aorta may lie parallel, distal end close to the probe or proximal end close to the probe situation [Figures 27–29].
Figure 29.
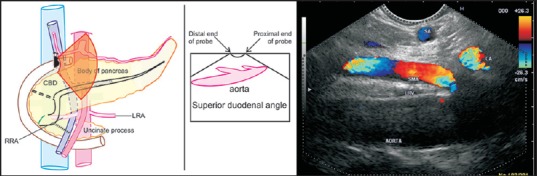
When the probe is placed near superior duodenal angle the distal end of the probe comes close to the lower part of the aorta below the origin of the superior mesenteric artery and the proximal part comes close to the origin of the superior mesenteric artery and sometimes the celiac artery. In this position the proximal end of the probe is close to the aorta and the distal end of the probe is usually away from the aorta
Figure 28.
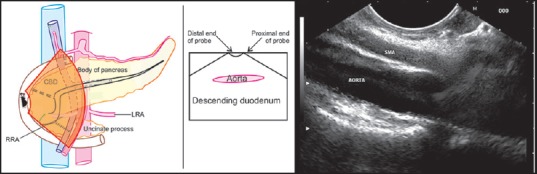
When the probe is placed in the descending duodenum the aorta generally lies parallel to the probe. In this position the proximal end of the probe as well as the distal end of the probe is equally close to aorta. In this position slow withdrawal of the probe will show the origin of the superior mesenteric artery and celiac artery
Imaging of branches
The branches of this segment include the renal arteries, the lumbar arteries, the gonadal artery and the inferior mesenteric artery before the bifurcation of the aorta [Figures 30–32 and Video 10].
Clockwise and anticlockwise rotation from this position is able to demonstrate the branches coming out of the aorta and the bifurcation [Figure 33].
As an alternative method the bifurcation of the aorta can be seen from the stomach also [Figure 32 and Video 11].
It is generally difficult to identify the inferior mesenteric artery in this position.
Sometimes the origin of the gonadal arteries can be identified at this level [Figure 32 and Video 12].
Figure 30.
Imaging from the duodenum shows the origin of the right and left renal artery. The artery coming towards the probe is the right renal artery and the artery going away from the probe is the left renal artery
Figure 32.
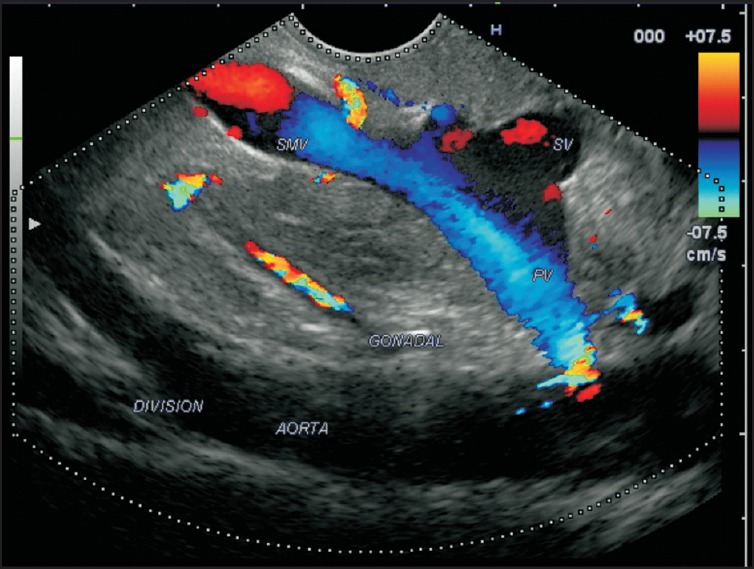
The bifurcation of the aorta is seen during imaging from the stomach. In this case, the gonadal artery is also seen taking origin from the aorta
Figure 33.
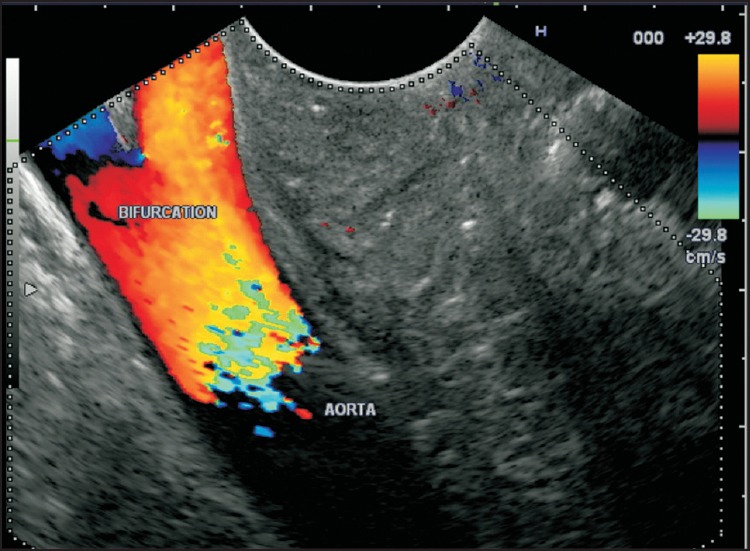
The bifurcation of the aorta is seen during imaging from the duodenum. It is generally difficult to trace the origin of the inferior mesenteric artery during endoscopic ultrasonography imaging
Figure 31.
