Abstract
Objective: Formation of a foreign body granuloma is one of the serious complications of silicone injection, which can be difficult to treat. In this paper, the authors report their successful experience with dermabrasion as an innovative treatment in a patient who presented with diffuse silicone granuloma. Case report: The patient was a 51-year-old woman, with areas of induration and hyperpigmentation on both her legs with intermittent fevers and generalized malaise. The patient had a history of numerous bilateral hip injections of liquid silicone five years ago for cosmetic purposes. A skin biopsy showed a foreign-body granuloma consistent with a paraffinoma with “Swiss cheese” appearance. After unsuccessful medical therapy and liposuction, an extensive bilateral dermabrasion was performed on both legs. Postoperatively, her wounds exuded a collection of thick, yellow viscous fluid under the transparent semi-occlusive dressings, which showed a markedly elevated level of silicone after analysis. She experienced no complication related to dermabrasion. Conclusion: The findings of this case demonstrate that dermabrasion may be an effective treatment option for diffuse silicone granuloma, particularly when the material resides superficially in the dermis.
Although the United States Food and Drug Administration (FDA) has never approved liquid silicone for general cosmetic injection purposes, silicone is widely used dermal filler substance to correct contour irregularities. As with other injectable dermal fillers, patients may experience edema, erythema, or ecchymosis at the injection site. Pain, skin induration, migration of material, and local vascular obstruction may also occur.1
The formation of a foreign body granuloma is one of the serious complications of silicone injection, which can be painful and disfiguring. Clinically, it can present as cellulitis with nodule formation, ulceration, skin induration, and local lymph duct and lymph node enlargement.2 Although the incidence of granuloma formation in patients injected with medical-grade silicone is relatively low, some reports suggest that complications can occur in up to 20 percent of patients exposed.3
In this paper, the authors report their successful experience with dermabrasion as an innovative treatment in a patient who presented with diffuse silicone granuloma.
CASE REPORT
A 51-year-old Latin American woman presented to the authors’ dermatology inpatient service complaining from areas of induration and hyperpigmentation on both her legs. The patient also complained of intermittent fevers and generalized malaise. A thorough history revealed that the patient had received numerous bilateral hip injections of liquid silicone five years ago for cosmetic purposes.
Her physical exam showed multiple well-defined, hyperpigmented, indurated, and focally infiltrated plaques over both her legs, particularly her lower legs due to migrated silicone material. The plaques exhibited multiple areas of oozing and vesicle granuloma, and there was an oily fluid discharge upon superficial puncturing. In addition, the patient’s ability to ambulate was compromised due to the associated pain and she had pitting edema over both ankles.
Vascular studies showed significant arterial and venous insufficiency in her lower extremities bilaterally. This insufficiency was secondary to external compression with vascular obstruction. X-ray of her foot showed no obvious cortical destruction or any clinical evidence of disruption to indicate the presence of active osteomyelitis. A skin biopsy showed a foreign-body granuloma consistent with a paraffinoma. Numerous ovoid or round cavities where the paraffin resided prior to processing were also seen in the biopsy, giving the “Swiss cheese” appearance.
The patient was admitted to the authors’ service, where she was initially treated with pulse steroids (methylprednisolone 1g IV) for five days. She also received a five-day course of cyclosporine (125mg bid); however, these treatments were ineffective and discontinued due to the possible side effects.
After initial medical management yielded minimal results, it was determined that operative intervention should be performed. On Day 5 of the patient’s hospitalization, she underwent liposuction of her right leg to directly remove the foreign substances. During this procedure, a local dermabrasion was also attempted on a 10cm2 area of her left leg, which resulted in a constant pooling of cloudy, oily fluid after occlusion with transparent semi-occlusive dressings (Tegaderm, 3M) postoperatively. Although the patient experienced some improvements on the site of dermabrasion, liposuction was not as successful, probably due to the deep localization of the silicone material within the fibrotic dermis. The patient was discharged with a two-week prescription of oral antibiotics. Considering the promising effects of initial dermabrasion therapy, the patient was scheduled for a more comprehensive dermabrasion of both legs.
Two months later, she underwent extensive bilateral dermabrasion of both lower extremities (Figure 1). The surgery was uncomplicated, and postoperatively her wounds exuded a collection of thick, yellow, viscous fluid under the transparent semi-occlusive dressings (Figure 2). The fluid collected from the dermabrasion procedure was sent to the National Medical Services Laboratory in Willow Grove, Pennsylvania, where the analysis of the fluid revealed a markedly elevated level of silicone. During her eight-day hospital stay, she was treated with intravenous steroids, which were tapered and then discharged on a graded dose of oral prednisone. Pain control was an issue and required oxycodone with breakthrough administration of intramuscular meperidine in addition to gabapentin and amitriptyline. Prior to discharge, the patient was ambulating well, her pain was well controlled, and her wounds showed healthy granulation tissue with areas of reepithelialization (Figure 3).
Figure 1.

Extensive dermabrasion of the patient’s lower extremities
Figure 2.
