Abstract
Evaluating patient-centered care (PCC) is crucial to its improvement. This pilot study tested the feasibility of an electronic format to assess PCC during hospitalization. Using a validated indicator of PCC imbedded on a mobile device, 86 older adults evaluated its delivery by registered nurses. Patients over 85 years of age rated PCC as poor (r=−0.22; p=.04). The electronic format was appraised as feasible, it performed well, and it took on average 30 minutes to complete.
Key Terms: iPAD, mobile device, older adults, patient outcomes, patient-centered care, technology
Over 12 million older adults receive hospital care annually in the United States (US), and such services are expected to rise 78% by 2027.1 Compared to others, hospitalized older adults are the most at risk for poor outcomes, including increased costs, rendering improvement in their health outcomes a national priority.2 One of the many recommendations for improving hospital outcomes is patient-centered care (PCC), viewed by the general public, health care systems, and funding/licensing agencies as an essential component of high quality health care.3 Although PCC has become a central aim for the nation’s health system, this approach remains underutilized and inconsistently applied in the hospital environment.3–7
PCC is especially important for older adults, who depend on registered nurses (RNs) during hospitalization for safe, quality care. At the heart of PCC is a healing (or caring) relationship where “patients are known as persons in context of their own social worlds, listened to, informed, respected, and involved in their care.”5(p100) RNs engage in the most direct contact with older adults during hospitalization and are key to providing PCC; yet few studies have been conducted to improve its delivery.
Measuring the quality of the patient-RN relationship through older adults’ assessments during hospitalization and using those results to efficiently revise RN practice is a first step in its improvement. While RNs deliver PCC in the hospital environment, patients themselves are considered the best authority for evaluating it; thus, efforts to measure and improve PCC should include their voice.8 An electronic platform would enable rapid-cycle performance improvement, provided older adults accept and can use the technology. Thus, the overall aim of this project was to explore the feasibility of measuring older adults’ perspectives of PCC during hospitalization. Specifically, the study aimed to explore feasibility (participation, functionality, acceptability, and usability) of measuring hospitalized older adults’ perceptions of PCC using electronic data collection; describe their perceptions of PCC; and examine the relationships of patient characteristics (selected demographics, acuity, co-morbidities, and LOS) to hospitalized older adults’ perceptions of PCC.
LITERATURE REVIEW
Patient-centered care and nursing
PCC is a complex phenomenon with several definitions, but a consistent theme among them is the quality of interactions between patients and clinicians,5 a core value of nursing. Little research has been conducted specifically examining PCC in the hospital environment; however, several nursing studies have shown positive associations between caring patient-nurse relationships and hospitalized patient outcomes, namely, patient satisfaction, decreased anxiety, increased knowledge, improved functional status, decreased symptom distress, authentic self-expression, sense of well-being, optimism, and trust in nurses.9,10 Outcomes of these studies are consistent with other studies that revealed positive associations between medically-delivered PCC and selected patient outcomes in the outpatient setting11–13
Despite the emerging associations between PCC and positive patient outcomes, barriers in the hospital environment continue to preclude its optimal delivery. A primary barrier to improving PCC is the lack of focus on it as a quality indicator and untimely performance reports that do not represent the patient’s perspective.14 The patient’s perspective of PCC, particularly at the point of care, is crucial in its evaluation and has been shown to be the best approach to its measurement.8 Recently, a 12-hospital performance improvement study used a validated indicator of PCC in the context of hospitalization, focusing on the improvement of patient-nurse relationships.15 Findings suggested that patients were willing to provide feedback about their care during hospitalization, but the administrative burden of manually entering patient responses into a statistical package, cleaning, analyzing, and disseminating the data was high. Delays in the availability of results prevented rapid improvement in PCC.
Real time feedback delivered directly to those providing care enhances performance improvement.16 To rapidly collect and disseminate patient feedback about PCC, the use of technology in the form of a bedside mobile device provides real-time data for use by RNs to revise their practice. Several concerns exist, however, related to implementing real-time data collection in hospitalized patients, especially those who are older. First, older adults may be reluctant to evaluate their care while they are hospitalized for fear of retaliation if they rate their care negatively.17 Second, hospitalized older adults are acutely ill and may be too sick or impaired to participate in any kind of data collection during their hospitalization. Third, concerns have been expressed about older adults’ abilities to use technology, especially if they have not previously been exposed to it.
