Abstract
Meningiomas are common, usually benign tumors, with a high postoperative recurrence rate. However, the genesis and development of these tumors remain controversial. We aimed to investigate the presence and implications of a mutated p53 protein and dopamine D2 receptor in a representative series of meningiomas and to correlate these findings with age, gender, tumor grade, and recurrence. Tumor tissue samples of 157 patients diagnosed with meningioma (37 males and 120 females, mean age 53.6±14.3 years) who underwent surgical resection between 2003 and 2012 at our institution were immunohistochemically evaluated for the presence of p53 protein and dopamine D2 receptor and were followed-up to analyze tumor recurrence or regrowth. Tumors were classified as grades I (n=141, 89.8%), II (n=13, 8.3%), or grade III (n=3, 1.9%). Dopamine D2 receptor and p53 protein expression were positive in 93.6% and 49.7% of the cases, respectively. Neither of the markers showed significant expression differences among different tumor grades or recurrence or regrowth statuses. Our findings highlight the potential role of p53 protein in meningioma development and/or progression. The high positivity of dopamine D2 receptor observed in this study warrants further investigation of the therapeutic potential of dopamine agonists in the evolution of meningiomas.
Keywords: Receptors, Dopamine D2, Immunohistochemistry, Meningioma, Tumor suppressor protein p53, Recurrence
Introduction
Meningiomas account for approximately 35% of all intracranial neoplasms, with an annual incidence of approximately 7.22 cases per 100,000 individuals. The peak incidence is between the sixth and seventh decades of life, afflicting females more often than males (2:1) (1). Approximately 90-95% of meningiomas are benign in nature, 5-7% are atypical, and 2% are malignant (2). These tumors have a high recurrence rate, reaching up to 50% after incomplete surgical resection (3).
Several hormones have been implicated as predisposing factors to meningioma development. Meningiomas express androgen receptors (4), estrogen and progesterone receptors (5), and nonsteroidal hormone receptors including receptors for growth hormone (6), somatostatin (7), and dopamine (8,9).
Dopamine receptors are prominent in the central nervous system and are divided into five subtypes (D1 to D5). The D1 and D5 receptors are members of the D1-like family, and the D2, D3, and D4 receptors are members of the D2-like family. The definitions of these groups are based on their relationships with transduction mechanisms. Activation of D1-like family receptors stimulates the enzyme adenylate cyclase and increases intracellular levels of cAMP (3′,5′-cyclic adenosine monophosphate), while those in the D2-like family inhibit this enzyme and decrease intracellular cAMP concentration. The short (D2S) and long (D2L) isoforms of the dopamine D2 receptor also activate pathways involved in the regulation of cell growth, differentiation, and apoptosis (10). In studies with rat pituitary tumor cells, dopamine agonists have been shown to exhibit an antiproliferative effect, inducing cell death and apoptosis through the activation of D2 receptors (11,12). Other studies have shown antiproliferative effects of the dopamine agonist bromocriptine in cultured meningioma cells (8,13).
Mutations in the gene encoding the tumor suppressor p53 protein are common in different types of human tumors (14). The role of p53 gene mutations in the genesis of meningiomas is controversial (15,16), with a high immunohistochemical expression rate of the mutated protein in atypical and malignant meningiomas but a low rate in benign tumors (17).
This study aimed to investigate the immunohistochemical expression of p53 protein and dopamine D2 receptor in meningiomas and correlate these findings with follow-up, age, gender, histologic tumor grade, and recurrence.
Material and Methods
The study sample included tumor tissue specimens obtained from 157 patients with an anatomopathologic diagnosis of meningioma who underwent surgical resection performed by the same surgeon (NPF) at Hospital São José, Complexo Hospitalar Santa Casa de Porto Alegre, Southern Brazil, between January 2003 and December 2012. Tumors were classified according to the World Health Organization (WHO) criteria for histological subtypes and tumor grading (grades I-III) (18). Patients' medical records were reviewed for data collection, and 80 patients were followed-up. The study was approved by the Research Ethics Committee of Hospital Santa Casa de Misericórdia de Porto Alegre, Brazil (Report No. 114/03) and was conducted in accordance with the provisions of the Declaration of Helsinki. Written informed consent was obtained from all patients before inclusion in the study, and patient anonymity was preserved.