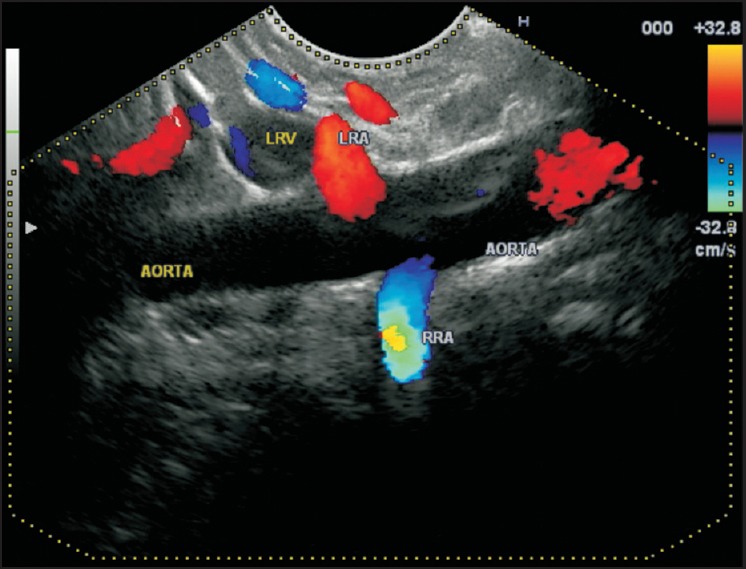
Imaging from the stomach shows the origin of the right and left renal artery. The artery coming towards the probe is the left renal artery and the artery going away from the probe is the right renal artery
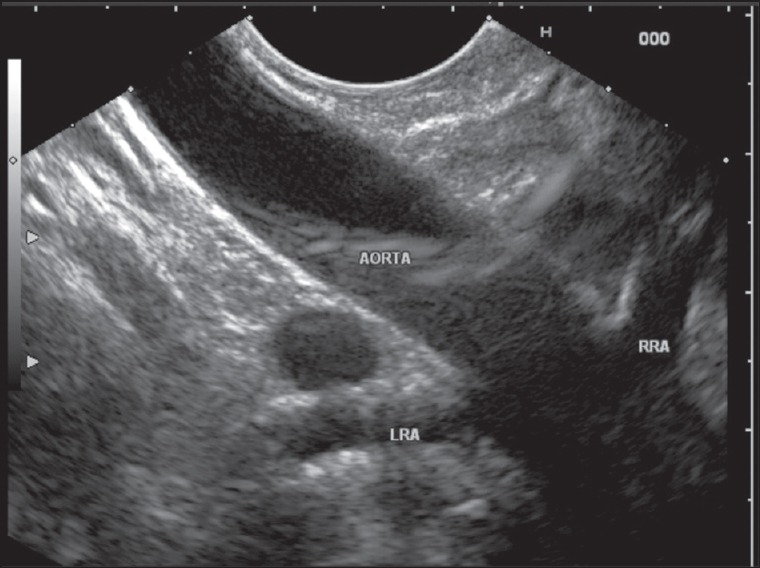
IMAGING FROM RECTUM
The bifurcation of the aorta can be traced from the rectosigmoid junction and also the DA can be followed-up for a limited distance above the bifurcation by rectal ultrasound [Figure 34 and Video 13].
Figure 34.
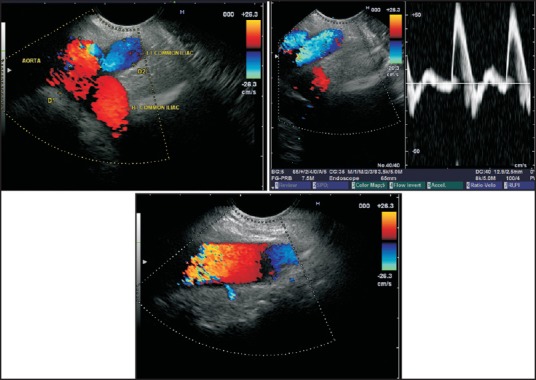
Imaging of the lowest part of the descending aorta is possible from the rectum. The scope should be positioned at about 20 cm distance (~rectosigmoid). From the rectosigmoid junction the vessel coming towards the probe is the left common iliac artery. The small lumbar arteries can be seen joining the aorta by clockwise and anticlockwise rotation
CONCLUSION
Endosonography can delineate the vascular anatomy of the aorta and its branches. The technique of imaging different parts of the aorta may be useful for beginners for proper orientation during EUS.
