Abstract
A six-year-old boy was diagnosed as recurrent posterior circulation stroke secondary to basilar artery occlusion with rapid progression of symptoms. Etiology of stroke was a dissection of V3 segment of left vertebral artery, which was treated using endovascular technique 26 hours after worsening of symptoms. Since the guidelines for acute revascularization in pediatric stroke are not well established, there is limited experience in the use of mechanical devices for acute ischemic stroke revascularization in children. To our knowledge, this is one of the youngest reported cases of acute ischemic stroke from Asia managed with newer mechanical clot removal devices.
Keywords: endovascular treatment, pediatric acute ischemic stroke, basilar occlusion, solitaire
BACKGROUND
Stroke in children differs from adult stroke in terms of etiology, symptomatology, management, and outcome. Guidelines regarding the management of acute ischemic stroke (AIS) in pediatric population are lacking. There are only a handful of described cases with successful endovascular revascularization in pediatric AIS. Posterior circulation strokes are associated with significant morbidity and mortality. We present our experience with a boy with recurrent posterior circulation infarcts due to basilar occlusion and vertebral artery dissection, refractory to medical management. Successful revascularization was performed using Solitaire™ FR (Covidien, Mansfield, MA) stent retriever.
CASE REPORT
Case Presentation and Investigations
A six-year-old male child was admitted at another institute with right-sided weakness which was noted on waking up. On examination, he had a Medical Research Council (MRC) power grade 3, right upper motor neuron facial palsy, and dysarthria with no cortical signs. There was no history of fever or trauma. He had been having intermittent giddiness and vomiting for the last two months and had an episode of transient left upper limb clumsiness two days before along with current symptoms.
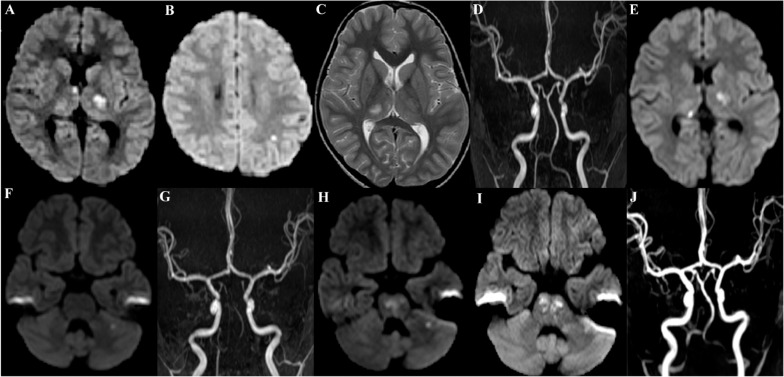
Magnetic resonance imaging (MRI) of brain showed acute infarction in the left thalamocapsular, anterior right thalamus, and left posterior parietal regions with normal intracranial angiogram. T2-weighted sequences also revealed a subacute infarct in the right thalamus [ Fig. 1(A–D)]. He was treated with aspirin (50 mg/day). Extensive workup for stroke in young was negative.
Figure 1. MRI brain at first presentation showing acute infarction in left thalamocapsular, right anterior thalamus, and left parietal areas (A, B) and subacute infarction in right thalamus (C) with normal intracranial angiogram (D). Subsequent MRI images showing occurrence of new recurrent infarcts in right posterior thalamus (E), left cerebellum (F), and pontomesencephalic areas (H). Images showing preintervention occlusion of BA (G) and 24 hours postrecanalization patent vertebrobasilar system (J) and residual areas of infarction (I).
Over the next 24 hours, he had complete clinical recovery. Two days later, he developed clumsiness on his left upper limb and a repeat MRI of brain showed a fresh infarct in the right posterior thalamus with normal intracranial angiogram ( Fig. 1E). After complete recovery, he was discharged on medical management after three days.
