Blood conservation strategies effectively decrease red blood cell (RBC) use in specific patient groups.1-3 However, the impact of RBC transfusion reduction on mortality in a diverse inpatient population remains poorly described. We detail the impact of declining RBC use on 30-day mortality within Kaiser Permanente Northern California (KPNC), an integrated health care delivery system serving 3.5 million members at 21 hospitals.
Methods
The KPNC and University of California, San Francisco (UCSF) institutional review boards approved this study and waived the requirement for informed consent based on the nature of the study. Beginning in 2010, KPNC initiated a regional blood conservation program whose key features included (1) clinician education in evidence-based transfusion guidelines; (2) focused multidisciplinary conservation efforts in specific high-use departments (eg, orthopedics, cardiovascular surgery); and (3) guideline-based clinical decision support embedded within the electronic medical record.
To study the impact of these initiatives, we quantified RBC transfusion in an inpatient cohort composed of all non-obstetric patients 18 years or older admitted to KPNC hospitals between July 1, 2009, and August 31, 2013. We evaluated the impact of decreased RBC use on unadjusted and risk-adjusted 30-day mortality prior to (2010) and following (2012-2013) reductions in blood use. We examined these rates in patients with hemoglobin levels below 10 g/dL (to convert to grams per liter, multiply by 10) during hospitalization (n = 218 056), accounting for nearly all (81 897 of 83 461 [98.1%]) transfused patients. We quantified patients’ predicted 30-day mortality rates based on prior methods adjusting for age, sex, comorbid disease burden, emergency or elective presentation, medical or surgical admission, admission diagnosis, severity of illness, first inpatient ward, and hospital facility.4 We also adjusted for patients’ pread-mission hemoglobin level and lowest hospital hemoglobin level.5 We then compared standardized mortality ratios for transfused vs nontransfused patients using Poisson regression. Trends in RBC use and unadjusted 30-day mortality were assessed using linear regression. Statistical analyses were performed in Stata 11 software (StataCorp).
Results
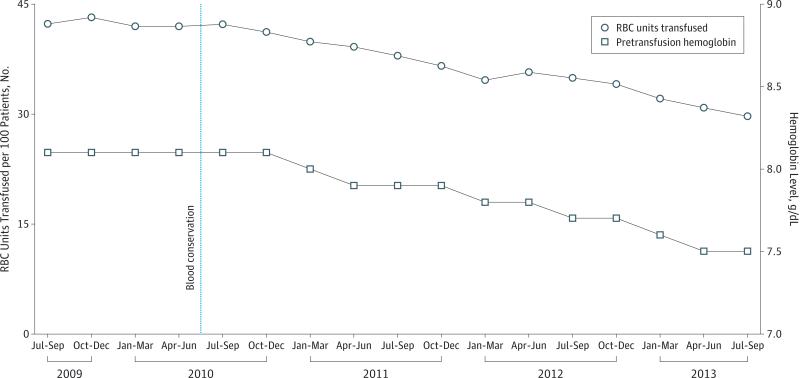
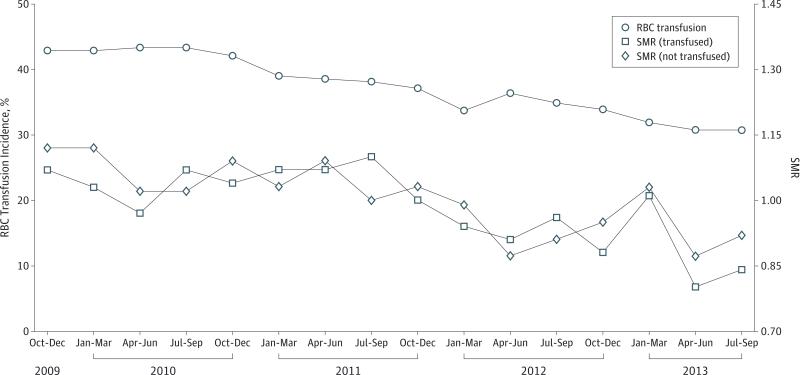
The number of RBC units transfused decreased 8.6% annually from 41.8 units per 100 patients in 2010 (95% CI, 41.1-42.6 units) to 31.0 units per 100 patients in 2013 (95% CI, 30.3-31.8 units) (P < .001) (Figure 1). From 2009 to 2013, the median pretransfusion hemoglobin decreased from 8.1 g/dL to 7.5 g/dL (P < .001). In patients with a hemoglobin level lower than 10 g/dL, RBC transfusion incidence decreased from 43.4% in 2010 to 30.7% in 2013 (P < .001) (Figure 2).
Figure 1. Trends in Inpatient RBC Use and Pretransfusion Hemoglobin Levels Across 21 KPNC Facilities.
The number of RBC units transfused per 100 patients and median pretransfusion hemoglobin level decreased following initiation of blood conservation strategies in 2010 (P < .001). To convert hemoglobin to grams per liter, multiply by 10. KPNC indicates Kaiser Permanente Northern California; and RBC, red blood cells.
Figure 2. Inpatient RBC Transfusion Incidence and SMRs.
The decline in RBC transfusion incidence in patients whose hemoglobin level fell below 10 g/dL (n = 218 056) was not associated with differences in SMRs in transfused and nontransfused patients. To convert hemoglobin to grams per liter, multiply by 10. RBC indicates red blood cells; and SMRs, standardized mortality ratios.
