Abstract
This study examined the utility of a lifetime cumulative adversities and trauma model in predicting the severity of mental health symptoms of depression, anxiety, and posttraumatic stress disorder. We also tested whether ethnicity and gender moderate the effects of this stress exposure construct on mental health using multigroup structural equation modeling. A sample of 500 low-socioeconomic status African American and Latino men and women with histories of adversities and trauma were recruited and assessed with a standard battery of self-report measures of stress and mental health. Multiple-group structural equation models indicated good overall model fit. As hypothesized, experiences of discrimination, childhood family adversities, childhood sexual abuse, other childhood trauma, and chronic stresses all loaded on the latent cumulative burden of adversities and trauma construct (CBAT). The CBAT stress exposure index in turn predicted the mental health status latent variable. Although there were several significant univariate ethnic and gender differences, and ethnic and gender differences were observed on several paths, there were no significant ethnic differences in the final model fit of the data. These findings highlight the deleterious consequences of cumulative stress and trauma for mental health and underscore a need to assess these constructs in selecting appropriate clinical interventions for reducing mental health disparities and improving human health.
Keywords: discrimination, stress, trauma, racial minorities
Extensive mental and physical health disparities exist among racial/ethnic groups (Jackson, Knight, & Rafferty, 2010; Karter et al., 2002; Krieger, Chen, Waterman, Rehkopf, & Subramanian, 2005). Many theories have been proposed to explain the robustness of these ethnic-based differences, including psychosocial stress models that suggest that minorities experience unique stressors that strongly impact health (Dressler, Oths, & Gravlee, 2005). These stressors include discrimination based on ethnicity and having multiple traumatic experiences. The need for research to guide prevention and intervention efforts to reduce these disparities is particularly relevant for African Americans and Latinos who carry a disproportionally high burden of physical and mental health disorders (Krieger et al., 2005; Myers, 2009).
Several large-scale epidemiological studies have recently confirmed that exposure to acute and chronic early life adversities and trauma is associated with increased risk for adult psychiatric disorders (Benjet, Borges, & Medina-Mora, 2010; Green et al., 2010; McLaughlin et al., 2010). For example, a greater number of childhood abuses predicts increased risk for adult depression (Chapman et al., 2004), health risk behaviors (Felitti et al., 1998), and for violence victimization and perpetration in adulthood (Whitfield, Anda, Dube, & Felitti, 2003). African Americans and Latinos, who often carry the greatest childhood exposure to adversities and traumas, are often underrepresented in these studies (Turner & Lloyd, 2004). Furthermore, these groups face ongoing adult trauma and chronic adversities, including the stress of racism and discrimination that is associated with their socioeconomic status (SES; Finch, Kolody, & Vega, 2000; Myers, 2009), national origin, and/or sexual minority status (Ayala, Bingham, Kim, Wheeler, & Millett, 2012; Glover, Williams, & Kissler, 2012).
For these reasons, there is a great need for research on lifetime exposure to adversities and trauma that include community samples of men and women from diverse ethnic and linguistic backgrounds (Delany-Brumsey, Joseph, Myers, Ullman, & Wyatt, 2011; Glover et al., 2010; Wyatt, Myers, & Loeb, 2004). In particular, there is a need to understand how early life traumas predict negative mental health outcomes, such as depression, anxiety, and posttraumatic stress disorder (PTSD), in these populations. Potential gender differences in the impact of these experiences also are poorly understood and require additional investigation (Greenfield, 2010; Grella, Stein, & Greenwell, 2005).
Lifetime Adversities and Traumas and Their Relations to Mental Health
Recent epidemiologic studies have indicated that a substantial percentage of people in the general population reported experiencing multiple types of trauma and adversities before reaching adulthood (e.g., Kessler, 2000). Early acute adversities include life events such as the death of a parent and witnessing violence or physical abuse. Chronic adversities include stressful experiences such as family financial difficulties, parental divorce or other separation from parents or caregivers, neglect, and life-threatening childhood illness, as well as parental maladjustment including mental illness, substance abuse, and criminality (Green et al., 2010). A large number of studies also have documented the extensive negative consequences of childhood sexual abuse (CSA) and its role as a vulnerability factor that enhances risk for mental health outcomes in both women and men. CSA is associated with elevated risk for depression (Putnam, 2003), PTSD (Cougle, Timpano, Sachs-Ericsson, Keough, & Riccardi, 2010; Glover et al., 2010; Sumner, Wong, Schetter, Myers, & Rodriguez, 2012), anxiety (Gold, Lucenko, Elhai, Swingle, & Sellers, 1999), substance use/abuse (Myers et al., 2009), and adult sexual abuse and high risk sexual behaviors (Loeb et al., 2002; Myers et al., 2006; Wyatt, Carmona, Loeb, Ayala, & Chin, 2002). Symptoms of depression and PTSD often co-occur, and comorbid PTSD and major depression have been found to be associated with trauma exposure (Delany-Brumsey et al., 2011). Furthermore, exposure to episodic and chronic life stresses in adulthood (e.g., chronic socioeconomic stresses, social instability, multiple losses, experiences of discrimination) also have been associated with an exacerbation of risk for, and severity of, chronic diseases and psychiatric disorders in adults, especially in those with preexisting early vulnerabilities (Breslau, Davis, Andreski, & Peterson, 1991; Halfon & Hochstein, 2002).
Discrimination is a construct that reflects an individual’s selfreported experiences of discrimination. Pascoe and Smart Richman (2009) defined it as “a behavioral manifestation of a negative attitude, judgment, or unfair treatment toward members of a group” (p. 533). Many minority groups have reported subtle and overt stressful discrimination experiences as part of their daily lives (Myers, 2009; Sue et al., 2007). Most research has focused on the relations between mental health outcomes and experiences of discrimination, with higher perceived discrimination being consistently associated with poorer mental health, including symptoms of anxiety, depression, and PTSD (e.g., Jackson et al., 1996; Kessler et al., 2010; Lee & Ahn, 2011; Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009). Although the effects of discrimination on physical health has received less research attention relative to mental health, discrimination has been found to be associated with chronic health conditions and with self-reported indicators of poor physical health in several large cross-sectional studies and reviews (Mays, Cochran, & Barnes, 2007; Smedley, 2012; Williams & Mohammed, 2009).