A day later, he had sudden onset of imbalance and vomiting. A small acute left cerebellar infarct was observed on brain MRI ( Fig. 1F). Noncontrast MRI angiogram (MRA) showed poor visualization of bilateral vertebral arteries (VA) and basilar artery (BA).
The following day, he developed worsening of sensorium with anarthria. MRI showed fresh infarcts in the pontomesencephalic region, and MRA showed nonvisualization of the BA [ Fig. 1. (G–H)]. He was referred to our institute for further management in view of worsening of symptoms with nonopacification of basilar artery.
Management and Follow-up
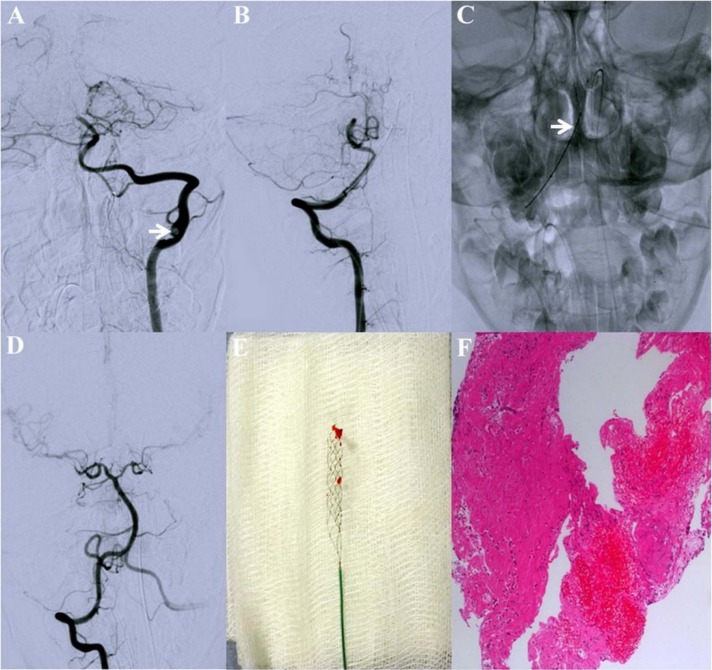
On arrival, the child was drowsy and irritable with multidirectional nystagmus, anarthria, right-sided weakness, and ataxia. Pediatric NIHS Score (Ped NIHSS) was 15. Cerebral angiogram under general anesthesia, using access via 5F femoral sheath, showed a dissection involving the left VA (V3 segment) with filling defect suggestive of thrombus and complete occlusion of the distal BA ( Fig. 2A).
Figure 2. Left VA angiogram showing left V3 dissection with thrombus (arrow head) and occlusion of distal BA (A). Microcatheter was negotiated through right VA (B) in to the BA. Proximal markers of Solitaire device (arrow head, C) and post-thrombectomy angiogram showing complete recanalization of BA (D). Macroscopic (E) and microscopic (F) view of thrombus.
In view of dissection of left VA, the right VA was used to access the BA (Fig. 2B). Microcatheter over microwire was negotiated in the right posterior cerebral artery (PCA) and its presence in the true lumen was confirmed. The clot was retrieved using Solitaire™ FR (4 × 20 mm) stent retriever in a single pass. Post-thrombectomy angiogram showed complete recanalization of the BA with faint flow in the PCA (Fig. 2D). The time to reperfusion from the onset of symptoms was 26 hours.
During postoperative period, anticoagulation was started after repeat imaging ruled out intracranial hemorrhage. Histopathological examination showed fragments of fibrinous material with many red blood cells (RBC) and chronic inflammatory cell infiltrate, consistent with a thrombus (Fig. 2F). He was discharged 10 days later on oral anticoagulation; Ped NIHSS and mRS were zero at the time of discharge. After three months, he is independent for ambulation and activities of daily living, without any focal deficits.
