Abstract
Building on an earlier study (Compas et al., 2011), tests of main effects and potential moderators of a family group cognitive-behavioral (FGCB) preventive intervention for children of parents with a history of depression are reported in a sample of 180 families (242 children ages 9-15 years) in a randomized controlled trial assessed at 2-, 6-, 12-, 18- and 24-months after baseline. Significant effects favoring the FGCB intervention over a written information (WI) comparison condition were found on measures of children's symptoms of depression, mixed anxiety/depression, internalizing problems, and externalizing problems, with multiple effects maintained at 18- and 24-months, and on incidence of child episodes of major depressive disorder over the 24-months. Effects were stronger for child self-reports than for parent-reports. Minimal evidence was found for child age, child gender, parental education, parental depressive symptoms, or presence of a current parental depressive episode at baseline as moderators of the FGCB intervention. The findings provide support for sustained and robust effects of this preventive intervention.
Keywords: parental depression, prevention, moderation
Depression is a major public health problem affecting the lives of millions in the U.S. and worldwide. It is estimated that 16% of Americans experience at least one episode of major depressive disorder (MDD) in their lifetime with significant impairment in interpersonal, work, and family roles (Kessler et al., 2003). Early onset of depression during childhood or adolescence is associated with a worse course of the disorder, including more frequent episodes of longer duration and greater impairment (National Research Council/Institute of Medicine [NRC/IOM], 2009). Further, a history of depression in a parent is one of the most powerful risk factors for a first episode of MDD during childhood or adolescence (Beardslee, Gladstone, & O'Connor, 2011). It is estimated that over 15 million children and adolescents in the U.S. live with a parent with depression and these children are at three to four times greater risk than the general population for developing depression and other psychiatric disorders before they reach adulthood (NRC/IOM, 2009). Therefore, the prevention of depression in offspring of parents with a history of depression is a major significant public health priority.
Four recent reviews have highlighted the importance of the prevention of depression and documented progress that has been made, especially in children and adolescents at risk due to parental depression (Beardslee et al., 2011; Cuijpers, Beekman, & Reynolds, 2012; Muñoz, Beardslee, & Leykin, 2012; Siegenthaler, Munder, & Egger, 2012). As summarized in these reviews, three randomized controlled trials have provided promising evidence that rates of MDD can be significantly reduced in children of depressed parents (Clarke et al., 2001; Compas et al., 2009, 2011; Garber et al., 2009). The relative risk for MDD in these trials for children in the intervention vs. controls ranged from .36 to .66 at follow-ups ranging from 8 to 24 months (Siegenthaler et al., 2012). More recently Beardslee et al. (2013), reporting a follow-up of the Garber et al. study, found that intervention effects maintained at a 33-month follow-up. In their review, Muñoz et al. (2012) specifically highlight a family-based intervention (Compas et al., 2009, 2011) as one of the most promising based on the significant reductions in depressive symptoms and incidence of MDD in children.
The progress toward preventing depression found in these studies notwithstanding, two significant gaps have been identified in this research. First, reviewers have highlighted the need for evidence of long-term effects (Cuijpers et al., 2012; Muñoz et al., 2012); i.e., many [but certainly not all (e.g., Beardslee et al., 2013)] assessments of preventive effects have been limited to one year or less from baseline (Clarke et al., 2001; Garber et al., 2009) and Merry, Hetrick, Cox, Brudevold-Iversen, Bir, and McDowell (2011) reported no evidence for efficacy at 24 months post-treatment. Evidence that effects are sustained over time is essential to document the prevention of symptoms and disorder in high-risk children and adolescents. Second, the identification of potential moderators of preventive interventions is important to determine if there are sub-groups for whom these interventions are more vs. less effective (e.g., Horowitz & Garber, 2006; Kazdin, 2008; Stice, Shaw, Bohon, Marti, & Rohde, 2009). Potential moderators include child age and gender, parental depression symptoms and diagnostic status, and family socioeconomic status.
The focus of the current study is on the effects of a family group cognitive-behavioral preventive intervention (FGCB) that includes components to teach parenting skills to depressed parents and coping skills to their adolescent-age children. The intervention is based on evidence regarding two factors related to the effects of parents’ depression on their children: stressful parent-child interactions (i.e., disrupted parenting) that are the result of the symptoms of parents’ depression, and the ways that children respond to and cope with these stressful interactions. These processes were selected because research has demonstrated that they are important influences on emotional and behavioral problems in children of depressed parents and are potentially malleable through psychological intervention (Compas, Keller, & Forehand, 2011). Previous reports have described the effects of the intervention at 2-, 6-, 12-, 18- and 24-months in a sample of 111 families of depressed parents (Compas et al., 2009, 2011). Significant effects were found on adolescents’ self-reports of depression, mixed anxiety/depression, internalizing symptoms, and externalizing symptoms; however, these effects diminished over time as only the effect for externalizing symptoms remained significant at 24-months. However, non-significant effect sizes at 18 and 24 months included d's ranging from .21 to .30, suggesting that the study may have been underpowered for detecting small to medium effects. Although the intervention led to significantly fewer adolescent episodes of MDD over the course of 24-months, the findings from the parent and adolescent reports on symptom measures just noted suggest that preventive effects may have dissipated over time. Moreover, because of the moderate sample size, analyses of possible moderators of this intervention were not conducted.
One goal of the current study is to further examine the effects of the FGCB intervention with the addition of a substantial number of families (n = 69) that were enrolled and analyzed since the initial published reports of this intervention with the original sample of 111 families (Compas et al., 2009, 2010, 2011) and the inclusion of all children per family in a nested design (i.e., 131 additional children for a total of 242 children in the current analyses). This represents a 62% increase in the number of families and more than twice the number of children available for the current analyses. The increased sample size provides increased power to test for main effects of the FGCB intervention, particularly to ascertain when prevention effects first emerge (i.e., 2-, 6- or 12-months) and if effects persist at 18- and 24-month follow-ups.
A second goal of this study is to examine possible moderators of the FGCB intervention. Moderators can be examined at several levels, including familial (e.g., family socioeconomic status), parental (e.g., parent depressive episodes), and child (e.g., age and gender). Three meta-analytic reviews of interventions to prevent depression in children and adolescents (Horowitz & Garber, 2006; Merry et al., 2011; Stice et al., 2009) found some evidence of moderator effects for child gender (larger effects for girls than boys), and in the two examining child age (Horowitz & Garber, 2006; Stice et al.), some evidence for larger effects for older adolescents. As Stice et al. note, these effects were expected as girls have higher levels of depressive symptoms and older adolescents can understand and implement skills more readily than younger adolescents and children. As both girls and boys were represented in our sample and as coping skills of youth is a major component of FGCB, we examine both of these child variables. In regard to parent variables serving as moderators, Garber et al. (2009) and Beardslee et al. (2013) reported significant moderation effects for parents’ baseline depressive episode in their analyses of a preventive intervention for adolescent offspring of depressed parents at 9-month follow-up. The intervention had a significant effect compared with usual care only for adolescents whose parents were not in a depressive episode at entry into the intervention even though parents were not included in the intervention. As parenting skills are a major component of the FGCB intervention and parent depression interferes with implementing these skills (see Lovejoy, Graczyk, O'Hare, & Neuman, 2000, for a review), we examine the role of parent depressive symptoms and parent depression episode as moderators. Finally, family socioeconomic status, particularly parental educational level, is related to parent-child interactions (see Hoffman, 2003). Although recent meta-analyses of child depression prevention programs (e.g., Merry et al., 2011; Stice et al., 2009) have not examined parental educational level as a moderator, we include this variable. Research with other childhood problems using prevention/intervention programs with similar components to those in FGCB (e.g., parenting) suggest proxies for socioeconomic status can qualify outcomes (see Lundhal, Risser, & Lovejoy, 2006, for a review).
Several hypotheses served as the focus for the present study. First, significant main effects were expected favoring the FGCB intervention as compared with a written information control condition across post-intervention and follow-up time points, including initial assessments at 2-, 6-, and 12-months after baseline and long-term outcomes assessed at 18- and 24-months after baseline. With a larger sample and increased statistical power, we expected that the intervention would have sustained significant effects on a wider range of internalizing and externalizing child outcomes than in our original analyses (Compas et al., 2009, 2011). Second, based on findings from previous prevention trials (Clarke et al., 2001; Compas et al., 2009, 2011), we expected a more consistent pattern of significant effects for self-reports than parent-reports of children's internalizing and externalizing problems. Third, we examined selected variables from familial (parent education), parent (depression), and child (age, gender) systems as potential moderators. Further, in order to broadly test for any potential moderators, we examined variables from the three systems (familial, parental, child) at each of five points in time following intervention. If we identify moderators consistently over these assessments, we can reach conclusions for whom the program is most effective and design modifications to enhance effectiveness for those adolescents not responding or not maintaining a response in follow-up to the prevention program. Alternately, if consistent patterns do not emerge for variables examined as moderators, evidence for the efficacy of the prevention program (within limits imposed by sample size) across familial, parent, and child characteristics will have been generated.