Recent studies have extended these analyses by investigating how cumulative lifetime exposure to these adversities and traumas impacts multiple mental and physical health outcomes. Studies using sum exposure scores have reported that greater cumulative exposure predicts negative mental health outcomes in adolescence and adulthood (Green et al., 2010; McLaughlin et al., 2010; Schilling, Aseltine, & Gore, 2008; Seery, Holman, & Silver, 2010; Toussaint, Shields, Dorn, & Slavich, 2014; Wickrama, Conger, & Abraham, 2005). For example, recent data from the U.S. National Comorbidity Survey Replication (McLaughlin et al., 2010) indicate that whereas childhood financial hardship predicts first onset of several psychiatric disorders, including anxiety, mood, behavioral, and substance disorders across the life span, this effect appears to be due to its association with greater exposure to multiple childhood family traumas rather than to childhood financial hardship per se (McLaughlin et al., 2010).
Taken together, the available evidence indicates that the cumulative effect of these adverse experiences account for greater risk and vulnerability, even when compared to other individual sources of early or later adversity or trauma (Kessler, 2000). Although there is growing evidence for the potential fruitfulness of a cumulative approach to investigating the detrimental effects of lifetime histories of exposure to adversities and traumas on mental health (Schilling et al., 2008; Schumm, Briggs-Phillips, & Hobfoll, 2006; Seery et al., 2010), there continues to be debate about the best method for estimating these effects (i.e., sum scores of discrete experiences or using more comprehensive cumulative measures). It also remains unclear whether more advanced statistical methods (i.e., structural equation modeling; SEM) may advance our understanding of ethnic group disparities in health and mental health (Geronimus, Hicken, Keene, & Bound, 2006; Myers, 2009).
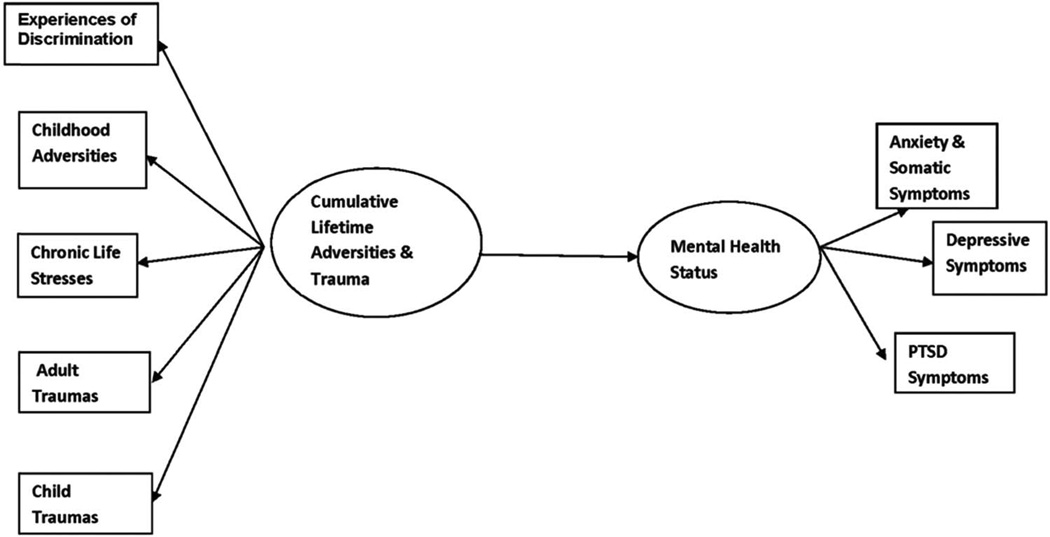
Therefore, the goal of the present study was to test a model of cumulative burden of adversities and trauma (CBAT) in a community sample of 500 low-SES African American and Latino/a men and women using SEM. It was designed to estimate the utility of CBAT in predicting risk for mental health symptoms (depression, anxiety, and PTSD), and to test whether ethnicity and gender moderate the hypothesized relationships in the model using multigroup SEM (see Figure 1). This approach provides a more holistic, multidimensional, and culturally relevant assessment of the cumulative lifetime burdens faced by many marginalized groups, especially those from racial/ethnic minority backgrounds.
Figure 1.
Conceptual model of cumulative lifetime adversities and trauma and mental health status in African Americans and Latino(as). PTSD = posttraumatic stress disorder.
Method
Participants and Procedure
A multiethnic sample of 500 participants, including 230 African Americans (167 men and 63 women) and 270 Latinos (50 men and 220 women) who reported histories of CSA and/or interpersonal violence (IPV) as adults were recruited to participate in four studies supported by the National Institute of Mental Health-funded Center for Culture, Trauma, and Mental Health Disparities. Three of the studies consisted of participants with self-reported experiences of child sexual abuse before the age of 18 years, and one study enrolled participants who reported previous experiences of spousal abuse. Participants in the four studies were recruited from a variety of community clinics and community-based organizations in south central Los Angeles, California following procedures that were approved by the Institutional Review Board at the University of California, Los Angeles and Charles R. Drew University of Medicine & Science. Community clinics and social service organizations that serve primarily low-income African American and Latino clients were approached to obtain their support in allowing the project teams to recruit at their agency. Both direct recruitment and staff referrals were used and all who expressed interest were prescreened by a trained multiethnic, multicultural team and enrolled in one of the four studies. Study-specific flyers and word-of-mouth referrals were used to supplement direct recruitment. Descriptions of the recruitment procedures have been previously published (see Glover et al., 2010; Glover, Williams, & Kissler, 2012; Rodriguez, Heilemann, Fielder, Ang, Nevarez, & Mangione, 2008 for more detailed descriptions of the recruitment procedures).
A standard core battery of psychosocial measures was administered in private sessions. The interview team included highly trained, culturally competent African American and Latina women who interviewed English-speaking African American and Latino men and women. The team was trained in 1-week workshops that were designed to sensitize interviewers to the fact that underserved populations often have not disclosed their trauma histories, and likely have not participated in research studies examining these experiences. Transportation, childcare, and refreshments were provided, and signed informed consents were obtained. Assessments were conducted in a standardized fashion for all participants. CSA and adult trauma questions were completed in face-to-face interviews due to the sensitive nature of the topics. All of the other measures were administered on laptop computers equipped with the audio computer-assisted self-interview system. All of the measures have been used and shown to be reliable in previous studies with this population. Assessments conducted in Spanish were translated and back-translated to ensure their appropriateness for use with monolingual Spanish-speaking participants. The assessment sessions lasted a maximum of 2.5 hrs and all participants received compensation up to $100, depending on time required to complete the study protocol. All participants received referral information for mental health and other services.