Immunohistochemistry
For immunohistochemical analysis, tumor tissue samples were fixed in 10% buffered formalin and embedded in paraffin. Blocks were sectioned at 4 µm, deparaffinized, and rehydrated. The streptavidin-biotin method (LSAB kit + peroxidase; Dako®, Denmark) was used to detect p53 protein (anti-p53 monoclonal antibody, clone DO-7, 1:100 dilution; Dako®, catalog No. M7001) and dopamine D2 receptor (anti-DRD2 polyclonal antibody, 1:150 dilution; Chemicon®, USA, catalog No. AB5084P). Normal human pituitary and breast tissues were used as positive controls for dopamine D2 receptor and p53 protein, respectively (19,20). As a negative control, the primary antibodies were replaced with saline.
The criterion for positive intracellular dopamine D2 receptor and p53 protein expression was the presence of at least one group of cells with clearly marked cytoplasm or nuclei, respectively (5,20). Specimens were analyzed by two independent observers, using light microscopy.
Statistical analysis
Age, according to the symmetry determined by the Kolmogorov-Smirnov test, was reported as means±SD and compared between immunohistochemistry groups (positive or negative) using Student's t-test. Categorical variables were compared using chi-square tests with Fisher's corrections. The Kaplan-Meier method was used to estimate the rate of survival free of recurrence. The level of significance was set at 5%. Data analysis was carried out using the Statistical Package for the Social Sciences (SPSS, version 19.0; IBM Corp., USA).
Results
Of the 157 patients, 120 were female (76.4%), corresponding to a female-to-male ratio of 3:1. The mean patient age was 53.6±14.3 years. According to the WHO grading scheme, 141 (89.8%) meningiomas were classified as grade I, 13 (8.3%) as grade II, and 3 (1.9%) as grade III. The histological subtypes were transitional (n=69, 43.9%), meningothelial (n=27, 17.2%), fibroblastic (n=19, 12.1%), psammomatous (n=14, 8.9%), atypical (n=13, 8.3%), angiomatous (n=6, 3.9%), microcystic (n=3, 1.9%), secretory (n=3, 1.9%), anaplastic (n=2, 1.3%), and rhabdoid (n=1, 0.6%).
Seventy-eight (49.7%) meningiomas stained positive for p53 protein. The p53 protein was positive in 66/141 (46.8%) grade I tumors, 11/13 (84.6%) grade II tumors, and 1/3 (33.3%) grade III tumors, with no statistically significant differences in positivity among tumor grades. However, meningiomas with higher grades of malignancy (grades II and III) displayed a tendency for a higher frequency of nuclear p53 positivity (P=0.06).
Regarding gender, 57 (47.5%) samples from females and 21 (56.8%) from males were positive for p53 protein, with no statistically significant differences between genders (P>0.05). The mean age was significantly higher in patients with positive p53 immunostaining compared to those with negative p53 immunostaining (55.9 vs 51.4 years, P=0.04).
With regard to dopamine D2 receptor, 147 (93.6%) meningiomas stained positive. Positivity percentages according to tumor grade were 93.6%, 100%, and 66.6% for grades I, II, and III tumors, respectively, with no statistically significant differences among tumor grades. There were no statistically significant differences in positivity between genders (93.3% of females and 94.6% of males) or mean patient age (53.9 vs 49.0 years, P>0.05).
Seventy-five (47.7%) tumors were positive for both dopamine D2 receptor and p53 protein. These tumors had higher histological malignancy compared to meningiomas that were not positive for both markers (n=82, 52.2%), with a statistically significant difference (P=0.021).
