Abstract
Background:
Low rates of thrombolysis for ischemic stroke in India and other developing countries have been attributed to delays in presentation to the hospital.
Materials and Methods:
A prospective study was carried out during a 12-month period ending December 2012 in the department of Neurology, Malabar Institute of Medical Sciences, Kerala, India, to look for the factors contributing to delay in hospital arrival of patients with acute stroke. Patients and or their relatives were interviewed within 48 hours of admission using a structured questionnaire.
Results:
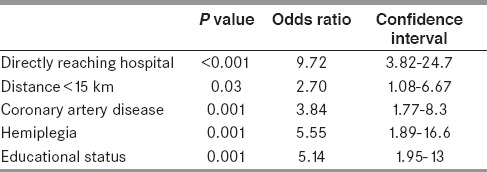
A total of 264 patients attending the emergency department were included. There were 170 men and 94 women. The mean age was 61.5 ± 12.4 years. A total of 67 (25%) patients presented within 4 hours of stroke onset. Factors associated with early arrival (multivariate logistic regression analysis) were distance 15 km or less from hospital (P 0.03, odds ratio (OR) 2.7), directly reaching the stroke department (P < 0.001, OR 9.7), history of coronary artery disease (P 0.001, OR 3.84), higher educational status (P 0.001, OR 3.7), and presence of hemiplegia (P 0.001, OR 5.5).
Conclusions:
We found a considerable delay in the early arrival of patients to our stroke department. Health promotion strategies to improve community awareness of early symptoms of stroke, education of local physicians about the importance of early referrals to the stroke centers, and wider availability and use of ambulance services are promising methods to help expedite presentation to hospital post stroke and thereby improve the management of stroke in India.
Keywords: Acute stroke, India, pre-hospital delay, stroke onset
Introduction
Prompt treatment of stroke, whether as thrombolytic therapy for ischemic stroke[1] or blood pressure control of hemorrhagic stroke,[2] is critical for improving patient outcome. The phrase “time is brain” emphasizes that human nervous tissue is rapidly and irretrievably lost as stroke progresses and that therapeutic interventions should be emergently pursued.[3] Recombinant tissue plasminogen activator (r-tPA) is currently the only Food and Drug Administration (FDA)-approved therapy for treatment of patients with acute stroke.[4] The therapeutic window is less than four and half hours and best results can be achieved with administration within 90 minutes.[1] However, only a small proportion of patients with acute stroke are currently eligible for thrombolysis because of excessive delay in presentation to hospital. Many factors have been shown to influence the time to hospital presentation of stroke patients. These factors include referral pattern, living alone, nocturnal onset, history of stroke or cardiovascular disease, transportation to the hospital, and clinical status.[5,6,7,8] Nonetheless, the majority of these studies have been undertaken in Western population. Factors associated with prolonged prehospital delays may differ between Indian and Western population due to variations in ethnicity, culture, socioeconomic features, and healthcare system.[9,10] Because of its differences from the West in social development patterns, India may also be unique in the management of stroke and in factors associated with prehospital delay. Previous two published series from India were from Northern part of the country. In this study, we therefore sought to evaluate the factors influencing the early and delayed presentations to hospital of patients with acute stroke in South India.
Materials and Methods
This was a cross-sectional study carried out between January 2012 to December 2012 in the department of Neurology, Malabar Institute of Medical Sciences, Calicut, Kerala, India. All patients of both gender, age >18 years with symptoms of stroke and neuro-imaging (computed tomography (CT) scan/magnetic resonance imaging (MRI) brain) findings consistent with stroke were included. Patients with in-hospital stroke were excluded from the study.