Measures
Self-reported demographic characteristics included age, race/ethnicity, personal and household income in the past year, years of education, employment (full/part-time, not employed), self-identified sexual orientation, and marital/relationship status.
Predictor Variables
The key predictors of interest were childhood family adversities, childhood traumas (i.e., CSA, other nonsexual traumas), adult adversities (i.e., chronic stress, experiences of discrimination), and adult sexual and nonsexual traumas.
Childhood family adversities were assessed with a brief 10-item version of the Family Adversity Questionnaire (Kessler & Magee, 1993). This questionnaire assessed participants’ number of nonsexual, adverse early life experiences (e.g., parental incarceration, illness, disability, death, severe poverty, etc.), and a reliable (α = .83) sum score was calculated and used in the analyses.
CSA was assessed with nine screening items from the Wyatt Sexual History Questionnaire–Revised (WSHQ–R), a 478-item structured interview that assesses consensual and nonconsensual sexual experiences (Wyatt, Lawrence, Voudonon, & Mickey, 1993). Participants were classified as experiencing CSA if they responded “yes” to any questions related to sexual experiences with an adult or with someone 5 years older before the age of 18 years, or if they were coerced in a sexual encounter by a perpetrator who was less than 5 years older than the victim (Loeb, Gaines, Wyatt, Zhang, & Liu, 2011). A reliable (α = .85) standardized composite severity of CSA was calculated by summing responses to each of four dimensions (i.e., type of physical contact, age at the time of the abuse, frequency of the abuse, and relationship of the victim to the perpetrator) for each CSA incident reported (Loeb et al., 2011) and used in the analyses.
Other childhood trauma was assessed with 13 questions about nonsexual abuse experiences such as physical abuse, disasters, accidents, exposure to community violence from the revised Green (1996) Trauma History Questionnaire, and a reliable (α = .80) sum score was calculated and used in the analyses.
Chronic life stresses was assessed with 15 items from the Chronic Burden Scale (Gurung, Taylor, Kemeny, & Myers, 2004) that measure difficulties experienced in the past month from a number of stressors (e.g., economic, employment, crime, legal problems). Respondents were asked to rate the degree to which each source of stress is a problem for them, with ratings ranging from 1 (not a problem) to 4 (a major problem), and a reliable (α = .84) sum score was calculated and used in the analyses.
Experiences of discrimination due to one’s race/ethnicity was assessed with the 17-item Brief Perceived Ethnic Discrimination Questionnaire–Community Version (Brondolo et al., 2005). This measure asks respondents to rate on a 5-point scale ranging from 1 (never) to 5 (very often) the frequency with which they experienced various forms of unfair treatment because of their ethnicity/race, such as “Because of your ethnicity/race…” “How often have policemen or security officers been unfair to you?” “Have you been treated unfairly by coworkers or classmates?” “Have people not trusted you?” “Has it been hinted that you must be lazy?” A very reliable (α = .94) sum score was calculated and used in the analyses.
Adult trauma was assessed with a series of yes/no items, including two questions about experiences of sexual abuse as an adult (i.e., attempted or completed rape as an adult); five questions about adult experiences of IPV from the Abuse Assessment Screen (Soeken, Parker, McFarlane, & Lominack, 1998) that inquired about psychological, physical, and sexual abuse experiences with a primary partner in the last 12 months; and nine questions about other adult trauma experiences (i.e., nonsexual or physical abuse experiences such as disasters, accidents, exposure to community violence) from the revised Green (1996) Trauma History Questionnaire. A reliable sum score (α = .75) was calculated for all items responded to as yes and used in the analyses.
All of these childhood and adult adversities and trauma experiences are conceptualized collectively as indicators of a CBAT latent construct.
Outcome Variables
The primary outcome of interest was mental health status as a latent construct that was indexed by severity of depression, somatic symptoms of anxiety, and PTSD symptoms.
Severity of depression symptoms was assessed with the 20-item Center for Epidemiological Studies–Depression Scale (CES–D; Radloff, 1977) that asked participants to rate the frequency with which they experienced each symptom in the last 2 weeks on a 4-point Likert-type scale ranging from 0 (not at all) to 3 (every day or almost every day). A very reliable sum score (α = .91) was calculated, with higher scores indicating more severe depression.
Severity of PTSD symptoms was assessed with the 17-item Posttraumatic Diagnostic Scale (Foa, Cashman, Jaycox, & Perry, 1997) that asks respondents to appraise the “worst” traumatic event experienced. Each item was rated on a 4-point Likert-type scale ranging from 0 (not at all or only 1 time) to 3 (5 or more times a week or almost always). A very reliable (α = .92) sum score was calculated, with higher scores indicating more severe symptoms.
Severity of anxiety and somatic symptoms was assessed with the 13-item Patient Health Questionnaire (PHQ–13; Kroenke & Spitzer, 2002). The measure asked respondents to rate how often in the last 2 weeks they experienced any of the 13 anxiety symptoms on a 4-point scale ranging from 0 (not at all) to 3 (nearly every day) and yielded a reliable sum score (α = .83), with higher scores indicating more severe somatic anxiety.
Data Analysis
A series of 2 (ethnicity) × 2 (gender) analyses of variances were conducted testing for differences on the demographic, psychosocial predictors, and psychiatric symptom outcomes. The means, standard deviations, and the tests of significant differences between the groups for all study measures are presented in Table 1.
Table 1.
