Abstract
Introduction
GlycA is a novel inflammatory biomarker measured using nuclear magnetic resonance (NMR). Its NMR signal primarily represents glycosylated acute phase proteins. GlycA was associated with inflammation and development of cardiovascular disease in initially healthy women. We hypothesized that GlycA is a biomarker of disease activity and is associated with coronary artery atherosclerosis in patients with rheumatoid arthritis (RA).
Methods
We conducted a cross-sectional study of 166 patients with RA and 90 control subjects. GlycA was measured from an NMR signal originating from N-acetylglucosamine residues on circulating glycoproteins. The relationship between GlycA and RA disease activity (Disease Activity Score based on 28 joints (DAS28)) and coronary artery calcium score was determined.
Results
GlycA concentrations were higher in patients with RA (median (interquartile range): 398 μmol/L (348 to 473 μmol/L)) than control subjects (344 μmol/L (314 to 403 μmol/L) (P < 0.001). In RA, GlycA was strongly correlated with DAS28 based on erythrocyte sedimentation rate (DAS28-ESR) and DAS28 based on C-reactive protein (DAS28-CRP) and their components, including tender and swollen joint counts, global health score, ESR and CRP (all P < 0.001). The area under the receiver operating characteristic curve for GlycA’s ability to differentiate between patients with low versus moderate to high disease activity based on DAS28-CRP was 0.75 (95 % confidence interval (CI): 0.68, 0.83). For each quartile increase in GlycA, the odds of having coronary artery calcium increased by 48 % (95 % CI: 4 %, 111 %), independent of age, race and sex (P = 0.03).
Conclusion
GlycA is a novel inflammatory marker that may be useful for assessment of disease activity and is associated with coronary artery atherosclerosis in patients with RA.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disorder affecting nearly 1 % of the US population. Tight control of disease activity, including monitoring of acute-phase reactants, is important to reduce joint destruction and disability in RA [1]. Currently, many rheumatologists consider that monitoring an acute-phase reactant is standard of care in RA management [2]. Indeed, measurement of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) is incorporated into the Disease Activity Score based on 28 joints (DAS28) [3], the core set of RA disease activity measures proposed by the American College of Rheumatology [4] and the American College of Rheumatology/European League Against Rheumatism RA remission criteria [5].
The markers of inflammation most commonly used to assess RA disease activity—ESR and CRP—have disadvantages. For example, ESR is altered by non-inflammatory conditions such as chronic kidney disease [6], pregnancy, anemia, abnormal red blood cell shape or size, and serum protein concentrations [7]. Because some of these confounding influences are unrelated to RA disease activity, the current treat-to-target recommendations include cautions about the use of ESR for monitoring RA activity [2]. Furthermore, CRP exhibits high variability over time in patients without inflammatory diseases [8–10], potentially making it unreliable for assessment of RA disease activity at one time point. Moreover, both ESR and CRP increase with age [11], female sex [12, 13] and body mass index (BMI) [14–17]. Thus, an alternative marker of inflammation not affected by some of these factors would be useful for assessing RA disease activity.
GlycA is a nuclear magnetic resonance (NMR) signal derived from mobile N-acetyl methyl groups, specifically the N-acetylglucosamine and N-acetylgalactosamine moieties, on the carbohydrate side chains of glycosylated proteins [18–20]. GlycA can be measured in the NMR spectra acquired for the quantification of serum or plasma lipoprotein particle numbers [10]. The majority of circulating glycosylated proteins are acute-phase proteins [18], and the main contributors to the GlycA signal are α1-acid glycoprotein, α1-antitrypsin, haptoglobin, α1-antichymotrypsin and transferrin [10]. Glycosylated immunoglobulin is not a main contributor to the GlycA signal, however [10].
GlycA is emerging as a new marker of inflammation and cardiovascular (CV) risk. GlycA concentrations were associated with known inflammatory markers, such as CRP, interleukin-6 (IL-6) and fibrinogen in 5,537 participants of the Multi-Ethnic Study of Atherosclerosis [10]. Moreover, GlycA was associated with incident CV events. For example, for every 1 standard deviation (SD) increase in baseline GlycA concentration, there was a 34 % increased incidence of CV events within the first 6 years of follow-up, independent of traditional risk factors, in over 27,000 women from the Women’s Health Study [21]. Little is known about GlycA concentrations in RA. We hypothesized that GlycA is a marker of disease activity and CV risk in patients with RA.
Methods
Study population
We conducted a cross-sectional study that included 166 patients with RA and 90 control subjects from a cohort of patients extensively characterized for CV risk [22]. Recruitment and study procedures, as well as predictors of coronary atherosclerosis, in this cohort have been described previously [22–30]. All subjects were older than 18 years of age, and patients with RA fulfilled the 1987 American College of Rheumatology classification criteria for RA [31]. The RA and control groups were frequency-matched for age, race and sex, and control subjects did not have RA or other inflammatory disease. Patients with RA were identified from an early RA registry, Vanderbilt University Medical Center or local rheumatologist referral, or advertisement. Control subjects were recruited from patient acquaintances, advertisement or volunteer database. Consecutive eligible patients were enrolled. The study was approved by the Vanderbilt University Medical Center Institutional Review Board, and all subjects gave us their written informed consent to participate.