Method
Participants
Participants included 180 parents with current or past MDD or dysthymic disorder during the lifetime of their child(ren) and 242 children of these parents from the areas in and around Nashville, Tennessee and Burlington, Vermont. This sample includes the 111 families that comprised the sample reported in Compas et al. (2009, 2011) plus an additional 69 families and 131 children who enrolled after the original cohort of families. Further, analyses in Compas et al. (2009, 2011) were based on one child per family, whereas the current nested analyses include all children (an increase from 111 children to the current sample of 242 children).
Target parents with a positive history of MDD or DY included 160 mothers (mean age = 41.16, SD = 7.17) and 20 fathers (mean age = 48.30, SD = 7.50). Parents’ level of education included less than high school (6%), completion of high school (9%), some college (30%), college degree (32%), and graduate education (23%). Eighty-two percent of target parents were Euro-American, 12% African-American, 2% Hispanic-American, 1% Asian-American, 1% Native American, and 2% mixed ethnicity. The racial and ethnic compositions of the samples were representative of the regions in Tennessee and Vermont from which they were drawn based on the 2000 U.S. Census data. Annual family income ranged from less than $5,000 to more than $180,000, with a median annual income between $40,000-60,000. Sixty-two percent of parents were married/partnered, 22% divorced, 5% separated, 10% had never married, and 1% were widowed. Families randomized to the FGCB and written information conditions did not differ significantly on any of these demographic variables.
Children enrolled in the study and included in the current analyses ranged from 9- to 15-years-old and included 121 girls (mean age = 11.38, SD = 2.00) and 121 boys (mean age = 11.68, SD = 2.03). Seventy-four percent of children were Euro-American, 13% African-American, 3% Asian American, 2% Hispanic American, 1% Native American, and 7% mixed ethnicity. We targeted ages 9 to 15-years-old in order to intervene before the documented increase in rates of depression that occurs in early to mid-adolescence (e.g., Hankin et al., 1998) and to include children who were old enough to learn the relatively complex cognitive coping skills taught in the intervention.
Forty-eight parents (27%) were in a current episode of major depression and 132 parents (73%) were not in episode at the time of the baseline assessment. At baseline, 147 (82%) parents reported experiencing multiple episodes of depression during their child's/children's life (Median = 3), 27 (15%) reported experiencing only a single episode during their child's/children's life, and 5 (2.7%) parents reported dysthymic disorder during their child's life (one parent did not provide enough information to determine frequency of depressive episodes).
Parents and children were able to receive other forms of mental health treatment throughout the course of the study. Seventy-six percent of parents and 23% of children received psychological and/or pharmacologic treatment during the 2 years of the study. The percentage of parents and children who received treatment did not differ for the FGCB vs. WI conditions.
Setting and Personnel
All study procedures were approved by the Institutional Review Boards at Vanderbilt University and the University of Vermont. All assessments and group intervention sessions were conducted in the Department of Psychology and Human Development at Vanderbilt University and the Psychology Department at the University of Vermont. Doctoral students in clinical psychology and staff research assistants, who were blind to condition, conducted the structured diagnostic interviews after receiving extensive training. Each group intervention was co-facilitated by one of three clinical social workers and one of nine doctoral students in clinical psychology. Facilitators were trained for approximately 30 hours by reading the intervention manual, listening to audiotapes of a pilot intervention, and discussing and role-playing each session with an experienced facilitator. Ongoing supervision was conducted weekly by two Ph.D. clinical psychologists.
Measures
Demographics
Demographics (e.g., age, gender, race, education) were reported by the parent.
Child Outcome Measures
Children's depressive symptoms
Depressive symptoms were assessed with the Center for Epidemiologic Studies-Depression scale (CES-D; Radloff, 1977), a self-report measure of the frequency of 20 depressive symptoms over the past week using a 4-point scale. The CES-D is short and easy to read, has been successfully administered in several large school samples (e.g., Roberts et al., 1991), and has good psychometrics with youth (α = .89; test-retest reliability = .61; sensitivity of 83.7 and specificity of 75.2 in predicting current MDD). Internal consistency in the current sample ranged from α = .87 to .91 across the six assessments.
Children's internalizing and externalizing symptoms
The Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) was used to assess symptoms of anxiety/depression (as a measure of general emotional distress) and total internalizing and externalizing problems in children and adolescents. These scales were selected to represent the range of problems that have been identified in children of depressed parents and to match the scales reported by Clarke et al. (2001), Beardslee et al. (2007) and Compas et al. (2009, 2011). The CBCL includes a 118-item checklist of problem behaviors that parents rate as not true (0), somewhat or sometimes true (1), or very true or often true (2) of their child in the past 6 months. Children and adolescents completed the Youth Self-Report (YSR; Achenbach & Rescorla, 2001), the self-report version of the CBCL for adolescents ages 11 to 18-years-old. Reliability and validity of the CBCL and YSR are well established (Achenbach & Rescorla, 2011). In the current sample, internal consistency for the scales used in this study ranged from α = .78 to .92 for the CBCL and α = .81 to .91 for the YSR. Nine and 10 year-old children completed the YSR to allow for complete data on all measures. The internal consistency for the YSR scales was adequate with this younger age group in the current sample (all alphas ≥ .80). Raw scores on the CBCL and YSR scores were used in all analyses to maximize variance (i.e., some variability is lost when the raw scores are converted to T scores because in some instances more than one raw score corresponds to a single T score) and to be consistent with our prior analyses of this dataset (Compas et al., 2009, 2010, 2011).
Child diagnostic interview
Episodes of MDD in children were determined using the Schedule for Affective Disorders and Schizophrenia for School-Age Children- Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997), a reliable and valid semi-structured interview that generates DSM-IV Axis I child psychiatric diagnoses. Separate interviews were conducted with parents and children and combined by taking the higher score for each symptomto yield both current and lifetime MDD diagnoses. Inter-rater reliability for diagnoses of MDD, calculated on 28 interviews, indicated 96% agreement (kappa = 0.76). For the current study, we examined the occurrence of MDD during the 24 months following baseline assessment.
Potential Moderators
Familial: Family socioeconomic status
Parent report of parent education was used as a proxy for family socioeconomic status as it is the most closely related to parent-child interactions and is the most stable of the possible SES indicators (Hoffman, 2003) (see Reyno & McGrath, 2006). Parents reported their educational attainment in one of 5 categories: (1) less than high school, (2) high school or equivalency exam, (3) some college or technical school, (4) college graduate- 4 year degree, and (5) any graduate education.
Parental: Parental depressive symptoms
Parents’ current depressive symptoms were assessed with the Beck Depression Inventory-II (BDI-II), a standardized and widely used self-report checklist of depressive symptoms with adequate internal consistency (α = .91) and validity in distinguishing severity of MDD (Beck, Steer, Ball, & Ranieri, 1996; Steer, Brown, Beck & Sanderson, 2001). Internal consistency in the current sample ranged from α = .92 to .95.
Parental: Parental depression diagnoses
Parents’ current and past history of MDD was assessed and other Axis I disorders were screened with the Structured Clinical Interview for DSM (SCID; First, Spitzer, Gibbon, & Williams, 2001), a semi-structured diagnostic interview to assess current and previous episodes of psychopathology based to DSM-IV criteria (American Psychiatric Association, 1994). Inter-rater reliability, calculated on a randomly selected subset of these interviews, indicated 93% agreement (kappa = 0.71) for diagnoses of MDD.
Child: Child age and gender
Child age and gender were tested as possible moderators of the effects of the FGCB intervention.