DISCUSSION
Pediatric arterial ischemic stroke is an important cause for morbidity, mortality, and dependency in children. Incidence of cerebrovascular disorders is observed to be 1.2–7.9 per 100,000 children [1] with the posterior circulation involved in 10–30% patients [2]. Stroke in children differs from those in adults in terms of etiology, clinical presentation, management, and recovery. In the absence of recanalization, mortality in BA stroke is observed to be around 15%, while those who survive may have residual deficits ranging from mild dysarthria to locked-in state [3]. Common underlying mechanisms for stroke in children include congenital or acquired cardiac diseases, trauma (especially leading to dissection), vascular (e.g., moya moya disease), hematological (e.g., sickle cell disease), infectious and metabolic disorders.[4]
Therapeutic options in adult acute ischemic stroke are intravenous (IV) tissue plasminogen activator (tPA) and mechanical thrombectomy. Unfortunately, in the absence of any randomized control trials (RCT), these validations cannot be extrapolated for use in pediatric patients. Early descriptions for the use of sophisticated clot retrieval devices in pediatric stroke can be traced back to early years of this century [5]. Newer clot retrieval devices, although validated for use in adults, have seen limited use in children [6–9].
Cases with mechanical clot removal in pediatric posterior circulation strokes were reported recently by Grunwald et al., [10] Fink et al., [7] Tatum et al., [8] and Bodey et al., [9]. Children with vertebrobasilar infarction are shown to have better outcome even with delayed recanalization. It appears that unlike adults, BA infarction in children has a better prognosis, probably due to greater neuroplasticity and fewer comorbid conditions [3]. Review of literature revealed a postrecanalization hemorrhage rate of 30.4% for intra-arterial (IA) tPA versus 9.1% (1 of 11) in those with mechanical revascularization, and this case had received IA tPA in addition to mechanical procedure [6].
The Solitaire™ FR device is a new generation device approved for mechanical thrombectomy. Tatum et al., [8] described three cases of BA infarcts treated with Merci and Penumbra devices. Although mean time to reperfusion in these cases was 12 hours and 41 minutes, modified Rankin score (mRS) of 0–3 was achieved in all cases at three months. Experience with Solitaire has been very limited, especially in BA occlusion. Bodey et al., [9] used Revive and Solitaire devices in three patients with BA infarct and mean time for recanalization was 19 hours and 20 minutes. Again, mRS of 0–3 was achieved in these patients at follow-up (Table 1). The common denominators in both these case reports are recanalization beyond 8 hours, excellent clinical outcome and the absence of reperfusion hemorrhage.
Table 1. Comparison with recently reported case series on use of advanced clot removal devices in pediatric basilar occlusion ischemic posterior circulation stroke.
| Present case | Tatum et al.,[8] | Bodey et al.,[9] | |
|---|---|---|---|
| Number of cases (n) | 1 | 3 | 3 |
| Mean pedNIHSS at presentation | 15 | 8 | 28 |
| Mean time to reperfusion | 26 hours | 12 hours 41 minutes | 19 hours 20 minutes |
| Hemorrhage | 0 | 0 | 0 |
| Clot removal device | Solitaire | Merci/Penumbra | Revive/Solitaire |
| Mean pedNIHSS at discharge | 0 | 6.33 | NA |
| Mean change in pedNIHSS | −15 | −3.5 | NA |
| mRS at follow-up | 0 | 0–3 | 0–3 |
Note: pedNIHSS, Pediatric National Institutes of Health Stroke Scale; mRS, Modified Rankin Scale; NA, Not available.
To the best of our knowledge, this is the first case from Asia to report the use of mechanical thrombectomy and the use of Solitaire device in pediatric posterior circulation stroke. The review of prior cases and the present case lead us to believe that the use of mechanical clot retrieval devices cannot be denied in large vessel pediatric stroke. Until further guidelines and recommendations, mechanical thrombectomy may be considered in carefully selected pediatric patients after consultation with pediatric and interventional neurologists.
