Abstract
Purpose
The majority of circulating human γδT lymphocytes are of the Vγ9Vδ2 lineage, and have TCR specificity for non-peptide phosphoantigens. Previous attempts to stimulate and expand these cells have therefore focussed on stimulation using ligands of the Vγ9Vδ2 receptor, whilst relatively little is known about variant blood γδT subsets and their potential role in cancer immunotherapy.
Experimental Design
To expand the full repertoire of γδT without bias towards specific T cell receptors, we made use of artificial antigen presenting cells loaded with an anti gamma delta T cell receptor antibody that promoted unbiased expansion of the γδT repertoire. Expanded cells from adult blood donors were sorted into 3 populations expressing respectively Vδ2 TCR chains (Vδ2+), Vδ1 chains (Vδ1+) and TCR of other delta chain subtypes (Vδ1negVδ2neg)
Results
Both freshly isolated and expanded cells showed heterogeneity of differentiation markers, with a less differentiated phenotype in the Vδ1 and Vδ1negVδ2neg populations. Expanded cells were largely of an effector memory phenotype although there were higher numbers of less differentiated cells in the Vδ1+ and Vδ1negVδ2neg populations. Using neuroblastoma tumor cells and the anti-GD2 therapeutic monoclonal antibody ch14.18 as a model system, all three populations showed clinically relevant cytotoxicity. Whilst killing by expanded Vδ2 cells was predominantly antibody dependent and proportionate to upregulated CD16, Vδ1 cells killed by antibody independent mechanisms.
Conclusions
In conclusion we have demonstrated that polyclonal expanded populations of γδT cells are capable of both antibody dependent and independent effector functions in neuroblastoma.
Keywords: gamma delta T cells, neuroblastoma
Introduction
Gamma delta T (γδT) lymphocytes have both cytotoxic and professional antigen presenting capacity (1-4) but have been relatively overlooked in terms of their potential role as mediators of antibody dependent cell mediated cytotoxicity (ADCC), particularly in the context of monoclonal antibody treatments of cancer. γδT have properties that make them highly effective mediators of ADCC. This stems from their capacity to be specifically activated and expanded by potent but non-toxic small molecule ligands of the gamma-delta T cell receptor (γδ-TCR) Vγ9Vδ2. The natural ligands of Vγ9Vδ2 are phosphoantigen by-products of the non-mevalonate pathway of cholesterol biosynthesis produced in bacteria and some cancer cells. In vitro, isoprenyl pyrophosphate (IPP) is the most commonly used, but BrHPP and zoledronic acid also possess powerful Vγ9Vδ2 agonist activity. Zoledronic acid is a drug with a proven safety record, currently used to treat osteoporosis and also beneficial in patients with multiple myeloma (5). The cytotoxicity of phosphoantigen stimulated Vγ9Vδ2 T cells against haematological malignancies increases significantly in the presence of antibodies targeting tumor associated surface antigens such as CD20 (1,2,6,7), but less is known about their cytotoxicity against solid tumours.
Whilst research has focussed on the Vγ9Vδ2 cells because of their expansion with phosphoantigens, these comprise only one subset of the total γδT cell repertoire. Much less is known about other subsets, which employ Vγ1-8 and Vδ1-9. Interestingly, whilst Vδ2+ cells predominate in the circulation of healthy Caucasians (8), individuals from West Africa have predominantly Vδ1+ γδT cells (9). This phenomenon may be linked to increased endemic levels of pathogens such as malaria, HIV and mycobacteria. Cytomegalovirus (CMV) infection is also known to be a stimulus of Vδ1+ γδT cell expansion (10). The ligands of the Vδ1 TCR are less well understood than those of the Vδ2 TCR, but are thought to include MHC associated proteins MICA (11) and MICB, CMV associated UL16 binding proteins ULPB1-4 and lipid antigens presented on CD1(12, 13). Vδ1+ γδT cells predominate in intestinal tissues, and studies of tumour infiltrating Vδ1+ γδT cells suggests a protective role against epithelial malignancies (14) whilst CMV-activated Vδ1+ γδT cells are protective against HT29 colonic carcinoma growth in a xenograft model (15). Very little is known about the potential role of Vδ1negVδ2neg γδT cells in cancer protection.