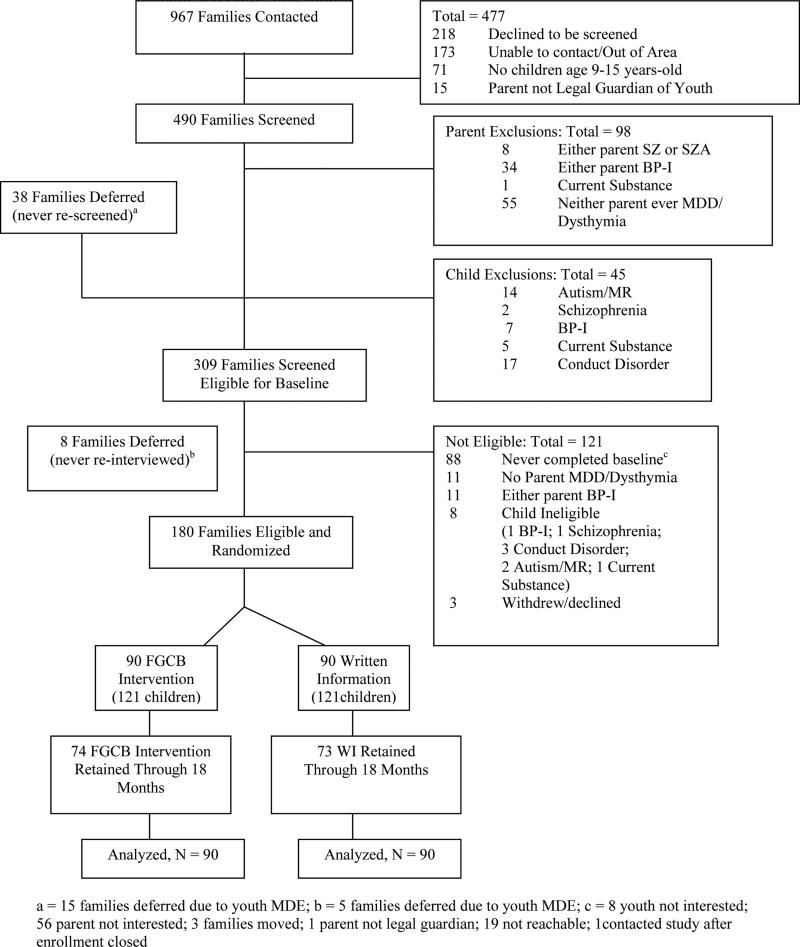
Design and Procedures
Figure 1 depicts screening and enrollment. In order to enroll a sample of parents with past or current MDD regardless of their history of seeking or receiving treatment, we recruited from several sources, including mental health clinics/practices, family and general medical practices, and media outlets. A total of 967 parents contacted the research teams. As shown in Figure 1, 490 of the 967 parents who contacted the research team were eligible and available to be screened (i.e., 49% of families who made initial contact with the research team were either unable to be contacted, declined to be screened, or did not meet basic eligibility criteria). The 490 parents were initially screened by telephone and moved to the next stage if the parent met criteria for MDD either currently or during the lifetime of her/his child(ren) and the following criteria were met: (a) parent had no history of bipolar I, schizophrenia, or schizoaffective disorder; (b) children had no history of autism spectrum disorders, mental retardation, bipolar I disorder, or schizophrenia; and (c) children did not currently meet criteria for conduct disorder or substance/alcohol abuse or dependence. Children with conduct disorder were excluded based on evidence that group interventions with children with disruptive behavior disorders can lead to contagion of these problems among group members (Dishion & Dodge, 2005). Therefore, the eligible families may under-represent families of depressed parents whose children have developmental disorders or conduct disorder and families with parents with BP-I.
Figure 1.
Participant screening and randomization.
Eligible families were deferred for later reassessment if a parent was currently suicidal with a Global Assessment of Functioning (GAF) ≤ 50 on the SCID, had current alcohol/substance abuse or dependence with a GAF ≤ 50, or if one of the target children had current MDD (n = 38). Such families were deemed unsuitable for the intervention at the current time and were assisted in obtaining appropriate mental health services in the community. Deferred families were re-screened every 2 months (if deferred for suicidality or child depression) or every 6 months (if deferred for alcohol or drug problems), until they screened eligible and could be invited to the next stage of recruitment.
Families were randomized in blocks of eight families to the FGCB (90 families with 121 children) or WI (90 families with 121 children) conditions. The parent with a history of depression completed all parent measures. Each child in the 9-15 year old age range completed the child measures. The order of randomization was determined by a random number generator, and the assignment order was kept in a series of sealed envelopes that were opened by research assistants who were blind to assignment until the envelope was opened for a family.
Retention rates
. Ninety (50%) families were assigned to FGCB and 90 (50%) families were assigned to WI (Figure 1). Ninety-three percent of families (92% and 93% in FGCB and WI, respecitvely) remained enrolled at 18 months (i.e., 7% of families withdrew from the study), and 88% of the families (87% and 89% in FGCB & WI, respectively) completed data collection through the 24-month follow-up, defined by the provision of data at any or all of the follow-ups.
Intervention and Comparison Conditions
Family group intervention
The FGCB intervention , for parents and 9-15 year old children, is a manualized 12-session program (8 weekly sessions and 4 monthly booster sessions) for 4 families in each group (Compas et al., 2011). The program is designed for participation by both parents and children. Goals are to educate families about depressive disorders, increase family awareness of the impact of stress and depression on functioning, help families recognize and monitor stress, facilitate the development of adaptive coping responses to stress, and improve parenting skills. Parents learn parenting skills (i.e., praise, positive time with children, encouragement of child use of coping skills, structure, and consequences for positive and problematic child behavior) from one facilitator and children learn skills for coping with their parents’ depression from the other facilitator. The core coping skills are summarized by the acronym ADAPT: Acceptance, Distraction, Activities, and Positive Thinking. The skills and teaching procedures are based on previous research on effective parenting skills and coping skills (e.g., Jaser et al., 2005; McMahon & Forehand, 2003). The monthly booster sessions, which occurred between the 2- and 6-month assessments, are designed to problem-solve difficulties with implementation of parenting skills and child coping skills at home, provide additional practice of skills, and support positive changes that have occurred. During sessions, parents and children meet together part of the time and separately part of the time. The FGCB intervention is similar in length to preventive interventions for family bereavement (12 sessions; Sandler et al., 2003) and children of divorce (11 sessions; Wolchik et al., 2000) that have shown long-term beneficial effects.
Treatment integrity
A detailed list of the content of each group intervention session was developed from the manual. Five individuals not involved in delivery of the intervention were trained to code for presence versus absence of each content area or strategy of the intervention for each session. Intervention sessions were audio recorded, and 20% were randomly selected for fidelity coding. The ratio of the number of checklist items covered during the sessions relative to the number of items that should have been covered was 92%. Reliability across coders was calculated for 31% of the sessions that were coded and yielded 93% agreement.
Written information condition
The Written Information (WI) comparison condition was modeled after a self-study program used successfully by Wolchik et al. (2000) in their preventive intervention trial for families coping with parental divorce and the lecture information condition used by Beardslee et al. (2007) in their preventive intervention for families coping with parental depression. Families were mailed three separate sets of written materials to provide education about the nature of depression, the effects of parental depression on families, and signs of depression in children (see Compas et al., 2009, for more details).
Data Analytic Approach
Analyses of symptom measures: Three-level partially-nested multivariate multilevel model
We used a similar data analytic approach as employed by Compas et al. (2009, 2011) to test for the effects of the FGCB intervention within a partially nested design. Compas et al. (2009, 2011) reported on the 2-, 6-, 12-,18-, and 24-month outcomes after baseline using only one randomly selected child per family (n = 111). Here we present analyses of the effects of the intervention at all of these time points using a larger sample of 180 families, including all children per family (n = 242), followed through 24 months.
The current study involves a three-level partially-nested design. In both conditions, children (level 1 units) are nested within families (level 2 units). The “partial nesting” refers to the fact that families are further nested within 23 FGCB intervention groups (level 3 units) in the FGCB intervention arm, but not in the WI comparison arm. Thus, families are independent (non-nested) in the WI comparison arm. In partial nesting designs the presence or absence of some clustering is systematically paired with a covariate (here, intervention), and different model-implied variances are anticipated in the nested vs. non-nested arms. To accommodate the dependencies generated by this design, univariate (Bauer, Sterba, & Hallfors, 2008) and multivariate (Compas et al., 2009, 2011) partially-nested multilevel models have been developed. We used a three-level multivariate version of the partially-nested multilevel model to test the effect of Condition (FGCB vs. WI) on outcomes at the 2-, 6-, 12-, 18-, and 24-month follow-ups, treating the baseline (time 1) measure of the outcome as a global covariate. We used a random intercept at the family-level to account for dependency of children within family. We also used a random effect only in the intervention arm (see Bauer et al., 2008 for procedures) at the FGCB intervention group level to account for partial nesting. We had planned to compare the fit of alternative child-level residual (co-)variance structures (allowing heterogeneity across time, condition, or both) using likelihood ratio tests (LRTs); however, only the model allowing residual heterogeneity across time but not condition could be fit without estimation problems. Hence, we retained this specification, which had also proved to be optimal using LRTs in our previous analyses (Compas et al., 2009, 2011).