Clinical and laboratory data
Clinical information, laboratory measurements and coronary artery calcium scores were obtained as described previously [22]. Disease activity of RA was determined on the basis of the DAS28-ESR and DAS28-CRP [3]. Categories of disease activity based on the DAS28-ESR were defined as follows [32]: remission = DAS28 < 2.6, low = DAS28-ESR between 2.6 and 3.2, moderate = DAS28-ESR between 3.2 and 5.1, and high = DAS28-ESR >5.1. Categories of disease activity based on the DAS28-CRP were defined as follows [32]: remission = DAS28-CRP <2.3, low = DAS28-CRP between 2.3 and 2.7, moderate = DAS28-CRP between 2.7 and 4.1, and high = DAS28-CRP >4.1. Prevalent coronary artery disease was defined as a history of myocardial infarction; coronary procedure such as stenting, balloon angioplasty or coronary artery bypass surgery; or angina. Estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease Study formula [33]: eGFR (ml/min/1.73 m2) = 175 × (serum creatinine) − 1.154 × (age) − 0.203 × (0.742 if female) × (1.212 if African American).
ESR was measured at the Vanderbilt University Medical Center Clinical Laboratory, and high-sensitivity CRP was measured at the same laboratory or by enzyme-linked immunosorbent assay (ELISA) (EMD Millipore, Billerica MA, USA). Tumor necrosis factor α (TNFα) and IL-6 concentrations were measured by multiplex ELISA (EMD Millipore).
Larsen score measurement
The Larsen score was calculated in 92 patients with RA based on radiographs of the hands and feet as described previously [34]. The radiographs were obtained a median of 1.9 years (interquartile range (IQR): 1.1 to 2.7) prior to study enrollment and scored by a blinded single investigator (TS). Larsen score was quantified by assessing the damage to 20 joints (wrists, first to fifth metacarpophalangeal joints and second to fifth metatarsophalangeal joints), yielding a total score ranging from 0 to 100 [35, 36].
Coronary artery calcium score measurement
Coronary artery calcium scores were calculated by performing electron beam computed tomography with an Imatron C-150 scanner (GE Medical Systems/Imatron, South San Francisco, CA, USA), as previously described [22], and quantified in Agatston units [37].
GlycA measurement
NMR spectra were acquired from ethylenediaminetetraacetic acid plasma samples as previously described for the NMR LipoProfile (lipoprotein particle) test at LipoScience (Raleigh, NC, USA) [26, 38]. The NMR Profiler platform is comprised of a 9.4-T (400-MHz 1H frequency) spectrometer (Bruker BioSpin, Billerica, MA, USA) with an integrated fluidic sample delivery system. The GlycA signal was quantified using proprietary deconvolution software that uses a non-negative linear least squares algorithm to fit the experimental signal to individual spectral components, including proteins and lipoproteins as well as signals representing the GlycA NMR resonance [10]. GlycA concentrations were quantified from these spectra without knowledge of any subject characteristics. The intra-assay and inter-assay variabilities for GlycA measurement are 1.9 % and 2.6 %, respectively [10].
Statistics
On the basis of a fixed sample size of 166 patients with RA and 90 control subjects and the SD of GlycA 57 μmol/L in control subjects, our study had 90 % power to detect a difference of approximately 25 μmol/L GlycA concentration between RA and control subjects. On the basis of the Women’s Health Study, a 1 SD increase in GlycA was independently associated with a 34 % increased rate of CV events within 6 years of follow-up [21]; thus, the study had sufficient power for us to detect a clinically meaningful difference in GlycA.
Descriptive statistics were calculated as medians with IQRs (25th to 75th percentiles) for continuous variables and as frequency and proportions for categorical variables. To compare variables between RA and control subjects, the Wilcoxon rank-sum test was used to compare continuous variables and the Pearson χ2 test was used to compare categorical variables. Correlation between GlycA concentrations and variables of interest was determined by Spearman correlation.
The ability of GlycA concentrations to differentiate between low and moderate to high disease activity, defined on the basis of the DAS28-ESR and DAS28-CRP values, was examined by calculating the area under the receiver operating characteristic (AUC) curve.
The association between quartiles of GlycA concentrations and presence of coronary artery calcium as well as presence of coronary artery disease was assessed by binary logistic regression. In these models, the presence of coronary artery calcium or a previous diagnosis of coronary artery disease was the dependent variable and GlycA was the independent variable. Separate analyses were performed, adjusting for age, race, and sex and adjusting for components of Framingham Risk Score, which we have termed traditional CV risk factors (age, sex, total cholesterol, high-density lipoprotein (HDL) cholesterol, smoking status, systolic blood pressure and anti-hypertensive use) [39], and then additionally for the presence of diabetes.
Data analysis was performed using IBM SPSS Statistics version 22 software (IBM, Armonk, NY, USA). Two-sided P-values <0.05 were considered statistically significant.
Results
Clinical characteristics
Patients with RA and control subjects were of similar age, race and sex (Table 1). In patients with RA, the median (IQR) DAS28-ESR and DAS28-CRP were 3.86 units (2.63 to 4.90 units) and 3.09 units (2.06 to 3.80 units), respectively. Patients with RA had higher CRP concentrations than control subjects (P < 0.001). The majority of patients with RA were taking methotrexate (71 %) and prednisone (54 %), and 20 % were taking an anti-TNFα agent (Table 1). Approximately 10 % of both RA and control subjects had known coronary artery disease, and coronary artery calcium was present in 52 % of patients with RA and 39 % of control subjects. GlycA concentrations were higher in patients with RA (median (IQR): 398 μmol/L (348 to 473 μmol/L)) compared with control subjects (344 μmol/L (314 to 403 μmol/L)) (P < 0.001) (Fig. 1).
