Abstract
Background and objective
Used as an integrated tool, mHealth may improve the ability of healthcare providers in rural areas to provide care, improve access to care for underserved populations, and improve biophysical outcomes of care for persons with diabetes in rural, underserved populations. Our objective in this paper is to present an integrated review of the impact of mHealth interventions for community dwelling individuals with type two diabetes.
Materials and methods
A literature search was performed using keywords in PubMed to identify research studies which mHealth technology was used as the intervention
Results and discussion
Interventions using mHealth have been found to improve outcomes, be cost effective, and culturally relevant. mHealth technology that has been used to improve outcomes include: seeking out health information via the web, access to appointment scheduling and medication refills, secure messaging, computerized interventions to manage a chronic condition, use of a personal health record, use of remote monitoring devices, and seeking support from others with similar health concerns through social networks.
Conclusion
Using the validated Chronic Care Model to translate what is known about mHealth technology to clinical practice has the potential to improve the ability of healthcare providers in rural areas to provide care, improve access to care for underserved populations, and improve biophysical outcomes of care for persons with diabetes in rural underserved populations. While these approaches were effective in improving some outcomes, they have not resulted in the establishment of the necessary electronic infrastructure for a sustainable mobile healthcare delivery model.
Keywords: mHealth, Rural, Diabetes, Chronic Care model
Mobile health (mHealth) is an emerging field that has been defined as “medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants, and other wireless devices” (Istepanian, Laxminarayan, & Pattichis, & 2006). In the United States, there is widespread use of mobile devices and access to broadband internet service is improving (Smith, 2010). Applications using mHealth devices are being developed to improve and augment the care of type 2 diabetes patients in the community (Katz R, 2012). However, careful attention to existing healthcare delivery structures must be considered during development of mHealth applications. Use of the validated Chronic Care Model will assist in successful and sustainable implementation of mHealth as a treatment option.
Background & Significance
Rural populations with low socioeconomic status are at higher risk of poor diabetes control, decreased self-management, and development of complications (Utz, 2008). There are 62 million Americans currently residing in rural areas (DeNavas-Walt, Proctor, & Smith, 2011) and it is estimated that 20 percent of this rural population is uninsured. Even with healthcare reform, this number is projected to increase to 25 percent by 2019 (Garrett, Loan, Headen, & Holahan, 2010). In the United States, diabetes is most prevalent in the rural southeastern region (Barker, Kirtland, Gregg, Geiss, & Thompson, 2011). Nearly 12 percent of people in this region have diabetes compared to 8.5 percent in the remainder of the country.
Due to a lack of primary care providers in rural, underserved areas, there is a critical need for development and effectiveness testing of novel interventions that could improve health outcomes such as: effective patient–provider communication, adherence to treatment, self-management ability, and biophysical outcomes. Achieving these improved outcomes must be done while allowing primary care providers to deliver culturally acceptable interventions that optimize time-efficiency and affordability (Barker et al., 2011). The ability of such interventions to improve care and reduce strain on rural healthcare practices will depend on the effective use of technology (Effken & Abbott, 2009).
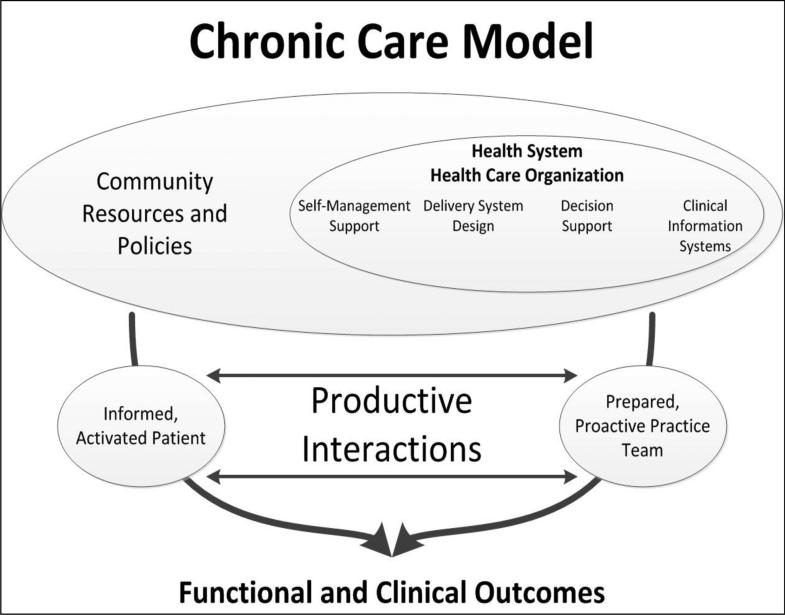
Our objective in this paper is to present an integrated review of the impact of mHealth interventions for community dwelling individuals with type 2 diabetes. The review structure is based on the Chronic Care Model and a model of evidence-based healthcare delivery is proposed. Structuring what we know about mHealth technology using the concepts of the model adds clarity to the literature review and assists with translation to clinical practice. The Chronic Care Model has been used in clinical practice for over 12 years and is designed to assist healthcare practices to improve patient health outcomes by changing the routine delivery of care.