Using an intent-to-treat approach, we fit all models with SAS 9.3 Proc Mixed and restricted maximum likelihood estimation (i.e., method = REML), which allows missing outcomes under missing-at-random assumptions and can provides less biased estimates of the variance components when the number of groups is small. We also stipulated ddfm = kr, which requests the computation of standard errors using the Kacker and Harville (1984) approximation and the computation of degrees of freedom using Kenward and Rogers (1997) method, as recommended by Bauer et al. (2008) due to the complex covariance structure. Similar to analyses reported by Compas et al. (2009, 2011), all tests were two-tailed unless otherwise noted.
Analyses of moderator effects
The same three-level partially-nested multivariate multilevel model was used in tests of moderation. All moderators were included simultaneously in the model. At each timepoint, a conditional main effect for the Moderator, and for Condition, were specified along with an interaction of Condition × Moderator. These conditional main effects and interaction effects were allowed to differ at each timepoint to account for any interactions with time. Significant interactions were followed with region of significance analyses designed to reveal the range of scores on the moderator variable for which the interaction is significant (Aiken & West, 1991; Dearing & Hamilton, 2006; and using Preacher, Curran, & Bauer's, 2006, online interaction utility).
Analyses of diagnostic measure
The categorical outcome (DSM-IV diagnosis on the K-SADS) was analyzed using Chi-square, odds ratio (odds of a diagnosis in the WI comparison group relative to the odds of a diagnosis in the FGCB intervention group), and Kaplan-Meier survival analyses.
Results
Preliminary Analyses
Several preliminary analyses were conducted prior to the three-level partially-nested multivariate multilevel models to test the primary hypotheses. First, for families randomized to the FGCB intervention, the number of group sessions attended or made up after an absence ranged from 0 to 12, with a mean of 8.2 sessions. For those who attended at least 1 session, the mean number of sessions attended or made up after an absence was 10.0 sessions.
Second, we compared families assigned to the FGCB intervention and to the WI condition on several variables at baseline. The percentage of parents currently in an episode of MDD was comparable for the two conditions (24% of parents in the FGCB intervention and 29% of parents in the WI comparison condition; chi-square non-significant). Although the CES-D was not used as part of the inclusion-exclusion criteria, the percentage of children exceeding the cut-off of 16 on the CES-D for elevated depressive symptoms was also comparable for the two conditions (27% of those assigned to the FGCB intervention and 35% of those assigned to the WI comparison condition; chi-square non-significant). Eighty-nine percent of those in the intervention and 80% of those in the WI comparison condition had no prior history of MDD FGCB (χ2 = 4.08, p = .043).
Third, because not all parents and children provided complete data at all five time points, a variable reflecting the amount of missing data was derived and participants assigned to the FGCB intervention and the WI comparison condition were compared on this variable. The amount of missing data (i.e., missing data at none, one, two, three, four or five of the follow-up assessments) did not differ between families assigned to the FGCB condition vs. WI condition.
Fourth, although raw scores were utilized in analyses to maximize variance and to be consistent with Compas et al. (2011), T scores on the YSR and CBCL scales at baseline were examined to provide a normative reference point for our sample (Achenbach & Rescorla, 2001). Mean T scores on the YSR and CBCL were, respectively, 56.3 and 59.9 for Anxiety/Depression, 54.2 and 59.0 for Internalizing, and 49.5 and 54.5 for Externalizing. The percent of children in the clinical range on Anxiety/Depression (i.e., T score > 70) was 7.3% on the YSR and 15.4% on the CBCL (based on normative data, 2% would be expected to exceed this cut-off). The percent in the clinical range on the Internalizing scale (i.e., T score > 63) was 23.2% on the YSR and 43.6% on the CBCL; for the Externalizing scale, 9.4% on the YSR and 22.6% on the CBCL (10% would be expected to exceed this cut-off based on normative data). These scores are similar to those reported for children of depressed parents in other studies, including the STAR*D trial (Foster et al., 2008). These data indicate that, as expected, this is an at-risk sample as reflected by moderately elevated mean T scores and the portion of the sample in the clinical range (2 to 4 times greater than would be expected based on the norms for most scales).
Finally, since families that were randomly assigned to the FGCB intervention met in groups of 4 families, we compared family groups on the outcome measures at baseline to ensure they were equivalent. A series of ANOVAs were run. The family groups did not differ significantly on any of the outcome measures at baseline except the CBCL anxious/depressed scales, F (22, 95) = 1.87, p = .02, and the BDI-II, F (22, 96) = 2.14, p = .006.
Analyses of Intervention Effects: Child Outcomes
Overview
Table 1 presents the Type 3 fixed effects of Intercept, Time 1 covariate, and Condition on each of the seven outcome variables at 2-, 6-, 12-, 18- and 24-months after baseline. As expected, the baseline covariate was a significant predictor of the outcome in most of the analyses. The tests of primary interest were the main effects of Condition on each outcome variable, controlling for the baseline score of the same outcome. The findings, delineated in detail below using conservative two-tailed tests, yielded a total of 13 significant effects.1 The FGCB intervention was more effective than the WI condition on one of the seven measures at 2-months (CBCL Internalizing), two of the seven measures at 6-months (YSR Anxiety/Depression and YSR Externalizing), four of the seven measures at 12-months (CES-D, YSR Anxiety/Depression, YSR Internalizing, YSR Externalizing), three of the seven measures at 18-months (YSR Anxiety/Depression, YSR Internalizing, YSR Externalizing), and three of the seven measures at 24-months (CES-D, YSR Anxiety/Depression, YSR Externalizing).
Table 1.