All patients who came to the Emergency Room (ER) of our center presenting with the symptoms of stroke were evaluated by the on-call Neurologist. A thorough clinical examination was conducted. Time of stroke onset was defined as the time the patient or an observer first noticed a neurological deficit. If the symptoms were present on waking, it was assumed that stroke had occurred during the night and the time of onset was taken when the patient was last seen without symptoms. Other studies have chosen the same definition of stroke onset for patients whose symptoms were detected on awakening.[11,12] The exact time of arrival at hospital is routinely marked on the form of ER. A standard structured questionnaire was completed for every patient by interviewing the patient (if possible) and accompanying attendant/relative after taking verbal consent. The questionnaire documented the patients age, sex, educational level, financial status. Education was categorized into illiterate and primary (below 5th standard), secondary (6th-12th standard), and college education. Information regarding the mode of transport to the hospital, whether the patients were living alone or in joint family, and the presence of any relative or friend during the time of onset of stroke was also gathered. Neurologic findings and the type of stroke was documented. Consciousness was assessed by Glasgow Coma Scale (GCS), which was further subgrouped into less than 8 and greater or equal to 8 to delineate patients who were conscious and unconscious. The stroke severity was documented using the National Institute of Health Stroke Scale (NIHSS). According to the time of presentation to the hospital after the onset of stroke symptoms, the patients were subclassified as early arrivers (<4 hours) and late arrivers (> 4 hours). The stroke onset time was broadly divided into day (7 am-7 pm) and night (7 pm-7 am). The distance travelled by the patients to hospital was categorized as 15 km or less and more than 15 km. This distance was arbitrarily considered because people living within a 15-km radius from the hospital, logically, would be able to arrive within 4-hour window period.
Data was analysed by using statistical package of social sciences (SPSS) version 10. Descriptive statistics, frequencies, and percentages were calculated for variables such as type of stroke, living conditions, time of stroke onset, status of financial support, and time of arrival to hospital after development of symptoms. Mean + standard deviation (SD) was used for continuous variables such as age. To assess the univariate relationship between early presentation to the hospital and the variables of interest, Chi-square test was used for qualitative data such as educational status, living conditions, time of onset, type of stroke, etc. For continuous data, t-test was applied where appropriate such as for mean age of patient in relation to delayed or timely arrival to hospital. Multivariate logistic regression analysis was performed to identify predictors of prehospital delay. Variables were eliminated in a stepwise backward fashion if they failed to reach significance which was <0.05 until a final model resulted. OR and 95% confidence intervals were generated for all the terms in the final model.
Results
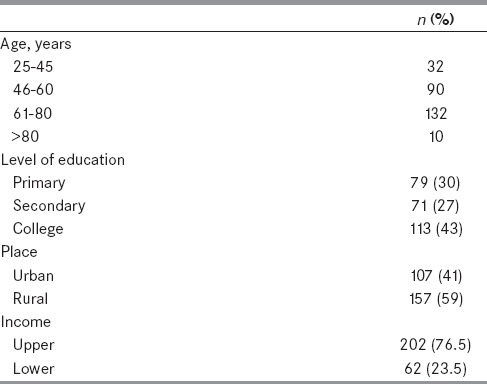
During the 12-months observational period, 264 patients that arrived in emergency department (ED) were included. There were 170 males and 94 females. The mean age was 61.5 ± 12.4 years. Demographic data of patients are given in Table 1. Of all patients, 136 (51.5%) patients had stroke onset in daytime (6 am to 6 pm) and 128 (48.5%) patients developed symptoms of stroke in the night (6 pm to 6 am). Seventy-four patients did not know that they were experiencing a stroke and 190 (72%) knew that they were experiencing stroke symptoms.
Table 1.
Demographic characteristics of patients
The stroke subtypes included ischemic stroke 191(72.3%); intracerebral hemorrhage 37 (14%); transient ischemic attacks (TIAs) 36 (13.6%). The mean National Institutes of Health (NIH) score was 8. In all, 234 (88%) patients had NIH score of less than 12. GCS score was 8 or higher in 238 (90%) patients. Fifty patients (19%) had a past history of stroke.
