Abstract
Researchers examining personality typologies of posttraumatic stress disorder (PTSD) have consistently identified 3 groups: low pathology, internalizing, and externalizing. These groups have been found to predict functional severity and psychiatric comorbidity. In this study, we employed Latent Profile Analysis to compare this previously established typology, grounded in temperament traits (negative emotionality; positive emotionality; constraint), to a novel typology rooted in interpersonal traits (dominance; warmth) in a sample of individuals with PTSD (n = 155). Using Schedule for Nonadaptive and Adaptive Personality (SNAP) traits to create latent profiles, the 3-group temperament model was replicated. Using Interpersonal Circumplex (IPC) traits to create latent profiles, we identified a 4-group solution with groups varying in interpersonal style. These models were nonredundant, indicating that the depiction of personality variability in PTSD depends on how personality is assessed. Whereas the temperament model was more effective for distinguishing individuals based on distress and comorbid disorders, the interpersonal model was more effective for predicting the chronicity of PTSD over the 10 year course of the study. We discuss the potential for integrating these complementary temperament and interpersonal typologies in the clinical assessment of PTSD.
Keywords: personality assessment, PTSD, latent profile analysis, interpersonal pathoplasticity, temperament
Personality trait models offer a promising framework for organizing the heterogeneity commonly observed among individuals with posttraumatic stress disorder (PTSD). To date, researchers have focused primarily on the “Big Three” temperament dimensions of negative emotionality (NEM), positive emotionality (PEM), and constraint (CON) when evaluating personality heterogeneity in PTSD. These three dimensions can be conceptualized as broadband individual differences in attributes involving affective experiences and regulation that confer risk for psychopathology (L. A. Clark, 2005). Using these traits, a typology of PTSD consisting of low pathology (low NEM), internalizing (high NEM and low PEM), and externalizing (high NEM and low CON) groups has been replicated in a number of samples (Flood et al., 2010; Forbes, Elhai, Miller, & Creamer, 2010; McDevitt-Murphy et al., 2012; Miller, Greif, & Smith, 2003; Miller, Kaloupek, Dillon, & Keane, 2004; Miller & Resick, 2007; Sellbom & Bagby, 2009; Wolf, Miller, Harrington, & Reardon, 2012).
Whereas the Big Three dimensions focus on individual differences in affective experience and self-regulation, interpersonal models focus on the ways individuals interact with one another and make meaning of relationships. For several disorders, individual differences in interpersonal traits involving dominance and warmth have been found to explain heterogeneity that cannot be accounted for by symptom severity (Pincus, Lukowitsky, & Wright, 2010), but interpersonal typologies of PTSD have not been examined. The extent to which a temperament typology will overlap with an interpersonal typology for explaining heterogeneity in PTSD is unknown. If these models augment one another in describing client characteristics or predicting outcome, it would open new avenues for understanding heterogeneity in PTSD and would suggest the potential clinical value of employing complementary personality models in PTSD assessment. In this study, we evaluate and compare temperament and interpersonal typologies of individuals with PTSD.
The Internalizing/Externalizing Typology of PTSD
The internalizing, externalizing, low pathology typology that has consistently been observed among individuals with PTSD is rooted in temperament traits of personality, organized around the Big 3 dimensions of NEM, PEM, and CON. NEM broadly refers to a tendency to experience negative emotional states such as anger, anxiety, depression, and vulnerability; PEM represents a tendency to experience positive emotions such as excitement and joy and to be actively engaged with the environment; CON reflects a disposition to avoid harm, minimize risk, and cautiously engage with the environment (Miller, 2003; Rothbart, Ahadi, & Evans, 2000).
Miller (2003) initially proposed a personality typology of PTSD in which high levels of NEM constitute a risk factor for the disorder, whereas levels of PEM and CON influence symptom expression. Miller and colleagues (2003) used cluster analysis to establish this typology in a sample of veterans who had experienced combat exposure. They found that 52% of veterans in a low pathology (i.e., low NEM) cluster met diagnostic criteria for PTSD, compared to 90% of veterans in both the internalizing (high NEM and low PEM) and externalizing (high NEM and low CON) clusters. Miller’s typology has been reliability identified across diverse samples, including male veterans with combat-related trauma (Flood et al., 2010; Miller et al., 2003, 2004), females with sexual assault trauma (Miller & Resick, 2007), mixed-gender participants with varied traumatic experiences (Sellbom & Bagby, 2009; Wolf et al., 2010), and individuals with PTSD and co-occurring personality disorders (PD; Wolf et al., 2012). Across these studies, individuals in low pathology groups tend to have relatively high scores on functioning measures and fewer co-occurring diagnoses; individuals in internalizing groups have high rates of avoidance, anxiety, and depression; and individuals in externalizing groups have high rates of antisociality, aggression, and substance abuse. These results indicate the usefulness of a temperament typology of PTSD for assessing functional severity and predicting likely patterns of comorbidity.
Importantly, all of the studies in which the low pathology, internalizing, and externalizing subtypes of PTSD were replicated employed one of three personality measures: the Multidimensional Personality Questionnaire (MPQ; Tellegen & Waller, 2008), the Minnesota Multiphasic Personality Inventory (MMPI) PSY-5 Scales (Harkness, McNulty, & Ben-Porath, 1995), or the Schedule for Nonadaptive and Adaptive Personality (SNAP; L. A. Clark, 1993). Although these personality measures differ in focus (e.g., clinical or normal range personality) and composition (e.g., different items and scales), all three assess the higher-order temperament traits of the Big Three model1 that focus on individual differences in affective experience and regulation.
The Interpersonal Model of Personality
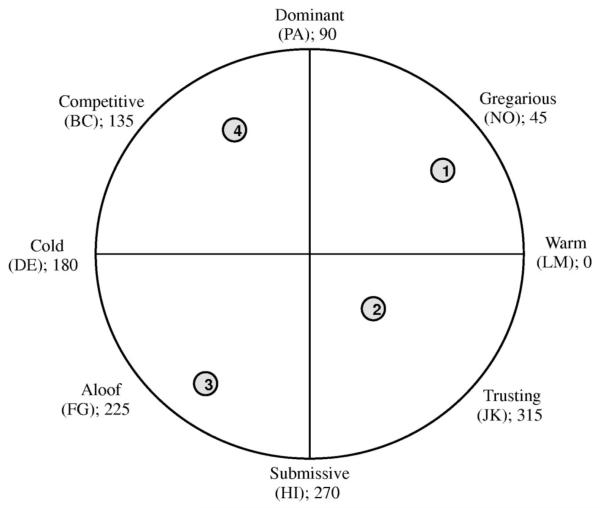
In contrast to temperament traits, which are associated with severity and style of psychopathology, interpersonal traits tend to yield typologies in which groups differ with regard to relationship style but do not differ with regard to disorder severity or comorbidity. Interpersonal traits can be measured using Interpersonal Circumplex (IPC) instruments (Leary, 1957; Wiggins, 1996), which assess the orthogonal traits dimensions of dominance and warmth as well as blends of each (Figure 1). Dominance reflects a tendency toward interpersonal assertion (as opposed to passivity); warmth reflects a tendency toward friendly interaction with others (as opposed to distance). Scores on these dimensions can be used to create groups such as warm-dominant (affiliative and controlling), warm-submissive (affiliative and passive), cold-submissive (distant and passive), and cold-dominant (distant and demanding).
Figure 1.
The interpersonal circumplex (IPC). The approximate group means for each latent profile are displayed in the figure above, with group membership indicated as follows: (1) warm-dominant, (2) warm-submissive, (3) cold-submissive, (4) cold-dominant. PA = Dominant; BC = Competitive; DE = Cold; FG = Aloof; HI = Submissive; JK = Trusting; LM = Warm; NO = Gregarious.