Neuroblastoma is a cancer arising from the nerγous system that primarily affects children. 50% of cases fall into a high-risk category with 5-year survival of around 40% despite intensive and highly toxic therapy. Current immunotherapy strategies target GD2, a ganglioside expressed abundantly on all neuroblastomas. Immunotherapy using a combination of anti-GD2 monoclonal antibody and immunostimulation with IL-2 and GM-CSF is of significant clinical benefit in neuroblastoma (16). Although neuroblastoma is one of the few solid tumours in which antibody-based immunotherapy has been successful, the precise cellular mechanisms contributing to clinical response are poorly defined. Given the clear increase in Vδ2+ cytotoxicity when used in combination with tumor specific antibodies in haematological cancers, and the sensitivity of neuroblastoma cells to NK-like killing (17), we hypothesised that neuroblastoma cells would be highly sensitive to γδT mediated killing by antibody dependent and independent mechanisms. Here, we show that polyclonal γδT cells can be expanded to large numbers from the blood of healthy donors and neuroblastoma patients. These cells show cytotoxicity against neuroblastoma cell lines but Vδ2+ cytotoxicity depends on antibody opsonisation of target cells, whereas Vδ2neg cytotoxicity is predominantly antibody independent.
Materials and methods
Cell lines
K562 Artificial antigen presenting cells engineered to express CD86, CD137L and IL-15 (clone 4) were provided by Laurence Cooper as described in the companion paper. Human neuroblastoma cells lines Kelly, SKNAS, SKNDZ, IMR32 and LAN1 were originally obtained from the ATCC.
Isolation of γδT cells from PBMC
Cells were obtained from neuroblastoma patients at the point of diagnosis or from healthy donors (via NHS national blood service). PBMC were isolated using Ficoll density gradient separation. γδT cells were isolated using 2 rounds of positive selection for the γδTCR with the Anti-TCRγ/δ MicroBead Kit (130-050-701, Miltenyi) according to the manufacturer’s protocol. If depletion of CD14+ and CD11c+ cells was performed, PBMC were first stained with mouse anti-human CD14-PE (BioLegend 301806; clone M5E2), mouse anti-human CD14-PE (Biolegend 301806; clone M5E2) before a PE depletion step using Anti-PE MicroBeads (130-048-801), in accordance with the manufacturer’s protocol. The CD14−/CD11c− fraction was then subjected to 2 rounds of positive selection for the γδTCR as described above.
Expansion of γδT cells from PBMC
γδT cells were expanded from freshly isolated PBMCs or from isolated pure populations of γδT cells. Cells were obtained from healthy donors (via NHS national blood service) or from neuroblastoma patients before exposure to cytotoxic chemotherapy. Phosphoantigen-based expansions were carried out as previously described (1). Expansion using anti human-γδTCR antibodies (Leaf-purified B1 - Biolegend 331204, purified anti-TCR Vγ9 clone B3 – Biolegend 331301, anti-TCR pan-γδ clone Immu510 – Beckman Coulter COIM1349, anti-Pan TCRγδ clone 5A6.E91 – Pierce antibodies TCR1061) or control antibody (purified mouse IgG1 isotype control antibody, clone MG1-45 – Biolegend 401402) was achieved by immobilising the antibody on the surface of plastic tissue culture wells overnight before adding PBMC in medium (RPMI, 10% FCS, 1% PS) containing 100u/ml IL-2. aAPC-only expansions used 2:1 aAPC:γδT cells, with aAPC added every 7 days. The aAPC were irradiated before use (80Gy). The medium (RPMI1640, 10% FCS, 1% PS) was supplemented with 100u/ml IL-2 (PeproTech 200-02) and 60ng/ul IL-21. For expansion of γδT cells with aAPC coated in B1 the same ratios and technique was used, but the aAPC were coated in B1 anti-γδTCR antibody before adding them to the γδT cells. Cells were incubated at 37°C, 5% CO2. Fold changes of γδT cells were derived by calculating the percentage of live cells in each γδT cell subset at a given time using flow cytometry and relating this to the number of trypan blue negative cells in the culture system.