Means and Tests of Group Differences on Main Study Variables
| African Americans | Latino/as | ||||||
|---|---|---|---|---|---|---|---|
| Variables | Men | Women | Men | Women | p(E) | p(G) | p(E × G) |
| Demographics | |||||||
| Age | 45.30 (9.17) | 36.70 (9.22) | 31.07 (9.02) | 33.53 (7.41) | <.001 | <.001 | <.001 |
| % <high school education | 36.17 (n = 34) | 13.83 (n = 13) | 6.38 (n < 6) | 43.62 (n < 41) | <.02 | <.01 | ns |
| % low income (<1,290 per month) | 62.36 (n = 111) | 6.274 (n = 12) | 7.87 (n < 14) | 23.03 (n < 44) | <.001 | <.02 | ns |
| % unemployed | 46.12 (n = 107) | 15.95 (n = 37) | 7.33 (n < 17) | 30.6 (n < 71) | ns | ns | ns |
| Psychosocial predictors | |||||||
| Family adversity | 3.96 (2.85) | 5.11 (3.114) | 6 (2.74) | 3.61 (2.79) | ns | ns | <.001 |
| Chronic stress | 33.04 (9.90) | 30.20 (11.35) | 38.59 (13.05) | 27.07 (8.42) | <.05 | <.001 | <.002 |
| Perceived discrimination | 36.11 (11.95) | 38.04 (13.44) | 34.52 (12.3) | 27.4 (10.26) | <.001 | <.001 | <.01 |
| CSA | 13.3 (2.25) | 13.08 (2.04) | 13.48 (1.93) | 6.03 (6.67) | <.001 | <.001 | <.001 |
| ASA | 0.75 (1.25) | 1.09 (1.4) | 0.38 (0.98) | 0.35 (0.91) | <.001 | ns | ns |
| IPV | 1.30 (1.46) | 2.36 (1.84) | 1.52 (1.5) | 1.57 (1.64) | ns | <.01 | <.03 |
| Other child trauma | 3.13 (3.0) | 3.49 (3.13) | 5.41 (4.65) | 2.23 (2.58) | ns | <.02 | <.001 |
| Other adult trauma | 3.86 (3.12) | 3.02 (2.78) | 2.52 (2.08) | 2.89 (2.60) | <.01 | <.04 | ns |
| Psychiatric symptoms | |||||||
| PTSD | 9.90 (10.76) | 15.89 (12.08) | 13.31 (9.06) | 11.66 (9.90) | ns | <.03 | <.02 |
| Anxiety | 4.69 (4.50) | 7.30 (4.56) | 5.97 (4.97) | 5.59 (4.28) | ns | <.02 | <.02 |
| Depression | 15.72 (11.18) | 21.13 (13.44) | 18.76 (12.04) | 15.1 (10.89) | ns | ns | <.01 |
Note. N = 500. African Americans: n = 180, African American men: n = 167, African American women: n = 63; Latino/as: n = 120, Latinos: n = 50, Latinas: n = 220. Standard deviations are given in parentheses. E = ethnicity; G = gender; CSA = child sexual abuse; ASA = adult sexual abuse; IPV = interpersonal violence (i.e., spousal abuse); PTSD = posttraumatic stress disorder.
Hypotheses were tested using multiple-group analysis within a SEM (Ullman, 2013). The models were estimated using maximum likelihood estimation and evaluated using the Yuan–Bentler scaled chi-square that is appropriate for models estimated with nonnormal data (Yuan & Bentler, 2000). Goodness-of-fit models were evaluated with both the root mean square error of approximation (RMSEA) and the comparative fit index (CFI); good-fitting models have RMSEAs < .06 and CFI indexes > .95 (Ullman, 2013).
In multiple-group analysis within a structural equation model, a series of models were tested. First, good-fitting models were established separately in each subgroup of participants (Latino, African American). The fit of the model and the significance of the prediction paths were tested within each model. The multiple-group models were then examined to test differences across the two groups. This multiple-group model is called the baseline model. In the baseline model, all of the path coefficients were allowed to vary across groups. A series of analyses in which paths are constrained (the coefficients are statistically forced to be equal) across the groups were conducted testing hypotheses about the ethnic group as a moderator. The hypothesized model tested in each group is presented in Figure 1. The indicators (i.e., measured variables) of the constructs are reported in Table 1. EQS 6.1 (Bentler & Wu, 2005) was employed for all analyses.
Results
Table 1 shows the means, standard deviations, and tests of group differences for all variables. The sample had a mean age of 39 years, was generally low-SES (73.25% with incomes at or below $1,249 per month), and unemployed (77.23%). However, the majority (68.46%) had at least a high school education. As shown in Table 1, there were a number of significant gender and ethnic group differences on several of the CBAT indicators and mental health outcomes, which suggest the need to investigate possible group differences in the pattern of relations in the hypothesized CBAT model.
Tests of Model Assumptions
There was evidence that multivariate normality was violated in each group (i.e., Mardia’s (1985) normalized coefficients were 12.97 and 6.3 in the Latino and African American samples, respectively, (ps < .001). There were no outliers. Given the non-normality, all models were estimated with maximum likelihood estimation and evaluated with the Yuan–Bentler scaled chi-square (Yuan & Bentler, 2000).
Separate SEM Models
The hypothesized model in Figure 1 was tested for each group individually and there was evidence that the two models fit well: Latino sample, Yuan–Bentler χ2(38, N = 270) = 84.71, p < .05, CFI = .94; African American sample Yuan–Bentler χ2(38, N = 230) = 56.64, p = .01, CFI = .97.
Multiple-Group Modeling Series of Models
Each model fit the data well; therefore, we then analyzed a series of models to test hypotheses about the role of ethnicity in moderating the strength of the relationships in the model. First, a baseline model was estimated with both groups simultaneously. This model fit the data well, Yuan–Bentler χ2(76, N = 500) = 145.34, p < .05, CFI = .95, and thus served as the comparison model for subsequent models tested.
Next, we examined whether ethnicity moderated the measurement model. To test these effects, a model was estimated to test that the path coefficients from the CBAT and mental health status latent constructs to their respective measured variables were statistically equivalent across groups. This model did not fit the data and had a significantly worse fit than the baseline model, Yuan–Bentler χ2(84, N = 500) = 263.01, p < .05, CFI = .89. This indicates that one or more of the relations in the model differed as a function of ethnicity.