This is done through six interrelated system changes meant to make patient-centered, evidence-based care easier to accomplish (Roger et al., 2012). The major concepts in the model are the health system, community support, self-management support, decision support, clinical information systems, and delivery system design (Pullicino et al., 2011). A prepared healthcare team delivering planned interactions, self-management support with effective use of community resources, integrated decision support, and supportive information technology (IT) are designed to work together to strengthen the provider-patient relationship and improve health outcomes (Pullicino et al., 2011). Therefore, the literature in this article will be presented based on the major concepts of the Chronic Care Model (See figure 1).
Figure 1. The Chronic Care Model.
Edward H. Wagner, MD, MPH, Chronic Disease Management: What Will It Take To Improve Care for Chronic Illness? Effective Clinical Practice, Aug/Sept 1998, Vol 1 (Wagner, 1998). Disclaimer: The American College of Physicians is not responsible for the accuracy of the translation.
Methods
The PubMed data base was searched from late June to mid-August 2012. The following search terms were used: ‘Diabetes AND mHealth’ ‘Diabetes AND Telemedicine’ ‘mHealth AND health disparities’, ‘mHealth AND Chronic Care Model’ ‘mHealth AND Clinical Information Systems’. Limits were set for articles that were published in the last five years, and published in the English language. The inclusion criteria were:
-
(1)
Studies which included participants with type 2 diabetes;
-
(2)
mHealth technology was used in the intervention
-
(3)
There was randomization of participants to intervention and control groups.
Literature reviews and State of the Science papers were reviewed for individual references, but not included in this review. A total of 157 articles were found. After examining the title, abstract and keywords of retrieved records, we identified 23 articles meeting the inclusion criteria. The articles were then reviewed via a matrix method and placed into categories based on the concepts of the Chronic Care Model.
Health System
Five articles were found that incorporated health system changes using mHealth interventions. Health system characteristics are traditional structure and process elements of organizations, such as size, ownership, skill mix, and technology. The health system characteristics are considered to directly affect and be affected by patient outcomes. The system characteristics mediate the relationship between patient characteristics and interventions in producing patient outcomes (Mitchell, Ferketich, & Jennings, 1998).
The system of interest to us is the rural healthcare delivery system. Compared with their urban counterparts, rural residents are more likely to be poor, be in fair or poor health, and have chronic conditions. Rural residents are less likely than their urban counterparts to receive recommended preventive services and on average report fewer visits to health care providers. Uninsured, rural adults are more likely to report the following difficulties: access to care, referrals to specialists, and timeliness of care for an illness or injury (Agency for Healthcare Research and Quality, 2008).
In recent years, the United States through the Center for Medicare and Medicaid Services (CMS) and a number of private health plans has relied on the use of technology with disease specific registries to facilitate tracking and the provision of quality care (Muntner et al., 2011). Diabetes is well suited to the use of clinical information technology and use of EMRs because its management is routinely characterized by easily quantifiable outcomes and process measures (Kleindorfer et al., 2011).
It is feasible to incorporate mHealth technologies into an existing Healthcare system (See Table 1). However, it is evident from this review that problems in mHealth technology use still exist and need consideration. Face-to-face communication, live technical support, and cost are found to affect use of mHealth tools by patients. Technical problems and difficulty of use increased the likelihood of patients stopping use of the mHealth technology and one study reported that telephone interventions were as likely to improve outcomes as mHealth interventions. Hence, developing a model of healthcare delivery using mHealth technologies must incorporate live technical support, be easy for users, include face-to-face communications, have a lower cost to patients than traditional interventions, and incorporate back-up interventions for technical issues that cannot be resolved in real time.