A total of 129 (49%) patients reached our hospital directly after the onset of symptoms. The rest consulted the local doctor before reaching our center. Among the 135 patients who consulted the local doctor after the symptom onset, only 11 (8%) arrived within 4 hours. The median delay from onset of symptoms to hospital arrival was 12 hours. Only 67 (25.3%) patients came within 4 hours, while 74.7% after 4 hours [Figure 1] (21.6% within 6 hours, 20.5% within 24 hours, and 32% more than 24 hours).
Figure 1.
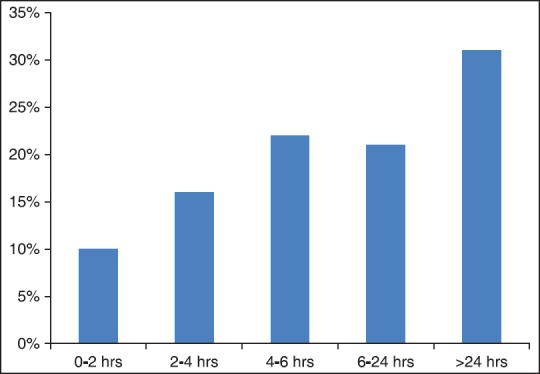
Time to presentation in A and E department
The mean time taken to consult a local doctor after the onset of stroke was 3 hours. The mean distance that patients had to travel was 31 km. There were 94 (35.6%) patients who were living within 15-km distance from our hospital; rest (170 patients, 64%) travelled more than 15 km to reach our hospital. Most of the patients used taxi as a mode of transport and only 79 patients (30%) were transported by ambulance. A relative or friend was present for 240 patients during the onset of stroke. The majority of our patients, 188 (71.2%) were living in a nuclear family. The mean NIH score was significantly higher in the early arrival group than late arrival group (6.5 versus 5.4- P value 0.002). The mean GCS score did not differ significantly in the two groups.
In the univariate analysis, living in the city (P 0.001), distance 15 km or less from the hospital (P 0.001), visit to local doctor (P < 0.001), symptom recognition (P 0.001), history of coronary artery disease (P < 0.001), hemiplegia (P < 0.001), hemorrhagic stroke (P < 0.001) were factors associated with an early arrival to the hospital [Table 2]. In the multivariate logistic regression analysis, directly arriving the hospital, distance less than 15 km from stroke department, history of coronary artery disease, and presence of hemiplegia were factors that remained significant [Table 3].
Table 2.
Factors contributing to an early arrival in univariate analysis
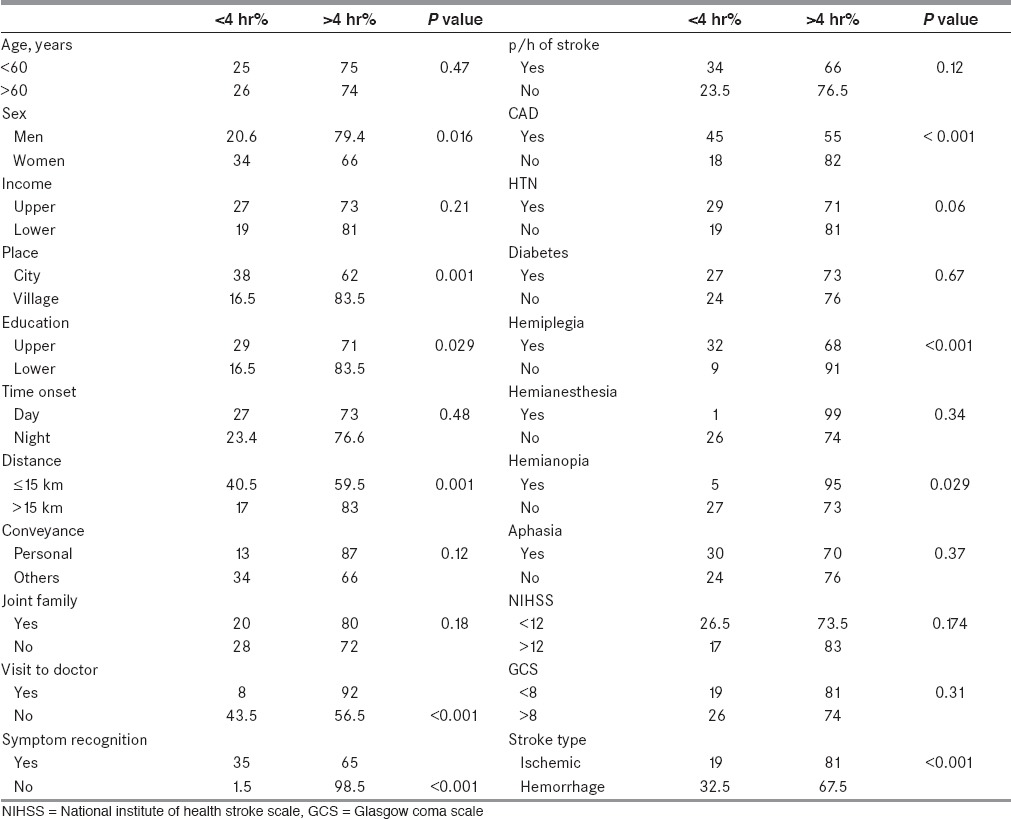
Table 3.
Factors contributing to an early arrival in multivariate logistic regression analysis
Discussion
We examined the various factors contributing to a delayed presentation to a stroke department in Southern India. The median prehospital delay of 12 hours is much longer than that reported by other Western, developed countries, which range from 3 to 6 hours,[13,14,15] but was shorter compared with a published series from China[16] and Denmark.