Distinct interpersonal groups have been identified among individuals with several forms of psychopathology, including bulimia nervosa (Ambwani & Hopwood, 2009), depression (Barrett & Barber, 2007; Cain et al., 2012), social phobia (Kachin, Newman, & Pincus, 2001), generalized anxiety disorder (GAD; Przeworski et al., 2011; Salzer et al., 2008), borderline personality disorder (Wright et al., 2013), and fear of failure (Wright, Pincus, Conroy, & Elliot, 2009). Across these studies, interpersonal traits were generally unrelated to psychopathology and functional severity; however, interpersonal traits have been found to relate to aspects of treatment. For instance, individuals with warm and submissive interpersonal styles have been found to have better therapy outcomes than individuals whose interpersonal styles consist of coldness and dominance (Borkovec, Newman, Pincus, & Lytle, 2002; Horowitz, Rosenberg, & Bartholomew, 1993). Drawing from a sample of individuals with major depressive disorder, Cain and colleagues (2012) found that, relative to individuals with dominant and/or warm interpersonal styles, individuals with submissive interpersonal styles did not suffer from a more severe depression at baseline but did experience more chronic levels of depression.
Such findings highlight the value of assessing interpersonal traits in clinical contexts. For instance, a cold-submissive interpersonal style may not put individuals at risk for developing PTSD. However, research suggests that a social support network is a protective factor in coping with and recovering from PTSD (Markowitz, Milrod, Bleiberg, & Marshall, 2009). Therefore, individuals who are distant and disengaged interpersonally may be at greater risk for maintaining PTSD than individuals who characteristically relate to others in warmer and more agentic ways. Despite the clinical potential of interpersonal typologies, they have not been investigated in PTSD samples, nor have interpersonal and temperament typologies been compared directly for any psychiatric diagnosis.
The Current Study
In summary, previous research using temperament models of personality have identified three types of individuals with PTSD: low pathology, internalizing, and externalizing. These types have differed with regard to functional severity and comorbidity patterns. Research using interpersonal measures has identified distinct interpersonal types in other disorders, including those with phenotypic similarities to PTSD. These interpersonal types are not distinguished by functional severity or comorbid conditions but differ instead in terms of course, treatment outcome, and relationship style. Interpersonal types have not been examined in PTSD and thus the degree to which these types provide unique information about individuals with PTSD relative to temperament types is unknown. Our goal was to extend research on personality heterogeneity in PTSD by examining the extent to which temperament and interpersonal typologies provide clinically useful but nonredundant information about individuals with PTSD.
Past research examining personality typologies of PTSD has primarily used cluster analysis to identify groups.2 The typical application of this technique assumes a priori that participants can be reliably categorized into a certain number of underlying groups (in the case of PTSD, researchers have selected three groups). In contrast, we used Latent Profile Analysis (LPA) to empirically identify the optimal number of groups underlying each personality model. We hypothesized that we would replicate Miller’s (2003) internalizing/externalizing/low pathology typology using the Big Three temperament traits as measured by the SNAP. We further hypothesized that a typology using interpersonal traits would yield a nonredundant and incrementally useful model of personality heterogeneity in PTSD. Based on research using the IPC with other disorders, we anticipated finding a four-group typology that arrayed around the quadrants of the circumplex. Specifically, we expected to find groups of individuals with PTSD that are prototypically warm-dominant, warm-submissive, cold-submissive, and cold-dominant. We tested the extent to which SNAP types and IPC types were redundant by comparing participants’ group membership in each typology.
We expected that whereas the SNAP typology would yield groups that varied in their degree of dysfunction and comorbidity, the IPC typology would consist of groups that differed in interpersonal style and prognosis but not in overall distress at the time of the assessment. To test this hypothesis, we examined rates of comorbid Axis I (generalized anxiety, alcohol, and substance use) and Axis II (antisocial and borderline) disorders across groups within each typology. For the SNAP typology, we expected a low pathology group to have the lowest rates of all disorders, an internalizing group to have higher rates of generalized anxiety, and an externalizing group to have higher rates of alcohol and substance use disorders and antisocial PD. In contrast, we did not expect interpersonal groups to differ with regard to rates of these comorbid diagnoses, with the exception that a group high in cold and dominant interpersonal traits would likely have higher rates of antisocial PD—given research indicating that antisocial PD is associated with cold-dominant interpersonal behavior (Hopwood & Morey, 2007; Wiggins & Pincus, 1989). Instead, we predicted that individuals with cold and submissive interpersonal styles would have the longest course of PTSD. This prediction was based on past research implicating poor social support as a maintaining mechanism of PTSD (Markowitz et al., 2009) and research suggesting that cold-submissive interpersonal styles are associated with less social support (Trobst, 2000). Additionally, in a previous study examining interpersonal typologies of depression, individuals with a cold-submissive interpersonal style had the longest symptom course (Cain et al., 2012).
Method
Participants
Data from the Collaborative Longitudinal Personality Disorders Study (CLPS; Gunderson et al., 2000) were used to test study hypotheses. CLPS participants met criteria for borderline (BPD), avoidant (AVPD), obsessive-compulsive (OCPD), or schizotypal (STPD) PD; or current major depressive disorder (MDD) without a PD. We drew individuals from this sample who also met Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; American Psychiatric Association, 1994) criteria for PTSD at baseline and completed the primary measures used in this study (n = 155). These participants had a mean age of 33.31 (SD = 7.64) and were largely female (75%, n = 117). The sample racial composition was 72% Caucasian, not of Hispanic origin (n = 112), 18% African American (n = 28), 8% Hispanic (n = 12), and 2% Asian (n = 3). These data were previously used to examine the replicability and 2-year stability of SNAP-derived typologies of PTSD using cluster analytic methods (McDevitt-Murphy et al., 2012). Results from this study indicated that Miller’s typology was recovered using Ward’s method. Whereas McDevitt-Murphy and colleagues (2012) examined the stability of cluster membership in temperament typologies over a 2-year period, our goal was to examine associations between aspects of psychiatric functioning and distinct temperament and interpersonal typologies to determine unique predictors of each personality typology.
Measures
Structured Clinical Interview for DSM–IV (SCID; First, Spitzer, Gibbon, & Williams, 1996)
The SCID was administered by experienced clinicians to identify individuals in the CLPS sample who met diagnostic criteria for PTSD. The kappa coefficient for interrater reliability of PTSD was .88 (Zanarini et al., 2000). SCID diagnoses were also used to evaluate patterns of comorbidity across distinct groups within each typology. Kappa coefficients for interrater reliability of Axis I disorders of interest in a baseline CLPS subsample (n = 52) were as follows: alcohol abuse/dependence (k = 1.00), drug abuse/dependence (k = 1.00), and GAD (k = .63).
Schedule for Nonadaptive and Adaptive Personality (SNAP; L. A. Clark, 1993)
The SNAP, a 375-item self-report questionnaire, assesses both normal and pathological personality characteristics. We estimated profiles using standardized scores on the three higher-order SNAP domains (viz., Negative Temperament [NEM], Positive Temperament [PEM], and Disinhibition [low CON]3) given the theoretical importance of these Big Three in previous personality typologies of PTSD. The median internal consistency of the higher-order SNAP scales in the CLPS sample was .89 (Morey et al., 2007). Scores were standardized within our sample and used to classify individuals with PTSD based on SNAP trait dimensions.
Revised NEO Personality Inventory (NEO-PI-R; Costa & McCrae, 1992)
The NEO-PI-R is a 240-item self-report measure that assesses the Five Factor Model (FFM) personality traits. Two factors, extraversion and agreeableness, can be conceptualized as rotated dimensions of the IPC (McCrae & Costa, 1989). Traupman and colleagues (2009) took advantage of this property to develop a method for deriving the eight octants of the IPC from a subset of NEO-PI-R items that emphasize interpersonal behavior. We tested the validity of these eight scales as IPC constructs with RANDALL (Tracey, 1997), a statistical program that assesses circumplex structure based on 288 predictions regarding the inter-correlations of octant scales. For instance, RANDALL predicts that adjacent circumplex octants should be more highly correlated than opposing octants (e.g., someone high in cold-dominance [octant BC] should be relatively high in coldness [DE] and in dominance [PA], but low in warm-submission [JK]; see Figure 1). Results yielded perfect RANDALL structure (288/288 predictions met, Correspondence Index = 1.00, p < .001), suggesting that this measure provides a valid representation of a circumplex model. Internal consistencies for these eight scales ranged from .58–.77 in this sample. Octant scales standardized within our sample were used to classify individuals with PTSD based on interpersonal dimensions.
Diagnostic Interview for DSM–IV Personality Disorders (DIPD-IV; Zanarini, Frankenburg, Sickel, & Yong, 1996)
The DIPD-IV, a semi-structured interview assessing diagnostic criteria for DSM–IV PDs, was administered by trained research assistants to select patients for the CLPS. Symptom counts from the DIPD-IV were also used to evaluate comorbid antisocial and borderline PDs across SNAP and IPC typologies. Kappa coefficients for interrater reliability of the study relevant PDs in a baseline subsample (n = 52) ranged from .86 – 1.0 (Zanarini et al., 2000).
Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al., 1987)
The LIFE is a semi-structured interview that was used to assess the longitudinal course of several disorders, including PTSD. It has demonstrated reliability in past research (e.g., Warshaw, Dyck, Allsworth, Stout, & Keller, 2001). The LIFE was administered at the baseline, 6-month, and each annual assessment over the 10-year course of the study. PTSD LIFE scores were coded as remitted (0), partial (1), or present (2) based on the number of symptoms met during a 1-week period for each week of the 10 year study. For the purposes of our analyses, PTSD was coded as either remitted (0) or [partially or fully] present (1) for each week. Scores for PTSD chronicity ranged the possible spectrum from 0–520 weeks (M = 268.77; SD = 186.49) over the 10-year study period.
Statistical Analyses
We conducted LPA in Mplus 6.1 (Muthén & Muthén, 2010) to empirically identify the optimal number of groups underlying each personality model. LPA is a person-centered technique that identifies underlying (i.e., latent) groups of individuals who share similar configurations on specified observed (i.e., manifest) variables. We conducted two separate LPAs on all participants. In the first model we used the three higher-order SNAP traits (NEM, PEM, and CON) as the manifest indicators. In the second model we used the IPC octant scores (PA, BC, DE, FG, HI, JK, LM, & NO; see Figure 1) as the manifest indicators.
We adjudicated fit (and thus the number of types to retain) based on the Akaike information criteria (AIC) and the Bayesian information criteria (BIC). The BIC index imposes a stricter penalty for estimating additional profiles and therefore tends to favor more parsimonious models relative to the AIC, which prefers the reduction in error that accompanies estimating additional profiles. In determining which model provides the best fit to the data, it is advantageous to consider both the AIC and BIC in conjunction (Burnham & Anderson, 2004). Given our relatively small sample, we applied a sample size correction to the AIC (referred to as the AICc) using the formula provided by Burnham and Anderson (2004). Additionally, to facilitate interpreting model fit across both the BIC and AIC, we subtracted the lowest obtained BIC value for each model from the BIC values obtained for all other solutions within that model (referred to as BICΔ); we did the same for AICc values (AICcΔ). This transformation sets the lowest BIC (AICc) value to zero and allows all other BIC (AICc) values to be readily interpreted within the context of the best fitting solution. Models that are within an absolute value of two from the best fitting model (i.e., the model that equals zero) are considered to have “substantial support” (Burnham & Anderson, 2004). Our model selection approach was to give serious consideration to models falling within the range of those suggested by the AICc and BIC while also evaluating them for substantive interpretability. In general, however, we preferred to select the more parsimonious model and therefore prioritized the BIC in selecting the optimal solution for each typology. We also evaluated entropy, which indicates the certainty of classification, for each solution. Entropy values above .80 are considered acceptable, whereas entropy values below .80 indicate too much uncertainty of how to classify individuals to be reliable (S. Clark & Muthén, 2012).
We took advantage of the circular properties of IPC data by evaluating circular statistics and IPC structural summary parameters (Gurtman & Balakrishnan, 1998; Wright, Pincus, Conroy, & Hilsenroth, 2009) for the full sample and each IPC profile. Structural summary parameters indicate the average IPC location of a group (angle), the variance around that location (amplitude), the average item endorsement (elevation), and the degree to which a profile conforms to prototypical expectations of a circumplex such that adjacent scales are rated more similarly than opposing scales (R2—with higher values indicating higher prototypicality). Circumplex statistics indicate the mean IPC placement of a group as well as the group’s variation around this mean and associated 95% confidence interval. Circumplex statistics can test mean differences in mean IPC placement across groups by examining the confidence interval around each group.
To test the hypothesis that the SNAP and IPC would yield unique typologies, we evaluated the degree of classification agreement using the adjusted Rand statistic (1971; Hubert & Arabie, 1985). The Rand statistic indicates how similar two classifications are by evaluating the percentage of instances in which they agree upon pair-wise decisions. For example, the SNAP and IPC solutions could agree that participant A and participant B belong to the same profile or agree that they belong to different profiles. If, however, participants A and B are in the same SNAP profile but different IPC profiles, this would indicate disagreement across the two solutions. We used the adjusted Rand statistic, which corrects for levels of chance agreement.
To test hypotheses concerning comorbidity, we evaluated diagnostic patterns across profiles using χ2 analyses. Specifically, we examined whether groups within each typology differed with regard to rates of GAD, alcohol use disorder, substance use disorder, antisocial and borderline PDs. We also examined whether groups from the IPC typology differed in mean levels of NEM using a one-way analysis of variance (ANOVA), to test the hypothesis that IPC groups would not differ with regards to distress. To evaluate PTSD chronicity, we summed LIFE ratings over 520 weeks (10 years) from participants who completed each assessment of the study (n = 137). We then compared differences in PTSD chronicity across SNAP and IPC groups using a one-way ANOVA with a post hoc Duncan test to test the hypothesis that interpersonal characteristics would predict the course of PTSD but temperamental characteristics would not.
Results
Profile Characteristics for Temperament and Interpersonal Typologies
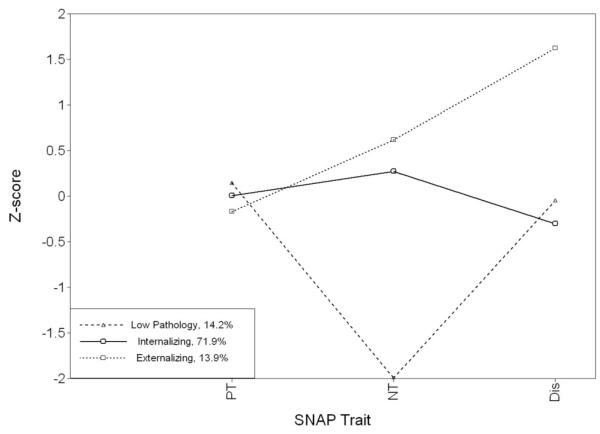
Individuals diagnosed with PTSD were classified using standardized scores from the higher-order SNAP traits and the NEO-PI-R derived IPC octants. For the SNAP model, the BICΔ value was lowest for a two-profile solution; however, the AICcΔ value for this solution indicated poor fit (see Table 1). The lowest combined AICcΔ and BICΔ value was observed for the three-profile solution. This solution also demonstrated acceptable classification certainty (i.e., entropy). The three resulting types were readily interpretable as low pathology, internalizing, and externalizing groups and were labeled accordingly4 (see Table 2). Figure 2 displays prototypical differences on SNAP traits among the three groups.
Table 1. Model Fit and Entropy Statistics for Latent Profile Analyses.
| Solution | AICc (AICc Δ) | BIC (BIC Δ) | Entropy |
|---|---|---|---|
| SNAP model | |||
| One-profile | 1,329.17 (55.40) | 1,346.86 (34.78) | — |
| Two-profile | 1,283.17 (9.40) | 1,312.08 (0.00) | .93 |
| Three-profile | 1,275.33 (1.56) | 1,314.94 (2.86) | .84 |
| Four-profile | 1,274.18 (0.41) | 1,323.93 (11.85) | .84 |
| Five-profile | 1,273.77 (0.00) | 1,333.06 (20.98) | .82 |
| Six-profile | 1,275.02 (1.25) | 1,343.18 (31.10) | .83 |
|
| |||
| IPC model | |||
| One-profile | 3,461.52 (228.06) | 3,506.28 (174.05) | — |
| Two-profile | 3,346.82 (113.36) | 3,412.82 (80.59) | .72 |
| Three-profile | 3,252.24 (18.78) | 3,335.88 (3.65) | .84 |
| Four-profile | 3,235.45 (1.99) | 3,332.23 (0.00) | .83 |
| Five-profile | 3,233.46 (0.00) | 3,337.68 (5.45) | .83 |
| Six-profile | 3,248.86 (15.40) | 3,353.17 (20.94) | .85 |
Note. AICc Δ (BIC Δ) values were computed by subtracting the lowest obtained AICc (BIC) value for each model from all other AICc (BIC) values within that model to set the value for the best-fitting model to zero. Dashes indicate that entropy is not calculated for a one-profile solution because classification is certain (i.e., all individuals are placed in the single estimated group). The preferred solution for each personality model is bolded. AICc = Aikake information criterion, corrected for sample size; BIC = Bayesian information criterion; SNAP = Schedule for Nonadaptive and Adaptive Personality; IPC = Interpersonal Circumplex.
