Abstract
Background
Alkali-burned corneas can seldom heal properly to restore corneal transparency. Treatment of this severe disorder of the ocular surface remains a challenge.
Aim of the Work
was to investigate whether systemically transplanted bone marrow mesenchymal stem cells (BM-MSCs) can promote corneal wound healing after alkali burn.
Material and Methods
Thirty five male New Zealand rabbits were used in this study. The animals were divided into three groups. Group I; the control group was sham operated. Group II; corneal alkali burn was created. Group III; underwent corneal alkali burn then treated with BM-MSCs. All corneas were collected after fourteen and twenty eight days. Evaluation using H&E, PAS & alkaline phosphatase reaction was carried out. Immune histo-chemical staining for CD44 and vimentin was performed as well.
Results
the corneal epithelium of (Group II) showed marked alterations. Vascularization, cellular infiltration and irregularity of the collagen fibers were also seen in the substantia propria. Increase in the thickness of the Descemet’s membrane was noticed as well. On the other hand, at the time of 28 days, Group III rabbits showed best histological results with nearly healed corneas compared to other groups. Meanwhile, vimentin was more strongly expressed in Group III assessing the differentiating ability of BM-MSCs.
Conclusion
BM-MSCs could effectively promote corneal alkali burn healing.
Keywords: Corneal wound healing, Mesenchymal stem cell, Alkaline phosphatase, Vimentin
Introduction
Corneal alkali burn is a common ophthalmologic emergency, often causes extensive damage and results in permanent visual impairment (1). The destruction of limbal stem cells caused by this pathologic condition may account for the complications (2).
Treatment of this severe disorder of the ocular surface remains a challenge. Limbal grafts are still the prevailing option. However, some potential disadvantages or complications including long-term immunosuppressant, potential risk of causing limbal stem cell deficiency in the healthy contralateral eye, still hinders their applications (2–4).
Therefore, the key method to resolving this problem is to look for cells that can be easily collected with sufficient quantity and that have the ability to replace limbal stem cells after transplantation.
Research has shown that bone marrow has multi-potential mesenchymal stem cells (MSCs) that are easily isolated, expanded and directly induced to differentiate into cardiac cells, fat cells, epithelial cells, endothelial cells, nerve cells, bone, cartilage under different conditions in vivo and ex vivo (5).
However, the feasibility of systemically administered BM-MSCs to home and promote corneal wound healing is still under investigations.
So, the purpose of this study was to isolate and culture (BM-MSCs) and to evaluate their role in healing of corneal alkali burn.
Materials and Methods
Thirty five New Zealand white rabbits each weighing between 2 and 2.5 kg were included in present study. The animals were purchased from the Medical Research Center, Ain Shams University. They were housed in plastic cages with mesh wire covers and were given food and water ad libitum. The study was conducted in Histology department, Faculty of Medicine, Ain Shams University. The practical work was performed in accordance to the guide for care and use of laboratory animals and approved by the Animal Ethical Committee of Ain Shams University.
Experimental design
The animals were divided into three groups:
Group I (Control group): consisted of 15 rabbits, to which sham operation was performed.
Group II (Experimental group): included 10 rabbits, the animals were anesthetized by intramuscular injection of 0.5mg/kg ketamine. Corneal alkali burn was then created on the right eye of each rabbit, while the other eye was left without burn so that the animals could eat and move freely. A filter paper was soaked in 1%NaoH and was applied on the whole cornea including the limbus for 25 seconds then was rinsed with 10 ml of distilled water. The animals were subdivided into two subgroups: (Subgroup IIa) sacrificed after 14 days and (Subgroup IIb) sacrificed after 28 days.
Group III (BM-MSCs treated experimental group): included 10 rabbits which were exposed to corneal alkali burn by the same way as Group III. Then after 24 hrs rabbits were anesthetized with intramuscular injection of 0.5 mg/kg of ketamine. After that MSCs suspended in 1ml PBS were administrated intravenously through an ear vein with a 26 gauge syringe. Then, the animals were subdivided into two subgroups: (Subgroup IIIa) sacrificed after 14 days and (Subgroup IIIb) sacrificed after 28 days.
The right corneas were extracted and processed for light microscopic examination. Paraffin sections were stained by using H&E, PAS (for demonstration of Descemet’s membrane & alkaline phosphatase reaction (was used as a marker for MSCs).
Immune histo-chemical study was done using CD44 and vimentin antibodies. They were purchased from (Labvision company, USA).
Morph metric analysis
The mid center region of the cornea in five different non overlapping fields from five different sections of different rabbits were examined in each group (40×). An image analyzer Leica Q win V.3 program (Wetzlar, Germany) in the Histology department, faculty of Medicine Ain Shams University was used to measure:
Mean total thickness of:
Corneal epithelial layer.
Descemet’s membrane layer.
The number of:
Alkaline phosphatase positive cells/high power field
CD 44 positive cells/high power field.
Vimentin positive cells/high power field
Statistical analysis was done using one way ANOVA test performed by SPSS 17 program. The significance of the data was determined by p-value p>0.05 non-significant (NS), p<0.05 significant (S).