Table 1.
mHealth and Health Systems
| Reference | Sample Size | Purpose | Results |
|---|---|---|---|
| Rabin and Bock, 2011 | 14 | To evaluate smart phone physical activity assistants | Smart phone physical activity assistants are feasible for tracking physical activity from a distance. |
| Basoglu, Daim, and Topacan, 2012 | 22 | To evaluate the attributes and preferences of mhealth service by users | Users preferred low input effort, availability of face-to face communication, live technical support, quick response time, and low cost |
| Istepanian et al., 2009 | 137 | Bluetooth transmitted glucose readings that were viewed with a web-based application. | Attrition was higher in the intervention group due to technical problems. Those who completed the intervention group had lower A1C than those in the control group. |
| Zolfaghari, Mousavifar, and Pedram, 2009 | 77 | Compare the effectiveness of SMS texting to nurse telephone calls for follow up care | Both groups had a significant reduction in A1C and were feasible for patients. |
| Lyles et al., 2011 | 8 | Use of the web and cell phones with a case manager to provide feedback on finger sticks | Qualitative analysis shows that participants expressed frustrations with using the cell phones but liked the wireless system for collaborating with healthcare professionals and receiving automatic feedback on their blood sugar trends. |
Community Resources & Policies
The Chronic Care model recognizes the influence of community on patient outcomes (Kabagambe et al., 2011). Patients traditionally seek health information in three ways: on their own, from professionals, and from friends and family (Ahern, Woods, Lightowler, Finley, & Houston, 2011). The use of technology does not change this pattern. Due to the ubiquitous nature of mobile devices and the internet, our idea of community has expanded from the traditional definition, people living in a particular area or place, to a much boarder network of social connections. Patients seek support from others with similar health concerns or conditions through lists-serves and social networks (Fox, 2011). Social networks bring peer support directly to patients without leaving one's home (Ahern et al., 2011). Therefore, current conceptualizations of community should include the on-line community, which can be defined as a network of individuals who interact through media, crossing geographical boundaries but united by a particular topic, interest, or goal.
Patients can now access health information, healthcare clinics, and providers through internet searches, secure e-mail, messaging, online medication refills, appointment requests, and secure patient access to electronic medical records (EMR) (Halanych et al., 2011; Judd et al.; Muntner et al., 2012; Wadley et al., 2011). The internet allows patients to quickly access vast amounts of disease specific information. Enhanced understanding of how patients seek health information may improve the way healthcare systems incorporate technology into the delivery of care. While an enormous amount of information is available with the click of a button, the quality of that material varies.
In the United States, there is widespread use of mobile devices and access to broadband internet service is improving (Smith, 2010). The accessibility of 3G service is available and reliable in the most densely populated areas of the United States. However, when considering implementing mHealth interventions in a rural population, 3G service is not always reliable. Still, many of these areas have access to 1G and wired connections that could allow participation in mHealth interventions. It has been reported that even in the most rural areas of the United States, 77% of adults have a cell phone, which is only 10% less than more urban areas (Zickuhr, 2013). Six in ten adults (63%) go online wirelessly with one of these devices (Smith, 2010).
Self-management
Diabetes self-management includes mindfulness related to: eating habits, physical activity, monitoring blood glucose, medication taking, and communicating with healthcare professionals (Unverzagt et al., 2011). Evidence shows that patients who participate actively in their care achieve valuable and sustained improvement in physical and psychological well-being (Howard et al., 2011). The use of technology is making it possible to empower patients to learn new skills, enhance their self-management abilities, and structure personal care routines related to their illness (Kleindorfer et al., 2011).
Handheld devices can be used by patients and health care providers to support self-management of diabetes. Through a phone and an internet site, patients can upload information about their illness so that it can be interpreted by health care providers and patients can receive more immediate feedback. Technology allow patients to receive appointment reminders, education, and health behavior support, as well as measure glucose levels, blood pressure and weight and transmit this health information directly to data stores for clinical evaluation (Ãrsand, Tufano, Ralston, & Hjortdahl, 2008; Cho, Lee, Lim, Kwon, & Yoon, 2009; Cox et al., 2011; Earle, Istepanian, Zitouni, Sungoor, & Tang, 2010; Faridi et al., 2008; Jae-Hyoung, Hye-Chung, Dong-Jun, Hyuk-Sang, & Kun-Ho, 2009; Logan et al., 2007; Quinn et al., 2009; Soliman et al., 2011; Turner, Larsen, Tarassenko, Neil, & Farmer, 2009; Yoo et al., 2009; Zweifler et al., 2011).
Not only have patients found that the use of mHealth tools are feasible and culturally acceptable, but as shown in table 2 there have been improved outcomes for diabetes patients include improved A1C, decreased blood pressure, improved cholesterol levels, improved adiponectin levels, stable C-reactive protein and stable interleukin-6 levels (Ãrsand et al., 2008; Cho et al., 2009; Cox et al., 2011; Earle et al., 2010; Faridi et al., 2008; Jae-Hyoung et al., 2009; Logan et al., 2007; Quinn et al., 2009; Soliman et al., 2011; Turner et al., 2009; Yoo et al., 2009; Zweifler et al., 2011).