Older adults and use of technology
Older adults are considered slow adopters of technology, such as computers, cell phones, iPads,19 and account for only 1% each of iPAD ownership, while those individuals ages 18–46 account for 5% each of iPAD ownership.17 Issues such as cost, lack of knowledge and experience, and interest are cited as reasons why older adults have limited use of technology. Furthermore, older adults may lack confidence in using technology and cognitive impairments may reduce their abilities to be effective users.18 Finally, older adults are concerned about maintaining their privacy when using technology17 and with design issues, such as font size and readability.19
While concerns exist about older adults’ abilities or desires to use technology, several indicators suggest that, when certain conditions are met, older adults can be successful users. Compared to using a mouse or keyboard, older adults are more comfortable with devices that have a touch screen, such as the iPad,20 and they are able to use these devices as accurately as younger adults.21 Suggestions to improve older adults’ ability to use technology include: providing a supportive, non-hurried environment,21 few to no graphics, 12–14 point font size, bolded and plain font such as Times New Roman, avoidance of colors especially in the yellow-blue-green hues, and no sound effects.19,22
The iPAD23 (Apple Inc, 2011) is a device that meets these needs while also allowing for accurate and reliable data collection. There is no keyboard or mouse, it has a pleasant user interface, and it is portable, lightweight, and easy to use. Furthermore, the iPAD costs less than other electronic devices, does not require wires or cables that might interfere with the hospital environment, and is easy to clean. The Pew Center indicated that the iPad has potential for adoption by older adults and was specifically designed by Apple with older adults in mind.24
Summary of literature review and related research questions
The literature available on older adults’ perceptions of PCC and the use of technology in the hospital setting is limited. Preliminary evidence suggests that the core relational aspect of PCC delivered by RNs during hospitalization is tied to important patient outcomes. However, older adults’ assessment of PCC during hospitalization has not been studied. While it seems clear that some older adults use technology, the vast majority of them do not have much experience with mobile devices, and there is little guidance on using technology with older adults during hospitalization to evaluate PCC. Gaps remain concerning whether electronically measuring PCC in hospitalized older adults is feasible. Research questions pertinent to this study were: (1) What is the feasibility of measuring hospitalized older adults’ perceptions of PCC using electronic data collection? (2) What are hospitalized older adults’ perceptions of PCC? and (3) What is the relationship between patient characteristics (selected demographics, acuity, co-morbidities, and LOS) and hospitalized older adults’ perceptions of PCC?
CONCEPTUAL FRAMEWORK
The Quality-Caring Model© (QCM)25,26 provided the conceptual framework for the study. The QCM is based on theory and research and postulates that caring patient-nurse relationships (a core aspect of PCC in the hospital environment) influences positive patient outcomes. It is used as a foundation for professional practice in over 40 US hospitals and was the basis for the e-CAT (used to measure PCC in this study) and in several research studies. For the purposes of this study, we examined the structural component; patient characteristics (selected demographics, acuity, comorbidities, and LOS); and PCC, a major process component of the model. This framework provides a strong rationale for attending to patient-nurse relationships as the central activity for improving PCC and ultimately, patient outcomes.
METHODS
Design, setting, and sample
A cross-sectional, non-experimental correlational design was used to explore the feasibility of electronically measuring patients’ perceptions of PCC during hospitalization. A Magnet-designated, Midwestern, 225-bed community hospital with 1,625 employees served as the study site. Subjects were recruited from 4 medical-surgical units with a large proportion of older adults. Inclusion criteria were: 1) ≥ 65 years of age, 2) can understand English, 3) admitted for at least 24 hours, and 4) not cognitively impaired (score of 6 or higher using the Short Portable Mental Status Questionnaire (SPMSQ).27 Enrollment averaged 7–9 participants per week over 12 weeks.
Instruments
Six instruments comprised the study tools. The SPMSQ27 has 10 items and was used to screen patients for inclusion in the study. It is valid and reliable (alpha = .0.81) and has been used as a screening tool in several other studies. The Departmental Questionnaire, developed for the study, was used to summarize the characteristics of the setting. Patient characteristics were abstracted from medical records using the Patient Questionnaire, a 12-item tool with general questions about age, educational level, gender, acuity, number of comorbities, and ethnicity. An electronic version of the 27-item Caring Assessment Tool (CAT),28 labeled the e-CAT, was used as the operational definition of PCC.