Isolation of BM-derived MSCs: Bone marrow was harvested by flushing the tibiae and femurs of rabbits with Dulbecco’s modified Eagle’s medium (DMEM, GIBCO/BRL) supplemented with 10% fetal bovine medium (GIBCO/BRL). Nucleated cells were isolated with a density gradient [Ficoll/Paque (Pharmacia)] and resuspended in complete culture medium supplemented with 1% penicillin-streptomycin (GIBCO/BRL). Cells were incubated at 37°C’ in 5% humidified Co2 for 12~14 days as primary culture or upon formation of large colonies. When large colonies developed (80~90% confluence), cultures were washed twice with phosphate buffer saline (PBS) and cells were trypsinized with 0.25% trypsin in 1 mM EDTA (GIBCO/BRL) for 5 minutes at 37°C. After centrifugation (at 2,400 rpm for 20 minutes), cells were resuspended with serum-supplemented medium and incubated in (50 cm2 culture flask Falcon). The resulting cultures were referred to as first-passage cultures (6).
Morphological identification of BM-derived MSCs: MSCs in culture were characterized by their adhesiveness and fusiform shape (7). characterization using CD29+ and CD45−, CD34−, CD44+ was also performed.
Examination of dishes and taking photographs were done using fluorescence inverted microscope (Axiovert 100-ZEISS, Denmark). Determining cell viability by trypan blue stain and the total cell count using hemocytometer.
Application of mesenchymal stem cells: MSCs 1×107 cells/ml were injected once in an ear vein 24 hours after induction of corneal alkali burn (8).
Results
Morphological identification of the primary culture of rabbit BM-MSCs as evident by the inverted microscope
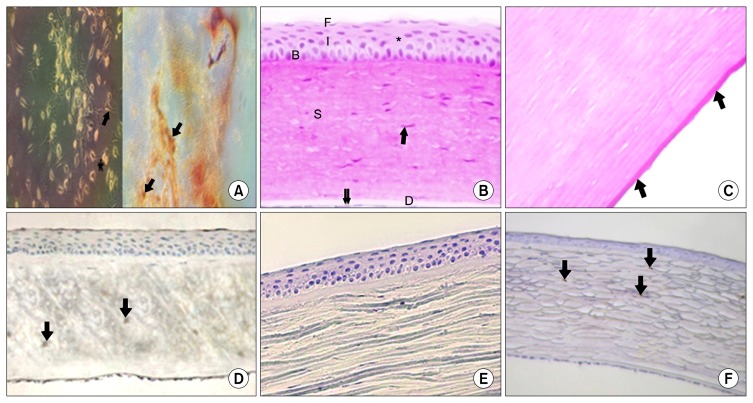
On day five of BM culture, colonies of adherent BM-MSCs appeared in the form of star-shaped cells with long processes, central vesicular nuclei and granular cytoplasm. Characterization using CD44+ was evident (Fig. 1A). Characterization using CD29+ and CD45−, CD34− was also detected as well (data not shown).
Fig. 1.
(A) BM-MSCs, on day five of isolation and culture, showing the appearance of a colony of star-shaped cells with long processes (↑), central vesicular nucleus and granular cytoplasm. Notice, a cell appears in the anaphase stage of division (*). Characterization of MSCs using CD44+ was evident as well. (B) Showing the usual layers of the cornea. The non-keratinized stratified squamous corneal epithelium (*) appears with basal columnar cells (B), intermediate polygonal cells (I) and flat surface cells (F). Thick stroma (S) containing regularly arranged fibers with sparsely distributed keratocytes (↑), homogenous Descemet’s membrane is seen (D). Notice, the simple squamous corneal endothelium (↓↓). (C) Showing PAS positive regular Descemet’s membrane (↑). (D) Showing weak alkaline phosphatase positive reaction in few corneal stromal cells (↓). (E) Showing negative immune-reaction for CD44 in the cytoplasm of epithelial and stromal cells. (F) Showing weak positive immune-reaction for vimentin in few substantia propria cells (↓). A=phase contrast inverted microscopy×200. Control group; B=H&E×250, C=PAS×560, D=Alkaline phosphatase reaction×250, E=Avidin–biotin peroxidase for CD44×250, F=Avidin–biotin peroxidase for vimentin×250.
Histological results
Group I: (Control group): H&E stained sections of control group (Group I) showed the four layers of the cornea. The stratified squamous non-keratinized epithelium appeared resting on a uniform basement membrane. It was formed of a single layer of columnar basal cells, intermediate layers of polygonal cells and superficial squamous cells. No Bowman’s membrane was seen. The substantia propria consisted of regularly arranged collagen fibers with scattered spindle shaped stromal cells (Keratocytes) in between. A homogenous acidophilic Descemet’s membrane appeared beneath the substantia propria. It was covered posterior by simple squamous corneal Descemet’s endothelium (Fig. 1B).
Examination of PAS stained sections showed the Descemet’s membrane with regular strong PAS positive reaction (Fig. 1C).
