Abstract
Objective
To examine the mechanisms of prolonged exposure (PE) and naltrexone (NAL) that underlie symptom reduction among individuals with comorbid posttraumatic stress disorder (PTSD) and alcohol dependence (AD). We hypothesized that: 1) reduction in negative cognitions mediates PTSD improvement during PE; and 2) reduction in alcohol craving mediates reduction in drinking frequency during NAL treatment; and (3) PTSD improvement mediates reduction in craving and alcohol use during PE.
Method
Participants were 159 individuals meeting the DSM-IV diagnosis of PTSD and AD randomly assigned to one of four conditions: PE+NAL, PE+placebo (PBO), supportive counseling (SC)+NAL; and SC+PBO. All participants received supportive counseling.
Results
Lagged multilevel mediational analyses indicated that: 1) a reciprocal relationship between cognitive change and PTSD improvement was observed in PE+NAL, PE+PBO, and SC+NAL but not in SC+PBO; 2) reduction in craving significantly mediated subsequent decrease in alcohol use in PE+NAL and SC+PBO, but not in PE+PBO and SC+NAL; and 3) PTSD improvement significantly mediated subsequent reduction of craving in PE+PBO, and mediated decrease in alcohol use in PE+NAL.
Conclusions
The efficacy of combining PE and NAL for reducing alcohol use among those with comorbid PTSD/AD seems to be through reduction in both PTSD symptoms and craving. These findings shed light on the mechanism of PE and highlight the central role of PTSD in the maintenance of alcohol craving and use in patients with comorbid PTSD/AD.
Keywords: Posttraumatic stress, mediation, prolonged exposure, naltrexone, alcohol dependence
Prolonged exposure (PE) and naltrexone (NAL) are evidence-based treatments for posttraumatic stress disorder (PTSD) (e.g., Powers, Halpern, Ferenschak, Gillihan, & Foa, 2010) and alcohol dependence (AD) (e.g., Balldin et al., 2003), respectively. Recently, the combination of PE and NAL was found effective for comorbid AD and PTSD in a randomized controlled trial (RCT) comparing NAL, PE, their combination, and supportive counseling (Foa et al., 2013). PTSD and AD improved for all participants, but those who received PE+NAL maintained low levels of drinking 6-months after treatment ended. To understand the efficacy of PE+NAL, we examined the mechanisms that underlie this intervention. Previous work has examined mediators of change in NAL and PE separately, but no study has examined mediators of a combined intervention for PTSD and AD.
PE is based on emotional processing theory (EPT; Foa, Huppert, & Cahill, 2006), which proposes that PTSD symptoms are maintained, in part, by negative trauma-related cognitions about the world as entirely dangerous and the self as entirely incompetent. Recovery from PTSD therefore involves modifying these cognitions, a hypothesis that is supported by research showing that negative cognitions mediate change in PTSD symptoms during exposure therapy (Mueser et al., 2008). Sophisticated mediation approaches also show that reductions in negative cognitions during PE lead to subsequent reductions in PTSD but not vice versa (Zalta et al., 2014). These results suggest that negative cognitions are a mechanism of PE, but to date, no study has tested this hypothesis in individuals with comorbid AD/PTSD.
A key mechanism of NAL's effect on AD is thought to be the attenuation of alcohol craving. This hypothesis is supported by studies showing that NAL decreases craving, which is negatively associated with drinking (e.g., Richardson et al., 2008). However, some studies find no effect of NAL on craving (e.g., Davidson et al., 2004). Importantly, no study has examined whether craving mediates decreases in drinking for those receiving NAL.
To understand the finding that PE+NAL for AD/PTSD was superior in maintaining low levels of drinking after treatment, it is important to identify the mechanisms of treatment for PTSD and AD separately, but also to understand how the combination of treatments affect change. One hypothesis relates to the self-medication hypothesis of AD/PTSD. This hypothesis emphasizes a functional relationship between alcohol use and PTSD symptoms wherein PTSD symptoms elicit alcohol craving (Kwako et al., 2014) and drinking, in order to soothe trauma-related distress. In this way, drinking is negatively reinforced by the alleviation of PTSD. This suggests that PE may decrease craving and drinking indirectly via the reduction of PTSD.