Table 2.
Self-Management of Diabetes via mHealth Technologies.
| Reference | Sample Size (N) | Length of Study | Intervention description | Outcome |
|---|---|---|---|---|
| Yoo et al., 2009 | 123 | 3 Months | Text messages with Bluetooth glucose monitoring & exercise monitoring. Feedback provided immediately based on algorithms. | Improved A1C & BP, Cholesterol. Decreased adiponectin levels in intervention group. C-reactive protein and interleukin-6 levels remained the same in both groups. |
| Faridi et al., 2008 | 30 | 3 Months | Impact on clinical outcomes using tailored daily messages via cell phone | Improved A1C and self-efficacy scores for intervention. Technology was not user friendly. |
| Jae-Hyoung et al., 2009 | 69 | 3 Months intervention | Glucose-monitoring data were automatically transferred to their EMR and they received medical recommendations by short text message. | Significant decrease in A1C levels. |
| Quinn et al., 2009 | 30 | 3 Months | Mobile phone application wirelessly obtained from the glucometer and transmitted glucose readings to automated database with real-time feedback and lifestyle recommendations | Significant decrease in A1C levels. |
| Turner et al., 2009 | 23 | 3 Months | Mobile phone wirelessly obtained and transmitted glucose readings; real-time feedback of input and semi-automated messages for self-management | Significant decrease in A1C levels. |
| Logan et al., 2007 | 33 | 4 Months | Bluetooth enabled BP cuffs and mobile phones were provided to patients in order to transmit data to a central server for data processing then fax was used to send reports to physicians. | BP decreased significantly. Patients perceived the system as acceptable and effective. |
| Earle et al., 2010 | 137 | 6 months | Patients used adapted sensors via BP cuffs and mobile phone to transmit weekly BP readings and received real time feedback using a web-based application | BP decreased significantly. Those with the most decreased BP also had decreased glucose levels. |
| Zweifler et al., 2011 | 51 | 6 months | Text messages sent by providers based on review of data provided by patient via internet. | Significant decrease in A1C levels. |
| Soliman et al., 2011 | 43 | 6 months | PDA recording of blood glucose, medications, meals, exercise, etc., with summary output | Significant decrease in A1C levels. |
| Cox et al., 2011 | 40 | 3 months | Customized schedule for SMS reminders to obtain blood glucose readings. Reading submitted via SMS resulted in positive feedback if in range, and instructions if out of range | Significant decrease in A1C levels. |
| Cho et al., 2009 | 69 | 3 Months | Combination mobile phone and glucometer transmitting glucose reading to provider who sent treatment adjustments via SMS | Significant decrease in A1C levels. |
Decision Support
Decision support is defined as embedding evidence-based guidelines into daily clinical practice and integrating the expertise of specialists into primary care practices (Kabagambe et al., 2011). A typical way of interacting with specialists is for primary care practices to send patients to specialist visits and hope to get a letter back in return. Through the use of technology, we can get beyond traditional referral letters to real-time consultation and exchanges with patients and providers in different locations. Primary care providers, specialists, care teams, and individual patients can benefit from problem or case-based learning, collaborating across geographical boundaries through the use of chat, voice, and video communications (Basoglu et al., 2012; Istepanian et al., 2009; Lyles et al., 2011; Rabin & Bock, 2011; Zolfaghari et al., 2009). These technologies will allow providers to jointly inform patients about guidelines and information pertinent to their care without lengthy waits between primary care visits and specialist appointments. This shift in the delivery of care allows for shared decision making and education between patients and the care team (Pullicino et al., 2011). This type of decision support will take a drastic change in the healthcare system. While mHealth tools have the potential to change practice, the authors could not find articles related to community dwelling type 2 diabetes patients and use of imbedded decision support.
Clinical Information Systems
Clinical information systems are used to collect, integrate and distribute information within the context of a healthcare setting (Pullicino et al., 2011). The extent to which these resources and services are available varies widely. While rural healthcare clinics are often the last to adopt such practice changes due to cost, there are several free Electronic Medical Record programs that can be incorporated into non-profit and free clinic settings. Integration of secure messaging, e-visits, home monitoring with feedback, health-risk appraisal with feedback, medication refills, tailored interventions, social network services, and links to community programs is now possible (Ahern et al., 2011). A delivery system redesign is needed to develop patient-centered clinical information systems. These information systems can be incorporated, with little cost, into free clinic settings.