Expansion of αβT cells using CD3/CD28 Dynabeads
PBMC from healthy donors were co-cultured with Dynabeads® Human T-cell activator CD3/28 (Life Technologies 111.31D) in accordance with the manufacturer’s protocol. The beads were added at day 0 and every 7 days thereafter. The cells were maintained in medium (RPMI1640, 10% FCS, 1% PS) supplemented with 100u/ml IL-2.
Flow cytometry
Flow cytometry analysis was carried out on BD LSRII or BD FACSAria flow cytometers and results were analysed using BD FACSDiva Software (Version 6.1.3, build 2009 05 13 13 29). The following antibodies were used in this investigation: Mouse anti-human CD11c-PE (Biolegend 301606; clone 3.9), mouse anti-human CD14-PE (BioLegend 301806; clone M5E2), mouse anti-human CD14-APC (Biolegend 301806; clone M5E2), mouse anti-human CD3-PE/Cy7 (Biolegend 3000316; clone HIT3a), mouse anti human CD45RA-PECy7 (BioLegend 304126; clone HI100), mouse anti human CD27-Violet 421 (BioLegend 302824; clone O323), mouse anti-human TCR Vδ1-FITC (Thermo Scientific TCR2730; clone TS8.2), mouse anti-human TCR Vδ2-PE (BioLegend 331408; clone B6), mouse anti-human CD45RA-APC (BioLegend 304114 clone HI100), mouse anti-human CD62L-APCCy7 (BioLegend 304814 clone DREG-56), mouse anti-Granzyme B-FITC (BioLegend 515403, clone GB11, mouse-anti human IFNγ-APCCy7 (BioLegend 502530 clone 4S.B3) mouse anti-human NKp30-APC (BioLegend 325210 clone P30-15), mouse anti-human FAS-L-PE (BioLegend 306407 clone NOK-1), mouse anti-human NKG2D-APC (BioLegend 320808 clone 1D11). Compensation was carried out using single-colour controls and eBioScience OneComp eBeads (eBioScience 01-1111). Where intracellular cytokine staining was performed, cells were prepared using BioLegend fixation and permeabilization buffers in accordance with the manufacturer’s protocol.
Fluorescence microscopy
Cells that were examined by fluorescence microscopy had already been stained with anti-CD11c-PE, anti-CD14-PE and anti-Hapten-FITC-(anti-γδTCR-Hapten) and fixed using Fixation Buffer. 20 μl of cell suspension at concentration 2×106 cells per ml was applied to each slide and the cover slip applied directly before sealing with glue. The slides were stored in the dark at 4°C overnight to allow the glue to dry before viewing.
Slides were viewed on a Zeiss Axioplan 2 microscope using a Plan-Apochromat 63x/1.40 oil objective. Images were captured at room temperature (20°C) using a Quantix digital camera (Photometrics, USA) and SmartCapture VP software. For immunofluorescence experiments, images were saved as TIFF files and viewed using Adobe Photoshop CS5. Brightfield images were collected using a Zeiss Axiovert 200 M microscope with a Plan-Apochromat 63x/1.40 oil objective. The microscope stage was maintained at 37°C with 5% CO2. Images were captured using a Zeiss axiocam and Axiovision 4.0 software.
Cytotoxicity assays
Expanded γδT cells were used as effector cells. Target cells were coated either with opsonizing antibody or a non-targeting isotype control and labeled with 100 μCi Na 512CrO4 in cell culture and tested in a standard chromium release assay as previously described. A range of E:T ratios was used in each case (10:1, 5:1, 2.5:1, 1.25:1) and cells were incubated for 4 hours for each assay. Human IgG1 anti-GD2 antibody ch14.18 (clinical grade) was used as a GD2 opsonizing antibody, with human IgG1 rituximab anti-CD20 antibody (clinical grade) as a control.