We examined the hypothesized mechanisms of PE and NAL among patients with AD/PTSD using data from a RCT (Foa et al., 2013), in which participants were randomly assigned to receive: PE+NAL, PE+placebo (PBO), supportive counseling (SC)+NAL, or SC+PBO. We hypothesized that: 1) reduction in negative cognitions mediates PTSD improvement during PE; and 2) reduction in alcohol craving mediates reduction in drinking during NAL; and (3) PTSD improvement mediates reduction in craving and alcohol use during PE.
Method
Participants
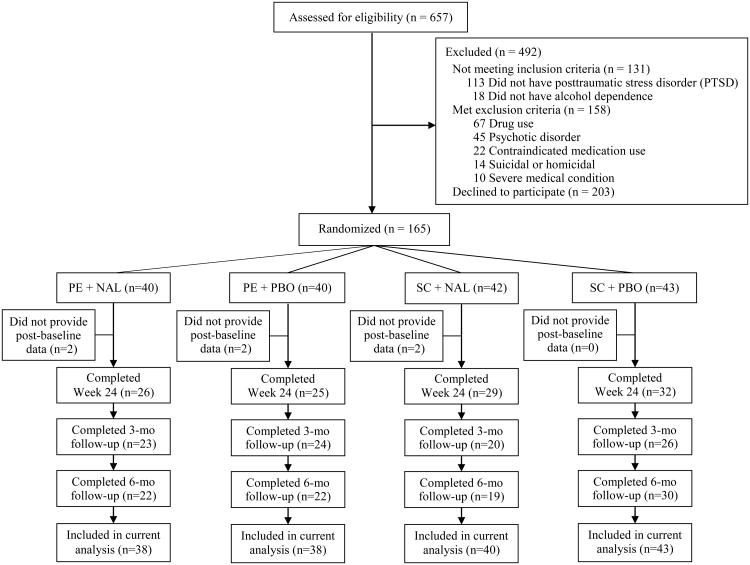
A total of 159 participants with DSM-IV AD and PTSD were drawn from Foa et al. (2013) (See Figure 1). Additional inclusion criteria: (a) significant PTSD symptoms (≥15 on the PTSD Symptom Scale-Interview Version [(PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993); and (b) heavy drinking in the past 30 days (>12 alcoholic drinks/week with at least 1 day of ≥4 drinks on the Time-Line Follow-Back interview) (TLFB; (Sobell & Sobell, 1992). The mean age was 42.9±9.8 years, with 65.4% males. Reported race was Black (63.5%), White (30.2%), and other (6.3%). Prior mental health treatment for trauma-related difficulties was reported by 40.1% of participants. Exclusion criteria: (a) current substance dependence other than alcohol, nicotine, or cannabis; (b) current severe psychiatric symptoms (e.g., psychosis, active suicidal ideation); (d) opiate use in the past month; (e) certain medical illnesses (e.g., AIDS, active hepatitis); or (f) pregnancy or nursing. The study was approved by the university's institutional review board.
Figure 1.
Participants flow through the study. PE = prolonged exposure; NAL = Naltrexone; PBO = placebo; SC = supportive counseling.
Procedure
Following informed consent, participants completed a psychiatric and physical evaluation. Eligible participants completed a baseline assessment and were randomly assigned to 100 mg/day NAL or PBO and to receive or not receive PE. All participants received supportive counseling (see below). Prior to treatment, participants completed outpatient medical detoxification (≥ 5 consecutive days of alcohol abstinence). Study measures were administered by blind independent evaluators at pre-treatment, every four weeks during treatment, and post-treatment. Alcohol craving was also measured weekly during treatment.
Treatment
Naltrexone (NAL)
NAL is an FDA-approved opiate antagonist for AD. The target dose was 100 mg/day. Compliance with the dosing regimen was monitored by weekly pill counts during the first 3 months and twice-monthly for the next 3 months.
Prolonged Exposure (PE)
PE (Foa, Hembree, & Rothbaum, 2007) consisted of 12 weekly 90-minute sessions followed by 6 twice-monthly sessions. PE includes in vivo exposure (i.e., approaching trauma-related situations and stimuli), imaginal exposure (i.e., revisiting the trauma memories) and processing (i.e., discussing thoughts and feelings related to revisiting).
Supportive Counseling (SC)
SC, modeled after BRENDA (Starosta, Leeman, & Volpicelli, 2006), consisted of 12 weekly 30-45 minute sessions followed by 6 twice-monthly sessions of medication management with compliance enhancement administered by the study nurse.