Delivery Redesign
Living in rural areas presents multiple barriers, one of which is limited access to care due to distance (Arcury, Preisser, Gesler, & Powers, 2005). Rural populations with low socioeconomic status have poor outcomes and the lack of primary care providers in rural, underserved areas demands a shift in healthcare practices. Through the widely validated Chronic Care Model, it is possible to deliver care to patients in their homes in remote underserved areas. Bluetooth enabled devices and the use of chat, voice, and video communications allows the healthcare team to provide many of the elements of a traditional office visit. A delivery system redesign is needed to develop patient-centered clinical information systems within the rural health care clinic setting. The use of innovative technology affords a low-cost, flexible means to supplement formal healthcare and is central in reshaping the care of rural populations. Developing a model of healthcare delivery using mHealth technologies should incorporate live technical support, be easy for users, include face-to-face communications, have a lower cost to patients and practices than traditional interventions and incorporate back-up interventions for technical issues that cannot be resolved. Provider approved educational content, social networking and access to EMR is still needed within the context of the healthcare system redesign (See figure 2).
Figure 2.
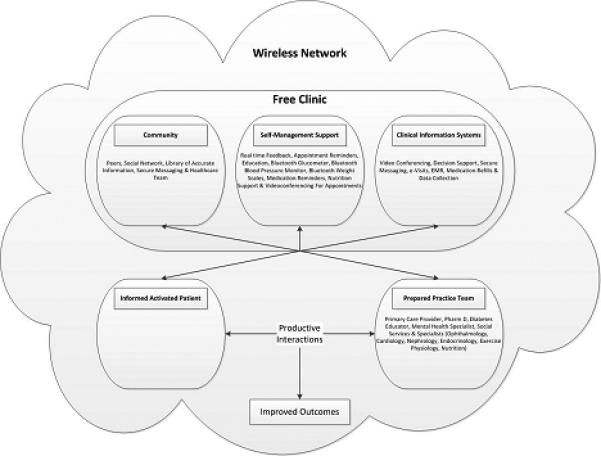
Conceptulization of mHealth using the Chronic Care Model.
Discussion
Individuals with low socioeconomic status living in rural parts of the U.S. suffer disproportionately from poor health status, health disparities, and problems in accessing healthcare. The current rural healthcare system places the burden of caring for diabetes on patients and families who have very few resources. The cost of travel due to long distances between rural healthcare clinics and patients’ homes frequently prevents patients from seeking needed healthcare. Mobile technologies are a promising approach to solving health disparities.
Used as an integrated tool and based on sound practice models such as the Chronic Care Model, mHealth may improve: the ability of healthcare providers in rural areas to provide care, access to care for underserved populations, and biophysical outcomes of care. Althoughindividual interventions to impact outcomes for Diabetes patients using technology have been studied, no approach to date has used an integrated system of mHealth tools to deliver healthcare at a distance within existing rural health clinics. Individual mHealth interventions have been found to improve outcomes, be cost effective, and culturally relevant. Examples of how technology has been used to improve outcomes include: patients seeking out health information via the web, access to services such as appointment scheduling and medication refills, communication with providers via secure messaging, engaging with computerized interventions to manage a chronic condition, use of a health record to store personal health information, use of remote monitoring devices such as blood pressure monitors, glucometers, and scales, and seeking support from others with similar health concerns or conditions through social networks.
Conclusion
Using the validated Chronic Care Model to translate what is known about mHealth technology to clinical practice will assist in developing a model of healthcare delivery using mHealth technologies that is usable and meaningful to both patients and rural healthcare providers. A delivery system redesign using mHealth technology must incorporate live technical support, be easy for users, include face-to-face communications, have a lower cost to patients and rural providers than traditional interventions, and incorporate back-up interventions for technical issues that cannot be resolved in real time. This article supports ongoing research and implementation of a substantive departure from the status quo. Namely, the approach of integrating multiple mHealth tools into an existing rural health clinic to go beyond traditional office visits and shifting to real-time exchanges between patients and providers across geographical boundaries.