Type 3 Fixed Effects of Intercept, Condition, and the Time 1 Covariate on Each Outcome Variable
| 2 Months | 6 Months | 12 Months | 18 Months | 24 Months | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Effect | df | F | p< | df | F | p< | df | F | p< | df | F | p< | df | F | p< |
| DV = CES-D | |||||||||||||||
| Intercept | 1, 254 | 64.02 | .001 | 1, 262 | 74.84 | .001 | 1, 232 | 68.75 | .001 | 1, 216 | 61.51 | .001 | 1, 235 | 83.83 | .001 |
| Baseline (covariate) | 1, 214 | 18.51 | .001 | 1, 222 | 2.78 | .096 | 1, 207 | 0.96 | .329 | 1, 175 | 2.60 | .109 | 1, 187 | .39 | .532 |
| Condition | 1, 133 | 0.61 | .435 | 1, 225 | 2.04 | .154 | 1, 191 | 4.33 | .039 | 1, 113 | 0.95 | .333 | 1, 218 | 4.07 | .045 |
| DV = YSR Anxiety/Depression | |||||||||||||||
| Intercept | 1, 234 | 29.12 | .001 | 1, 246 | 50.84 | .001 | 1, 244 | 52.14 | .001 | 1, 225 | 56.89 | .001 | 1, 232 | 55.41 | .001 |
| Baseline (covariate) | 1, 204 | 79.10 | .001 | 1, 222 | 36.38 | .001 | 1, 199 | 16.87 | .001 | 1, 176 | 11.54 | .001 | 1, 173 | 7.58 | .007 |
| Condition | 1, 213 | 3.10 | .080 | 1, 107 | 9.49 | .003 | 1, 234 | 8.98 | .003 | 1, 216 | 8.83 | .003 | 1, 234 | 4.75 | .030 |
| DV = CBCL Anxiety/Depression | |||||||||||||||
| Intercept | 1, 245 | 16.07 | .001 | 1, 243 | 7.74 | .006 | 1, 273 | 23.34 | .001 | 1, 239 | 16.16 | .001 | 1, 248 | 13.48 | .001 |
| Baseline (covariate) | 1, 213 111.33 | .001 | 1, 207 | 140.58 | .001 | 1, 205 | 79.74 | .001 | 1, 198 | 66.66 | .001 | 1, 200 | 72.82 | .001 | |
| Condition | 1, 101 | 3.11 | .081 | 1, 97 | 1.38 | .243 | 1, 261 | 3.27 | .072 | 1, 101 | 1.54 | .217 | 1, 238 | 1.67 | .198 |
| DV = YSR Internalizing | |||||||||||||||
| Intercept | 1, 255 | 46.04 | .001 | 1, 275 | 71.30 | .001 | 1, 272 | 69.17 | .001 | 1, 261 | 76.85 | .001 | 1, 250 | 68.12 | .001 |
| Baseline (covariate) | 1, 225 | 44.07 | .001 | 1, 245 | 22.75 | .001 | 1, 220 | 10.06 | .002 | 1, 201 | 6.50 | .012 | 1, 195 | 4.80 | .030 |
| Condition | 1, 226 | 1.49 | .224 | 1, 138 | 4.88 | .029 | 1, 245 | 4.88 | .003 | 1, 231 | 8.09 | .005 | 1, 231 | 1.60 | .207 |
| DV = CBCL Internalizing | |||||||||||||||
| Intercept | 1, 255 | 23.25 | .001 | 1, 255 | 23.30 | .001 | 1, 287 | 37.89 | .001 | 1, 233 | 27.58 | .001 | 1, 239 20.81 | .001 | |
| Baseline (covariate) | 1, 220 | 87.93 | .001 | 1, 225 | 76.80 | .001 | 1, 221 | 46.29 | .001 | 1, 188 | 36.92 | .001 | 1, 194 41.11 | .001 | |
| Condition | 1, 119 | 3.93 | .050 | 1, 100 | 1.43 | .235 | 1, 261 | 3.53 | .062 | 1, 78 | 2.43 | .123 | 1, 98 | 1.11 | .294 |
| DV = YSR Externalizing | |||||||||||||||
| Intercept | 1, 241 | 16.75 | .001 | 1, 253 | 51.28 | .001 | 1, 261 | 48.22 | .001 | 1, 225 | 54.61 | .001 | 1, 221 | 53.15 | .001 |
| Baseline (covariate) | 1, 202 142.80 .001 | 1, 216 | 45.84 | .001 | 1, 192 | 66.22 | .001 | 1, 169 | 51.32 | .001 | 1, 175 | 38.39 | .001 | ||
| Condition | 1, 220 | 0.11 | .745 | 1, 229 | 2.51 | .114 | 1, 247 | 6.14 | .014 | 1, 229 | 11.29 | .001 | 1, 230 | 4.78 | .030 |
| DV = CBCL Externalizing | |||||||||||||||
| Intercept | 1, 267 | 21.38 | .001 | 1, 261 | 18.16 | .001 | 1, 278 | 15.22 | .001 | 1, 266 | 16.15 | .001 | 1, 269 | 15.93 | .001 |
| Baseline (covariate) | 1, 244 | 128.64 | .001 | 1, 249 | 167.71 | .001 | 1, 235 | 147.70 | .001 | 1, 220 | 116.60 | .001 | 1, 226 | 104.00 | .001 |
| Condition | 1, 242 | 1.81 | .180 | 1, 217 | 1.78 | .184 | 1, 251 | 0.75 | .389 | 1, 252 | 2.37 | .125 | 1, 240 | .70 | .402 |
Notes. Degrees of freedom are estimated using the Kenward-Rogers (1997) method, as discussed in the text. This is why degrees of freedom can take on non-integer values.
Table 2 provides means and standard deviations for all of the continuous child outcome variables at each time point, the significance of the effect of the intervention on the dependent variable at each time point, and the effect size (Cohen's d). Significant effects ranged from d = .22 to .45 which reflect small to approaching medium effects. Three effects on the CBCL approached significance (p < .10) and ranged in magnitude from .27 to .30.
Table 2.
Means and Effect Sizes for Each Outcome Variable at Each Time Point
| Baseline | 2 Months | 6 Months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Means | Means | Means | ||||||||||
| Outcome | FGCB | WI | Pooled SD | Cohen's d | FGCB | WI | Pooled SD | Cohen's d | FGCB | WI. | Pooled SD | Cohen's d |
| CES-D | 12.86 | 14.23 | 10.55 | −0.13 | 12.55 | 13.17 | 9.86 | −0.06 | 10.43 | 11.78 | 9.34 | −0.14 |
| YSR Anxiety/Depression | 5.26 | 5.23 | 4.53 | 0.01 | 3.78 | 4.66 | 3.52 | −0.25† | 2.89 | 4.42 | 3.41 | −0.45** |
| CBCL Anxiety/Depression | 5.81 | 5.68 | 4.11 | 0.03 | 3.92 | 4.97 | 3.55 | −0.30† | 3.66 | 4.42 | 3.29 | −0.23 |
| YSR Internalizing | 13.85 | 13.85 | 9.44 | 0.15 | 9.56 | 11.14 | 7.47 | −0.21 | 7.70 | 10.39 | 7.50 | −0.36* |
| CBCL Internalizing | 11.86 | 10.96 | 7.56 | 0.12 | 7.60 | 9.79 | 6.59 | −0.33* | 7.04 | 8.53 | 6.04 | −0.25 |
| YSR Externalizing | 9.47 | 9.39 | 7.11 | 0.01 | 8.13 | 8.14 | 5.52 | 0.00 | 7.06 | 8.24 | 5.79 | −0.20 |
| CBCL Externalizing | 10.73 | 8.80 | 8.10 | 0.24 | 6.60 | 8.10 | 6.05 | −0.25 | 5.98 | 7.42 | 5.58* | −0.26 |
| 12 Months | 18 Months | 24 Months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Means | Means | Means | ||||||||||
| Outcome | FGCB | WI | Pooled SD | Cohen's d | FGCB | WI | Pooled SD | Cohen's d | FGCB | WI | Pooled SD | Cohen's d |
| CES-D | 8.01 | 10.19 | 8.45 | −0.26* | 10.42 | 11.44 | 10.97 | −0.04 | 8.48 | 10.53 | 9.37 | −0.22* |
| YSR Anxiety/Depression | 3.01 | 4.67 | 4.08 | −0.41** | 2.78 | 4.26 | 3.87 | −0.38** | 3.42 | 4.57 | 4.33 | −0.27* |
| CBCL Anxiety/Depression | 3.36 | 4.31 | 3.53 | −0.27† | 3.30 | 4.11 | 3.70 | −0.21 | 3.16 | 3.94 | 3.33 | −0.23 |
| YSR Internalizing | 7.15 | 10.87 | 8.70 | −0.43** | 6.45 | 9.78 | 7.99 | −0.39** | 8.25 | 9.83 | 8.28 | −0.19 |
| CBCL Internalizing | 6.67 | 8.59 | 6.72 | −0.28† | 6.85 | 9.11 | 7.79 | −0.26 | 6.74 | 8.29 | 6.70 | −0.23 |
| YSR Externalizing | 6.81 | 8.69 | 6.46 | −0.29* | 6.62 | 9.31 | 6.42 | −0.41*** | 7.96 | 9.94 | 7.19 | −0.28* |
| CBCL Externalizing | 6.62 | 7.61 | 6.28 | −0.16 | 6.00 | 7.84 | 6.63 | −0.25 | 5.90 | 7.08 | 5.87 | −0.20 |
Note. FGCB = Family Group Cognitive Behavioral Intervention Group; WI = Written Information Comparison Condition.
p < .10
p < .05
p < .01
Child depressive and internalizing symptoms
We assessed three levels of internalizing symptoms: child reported depressive symptoms (CES-D), child and parent reported anxiety/depression symptoms (YSR & CBCL syndrome scales), and child and parent reported internalizing problems (YSR & CBCL broadband scales; see Tables 2 and 3). For the CES-D, the main effect of Condition was significant at 12- and 24-months. For anxiety/depression symptoms, the main effect of Condition was significant for the YSR Anxiety/Depression scale at 6-, 12-, 18-, and 24-months; effects on the CBCL Anxiety/Depression scale were not significant at any time point but approached significance (p < .10) at 2- and 12-months. In analyses of the Internalizing scales, the Condition effect was significant on the YSR Internalizing scale at 6-, 12- and 18-months; effects on the CBCL Internalizing scale were significant at 2-months, approached significance (p < .10) at 12 months, but were not significant at the other three time points.
Table 3.