Measures
PTSD symptoms
The PSS-I is a 17-item clinical interview that evaluates DSM-IV PTSD symptoms on a frequency/severity scale over the past two weeks (Foa et al., 1993). The PSS-I includes subscales for the three PTSD symptom clusters. The PSS-I has good excellent internal reliability, test–retest reliability, and interrater reliability for PTSD diagnosis (Foa et al., 1993).
Trauma-related negative cognitions
The Posttraumatic Cognitions Inventory (PTCI; Foa, Ehlers, Clark, Tolin, & Orsillo, 1999) is a 33-item self-report measure of negative trauma-related cognitions. The PTCI has excellent internal consistency, test-retest reliability, convergent validity, and sensitivity and specificity for PTSD diagnosis (Foa et al., 1999).
Percent days drinking
The Alcohol Timeline Follow-Back Interview (TLFB; Sobell & Sobell, 1992) uses a calendar method to assess alcohol consumption over a specified time period. The TLFB has excellent psychometric properties (Fals-Stewart, O'Farrell, Freitas, McFarlin, & Rutigliano, 2000). The TLFB was used to calculate the percent days drinking (PDD)
Alcohol Craving
The Penn Alcohol Craving Scale (PACS; Flannery, Volpicelli, & Pettinati, 1999) is a 5-item self-report measure of the frequency, intensity, and duration of alcohol craving during the past week. The PACS has excellent internal consistency and has been shown to predict relapse to drinking (Flannery et al., 1999).
Statistical Analysis
Hierarchical linear modeling in which Level 1 data (PTCI, PSS-I, PACS, and PDD) were nested within Level 2 data (participants) was conducted using SPSS 18.0 mixed models with restricted maximum likelihood estimation. All Level 1 data included seven time points (week 0, 4, 8, 12, 16, 20, 24), except the PACS which included 19 time points (weeks 0-12, 14, 16 18, 20, 22, 24). A linear time variable was used for following analyses. Multilevel mediation analyses examined within-subject mediation and moderated multilevel mediation examined whether the strength of mediating effect varied by treatment conditions (Bauer, Preacher, & Gil, 2006). The covariance of path a (predictors causes mediators) Lagged mediation analysis was used to establish the temporal precedence of the mediators. Reverse mediation was also conducted to evaluate the temporal dynamics of the relationship between the proposed mediator and outcome variable. Treatment conditions were dummy-coded and included as Level 2 covariates. The PRODCLIN program was used to test the significance and confidence limits (CI) of random indirect effects (MacKinnon, Fritz, Williams, & Lockwood, 2007). Percent mediation (pM) was calculated as an indicator of effect size of the mediator. The potential covariance between Paths a (predictor→mediator) and b (mediator→outcome) was taken into account when calculating the CI of indirect effects and percent mediation.
Results
At the baseline assessment, the mean PSS-I total score was 28.24±7.91. Table 1 presents the means and standard deviations of the study variables across time points.
Table 1. Means and Standard Deviations of Measured Outcome and Mediators.
| PSS-I | PTCI | PDD | PACS | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Time point | M | SD | M | SD | M | SD | M | SD |
| Week 1 (pre-tx) | 28.24 | 7.91 | 127.84 | 38.95 | 74.66 | 25.25 | 18.36 | 6.86 |
| Week 4 | 22.62 | 9.22 | 114.21 | 41.11 | 19.77 | 26.04 | 13.23 | 7.54 |
| Week 8 | 19.53 | 10.52 | 110.33 | 43.59 | 13.78 | 21.65 | 11.66 | 7.94 |
| Week 12 (mid-tx) | 17.05 | 10.96 | 104.60 | 42.98 | 11.24 | 19.39 | 10.30 | 7.48 |
| Week 16 | 15.53 | 10.63 | 96.86 | 41.56 | 10.41 | 18.46 | 9.37 | 7.21 |
| Week 20 | 15.28 | 10.57 | 104.26 | 41.76 | 10.53 | 17.69 | 8.01 | 6.31 |
| Week 24 (post-tx) | 12.31 | 10.56 | 93.25 | 43.22 | 11.20 | 18.39 | 7.72 | 7.08 |
Note. tx = treatment; PSS-I = PTSD Symptoms Scale-Interview; PTCI = Posttraumatic Cognitions Inventory; PDD = percent days drinking (assessed by Timeline Follow-Back Interview). PACS = Penn Alcohol Craving Scale
Does Change in Negative Cognitions Mediate PTSD Improvement during PE?