Alkaline phosphatase stained sections: revealed few weak alkaline phosphatase positive cells in the substantia propria (Fig. 1D).
Immune histo-chemical results
Negative immune-reaction for CD44 was observed in both epithelial and stromal cells (Fig. 1E), while weak positive immune reaction for vimentin was detected in few stromal cells (Fig. 1F).
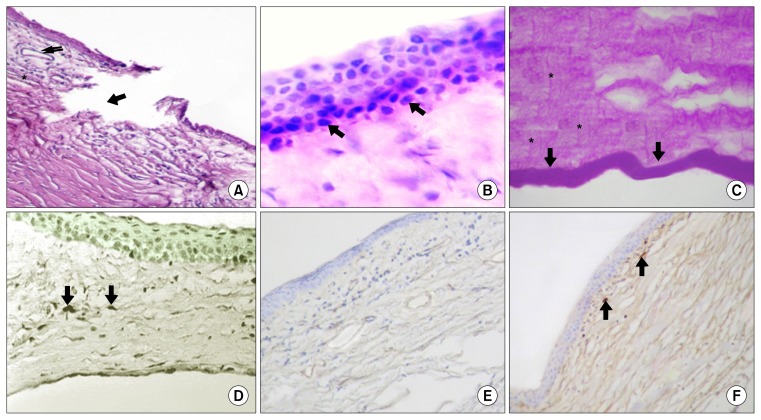
Subgroup IIa (14 days after corneal alkali burn): The cornea of animals of subgroup IIa was markedly affected. Discontinuation and interruption of the corneal epithelium were noticed. The underlying substantia propria showed irregularity of their collagen fibers. Mononuclear cellular infiltration was also observed in between the widely separated and irregularly dispersed collagen fibers. Sub-epithelial invasion of corneal stroma by blood vessels was also noticed (Fig. 2A). The intact corneal epithelium in other parts was disorganized and hyperplasic. Loss of demarcation between the epithelium and the underlying lamina propria was well recognized, together with loss of the superficial squamous cell layer (Fig. 2B).
Fig. 2.
(A) Showing an area of discontinuation of the corneal epithelium and underlying substantia propria (↓). Notice, the formation of granulation tissue with appearance of blood vessels in the stroma (↓↓) together with mononuclear cellular infiltration (*). (B) Showing disorganization and hyperplasia of the corneal epithelial cells. Notice, the loss of demarcation between the epithelium and the underlying substantia propria (↑) together with absence of flat superficial epithelial cells. (C) Showing an apparent increase in the thickness of the wavy, irregular PAS positive Descemet’s membrane (↓). Notice, an increase in PAS positive reaction in some perpendicularly oriented fibrils of corneal stroma (*). (D) Showing few alkaline phosphatase positive stromal cells (↓). (E) Showing negative immune expression for CD44 in both epithelial and stromal cells. (F) Showing positive immue-reaction in few stromal cells in the anterior part of the substantia propria (↑). Subgroup IIa ; A=H&E×250, B=H&E×560, C=PAS×560, D=Alkaline phosphatase reaction×250, E=Avidin–biotin peroxidase for CD44×250, F=Avidin–biotin peroxidase for vimentin×250.
Examination of PAS stained sections showed an apparent increase in PAS positive reaction in some perpendicularly oriented fibrils of corneal stroma. An apparent increase in the thickness of the wavy Descemet’s membrane was noticed as well (Fig. 2C).
Alkaline phosphatase stained section showed positive alkaline phosphatase activity in few stromal cells (Fig. 2D).
Immune histo-chemical results
Immune histo-chemical reaction for detection of BM-MSCs using CD44 showed negative immune expression for CD44 in epithelial and stromal cells (Fig. 2E) Few stromal cells in the anterior part of the substantia propria showed weak positive reaction for vimentin. Whereas, the cells of the posterior part were totally devoid of any vimentin reaction (Fig. 2F).
Subgroup IIb (28 days group after corneal alkali burn): Examination of H&E stained sections revealed persistence of most of the previously observed histological results. Discontinuation and interruption of the corneal epithelium and the underlying substantia propria were still noticed. An apparent increase in the thickness of the corneal epithelium was seen. The layers of the epithelium were disorganized, the cells were overcrowded. Some epithelial cells appeared with clear cytoplasm and deeply stained nuclei. Sloughing of the superficial epithelial cells was also detected. The collagen fibers in the substantia propria were still widely separated and showed irregular arrangement. They were separated by clear spaces. Mononuclear cellular infiltration in addition to some eosinophils which appeared with acidophilic cytoplasm and bilobed nuclei were seen between the collagen fibers (Fig. 3A). An apparent increase in the thickness of the irregular Descemet’s membrane was also noticed. The membrane as well as the substantia propria were heavily infiltrated by many fibroblasts. They appeared as branched cells with many cell processes and basophilic cytoplasm (Fig. 3B).
Fig. 3.