Summary of tests of moderation.
| 2 Months | 6 Months | 12 Months | 18 Months | 24 Months | |
|---|---|---|---|---|---|
| Moderators | |||||
| Child Age | Yes (1/7)a | Yes (1/7)a | No (0/7) | Yes (1/7)d | Yes (1/7)c |
| Child Gender | No (0/7) | No (0/7) | Yes (1/7)d | Yes (1/7)d | No (0/7) |
| Parent BDI-II | No (0/7) | No (0/7) | No (0/7) | No (0/7) | No (0/7) |
| Parent MDE | No (0/7) | No (0/7) | No (0/7) | No (0/7) | No (0/7) |
| Parental Education | Yes (1/7)b | No (0/7) | Yes (1/7)b | No (0/7) | No (0/7) |
Note. The number of significant moderators found for the seven dependent variables is indicated at each time point.
Center for Epidemiologic Studies-Depression
Youth Self-Report Externalizing.
Child Behavior Checklist Internalizing.
Child Behavior Checklist Externalizing.
Child externalizing problems
Externalizing problem behaviors were assessed by parent and child report at a broadband level (YSR & CBCL Externalizing problems; see Tables 2 and 3). For the YSR Externalizing scale, there were significant effects for Condition at 12-,18-, and 24-months. On the CBCL Externalizing scale, the effect for Condition was not significant at any of the time points.
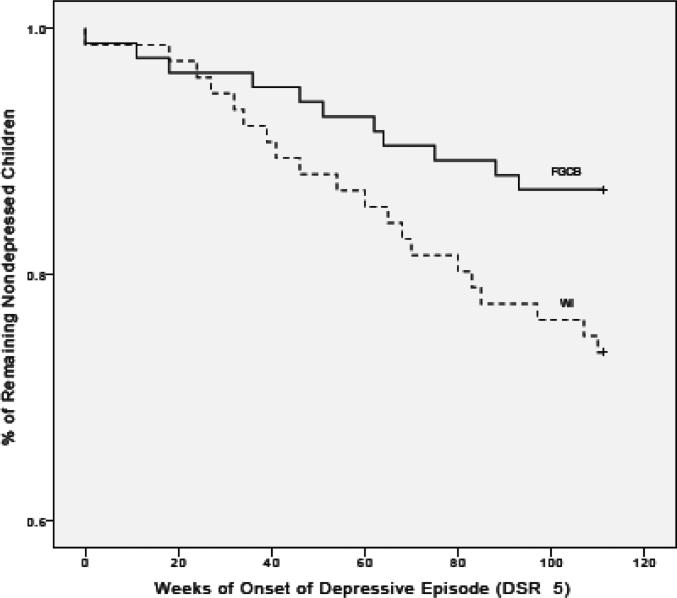
Child DSM-IV diagnosis
Child diagnosis of MDD was assessed on the K-SADS at baseline, 6-, 12-, and 24-months. Child and parent reports on the K-SADS at each time point were combined by how to determine the number of children who met criteria for an episode of MDD and for any non-mood DSM disorder during the baseline to 24-month follow-up period. Odds ratios, chi-square analyses, and Kaplan-Meier survival analyses (Mantel-Cox log rank and Generalized Wilcoxon analyses) were utilized to analyze for child MDD diagnosis (see Figure 2). Based on parent and child interviews, the percentage of children in the FGCB intervention who experienced an episode of MDD from baseline to 24-months was 13.1% compared to 26.3% of children who experienced an episode of MDD in the WI condition. This resulted in an odds ratio of 2.37, 95% CI = 1.05 to 5.35, and the chi-square test was significant, χ2 (1) = 4.46, p = .035. Using a formula developed by Chinn (2000) to convert odds-ratios to effect sizes, the effect size for the MDD odds-ratio was 1.31, equivalent to a large effect. The duration of major depressive episodes did not differ for those children in the FGCB intervention (mean duration = 13.09 weeks, SD = 11.78; however, mean = 9.9, SD = 5.54, when one extreme outlier with a duration of 45 weeks was removed) as compared with those in the WI comparison condition (mean duration = 9.55 weeks, SD = 7.43). Because of a higher rate of a history of previous MDD in children assigned to the WI vs. the FGCB condition, we examined depressive episodes over 24-months as a function of condition and prior history and the effect of prior history was not significant, χ2 (3) = 5.75, p = .124.
Figure 2.
Kaplan-Meier survival analyses of major depression in children in Family Group Cognitive-Behavioral Preventive Intervention vs. Written Information Condition.
Although there is not a standard approach to accounting for partial nesting in analyses of categorical data, we conducted supplemental analyses with a three-level binary logistic regression as a way to account for nesting in family and partial nesting in the FGCB condition. This multilevel model was run using two different estimators because for categorical outcomes multilevel models results can be sensitive to estimation method (see Bauer & Sterba, 2011). Using a maximum pseudo-likelihood expansion around random effect model the OR = 2.34 (95% CI = 0.99, 5.50), χ2 (1) = 3.83, p = 0.0503. Using a maximum pseudo-likelihood expansion around fixed effect mode the OR = 2.33 (95% CI= 0.99, 5.48) χ2 (1) = 3.85, p = 0.0499.
Moderator Analyses
Five possible moderators (child age, child gender, parent BDI-II score as baseline, parent MDE status at baseline, and parental education) were tested on each of the seven continuous child outcome measures (CES-D, YSR and CBCL anxiety/depression, internalizing, and externalizing) at each of the five time points (2-, 6-, 12-, 18-, and 24-months after baseline; see Table 3 for a summary of these analyses). The five moderators were tested together for each child outcome measure at each time point. Only eight of the 175 (4.5%) tests of moderation were significant: four effects for age, two effects for gender, and two effects for parental education (see Table 3 for a summary of these analyses). There were no significant moderator effects for parent BDI-II or MDE baseline status on any of the seven child mental health measures at any of the five follow-up assessments. Although there was evidence of child age as a moderator at four of the five follow-up assessments, the effect was significant on only one of the seven measures of child mental health at each of these time points (i.e., CES-D at 2- and 6-months, CBCL internalizing at 18-months, and CBCL externalizing at 24-months). Thus, only four out of 35 tests of child age were significant and the direction of effect was stronger for older vs. younger children. Effects were found for child gender only on the CBCL externalizing scale at 12- and 18-months (i.e., two significant effects out of 35), and for parental education only on the YSR externalizing scale at 2- and 12-months (i.e., two significant tests out of 35). Further, none of the 70 tests of parental BDI-II scores at baseline or depression status at baseline based on the SCID as moderators of the effects of the intervention were significant. Because less than 5% of the interactions were significant and moderators did not interact with same outcome variables across assessments (e.g., age of child moderated different outcomes at 2, 18, & 24 months), it is plausible that the moderator effects may be nil in the population, and these findings simply represent sampling variability around 0.2 Note that a post hoc power analysis cannot shed light on our suspicion that the moderator effects are 0 in the population. Since power is defined as the probability of detecting an effect that exists at a specified level in the population, if an effect is 0, power cannot be calculated, only type I error could be calculated.3
Child diagnoses of MDD were further analyzed as a function of parental depression status at baseline (i.e., whether the parent was or was not in a depressive episode at baseline) in a 2 (FGCB vs. WI condition) X 2 (parent in depressive episode vs. not in episode) chi-square and the effect was not significant, χ2 (3) = 5.21, p = .15. Secondary, exploratory analyses of parental depression status at baseline and child depressive episodes over the subsequent 24-months suggested a potential effect. That is, although the overall 2 by 2 chi-square analysis of parental baseline depression status by group was not significant, when condition effects were examined separately as a function of parental depression status, there was a significant effect favoring the FGCB intervention (11% experienced at least one depressive episode) compared with the WI condition (27% with at least one episode) for children whose parents were not in a depressive episode at baseline. For children whose parents were in a depressive episode at baseline, however, the groups did not differ (20% of those in the FGCB as compared with 25% in the WI condition had a depressive episode over 24-months). However, because the overall chi-square was non-significant, these analyses should be viewed as exploratory.
Discussion
Evidence is accumulating to suggest that depression, particularly in at-risk children and adolescents, can be prevented (Beardslee et al., 2011; Cuijpers et al., 2012; Muñoz et al., 2012; Siegenthaler et al., 2012). However two important gaps have been identified. First, with some notable recent exceptions (e.g., Beardslee et al., 2013), support for the maintenance of prevention effects beyond 6- to 12-months has been scarce in previous studies (e.g., Merry et al., 2011; Muñoz et al.). Evidence of sustained effects over periods of at least one to two years is crucial to determine if interventions can actually reduce clinically relevant symptoms and reduce the incidence of MDD. And second, identifying for whom child depression prevention programs are most and least effective (i.e., moderation) is only beginning to be examined. The current study was designed to address these two issues.