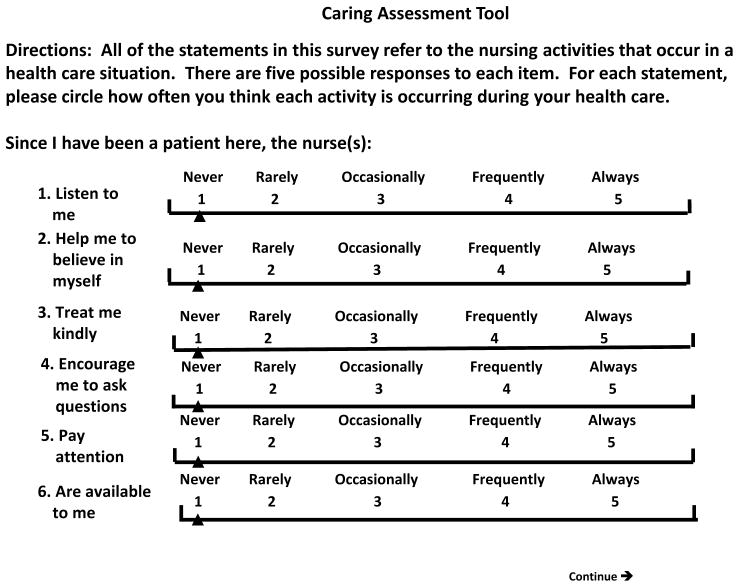
The CAT was originally developed based on theory, is arranged in Likert format (1 = never to 5 = always), and assesses the degree of nurse caring behaviors. The 27 items on the e-CAT are congruent with the definition of PCC, are low in burden, and take into account RNs’ contributions to PCC. The instrument has established validity and reliability (alpha = 0.97) with one overall factor structure explaining 73% of the variance and acceptable fit indices (CFI = 0.989; TLI = 0.988). It has been used extensively in studies of patient-nurse interactions. The e-CAT Usability Scale (10 items with a 5-point Likert scale) and Performance of e-CAT tool (5 items with Likert responses) collect data related to feasibility and functionality of the e-CAT.
Procedures
After human subjects approval, data collection techniques using the Research Electronic Data Capture (REDCap)29 survey application were developed and loaded on an iPAD. REDCap is an electronic data capture system that provides a secure Web connection, with authentication and data logging accessible via any Internet-connected computer. It also provides tools for data verification, including identification of discrepant or invalid data facilitating data collection, entry at remote sites, and export capabilities for analysis. The electronic database was established with the functionality to capture unit and patient characteristics, score individual items on the e-CAT, gather feasibility and functionality data, and export the results to a secure statistical database for analysis.
A Research Assistant (RA) randomly selected older adult patients using a computer-generated random list of numbers. Potential study subjects were identified based on their order on the hospital daily census and charge nurses on the 4 units approached them to inquire about their willingness to participate. They then notified the RA who verified inclusion criteria, obtained informed consent, and enrolled study subjects. Using the Departmental Questionnaire, the RA first gathered nursing unit characteristics. After patient enrollment, patient characteristics were abstracted from medical records using the Patient Questionnaire.
Next, using an iPAD touch screen, study participants completed the e-CAT. Study subjects were included only once and were asked (consistent with the instructions on the e-CAT) to consider their interactions with nurses (RNs) since they had been admitted to the specific unit. With assistance from the RA, older adults logged onto the iPAD using a code number and completed the e-CAT. If necessary (depending on the patient’s condition), the RA asked the question and assisted patients to enter their responses on the iPAD. The e-CAT items were displayed in easy-to-read, large font (Figure 1), and responses were captured as soon as the patient selected one. Responses were linked to the question, session, and time, but were not linked to any information that could identify an individual participant, ensuring confidentiality. When the patient completed answering the questions, the session and application were closed. To maintain hygiene, the iPAD was cleaned between study participants with water, per hospital policy. At the completion of the e-CAT, study participants were asked to evaluate the session using the e-CAT Usability Scale while the RA completed the Performance of e-CAT Tool. To generate participation rates, the RA documented the number of older adults approached, whether eligible/ineligible, interested/not interested, and enrolled/not enrolled in a separate file.
Figure 1. Visual Display of the e-CAT on the iPAD.