Acknowledgments
Funding Agencies
This project is supported by the WVCTSI through the National Institute of General Medical NIH/NIGMS Award Number U54GM104942
References
- Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP) 2008 http://www.hcup-us.ahrq.gov/toolssoftware/icd_10/ccs_icd_10.jsp. [PubMed]
- Ahern DK, Woods SS, Lightowler MC, Finley SW, Houston TK. Promise of and potential for patient-facing technologies to enable meaningful use. American Journal of Preventive Medicine. 2011;40(5, Supplement 2):S162–S172. doi: 10.1016/j.amepre.2011.01.005. http://dx.doi.org/10.1016/j.amepre.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Arcury TA, Preisser JS, Gesler WM, Powers JM. Access to transportation and health care utilization in a rural region. Journal of Rural Health. 2005;21(1):31–38. doi: 10.1111/j.1748-0361.2005.tb00059.x. MEDLINE. [DOI] [PubMed] [Google Scholar]
- Ãrsand E, Tufano JT, Ralston JD, Hjortdahl P. Designing mobile dietary management support technologies for people with diabetes. Journal of Telemedicine & Telecare. 2008;14(7):329–332. doi: 10.1258/jtt.2008.007001. http://dx.doi.org/10.1258/jtt.2008.007001. [DOI] [PubMed] [Google Scholar]
- Barker LE, Kirtland KA, Gregg EW, Geiss LS, Thompson TJ. Geographic distribution of diagnosed diabetes in the U.S.: A diabetes belt. American Journal of Preventive Medicine. 2011;40(4):434–439. doi: 10.1016/j.amepre.2010.12.019. http://dx.doi.org/10.1016/j.amepre.2010.12.019. [DOI] [PubMed] [Google Scholar]
- Basoglu N, Daim T, Topacan U. Determining patient preferences for remote monitoring. Journal of Medical Systems. 2012;36(3):1389–1401. doi: 10.1007/s10916-010-9601-1. [DOI] [PubMed] [Google Scholar]
- Cho JH, Lee HC, Lim DJ, Kwon HS, Yoon KH. Mobile communication using a mobile phone with a glucometer for glucose control in Type 2 patients with diabetes: As effective as an Internet-based glucose monitoring system. Journal of Telemedicine and Telecare. 2009;15(2):77–82. doi: 10.1258/jtt.2008.080412. http://dx.doi.org/10.1258/jtt.2008.080412. [DOI] [PubMed] [Google Scholar]
- Cox TL, Ard JD, Beasley TM, Fernandez JR, Howard VJ, Affuso O. Body image as a mediator of the relationship between body mass index and weight-related quality of life in black women. Journal of Womens Health (Larchmt) 2011;20(10):1573–1578. doi: 10.1089/jwh.2010.2637. http://dx.doi.org/10.1089/jwh.2010.2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. U.S. Census Bureau, Current Population Reports. U.S. Government Printing Office; Washington, DC.: 2011. Income, poverty, and health insurance Coverage in the United States: 2010. pp. 60–239. [Google Scholar]
- Earle KA, Istepanian RSH, Zitouni K, Sungoor A, Tang B. Mobile telemonitoring for achieving tighter targets of blood pressure control in patients with complicated Diabetes: A pilot study. Diabetes Technology & Therapeutics. 2010;12(7):575–579. doi: 10.1089/dia.2009.0090. http://dx.doi.org/10.1089/dia.2009.0090. [DOI] [PubMed] [Google Scholar]
- Effken JA, Abbott PA. Health IT-enabled care for underserved rural populations: The role of nursing. Journal of the American Medical Informatics Association [JAMIA] 2009;16(4):439–445. doi: 10.1197/jamia.M2971. http://dx.doi.org/10.1197/jamia.M2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz DL. Evaluating the impact of mobile telephone technology on type 2 diabetic patients' self-management: The NICHE pilot study. Journal of Evaluation In Clinical Practice. 2008;14(3):465–469. doi: 10.1111/j.1365-2753.2007.00881.x. http://dx.doi.org/10.1111/j.1365-2753.2007.00881.x. [DOI] [PubMed] [Google Scholar]
- Fox S. The social life of health information. 2011 Retrieved from http://www.pewinternet.org/Reports/2011/Social-Life-of-Health-Info.aspx.