Findings from this study provide some of the strongest evidence to date for the efficacy of a selected preventive intervention for at-risk offspring of depressed parents. Significant effects favoring the FGCB intervention as compared with the WI condition were found at multiple follow-ups, persisting over a period of 2-years on a wide range of internalizing and externalizing symptoms/problems. Specifically, at the 2-year follow-up participants in the FGCB program were significantly lower on self-report measures of depressive symptoms, mixed anxiety/depression, and externalizing problems. Further, only one significant effect was found immediately after completion of the acute phase of the intervention at 2-months, only two significant effects were found at completion of the booster sessions at 6-months, but four significant effects were found at the 12-month follow-up and three significant effects at each of the 18- and 24-month follow-ups. Consistent with what would be expected in a preventive intervention, effects of the FGCB program strengthened over time as families had more time to use the skills that were learned in the intervention. This is consistent with prior analyses that found changes in parenting skills and children's coping skills were significant mediators of subsequent effects of the FGCB intervention on children's symptoms (Compas et al., 2010). Moreover, based on diagnostic interviews with children and parents, children in the FGCB intervention were significantly less likely to experience an episode of MDD over the 2-year period. Thus, the FGCB intervention produced sustained effects in reducing the incidence of depressive episodes, depressive symptoms, other internalizing symptoms, and externalizing problems.
It is noteworthy that the significant effects were found on three of four child-report measures at both 18- and 24-months after baseline but none of the three parent-report measures at either of these follow-ups. In fact, only one significant effect (at 2-months) and three effects approaching significance (p < .10) (at 2- and12-months) were found for parent-reports on the CBCL. These findings are consistent with previous prevention trials with children of depressed parents that have also failed to find evidence of change on parent-report measures. For example, Clarke et al. (2001) also did not find significant effects on the CBCL at 24-months in their outcome study. Together these findings suggest that reports by parents with a history of MDD may be relatively less sensitive indicators of the effects of interventions for their children. There are four potential explanations for this finding based on the recent consideration of multiple informants’ reports by De Los Reyes, Thomas, Goodman, and Kundey (2013). First, relative to child self-report, parents observe children in fewer settings and, therefore, observe a smaller sample of behavior. Second, parental depressive symptoms may impose a ceiling on the extent to which parents report changes in children's emotional and behavioral problems, thus preventing differences from emerging between the intervention and comparison groups. Third, there may be measurement error in parent and/or child report, leading to discrepant outcomes for these reporters. The measurement error may be due to one or both reporters, or it may be restricted to the particular assessment instruments used in this study. Fourth, the effects of the intervention may have been more evident in the child's subjective mood and thoughts and less on observable behaviors. Regardless of which explanations offered above best fit our findings, low agreement among informants is frequent (see De Los Reyes et al.) and highlights the importance of having multiple reporters of outcome in prevention research.
The significant difference found on rates of depression as measured on the K-SADS provides strong evidence for the effects of the intervention in several ways. First, diagnoses of MDD on the K-SADS were based on the combination of parent and child reports, providing evidence that the effects of the FGCB intervention were not limited to only child self-reports. Second, evidence of a reduction of episodes of MDD provides a more stringent criterion than reliance only on questionnaires, as the criteria for an episode of MDD based on the K-SADS require the presence of the key symptoms of depression that have persisted for at least 1-week and are documented by clinical interviews. Third, survival analyses indicate that the difference in the onset of MDD was sustained over the full 24-month follow-up period. The onset of depressive episodes indicates a true prevention effect in that the WI condition continued to accumulate episodes of depression while the FBCB group did so at a much lower rate (Horowitz & Garber, 2006).
The current study also provided tests of possible moderators of the FGCB intervention at the child, parent, and family levels on all seven measures of child mental health at all five follow-up assessments. Contrary to recent meta-analyses (Merry et al., 2011; Stice et al., 2009), minimal evidence of moderation was found, as less than 5% of the tests of moderation were significant and these significant effects were relatively sporadic and did not reflect a cohesive pattern. In general, the analyses of potential moderators indicate that the effects of the FGCB were not qualified or contingent on any of several family, parent, or child factors. The intervention appears to be robust and equally effective for children who entered the program at ages 9 to 15 years old (and who were 11 to 17 years old at the 24-month follow-up), for boys and girls, for families of varying SES, and for children regardless of their parents’ initial levels of depression. Unlike Garber et al. (2009), with the exception of an exploratory analysis, we did not find evidence for parental depression status at baseline as a moderator of subsequent intervention effects. This may be because the Garber et al. study was an indicated intervention (children had a history of MDD or elevated depressive symptoms at baseline) and included only children in the intervention, whereas the current study was a selected intervention (no criteria were used regarding children's depression status or history) and included both a parent arm and a child arm in the intervention.
This study had several features that strengthen the overall implications of the findings. First, the sample is one of the largest enrolled in a prevention trial of at-risk children of depressed parents. Second, the FGCB intervention was compared with an active control condition in which parents and children were provided with information about depression and its effects on families, providing evidence that the parenting and children's coping skills taught in the intervention may play an active role in the positive effects. However, it is important to note that the current study did not control for increased attention and social support the FGCB intervention received relative to the WI condition. Third, reports of children's internalizing and externalizing symptoms and disorders were obtained from parents and children using well-established measures. Fourth, families were followed for 2 years, allowing for analyses of sustained effects beyond those reported in previous studies. Fifth, a comprehensive set of child, parent and family factors were tested as potential moderators and the absence of consistent effects suggests that the effects of the FGCB intervention are relatively robust.
The current study also had several limitations that can be addressed in future research. First, although representative of the two research sites, the sample was somewhat limited in diversity and future studies should test the effects of the FGCB intervention with more diverse samples. Second, even though the intervention maintained significant effects for 2-years, it is important to document prevention effects over even longer periods of time. Third, although multiple informants (parent, child, interviewer) provided data, other independent sources data (e.g., behavioral observations, teachers) would strengthen the findings. Fourth, although fathers were included, the vast majority of parents were mothers, limiting conclusions that can be reached about fathers and differential effects of mothers versus fathers. Fifth, our efforts to blind the interviewers involved not informing them of the participants’ condition; however, we did not assess the success of the “blinding.” Sixth, multiple outcomes were examined at multiple time points, which could have led to some significant findings emerging by chance. Seventh, we did not assess the extent to which families in the WI comparison condition read the material presented to them. Finally, the FGCB and WI groups did not differ significantly on the demographic variables and whether parents were in a current episode of depression; however, a small, but significant, group difference was evident on past history of MDD.
In conclusion, the current study provides additional evidence to the growing literature on the promise of our ability to prevent psychiatric symptoms and disorder in high-risk offspring of depressed parents. The field is now poised to begin to bring interventions to scale and to integrate them with comprehensive approaches to mental health care for children and parents. Future research with the FGCB intervention tested here is needed to establish the effectiveness of this program with more diverse samples of families coping with parental depression. For example, the current sample of parents was relatively well educated. The skills taught to both parents and children were discrete behavioral ones that were delivered through didactics, modeling, and role playing and generalized outside of the group setting through weekly homework. Work with other samples suggests that these techniques can be effective with less educated samples (see McMahon & Forehand, 2003); however, demonstration of such effectiveness will be critical with programs such as FGCB. The current efficacy trial serves as a first step toward demonstrating that FGCB is a promising intervention.
Public Health Significance Statement.
This study provides strong support for the efficacy of a family group cognitive-behavioral preventive intervention for children of parents with a history of major depressive disorder. The intervention led to reduced internalizing and externalizing symptoms and prevented the onset of major depression over a period of 2 years.
Acknowledgments
This research was supported by grants R01MH069940 and R01MH069928 from the National Institute of Mental Health and by gifts from Patricia and Rodes Hart and from the children of Heinz and Rowena Ansbacher.
The authors are grateful to MJ Merchant, Diana Apostle, Nicole Coffelt, Mary Jo Coiro, Madeleine Dunn, Christina Grice, Sheryl Margolis, Erin Roland, Lauren Simmons, Darlene Whetsel, Lori Roberts, Mi Wu, Mary Ellen Copeland, and Katelyn Watkins for their many contributions to this project.