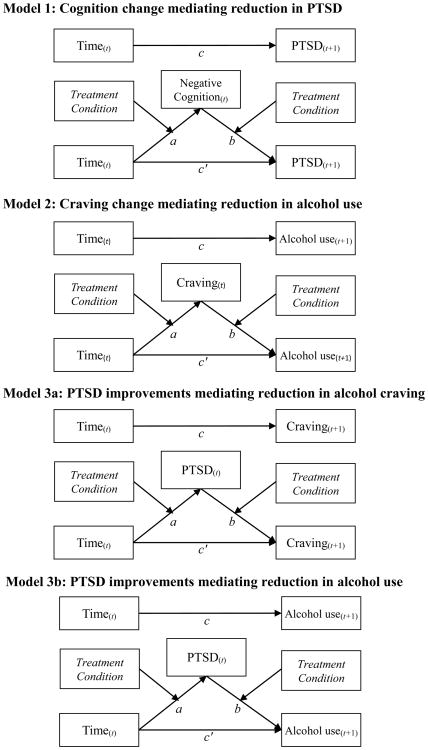
Lagged multilevel mediation in which time, negative cognitions (PTCI), and PTSD symptoms (PSS-I) were the predictor, mediator, and outcome, respectively showed that each path (c, a, b, and c′) and the indirect effect (ab = -0.48, 95%CI [-0.33, -0.66]) were all significant (see Table 2 and Figure 2: Model 1), indicating that reduction in negative cognitions significantly mediated PTSD improvement. After entering treatment condition as a Level 2 predictor, we found that PTSD improved in all conditions (Path c), and negative cognitions decreased in all conditions except SC+PBO (Path a). Lagged negative cognitions were significantly associated with PTSD symptoms in all conditions (Path b) and the indirect effects of time on PTSD through negative cognitions were significant in all conditions except SC+PBO. Moderated mediation analyses indicated that Path a (i.e., cognitive change) was significantly weaker in SC+PBO than in PE+NAL (bdiff = -6.46, t(141.3)=-3.81, p<.001; 95% CI [-9.77, -3.09]), PE+PBO (bdiff=-3.93, t(139.4)=-2.33, p=.021; 95%CI [-7.26, -0.56]), and SC+NAL (bdiff=-3.65, t(134.9)=-2.24, p= .027; 95%CI [-6.88, -0.43]). Path b and c′ did not significantly differ across conditions. The reverse mediation model, in which lagged PTSD mediates the effect of time on negative cognitions, was supported in all conditions except SC+PBO.
Table 2. Lagged Multilevel Moderated Mediation Analysis.
| c | a | b | c′ | ab | ||
|---|---|---|---|---|---|---|
|
|
||||||
| Treatment | Change in Y | Change in M | M→Y controlling for time | Change in Y controlling for M | Indirect effect [95% CI] | Percent mediation (%) |
| Model 1: time → negative cognitions (M) → PTSD (Y) | ||||||
| PE + NAL | -2.33*** | -8.22***a | 0.09*** | -1.60*** | -0.73 [-0.32, -1.21] | 31.5 |
| PE + PBO | -2.56*** | -5.65***a | 0.10*** | -1.97*** | -0.59 [-0.26, -0.99] | 22.9 |
| SC + NAL | -1.56*** | -5.42***a | 0.09*** | -1.09** | -0.47 [-0.20, -0.82] | 30.1 |
| SC + PBO | -1.60*** | -1.77b | 0.10*** | -1.43*** | -0.17 [0.05, -0.45] | 10.8 |
| Reverse model:time → PTSD (M) → negative cognitions (Y) | ||||||
| PE + NAL | -6.58*** | -3.33***a | 1.06*** | -3.03 | -3.55 [-5.71, -1.55] | 53.9 |
| PE + PBO | -4.82** | -2.68***a | 0.92** | -2.36 | -2.46 [-4.36, -0.75] | 51.1 |
| SC + NAL | -4.04** | -1.97***b | 0.71* | -2.63 | -1.41 [-2.82, -0.17] | 34.9 |
| SC + PBO | -1.86 | -1.80***b | 0.52 | -0.91 | -0.94 [-2.27, 0.25] | 50.9 |
|
| ||||||
| Model 2: time → craving (M) → drinking (Y) | ||||||
| PE + NAL | -2.30* | -2.06***a | 0.81** | -0.65 | -1.65 [-0.48, -2.92] | 71.7 |