Reprinted by permission, 2012. Copyright J. R. Duffy.
RESULTS
Of the 4 medical-surgical units on which the study was conducted, unit size ranged from 16–37 beds (M=28.9; SD 9.0). A total of 151 RNs staffed the units. RN hours per patient day ranged from 6.9 to 8.6 (M=7.4; SD .80). RNs were, on average, 44 years old with almost 5 years of experience, and the majority (58%) held associate degrees while almost 20% held specialty certifications. Although clinical nurse specialists (CNSs) were available to answer clinical questions, none were dedicated to the involved study units.
Study participation
The total available participant pool was 376, with an average pool of 40.34 per day. Based on inclusion criteria, the random sampling scheme, and enrollment procedures, subject selection per study day averaged 10.74 with a mean of 2.57 subjects enrolled per day. Of the 152 subjects who were approached, 90 agreed to participate (59% participation rate). Documented reasons for not participating included: “being too sick,” going for tests, impending discharge, or family member recommendation not to participate. This is consistent with literature concerning older adults’ participation in research30 and is sufficient for a pilot study. Of the 90 participants enrolled into the study, 4 were deleted due to missing values, leaving a final sample size of 86.
Patient characteristics
Sixty-two percent of the sample was female (n=53); 51% was married (n=44) or widowed (n=31); and 78% had completed high school or above (n=67). However, 26% of the participants (n=22) only completed grade school. Age of participants ranged from 65 to 97 years (M=76; SD 7.6). The majority of participants (n=67) were retired and white (n=89). The SPMSQ scores of participants ranged from 6 to 10 (M=9.2; SD 0.99). Comorbid illnesses ranged from 1 to 18 with a mean of 6 (SD 2.7), and at the time of data collection, subjects had spent a mean of 2.8 days in the hospital (range 1 to 9 days; SD 1.8). Patient acuity was most often scored as: predictable, low complexity (n=36) or resilient, moderate complexity care (n=42). Thirty-four percent of the participants could walk with help (n=29); the remainder of the activity categories were evenly distributed: bedridden (n=21), up to chair (n=18), and walk without help (n=21).
Feasibility of e-CAT
The majority of participants (88%) agreed or strongly agreed that the e-CAT display was easy to use, and 81% of participants agreed or strongly agreed they were satisfied with this way of completing the CAT. Most participants (85%) disagreed or strongly disagreed that the questionnaire took too much time, and 70% would complete the questionnaire again. Seventy-four percent of participants preferred to answer questions using the iPAD. Most participants (83%) agreed or strongly agreed that they learned to do the questionnaire quickly, and 85% disagreed or strongly disagreed that the system was too difficult to use. The majority of participants would use the system again (87%), but 76% of all participants needed help.
As reported narratively on the Performance of e-CAT tool by the study RA, some barriers to use included: patients’ vision, calcified fingers, peripheral neuropathy, arthritis, difficulty hearing instructions, tremors, need for 2 fingers to scroll from item-to-item and page-to-page, and bed positioning. Facilitators included: the attitude and willingness of older adults to contribute to research and their interest in the electronic device. In spite of the need for help using the system and some physical barriers, 67% of the sample agreed or strongly agreed they could manage the system by themselves.
Functionality of electronic format
Five minutes were reported as necessary to log onto and set up the e-CAT for each participant. The e-CAT took between 6 and 65 minutes for participants to complete, with an average of 31 minutes (median = 30 minutes) for completion. The RA disagreed or strongly disagreed (65%) that the e-CAT took too long to administer, and patients were able to complete all of the e-CAT items 96% of the time. The survey application accurately calculated the total scores and transferred them to SPSS 100% of the time. However, the scrolling feature of the survey application required manipulation with 2 fingers, slightly limiting efficiency.
Older adults’ perceptions of patient-centered care
Overall, e-CAT reliability was consistent with prior studies (alpha = 0.93) as expected, and the time for completion using the electronic format, at an average of 31 minutes, was satisfactory. No significant differences in e-CAT scores were found among the 4 units. The overall e-CAT mean was 109.10 (SD 18.25), and the total item mean was 4.04 (SD .67), indicating a high degree of perceived PCC delivered by RNs. Analysis of higher and lower e-CAT items reflect themes consistent with our previous work suggesting that RNs frequently convey human respect to patients but attend to mutual problem-solving less often (Table 1).
Table 1.