Footnotes
Although we used the conservative approach of employing two-tailed in all analyses, we also took the additional step of conducting supplemental analyses using the False Discovery Rate (FDR; Benjamini & Hochberg, 2000) to control for multiple comparisons. Originally, 13/35 of the tests were significant, using the standard alpha of .05. Using the FDR, 6/35 effects were significant. The p-values for the tests of the treatment effect in Table 1 that were still significant using an adjusted alpha were for YSR anxiety/depression at 6 (p < .001), 12 (p < .003), 18 (p < .003), and 24 months (p < .003), and for YSR internalizing at 12 months (p < .003) and for YSR externalizing at 18 months (p < .005).
Additional information on statistical power for the moderator effects can be obtained based on estimates of precision; i.e., the variability of our moderator effect estimates across repeated samples. We have calculated confidence intervals for our moderation effects based on the sum of the estimate of the moderator effect plus the critical z value (1.96) times the standard error of the estimate. These values for each of the 5 moderators at each of the 5 follow-up data points are available from the authors on request.
It is possible that baseline levels of child depression symptoms, anxiety/depression, and internalizing and externalizing symptoms may moderate the effects of the intervention. However, we did not hypothesize these effects and testing all of the possible moderation effects for baseline levels of symptoms would add 245 additional moderator analyses. Although the possibility that baseline levels of child symptoms may moderate the effects of the GFCB intervention is interesting, we could not include the large number additional analyses. However, we conducted exploratory analyses using CES-D scores as a measure of child depressive symptoms as a moderator of the effects of the intervention only on CES-D as an outcome. The interaction of baseline CES-D by group was only significant at time points 2 and 4, and not significant at times 3, 5, and 6. At time 2, t = (191) = 2.17, p = .031; and at time 4, t (182) = −.259, p = .010. In both cases, the effects of the FGCB intervention was stronger for those with higher baseline CES-D symptoms.
References
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms and Profiles. University of Vermont, Research Center for Children, Youth, and Families; Burlington, VT: 2001. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage Publications; Thousand Oaks, CA: 1991. [Google Scholar]
- Bauer DJ, Sterba SK. Fitting multilevel models with ordinal outcomes: Performance of alternative specifications and methods of estimation. Psychological Methods. 2011;16:373–390. doi: 10.1037/a0025813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer DJ, Sterba SK, Halfors DD. Evaluating group-based interventions when control participants are ungrouped. Multivariate Behavioral Research. 2008;43:210–236. doi: 10.1080/00273170802034810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Brent DA, Weersing R, Clarke GN, Porter G, Hollon SD, Garber J. Prevention of depression in at-risk adolescents longer-term effects. JAMA: Psychiatry. 2013;295:2650–2657. doi: 10.1001/jamapsychiatry.2013.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Wright EJ, Gladstone TRG, Forbes P. Long-term effects from a randomized trial of two public health preventive interventions for parental depression. Journal of Family Psychology. 2007;21:703–713. doi: 10.1037/0893-3200.21.4.703. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Gladstone TRG, O’Connor EE. Transmission and prevention of mood disorders among children of affectively ill parents: A review. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:1098–1109. doi: 10.1016/j.jaac.2011.07.020. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer R,A, Ball R, Ranieri WF. Comparison of Beck Depression Inventories 1A and II in psychiatric outpatients. Journal of Personality Assessment. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. On the adaptive control of the false discovery rate in multiple testing with independent statistics. Journal of Educational and Behavioral Statistics. 2000;25:60–83. [Google Scholar]
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics in Medicine. 2000;19:3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::aid-sim784>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Seeley J. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Archives of General Psychiatry. 2001;58:1127–1134. doi: 10.1001/archpsyc.58.12.1127. [DOI] [PubMed] [Google Scholar]
- Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Roberts L. Coping and parenting: Mediators of 12-month outcomes of a family group cognitive–behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology. 2010;78:623–634. doi: 10.1037/a0020459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Forehand R, Keller G. Prevention of depression in families of depressed parents. In: Strauman T, Costanzo PR, Garber J, editors. Prevention of depression in adolescent girls. Duke University Press; 2011. pp. 318–339. [Google Scholar]
- Compas BE, Forehand R, Keller G, Champion JE, Reeslund KL, Cole DA. Randomized clinical trial of a family cognitive-behavioral preventive intervention for children of depressed parents. Journal of Consulting and Clinical Psychology. 2009;77:1007–1020. doi: 10.1037/a0016930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Forehand R, Thigpen JC, Keller G, Hardcastle EJ, Roberts L. Family group cognitive-behavioral preventive intervention for families of depressed parents: 18- and 24-month outcomes. Journal of Consulting and Clinical Psychology. 2011;79:488–499. doi: 10.1037/a0024254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Beekman ATF, Reynolds CF. Preventing depression: A global priority. JAMA. 2012;307:1033–1034. doi: 10.1001/jama.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearing E, Hamilton LC, McCartney K, Burchinal MR, Bub KL. Contemporary advances and classic advice for analyzing mediating and moderating variables. Monographs of the Society for Research in Child Development. 2006;71(3):88–104. doi: 10.1111/j.1540-5834.2006.07103001.x. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas SA, Goodman KL, Kundey SMA. Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology. 2013;9:123–149. doi: 10.1146/annurev-clinpsy-050212-185617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M.l., Williams JBW. Structured clinical interview for DSM-IV Axis I disorders -- Non-patient edition. New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Foster CE, Webster MC, Weissman MM, Pilowsky DJ, Wickramarante PJ, Talati A, King CA. Remission of maternal depression: Relations to family functioning and youth internalizing and externalizing symptoms. Journal of Clinical Child and Adolescent Psychology. 2008;37:714–724. doi: 10.1080/15374410802359726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Clarke G, Weersing VR, Beardslee WR, Brent D, Iyengar S. Prevention of depression in at-risk children: A randomized controlled trial. JAMA. 2009;301:2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hoffman LW. Methodological issues in studies of SES, parenting, and child development. In: Bornstein MH, Bradley RH, editors. Socioeconomic status, parenting, and child development. Lawrence Erlbaum; Mahuah, N.J.: 2003. [Google Scholar]
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- Kacker RN, Harville DA. Approximations for standard errors of estimators of fixed and random effects in mixed linear models. Journal of the American Statistical Association. 1984;79:853–862. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School Aged Children: Present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Evidence-based treatment and practice: New opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. American Psychologist. 2008;63:146–159. doi: 10.1037/0003-066X.63.3.146. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kenward MG, Rogers JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. [PubMed] [Google Scholar]
- Kessler RC, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication Survey (NCS-R). JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Lundahl B, Risser HJ, Lovejoy MC. A meta-analysis of parent training: Moderators and follow-up effects. Clinical Psychology Review. 2006;26:86–104. doi: 10.1016/j.cpr.2005.07.004. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon RJ, Forehand R. Helping the noncompliant child: Family-based treatment for oppositional behavior. 2nd ed. Guilford Press; New York, NY: 2003. [Google Scholar]
- Merry SN, Helrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H. Psychological and educational interventions for preventing depression in children and adolescents. Cochrane Database Systematic Review. 2011;2011;12:CD003380. doi: 10.1002/14651858.CD003380.pub3. [DOI] [PubMed] [Google Scholar]
- Muñoz RF, Beardslee WR, Leykin Y. Major depression can be prevented. American Psychologist. 2012;67:285–295. doi: 10.1037/a0027666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NRC/IOM . In: Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. England MJ, Sim LJ, editors. The National Academies Press; Washington, DC: 2009. 2009. [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in linear regression, multilevel modeling, and latent curve analyses. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in children and young adults. Journal of Youth and Adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problems – a meta-analytic review. Journal of Child Psychology and Psychiatry. 2006;47:99–111. doi: 10.1111/j.1469-7610.2005.01544.x. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: A comparison of depression scales. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Siegenthaler E, Munder T, Egger M. Effect of preventive interventions in mentally ill parents on the mental health of the offspring: Systematic review and meta-analysis. Journal of the American Academy of Child and Adolesent Psychiatry. 2012;51:8–17. doi: 10.1016/j.jaac.2011.10.018. [DOI] [PubMed] [Google Scholar]
- Steer RA, Brown GK, Beck AT, Sanderson WC. Mean Beck Depression Inventory-II scores by severity of major depressive disorder. Psychological Reports. 2001;88:1075–1076. doi: 10.2466/pr0.2001.88.3c.1075. [DOI] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rhode P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolchik SA, West SG, Sandler IN, Tein J-Y, Coatsworth D, Lengua L, Weiss L, Anderson ER, Greene SM, Griffin WA. An experimental evaluation of theory-based mother and mother-child programs for children of divorce. Journal of Consulting and Clinical Psychology. 2000;68:843–856. [PubMed] [Google Scholar]