Table 1.
Participant characteristicsa
| RA (n = 166) | Control (n = 90) | P-value | |
|---|---|---|---|
| Median age (IQR), yr | 54 (45 to 63) | 53 (44 to 60) | 0.38 |
| Caucasian race, n (%) | 147 (89) | 77 (86) | 0.55 |
| Female sex, n (%) | 114 (69) | 56 (62) | 0.30 |
| RF-positive, n (%) | 114 (72) | – | – |
| Median DAS28-ESR (IQR) | 3.86 (2.63–4.90) | – | – |
| Median DAS28-CRP (IQR) | 3.09 (2.06–3.80) | – | – |
| Tender joints, n (IQR) | 2 (0 to 7) | – | – |
| Swollen joints, n (IQR) | 3 (0 to 8) | – | – |
| Median CRP (IQR), mg/L | 4.0 (1.2 to 11) | 0.5 (0.2 to 1.5) | <0.001 |
| Median ESR (IQR), mm/hr | 15 (7 to 36) | – | – |
| Known CAD, n (%) | 17 (10) | 9 (10) | 0.95 |
| Coronary artery calcium, n (%) | 83 (52) | 34 (39) | 0.05 |
| Coronary calcium score, Agatston units | 2.7 (0 to 178.7) | 0 (0 to 19.2) | 0.02 |
| Methotrexate use, n (%) | 118 (71) | – | – |
| Leflunomide use, n (%) | 29 (18) | – | – |
| Hydroxychloroquine use, n (%) | 42 (25) | – | – |
| Anti-TNFα agent use, n (%) | 33 (20) | – | – |
| Prednisone use, n (%) | 89 (54) | – | – |
| NSAID use, n (%) | 55 (33) | 33 (37) | 0.53 |
aRF data were available in 159 patients with RA. Coronary artery calcium scores were available for 161 patients with RA and 88 control subjects. CAD, Coronary artery disease; CRP, High-sensitivity C-reactive protein; DAS28, Disease Activity Score based on 28 joints; ESR, Erythrocyte sedimentation rate; IQR, Interquartile range; NSAID, Non-steroidal anti-inflammatory drug; RA, Rheumatoid arthritis; RF, Rheumatoid factor; TNFα, Tumor necrosis factor α
Fig. 1.
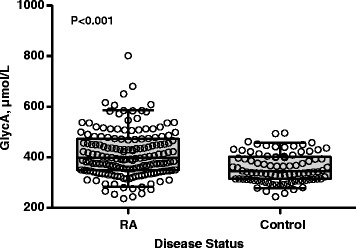
GlycA is higher in patients with rheumatoid arthritis compared with control subjects. Boxes represent the median (middle horizontal line) and the 25th and 75th percentiles. Whiskers represent the 5th and 95th percentiles. Each data point is presented as an open circle. Patients with rheumatoid arthritis had a higher GlycA concentration (median (interquartile range): 398 μmol/L (348 to 473 μmol/L)) compared with control subjects (344 μmol/L (314 to 403 μmol/L); P < 0.001)
GlycA relationship to disease activity in rheumatoid arthritis and disease-related factors
Increasing GlycA concentrations were significantly associated with increasing RA disease activity (P < 0.001) (Fig. 2). GlycA was correlated with DAS28-ESR (Spearman ρ = 0.58, P < 0.001) and DAS28-CRP (ρ = 0.47, P < 0.001). These correlations were similar or slightly stronger than those between CRP and DAS28-ESR (ρ = 0.48, P < 0.001) and between ESR and DAS28-CRP (ρ = 0.36, P < 0.001) (Table 2). Similarly, the cross-sectional relationship between Larsen score and GlycA (ρ = 0.24, P = 0.02) was similar or slightly stronger than the relationship with CRP (ρ = 0.18, P = 0.09) or ESR (ρ = 0.16, P = 0.13) (Table 2).
Fig. 2.
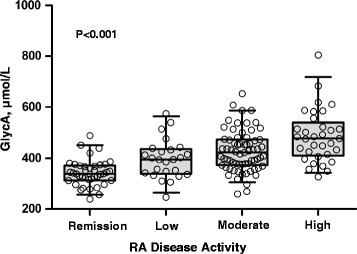
GlycA increases with increasing rheumatoid arthritis disease activity. Boxes represent the median (middle horizontal line) and the 25th and 75th percentiles. Whiskers represent the 5th and 95th percentiles. Each data point is presented as an open circle. Rheumatoid arthritis (RA) disease activity on the basis of Disease Activity Score based on 28 joints using erythrocyte sedimentation rate (DAS28-ESR) was defined as follows: remission = DAS28 < 2.6 (n = 39); low = DAS28 between 2.6 and 3.2 (n = 25); moderate = DAS28 between 3.2 and 5.1 (n = 67); and high = DAS28 > 5.1 (n = 33)
Table 2.