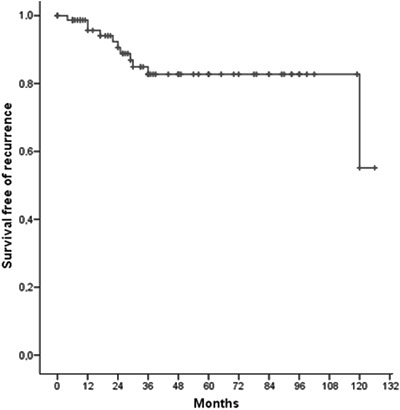
Among the 157 patients included in the immunohistochemical analysis, 80 were followed-up during a period of 4±2.9 years (range 0.5-10.5 years). According to Kaplan-Meier analysis, the rate of survival free of recurrence at 3 years was 82.7% (Figure 1). Among these 80 patients, 4 (5%) died due to acute surgical complications, 65 (81.3%) had stable disease without tumor recurrence or regrowth, and 11 (13.8%) showed meningioma recurrence or regrowth (6 and 5 who had previously underwent partial and total resection, respectively). For the patients with recurrence, 8, 1, and 2 had grade I, II, and III, respectively. Of these, 5 are being followed-up, 2 received radiotherapy, 3 underwent a single surgical resection, and 1 had 3 resections.
Figure 1. Kaplan-Meier curve showing the rate of survival free of recurrence in meningiomas analyzed.
Among the 4 patients that underwent reoperation, 2, 1, and 1 were grades I, II, and III, respectively. Following reoperation, 2 maintained the same anatomopathological diagnosis (transitional and anaplastic), 1 meningotelial turned to atypical, and 1 atypical changed to anaplastic. Both cases with a new anatomopathological diagnosis began to express p53 protein even though the samples from the first surgeries were negative. Neither immunohistochemical expression of p53 nor dopamine D2 receptor showed statistically significant differences between patients with recurrence or regrowth and those with stable disease. Comparing disease evolution with age, we observed that those patients with recurrence or regrowth had a significantly lower mean age than those with stable disease (41.36 vs 54.03, P=0.02).
Discussion
The present study analyzed a representative series of meningiomas. The findings were consistent with data reported in the literature regarding age of incidence and female predominance (1,21), as well as greater occurrence of grade I tumors (2,22). The mean follow-up time in 80 patients was 4 years (range 6 months to 10.5 years). The results are similar to data previously published in the literature describing from 26 (17) to 120 (23) patients followed for a period of 8 months (24) to 21 years (23).
The p53 protein functions as a tumor suppressor and acts to protect DNA. Following irreversible DNA damage, the p53 protein induces cell apoptosis. The wild-type protein has an inhibitory effect on cell proliferation and transformation, but gene mutations alter its tumor suppressor activity (25). A high proportion of cells with mutant protein indicate increased tumor aggressiveness (26).
With regard to p53 expression in meningiomas, Matsuno et al. (27) studied 51 meningiomas and found that approximately 20% were immunopositive for p53. Cho et al. (17) assessed 41 meningiomas and reported 43.9% positive immunoreactivity for p53 (9.5% grade I, 72.7% grade II, and 88.9% grade III meningiomas), and this immunoreactivity was stronger in tumors with higher histological malignancy. Lanzafame et al. (28) immunohistochemically examined 69 meningiomas and found p53 protein expression in 57% of cases, with higher levels in atypical and malignant meningiomas compared to benign tumors. Amatya et al. (29) analyzed 146 meningiomas and found positive p53 protein expression in 19.8% of cases; of these, few benign meningiomas had p53 protein expression, anaplastic meningiomas expressed p53 protein in most cases, and atypical meningiomas had an intermediate level of p53 labeling, with statistically significant expression differences among them. Karamitopoulou et al. (30) examined 60 meningiomas and found positive p53 protein expression in 31.6% of cases - 10.8% of grade I, 50% of grade II, and 77% of grade III tumors, with significantly higher p53 expression in atypical and anaplastic meningiomas (P=0.000003). On the other hand, Pavelin et al. (31) studied 170 meningiomas and found no statistically significant association between p53 levels and tumor grade. In our series, approximately 50% of cases showed positive p53 protein expression, which is consistent with the range from 19.8% to 57% reported in the literature (17,27-30). Similar to the findings of Pavelin (31), we only observed a trend for atypical and anaplastic meningiomas (grades II and III) showing higher p53 expression (P=0.06).