[17] Only one-fourth of patients arrived at the hospital within 4 hours. The detrimental impact on management and patient outcome associated with such delays makes reduction of prehospital delay a primary focus for healthcare professionals. Directly reaching the stroke department, distance of 15 km or less from hospital, presence of coronary artery as risk factor, higher educational status, and presence of hemiplegia were associated with an early arrival, both in univariate and multivariate analysis.
Previous Indian studies kept 3 hours as the cut-off point for classifying early arrivers and late arrivers.[9,10] Some other studies kept 2 hours as cut-off point, considering the hospital delay (door to needle time).[18] With improvement in facilities for emergency stroke care, the median door to needle time has been even brought down to 20 minutes.[19] Various other studies done after the landmark Economic Community of Central African States (ECCAS) III trial, extending thrombolytic window to 4.5 hours, kept 4.5 hours as a cut-off point.[20] But we kept 4 hours as the cut-off point, considering the hospital delay for stroke thrombolysis.
Univariate analysis showed that female patients had shorter prehospital delays. Jin et al., reported that patients >65 years of age and female patients were more likely to arrive early than younger patients and males.[16] We did not find age ≥60 as a significant factor for early arrival. In many other reports, gender and age were not associated with prehospital delay.[14,21]
Our study showed that higher educational status, those from the city had shorter prehospital delays in univariate analysis. But income status was unrelated to prehospital delay in our data. Studies from Western world have shown that living alone is one of the important reasons for delay in seeking medical treatment.[17,22] Majority of our patients were living in a nuclear family (71%) unlike the previous Indian cohort from Punjab.[10] In this particular Indian study, 87% were living in joint family. In our study family type did not affect the arrival of stroke patients.
In this study, patients with prior strokes or transient ischemic attacks or comorbidities such as hypertension, diabetes did not seek medical help any faster than other patients. Patient's misperception or neglect of the seriousness of their condition may make it difficult for them to differentiate between pre-existing symptoms and new symptoms. Our findings therefore highlight the urgent need to educate this high risk patient group. Patients with a history of coronary artery disease had shorter prehospital delay times; however, this may be a reflection of greater awareness of heart disease than stroke.