Association between GlycA, C-reactive protein and erythrocyte sedimentation rate with measures of disease activity and clinical characteristics in patients with rheumatoid arthritisa
| GlycA | ESR | CRP | |
|---|---|---|---|
| ρ | ρ | ρ | |
| DAS28-ESR | 0.58b | 0.65b | 0.48b |
| DAS28-CRP | 0.47b | 0.36b | 0.50b |
| Tender joints | 0.28b | 0.12 | 0.16c |
| Swollen joints | 0.29b | 0.28b | 0.29b |
| Global health score | 0.25b | 0.21c | 0.22c |
| Larsen scored | 0.24c | 0.16 | 0.18 |
| ESR | 0.64b | – | 0.59b |
| CRP | 0.61b | 0.59b | – |
| IL-6 | 0.39b | 0.38b | 0.40b |
| TNFα | 0.25c | 0.28b | 0.21c |
| Age | 0.04 | 0.18c | 0.08 |
| BMI | 0.08 | 0.09 | 0.17c |
| Hemoglobin | −0.12 | −0.51b | −0.21c |
| eGFR | 0.02 | −0.04 | 0.05 |
aCorrelation data are based on Spearman’s correlation coefficient (ρ). BMI, Body mass index; CRP, High-sensitivity C-reactive protein; DAS28, Disease Activity Score based on 28 joints; eGFR, Estimated glomerular filtration rate; ESR, Erythrocyte sedimentation rate; IL-6, Interleukin-6; TNFα, Tumor necrosis factor α. b P ≤ 0.001. c P < 0.05. dLarsen scores were available for 92 patients with RA
The AUC for GlycA’s ability to discriminate between patients with low versus moderate to high disease activity was 0.78 (95 % CI: 0.71, 0.86) based on DAS28-ESR and 0.75 (0.68, 0.83) based on DAS28-CRP. Such discrimination was similar or better with GlycA compared with ESR (AUC: 0.68 (95 % CI: 0.60, 0.76)) using DAS28-CRP and compared with CRP (AUC: 0.74 (95 % CI: 0.67, 0.82)) using DAS28-ESR. GlycA was also associated with components of the DAS28 scores including tender and swollen joint counts, patient-reported global health score, ESR and CRP (all P < 0.001) (Table 2).
The relationship between GlycA concentrations and radiographic damage was assessed in a subset of 92 patients with RA for whom radiographic data were obtained. GlycA was significantly correlated with Larsen score (ρ = 0.24, P = 0.02) (Table 2). GlycA concentration was not significantly different between rheumatoid factor–positive (median (IQR) 408 μmol/L (351 to 479 μmol/L) and rheumatoid factor–negative patients with RA (385 μmol/L (336 to 452 μmol/L) (P = 0.09). Also, there were no significant differences in GlycA concentration between patients with RA who were receiving methotrexate, leflunomide, hydroxychloroquine, corticosteroids, anti-TNFα agents, non-steroidal anti-inflammatories, anti-hypertensives or statins compared with those not receiving the respective drugs (all P > 0.07).
Relationship between GlycA and subclinical atherosclerosis in rheumatoid arthritis
We examined the cross-sectional relationship between GlycA and the presence of coronary artery calcium, a marker of subclinical atherosclerosis (Table 3). Among patients with coronary artery calcium, the median (IQR) GlycA concentration was 415 μmol/L (356 to 477 μmol/L), which trended higher than the median GlycA concentration of those without coronary calcium (379 μmol/L ([337 to 457 μmol/L)) (P = 0.06). For each quartile increase in GlycA, the odds of having coronary artery calcium increased by 48 % (95 % CI: 4 %, 111 %), independent of age, race and sex (P = 0.03). This relationship was attenuated after adjustment for traditional CV risk factors, including age, sex, total cholesterol, HDL cholesterol, smoking status, systolic blood pressure and anti-hypertensive use (P = 0.07), and additionally for diabetes (P = 0.12). Although only 17 of 166 patients with RA had a diagnosis of established coronary artery disease, we performed an exploratory analysis to determine the relationship between GlycA and prevalent coronary artery disease. Among patients with coronary artery disease, the median (IQR) GlycA concentration was 453 μmol/L (380 to 487 μmol/L), which was significantly higher than the median GlycA concentration of those without coronary artery disease (395 μmol/L (344 to 487 μmol/L) (P = 0.03). Similarly, with each quartile increase in GlycA, the odds of having a diagnosis of coronary artery disease increased 110 % (17 % to 277 %), independent of age, race and sex (P = 0.01), and remained significant with additional adjustment for traditional CV risk factors (P = 0.01) and additionally for diabetes (P = 0.02) (Table 3).
Table 3.