Table 2. Mean Z-Scores (and Standard Deviations) for SNAP and IPC Profile Solutions and Structural Summary and Circular Statistics for IPC Groups.
| SNAP profiles |
|||
|---|---|---|---|
| Dimension | Low pathology | Internalizing | Externalizing |
| Traits | |||
| n (percentage of sample) | 22 (14%) | 115 (74%) | 18 (12%) |
| Negative temperament (NEM) | −2.02 (.71) | .29 (.54) | .61 (.48) |
| Positive temperament (PEM) | .17 (1.00) | −.02 (.99) | −.09 (1.10) |
| Disinhibition (CON) | −.06 (.98) | −.29 (.69) | 1.92 (.43) |
| IPC profiles |
||||
|---|---|---|---|---|
| Octants | Warm-dominant | Warm-submissive | Cold-submissive | Cold-dominant |
| n | 23 (14%) | 59 (39%) | 40 (25%) | 33 (22%) |
| Dominant (PA) | .94 (.75) | −.42 (.57) | −.72 (.82) | .93 (.90) |
| Competitive (BC) | −.66 (.72) | −.46 (.61) | −.56 (.79) | 1.08 (.77) |
| Cold (DE) | −.75 (.70) | −.39 (.67) | .89 (.67) | 1.08 (.63) |
| Aloof (FG) | −.77 (.67) | −.01 (.62) | 1.18 (.58) | .13 (.66) |
| Submissive (HI) | −.53 (.87) | .22 (.80) | .80 (.78) | −.53 (.97) |
| Trusting (JK) | .18 (.90) | .42 (.72) | .10 (.88) | −.70 (.83) |
| Warm (LM) | .80 (.74) | .25 (.79) | −.43 (1.18) | −.28 (.91) |
| Gregarious (NO) | .98 (.56) | −.22 (.53) | −1.16 (.58) | .31 (.85) |
| Structural summary | ||||
| Angle | 32.05° | 308.14° | 235.29° | 131.00° |
| Amplitude | 0.99 | 0.45 | 1.11 | 0.95 |
| R 2 | 0.91 | 0.98 | 0.94 | 0.98 |
| Circular statistics | ||||
| Circular mean (95% circular CI) | 33.73° [22.53°, 44.93°] | 307.22° [294.17°, 320.27°] | 234.85° [226.92°, 242.78°] | 133.22° [122.89°, 144.55°] |
| Circular variance | 27.40° | 51.14° | 25.59° | 30.28° |
Note. Structural summary and circular statistics for the full sample are as follows: angle = 245.23°; amplitude = 0.15; r2 = .59; circular m = 268.06°; circular variance = 80.01°; and 95% circular confidence interval (CI) = 255.46°, 280.65°. IPC = Interpersonal Circumplex; SNAP = Schedule for Nonadaptive and Adaptive Personality.
Figure 2.
Mean trait scores for each latent profile using the SNAP. NT = Negative Temperament; PT = Positive Temperament; Dis = Disinhibition; SNAP = Schedule for Nonadaptive and Adaptive Personality.
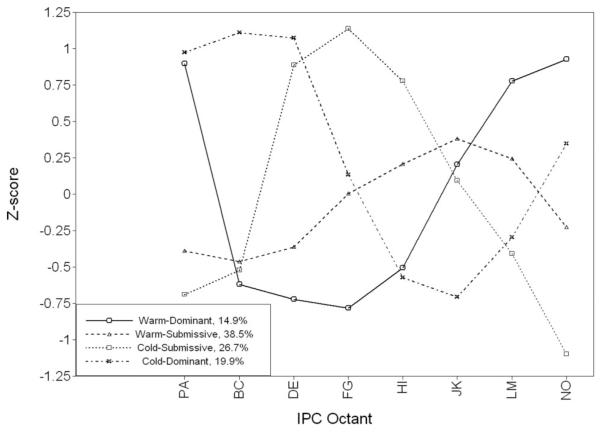
For the IPC model, structural summary and circular statistics indicate that the full PTSD sample was located in the cold-submissive quadrant of the IPC; however, this location is not readily interpretable given the high degree of variance in the overall group and thus low prototypicality of this profile (see Table 2). This finding indicates the utility of examining distinct interpersonal groups. LPA results indicated that the four-profile solution yielded the lowest BICΔ value and was also supported by the AICcΔ value (see Table 1). Entropy for this solution was also acceptable. As expected, these four profiles arrayed across the circumplex quadrants and were labeled based on the dimensions of coldness to warmth and dominance to submission (Table 2). Membership was relatively balanced across groups, although results from a binomial probability test indicate significantly more participants in the warm-submissive group than would be expected by chance (38%, whereas 25% were expected based on chance; p < .05). Each of the four IPC groups was highly prototypical (i.e., R2 > .90) and each had distinct angles located across the four quadrants of the IPC, respectively (Table 2). Prototypical differences on IPC octant scores across groups are visually displayed in Figure 3. Groups within each personality typology did not differ demographically (Table 3).
Figure 3.
Mean octant scores for each latent profile using the IPC. PA = Dominant; BC = Competitive; DE = Cold; FG = Aloof; HI = Submissive; JK = Trusting; LM = Warm; NO = Gregarious; IPC = interpersonal circumplex.
Table 3. Demographic Characteristics for Each Profile.
| Profile | Mean age (SD) |
% Female | % Caucasian |
|---|---|---|---|
| SNAP | |||
| Low pathology | 34.41 (7.86) | 64 | 59 |
| Internalizing | 33.47 (7.67) | 77 | 72 |
| Externalizing | 30.67 (7.19) | 72 | 89 |
| Test statistics | F(2) = 1.33 | η(2) = .11 | η(2) = .14 |
| IPC | |||
| Warm-dominant | 31.39 (8.54) | 82 | 70 |
| Warm-submissive | 34.37 (7.56) | 81 | 75 |
| Cold-submissive | 34.03 (7.05) | 65 | 70 |
| Cold-dominant | 31.73 (7.75) | 70 | 73 |
| Test statistics | F(3) = 1.46 | η(3) = .21 | η(3) = .12 |
Note. There were no significant (p < .05) demographic differences between groups in either model. Age was assessed using a one-way analysis of variance; gender and ethnicity were assessed using a χ2 test; IPC = Interpersonal Circumplex; SNAP = Schedule for Nonadaptive and Adaptive Personality.
Distinctness of Temperament and Interpersonal Typologies
We examined overlap between the interpersonal and temperamental typologies using the adjusted Rand statistic (Hubert & Arabie, 1985). Results indicated very minimal overlap between the typologies (adjusted Rand = .05), suggesting that they provide nonredundant information about patient heterogeneity (Table 5). This value is substantially lower than values reported by Morey and colleagues (1983) for clustering solutions in which scores from the same instrument were tested for replication across samples. Using Ward’s method, they found relatively high agreement when comparing two 3-cluster solutions to one another (adjusted Rand = .53) and when comparing a 3- to a 4-cluster solution (adjusted Rand = .49). To the degree that such replications reflect an upper expectation for agreement, the value in our study suggests substantial disagreement across the SNAP and IPC models. Where overlap was observed, it was highest between the SNAP externalizing group and the IPC cold-dominant group. In general, however, knowing an individual’s group membership in one model does not permit accurate predictions regarding his or her group membership in the other model, suggesting that these two models provide distinct information about personality among the individuals in this sample.
Table 5. Crosstabs of Profiles Across the SNAP and IPC Models.
| SNAP profile |
|||
|---|---|---|---|
| IPC profile | Low pathology | Internalizing | Externalizing |
| Warm-dominant | 18.2% | 14.8% | 11.1% |
| Warm-submissive | 40.9% | 41.7% | 11.1% |
| Cold-submissive | 9.1% | 28.7% | 27.8% |
| Cold-dominant | 31.8% | 14.8% | 50.0% |
Note. Percentages were computed vertically (e.g., 18.2% of individuals in the low pathology SNAP group were in the warm-dominant IPC group). IPC = Interpersonal Circumplex; SNAP = Schedule for Nonadaptive and Adaptive Personality.