(A) Showing discontinuation of the corneal epithelium (↓). Notice, the substantia propria with heavy mononuclear cellular infiltration (↓↓). The inset shows an apparent increase in thickness of corneal epithelium. The cells are overcrowded, some of the epithelial cells appear with clear cytoplasm and deeply stained nuclei (*). Sloughing of the superficial flat cells is obvious. Notice, the eosinophil with their acidophilic cytoplasm and bilobed nucleus in the underlying stroma (↑). (B) Showing the collagen fibers of substantia propria widely separated and irregularly oriented. An apparent increase in the thickness of Descemet’s membrane (D). Both substantia propria and Descemet’s membrane are heavily infiltrated by fibroblast (↓↓). the inset shows, Descemet’s membrane infiltration by branched basophilic fibroblast (→). (C) Showing an apparent thickening of PAS positive Descemet’s membrane as compared to control group (→). (D) Showing moderate alkaline phosphatase activity in some stromal cells (↓). (E) Showing negative immune expression for CD44 in both epithelial and stromal cells. (F) Showing few positive vimentin stromal cells in anterior part of substantia propria (↓). Subgroup IIb ; A=H&E×250 and inset×560, B=H&E×250 and inset×560, C=PAS×560, D=Alkaline phosphatase reaction ×250, E=Avidin–biotin peroxidase for CD44×250, F=Avidin–biotin peroxidase for vimentin×250.
In PAS stained sections, an apparent increase in the Descemet’s membrane was obvious (Fig. 3C).
Examination of Alkaline phosphatase stained sections showed an apparent increase in the number of positive stromal cells (Fig. 3D).
Immune histo-chemical results
Immune histo-chemical stain for detection of BM-MSCs using CD44 showed negative immune expression for CD44 in both epithelial and stromal cells (Fig. 3E). Whereas immune-histo-chemical stain for detection of BM-MSCs differentiation using vimentin showed few positive stromal cells in anterior part of substantia propria (Fig. 3F).
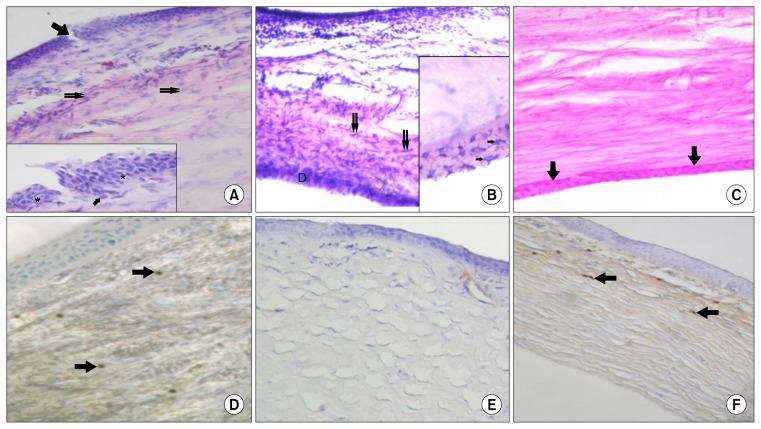
Subgroup IIIa (14 days after corneal alkali burn and MSCs injection): Examination of H&E stained sections revealed that the surface epithelium appeared to be covered by superficial flat cells. Clear epithelial cells with deeply stained nuclei were still recognized. The collagen fibers in the substantia propria were nearly regular in arrangement, however, some spaces were still present (Fig. 4A).
Fig. 4.
(A) Showing. some epithelial cells with clear cytoplasm and deeply stained nuclei (↑). (B) Showing, regular arrangement of Descemet’s membrane together with an apparent decrease in its thickness compared to subgroup IIIa (↑). (C) Showing, dense alkaline phosphatase positive cells in stroma (↓). Notice, the increase in the density of their reaction. (D) Showing, positive expression of CD44 in some basal epithelial cells (↑) as well as in stromal cells (↑↑). (E) Showing, positive expression of vimentin in most of stromal cells (↓). Subgroup IIIa ; A=H&E×560, B=PAS×560, C=Alkaline phosphatase reaction ×250, D=Avidin–biotin peroxidase for CD44×560, E=Avidin–biotin peroxidase for vimentin×250.
PAS stained sections, showed regular arrangement of PAS positive Descemet’s membrane and apparent decrease in its thickness compared to subgroup IIIa (Fig. 4B).
Alkaline phosphatase stained sections showed an apparent increase in the number of positive cells, together with moderate reaction intensity in most of stromal cells compared to subgroup IIIa (Fig. 4C).
Immune histo-chemical results
Immune-histochemical stain for detection of BM-MSCs using CD44 showed positive cells in the basal epithelial cells as well as the stromal cells (Fig. 4D).
Positive vimentin expression in many stromal cells was also evident (Fig. 4E).