Relationship between GlycA and cardiovascular diseasea
| GlycA | OR (95 % CI) | P-value | ORb (95 % CI) | Adjusted P-valueb | ORc (95 % CI) | Adjusted P-valuec | ORd (95 % CI) | Adjusted P-valued |
|---|---|---|---|---|---|---|---|---|
| Coronary calcium | 1.32 (0.99, 1.74) | 0.06 | 1.48 (1.04, 2.11) | 0.03 | 1.39 (0.97, 2.01) | 0.07 | 1.35 (0.93, 1.95) | 0.12 |
| Known CAD | 1.83 (1.10, 3.03) | 0.02 | 2.10 (1.17, 3.77) | 0.01 | 2.14 (1.17, 3.92) | 0.01 | 2.10 (1.13, 3.88) | 0.02 |
aAll analyses were performed using logistic regression. CAD, Coronary artery disease; CI, Confidence interval; OR, Odds ratio per quartile increase in GlycA concentration. bAdjusted for age, race and sex. cAdjusted for age, sex, total cholesterol, high-density lipoprotein (HDL) cholesterol, smoking status, systolic blood pressure and anti-hypertensive use. dAdjusted for age, sex, total cholesterol, HDL cholesterol, smoking status, systolic blood pressure, anti-hypertensive use and diabetes
Relationship between potential confounders and GlycA
As discussed above, CRP and ESR have been reported to be altered by age, sex and BMI. We found no significant association between either age or BMI and GlycA concentration (all P ≥ 0.30) (Table 2), and we observed no difference between men and women (P = 0.31). Similarly, because anemia and impaired renal function may alter ESR, we compared the association between GlycA and hemoglobin and eGFR. There was no significant correlation between GlycA and hemoglobin or eGFR (all P > 0.60) (Table 2). Conversely, CRP was significantly correlated with BMI (positively) and hemoglobin (inversely), and ESR was significantly correlated with age (positively) and hemoglobin (inversely) (Table 2). Neither CRP nor ESR was significantly correlated with eGFR. However, most patients in this cohort had normal renal function (median eGFR: 87 ml/min/1.73 m2 (IQR: 74 to 103 ml/min/1.73 m2), range: 28 to 161 ml/min/1.73 m2).
Discussion
The major new findings of the present study are that GlycA may be a useful marker of disease activity and CV risk in patients with RA. GlycA was strongly correlated with all components of DAS28 scores and was correlated with radiographic damage in cross-sectional analysis. Moreover, it was associated with the presence of coronary artery calcium and prevalent coronary artery disease in patients with RA.
GlycA is measured from an NMR signal that primarily represents glycosylated acute-phase proteins [10, 18]. Glycosylation, not to be confused with the non-enzymatic binding of simple sugars as occurs with hemoglobin A1c in patients with diabetes mellitus [40], is an enzymatic modification whereby an oligo or polysaccharide moiety is attached to a protein or lipid. This modification has an important role in protein folding and stabilization, cell signaling, cellular adhesion and antigen recognition [41]. In fact, during an acute-phase response, not only are levels of serum acute phase glycoproteins altered, but their glycan structures are also dynamically modified by circulating glycosidases and glycosyltransferases [42, 43]. Therefore, the measurement of these protein glycans via NMR (GlycA) incorporates alterations in both protein and glycan concentrations that occur during inflammatory responses.
Previous studies have identified glycosylation products as markers of RA and inflammatory disease. In one study [19], 47 patients with RA and 51 control subjects were followed longitudinally and metabolic profiles using NMR spectroscopy were assessed over time from plasma samples. Peaks arising from glycosylated proteins (including the GlycA signal), cholesterol, lactate and unsaturated lipids appeared to be biomarkers of the presence of RA, but these measures used together were not robust markers of changes in RA disease activity [19]. Others found that NMR measurements of total glycosylated residues (including the signal for GlycA) and of N-acetylglucosamine (a component of GlycA) plus N-acetylneuraminic acid were elevated in 21 patients with rheumatic or infectious diseases compared with 186 control subjects or patients with cancer [20]. Although previous authors have shown interesting correlations between the NMR signal arising from glycosylated proteins and various disease states, the standardized measurement of GlycA from the profile spectra obtained on a clinical NMR analyzer allows for more robust clinical investigations.
Given that the GlycA peak represents glycosylated acute-phase proteins, it is not surprising that GlycA is closely associated with disease activity in RA. Interestingly, GlycA correlated at least as well as CRP or ESR with several measures of disease activity, radiographic damage and presence of coronary calcium. Moreover, GlycA had similar discriminative capacity to differentiate between low and moderate to high disease activity (AUC: 0.75) compared with published data for the multibiomarker disease activity test (AUC: 0.76) in which CRP was used as a component of both the predictor multibiomarker test and outcome of disease activity measured by DAS28-CRP [44].
Correlations with disease activity in a cross-sectional study may be stronger with GlycA than with CRP or ESR if GlycA is a more stable marker of inflammation that is less susceptible to alterations by both day-to-day variability and non-inflammatory factors. Indeed, the day-to-day variability of GlycA concentrations is lower than for CRP [10]. The speed at which GlycA rises and falls after an inflammatory stimulus is not known; however, given its components, it is likely that GlycA rises over several days and falls over several weeks. This is similar to the pattern of ESR’s rise and fall due to fibrinogen’s impact on ESR [45], though fibrinogen is not a component of GlycA. Interestingly, GlycA appears to be influenced less by non-inflammatory conditions such as age, anemia, and BMI than by CRP or ESR.
Our findings in patients with RA are concordant with findings in the general population. GlycA was measured in participants of the Women’s Health Study, which included 27,491 women with a median of 17.2 years of follow-up [21]. GlycA concentrations were correlated strongly with CRP (ρ = 0.61, P < 0.0001), and baseline GlycA concentrations were associated with incident CV events. For example, within the first 6 years of follow-up, the hazard ratio Q4 for CV events was 1.34 (95 % CI: 1.22, 1.48) (P < 0.0001 for each 1 SD increase in GlycA). Notably, this unit of increase is similar to the observed difference in GlycA concentration between RA and control subjects in the present study.
We have evaluated the use of a novel inflammatory marker for utility in assessing disease activity and CV risk. There are other novel biomarkers that have similarly been proposed as important biomarkers of both RA disease activity and atherosclerosis or CV disease. Some recent examples include osteoprotegerin [46, 47] and angiopoietin-2 [48].