| PE + PBO | -1.40 | -1.60*** | 0.75** | -0.20 | -1.21 [-0.38, -2.14] | 86.1 |
| SC + NAL | 0.96 | -1.39***b | 0.17 | 1.21a | -0.23 [0.49, -0.97] | — a |
| SC + PBO | -2.83*** | -1.48***b | 0.71** | -1.80**b | -1.01 [-0.25,-1.87] | 35.8 |
| Reverse model: time → drinking (M) → craving (Y) | ||||||
| PE + NAL | -0.87** | -8.44*** | 0.032 | -0.61* | -0.27 [-0.61, 0.06] | 30.6 |
| PE + PBO | -0.81** | -7.75*** | 0.034* | -0.55 | -0.26 [-0.51, -0.00] | 32.5 |
| SC + NAL | -0.75** | -7.23*** | 0.00 | -0.72** | -0.03 [-0.28, 0.21] | 4.1 |
| SC + PBO | -1.04*** | -8.22*** | 0.035 | -0.75** | -0.29 [-0.60, 0.01] | 27.8 |
|
| ||||||
| Model 3a: time → PTSD (M) → craving (Y) | ||||||
| PE + NAL | -1.33*** | -3.33***a | 0.10 | -1.01*** | -0.33 [0.05, -0.72] | 24.5 |
| PE + PBO | -1.25*** | -2.68***a | 0.21*** | -0.67* | -0.57 [-0.25, -0.93] | 45.9 |
| SC + NAL | -0.97*** | -1.97***b | 0.07 | -0.83** | -0.14 [0.10, -0.41] | 14.8 |
| SC + PBO | -1.17*** | -1.80***b | 0.04 | -1.10*** | -0.07 [0.16, -0.31] | 5.8 |
| Reverse model: time → craving (M) → PTSD (Y) | ||||||
| PE + NAL | -2.48*** | -2.06***a | 0.35** | -1.74*** | -0.73 [-1.28, -0.23] | 29.5 |
| PE + PBO | -2.16*** | -1.60*** | 0.10 | -2.00*** | -0.16 [-0.48, 0.15] | 7.4 |
| SC + NAL | -1.73*** | -1.39***b | 0.15 | -1.52*** | -0.21 [-0.51, 0.06] | 12.1 |
| SC + PBO | -1.21** | -1.48***b | 0.07 | -1.11** | -0.10 [-0.43, 0.22] | 8.1 |
|
| ||||||
| Model 3b: time → PTSD (M) → drinking (Y) | ||||||
| PE + NAL | -2.67* | -3.33***a | 0.39* | -1.38 | -1.29 [-0.08, -2.56] | 48.2 |
| PE + PBO | -1.57 | -2.68***a | 0.11 | -1.28 | -0.29 [0.72, -1.32] | 18.5 |
| SC + NAL | 0.31 | -1.95***b | 0.17 | 0.60a | -0.33 [0.44, -1.15] | — a |
| SC + PBO | -2.53** | -1.80***b | 0.25 | -2.08**b | -0.46 [0.25, -1.21] | 17.7 |
| Reverse model: time → drinking (M) → PTSD (Y) | ||||||
| PE + NAL | -1.96*** | -8.44*** | 0.036 | -1.65***a | -0.30 [-0.69, 0.73] | 15.4 |
| PE + PBO | -1.72*** | -7.75*** | 0.037a | -1.44** | -0.28 [-0.59, 0.01] | 16.5 |
| SC + NAL | -1.46*** | -7.23*** | -0.017b | -1.58***a | 0.12 [-0.14, 0.39] | — a |
| SC + PBO | -0.76 | -8.22*** | 0.042*a | -0.42b | -0.34 [-0.70, -0.01] | 45.1 |
Note. c, a, b, c′ represent the paths of the lagged mediation model as depicted in Figure 2. Bold type for ab (indirect effect) column indicates p < .05. Y = outcome variable; M = mediator; 95% CI = 95 percent confidence interval. Superscripts a and b denote significant difference between two treatment conditions (p < .05). PTSD = posttraumatic stress disorder. PE = prolonged exposure; NAL = Naltrexone; PBO = placebo; SC = supportive counseling.