Patterns of Comorbidity and Chronicity
Patterns of comorbidity with Axis I and Axis II disorders were assessed using χ2 tests (Table 4). As expected, the externalizing SNAP group had the highest rates of alcohol and substance use as well as antisocial and borderline PDs. Although we expected GAD would be highest for the internalizing group, no significant differences across groups were found for this diagnosis between the externalizing and internalizing groups However, the low pathology group had substantially fewer individuals diagnosed with GAD than the other groups. There were no significant differences between the SNAP groups in weekly PTSD chronicity over 10 years.
Table 4. Percentage of Individuals in Each Profile With Select Diagnoses and Mean (SD) Number of Weeks Participants Met Partial or Full PTSD Criteria Over 10 Years.
| Profile | Generalized anxiety disorder |
Alcohol use disorder |
Substance use disorder |
Antisocial PD |
Borderline PD |
10-year PTSD chronicity |
|---|---|---|---|---|---|---|
| SNAP | ||||||
| Low pathology | 4.5% | 40.9% | 72.7% | 45.5% | 36.3% | 277.00 (271.83) |
| Internalizing | 26.1% | 47.0% | 51.3% | 37.4% | 60.9% | 385.94 (331.30) |
| Externalizing | 22.2% | 94.4% | 88.9% | 88.9% | 94.4% | 325.00 (325.55) |
| Test statistic | 4.93 | 15.23 | 11.19 | 16.72 | 14.11 | 1.14 |
| IPC | ||||||
| Warm-dominant | 8.7% | 39.1% | 52.2% | 30.4% | 52.2% | 255.71 (224.92)a |
| Warm-submissive | 16.9% | 45.8% | 55.9% | 39.0% | 66.1% | 365.61 (325.43)a,b |
| Cold-submissive | 40.0% | 60.0% | 62.5% | 40.0% | 47.5% | 519.03 (319.02)b |
| Cold-dominant | 21.2% | 60.6% | 63.6% | 69.7% | 75.8% | 252.48 (319.48)a |
| Test statistic | 10.59 | 4.44 | 1.61 | 11.38 | 7.50 | 4.87 |
Note. Test statistics for each disorder are Pearson chi-square values; the test statistic for 10-year PTSD chronicity is an F value from a one-way analysis of variance. Values for 10-year PTSD chronicity indicate the mean (and standard deviation) number of weeks that participants in each group met at least partial criteria for PTSD. Bolded values are significant at p < .05. Subscripts with the same letter indicate that those group means do not significantly differ from one another based on a post-hoc Duncan test. The mean value for PTSD chronicity was 361.77 weeks (SD = 322.4). In examining chronicity, we only included participants who had data for all 10 years of the study (n = 137). This resulted in smaller group sizes for this analysis. Specifically, the following percentage of participants initially classified in each group completed all 10 years of the study: SNAP low pathology (100%), internalizing (87%), externalizing (83%), IPC warm-dominant (91%), warm-submissive (92%), cold-submissive (83%), cold-dominant (88%). PTSD = posttraumatic stress disorder; PD = personality disorder; IPC = Interpersonal Circumplex; SNAP = Schedule for Nonadaptive and Adaptive Personality.
We expected that IPC traits would be unrelated to psychiatric severity and therefore no significant differences would be observed across IPC groups for comorbid diagnoses. Consistent with our expectations, significant differences in alcohol and substance use disorders were not observed across IPC groups and the cold-dominant group had significantly more members who met criteria for antisocial PD. Unexpectedly, individuals in the cold-submissive IPC group had significantly higher rates of generalized anxiety disorder than individuals in the other three groups. Thus, generalized anxiety, at least within this sample selected for PTSD, was related to interpersonal style (however, see also Przeworski et al., 2011; Salzer et al., 2008).
Consistent with our hypothesis regarding the impact of interpersonal style on symptom course, the warm-dominant and cold-dominant groups both had less chronic PTSD than the cold-submissive group. Specifically, whereas individuals in the warm-dominant and cold-dominant groups met criteria for PTSD for an average of 256 and 252 weeks of the 10-year study, respectively, individuals in the cold-submissive group met criteria for PTSD for an average of 519 weeks (see Table 4).
Discussion
Temperament and Interpersonal Typologies of PTSD
The purpose of this study was to better understand temperamental and interpersonal variability among individuals with PTSD. Using a measure that focuses on temperament traits related to affective experiences and regulation, we replicated the low pathology, internalizing, and externalizing typology that has been identified in previous research in PTSD samples (Flood et al., 2010; Forbes et al., 2010; Miller et al., 2003, 2004; Miller & Resick, 2007; Sellbom & Bagby, 2009; Wolf et al., 2010, 2012). Our replication of this typology in a high-severity sample enhances the credibility of this model. Individuals in this typology could be distinguished based on the presence of relatively low NEM (low pathology), high NEM and high CON (internalizing), or high NEM and low CON (externalizing). Unlike much past research that has found higher levels of PEM in a low pathology group relative to an internalizing group, mean PEM scores did not differ across groups in our sample. Further, the number of individuals in the internalizing group was disproportionally high. Both of these findings may reflect the severity of disturbance of individuals in the CLPS sample, in whom levels of NEM were found to be higher, and levels of PEM lower, than community norms (Morey et al., 2003).
Consistent with past research, individuals in the low pathology group had the lowest rates of co-occurring GAD, and individuals in the externalizing group had higher rates of comorbid alcohol, substance abuse, and antisocial personality pathology. Results from the temperament typology in this study suggest that NEM may predict the severity of PTSD, whereas CON is likely to differentiate individuals with internalizing and externalizing PTSD from one another in a high severity clinical sample.
The IPC yielded an alternative perspective on personality heterogeneity that has been unrecognized in previous research with PTSD, although it has been identified in research focusing on other disorders. This typology distinguished individuals with PTSD based on their tendencies to be both friendly and controlling toward others (warm-dominant), to be engaged but passive in their interpersonal interactions (warm-submissive), to have limited interest in interpersonal engagement or control (cold-submissive), or to be competitive and antagonistic with others (cold-dominant). As predicted, this model was not as strongly related to severity or comorbid psychopathology as the temperament-based typology; however, unlike past research (Przeworski et al., 2011; Salzer et al., 2008), rates of GAD were higher in the cold-submissive group than in other groups. This finding may have been, in part, a function of the composition of the sample. For instance, 25.9% of individuals with GAD also had avoidant PD (see McGlashan et al., 2000, for results from full sample), which was a selection criterion and has been associated with cold-submissive interpersonal behavior (Wiggins & Pincus, 1989).
Unlike the temperament model, the IPC typology predicted PTSD chronicity over the 10 years of the study. The interpersonal approach to personality assessment therefore appears to complement the more established temperament typology by providing a useful means for conceptualizing how an individual with PTSD is likely to function within relationships and how this might influence symptom chronicity. For instance, given their tendency to withdraw from others, individuals with cold and submissive interpersonal styles may be likely to have fewer social connections than individuals with warm interpersonal styles, which may in turn serve to extend the course of their PTSD (Markowitz et al., 2009). Furthermore, given that interpersonal dominance is associated with agentic goals and behaviors (Kiesler, 1996), individuals with low levels of dominance may be less likely to be agentic in their recovery process compared to individuals wither more dominant interpersonal styles and may therefore experience a more prolonged recovery. Given the utility of this kind of information for treatment planning (Anchin & Pincus, 2010; Pincus et al., 2010), these results suggest that there is considerable value in the clinical assessment of interpersonal characteristics among individuals with PTSD.
An analysis comparing group membership across each typology indicated that temperament and interpersonal models largely provided nonredundant information. To the extent that overlap was observed, it was highest between the externalizing SNAP group and the cold-dominant IPC group (Table 5). This pattern may reflect the association antisocial personality pathology shares with both the externalizing spectrum (e.g., Krueger, 1999) and the cold-dominant quadrant of the IPC (Hopwood & Morey, 2007; Wiggins & Pincus, 1989).