The protective function of the p53 protein declines with age, and this decline might lead to an inability of cells to respond to stressors and a consequent increase in tumor incidence (32). We found a significantly higher mean age among patients with p53-positive tumor samples. However, we did not observe a significant association between p53 protein expression and gender, which is in agreement with the findings of Amatya et al. (29).
Dopamine D2 receptor activation induces several pathways involved in the regulation of cell metabolism, growth, differentiation, and apoptosis, especially the mitogen-activated protein kinase (MAPK) and/or extracellular signal-regulated kinase (ERK) pathway. This activation has been associated with antiproliferative effects (10). Dopamine and its agonists bromocriptine (predominant action on D2 receptor), apomorphine (D1 and D2), and SKF-38393 (D1 agonist) at micromolar concentrations lead to a significant decrease in the proliferation rate of meningioma cells in culture (8). Incubation of meningioma cells with bromocriptine induces significant dose-dependent inhibition of cell proliferation ranging from 25% to 56% (13). More recently, Castelo-Branco et al. (33) reported the case of a patient with recurrent meningioma who responded well to treatment with cabergoline (a dopamine agonist acting predominantly via D2 receptors) with no compressive symptoms or increase in neoplasm size 11 years after treatment, suggesting that meningioma cell proliferation may be under dopaminergic control to some extent.
The evaluation of dopamine D2 receptor expression in meningiomas has been shown to be negative by Scatchard analysis (9,34), detectable in some cases by Northern blot analysis (9), and positive in 100% of cases using polymerase chain reaction assays, in which the sequences of dopamine D2 receptor were identical to those published by GenBank™ (9). In accordance with a previous study (30), we employed a qualitative method for immunohistochemical analysis given the syncytial features observed in these neoplasms (35) and detected 93.6% immunopositivity for dopamine D2 receptor. We found no statistically significant association of immunohistochemical dopamine D2 receptor expression with gender, patient age, or tumor recurrence or regrowth. To date, there are no reports of data related to the immunohistochemical expression of dopamine D2 receptors in meningiomas, precluding a comparison of results.
Follow-up studies in meningiomas describe recurrence in 6% to 39% of patients (23,24). In our follow-up with a mean time of 4 years, 13.8% of the cases showed tumor recurrence or regrowth, a percentage consistent with the data above. In relation to the rate of survival free of recurrence, Nakasu et al. (23) described rates of 92.5% and 90.7% at 10 and 20 years, respectively. Kim et al. (24) reported rates of 67.8% and 28.3% at 5 and 10 years, respectively. In the present study, the rate of survival free of recurrence was 82.7% at 3 years.
Several studies have shown that recurrent tumors present significantly increased p53 expression (17,23,24). However, when we analyzed tumor recurrence or regrowth in relation to immunohistochemical p53 expression, our results were in accordance with others that reported no significant difference between immunohistochemical expression of p53 and tumor recurrence or regrowth (28,30).
There is no description in the literature of statistically significant differences between patients of different ages and meningioma tumor recurrence (24,28,36). However, it is known that meningiomas with more advanced grades (III and II) tend to recur more (17) and affect younger patients (18). Our study revealed that the average age of patients with recurrence or regrowth was significantly lower than that of those with stable disease, indicating that age may be inversely related to meningioma prognosis.
Meningiomas are characterized by high recurrence rates, and they tend to evolve into atypical and anaplastic subtypes (37). In the present study, 2/4 patients who underwent reoperation had a modified anatomopathologic diagnosis: meningothelial to atypical and atypical to anaplastic. Both tumors began to express p53 protein although they were previously negative, confirming the trend found in this study and the findings in the literature that meningiomas with more malignant features have higher p53 expression rates (17,28-30).
In conclusion, the present findings support a role of p53 protein in meningioma development and/or progression. Moreover, the presence of dopamine D2 receptor in over 90% of the analyzed meningioma samples, including those with higher histological malignancy, warrants further investigation of the therapeutic potential of dopaminergic agents to treat these tumors.