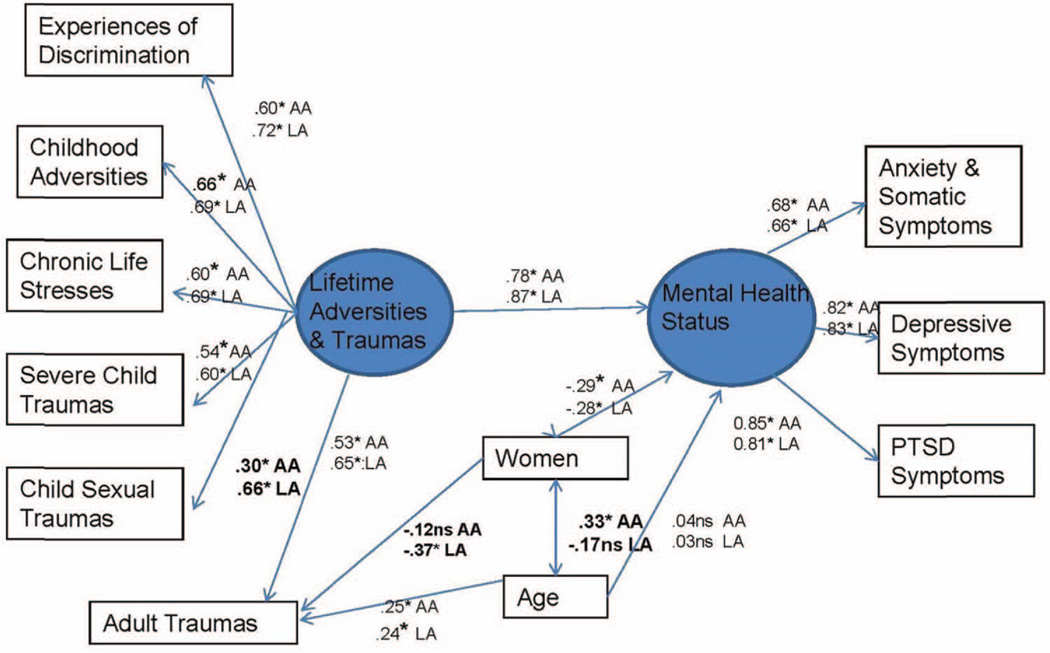
Using theoretical relevance and the Lagrange multiplier test, we next estimated a model that allowed the strength of the association between child sexual trauma and lifetime CBAT to differ between the Latino and African American sample. This model fit the data extremely well, Yuan–Bentler χ2(83, N = 500) = 84.183, p = .44, CFI = .99. The relation between lifetime adversity and child sexual trauma was stronger in the Latino sample versus the African American sample (unstandardized coefficient Latino sample = 6.41, African American sample = .71).
Next, we examined whether ethnicity moderated the relationship between the structural models. To test these effects, a model was estimated that tested the statistical equivalence of the regression paths between CBAT and mental health and the gender and age relationships. This model also fit the data well, Yuan–Bentler χ2(86, N = 500) = 86.987, p = .44, CFI = .99, and was significantly different from the baseline model. This indicates that ethnicity did not moderate the structural relationships in the model.
A final model tested the statistical equivalence of the covariances between the gender, age, and CBAT. Although the model did fit the data well, when these covariances were statistically forced to be equal, Yuan–Bentler χ2(89, N = 500) = 133.98, p < .01 CFI = .97, the model was significantly worse than the baseline model. This means that the covariances between gender and age, age and CBAT, and gender and CBAT differed by ethnicity. In the Latino sample, the correlations between gender (women) and age = −.17, p < .05, and gender (women) and CBAT = .58 p < .05 were significant, but age and CBAT = −.13, p > .05 was not. In the African American sample, the correlations between gender (women) and age = .33 p < .05, age and CBAT = −.20, p < .05 were significant, and gender (women) and CBAT was not = −.03, p > .05. Therefore, although there was no association between gender and CBAT in the sample as a whole, there was suggestive evidence that the Latinas were more likely to experience higher cumulative burden of adversity and trauma than the Latino men, but no such difference was found among the African Americans. The final model with significant standardized coefficients is presented in Figure 2.
Figure 2.
Final model of cumulative lifetime adversities and trauma and mental health by ethnic group (standardized coefficient). AA = African American; LA = Latino/Latina; PTSD = posttraumatic stress disorder. * p < .05. See the online article for the color version of this figure.
Discussion
Although there is growing evidence for the potential fruitfulness of a cumulative approach to investigating the detrimental effects of lifetime histories of exposure to adversities and traumas on mental health (Schilling et al., 2008; Schumm et al., 2006; Seery et al., 2010), there continues to be debate about the best method for estimating these effects (i.e., sum scores of discrete experiences or using more comprehensive cumulative measures). It also remains unclear whether more advanced statistical methods may advance our understanding of ethnic group disparities in health and mental health (Geronimus et al., 2006; Myers, 2009). To address these issues, we used multigroup SEM to test a cumulative model of risk for psychological symptoms of distress in a sample of low-SES adult African Americans and Latinos/as who reported histories of adversities and traumas in childhood and adulthood (CBAT). These analyses confirmed hypothesized associations between experiences of greater lifetime adversities and trauma with poorer mental health status for both the overall sample and for each ethnic group. This study offers an important glimpse into these linkages in an understudied and underserved sample of men and women with high levels of chronic stress, perceived discrimination, and histories of severe child sexual and nonsexual trauma.
Contrary to expectations but consistent with some of the findings from Jackson and colleagues (1996), both the African Americans and Latinos(as) appear to be relatively resilient, despite their high burdens of adversities and traumas. Both groups reported relatively modest levels of PTSD and anxiety symptoms, but higher levels of depressive symptoms. The men and women in the sample reported severe histories of CSA involving penetration, with the men reporting higher levels of CSA severity than the women, and Latinas reporting the lowest levels of CSA severity. On the other hand, African American men and women reported significantly more incidents of adult sexual abuse than the Latinos(as), although Latino men reported significantly more incidents of sexual abuse as adults than the Latina women.
The sample also reported high levels of experiences of discrimination due to ethnicity, with African American men and women reporting higher levels of discrimination than Latinos(as), and African American women reported the highest levels overall and Latinas the lowest. This is one of the first studies to conceptualize and estimate the relative impact of experiences of discrimination in adulthood as part of a lifetime burden of adversities and traumas. This study supports that experiences of discrimination and other stressors in a latent factor characterizing histories of adversities and traumas, significantly predicts psychological distress and dysfunction. This occurred even though many of these adults had lower than expected symptoms of psychological distress, especially general anxiety and PTSD. Future studies should assess for experiences of discrimination in addition to chronic stress and other life adversities and traumas to confirm this finding and to determine whether these results generalize to other populations.
Although the path from cumulative lifetime adversities and traumas to mental health status was confirmed, both for the total sample and for each ethnic group separately, ethnicity was not a significant moderator in the final model. However, some of the associations between the latent constructs to their respective measured variables differed between the African American and Latino samples. In particular, the salience of childhood sexual abuse as a contributor to the CBAT construct was stronger for the Latino sample than for the African American sample. This finding supports the importance of testing for both the overall impact of these risk factors, as well as the possibility that there might be important ethnic group differences in the relative impact that some of these risk factors have. The model also suggests that the relation between adult trauma and mental health status was significant only in the Latina women in the sample, and that the relationship between age and mental health status was only significant in the African American women in the sample. In particular, Latina women reported the lowest adult trauma experiences and the lowest symptoms of PTSD, anxiety, and depression of all groups. On the other hand, African American women had the highest adult trauma scores and the highest psychological distress symptom scores, which suggests greater relative psychosocial vulnerability.