Videos are available at www.eusjournal.com
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Yamao K, Irisawa A, Inoue H, et al. Standard Imaging Techniques of endoscopic ultrasound-guided fine-needle aspiration using a curved linear array echoendoscope. Dig Endosc. 2007;19:S180–205. [Google Scholar]
- 2.Sharma M, Babu CS, Garg S, et al. Portal venous system and its tributaries: A radial endosonographic assessment. Endosc Ultrasound. 2012;1:96–107. doi: 10.7178/eus.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rameshbabu CS, Wani ZA, Rai P, et al. Standard imaging techniques for assessment of portal venous system and its tributaries by linear endoscopic ultrasound: A pictorial essay. Endosc Ultrasound. 2013;2:16–34. doi: 10.7178/eus.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma M, Rameshbabu CS, Mohan P. Standard techniques of imaging of IASLC borders by endoscopic ultrasound. J Bronchology Interv Pulmonol. 2011;18:99–110. doi: 10.1097/LBR.0b013e318207e6d5. [DOI] [PubMed] [Google Scholar]
- 5.Sharma M, Arya CL, Somasundaram A, et al. Techniques of linear endobronchial ultrasound imaging. J Bronchology Interv Pulmonol. 2010;17:177–87. doi: 10.1097/LBR.0b013e3181dca122. [DOI] [PubMed] [Google Scholar]
- 6.Sharma M, Chittapuram RS, Rai P. Endosonography of the normal mediastinum: The experts approach. Video Journal and Encyclopedia of GI Endoscopy. 2013;1:56–59. [Google Scholar]
- 7.Gotway MB, Helical CT. Evaluation of the thoracic aorta. Appl Radiol. 2000:29. [Google Scholar]
- 8.Hager A, Kaemmerer H, Rapp-Bernhardt U, et al. Diameters of the thoracic aorta throughout life as measured with helical computed tomography. J Thorac Cardiovasc Surg. 2002;123:1060–6. doi: 10.1067/mtc.2002.122310. [DOI] [PubMed] [Google Scholar]
- 9.Chuang ML, Gona P, Salton CJ, et al. Normal reference values for thoracic and abdominal aorta and main pulmonary artery dimensions by cardiovascular magnetic resonance: The Framingham Heart study. J Cardiovasc Magn Reson. 2013;15(Suppl 1):256. [Google Scholar]
- 10.Mao SS, Ahmadi N, Shah B, et al. Normal thoracic aorta diameter on cardiac computed tomography in healthy asymptomatic adults: Impact of age and gender. Acad Radiol. 2008;15:827–34. doi: 10.1016/j.acra.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaiser T, Kellenberger CJ, Albisetti M, et al. Normal values for aortic diameters in children and adolescents – assessment in vivo by contrast-enhanced CMR-angiography. J Cardiovasc Magn Reson. 2008;10:56. doi: 10.1186/1532-429X-10-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wanhainen A, Themudo R, Ahlström H, et al. Thoracic and abdominal aortic dimension in 70-year-old men and women – a population-based whole-body magnetic resonance imaging (MRI) study. J Vasc Surg. 2008;47:504–12. doi: 10.1016/j.jvs.2007.10.043. [DOI] [PubMed] [Google Scholar]
- 13.Demertzis S, Hurni S, Stalder M, et al. Aortic arch morphometry in living humans. J Anat. 2010;217:588–96. doi: 10.1111/j.1469-7580.2010.01297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Luca L, Bergman JJ, Tytgat GN, et al. EUS imaging of the arteria lusoria: Case series and review. Gastrointest Endosc. 2000;52:670–3. doi: 10.1067/mge.2000.109808. [DOI] [PubMed] [Google Scholar]
- 15.Yusuf TE, Levy MJ, Wiersema MJ, et al. Utility of endoscopic ultrasound in the diagnosis of aberrant right subclavian artery. J Gastroenterol Hepatol. 2007;22:1717–21. doi: 10.1111/j.1440-1746.2006.04622.x. [DOI] [PubMed] [Google Scholar]
- 16.Masri KR, Salyers WJ. Endoscopy ultrasound imaging of an abdominal aortic aneurysm. Kansas J Med. 2010;5:70–2. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