Longer prehospital delays may be associated with the severity of stroke, because severe stroke may render patients unable to apply for help.[21,23] In patients who experiences relatively mild symptoms, prehospital delay times were longer compared with other subtypes of stroke. Though in univariate analysis NIHS score or GCS score was not a significant factor for early arrival of stroke patients, mean NIH stroke score was significantly higher in the early arrival group in our study. Patients with hemorrhagic strokes experienced reduced delays than those who had ischemic stroke. These findings imply that the perceived urgency due to severity of the condition may be a factor contributing to decreased prehospital delay. Similar findings have been reported in studies using different measures of stroke severity.[17,24]
The recognition of stroke symptoms by our patients was higher than the previous Indian studies and comparable to other western studies. Kothari et al., also found that level of stroke knowledge had no notable impact on prompt ED arrival. Many studies have demonstrated that use of ambulances can shorten prehospital delays.[25,26] Only 29% of patients in the study sought ambulance post onset. This rate is much lower than that in other developed countries, where ambulance use rates have been reported to be as high as 60%.[11] In India, emergency ambulance services are not readily available and, hence patients has to depend on other modes of transport to reach the hospital. One major determinant of delay is the referral pattern. It was noted that substantial proportion of patients (51%) contacted their local or community doctor first rather than going directly to ED. Contact with local doctor was associated with significant delay. This has been seen in other studies as well.[11,12,13,14,15,16,17,21,27] Majority of patients 63%, who came to our hospital after four hours had contacted their local or community doctor first which contributed to significant delay. Organization of a good network especially with the local physicians close to the hospital, and improving the emergency transport facilities, are essential for the effective use of thrombolytic therapy in India. The mean distance the patient had to travel to reach the stroke unit (31 km) was shorter than the previous North Indian study,[10] but longer than Western studies.[11,22] In the univariate and multivariate analysis, distance remained as a significant factor for an early arrival to the stroke department.
Factors causing early arrival of patients with stroke vary across different countries. It seems that arrival by ambulance, sudden onset of symptoms, and severe stroke are factors leading to early arrival in most of the developed nations. Studies from other Asian countries have shown contact with a local doctor, lack of knowledge of stroke symptoms, Intracerebral hemorrhage, younger age, transfer by ambulance, and history of coronary artery disease.[16,28,29,30] Factors contributing to an early arrival in previous Indian studies were older age, living in a city, direct arrival to ED, distance <10 km and presence of aphasia.[9,10] The factors for early presentation to our hospital are slightly different from these studies. This can be explained by variation in geographic, demographic, and organizational factors.
We acknowledge the limitations in our study. First it is a single-centered study using a small sample size. But this study provides a useful, representative picture of the current issues surrounding prehospital delay in presentation of acute stroke in this part of the world. Further studies are needed in large cohort of patients involving different stroke centers to confirm our findings.
The present study examined a multitude of factors that may contribute to delays in time to hospital presentation in large group of patients with stroke in India. Though the recognition of stroke symptoms was far better than previous observations, we found considerable delay in early presentation of our patients to the stroke unit. Living within 15 km from hospital, directly reaching the ED after the onset of symptoms, presence of hemiparesis, higher educational status, and previous history of coronary artery disease were factors associated with an early arrival. Many challenges to patients, physicians, and the healthcare systems exist; however, some of these challenges may be overcome. Notably, health promotion strategies to improve community awareness of early symptoms of stroke, transfer of patients directly to hospitals with thrombolysis facilities and wider feasibility and use of ambulance services are promising methods to help expedite presentation to hospital post stroke and thereby improve the management of stroke in India.