- Garrett AB, Loan L, Headen I, Holahan J. The cost of failure to enact health reform: Implications for states. Robert Wood Johnosn Foundation; RWJF: 2010. [Google Scholar]
- Halanych JH, Shuaib F, Parmar G, Tanikella R, Howard VJ, Roth DL, Safford MM. Agreement on cause of death between proxies, death certificates, and clinician adjudicators in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. American Journal of Epidemiology. 2011;173(11):1319–1326. doi: 10.1093/aje/kwr033. http://dx.doi.org/10.1093/aje/kwr033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, Howard VJ. Traditional risk factors as the underlying cause of racial disparities in stroke: lessons from the half-full (empty?) glass. Stroke. 2011;42(12):3369–3375. doi: 10.1161/STROKEAHA.111.625277. http://dx.doi.org/10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Istepanian R, Laxminarayan S, Pattichis C, editors. M-Health: Emerging Mobile Health Systems. Springer; Berlin, Germany: 2006. [Google Scholar]
- Istepanian RSH, Zitouni K, Harry D, Moutosammy N, Sungoor A, Tang B, Earle KA. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. Journal of Telemedicine and Telecare. 2009;15(3):125–128. doi: 10.1258/jtt.2009.003006. http://dx.doi.org/10.1258/jtt.2009.003006. [DOI] [PubMed] [Google Scholar]
- Jae-Hyoung C, Hye-Chung L, Dong-Jun L, Hyuk-Sang K, Kun-Ho Y. Mobile communication using a mobile phone with a glucometer for glucose control in Type 2 patients with diabetes: as effective as an Internet-based glucose monitoring system. Journal of Telemedicine & Telecare. 2009;15(2):77–82. doi: 10.1258/jtt.2008.080412. http://dx.doi.org/10.1258/jtt.2008.080412. [DOI] [PubMed] [Google Scholar]
- Judd SE, McClure LA, Howard VJ, Lackland DT, Halanych JH, Kabagambe EK. Heavy drinking is associated with poor blood pressure control in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. International Journal of Environmental Research and Public Health. 2011;8(5):1601–1612. doi: 10.3390/ijerph8051601. http://dx.doi.org/10.3390/ijerph8051601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabagambe EK, Judd SE, Howard VJ, Zakai NA, Jenny NS, Hsieh M, Cushman M. Inflammation biomarkers and risk of all-cause mortality in the Reasons for Geographic And Racial Differences in Stroke cohort. American Journal of Epidemiology. 2011;174(3):284–292. doi: 10.1093/aje/kwr085. http://dx.doi.org/10.1093/aje/kwr085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz R MT, Barr K. Lessons from a community-based mHealth diabetes self-management program: “It's not just about the cell phone.”. Journal of Health Communication. 2012;17(1):67–72. doi: 10.1080/10810730.2012.650613. http://dx.doi.org/10.1080/10810730.2012.650613. [DOI] [PubMed] [Google Scholar]
- Kleindorfer D, Judd S, Howard VJ, McClure L, Safford MM, Cushman M, Howard G. Self-reported stroke symptoms without a prior diagnosis of stroke or transient ischemic attack: a powerful new risk factor for stroke. Stroke. 2011;42(11):3122–3126. doi: 10.1161/STROKEAHA.110.612937. http://dx.doi.org/10.1161/STROKEAHA.110.612937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan AG, McIsaac WJ, Tisler A, Irvine MJ, Saunders A, Dunai A, Cafazzo JA. Mobile phone-based remote patient monitoring system for management of hypertension in diabetic patients. American Journal Of Hypertension. 2007;20(9):942–948. doi: 10.1016/j.amjhyper.2007.03.020. MEDLINE. [DOI] [PubMed] [Google Scholar]
- Lyles CR, Harris LT, Le T, Flowers J, Tufano J, Britt D, Ralston JD. Qualitative evaluation of a mobile phone and web-based collaborative care intervention for patients with type 2 diabetes. Diabetes Technology & Therapeutics. 2011;13(5):563–569. doi: 10.1089/dia.2010.0200. http://dx.doi.org/10.1089/dia.2010.0200. [DOI] [PubMed] [Google Scholar]
- Mitchell PH, Ferketich S, Jennings BM. Quality health outcomes model. American Academy of Nursing Expert Panel on Quality Health Care. Image: Journal of Nursing Scholarship. 1998;30(1):43–46. doi: 10.1111/j.1547-5069.1998.tb01234.x. MEDLINE. [DOI] [PubMed] [Google Scholar]