Footnotes
First published online.
References
- 1.Dolecek TA, Propp JM, Stroup NE, Kruchko C. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005-2009. Neuro Oncol. 2012;14((Suppl 5)):v1–v49. doi: 10.1093/neuonc/nos218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santana PA, Jr, Marie SKN, Aguiar PHP. Biologia molecular dos meningiomas: um caminho promissor para a sua abordagem? In: Aguiar PHP, Ramina R, Veiga JCE, Tella O Jr, editors. Meningiomas - Diagnóstico e tratamento clínico e cirúrgico: aspectos gerais. 1st edn. Rio de Janeiro: Revinter; 2014. pp. 11–14. [Google Scholar]
- 3.Wahab M, Al-Azzawi F. Meningioma and hormonal influences. Climacteric. 2003;6:285–292. doi: 10.1080/713605429. [DOI] [PubMed] [Google Scholar]
- 4.Carroll RS, Zhang J, Dashner K, Sar M, Wilson EM, Black PM. Androgen receptor expression in meningiomas. J Neurosurg. 1995;82:453–460. doi: 10.3171/jns.1995.82.3.0453. [DOI] [PubMed] [Google Scholar]
- 5.Leaes CG, Meurer RT, Coutinho LB, Ferreira NP, Pereira-Lima JF, da Costa OM. Immunohistochemical expression of aromatase and estrogen, androgen and progesterone receptors in normal and neoplastic human meningeal cells. Neuropathology. 2010;30:44–49. doi: 10.1111/j.1440-1789.2009.01047.x. [DOI] [PubMed] [Google Scholar]
- 6.Friend KE, Radinsky R, McCutcheon IE. Growth hormone receptor expression and function in meningiomas: effect of a specific receptor antagonist. J Neurosurg. 1999;91:93–99. doi: 10.3171/jns.1999.91.1.0093. [DOI] [PubMed] [Google Scholar]
- 7.Reubi JC, Maurer R, Klijn JG, Stefanko SZ, Foekens JA, Blaauw G, et al. High incidence of somatostatin receptors in human meningiomas: biochemical characterization. J Clin Endocrinol Metab. 1986;63:433–438. doi: 10.1210/jcem-63-2-433. [DOI] [PubMed] [Google Scholar]
- 8.Schrell UM, Fahlbusch R, Adams EF, Nomikos P, Reif M. Growth of cultured human cerebral meningiomas is inhibited by dopaminergic agents. Presence of high affinity dopamine-D1 receptors. J Clin Endocrinol Metab. 1990;71:1669–1671. doi: 10.1210/jcem-71-6-1669. [DOI] [PubMed] [Google Scholar]
- 9.Carroll RS, Schrell UM, Zhang J, Dashner K, Nomikos P, Fahlbusch R, et al. Dopamine D1, dopamine D2, and prolactin receptor messenger ribonucleic acid expression by the polymerase chain reaction in human meningiomas. Neurosurgery. 1996;38:367–375. doi: 10.1097/00006123-199602000-00027. [DOI] [PubMed] [Google Scholar]
- 10.Pivonello R, Ferone D, Lombardi G, Colao A, Lamberts SW, Hofland LJ. Novel insights in dopamine receptor physiology. Eur J Endocrinol. 2007;156((Suppl 1)):S13–S21. doi: 10.1530/eje.1.02353. [DOI] [PubMed] [Google Scholar]
- 11.An JJ, Cho SR, Jeong DW, Park KW, Ahn YS, Baik JH. Anti-proliferative effects and cell death mediated by two isoforms of dopamine D2 receptors in pituitary tumor cells. Mol Cell Endocrinol. 2003;206:49–62. doi: 10.1016/S0303-7207(03)00236-3. [DOI] [PubMed] [Google Scholar]
- 12.Kanasaki H, Fukunaga K, Takahashi K, Miyazaki K, Miyamoto E. Involvement of p38 mitogen-activated protein kinase activation in bromocriptine-induced apoptosis in rat pituitary GH3 cells. Biol Reprod. 2000;62:1486–1494. doi: 10.1095/biolreprod62.6.1486. [DOI] [PubMed] [Google Scholar]