Although we included a relatively large cohort of patients with RA who were well characterized with respect to inflammation and CV risk, the present study has limitations. The adjusted analyses for the relationship between GlycA and prevalent coronary artery disease should be interpreted with caution because models were overfitted, owing to the relatively small number of patients with RA and prevalent coronary artery disease (N = 17). Because this was a cross-sectional study, the longitudinal implications of the findings regarding an association are uncertain. For example, although the finding that GlycA was associated with radiographic damage is interesting, additional studies are required to determine if GlycA has utility as a marker of the risk of radiographic progression. Moreover, future investigation of GlycA’s ability to measure changes in disease activity in response to therapy and development of CV events is important to fully evaluate its utility in patients with RA.
Conclusions
GlycA is increased in patients with RA compared with control subjects. It is strongly correlated with DAS28 and its components, and it is also correlated with radiographic damage. Moreover, increased GlycA concentrations are associated with the presence of coronary artery calcification.
Acknowledgements
This study was funded by a Arthritis Foundation Clinical to Research Transition Award (CTSA); National Institutes of Health grants P60 AR056116, K23 AR064768 and KL2TR000446; and CTSA award UL1TR000445 from the National Center for Advancing Translational Sciences. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Abbreviations
- AUC
Area under the curve
- BMI
Body mass index
- CAD
Coronary artery disease
- CI
Confidence interval
- CRP
C-reactive protein
- CV
Cardiovascular
- DAS28
Disease Activity Score based on 28 joints
- eGFR
Estimated glomerular filtration rate
- ELISA
Enzyme-linked immunosorbent assay
- ESR
Erythrocyte sedimentation rate
- HDL
High-density lipoprotein
- IL-6
Interleukin-6
- IQR
Interquartile range
- NMR
Nuclear magnetic resonance
- NSAID
Non-steroidal anti-inflammatory drug
- OR
Odds ratio
- RA
Rheumatoid arthritis
- RF
Rheumatoid factor
- SD
Standard deviation
- TNFα
Tumor necrosis factor α
Footnotes
Competing interests
MAC and JDO are former employees of LipoScience, which is now owned by LabCorp. The remaining authors declare that they have no competing interests.
Authors’ contributions
All authors made substantial contributions to the study conception and design, the acquisition of data or the analysis and interpretation of data as indicated below. All authors were involved in drafting the article or revising it critically for important intellectual content. MJO, CPC and CMS were responsible for study conception and design. AMO, MAC, TS, PR, JFS and JDO were responsible for acquisition of data. MJO, CPC and CMS were responsible for the analysis and interpretation of data. All authors read and approved the final manuscript version to be published and agree to be accountable for all aspects of the work.
Contributor Information
Michelle J. Ormseth, Email: michelle.ormseth@vanderbilt.edu
Cecilia P. Chung, Email: c.chung@vanderbilt.edu
Annette M. Oeser, Email: annette.oeser@vanderbilt.edu
Margery A. Connelly, Email: margery.commelly@liposcience.com
Tuulikki Sokka, Email: tuulikki.sokka-isler@ksshp.fi.
Paolo Raggi, Email: raggip@gmail.com.
Joseph F. Solus, Email: joseph.f.solus@vanderbilt.edu
James D. Otvos, Email: jotvos@liposcience.com
C. Michael Stein, Email: mike.stein@vanderbilt.edu.
References
- 1.van Leeuwen MA, van der Heijde DM, van Rijswijk MH, Houtman PM, van Riel PL, van de Putte LB, et al. Interrelationship of outcome measures and process variables in early rheumatoid arthritis: a comparison of radiologic damage, physical disability, joint counts, and acute phase reactants. J Rheumatol. 1994;21:425–9. [PubMed] [Google Scholar]
- 2.Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G, et al. Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis. 2010;69:631–7. A published erratum appears in. Ann Rheum Dis. 2011;70:1519. doi: 10.1136/annrheumdis-2011-70-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–8. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 4.Felson DT, Anderson JJ, Boers M, Bombardier C, Chernoff M, Fried B, et al. The American College of Rheumatology preliminary core set of disease activity measures for rheumatoid arthritis clinical trials. Arthritis Rheum. 1993;36:729–40. doi: 10.1002/art.1780360601. [DOI] [PubMed] [Google Scholar]
- 5.Felson DT, Smolen JS, Wells G, Zhang B, van Tuyl LH, Funovits J, et al. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum. 2011;63:573–86. doi: 10.1002/art.30129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shusterman N, Kimmel PL, Kiechle FL, Williams S, Morrison G, Singer I. Factors influencing erythrocyte sedimentation in patients with chronic renal failure. Arch Intern Med. 1985;145:1796–9. doi: 10.1001/archinte.1985.00360100056007. [DOI] [PubMed] [Google Scholar]