These results add to the growing evidence that a cumulative burden of lifetime adversities and traumas is a useful approach for testing for relative mental health risk (Schilling et al., 2008) among low-SES, high stressed populations, and for disentangling the effects that ethnicity and gender might play in these relationships. These results also support and extend previous findings of greater psychological resilience in these populations despite their high lifetime burdens of chronic stress, discrimination and trauma (Jackson et al., 2010; Seery et al., 2010), even when they evidence substantially greater risk for chronic illnesses than non-Hispanic Whites (Jackson et al., 2010). Although specific resilience factors were not modeled in this study, these groups could provide a basis for the development of resilience interventions. For example, breast cancer survivors demonstrate enhanced resilience when trained to adopt a more flexible (than fixed) view of challenges, and to increase their thoughts of compassion, acceptance, and forgiveness (Loprinzi, Prasad, Schroeder, & Sood, 2011). Likewise, African American communities use compassionate approaches (Daly, Jennings, Beckett, & Leashore, 1995) that could be instructive for such interventions.
A number of limitations of this study are worth noting. First, data from four source studies were used in the analyses, and although project differences were partially controlled for by testing for ethnicity and gender differences, there is no assurance that all of the study effects were effectively controlled. For example, sexual orientation likely varied between studies, but not all projects collected these data. Second, differences in sample sizes across ethnicity and gender groups likely limited our ability to detect some group differences. Therefore, studies with larger, gender-balanced and representative samples are needed to confirm these findings. Third, because all four studies were based on samples of convenience, additional research is needed to generalize the results described here to the general population. Fourth, the standardized measures of the three mental health outcomes used may miss some negative consequences of lifetime adversities and trauma, including assessing for clinically meaningful levels of disorders. Fifth, collecting retrospective data from participants during childhood and adulthood may underestimate the true magnitude of the adversities and traumas they experienced over their lifetime. To address this issue, future studies should use contemporaneous assessments of stress exposure in the context of a longitudinal study. Finally, neither the number of exposures experienced, nor the precise ages at which exposure to the adversities and trauma occurred, nor the possibility that there were varied times since the exposure to the adversities and trauma were addressed in this study. All of these could have affected the pattern of relationships observed.
Despite these limitations, this study makes a number of important contributions. First, it is one of the first studies to use a multidimensional assessment of the range of lifetime adversities and trauma that these populations experienced in estimating their risk for psychological distress and dysfunction. Second, established and reliable measures of the constructs of interest were used, and the contributions of the different life adversities and trauma to the overall burden of adversities and trauma were assessed. Third, ethnic differences on each of these paths were estimated. Fourth, the CBAT conceptual model was tested using multigroup SEM, which is a more efficient and statistically robust way of testing the hypothesized effect paths, both in the overall sample and for each ethnic group separately. Finally, three different measures of symptoms of psychological distress and dysfunction were used to estimate their relative mental health status, which is more robust and sensitive than using only one measure.
In summary, the present results are among the first to demonstrate the effects of childhood and adult adversities and traumas on levels of psychological distress symptoms in a multiethnic sample of adults with high burdens of adversities. This model applied equally well to both ethnic and gender groups, with only relatively few differences observed. These results are also consistent with previous findings of higher than expected levels of psychological resilience given the level of burden of adversities that these populations experience. An important next step in future studies using models such as this is to include the assessment of biomarkers to assess the biological mechanisms through which these psychosocial risk factors exert their effects.
Looking forward, the results support the need for more interventions that focus on reducing exposure to these negative contextual factors and more effective ways to bolster coping skills to reduce psychiatric risks. Additional studies are also needed that use a cumulative burden of risk approach with populations that differ by race/ethnicity, gender, and SES to precisely map targets for prevention interventions. This research should also confirm the present results with larger, more representative and ethnic and gender-balanced samples. In the meantime, these initial findings suggest that mental health and primary care providers should assess for lifetime history of adversities and trauma while assessing patients’ psychosocial history to better understand the determinants of patients’ current functioning.
Acknowledgments
Preparation of this article was supported by National Institute of Mental Health Grants P50 MH73453 and R34 MH077550. We thank Dorothy Glover and Erica Marchand for their contributions to previous drafts of this article. We also thank Whitney Cale and Rebecca Elbogen for their assistance in manuscript preparation.
Contributor Information
Hector F. Myers, Center for Medicine, Health, & Society and Psychology, Vanderbilt University
Gail E. Wyatt, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles
Jodie B. Ullman, Department of Psychology, California State University, San Bernardino
Tamra B. Loeb, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles
Dorothy Chin, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles.
Nicole Prause, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles.
Muyu Zhang, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles.
John K. Williams, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles
George M. Slavich, Cousins Center for Psychoneuroimmunology and Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles
Honghu Liu, School of Dentistry, University of California, Los Angeles.