- 13.Adams EF, Schrell UM, Fahlbusch R, Thierauf P. Hormonal dependency of cerebral meningiomas. Part 2: In vitro effect of steroids, bromocriptine, and epidermal growth factor on growth of meningiomas. J Neurosurg. 1990;73:750–755. doi: 10.3171/jns.1990.73.5.0750. [DOI] [PubMed] [Google Scholar]
- 14.Hollstein M, Sidransky D, Vogelstein B, Harris CC. p53 mutations in human cancers. Science. 1991;253:49–53. doi: 10.1126/science.1905840. [DOI] [PubMed] [Google Scholar]
- 15.Verheijen FM, Sprong M, Kloosterman JM, Blaauw G, Thijssen JH, Blankenstein MA. TP53 mutations in human meningiomas. Int J Biol Markers. 2002;17:42–48. doi: 10.5301/jbm.2008.3174. [DOI] [PubMed] [Google Scholar]
- 16.Pavelin S, Becic K, Forempoher G, Tomic S, Capkun V, Drmic-Hofman I, et al. The significance of immunohistochemical expression of merlin, Ki-67, and p53 in meningiomas. Appl Immunohistochem Mol Morphol. 2014;22:46–49. doi: 10.1097/PAI.0b013e318289f490. [DOI] [PubMed] [Google Scholar]
- 17.Cho H, Ha SY, Park SH, Park K, Chae YS. Role of p53 gene mutation in tumor aggressiveness of intracranial meningiomas. J Korean Med Sci. 1999;14:199–205. doi: 10.3346/jkms.1999.14.2.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stefaneanu L, Kovacs K, Horvath E, Buchfelder M, Fahlbusch R, Lancranjan L. Dopamine D2 receptor gene expression in human adenohypophysial adenomas. Endocrine. 2001;14:329–336. doi: 10.1385/ENDO:14:3:329. [DOI] [PubMed] [Google Scholar]
- 20.Meurer RT, Martins DT, Hilbig A, Ribeiro MC, Roehe AV, Barbosa-Coutinho LM, et al. Immunohistochemical expression of markers Ki-67, neun, synaptophysin, p53 and HER2 in medulloblastoma and its correlation with clinicopathological parameters. Arq Neuropsiquiatr. 2008;66:385–390. doi: 10.1590/S0004-282X2008000300020. [DOI] [PubMed] [Google Scholar]
- 21.Pitella S, Jr, Hahn MD, Chimelli L, et al. Sistema nervoso. In: Brasileiro Filho G, editor. Bogliolo patologia. 8th edn. Rio de Janeiro: Guanabara Koogan; 2011. pp. 1008–1009. [Google Scholar]
- 22.Hilbig A, Barbosa-Coutinho LM. Meningiomas and hormonal receptors. Immunohistochemical study in typical and non-typical tumors. Arq Neuropsiquiatr. 1998;56:193–199. doi: 10.1590/S0004-282X1998000200005. [DOI] [PubMed] [Google Scholar]
- 23.Nakasu S, Fukami T, Jito J, Nozaki K. Recurrence and regrowth of benign meningiomas. Brain Tumor Pathol. 2009;26:69–72. doi: 10.1007/s10014-009-0251-2. [DOI] [PubMed] [Google Scholar]
- 24.Kim MS, Kim KH, Lee EH, Lee YM, Lee SH, Kim HD, et al. Results of immunohistochemical staining for cell cycle regulators predict the recurrence of atypical meningiomas. J Neurosurg. 2014;121:1189–1200. doi: 10.3171/2014.7.JNS132661. [DOI] [PubMed] [Google Scholar]
- 25.Adimoolam S, Ford JM. p53 and regulation of DNA damage recognition during nucleotide excision repair. DNA Repair. 2003;2:947–954. doi: 10.1016/S1568-7864(03)00087-9. [DOI] [PubMed] [Google Scholar]