- 7.Sox HC, Jr, Liang MH. The erythrocyte sedimentation rate: guidelines for rational use. Ann Intern Med. 1986;104:515–23. doi: 10.7326/0003-4819-104-4-515. [DOI] [PubMed] [Google Scholar]
- 8.Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, 3rd, Criqui M, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.CIR.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 9.DeGoma EM, French B, Dunbar RL, Allison MA, Mohler ER, 3rd, Budoff MJ. Intraindividual variability of C-reactive protein: the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2012;224:274–9. doi: 10.1016/j.atherosclerosis.2012.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Otvos JD, Shalaurova I, Wolak-Dinsmore J, Connelly MA, Mackey RH, Stein JH, et al. GlycA: a composite nuclear magnetic resonance biomarker of systemic inflammation. Clin Chem. 2015;61:714–23. doi: 10.1373/clinchem.2014.232918. [DOI] [PubMed] [Google Scholar]
- 11.Ranganath VK, Elashoff DA, Khanna D, Park G, Peter JB, Paulus HE. Western consortium of practicing rheumatologists. Age adjustment corrects for apparent differences in erythrocyte sedimentation rate and C-reactive protein values at the onset of seropositive rheumatoid arthritis in younger and older patients. J Rheumatol. 2005;32:1040–2. [PubMed] [Google Scholar]
- 12.Lear SA, Chen MM, Birmingham CL, Frohlich JJ. The relationship between simple anthropometric indices and C-reactive protein: ethnic and gender differences. Metabolism. 2003;52:1542–6. doi: 10.1016/j.metabol.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Wener MH, Daum PR, McQuillan GM. The influence of age, sex, and race on the upper reference limit of serum C-reactive protein concentration. J Rheumatol. 2000;27:2351–9. [PubMed] [Google Scholar]
- 14.Kawamoto R, Kusunoki T, Abe M, Kohara K, Miki T. An association between body mass index and high-sensitivity C-reactive protein concentrations is influenced by age in community-dwelling persons. Ann Clin Biochem. 2013;50:457–64. doi: 10.1177/0004563212473445. [DOI] [PubMed] [Google Scholar]
- 15.Rommel J, Simpson R, Mounsey JP, Chung E, Schwartz J, Pursell I, et al. Effect of body mass index, physical activity, depression, and educational attainment on high-sensitivity C-reactive protein in patients with atrial fibrillation. Am J Cardiol. 2013;111:208–12. doi: 10.1016/j.amjcard.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 16.Rawson ES, Freedson PS, Osganian SK, Matthews CE, Reed G, Ockene IS. Body mass index, but not physical activity, is associated with C-reactive protein. Med Sci Sports Exerc. 2003;35:1160–6. doi: 10.1249/01.MSS.0000074565.79230.AB. [DOI] [PubMed] [Google Scholar]
- 17.Piéroni L, Bastard JP, Piton A, Khalil L, Hainque B, Jardel C. Interpretation of circulating C-reactive protein levels in adults: body mass index and gender are a must. Diabetes Metab. 2003;29:133–8. doi: 10.1016/S1262-3636(07)70019-8. [DOI] [PubMed] [Google Scholar]
- 18.Bell JD, Brown JC, Nicholson JK, Sadler PJ. Assignment of resonances for ‘acute-phase’ glycoproteins in high resolution proton NMR spectra of human blood plasma. FEBS Lett. 1987;215:311–5. doi: 10.1016/0014-5793(87)80168-0. [DOI] [PubMed] [Google Scholar]
- 19.Lauridsen MB, Bliddal H, Christensen R, Danneskiold-Samsøe B, Bennett R, Keun H, et al. 1H NMR spectroscopy-based interventional metabolic phenotyping: a cohort study of rheumatoid arthritis patients. J Proteome Res. 2010;9:4545–53. doi: 10.1021/pr1002774. [DOI] [PubMed] [Google Scholar]
- 20.Kriat M, Vion-Dury J, Fayre R, Maraninchi D, Harlé JR, Confort-Gouny S, et al. Variations of plasma sialic acid and N-acetylglucosamine levels in cancer, inflammatory diseases and bone marrow transplantation: a proton NMR spectroscopy study. Biochimie. 1991;73:99–104. doi: 10.1016/0300-9084(91)90081-B. [DOI] [PubMed] [Google Scholar]
- 21.Akinkuolie AO, Buring JE, Ridker PM, Mora S. A novel protein glycan biomarker and future cardiovascular disease events. J Am Heart Assoc. 2014;3:e001221. doi: 10.1161/JAHA.114.001221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chung CP, Oeser A, Raggi P, Gebretsadik T, Shintani AK, Sokka T, et al. Increased coronary-artery atherosclerosis in rheumatoid arthritis: relationship to disease duration and cardiovascular risk factors. Arthritis Rheum. 2005;52:3045–53. doi: 10.1002/art.21288. [DOI] [PubMed] [Google Scholar]
- 23.Chung CP, Oeser A, Avalos I, Gebretsadik T, Shintani A, Raggi P, et al. Utility of the Framingham risk score to predict the presence of coronary atherosclerosis in patients with rheumatoid arthritis. Arthritis Res Ther. 2006;8:R186. doi: 10.1186/ar2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chung CP, Oeser A, Solus JF, Avalos I, Gebretsadik T, Shintani A, et al. Prevalence of the metabolic syndrome is increased in rheumatoid arthritis and is associated with coronary atherosclerosis. Atherosclerosis. 2008;196:756–63. doi: 10.1016/j.atherosclerosis.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Rho YH, Chung CP, Oeser A, Solus J, Asanuma Y, Sokka T, et al. Inflammatory mediators and premature coronary atherosclerosis in rheumatoid arthritis. Arthritis Rheum. 