Acknowledgments
We are grateful to Mr. Sadjith of Malabar Institute of Medical Sciences Academy for statistical analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Eng J Med. 2008;359:317–29. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 2.Anderson CS, Huang Y, Wang JG, Arima H, Neal B, Peng B, et al. INTERACT Investigators. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): A randomised pilot trial. Lancet Neurol. 2008;7:391–9. doi: 10.1016/S1474-4422(08)70069-3. [DOI] [PubMed] [Google Scholar]
- 3.Saver LJ. Time is brain-quantified. Stroke. 2006;37:263–6. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 4.Marler JR, Tilley BC, Lu M, Brott TG, Lyden PC, Grotta JC, et al. Early stroke treatment associated with better outcome: The NINDS rt-PA study. Neurology. 2000;55:1649–55. doi: 10.1212/wnl.55.11.1649. [DOI] [PubMed] [Google Scholar]
- 5.Pittok SJ, Meldrum D, Hardiman O, Deane C, Dunney P, Hussey A, et al. Patient and hospital delays in acute stroke in Dublin teaching hospital. Iran Med J. 2003;96:167. [PubMed] [Google Scholar]
- 6.Mandelzweig L, Goldbourt U, Boyko V, Tanne D. Perceptual, social, and behavioural factors associated with delays in seeking medical care in patients with symptoms of acute stroke. Stroke. 2006;37:1248–53. doi: 10.1161/01.STR.0000217200.61167.39. [DOI] [PubMed] [Google Scholar]
- 7.Lacey CR, Suh DC, Beuno M, Kostis JB. Delay in presentation and evaluation for acute stroke: Stroke time registry for outcomes knowledge and epidemiology (S.T.R.O.K.E) Stroke. 2001;32:63–9. doi: 10.1161/01.str.32.1.63. [DOI] [PubMed] [Google Scholar]
- 8.Wester P, Radberg J, Lundgren B, Peltonen M. Factors associated with delayed admission to hospital and in hospital delays in acute stroke and TIA; A prospective, multicentre study. Seek-medical attention in time group. Stroke. 1999;30:40–8. doi: 10.1161/01.str.30.1.40. [DOI] [PubMed] [Google Scholar]
- 9.Srivastava AK, Prasad K. A study of factors delaying hospital arrival of patients with acute stroke. Neurol India. 2001;49:272–6. [PubMed] [Google Scholar]
- 10.Pandian JD, Kalra G, Jaison A, Deepak SS, Shamsher S, Padala S, et al. Factors delaying admission to a hospital-based stroke unit in India. J Stroke Cerebrovasc Dis. 2006;15:81–7. doi: 10.1016/j.jstrokecerebrovasdis.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Derex L, Adeline P, Nighoghossian N, Honnorat J, Trouillas P. Factors influencing early admission in a French stroke unit. Stroke. 2002;33:153–9. doi: 10.1161/hs0102.100533. [DOI] [PubMed] [Google Scholar]
- 12.Ferro JM, Melo TP, Oliveira V, Crespo M, Canhao P, Pinto AN. An analysis of admission delay of acute strokes. Cerebrovasc Dis. 1994;4:72–5. [Google Scholar]
- 13.Harraf F, Sharma AK, Brown MM, Lees KR, Vass RI, Kalra L. A multicentre observational study of presentation and early assessment of acute stroke. BMJ. 2002;325:17. doi: 10.1136/bmj.325.7354.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: The Genentech stroke presentation survey. Stroke. 2000;31:2585–90. doi: 10.1161/01.str.31.11.2585. [DOI] [PubMed] [Google Scholar]