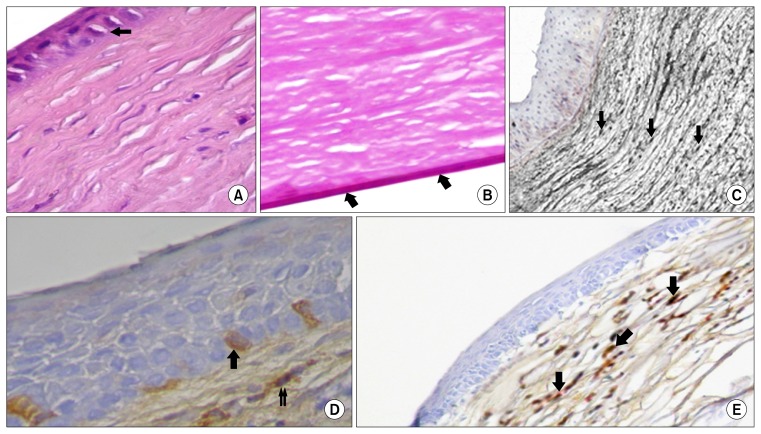
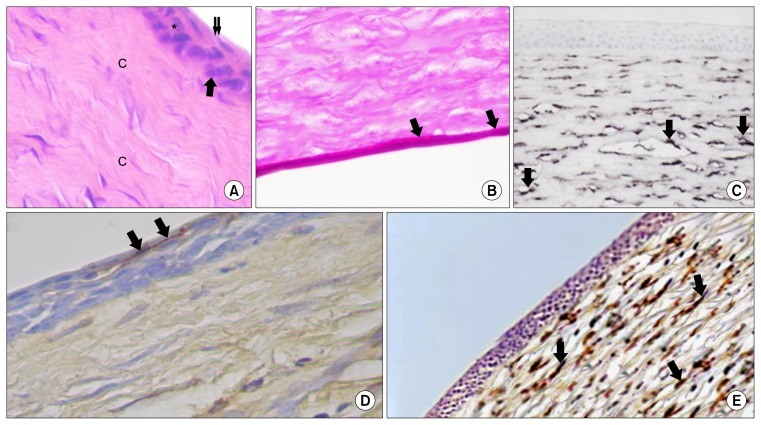
Subgroup IIIb (28 days after corneal alkali burn and MSCs injection): H&E stained sections showed that the cornea of rabbits of this subgroup appeared nearly as comparable to control ones. The layers of the cornea could be easily identified. The corneal epithelium appeared continuous. It was formed of basal cell layer, polygonal intermediate cells and superficial flat squamous cells. The substantia propria appeared to be formed of regularly arranged collagen fibers (Fig. 5A).
Fig. 5.
(A) Showing the epithelial cells is formed of basal layer (↑), intermediate polygonal cells (*) and superficial flat cells (↓↓). Notice, regular arrangement of the collagen fibers in the stroma (c). (B) Showing the thickness of the Descemet’s membrane (↓) nearly similar to control group. (C) Showing an apparent increase in the number of alkaline phosphatase positive cells in the substantia propria (↓). (D) Showing brown cytoplasmic positive reaction of CD44 in some superficial epithelial cells (↓). (E) Showing an apparent increase in the number of vimentin positive cells in stroma. Notice the strong intensity of their reaction (↓). Subgroup IIIb ; A=H&E×560, B=PAS×560, C=Alkaline phosphatase reaction×250, D=Avidin–biotin peroxidase for CD44×560, E=Avidin–biotin peroxidase for vimentin×250.
PAS reaction revealed the thickness of Descemet’s membrane nearly as comparable to control ones (Fig. 5B).
Alkaline phosphatase staining showed an apparent increase in number of alkaline phosphatase positive cells in substantia propria which showed intense reaction for the enzyme (Fig. 5C).
Immune histo-chemical results
Immune histo-chemical stained sections for detection of BM-MSCs using CD44 revealed positive CD44 cells in the superficial layer of the epithelium (Fig. 5D).
Immune-histo-chemical stained sections for detection of BM-MSCs differentiation using vimentin showed an apparent increase in the number of positive stromal cells. There was an apparent increase in the intensity of the reaction as well (Fig. 5E, Table 1).
Table 1.
Showing the difference between mean±SEM of thickness of corneal epithelial layer and Descemet’s membrane layer and the number of CD 44+cells, vimentin+cells and alkaline phosphatase+cells/high power field
| Group I | Subgroup IIa | Subgroup IIb | Subgroup IIIa | Subgroup IIIb | F value | p-value | |
|---|---|---|---|---|---|---|---|
| Total epithelial thickness | 47.5±3.6 (■♣) | 77.6±9.4 (▲●♣*) | 67.4±6.3 (*■▲●) | 7 54.8±7. (■♣) | 49.4±6.4 (■♣) | 155.13 | p=0.00 |
| Thickness of desemet’s membrane | 6.2±3.5 (■♣) | 17.4±9.6 (●▲*) | 14.9±5.7 *■♣▲●)) | 9.9±2.8 (■♣●) | 7.6±2.1 (■♣▲) | 240.55 | p=0.000 |
| Number of alkaline phospatase+ve cell/hpf | 4.90±0.525 (■♣▲●) | 14.90±0.60 (*♣▲●) | 19.50±.94 (*■▲●) | 30.70±0.94 (*■♣●) | 45.10±0.48 (*■♣▲) | 25.34 | p=0.001 |
| Number of CD44+ve cells/hpf | 0.00±0.00 (▲●) | 0.00±0.00 (●▲) | 0.00±0.00 (●▲) | 9.40±.50 (*■♣●) | 17.40±1.2 (*■♣▲) | 70.63 | p=0.001 |
| Number of vimentin+cell/hpf | 3.10±0.37 (■♣▲●) | 4.90±0.31 (*♣▲●) | 7.10±0.67 (*■▲●) | 21.50±0.65 (*■♣●) | 32.30±.74 (*■♣▲) | 38.53 | p=0.001 |
Significant difference from group I.