The percent mediation did not apply because the sign of the indirect effect and the total effect was opposite in both cases.
p < .05.
p < .01.
p < .001.
Figure 2.
Lagged moderated mediation models. Across all models, the mediator was lagged so that the mediator at time t predicted the outcome at time t + 1. PTSD = posttraumatic stress disorder.
Does Change in Craving Mediate Reduction in Alcohol Use during NAL treatment?
Lagged multilevel mediation in which time, craving (PACS), and alcohol use (percent days drinking) were the predictor, mediator, and outcome, respectively showed that the mediation paths and the indirect effect (ab=-1.04, 95%CI [-0.60, -1.50]) were all significant, indicating that reduction in craving significantly mediated reduction in alcohol use (see Table 2 and Figure 2: Model 2). After entering treatment as a Level 2 predictor, alcohol use significantly decreased only in PE+NAL and SC+PBO (Path c), and craving significantly decreased in all conditions (Path a). Lagged craving score was significantly associated with alcohol use in all conditions except SC+NAL (Path b). The indirect effects of time on alcohol use via craving were significant in all conditions except SC+NAL. Moderated mediation analyses indicated that Path a (i.e., change in PACS) was significantly stronger in PE+NAL than SC+NAL (bdiff=0.67, t(172.5)=2.29, p=.023, 95%CI [0.09, 1.24]) and SC+PBO (bdiff=0.58, t(166.9)=2.02, p=.044, 95%CI [0.02, 1.14]). The reverse mediation model, in which alcohol use mediates the effect of time on craving, was supported only in PE+PBO.
Does PTSD Improvement Mediate Reduction in Craving and Alcohol Use during PE?
Lagged multilevel mediation in which time, PTSD (PSS-I), craving (PACS) and alcohol use were the predictor, mediator, and outcomes, respectively showed that all individual mediation paths and the indirect effects were significant (model 3a: ab=-0.27, 95%CI [-0.13, -0.42]; model 3b: ab=-0.57, 95%CI [-0.11, -1.05]), indicating that PTSD improvement significantly mediated reductions in craving and drinking (see Table 2 and Figure 2: Model 3a & 3b).
Model 3a
After treatment condition was entered as a Level 2 predictor, craving (Path c) and PTSD (Path a) both significantly decreased in all conditions. The association of lagged PTSD and craving (Path b), and the indirect effect of time on craving via PTSD symptoms was significant only in PE+PBO. Moderated mediation analyses found that PTSD improvement (Path a) was significantly stronger in PE+NAL than SC+NAL (bdiff=1.36, t(123.0)=3.07, p=.003; 95%CI [0.48, 2.23]) and SC+PBO (bdiff=1.53, t(123.2)=3.52, p<.001; 95%CI [0.67, 2.39]), and significantly greater in PE+PBO than SC+PBO (bdiff=0.88, t(126.1)=2.01, p=.047; 95%CI [0.01, 1.75]). The reverse mediation model, in which craving mediates the effect of time on PTSD symptoms, was supported only in PE+NAL.
Model 3b
Alcohol use significantly decreased in PE+NAL and SC+PBO (Path c), and PTSD symptoms significantly improved in all conditions (Path a). The association of lagged PTSD and craving (Path b), and the indirect effect of time on alcohol use via PTSD symptoms were significant only in PE+NAL. Moderated mediation analysis showed that the results for Path a (i.e., change in PTSD symptoms) were similar to those of model 3. The reverse mediation model, in which drinking mediates the effect of time on PTSD were non-supported in all models.
Discussion
The current study tested theoretically derived mediators of PE and NAL alone and in combination for the treatment of AD/PTSD. The hypothesis that reductions in trauma-related negative cognitions would mediate PTSD improvement during PE (i.e., PE+NAL, PE+PBO) was supported. Moreover, there was a reciprocal relationship between negative cognitions and PTSD symptoms during PE such that changes in PTSD symptoms mediated changes in cognitions. This finding extends prior research (e.g., Mueser et al., 2008) by showing that changes in negative cognitions mediate subsequent reductions in PTSD symptoms, and vice versa, using a lagged multilevel mediation analysis. Contrary to hypothesis, negative cognitions also mediated PTSD symptoms in SC+NAL. This suggests that NAL improved PTSD via negative cognitions, a conclusion that is consistent with studies showing that antidepressant medications are as effective as cognitive therapy in reducing depressive cognitions among depressed patients (e.g., Fournier et al., 2013). It is also possible that NAL helped individuals utilize the potential benefits of SC such that SC, in the context of NAL, impacted PTSD via negative cognitions.