Top 5 Highest and Lowest Mean Scoresa on e-CAT
| Item Number | Item | Mean Scores |
|---|---|---|
| 2 | Make me feel as comfortable as possible. | 4.6 |
| 4 | Pay attention to me when I am talking. | 4.5 |
| 11 | Respect me. | 4.5 |
| 19 | Respect my need for privacy. | 4.5 |
| 21 | Treat my body carefully. | 4.6 |
| 9 | Are concerned about how I view things. | 3.7 |
| 15 | Help me explore alternative ways of dealing with my health problems. | 3.6 |
| 16 | Ask me what I know about my illness. | 3.6 |
| 17 | Help me figure out questions to ask other health care professionals. | 3.5 |
| 24 | Help me deal with my bad feelings. | 3.4 |
Range of possible scores = 1 to 5
Relationships of patient characteristics to perceptions of PCC
No statistically different patient characteristics were noted across study units. Of the patient characteristics examined, only age demonstrated a statistically significant, though weak, association with PCC (r=− 0.22; p=.04). This is consistent with prior studies in which older-old patients rated their experiences with health care providers lower.31, 32
DISCUSSION
Results of this pilot study demonstrated that older adults can use technology during hospitalization to evaluate their care. Contrary to contemporary images of hospitalized older adults, most participants in this study scored highly on mental status, could use a technological device to answer questions about their care, found the electronic version of the e-CAT quick and easy to use, and preferred this way of participating in survey research. Despite a high number of participants indicating they needed some help using the system, most agreed or strongly agreed they could manage the system by themselves, suggesting that many older adults can engage in electronic data collection for rapid-cycle performance improvement during hospitalization. Concerns that older adults may choose not to participate in the study for fear that their evaluations might negatively affect their care were never expressed by actual or potential participants. In fact, many subjects suggested that interacting with the study RA (who was a nurse) was the only time anyone sat down and actually talked to them during their hospitalization.
The participation rate in this study was slightly less than our prior studies of older adults, who were ready for discharge,33 and may reflect patients’ acuity during the earlier period of hospitalization and the many system activities (eg, discharges, tests) that limited availability of patients for participation. Trepidation about rating their nursing care during hospitalization was not a factor adversely affecting subject recruitment. Although the overall and item scores for PCC were higher, older-old adults tended to rate the quality of PCC lower than younger patients.
Strengths and limitations
Strengths of the study were the randomly selected participants, sample size, consistent performance of the e-CAT, and functionality of the electronic application. Limitations of the study included the predominately white population who were recruited from 1 Magnet hospital’s medical-surgical nursing units; thus, results cannot be generalized to other populations or communities.
CONCLUSIONS
Results of this study provided an understanding of the complexity of real-time PCC measurement. Specifically, findings provided evidence that PCC evaluations can be done by hospitalized older adults in real-time using the iPAD for data collection, an understanding of the performance of the e-CAT in this population, and a basis for tailoring an intervention to busy hospital departmental RNs to assist them in PCC performance improvement. The majority of older adults in this sample accepted and used the mobile device, with over 70% stating they preferred this way of evaluating their care and most enjoying the experience. Further work must be done to find ways to incorporate patients’ perspectives of PCC into ongoing performance improvement, and practical strategies for using their assessments by RNs to optimize PCC must be tested.
Although the research team successfully imbedded a validated indicator of PCC on an iPAD and it functioned well, the features of the REDCap survey application limited efficiency. Implications for future research are: 1) designing an improved web-based application for hospitalized older adults’ data collection that allows easier manipulation of the text, 2) developing and testing an intervention targeted to RNs to improve PCC, 3) including additional hospitalized patients with diverse characteristics, and 4) expanding the study to other sites, including those in the community.
“The goal of PCC is to provide care that is concordant with patients’ values, needs and preferences, and that allows patients and families to provide input and participate actively in decisions regarding their health and health care.”34(p1516) Consistently measuring the quality of PCC from the patient’s perspective and in real time is a first step in making practice changes, sharing lessons learned, and improving patient outcomes. A mobile device used to gather their feedback about PCC is a practical way to engage hospitalized older adults, a vulnerable, high priority population that is increasing. Evaluating PCC from older adults’ perspectives and in the context of hospitalization shifts the focus of care to a ‘patient-led’ health system, addressing the national call for safe, high quality, and patient-centered services that improve outcomes.35
Acknowledgments
The project was funded by an Indiana University School of Nursing Research Investment Grant.