Integrating Temperament and Interpersonal Models
Previous authors have speculated various ways that personality and psychopathology relate to one another (e.g., Klein, Wonderlich, & Shea, 1993; Widiger & Smith, 2008). Alternatives include a direct model, which emphasizes the diathetic potential of personality traits to predispose psychopathology, a scar model, which highlights the possibility that traumatic experiences alter personality functioning, and a pathoplastic model, which highlights aspects of personality that are largely unrelated to symptoms or severity of psychopathology. Our study suggests that a temperament model provides information relevant to direct and/or scar associations between personality and PTSD, whereas an interpersonal model informs a pathoplastic understanding of personality and psychopathology. For instance, an individual with high NEM and low PEM is likely to experience an internalizing form of PTSD following exposure to a trauma, whether this is because the dispositions increased risk for PTSD, trauma affected these traits, or there was some interplay between these factors. In contrast, these results suggest that one’s interpersonal style is mostly unrelated to risk for developing PTSD. However, interpersonal style is related to recovery from PSTD symptoms such that individuals, who tend to be cold and submissive, are more likely to experience a chronic form of PTSD.
Thus, a broad implication of this study is that temperament and interpersonal models may provide different kinds of information about individuals with the same diagnosis. The groups in the temperament model convey the severity and type of distress an individual with PTSD is most likely to experience. Individuals in the low pathology group experience less functional distress than members in either the internalizing or externalizing groups. Members of the internalizing group may suffer from prominent mood and anxiety symptoms associated with PTSD, whereas those in the externalizing type might be more likely to “act out” or attempt to self-medicate with substances, leading to others kinds of problems.
In contrast, interpersonal traits provide context for the way symptoms may be expressed and indicate the rate at which individuals will tend to recover. The results of this study suggest that individuals with cold and submissive interpersonal styles are at risk for experiencing more chronic PTSD, perhaps as a result of their difficulties engaging with social supports to the extent that an individual with a warm interpersonal style might. The IPC profiles can additionally convey the manner and motives of PTSD symptom expression. For instance, social avoidance is symptomatic of PTSD; however, the motive behind such avoidance might differ for individuals with differing interpersonal styles. Whereas a cold-dominant person with PTSD might view others as irritating and unhelpful and thus avoid interactions, a warm-submissive person with PTSD might avoid interactions out of concerns that discussing PTSD-related problems would burden others. Importantly, these patterns would be expected to hold regardless of whether an individual would be classified as having low pathology, internalizing, or externalizing PTSD using the SNAP model.
Ultimately, personality models that focus on temperament traits appear more likely to indicate the severity and type of symptoms, whereas personality models that focus on interpersonal variability appear more likely to indicate style and chronicity. Given the clinical importance of these distinctions, researchers should continue to test the complementarity of these different personality models for describing heterogeneity in PTSD as well as other forms of psychopathology.5
Limitations and Future Directions
Although the primary aim of this study was to better understand personality-PTSD relations, individuals in this sample all had comorbid diagnoses, raising potential concerns about generalizability. In a veteran sample Southwick, Yehuda, and Giller (1993) found that BPD (76%), AVPD (41%), and OCPD (44%), three of the four PDs sampled for the CLPS, had the highest rates of co-occurrence with PTSD (comorbidity with STPD was 26%). Research further suggests that the concurrent comorbidity of PTSD with MDD is approximately 50% in treatment-seeking individuals (Brady & Clary, 2003). Likewise, Kessler, Sonnega, Bromet, Hughes, and Nelson (1995) found 50% comorbidity between lifetime PTSD and MDD. Rates of co-occurrence between PTSD and these disorders in the CLPS sample showed a relatively similar distribution, except that rates of co-occurring depression were somewhat higher in CLPS: MDD (80%), BPD (61%), AVPD (56%), STPD (19%), and OCPD (36%). Thus, that individuals were selected into CLPS for the presence of other disorders does not necessarily indicate that results from this sample would not generalize to other PTSD samples, although PTSD in this sample is likely relatively severe given that it necessarily co-occurs with at least one other psychiatric disorder. Furthermore, the relatively high rates of comorbidity between PTSD and depression in this sample may have increased the number of individuals who were classified as “internalizing” in the SNAP model relative to what would be expected in a purer PTSD sample. Given that an IPC typology of heterogeneity in PTSD has not previously been identified, research on its generalizability using different kinds of samples and methods would increase confidence in the current findings.
We lacked sufficiently specific data to evaluate trauma with the same scrutiny as personality. It is likely that whereas some individuals in the sample received a PTSD diagnosis based on an isolated trauma, others developed PTSD following more chronic, severe, or complex traumata. Further, given the polythetic nature of the DSM–IV PTSD diagnosis, it is possible that groups within each typology could have consisted of individuals with different symptoms profiles (e.g., perhaps more individuals in the cold-submissive IPC group endorsed avoiding others that remind them of the trauma). Unfortunately, no indicator was available in the CLPS data to examine PTSD symptom severity across groups within each typology.
There were also limitations to other study measures. First, all personality measures were self-report, and thus important aspects of personality may not have been captured. Additionally, we used a relatively novel measure of the IPC. Although this measure demonstrated excellent circumplex fit, some of its scales had relatively low internal consistency values. Overall, however, the IPC typology was highly consistent with typological research with other disorders in suggesting a general tendency for groups of individuals with PTSD to array around the IPC (e.g., Ambwani & Hopwood, 2009; Cain et al., 2012; Kachin et al., 2001; Przeworski et al., 2011; Salzer et al., 2008; Wright et al., 2013). It would be useful to examine the degree to which our findings are consistent with research using different IPC-based measures, such as those measuring interpersonal problems, sensitivities, and values.
Conclusion
Whereas previous typological research in PTSD shows that clinical diagnoses can be informed by drawing upon models of personality, the present study demonstrates that it may be useful to assess distinct models of personality for predicting important clinical issues such as comorbid psychopathology and prognosis. Ultimately, this research highlights that constructs broadly falling within the domain of personality may have different meanings for psychopathology and different capacities to indicate factors such as risk, scar, severity, comorbidity, course, and heterogeneity. Personality is inherently intertwined with the measures used to assess it, and these measures are influenced heavily by their underlying theoretical models. The present study demonstrates that measures based on personality theories emphasizing temperament and interpersonal traits provide nonredundant and clinically important information regarding heterogeneity among individuals with PTSD. Future research and practice should consider carefully the potential utility of conceptualizing distinct aspects of personality in clinical assessment.
Acknowledgments
This research was supported by National Institute of Mental Health Grants MH 50837, 50838, 50839, 50840, 50850, and 01654 awarded to Thomas H. McGlashan. This publication has been reviewed and approved by the Publications Committee of the Collaborative Longitudinal Personality Disorders Study. We thank Alytia A. Levendosky for her support and guidance throughout this study.
Footnotes
NEM, PEM, and CON are the explicit higher-order factors of the MPQ; the SNAP is hierarchically organized around Negative Temperament (NEM), Positive Temperament (PEM), and Disinhibition (reverse CON); the MMPI PSY-5 scales include five traits, three of which correspond to NEM, PEM, and CON (Trull, Useda, Costa, & McCrae, 1995).
Forbes et al. (2010) and Wolf et al. (2012) also employed LPA in their studies, while the remainder of studies used cluster analysis.
We refer to the three higher-order SNAP dimensions as NEM, PEM, and CON throughout this article in order to maintain consistency with our broader discussion that these dimensions comprise a temperament model of personality.
The term “low pathology” was adopted to maintain consistency with Miller’s (2003) terminology. However, given that all participants had at least two clinical diagnoses (PTSD and either MDD or a PD), this term is relative.
We speculated that the FFM, a comprehensive model that incorporates both temperament and interpersonal dimensions, might be able to effectively classify individuals with respect to diathetic as well as pathoplastic features. Given that FFM data were available for participants in our sample, we tested the ability of the NEO-PI-R domains to recover similar groups as those identified by the SNAP and IPC models within a single typology. Using the procedures outlined above, LPA results for the FFM variables indicated a high degree of classification uncertainty, suggesting an inability of profiles based on the FFM factors to distinguish individuals in our sample into clearly distinct groups. Model fit statistics suggested either a two (BICΔ) or a three (AICΔ) profile solution; neither solution was tenable based on entropy values (.61 and .60), which were well below the suggested cut-off of .80. Although these solutions are not interpretable given the low entropy values, an examination of the two and three profile solutions indicated an adaptive (low neuroticism, high extraversion and conscientiousness) and a maladaptive (high neuroticism, low extraversion and conscientiousness) group for the two profile solution, with an undifferentiated (no significant differences across traits) group emerging from the other two in the three profile solution. We interpret these results as indicating the usefulness of separating temperament and interpersonal traits when examining the role of personality in PTSD. Interpersonal models that meaningfully explain personality heterogeneity within a diagnosis are less likely to emerge in models with strong direct relations to psychopathology such as the “Big Three” or the FFM, even if those models capture interpersonal variance. Results from FFM analyses are available from Katherine M. Thomas upon request.