In inpatients with a hemoglobin level lower than 10 g/dL, 30-day mortality rates did not differ prior to (2010) and following (2013) declines in RBC use (7.8% and 7.8%, respectively; P = .49 for trend). Standardized mortality ratios in transfused and nontransfused anemic patients did not differ prior to (rate ratio in 2010, 0.96; 95% CI, 0.91-1.03) (P = .26) and following (rate ratio in equal period [2012-2013], 0.96; 95% CI, 0.90-1.02) (P = .20) reductions in RBC use (Figure 2).
Discussion
Our study demonstrates the impact of blood conservation strategies on transfusion practice and mortality outside the clinical trial setting. We found a greater than 20% reduction in RBC use over 3 years and a concurrent drop in median pretransfusion hemoglobin level. Over the same period, we did not detect an impact of decreased RBC use and more restrictive transfusion practice on adjusted and unadjusted mortality rates.
Observational studies using large health care databases can complement findings from randomized clinical trials by confirming and expanding on outcomes in clinical practice. In this case, we examined the broad application of clinical trial-based recommendations that could conceivably negatively affect a diverse population.6 Our study demonstrates, in a real-world setting, that reductions in transfusion incidence are occurring without affecting mortality. Future studies will need to assess whether further reductions in RBC use and hemoglobin thresholds have an impact on morbidity and mortal ity. These data support the safety of more restrictive transfusion practice as currently implemented in a large community hospital network.
Acknowledgments
Funding/Support: The authors were supported by research contracts from the National Heart, Lung, and Blood Institute (NHLBI) contracts HHSN2682011000005I and HHSN268201100004I for the Recipient Epidemiology and Donor Evaluation Study-III (REDS-III).
Role of the Sponsors: The NHLBI had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Roubinian had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Roubinian, Escobar, Liu, Murphy.
Acquisition, analysis, or interpretation of data: Roubinian, Escobar, Liu, Gardner, Carson, Kleinman.
Drafting of the manuscript: Roubinian, Liu, Carson.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Roubinian.
Obtained funding: Escobar, Murphy.
Administrative, technical, or material support: Liu, Gardner, Murphy.
Study supervision: Kleinman, Murphy.
Additional Contributions: We acknowledge Chaya Prasad, MD, Richard Ray, MD, Jason Lee, MD, and the other members of the Kaiser Permanente Northern California (KPNC) Blood Bank for facilitating access to blood bank data used in the study. We thank Cynthia Vasallo, BSN, and Linda Gliner, BSN (KPNC Department of Quality and Operation Support), for performing data quality audits and Bix Swain, MS, and John Greene, MS (KPNC Division of Research), for assistance with electronic medical record programming. Contributors did not receive financial compensation.
Conflict of Interest Disclosures: None reported.
Group Information: The NHLBI Recipient Epidemiology Donor Evaluation Study–III (REDS-III), domestic component, is the responsibility of the following persons: Hubs: A. E. Mast and J. L. Gottschall, BloodCenter of Wisconsin, Milwaukee; D. J. Triulzi and J. E. Kiss, The Institute For Transfusion Medicine, Pittsburgh, Pennsylvania; E. L. Murphy and E. W. Fiebig, University of California, San Francisco; E. L. Snyder, Yale University School of Medicine, New Haven, Connecticut; R. G. Cable, American Red Cross Blood Services, Farmington, Connecticut; Data Coordinating Center: D. J. Brambilla and M. T. Sullivan, RTI International, Rockville, Maryland; Central Laboratory: M. P. Busch and P. J. Norris, Blood Systems Research Institute, San Francisco, California; Publication Committee Chairman: R. Y. Dodd, American Red Cross, Holland Laboratory, Rockville; Steering Committee Chairman: S. H. Kleinman, University of British Columbia, Victoria, British Columbia, Canada; and National Heart, Lung, and Blood Institute, National Institutes of Health: S. A. Glynn and A. M. Cristman, Bethesda, Maryland.
References
- 1.Cohn CS, Welbig J, Bowman R, Kammann S, Frey K, Zantek N. A data-driven approach to patient blood management. Transfusion. 2014;54(2):316–322. doi: 10.1111/trf.12276. [DOI] [PubMed] [Google Scholar]
- 2.Freedman J. The ONTraC Ontario program in blood conservation. Transfus Apher Sci. 2014;50(1):32–36. doi: 10.1016/j.transci.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 3.Paone G, Brewer R, Likosky DS, et al. Membership of the Michigan Society of Thoracic and Cardiovascular Surgeons. Transfusion rate as a quality metric: is blood conservation a learnable skill? Ann Thorac Surg. 2013;96(4):1279–1286. doi: 10.1016/j.athoracsur.2013.05.045. [DOI] [PubMed] [Google Scholar]
- 4.Escobar GJ, Gardner MN, Greene JD, Draper D, Kipnis P. Risk-adjusting hospital mortality using a comprehensive electronic record in an integrated health care delivery system. Med Care. 2013;51(5):446–453. doi: 10.1097/MLR.0b013e3182881c8e. [DOI] [PubMed] [Google Scholar]
- 5.Roubinian NME, Swain BE, Gardner MN, Liu V, Escobar GJ. Predicting Red Blood Cell Transfusion in Hospitalized Patients: Role of Hemoglobin Level, Comorbidities, and Illness Severity. BMC Health Serv Res. 2014;14:213. doi: 10.1186/1472-6963-14-213. doi:10.1186/1472-6963-14-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carson JL, Grossman BJ, Kleinman S, et al. Clinical Transfusion Medicine Committee of the AABB. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2012;157(1):49–58. doi: 10.7326/0003-4819-157-1-201206190-00429. [DOI] [PubMed] [Google Scholar]