- 26.Soussi T, Dehouche K, Beroud C. p53 website and analysis of p53 gene mutations in human cancer: forging a link between epidemiology and carcinogenesis. Hum Mutat. 2000;15:105–113. doi: 10.1002/(SICI)1098-1004(200001)15:1<105::AID-HUMU19>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 27.Matsuno A, Nagashima T, Matsuura R, Tanaka H, Hirakawa M, Murakami M, et al. Correlation between MIB-1 staining index and the immunoreactivity of p53 protein in recurrent and non-recurrent meningiomas. Am J Clin Pathol. 1996;106:776–781. doi: 10.1093/ajcp/106.6.776. [DOI] [PubMed] [Google Scholar]
- 28.Lanzafame S, Torrisi A, Barbagallo G, Emmanuele C, Alberio N, Albanese V. Correlation between histological grade, MIB-1, p53, and recurrence in 69 completely resected primary intracranial meningiomas with a 6 year mean follow-up. Pathol Res Pract. 2000;196:483–488. doi: 10.1016/S0344-0338(00)80050-3. [DOI] [PubMed] [Google Scholar]
- 29.Amatya VJ, Takeshima Y, Sugiyama K, Kurisu K, Nishisaka T, Fukuhara T, et al. Immunohistochemical study of Ki-67 (MIB-1), p53 protein, p21WAF1, and p27KIP1 expression in benign, atypical, and anaplastic meningiomas. Hum Pathol. 2001;32:970–975. doi: 10.1053/hupa.2001.27119. [DOI] [PubMed] [Google Scholar]
- 30.Karamitopoulou E, Perentes E, Tolnay M, Probst A. Prognostic significance of MIB-1, p53, and bcl-2 immunoreactivity in meningiomas. Hum Pathol. 1998;29:140–145. doi: 10.1016/S0046-8177(98)90224-6. [DOI] [PubMed] [Google Scholar]
- 31.Pavelin S, Becic K, Forempoher G, Mrklic I, Pogorelic Z, Titlic M, et al. Expression of Ki-67 and p53 in meningiomas. Neoplasma. 2013;60:480–485. doi: 10.4149/neo_2013_062. [DOI] [PubMed] [Google Scholar]
- 32.Feng Z, Hu W, Teresky AK, Hernando E, Cordon-Cardo C, Levine AJ. Declining p53 function in the aging process: a possible mechanism for the increased tumor incidence in older populations. Proc Natl Acad Sci U S A. 2007;104:16633–16638. doi: 10.1073/pnas.0708043104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Castelo-Branco C, Martinez MJ, Balasch J. Further data favouring hormonal dependency of cerebral meningiomas: evidence from a patient treated with cabergoline. Gynecol Endocrinol. 2011;27:134–137. doi: 10.3109/09513590.2010.487620. [DOI] [PubMed] [Google Scholar]
- 34.Schrell UM, Nomikos P, Fahlbusch R. Presence of dopamine D1 receptors and absence of dopamine D2 receptors in human cerebral meningioma tissue. J Neurosurg. 1992;77:288–294. doi: 10.3171/jns.1992.77.2.0288. [DOI] [PubMed] [Google Scholar]
- 35.Russell DS, Rubinstein LJ. Pathology of tumours of the nervous system. 5th edn. London: Edward Arnold; 1989. [Google Scholar]
- 36.Kamei Y, Watanabe M, Nakayama T, Kanamaru K, Waga S, Shiraishi T. Prognostic significance of p53 and p21WAF1/CIP1 immunoreactivity and tumor micronecrosis for recurrence of meningiomas. J Neurooncol. 2000;46:205–213. doi: 10.1023/A:1006440430585. [DOI] [PubMed] [Google Scholar]
- 37.LeMay DR, Bucci MN, Farhat SM. Malignant transformation of recurrent meningioma with pulmonary metastases. Surg Neurol. 1989;31:365–368. doi: 10.1016/0090-3019(89)90068-2. [DOI] [PubMed] [Google Scholar]