The hypothesis that reductions in alcohol craving mediate reduction in drinking frequency during NAL was not supported. Contrary to hypothesis, reduction in craving significantly mediated reduction in drinking in PE+NAL and SC+PBO but not in SC+NAL or PE+PBO. NAL was not superior to PBO in reducing craving, which is consistent with some (e.g., Davidson et al., 2004) but not all prior studies (e.g., Richardson et al., 2008). The nonsignificant mediating effect for SC+NAL suggests that although the attenuation of alcohol craving is involved in reducing drinking, it is not a key mechanism of NAL. Alternate mechanisms (e.g., aversive responses to alcohol; McCaul, Wand, Eissenberg, Rohde, & Cheskin, 2000) may better account for the effects of NAL on drinking. Alternately, the effect of NAL on drinking may depend on the presence of other interventions (e.g., PE). Given that the effect of craving was stronger in PE+NAL than SC+NAL, it could be that adding PE to NAL contributes to its craving mediating effect. Notably, the reverse mediation (alcohol use→craving) was supported only in PE+PBO.
The result is unexpected and approached nonsignificance (p = .049), and thus warrants further replication before given further consideration. Overall, our findings did not support the reciprocal relationship between reductions in craving and decrease in alcohol use.
A primary goal of this study was to understand the superiority of PE+NAL in helping patients maintain abstinence from drinking (Foa et al., 2013). In partial support of our hypothesis that PE reduced craving and drinking via reduction in PTSD symptoms, we found that PTSD improvement significantly mediated reduction in craving in PE+PBO, but not in PE+NAL. Given the use of lagged analysis, this suggests that PE reduced PTSD, which then lowered craving. PTSD improvement also mediated drinking in PE+NAL, but because the indirect effect of PE+PBO was similar to the two SC conditions, it is unclear whether the mediating effect observed in PE+NAL is attributable to PE. Interestingly, the reverse mediation (craving→PTSD) was observed in PE+NAL but not in PE+PBO. As shown in Table 2, this finding might be explained by the higher association between craving and subsequent PTSD severity in PE+NAL (i.e., Path b) than in PE+PBO. In contrast, the association between PTSD and subsequent craving was stronger in PE+PBO than in PE+NAL (which was nonsignificant). Therefore, the direction of mediation between reduction in craving and PTSD improvement might depend on the combination of PE and NAL.
Several limitations warrant discussion. First, all participants received SC, which precludes ruling out the possibility that SC contributed to the effects of PE and NAL. Second, although lagged mediation analyses were used to establish the temporal precedence, the analyses did not control for autoregressive effect, which could help control for confounding variables. Despite these limitations, a major contribution of this study is the demonstration that the superiority of PE+NAL in maintaining abstinence in those with combined AD and PTSD might be that it effectively targeted the important hypothesized mechanisms in a way that lead to meaningful change, including alcohol craving, PTSD as well as negative cognitions.
Public Health Significance of the Study.
This study found that the mechanism by which combined naltrexone (NAL) and prolonged exposure (PE) therapy reduces alcohol use among those with comorbid alcohol dependence (AD) and post-traumatic stress disorder (PTSD) is the reduction of both PTSD symptoms and alcohol craving. Our findings shed light on the mechanisms of the combined treatment and highlight the crucial role of PTSD symptomatology in the maintenance of alcohol craving and use in patients with comorbid AD and PTSD.
Acknowledgments
This study was supported by National Institute on Alcohol Abuse and Alcoholism (RO1 AA012428) PI: Edna Foa.
Contributor Information
Carmen P. McLean, Department of Psychiatry, University of Pennsylvania
Yi-Jen Su, Graduate Institute of Behavioral Sciences, Chang Gung University and Department of Psychiatry, University of Pennsylvania.