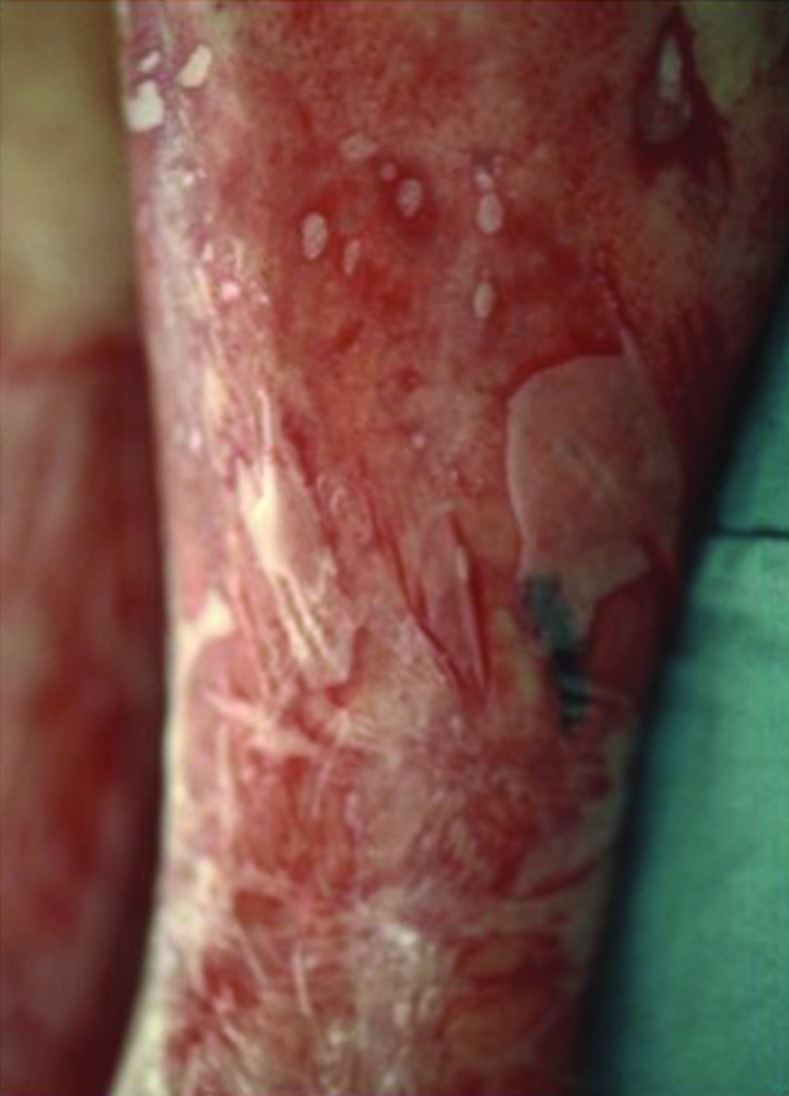
Exudation of silicone-laden fluid under transparent semi-occlusive dressing after extensive, bilateral dermabrasion
Figure 3.

Healthy granulation tissue formation with areas of re-epithelialization after dermabrasion
DISCUSSION
Silicone granuloma is a severe granulomatous tissue reaction following injection or implantation of silicone.2 The time between injection and onset of cutaneous symptoms can vary from a few weeks to 20 years after administration.3 In the authors’ patient, the symptoms started five years after the silicone injection. Silicone granuloma in this patient presented as multiple, well-defined, hyperpigmented, indurated, and focally infiltrated plaques over both legs; however, she did not have any lymph node involvement.
Although the pathogenesis of granuloma formation is still unknown, it is believed that some form as a result of poorly digestible antigen (foreign body granuloma) while others result from a T-cell mediated immune reaction to an antigen (immune granuloma). Other possible causes of silicone granuloma formation include immunologic cross-reaction to a viral agent, acting of material as a nidus for infection, impurity of the material, and cross contamination via injection technique.4
Most treatments of silicone granuloma target the inflammatory process or suspected underlying infection. Therefore, treatment modalities have included long-term broad spectrum antibiotics, oral and intralesional steroids, and the use of oral, IV, or topical immunomodulating agents.4 Unfortunately, as happened to our patient, dramatic improvements are rarely seen and duration of treatment might take months, leading to a high risk of potentially serious side effects. When medical management fails, surgical intervention is an option. However, as described in this case, surgical excision or liposuction can be challenging because of the tendency of silicone to migrate to adjacent tissues. In turn, a wider surgical excision may be necessary, increasing patient morbidity without guaranteed success.
In this case, the patient’s diffuse silicone granuloma was treated with complete bilateral dermabrasion of the lower extremities after observing the extraction of material following a local dermabrasion. After occlusion of the dermabrasion wounds with transparent semi-occlusive dressings, there was a constant release of silicone-laden fluid. The patient’s symptoms improved dramatically and the wounds exhibited healthy granulation tissue within days. In addition, postoperative vascular studies showed a regression of her venous and arterial impingement. Clinically, the patient regained normal ambulation and the edema in her ankles improved. These findings demonstrate that dermabrasion may be an effective treatment option for diffuse silicone granuloma, particularly when the material resides superficially in the dermis.
Footnotes
DISCLOSURE:The authors declare no conflicts of interest.
REFERENCES
- 1.Ellenbogen R, Rubin L. Injectable fluid silicone therapy. Human morbidity and mortality. JAMA. 1975;234:308–309. [PubMed] [Google Scholar]
- 2.Arin MJ, Bäte J, Krieg T, Hunzelmann N. Silicone granuloma of the face treated with minocycline. J Am Acad Dermatol. 2005;52(2 Suppl 1):53–56. doi: 10.1016/j.jaad.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 3.Rapaport MJ, Vinnik C, Zarem H. Injectable silicone: cause of facial nodules, cellulitis, ulceration, and migration. Aesthetic Plast Surg. 1996;20:267–276. doi: 10.1007/s002669900032. [DOI] [PubMed] [Google Scholar]
- 4.Baumann LS, Halem ML. Lip silicone granulomatous foreign body reaction treated with aldara (imiquimod 5%) Dermatol Surg. 2003;29:429–432. doi: 10.1046/j.1524-4725.2003.29102.x. [DOI] [PubMed] [Google Scholar]