- 15.Evenson KR, Foraker RE, Morris DL, Rosamond WD. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. Int J Stroke. 2009;4:187–99. doi: 10.1111/j.1747-4949.2009.00276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jin H, Zhu S, Wei WJ, Wang J, Liu M, Wu Y, et al. for China QUEST (Quality Evaluation of Stroke Care and Treatment) Investigators. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke. 2012;43:362–70. doi: 10.1161/STROKEAHA.111.623512. [DOI] [PubMed] [Google Scholar]
- 17.Jorgensen HS, Nakayama H, Reith J, Raaschou HO, Olsen TS. Factors delaying hospital admission in acute stroke: The Copenhagen stroke study. Neurology. 1996;47:383–7. doi: 10.1212/wnl.47.2.383. [DOI] [PubMed] [Google Scholar]
- 18.Tan TY, Chang KC, Liou CW. Factors delaying hospital arrival after acute stroke in Southern Taiwan. Chang Gung Med J. 2002;25:458–63. [PubMed] [Google Scholar]
- 19.Meretoja A, Strbian D, Mustanoja S, Tatlisumak T, Lindsberg PJ, Kaste M. Reducing in hospital delay to 20 minutes in stroke thrombolysis. Neurology. 2012;79:306–13. doi: 10.1212/WNL.0b013e31825d6011. [DOI] [PubMed] [Google Scholar]
- 20.Muengtaweepongsa S, Hunghok W, Harnirattisai T. Poor recognition of prompted treatment seeking even with good knowledge of stroke warning signs contribute to delayed arrival of acute ischemic stroke patients in Thailand. J Stroke Cerebrovasc Dis. 2014;23:948–52. doi: 10.1016/j.jstrokecerebrovasdis.2013.07.044. [DOI] [PubMed] [Google Scholar]
- 21.Kothari R, Jauch E, Broderick J, Brott T, Sauerbeck L, Khoury J, et al. Acute stroke: Delays to presentation and emergency department evaluation. Ann Emerg Med. 1999;33:3–8. doi: 10.1016/s0196-0644(99)70431-2. [DOI] [PubMed] [Google Scholar]
- 22.Alberts MJ, Bertels C, Dawson DV. An analysis of time of presentation after stroke. JAMA. 1990;263:65–8. [PubMed] [Google Scholar]
- 23.Zweifler RM, Mendizabal JE, Cunningham S, Shah AK, Rothrock JF. Hospital presentation after stroke in a community sample: The Mobile Stroke Project. South Med J. 2002;95:1263–8. [PubMed] [Google Scholar]
- 24.Cheung RT. Hong Kong patients’ knowledge of stroke does not influence time-to-hospital presentations. J Clin Neurosci. 2001;8:311–4. doi: 10.1054/jocn.2000.0805. [DOI] [PubMed] [Google Scholar]
- 25.Nedeltchev K, Arnold M, Brekenfeld C, Isenegger J, Remonda L, Schroth G, et al. Pre- and in-hospital delays from stroke onset to intra arterial thrombolysis. Stroke. 2003;34:1230–4. doi: 10.1161/01.STR.0000069164.91268.99. [DOI] [PubMed] [Google Scholar]
- 26.Williams LS, Bruno A, Rouch D, Marriott DJ. Stroke patients’ knowledge of stroke: Influence on time to presentation. Stroke. 1997;28:912–5. doi: 10.1161/01.str.28.5.912. [DOI] [PubMed] [Google Scholar]
- 27.Carroll C, Hobart J, Fox C, Teare L, Gibson J. Stroke in Devon: Knowledge was good, but action was poor. J Neurol Neurosurg Psychiatry. 2004;75:567–71. doi: 10.1136/jnnp.2003.018382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siddhiqui M, Siddiqui SR, Zafar A, Khan SF. Factors delaying hospital arrival of patients with acute stroke. J Pak Med Assoc. 2008;58:178–82. [PubMed] [Google Scholar]
- 29.Chang KC, Tseng MC, Tan TY. Prehospital delay after acute stroke in Kaohsiung, Taiwan. Stroke. 2004;35:700–4. doi: 10.1161/01.STR.0000117236.90827.17. [DOI] [PubMed] [Google Scholar]
- 30.Yu RF, San Jose MC, Manzanilla BM, Oris MY, Gan R. Sources and reasons for delays in the care of stroke patients. J Neurol Sci. 2002;199:49–54. doi: 10.1016/s0022-510x(02)00103-x. [DOI] [PubMed] [Google Scholar]