References
- Ayala G, Bingham T, Kim J, Wheeler DP, Millett GA. Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. American Journal of Public Health. 2012;102(Suppl. 2):S242–S249. doi: 10.2105/AJPH.2011.300641. http://dx.doi.org/10.2105/AJPH.2011.300641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet C, Borges G, Medina-Mora ME. Chronic childhood adversity and onset of psychopathology during three life stages: Childhood, adolescence and adulthood. Journal of Psychiatric Research. 2010;44:732–740. doi: 10.1016/j.jpsychires.2010.01.004. http://dx.doi.org/10.1016/j.jpsychires.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Wu EJC. EQS 6.1 for Windows: User Guide. Encino, CA: Multivariate Software Inc.; 2005. [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. http://dx.doi.org/10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, Contrada RJ. The perceived ethnic discrimination questionnaire: Development and preliminary validation of a community version. Journal of Applied Social Psychology. 2005;35:335–365. http://dx.doi.org/10.1111/j.1559-1816.2005.tb02124.x. [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders. 2004;82:217–225. doi: 10.1016/j.jad.2003.12.013. http://dx.doi.org/10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Timpano KR, Sachs-Ericsson N, Keough ME, Riccardi CJ. Examining the unique relationships between anxiety disorders and childhood physical and sexual abuse in the National Comorbidity Survey–Replication. Psychiatry Research. 2010;177:150–155. doi: 10.1016/j.psychres.2009.03.008. http://dx.doi.org/10.1016/j.psychres.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Daly A, Jennings J, Beckett JO, Leashore BR. Effective coping strategies of African Americans. Social Work. 1995;40:240–248. [Google Scholar]
- Delany-Brumsey AD, Joseph NT, Myers HF, Ullman JB, Wyatt GE. Modeling the relationship between trauma and psychological distress among HIV-positive and HIV-negative women. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:69–76. doi: 10.1037/a0022381. http://dx.doi.org/10.1037/a0022381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: Models to explain health disparities. Annual Review of Anthropology. 2005;34:231–252. http://dx.doi.org/10.1146/annurev.anthro.34.081804.120505. [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. http://dx.doi.org/10.1016/ S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. Journal of Health and Social Behavior. 2000;41:295–313. http://dx.doi.org/10.2307/2676322. [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. http://dx.doi.org/10.1037/1040-3590.9.4.445. [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. http://dx.doi.org/10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover DA, Loeb TB, Carmona JV, Sciolla A, Zhang M, Myers HF, Wyatt GE. Childhood sexual abuse severity and disclosure predict posttraumatic stress symptoms and biomarkers in ethnic minority women. Journal of Trauma & Dissociation. 2010;11:152–173. doi: 10.1080/15299730903502920. http://dx.doi.org/10.1080/15299730903502920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover DA, Williams JK, Kissler KA. Using novel methods to examine stress among HIV-positive African American men who have sex with men and women. Journal of Behavioral Medicine. 2012;36:283–294. doi: 10.1007/s10865-012-9421-5. http://dx.doi.org/10.1007/s10865-012-9421-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold SN, Lucenko BA, Elhai JD, Swingle JM, Sellers AH. A comparison of psychological/psychiatric symptomatology of women and men sexually abused as children. Child Abuse & Neglect: The International Journal. 1999;23:683–692. doi: 10.1016/s0145-2134(99)00041-1. http://dx.doi.org/10.1016/S0145-2134(99)00041-1. [DOI] [PubMed] [Google Scholar]
- Green BL. Trauma history questionnaire. In: Stamm BH, Varra E, editors. Measurement of stress, trauma and adaptation. Lutherville, MD: Sidram Press; 1996. pp. 366–368. [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM–IV disorders. Archives of General Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. http://dx.doi.org/10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA. Child abuse as a life-course social determinant of adult health. Maturitas. 2010;66:51–55. doi: 10.1016/j.maturitas.2010.02.002. http://dx.doi.org/10.1016/j.maturitas.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Grella CE, Stein JA, Greenwell L. Associations among childhood trauma, adolescent problem behaviors, and adverse adult outcomes in substance-abusing women offenders. Psychology of Addictive Behaviors. 2005;19:43–53. doi: 10.1037/0893-164X.19.1.43. http://dx.doi.org/10.1037/0893-164X.19.1.43. [DOI] [PubMed] [Google Scholar]
- Gurung RAR, Taylor SE, Kemeny M, Myers HF. HIV is not my biggest problem: The impact of HIV and chronic burden on depression in women at risk for AIDS. Journal of Social and Clinical Psychology. 2004;23:490–511. http://dx.doi.org/10.1521/jscp.23.4.490.40305. [Google Scholar]
- Halfon N, Hochstein M. Life course health development: An integrated framework for developing health, policy, and research. The Milbank Quarterly. 2002;80:433–479. doi: 10.1111/1468-0009.00019. iii. http://dx.doi.org/10.1111/1468-0009-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Brown TN, Williams DR, Torres M, Sellers SL, Brown K. Racism and the physical and mental health status of African Americans: A thirteen year national panel study. Ethnicity & Disease. 1996;6:132–147. [PubMed] [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100:933–939. doi: 10.2105/AJPH.2008.143446. http://dx.doi.org/10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. Journal of the American Medical Association. 2002;287:2519–2527. doi: 10.1001/jama.287.19.2519. http://dx.doi.org/10.1001/jama.287.19.2519. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61(Suppl. 5):4–12. [PubMed] [Google Scholar]
- Kessler RC, Magee WJ. Childhood adversities and adult depression: Basic patterns of association in a US national survey. Psychological Medicine. 1993;23:679–690. doi: 10.1017/s0033291700025460. http://dx.doi.org/10.1017/S0033291700025460. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Williams DR. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. The British Journal of Psychiatry. 2010;197:378–385. doi: 10.1192/bjp.bp.110.080499. http://dx.doi.org/10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: The Public Health Disparities Geocoding Project. American Journal of Public Health. 2005;95:312–323. doi: 10.2105/AJPH.2003.032482. http://dx.doi.org/10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ–9: A new depression and diagnostic severity measure. Psychiatric Annals. 2002;32:509–515. Retrieved from http://www.lphi.org/LPHIadmin/uploads/.PHQ-9-Review-Kroenke-63754.PDF. [Google Scholar]
- Lee DL, Ahn S. Racial discrimination and Asian mental health: A meta analysis. The Counseling Psychologist. 2011;39:463–489. http://dx.doi.org/10.1177/0011000010381791. [Google Scholar]
- Loeb TB, Gaines T, Wyatt GE, Zhang M, Liu H. Associations between child sexual abuse and negative sexual experiences and revictimization among women: Does measuring severity matter? Child Abuse & Neglect. 2011;35:946–955. doi: 10.1016/j.chiabu.2011.06.003. http://dx.doi.org/10.1016/j.chiabu.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb TB, Williams JK, Carmona JV, Rivkin I, Wyatt GE, Chin D, Asuan-O’Brien A. Child sexual abuse: Associations with the sexual functioning of adolescents and adults. Annual Review of Sex Research. 2002;13:307–345. [PubMed] [Google Scholar]