Footnotes
The authors declare no conflict of interest
Contributor Information
Joanne R. Duffy, Email: jrduffy@iupui.edu, Professor and Coordinator, Nursing Leadership in Health Systems, Indiana University School of Nursing, Indianapolis, IN.
Wendy Carter Kooken, Assistant Professor, Western Illinois University, Macomb, IL.
Cheryl Wolverton, Research Assistant, Indiana University School of Nursing, Indianapolis, IN.
Michael T. Weaver, Professor & Director. Statistical Service, Center for Nursing Research and Scholarship, Indiana University School of Nursing, Indianapolis, IN.
References
- 1.Walker CP, Hogstel MO, Curry LC. Hospital discharge of older adults: How nurses can ease the transition. Am J Nurs. 2007;107(6):60–70. doi: 10.1097/01.NAJ.0000271853.38215.20. [DOI] [PubMed] [Google Scholar]
- 2.Moore SM, Duffy E. Maintaining vigilance to promote best outcomes for hospitalized elders. Crit Care Nurs Clin. 2007;19(3):313–319. doi: 10.1016/j.ccell.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Berwick D. What “patient centered” should mean: confessions of an extremist. Health Aff (Millwood) 2008;28(4):w555–w565. doi: 10.1377/hlthaff.28.4.w555. [DOI] [PubMed] [Google Scholar]
- 4.Henrich A, Chow MP, Gosher WS. A proclamation for change: Transforming the hospital patient care environment. J Nurs Adm. 2009;39(6):266–275. doi: 10.1097/NNA.0b013e3181a72927. [DOI] [PubMed] [Google Scholar]
- 5.Epstein RM, Street RL. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100–102. doi: 10.1370/afm.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wasson JH, Baker NJ. Balanced measures for patient-centered care. J Ambul Care Manage. 2009;32(1):44–55. doi: 10.1097/01.JAC.0000343123.53585.51. [DOI] [PubMed] [Google Scholar]
- 7.Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient--centered health care. Health Aff (Millwood) 2010;29(8):1489–1495. doi: 10.1377/hlthaff.2009.0888. [DOI] [PubMed] [Google Scholar]
- 8.Hudon C, Fortin M, Haggerty JL, Lambert M, Poitras ME. Measuring patients’ perceptions of patient-centered care: A systematic review of tools for family medicine. Ann Fam Med. 2011;9(2):155–164. doi: 10.1370/afm.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Radwin LE, Cabral HJ, Wilkes G. Relationships between patient-centered cancer nursing interventions and desired health outcomes in the context of the health care system. Res Nurs Health. 2009;32(1):4–17. doi: 10.1002/nur.20302. [DOI] [PubMed] [Google Scholar]
- 10.Yeakel S, Maljanian R, Bohannon R, Coulombe K. Nurse caring behaviors and patient satisfaction: Improvement after a multifaceted staff intervention. J Nurs Adm. 2003;33(9):434–436. doi: 10.1097/00005110-200309000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Bertakis K, Azari R. Patient-centered care is associated with decreased health care utilization. J Fam Prac Med. 2011;24(3):229–239. doi: 10.3122/jabfm.2011.03.100170. [DOI] [PubMed] [Google Scholar]
- 12.Lewin S, Skea Z, Entwistle VA, Zwarenstein M, Dick J. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database of Systematic Reviews. 2001;4(CD003267) doi: 10.1002/14651858.CD003267. [DOI] [PubMed] [Google Scholar]
- 13.Mead N, Bower P. Patient-centered consultations and outcomes in primary care: a review of the literature. Patient Educ Couns. 2002;48(1):51–61. doi: 10.1016/s0738-3991(02)00099-x. [DOI] [PubMed] [Google Scholar]
- 14.Davies E, Cleary PD. Hearing the patient’s voice? Factors affecting the use of patient survey data in quality improvement. Qual Saf Health Care. 2005;14(6):428–432. doi: 10.1136/qshc.2004.012955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duffy J, Brewer B. Feasibility of a multi-institution collaborative to improve patient- nurse relationship quality. J Nurs Adm. 2010;41(2):78–83. doi: 10.1097/NNA.0b013e3182059463. [DOI] [PubMed] [Google Scholar]
- 16.Nelson EC, Godfrey MM, Batalden PB, et al. Clinical microsystems part 1. The building blocks of health systems. Jt Comm J Qual Patient Saf. 2008;34(7):367–378. doi: 10.1016/s1553-7250(08)34047-1. [DOI] [PubMed] [Google Scholar]
- 17.Coughlin J, D’Ambrosio LA, Reimer B, Pratt MR. Older adult perceptions of smart home technologies: implications for research, policy & market innovations. Conf Proc IEEE Eng Med Biol Soc. 2007:1810–1815. doi: 10.1109/IEMBS.2007.4352665. [DOI] [PubMed] [Google Scholar]
- 18.Zickuhr K. Generations and their gadgets. [Accessed December 28, 2011];The Pew Research Center Web site. http://pewinternet.org/~/media//Files/Reports/2011/PIP_Generations_and_Gadgets.pdf. Published February 3, 2011.