Significant difference from subgroup IIa.
Significant difference from subgroup IIb.
Significant difference from subgroup IIIa.
Significant difference from subgroup IIIb.
The mean total thickness of corneal epithelium and Descemet’s membrane
A significant increase in mean thickness of corneal epithelium and Descemet’s membrane in animals of subgroups IIa & b was detected as compared to that of control animals. On the other hand, there was also a significant reduction in the epithelial thickness and Descemet’s membrane thickness of subgroups IIIa & IIIb as compared to subgroup IIa &b respectively.
As regard the mean number of alkaline phosphatase+cells, CD44 cells and vimentin positive cells:
There was a significant increase in number of positive cells concerning the three parameters in subgroups IIIa & b compared to control group and subgroup IIa & b respectively.
Discussion
The current study was designed to isolate and culture BM-MSCs from adult male New Zealand rabbits and to evaluate their benefit in corneal alkali burn healing.
In the present work, an apparent increase in the thickness of the PAS positive Descemet’s membrane of the cornea of rabbits of subgroups IIa & b was observed compared to control group. This finding was confirmed by statistical results. These findings coincided with those of a previous workers, reporting an increase in thickness, abnormality and altered structure of Descemet’s membrane in alkali burned corneas. They attributed these alterations to the change in pH of the corneal endothelium resulting in decreased barrier effectiveness together with a decrease in the pump function (9).
Additionally, it was formerly described that the Descemet’s membrane was disfigured by the presence of an abnormal region of extracellular matrix, termed a posterior collagenous layer, which is laid down by the diseased endothelial cells (10).
The Descemet’s membrane as well as the substantia propria of cornea of animals of subgroup IIb were heavily infiltrated by branched basophilic cells with many cell processes, most probably they are fibroblastic cells. Similarly, it was stated that the corneal endothelial cells were transformed into fibroblasts which might be responsible for the fibrosis encountered after corneal injury (11). Moreover, myofibroblastic metaplasia of attenuated corneal endothelial cells with formation of an abnormal posterior collagenous layer might contribute to an impaired visual function (12).
On the other hand, Descement’s membrane of corneas of subgroup III a &b showed non significant increase in thickness as compared to control group. It was formerly suggested to be due to restoration of corneal keratocytes and endothelial cells by MSCs (13).
Moreover, the present work demonstrated moderate improvement 14 days after corneal alkali burn with MSCs transplantation. Few changes were still obvious; some of the epithelial cells appeared with clear cytoplasm and deeply stained nuclei. The substantia propria was formed of nearly regular collagen fibers. More improvement of these lesions was recorded in subgroup III b (28 days after corneal burn and MSCs transplantation) where their corneas appeared nearly similar to control group. These finding were in agreement with former workers (14, 15). Moreover, the release of stem cell specific chemoattractants as stromal cell-derived factor-1 and substance P from injured tissues might be implicated in mobilization of MSCs from peripheral blood and their homing to the injured cornea (16, 17).
Some authors explained the different mechanisms by which the MSCs restore the corneal lesions after alkali burn. They attributed their role to the secretion of some growth factors and cytokines, which regulate cellular processes such as chemotaxis, cell proliferation, cell signaling, extracellular matrix formation and angiogenesis in the wound (18, 19). Moreover, it was reported that, MSCs have immune modulatory effects, and can produce numerous trophic and growth factors and can also differentiate to the corneal epithelial and endothelial cells (20).
In the present work, weak positive alkaline phosphatase reaction was observed in few cells in the substantia propria of control rabbits. It was suggested that these cells were undifferentiated cells which were positive for the enzyme. It was recorded that, the substantia propria of the cornea contains keratocytes and quiescent mesenchymal cells of neural crest, a small population of them displays properties of mesanchymal stem cells (21). Moreover, significant increase in the number of alkaline phosphatase positive cells was detected between subgroups IIIa & b and subgroup IIa &b respectively. Alkaline phosphatase reaction was therefore used as a marker to detect mesenchymal stem cells (22).
Immunohistochemical stained sections of animals of control group as well as animals of subgroups IIa and IIb of the present work showed negative CD44 immune-reaction in cytoplasm of both epithelial and stromal cells. These findings were in accordance with that of a previous workers, who reported that CD44 positive cells were absent in human corneal epithelium (23).