Learning Objectives
Unlike adults, stroke in pediatric population needs extensive investigations for etiological diagnosis
Large vessel stroke in children has a better outcome even with delayed recanalization, due to better neuroplasticity and lesser comorbid conditions
Experience with Solitaire device in pediatric AIS is limited but positive
Mechanical clot removal may be considered in large vessel pediatric stroke
REFERENCES
- Fullerton HJ, Wu YW, Zhao S, Johnston SC. Risk of stroke in children: ethnic and gender disparities. Neurology. 2003;61(2):189–194. doi: 10.1212/01.wnl.0000078894.79866.95. [DOI] [PubMed] [Google Scholar]
- Touré A, Chabrier S, Plagne MD, Presles E, des Portes V, Rousselle C. Neurological outcome and risk of recurrence depending on the anterior vs. posterior arterial distribution in children with stroke. Neuropediatrics. 2009;40(3):126–128. doi: 10.1055/s-0029-1238306. [DOI] [PubMed] [Google Scholar]
- Rosman NP, Adhami S, Mannheim GB, Katz NP, Klucznik RP, Muriello MA. Basilar artery occlusion in children: misleading presentations, “locked-in” state, and diagnostic importance of accompanying vertebral artery occlusion. J Child Neurol. 2003;18(7):450–462. doi: 10.1177/08830738030180070601. [DOI] [PubMed] [Google Scholar]
- Roach ES, Golomb MR, Adams R, Biller J, Daniels S, Deveber G, Ferriero D, Jones BV, Kirkham FJ, Scott RM, Smith ER. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke J Cereb Circ. 2008;39(9):2644–2691. doi: 10.1161/STROKEAHA.108.189696. [DOI] [PubMed] [Google Scholar]
- Turk AS, Campbell JM, Spiotta A, Vargas J, Turner RD, Chaudry MI, Battenhouse H, Holmstedt CA, Jauch E. An investigation of the cost and benefit of mechanical thrombectomy for endovascular treatment of acute ischemic stroke. J Neurointerv Surg. 2014;6(1):77–80. doi: 10.1136/neurintsurg-2012-010616. [DOI] [PubMed] [Google Scholar]
- Ellis MJ, Amlie-Lefond C, Orbach DB. Endovascular therapy in children with acute ischemic stroke: review and recommendations. Neurology. 2012;79(13):S158–S164. doi: 10.1212/WNL.0b013e31826958bf. [DOI] [PubMed] [Google Scholar]
- Fink J, Sonnenborg L, Larsen LL, Born AP, Holtmannspotter M, Kondziella D. Basilar artery thrombosis in a child treated with intravenous tissue plasminogen activator and endovascular mechanical thrombectomy. J Child Neurol. 2013 Nov 1;28(11):1521–1526. doi: 10.1177/0883073812460334. [DOI] [PubMed] [Google Scholar]
- Tatum J, Farid H, Cooke D, Fullerton H, Smith W, Higashida R, Halbach VV, Dowd C. Mechanical embolectomy for treatment of large vessel acute ischemic stroke in children. J Neurointerv Surg. 2013;5(2):128–134. doi: 10.1136/neurintsurg-2011-010100. [DOI] [PubMed] [Google Scholar]
- Bodey C, Goddard T, Patankar T, Childs AM, Ferrie C, McCullagh H, Pysden K. Experience of mechanical thrombectomy for paediatric arterial ischaemic stroke. Eur J Paediatr Neurol. 2014;18(6):730–735. doi: 10.1016/j.ejpn.2014.07.006. [DOI] [PubMed] [Google Scholar]
- Grunwald IQ, Walter S, Shamdeen MG, Dautermann A, Roth C, Haass A, Bolar LJ, Reith W, Kuhn AL. New mechanical recanalization devices—the future in pediatric stroke treatment? J Invasive Cardiol. 2010;22(2):63–66. [PubMed] [Google Scholar]