Contributor Information
Katherine M. Thomas, Department of Psychology, Michigan State University
Christopher J. Hopwood, Department of Psychology, Michigan State University
M. Brent Donnellan, Department of Psychology, Michigan State University.
Charles A. Sanislow, Department of Psychology, Wesleyan University
Emily B. Ansell, Department of Psychiatry, Yale University School of Medicine
Carlos M. Grilo, Department of Psychiatry, Yale University School of Medicine
Thomas H. McGlashan, Department of Psychiatry, Yale University School of Medicine
John C. Markowitz, New York State Psychiatric Institute, New York, New York, and College of Physicians and Surgeons, Columbia University
Mary C. Zanarini, Department of Psychiatry, McLean Hospital, Belmont, Massachusetts, and Department of Psychiatry, Harvard Medical School
Aidan G. C. Wright, Department of Psychology, University of Pittsburgh
Meghan E. McDevitt-Murphy, Department of Psychology, University of Memphis
M. Tracie Shea, PTSD Clinic, Department of Veterans Affairs, Providence, Rhode Island and Warren Alpert School of Medicine, Brown University.
Andrew E. Skodol, College of Medicine, University of Arizona, and The Sunbelt Collaborative, Tucson, Arizona
Leslie C. Morey, Department of Psychology, Texas A&M University
References
- Ambwani S, Hopwood CJ. The utility of considering interpersonal problems in the assessment of bulimic features. Eating Behaviors. 2009;10:247–253. doi: 10.1016/j.eatbeh.2009.07.007. doi:10.1016/j.eatbeh.2009.07.007. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Anchin JC, Pincus AL. Evidence-based interpersonal psychotherapy with personality disorders: Theory, components, and strategies. In: Magnavita JJ, editor. Evidence-based treatment of personality dysfunction: Principles, methods, and processes. American Psychological Association; Washington, DC: 2010. pp. 113–166. [Google Scholar]
- Barrett MS, Barber JP. Interpersonal profiles in major depressive disorder. Journal of Clinical Psychology. 2007;63:247–266. doi: 10.1002/jclp.20346. doi: 10.1002/jclp.20346. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. doi:10.1037/0022-006X.70.2.288. [PubMed] [Google Scholar]
- Brady KT, Clary CM. Affective and anxiety comorbidity in post-traumatic stress disorder treatment trials of sertraline. Comprehensive Psychiatry. 2003;44:360–369. doi: 10.1016/S0010-440X(03)00111-1. doi:10.1016/S0010-440X(03)00111-1. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Multimodal inference: understanding AIC and BIC in model selection. Sociological Methods & Research. 2004;33:261–304. doi:10.1177/0049124104268644. [Google Scholar]
- Cain NM, Ansell EB, Wright AGC, Hopwood CJ, Thomas KM, Pinto A, Grilo CM. Interpersonal pathoplasticity in the course of major depression. Journal of Consulting and Clinical Psychology. 2012;80:78–86. doi: 10.1037/a0026433. doi:10.1037/a0026433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA. Schedule for Nonadaptive and Adaptive Personality: Manual for administration, scoring and interpretation. University of Minnesota Press; Minneapolis, MN: 1993. [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clark S, Muthén B. Relating latent class analysis results to variables not included in the analysis. 2012 Manuscript submitted for publication. Retrieved from www.statmodel.com.
- Costa PT, McCrea RR. NEO Five-Factor Inventory. Psychological Assessment Resources; Lutz, FL: 1992. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM–IV Axis I Disorders, Patient Editions (SCID-P) New York State Psychiatric Institute, Biometrics Research; New York, NY: 1996. [Google Scholar]
- Flood AM, Boyle SH, Calhoun PS, Dennis MF, Barefoot JC, Moore SD, Beckham JC. Prospective study of externalizing and internalizing subtypes of posttraumatic stress disorder and their relationship to mortality among Vietnam veterans. Comprehensive Psychiatry. 2010;51:236–242. doi: 10.1016/j.comppsych.2009.08.002. doi:10.1016/j.comppsych.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes D, Elhai JD, Miller MW, Creamer M. Internalizing and externalizing classes in posttraumatic stress disorder: A latent class analysis. Journal of Traumatic Stress. 2010;23:340–349. doi: 10.1002/jts.20526. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Shea MT, Skodol AE, McGlashan TH, Morey LC, Stout RL, Keller MB. The collaborative longitudinal personality disorders study: Development, aims, design and sample characteristics. Journal of Personality Disorders. 2000;14:300–315. doi: 10.1521/pedi.2000.14.4.300. doi:10.1521/pedi.2000.14.4.300. [DOI] [PubMed] [Google Scholar]
- Gurtman MB, Balakrishnan JD. Circular measurement redux: The analysis and interpretation of interpersonal circle profiles. Clinical Psychology: Science and Practice. 1998;5:344–360. doi:10.1111/j.1468-2850.1998.tb00154.x. [Google Scholar]
- Harkness AR, McNulty JL, Ben-Porath YS. The Personality Psychopathology Five (PSY-5): Constructs and MMPI–2 Scales. Psychological Assessment. 1995;7:104–114. doi:10.1037/1040-3590.7.1.104. [Google Scholar]
- Hopwood CJ, Morey LC. Psychological conflict in borderline personality as represented by inconsistent self-report item responding. Journal of Social and Clinical Psychology. 2007;26:1065–1075. doi: 10.1521/jscp.2007.26.9.1065. [Google Scholar]
- Horowitz LM, Rosenberg SE, Bartholomew K. Interpersonal problems, attachment styles, and outcome in brief dynamic psychotherapy. Journal of Consulting and Clinical Psychology. 1993;61:549–560. doi: 10.1037//0022-006x.61.4.549. doi:10.1037/0022-006X.61.4.549. [DOI] [PubMed] [Google Scholar]
- Hubert L, Arabie P. Comparing partitions. Journal of Classification. 1985;2:193–218. doi:10.1007/BF01908075. [Google Scholar]
- Kachin KE, Newman MG, Pincus AL. An interpersonal problem approach to the division of social phobia subtypes. Behavior Therapy. 2001;32:479–501. doi:10.1016/S0005-7894(01)80032-0. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nelson E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-Up Evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. doi:10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. doi:10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kiesler DJ. Contemporary interpersonal theory and research: Personality, psychopathology, and psychotherapy. Wiley; Oxford, England: 1996. [Google Scholar]
- Klein MH, Wonderlich S, Shea MT. Models of relationships between personality and depression: Toward a framework for theory and research. In: Klein MH, Kupfer DJ, Shea MT, editors. Personality and depression. Guilford Press; New York, NY: 1993. pp. 1–54. [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. doi:10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Leary T. Interpersonal diagnosis of personality. Ronald Press; New York, NY: 1957. [Google Scholar]
- Markowitz JC, Milrod B, Bleiberg KL, Marshall RD. Interpersonal factors in understanding and treating posttraumatic stress disorder. Journal of Psychiatric Practice. 2009;15:133–140. doi: 10.1097/01.pra.0000348366.34419.28. doi:10.1097/01.pra.0000348366.34419.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae RR, Costa PT. The structure of interpersonal traits: Wiggins’s circumplex and the five-factor model. Journal of Personality and Social Psychology. 1989;56:586–595. doi: 10.1037//0022-3514.56.4.586. doi:10.1037/0022-3514.56.4.586. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Shea MT, Yen S, Grilo CM, Sanislow CA, Markowitz JC, Skodol AE. Prospective investigation of a PTSD personality typology among individuals with personality disorders. Comprehensive Psychiatry. 2012;53:441–450. doi: 10.1016/j.comppsych.2011.07.002. doi:10.1016/j.comppsych.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlashan TH, Grilo CM, Skodal AE, Gunderson JG, Shea MT, Morey LC, Stout RL. The collaborative longitudinal personality disorders study: Baseline Axis I/II and II/II diagnostic co-occurrence. Acta Psychiatrica Scandinavica. 2000;102:256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. doi:10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- Miller MW. Personality and the etiology and expression of PTSD: A three-factor model perspective. Clinical Psychology: Science and Practice. 2003;10:373–393. doi:10.1093/clipsy.bpg040. [Google Scholar]