Strong CD44 immune expression was detected in sections of animals of subgroups IIIa & b (14 and 28 days after MSCs injection) of current study in some basal and superficial epithelial cells as well as in some stromal cell. It was suggested that the MSCs differentiated into epithelial cells and keratocytes to restore the histological structure of the cornea. As mesenchymal stem cells were found to be easily isolated and to have the potential to differentiate into epithelial cells (24). Moreover, it was also confirmed by immune staining with anti-keratocan antibody that BM-MSCs could differentiate into a keratocyte phenotype (25).
Vimentin is type III intermediate filaments expressed in mesenchymal cells such as fibroblasts, endothelial cells and adipocytes. Although, it is a cytoplasmic marker (26), vimentin expression in our sections was found to be nuclear. This was explained that, vimentin forms arrays of cytoplasmic filaments which encapsulate the nucleus, form a perinuclear ring and extend to the cell periphery. It was also reported that vimentin is one of the anchored filaments to the apical junctions, responsible for nuclear centration and cell-to-cell contacts (27).
In the current work, positive vimentin stromal cells expression was detected in subgroups IIa &b in anterior part of cornea beneath basement membrane while, the posterior part of cornea was totally devoid of vimentin. This coincided with a previous report suggesting that, after corneal injury there might be a phenotypic difference in vimentin expression between anterior stromal and posterior stromal keratocytes (28).
Moreover, it was stated that vimentin was expressed in myofibroblasts in alkali-injured stroma. They added that the keratocytes that migrated to injured stroma became transformed into myofibroblasts which expressed high levels of vimentin (29, 30).
In the current study, sections of animals of subgroups IIIa & b (14 and 28 days after MSCs injection) showed a significant increase in vimentin expression in their corneal stroma compared to that of control group and subgroups IIIa & b. These findings were in agreement with a former work, reporting high levels of vimentin in the corneal stroma on day 14 and at one month after MSCs transplantation confirming the differentiating ability of MSCs (12).
From the previously discussed results, it was obvious that the injured corneas of rabbits treated with MSCs showed a good progress to restore their histological picture, compared to animals which were left to recover without MSCs injection.
Footnotes
Potential conflict of interest
The authors have no conflicting financial interest.
References
- 1.Kao WW, Zhu G, Benza R, Kao CW, Ishizaki M, Wander AH. Appearance of immune cells and expression of MHC II DQ molecule by fibroblasts in alkali-burned corneas. Cornea. 1996;15:397–408. doi: 10.1097/00003226-199607000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Tsai RJ, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med. 2000;343:86–93. doi: 10.1056/NEJM200007133430202. [DOI] [PubMed] [Google Scholar]
- 3.Tseng SC. Regulation and clinical implications of corneal epithelial stem cells. Mol Biol Rep. 1996;23:47–58. doi: 10.1007/BF00357072. [DOI] [PubMed] [Google Scholar]
- 4.Swift GJ, Aggarwal RK, Davis GJ, Coster DJ, Williams KA. Survival of rabbit limbal stem cell allografts. Transplantation. 1996;62:568–574. doi: 10.1097/00007890-199609150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 6.Alhadlaq A, Mao JJ. Mesenchymal stem cells: isolation and therapeutics. Stem Cells Dev. 2004;13:436–448. doi: 10.1089/scd.2004.13.436. [DOI] [PubMed] [Google Scholar]
- 7.Campagnoli C, Roberts IA, Kumar S, Bennett PR, Bellantuono I, Fisk NM. Identification of mesenchymal stem/progenitor cells in human first-trimester fetal blood, liver, and bone marrow. Blood. 2001;98:2396–2402. doi: 10.1182/blood.V98.8.2396. [DOI] [PubMed] [Google Scholar]
- 8.Ye J, Yao K, Kim JC. Mesenchymal stem cell transplantation in a rabbit corneal alkali burn model: engraftment and involvement in wound healing. Eye (Lond) 2006;20:482–490. doi: 10.1038/sj.eye.6701913. [DOI] [PubMed] [Google Scholar]
- 9.Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol. 1997;41:275–313. doi: 10.1016/S0039-6257(96)00007-0. [DOI] [PubMed] [Google Scholar]
- 10.Levy SG, McCartney AC, Sawada H, Dopping-Hepenstal PJ, Alexander RA, Moss J. Descemet’s membrane in the iridocorneal-endothelial syndrome: morphology and composition. Exp Eye Res. 1995;61:323–333. doi: 10.1016/S0014-4835(05)80127-7. [DOI] [PubMed] [Google Scholar]
- 11.Leung EW, Rife L, Smith RE, Kay EP. Extracellular matrix components in retrocorneal fibrous membrane in comparison to corneal endothelium and Descemet’s membrane. Mol Vis. 2000;6:15–23. [PubMed] [Google Scholar]