2009;61:1580–5. doi: 10.1002/art.25009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chung CP, Oeser A, Raggi P, Sokka T, Pincus T, Solus JF, et al. Lipoprotein subclasses determined by nuclear magnetic resonance spectroscopy and coronary atherosclerosis in patients with rheumatoid arthritis. J Rheumatol. 2010;37:1633–8. doi: 10.3899/jrheum.090639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rho YH, Chung CP, Oeser A, Solus JF, Gebretsadik T, Shintani A, et al. Interaction between oxidative stress and high-density lipoprotein cholesterol is associated with severity of coronary artery calcification in rheumatoid arthritis. Arthritis Care Res (Hoboken) 2010;62:1473–80. doi: 10.1002/acr.20237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rho YH, Chung CP, Solus JF, Raggi P, Oeser A, Gebretsadik T, et al. Adipocytokines, insulin resistance, and coronary atherosclerosis in rheumatoid arthritis. Arthritis Rheum. 2010;62:1259–64. doi: 10.1002/art.27376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rho YH, Solus J, Raggi P, Oeser A, Gebretsadik T, Shintani A, et al. Macrophage activation and coronary atherosclerosis in systemic lupus erythematosus and rheumatoid arthritis. Arthritis Care Res (Hoboken) 2011;63:535–41. doi: 10.1002/acr.20365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ormseth MJ, Swift LL, Fazio S, Linton MF, Chung CP, Raggi P, et al. Free fatty acids are associated with insulin resistance but not coronary artery atherosclerosis in rheumatoid arthritis. Atherosclerosis. 2011;219:869–74. doi: 10.1016/j.atherosclerosis.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 32.Inoue E, Yamanaka H, Hara M, Tomatsu T, Kamatani N. Comparison of Disease Activity Score (DAS)28-erythrocyte sedimentation rate and DAS28-C-reactive protein threshold values. Ann Rheum Dis. 2007;66:407–9. doi: 10.1136/ard.2006.054205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–54. A published erratum appears in. Ann Intern Med. 2008;149:519. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 34.Rho YH, Solus J, Sokka T, Oeser A, Chung CP, Gebretsadik T, et al. Adipocytokines are associated with radiographic joint damage in rheumatoid arthritis. Arthritis Rheum. 2009;60:1906–14. doi: 10.1002/art.24626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaarela K, Kautiainen H. Continuous progression of radiological destruction in seropositive rheumatoid arthritis. J Rheumatol. 1997;24:1285–7. [PubMed] [Google Scholar]
- 36.Larsen A. How to apply Larsen score in evaluating radiographs of rheumatoid arthritis in long-term studies. J Rheumatol. 1995;22:1974–5. [PubMed] [Google Scholar]
- 37.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-T. [DOI] [PubMed] [Google Scholar]
- 38.Jeyarajah EJ, Cromwell WC, Otvos JD. Lipoprotein particle analysis by nuclear magnetic resonance spectroscopy. Clin Lab Med. 2006;26:847–70. doi: 10.1016/j.cll.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 39.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III): final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 40.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414:813–20. doi: 10.1038/414813a. [DOI] [PubMed] [Google Scholar]
- 41.Rudd PM, Elliott T, Cresswell P, Wilson IA, Dwek RA. Glycosylation and the immune system. Science. 2001;291:2370–6. doi: 10.1126/science.291.5512.2370. [DOI] [PubMed] [Google Scholar]
- 42.van Dijk W, Turner GA, Mackiewicz A. Changes in glycosylation of acute-phase proteins in health and disease: occurrence, regulation and function. Glycosylation Dis. 1994;1:5–14. doi: 10.1007/BF00917463. [DOI] [Google Scholar]
- 43.Ceciliani F, Pocacqua V. The acute phase protein α1-acid glycoprotein: a model for altered glycosylation during diseases. Curr Protein Pept Sci. 2007;8:91–108. doi: 10.2174/138920307779941497. [DOI] [PubMed] [Google Scholar]
- 44.Curtis JR, van der Helm-van Mil AH, Knevel R, Huizinga TW, Haney DJ, Shen Y, et al. Validation of a novel multibiomarker test to assess rheumatoid arthritis disease activity. Arthritis Care Res (Hoboken) 2012;64:1794–803. doi: 10.1002/acr.21767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448–54. A published erratum appears in. N Engl J Med. 1999;340:1376. doi: 10.1056/NEJM199904293401723. [DOI] [PubMed] [Google Scholar]
- 46.López-Mejias R, Ubilla B, Genre F, Corrales A, Hernández JL, Ferraz-Amaro I, et al. Osteoprotegerin concentrations relate independently to established cardiovascular disease in rheumatoid arthritis. J Rheumatol. 2015;42:39–45. doi: 10.3899/jrheum.140690. [DOI] [PubMed] [Google Scholar]
- 47.Dessein PH, López-Mejias R, González-Juanatey C, Genre F, Miranda-Filloy JA, Llorca J, et al. Independent relationship of osteoprotegerin concentrations with endothelial activation and carotid atherosclerosis in patients with severe rheumatoid arthritis. J Rheumatol. 2014;41:429–36. doi: 10.3899/jrheum.131037. [DOI] [PubMed] [Google Scholar]
- 48.López-Mejías R, Corrales A, Genre F, Hernández JL, Ochoa R, Blanco R, et al. Angiopoietin-2 serum levels correlate with severity, early onset and cardiovascular disease in patients with rheumatoid arthritis. Clin Exp Rheumatol. 2013;31:761–6. [PubMed] [Google Scholar]