- 19.Chaffin AJ, Maddux CD. Accessibility accommodations for older adults seeking e-health information. J Gerontol Nurs. 2007;33(3):6–12. doi: 10.3928/00989134-20070301-03. [DOI] [PubMed] [Google Scholar]
- 20.Bajarin B. Why tablets represent the future of computing. [Accessed December 29, 2011];Time Techland Web site. http://techland.time.com/2011/06/24/why-tablets-represent-the-future-of-computing/. Published June 24, 2011.
- 21.Murata A, Iwase H. Usability of touch-panel interfaces for older adults. J Human Factors Ergonomics Soc. 2005;47(4):767–776. doi: 10.1518/001872005775570952. [DOI] [PubMed] [Google Scholar]
- 22.Czaja S, Charness N, Fisk A, et al. Factors predicting the use of technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE) Psych Aging. 2006;21(2):333–352. doi: 10.1037/0882-7974.21.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Apple Inc. iPAD. [Accessed January 2011];Apple Web site. 2010 Jun; http://www.apple.com/ipad.
- 24.Grandison T, Williams C, Heyning E, Muradaz R, Tonelli P, Adler R. The SCAN Foundation Technology Summit: Enhancing social action for older adults through Technology expert panel report. The Center for Technology and Aging. 2010:1–57. [Google Scholar]
- 25.Duffy J, Hoskins LM. The Quality-Caring Model: Blending dual paradigms. ANS Adv Nurs Sci. 2003;26(1):77–88. doi: 10.1097/00012272-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Duffy J. quality caring in nursing: Applying theory to clinical practice, education, and leadership. New York: Springer; 2009. [Google Scholar]
- 27.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 28.Duffy J, Brewer B, Weaver M. Revision and psychometric properties of the Caring Assessment Tool. Clin Nurs Res. 2010 May 17; doi: 10.1177/1054773810369827. [DOI] [PubMed] [Google Scholar]
- 29.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jacelon CS. Older adults’ participation in research. Nurs Res. 2007;14(4):64–73. doi: 10.7748/nr2007.07.14.4.64.c6044. [DOI] [PubMed] [Google Scholar]
- 31.Schoen C, Strumpf E, Davis K, Osborn R, Donelan K, Blendon RJ. The elderly’s experiences with health care in five nations. [Accessed May 2011];The Commonwealth Fund Web site. 2002 Mar; Available at www.cmwf.org.
- 32.Jaipaul CK, Rosenthal GE. Are older patients more satisfied with hospital care than younger patients? J Gen Int Med. 2003;18(1):23–30. doi: 10.1046/j.1525-1497.2003.20114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duffy J, Hoskins LM, DudleyBrown S. Improving outcomes for older adults with heart failure: A randomized trial using a theory-guided nursing intervention. J Nurs Care Qual. 2010;25(1):56–64. doi: 10.1097/NCQ.0b013e3181ad0fbd. [DOI] [PubMed] [Google Scholar]
- 34.Epstein RM, Franks P, Fiscella K, et al. Measuring patient-centered communication in patient-physician consultations: Theoretical and practical issues. Soc Sci Med. 2005;61(7):1516–1528. doi: 10.1016/j.socscimed.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 35.The Center for Alternative Futures. Patient centered care 2015: Scenario, vision, goals and next steps. [Accessed December 2010];Picker Institute Web site. 2004 Jul; http://www.altfutures.com/pubs/Picker%20Final%20Report%20May%2014%202004.pdf.