- 12.Heindl LM, Schlötzer-Schrehardt U, Cursiefen C, Bachmann BO, Hofmann-Rummelt C, Kruse FE. Myofibroblast metaplasia after descemet membrane endothelial keratoplasty. Am J Ophthalmol. 2011;151:1019–1023.e2. doi: 10.1016/j.ajo.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 13.Coulson-Thomas VJ, Caterson B, Kao WW. Transplantation of human umbilical mesenchymal stem cells cures the corneal defects of mucopolysaccharidosis VII mice. Stem Cells. 2013;31:2116–2226. doi: 10.1002/stem.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yao L, Li ZR, Su WR, Li YP, Lin ML, Zhang WX, Liu Y, Wan Q, Liang D. Role of mesenchymal stem cells on cornea wound healing induced by acute alkali burn. PLoS One. 2012;7:e30842. doi: 10.1371/journal.pone.0030842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ma Y, Xu Y, Xiao Z, Yang W, Zhang C, Song E, Du Y, Li L. Reconstruction of chemically burned rat corneal surface by bone marrow-derived human mesenchymal stem cells. Stem Cells. 2006;24:315–321. doi: 10.1634/stemcells.2005-0046. [DOI] [PubMed] [Google Scholar]
- 16.Hannoush EJ, Sifri ZC, Elhassan IO, Mohr AM, Alzate WD, Offin M, Livingston DH. Impact of enhanced mobilization of bone marrow derived cells to site of injury. J Trauma. 2011;71:283–289. doi: 10.1097/TA.0b013e318222f380. discussion 289–291. [DOI] [PubMed] [Google Scholar]
- 17.Smith H, Whittall C, Weksler B, Middleton J. Chemokines stimulate bidirectional migration of human mesenchymal stem cells across bone marrow endothelial cells. Stem Cells Dev. 2012;21:476–486. doi: 10.1089/scd.2011.0025. [DOI] [PubMed] [Google Scholar]
- 18.Joo YO. The Anti-Inflammatory protein TSG-6 reduces inflammatory damage to the cornea following chemical injury. Am J Ophthalmo. 2012;107:459–467. doi: 10.1073/pnas.1012451107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang W, Ge W, Li C, You S, Liao L, Han Q, Deng W, Zhao RC. Effects of mesenchymal stem cells on differentiation, maturation, and function of human monocyte-derived dendritic cells. Stem Cells Dev. 2004;13:263–271. doi: 10.1089/154732804323099190. [DOI] [PubMed] [Google Scholar]
- 20.Holan V, Javorkova E. Mesenchymal stem cells, nanofiber scaffolds and ocular surface reconstruction. Stem Cell Rev. 2013;9:609–619. doi: 10.1007/s12015-013-9449-0. [DOI] [PubMed] [Google Scholar]
- 21.Pinnamaneni N, Funderburgh JL. Concise review: Stem cells in the corneal stroma. Stem Cells. 2012;30:1059–1063. doi: 10.1002/stem.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Osathanon T, Nowwarote N, Manokawinchoke J, Pavasant P. bFGF and JAGGED1 regulate alkaline phosphatase expression and mineralization in dental tissue-derived mesenchymal stem cells. J Cell Biochem. 2013;114:2551–2561. doi: 10.1002/jcb.24602. [DOI] [PubMed] [Google Scholar]
- 23.Alho AM, Underhill CB. The hyaluronate receptor is preferentially expressed on proliferating epithelial cells. J Cell Biol. 1989;108:1557–1565. doi: 10.1083/jcb.108.4.1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen J, Li Y, Wang L, Zhang Z, Lu D, Lu M, Chopp M. Therapeutic benefit of intravenous administration of bone marrow stromal cells after cerebral ischemia in rats. Stroke. 2001;32:1005–1011. doi: 10.1161/01.STR.32.4.1005. [DOI] [PubMed] [Google Scholar]
- 25.Liu H, Zhang J, Liu CY, Hayashi Y, Kao WW. Bone marrow mesenchymal stem cells can differentiate and assume corneal keratocyte phenotype. J Cell Mol Med. 2012;16:1114–1124. doi: 10.1111/j.1582-4934.2011.01418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paulin-Levasseur M. Intermediate filament proteins: many unanswered questions, few unquestioned answers. Biochem Cell Biol. 1992;70:842–848. doi: 10.1139/o92-132. [DOI] [PubMed] [Google Scholar]
- 27.Risen LA, Binder PS, Nayak SK. Intermediate filaments and their organization in human corneal endothelium. Invest Ophthalmol Vis Sci. 1987;28:1933–1938. [PubMed] [Google Scholar]
- 28.Chaurasia SS, Kaur H, de Medeiros FW, Smith SD, Wilson SE. Dynamics of the expression of intermediate filaments vimentin and desmin during myofibroblast differentiation after corneal injury. Exp Eye Res. 2009;89:133–139. doi: 10.1016/j.exer.2009.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ishizaki M, Zhu G, Haseba T, Shafer SS, Kao WW. Expression of collagen I, smooth muscle alpha-actin, and vimentin during the healing of alkali-burned and lacerated corneas. Invest Ophthalmol Vis Sci. 1993;34:3320–3328. [PubMed] [Google Scholar]
- 30.Wilson SE. Analysis of the keratocyte apoptosis, keratocyte proliferation, and myofibroblast transformation responses after photorefractive keratectomy and laser in situ kerato-mileusis. Trans Am Ophthalmol Soc. 2002;100:411–433. [PMC free article] [PubMed] [Google Scholar]