- Miller MW, Greif JL, Smith AA. Multidimensional personality questionnaire profiles of veterans with traumatic combat exposure: Externalizing and internalizing subtypes. Psychological Assessment. 2003;15:205–215. doi: 10.1037/1040-3590.15.2.205. doi:10.1037/1040-3590.15.2.205. [DOI] [PubMed] [Google Scholar]
- Miller MW, Kaloupek DG, Dillon AL, Keane TM. Externalizing and internalizing subtypes of combat-related PTSD: A replication and extension using the PSY-5 scales. Journal of Abnormal Psychology. 2004;113:636–645. doi: 10.1037/0021-843X.113.4.636. doi:10.1037/0021-843X.113.4.636. [DOI] [PubMed] [Google Scholar]
- Miller MW, Resick PA. Internalizing and externalizing subtypes in female sexual assault survivors: Implications for the understanding of complex PTSD. Behavior Therapy. 2007;38:58–71. doi: 10.1016/j.beth.2006.04.003. doi:10.1016/j.beth.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey LC, Blashfield RK, Skinner HA. A comparison of cluster analysis techniques within a sequential validation framework. Multivariate Behavioral Research. 1983;18:309–329. doi: 10.1207/s15327906mbr1803_4. doi:10.1207/s15327906mbr1803_4. [DOI] [PubMed] [Google Scholar]
- Morey LC, Hopwood CJ, Gunderson JG, Skodol AE, Shea MT, Yen S, McGlashan TH. Comparison of alternative models for personality disorders. Psychological Medicine. 2007;37:983–994. doi: 10.1017/S0033291706009482. doi:10.1017/S0033291706009482. [DOI] [PubMed] [Google Scholar]
- Morey LC, Warner MB, Shea TM, Gunderson JG, Sanislow CA, Grilo AE, McGlashan TH. The representation of four personality disorders by the Schedule for Nonadaptive and Adaptive Personality dimensional model of personality. Psychological Assessment. 2003;15:326–332. doi: 10.1037/1040-3590.15.3.326. doi:10.1037/1040-3590.15.3.326. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Muthén and Muthén; Los Angeles, CA: 2010. Version 6.1. [Google Scholar]
- Pincus AL, Lukowitsky MR, Wright AGC. The interpersonal nexus of personality and psychopathology. In: Millon T, Kreuger R, Simonsen E, editors. Contemporary directions in psychopathology: Toward DSM–V and ICD-11. Guilford Press; New York, NY: 2010. pp. 523–552. [Google Scholar]
- Przeworski A, Newman MG, Pincus AL, Kasoff MB, Yamasaki AS, Castonguay LG, Berlin KS. Interpersonal pathoplasticity in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. 2011;120:286–298. doi: 10.1037/a0023334. doi:10.1037/a0023334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, Evans DE. Temperament and personality: Origins and outcomes. Journal of Personality and Social Psychology. 2000;78:122–135. doi: 10.1037//0022-3514.78.1.122. doi:10.1037/0022-3514.78.1.122. [DOI] [PubMed] [Google Scholar]
- Salzer S, Pincus AL, Hoyer J, Kreische R, Leichsenring F, Leibing E. Interpersonal subtypes within generalized anxiety disorder. Journal of Personality Assessment. 2008;90:292–299. doi: 10.1080/00223890701885076. doi:10.1080/00223890701885076. [DOI] [PubMed] [Google Scholar]
- Sellbom M, Bagby RM. Identifying PTSD personality subtypes in a workplace trauma sample. Journal of Traumatic Stress. 2009;22:471–475. doi: 10.1002/jts.20452. doi:10.1002/jts.20452. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Yehuda R, Giller EL., Jr. Personality disorders in treatment-seeking combat veterans with posttraumatic stress disorder. The American Journal of Psychiatry. 1993;150:1020–1023. doi: 10.1176/ajp.150.7.1020. [DOI] [PubMed] [Google Scholar]
- Tellegen A, Waller NG. Exploring personality through test construction: Development of the Multidimensional Personality Questionnaire. In: Boyle GJ, Matthews G, Saklofske DH, editors. The Sage handbook of personality theory and assessment: Vol. 2. Personality measurement and testing. Sage; Thousand Oaks, CA: 2008. pp. 261–292. [Google Scholar]
- Tracey TJ. RANDALL: A Microsoft FORTRAN program for a randomization test of hypothesized order relations. Educational and Psychological Measurement. 1997;57:164–168. doi:10.1177/0013164497057001012. [Google Scholar]
- Traupman EK, Smith TW, Uchino BN, Berg CA, Trobst KK, Costa PT. Interpersonal circumplex octant, control, and affiliation scales for the NEO-PI-R. Personality and Individual Differences. 2009;47:457–463. doi: 10.1016/j.paid.2009.04.018. doi:10.1016/j.paid.2009.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trobst KK. An interpersonal conceptualization and quantification of social support transactions. Personality and Social Psychology Bulletin. 2000;26:971–986. doi:10.1177/01461672002610007. [Google Scholar]
- Trull TJ, Useda JD, Costa PT, Jr., McCrae RR. Comparison of the MMPI-2 Personality Psychopathology Five (PSY-5), the NEO-PI, and the NEO-PI–R. Psychological Assessment. 1995;7:508–516. doi:10.1037/1040-3590.7.4.508. [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study: An ongoing inter-rater reliability monitoring program using the Longitudinal Interval Follow-Up Evaluation. Journal of Psychiatric Research. 2001;35:297–305. doi: 10.1016/s0022-3956(01)00030-9. doi:10.1016/S0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Smith GT. Personality and psychopathology. In: John OP, Robins RW, Pervin LA, editors. Handbook of personality theory and research. 3rd ed. Guilford Press; New York, NY: 2008. pp. 743–769. [Google Scholar]
- Wiggins JS. An informal history of the interpersonal circumplex tradition. Journal of Personality Assessment. 1996;66:217–233. doi: 10.1207/s15327752jpa6602_2. doi:10.1207/s15327752jpa6602_2. [DOI] [PubMed] [Google Scholar]
- Wiggins JS, Pincus AL. Conceptions of personality disorders and dimensions of personality. Psychological Assessment. 1989;1:305–316. doi:10.1037/1040-3590.1.4.305. [Google Scholar]
- Wolf EJ, Miller MW, Harrington KM, Reardon A. Personality-based latent classes of posttraumatic psychopathology: Personality disorders and the internalizing/externalizing model. Journal of Abnormal Psychology. 2012;121:256–262. doi: 10.1037/a0023237. doi:10.1037/a0023237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Krueger RF, Lyons MJ, Tsuang MT, Koenen KC. Posttraumatic stress disorder and the genetic structure of comorbidity. Journal of Abnormal Psychology. 2010;119:320–330. doi: 10.1037/a0019035. doi:10.1037/a0019035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Hallquist MN, Morse JQ, Scott LN, Stepp SD, Nolf KA, Pilkonis PA. Clarifying interpersonal heterogeneity in borderline personality disorder using latent mixture modeling. Journal of Personality Disorders. 2013;27:125–143. doi: 10.1521/pedi.2013.27.2.125. doi:10.1521/pedi.2013.27.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Conroy DE, Elliot AJ. The pathoplastic relationship between interpersonal problems and fear of failure. Journal of Personality. 2009;77:997–1024. doi: 10.1111/j.1467-6494.2009.00572.x. doi:10.1111/j.1467-6494.2009.00572.x. [DOI] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Conroy DE, Hilsenroth MJ. Integrating methods to optimize circumplex description and comparison of groups. Journal of Personality Assessment. 2009;91:311–322. doi: 10.1080/00223890902935696. doi:10.1080/00223890902935696. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg RF, Sickel AE, Yong L. The Diagnostic Interview for DSM–IV Personality Disorders (DIPD-IV) McLean Hospital; Belmont, MA: 1996. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Gunderson JG. The collaborative longitudinal personality disorders study: Reliability of axis I and axis II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]