- Loprinzi CE, Prasad K, Schroeder DR, Sood A. Stress management and resilience training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: A pilot randomized clinical trial. Clinical Breast Cancer. 2011;11:364–368. doi: 10.1016/j.clbc.2011.06.008. http://dx.doi.org/10.1016/j.clbc.2011.06.008. [DOI] [PubMed] [Google Scholar]
- Mardia KV. Mardia’s test of multi-normality. In: Kotz S, Johnson NL, editors. Encyclopedia of statistical sciences. Vol. 5. Cambridge, England: Cambridge University Press; 1985. pp. 217–221. [Google Scholar]
- Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annual Review of Psychology. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. http://dx.doi.org/10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication II: Associations with persistence of DSM–IV disorders. Journal of the American Medical Association Psychiatry. 2010;67:124–132. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers HF. Ethnicity- and socio-economic status-related stresses in context: An integrative review and conceptual model. Journal of Behavioral Medicine. 2009;32:9–19. doi: 10.1007/s10865-008-9181-4. http://dx.doi.org/10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- Myers HF, Sumner LA, Ullman JB, Loeb TB, Carmona JV, Wyatt GE. Trauma and psychosocial predictors of substance abuse in women impacted by HIV/AIDS. The Journal of Behavioral Health Services & Research. 2009;36:233–246. doi: 10.1007/s11414-008-9134-2. http://dx.doi.org/10.1007/s11414-008-9134-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers HF, Wyatt GE, Loeb TB, Carmona JV, Warda U, Longshore D, Liu H. Severity of child sexual abuse, post-traumatic stress and risky sexual behaviors among HIV-positive women. AIDS and Behavior. 2006;10:191–199. doi: 10.1007/s10461-005-9054-6. http://dx.doi.org/10.1007/s10461-005-9054-6. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. http://dx.doi.org/10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam FW. Ten-year research update review: Child sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:269–278. doi: 10.1097/00004583-200303000-00006. http://dx.doi.org/10.1097/00004583-200303000-00006. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES–D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Rodriguez MA, Heilemann MV, Fielder E, Ang A, Nevarez F, Mangione CM. Intimate partner violence, depression, and PTSD among pregnant Latina women. Annals of Family Medicine. 2008;6:44–52. doi: 10.1370/afm.743. http://dx.doi.org/10.1370/afm.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A, Bentler P. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. http://dx.doi.org/10.1007/BF02296192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling EA, Aseltine RH, Gore S. The impact of cumulative childhood adversity on young adult mental health: Measures, models, and interpretations. Social Science & Medicine. 2008;66:1140–1151. doi: 10.1016/j.socscimed.2007.11.023. http://dx.doi.org/10.1016/j.socscimed.2007.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. Journal of Traumatic Stress. 2006;19:825–836. doi: 10.1002/jts.20159. http://dx.doi.org/10.1002/jts.20159. [DOI] [PubMed] [Google Scholar]
- Seery MD, Holman EA, Silver RC. Whatever does not kill us: Cumulative lifetime adversity, vulnerability, and resilience. Journal of Personality and Social Psychology. 2010;99:1025–1041. doi: 10.1037/a0021344. http://dx.doi.org/10.1037/a0021344. [DOI] [PubMed] [Google Scholar]
- Smedley BD. The lived experience of race and its health consequences. American Journal of Public Health. 2012;102:933–935. doi: 10.2105/AJPH.2011.300643. http://dx.doi.org/10.2105/AJPH.2011.300643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soeken K, Parker G, McFarlane J, Lominack MC. The abuse assessment screen: A clinical instrument to measure frequency, severity, and perpetrator of abuse against women. In: CCampbell J, editor. Empowering survivors of abuse: Health care for battered women and their children. Thousand Oaks, CA: Sage; 1998. pp. 195–203. [Google Scholar]
- Sue DW, Capodilupo CM, Torino GC, Bucceri JM, Holder AMB, Nadal KL, Esquilin M. Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist. 2007;62:271–286. doi: 10.1037/0003-066X.62.4.271. http://dx.doi.org/10.1037/0003-066X.62.4.271. [DOI] [PubMed] [Google Scholar]
- Sumner LA, Wong L, Schetter CD, Myers HF, Rodriguez M. Predictors of posttraumatic stress disorder symptoms among low-income Latinas during pregnancy and postpartum. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4:196–203. http://dx.doi.org/10.1037/a0023538. [Google Scholar]
- Toussaint L, Shields GS, Dorn G, Slavich GM. Effects of lifetime stress exposure on mental and physical health in young adulthood: How stress degrades and forgiveness protects health. Journal of Health Psychology. 2014 doi: 10.1177/1359105314544132. Advance online publication. http://dx.doi.org/10.1177/1359105314544132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Stress burden and the lifetime incidence of psychiatric disorder in young adults: Racial and ethnic contrasts. Archives of General Psychiatry. 2004;61:481–488. doi: 10.1001/archpsyc.61.5.481. http://dx.doi.org/10.1001/archpsyc.61.5.481. [DOI] [PubMed] [Google Scholar]
- Ullman JB. Structural equation modeling. In: Tabachnick BG, Fidell LS, editors. Using multivariate statistics. 6th ed. Boston, MA: Allyn & Bacon; 2013. pp. 676–780. [Google Scholar]
- Whitfield CL, Anda RF, Dube SR, Felitti VJ. Violent childhood experiences and the risk of intimate partner violence in adults: Assessment in a large health maintenance organization. Journal of Interpersonal Violence. 2003;18:166–185. http://dx.doi.org/10.1177/0886260502238733. [Google Scholar]
- Wickrama KAS, Conger RD, Abraham WT. Early adversity and later health: The intergenerational transmission of adversity through mental disorder and physical illness. Journal of Gerontology. 2005;60(Special Issue 2):S125–S129. doi: 10.1093/geronb/60.special_issue_2.s125. Retrieved from http://psychsocgerontology.oxfordjournals.org/content/60/Special_Issue_2/S125.full. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. http://dx.doi.org/10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt GE, Carmona JV, Loeb TB, Ayala A, Chin D. Sexual abuse. In: Wingood GM, DiClemente RJ, editors. Handbook of women’s sexual and reproductive health: Issues in women’s health. New York, NY: Kluwer Academic/Plenum Press; 2002. pp. 195–216. http://dx.doi.org/10.1007/978-1-4615-0689-8_11. [Google Scholar]
- Wyatt GE, Laurence J, Vodounon A, Mickey MR. The Wyatt sex history questionnaire: A structured interview for female sexual history taking. Journal of Child Sexual Abuse. 1993;1:51–68. http://dx.doi.org/10.1300/J070v01n04_04. [Google Scholar]
- Wyatt GE, Myers HF, Loeb TB. Women, trauma, and HIV: An overview. AIDS and Behavior. 2004;8:401–403. doi: 10.1007/s10461-004-7324-3. http://dx.doi.org/10.1007/s10461-004-7324-3. [DOI] [PubMed] [Google Scholar]
- Yuan K-H, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology. 2000;30:165–200. http://dx.doi.org/10.1111/0081-1750.00078. [Google Scholar]