Edna B. Foa, Department of Psychiatry, University of Pennsylvania
References
- Balldin J, Berglund M, Borg S, Månsson M, Bendtsen P, Franck J, et al. Stolt G. A 6-Month Controlled Naltrexone Study: Combined Effect With Cognitive Behavioral Therapy in Outpatient Treatment of Alcohol Dependence. Alcoholism: Clinical and Experimental Research. 2003;27:1142–1149. doi: 10.1097/01.ALC.0000075548.83053.A9. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychological Methods. 2006;11:142–163. doi: 10.1037/1082-989X.11.2.142. [DOI] [PubMed] [Google Scholar]
- Davidson D, Saha C, Scifres S, Fyffe J, O'Connor S, Selzer C. Naltrexone and brief counseling to reduce heavy drinking in hazardous drinkers. Addictive Behaviors. 2004;29:1253–1258. doi: 10.1016/j.addbeh.2004.03.027. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037/0022-006X.68.1.134. [DOI] [PubMed] [Google Scholar]
- Flannery B, Volpicelli J, Pettinati H. Psychometric properties of the Penn Alcohol Craving Scale. Alcoholism: Clinical and Experimental Research. 1999;23:1289–1295. doi: 10.1111/j.1530-0277.1999.tb04349.x. [DOI] [PubMed] [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, Orsillo SM. The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment. 1999;11:303–314. doi: 10.1037/1040-3590.11.3.303. [DOI] [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic Experiences:Therapist guide. New York: Oxford University Press; 2007. [Google Scholar]
- Foa EB, Huppert JD, Cahill SP. Emotional Processing Theory: An Update. In: Rothbaum BO, editor. Emotional Processing Theory: An Update. New York: Emotional Processing Theory; 2006. pp. 3–24. An Update. [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. doi: 10.1002/jts.2490060405. [DOI] [Google Scholar]
- Foa EB, Yusko DA, McLean CP, Suvak MK, Bux DA, Oslin D, et al. Volpicelli J. Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: A randomized clinical trial. Journal of the American Medical Association. 2013;310:488–495. doi: 10.1001/jama.2013.8268. [DOI] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Hollon SD, Gallop R, Shelton RC, Amsterdam JD. Differential change in specific depressive symptoms during antidepressant medication or cognitive therapy. Behaviour Research and Therapy. 2013;51:392–398. doi: 10.1016/j.brat.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwako LE, Schwandt ML, Sells JR, Ramchandani VA, Hommer DW, George DT, et al. Heilig M. Methods for inducing alcohol craving in individuals with comorbid alcohol dependence and posttraumatic stress disorder: Behavioral and physiological outcomes. Addiction biology, Advanced online publication. 2014 doi: 10.1111/adb.12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavior Research Methods. 2007;39:384–389. doi: 10.3758/BF03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaul ME, Wand GS, Eissenberg T, Rohde CA, Cheskin LJ. Naltrexone alters subjective and psychomotor responses to alcohol in heavy drinking subjects. Neuropsychopharmacology. 2000;22:480–492. doi: 10.1016/S0893-133X(99)00147-5. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Rosenberg SD, Xie H, Jankowski MK, Bolton EE, Lu W, et al. Wolfe R. A randomized controlled trial of cognitive-behavioral treatment for posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology. 2008;76:259–271. doi: 10.1037/0022-006X.76.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review. 2010;30:635–641. doi: 10.1016/j.cpr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Richardson K, Baillie A, Reid S, Morley K, Teesson M, Sannibale C, et al. Haber P. Do acamprosate or naltrexone have an effect on daily drinking by reducing craving for alcohol? Addiction. 2008;103:953–959. doi: 10.1111/j.1360-0443.2008.02215.x. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back. In: Litte RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Starosta AN, Leeman RF, Volpicelli JR. The BRENDA model: Integrating psychosocial treatment and pharmacotherapy for the treatment of alcohol use disorders. Journal of Psychiatric Practice. 2006;12:80–89. doi: 10.1097/00131746-200603000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalta AK, Gillihan SJ, Fisher AJ, Mintz J, Cahill SP, Yehuda R, Foa EB. Change in trauma-related cognitions drives symptom reduction in prolonged exposure for PTSD. Journal of Consulting and Clinical Psychology. 2014;82:171–175. doi: 10.1037/a0034735. [DOI] [PMC free article] [PubMed] [Google Scholar]