- Muntner P, Halanych JH, Reynolds K, Durant R, Vupputuri S, Sung VW, Krousel-Wood M. Low medication adherence and the incidence of stroke symptoms among individuals with hypertension: The REGARDS study. Journal of Clinical Hypertension (Greenwich) 2011;13(7):479–486. doi: 10.1111/j.1751-7176.2011.00464.x. http://dx.doi.org/10.1111/j.1751-7176.2011.00464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntner P, Judd SE, McClellan W, Meschia JF, Warnock DG, Howard VJ. Incidence of stroke symptoms among adults with chronic kidney disease: results from the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Nephrol Dial Transplant. 2012;27(1):166–173. doi: 10.1093/ndt/gfr218. http://dx.doi.org/10.1093/ndt/gfr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pullicino PM, McClure LA, Howard VJ, Wadley VG, Safford MM, Meschia JF, Soliman EZ. Identifying a high stroke risk subgroup in individuals with Heart Failure. Journal of Stroke and Cerebrovascular Diseases. 2011 doi: 10.1016/j.jstrokecerebrovasdis.2011.10.012. http://dx.doi.org/10.1016/j.jstrokecerebrovasdis.2011.10.012. [DOI] [PMC free article] [PubMed]
- Quinn CC, Gruber-Baldini AL, Shardell M, Weed K, Clough SS, Peeples M, Lender D. Mobile diabetes intervention study: Testing a personalized treatment/behavioral communication intervention for blood glucose control. Contemporary Clinical Trials. 2009;30(4):334–346. doi: 10.1016/j.cct.2009.02.004. http://dx.doi.org/10.1016/j.cct.2009.02.004. [DOI] [PubMed] [Google Scholar]
- Rabin C, Bock B. Desired features of smartphone applications promoting physical activity. Telemedicine & e-Health. 2011;17(10):801–803. doi: 10.1089/tmj.2011.0055. http://dx.doi.org/10.1089/tmj.2011.0055. [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Turner MB. Heart disease and stroke statistics--2012 update: A report from the American Heart Association. [Comparative Study]. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. http://dx.doi.org/10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A. Home Broadband 2010. Pew Internet & American Life Projec. 2010 Retrieved from http://www.altfutures.com/pubs/DRA/Report_06_02_Cell_Phones_and_Health_Disparities.pdf.
- Soliman EZ, Howard G, Meschia JF, Cushman M, Muntner P, Pullicino PM, Howard VJ. Self-reported atrial fibrillation and risk of stroke in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke. 2011;42(10):2950–2953. doi: 10.1161/STROKEAHA.111.621367. http://dx.doi.org/10.1161/STROKEAHA.111.621367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner J, Larsen M, Tarassenko L, Neil A, Farmer A. Implementation of telehealth support for patients with type 2 diabetes using insulin treatment: An exploratory study. Informatics in Primary Care. 2009;17(1):47–53. doi: 10.14236/jhi.v17i1.714. MEDLINE. [DOI] [PubMed] [Google Scholar]
- Unverzagt FW, McClure LA, Wadley VG, Jenny NS, Go RC, Cushman M, Howard G. Vascular risk factors and cognitive impairment in a stroke-free cohort. Neurology. 2011;77(19):1729–1736. doi: 10.1212/WNL.0b013e318236ef23. http://dx.doi.org/10.1212/WNL.0b013e318236ef23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utz SW. Diabetes care among rural Americans. Annual Review of Nursing Research. 2008;26:3–39. MEDLINE. [PubMed] [Google Scholar]
- Wadley VG, Unverzagt FW, McGuire LC, Moy CS, Go R, Kissela B, Howard G. Incident cognitive impairment is elevated in the stroke belt: The REGARDS study. Annuals of Neurology. 2011;70(2):229–236. doi: 10.1002/ana.22432. http://dx.doi.org/10.1002/ana.22432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice. 1998;1:2–4. MEDLINE. [PubMed] [Google Scholar]
- Yoo HJ, Park MS, Kim TN, Yang SJ, Cho GJ, Hwang TG, Choi KM. A ubiquitous chronic disease care system using cellular phones and the internet. Diabetic Medicine. 2009;26(6):628–635. doi: 10.1111/j.1464-5491.2009.02732.x. MEDLINE. [DOI] [PubMed] [Google Scholar]
- Zickuhr K, Smith A. Digital differences. 2013 3/8/2013. Retrieved from http://pewinternet.org/Reports/2012/Digital-differences.aspx.
- Zolfaghari M, Mousavifar SA, Pedram S. Mobile phone text tessaging and telephone follow-up in Iranian Type 2 Diabetic Patients for 3 Months: A comparative study. Iranian Journal of Diabetes & Obesity (IJDO) 2009;1(1):45–51. [Google Scholar]
- Zweifler RM, McClure LA, Howard VJ, Cushman M, Hovater MK, Safford MM, Goff DC., Jr. Racial and geographic differences in prevalence, awareness, treatment and control of dyslipidemia: The reasons for geographic and racial differences in stroke (REGARDS) study. Neuroepidemiology. 2011;37(1):39–44. doi: 10.1159/000328258. http://dx.doi.org/10.1159/000328258. [DOI] [PMC free article] [PubMed] [Google Scholar]