Cytokine production assays
The BD cytokine bead array was used in accordance with the manufacturer’s protocol to analyze production of IFN-γ, Granzyme B and TNFα by γδT cells co-cultured with neuroblastoma cells. Briefly, 0.25×106 γδT cells were co-cultured with 0.25×106 target cells opsonized with ch14.18 anti-GD2 or control antibody (rituximab). The cells were co-cultured for 24 hours and the supernatant analyzed for cytokine content.
High-Throughput Sequencing of Gamma Delta T-Cells Using Targeted Capture
RNA was isolated from PBMC, Vd1+, Vd2+ and double negative cell populations using TRIzol (Invitrogen). 1μg RNA from each sample was used to prepare and multiplex libraries for 500 cycle paired-end sequencing on the MiSeq using Ultra Library Prep Kit for Illumina and Multiplex Oligos for Illumina (NEBNext E7530 and E7335 respectively). A custom bait library of Agilent’s SureSelect targeted capture system, based on complementary V and J gene segment sequences, as downloaded from the IMGT database was used to enrich for T-cell receptor gamma and delta chain sequences (18). Post-capture libraries were amplified from the Illumina P5 and P7 adapter sequences and sequenced on a MiSeq genetic analyser (Illumina). Quality and quantity of libraries were assessed throughout using Agilent’s Bioanalyzer. FASTQ files were downloaded from BaseSpace following MiSeq runs. Fastx Toolkit was used to discard reads with a quality score of less than Q30 and paired reads were aligned using Fast Length Adjustment of Short Reads (19). Identification and analysis of T-cell receptor gamma and delta chain content was carried out using the Decombinator (20).
Statistical analysis
Statistical analyses were performed using GraphPad Prism Version 6.0c. Error bars, where displayed, indicate the standard error of the mean of data from replicate experiments. Significance of difference between samples within figures was confirmed using paired or unpaired t-tests, depending on the experimental setting, with p = <0.05 indicating significance.
Results
Isolation of pure populations of γδT cells from thawed PBMC aliquots
Whilst isolation of γδT cells to a high degree of purity from fresh blood can be achieved with either one or two rounds of antibody conjugated bead positive selection, this is not possible from frozen aliquots of PBMCs due to non-specific uptake of magnetic FITC labelled beads. The major contaminating cells express CD14 and/or CD11c and fall within the monocyte forward and side scatter gate on flow cytometric profiles (supplemental figure 1A). Fluorescent microscopy of isolates from thawed samples demonstrate FITC conjugated anti-γδTCR beads co-staining with CD14/11c (supplementary figure 1B). These contaminants were eliminated by adding a CD14/11c depletion step prior to 2 rounds of positive selection for the γδTCR (supplementary figure 1C and 1D). Subsequent experiments therefore employed this initial depletion step prior to γδT cell expansions from frozen PBMC, allowing for repeated experiments on aliquots from the same blood sample.
Expansion of polyclonal γδT cells from PBMC and from purified populations
The Vγ9Vδ2 subset of human γδT cells in peripheral blood can be preferentially expanded using phosphoantigens or aminobisphosphonates. There is a relative paucity of knowledge about other γδT cell subsets, which employ Vδ chains 1-8 and Vγ chains 1-9. Expansion of Vδ2neg γδT cells using immobilised anti-γδTCR antibody has been previously demonstrated (21) but the authors used only one antibody clone. We compared the ability of 5 commercially available monoclonal antibodies to expand Vδ1 and Vδ2 γδT cells from healthy donor PBMC with a view to identify antibodies that led to a balanced expansion of both subsets. The differences were not statistically significant in terms of mean fold change for each antibody. Anti-γδTCR Clone B1 (BioLegend) provided the greatest fold-change overall, taking into account Vδ1 and Vδ2 expansion (Figure 1A).
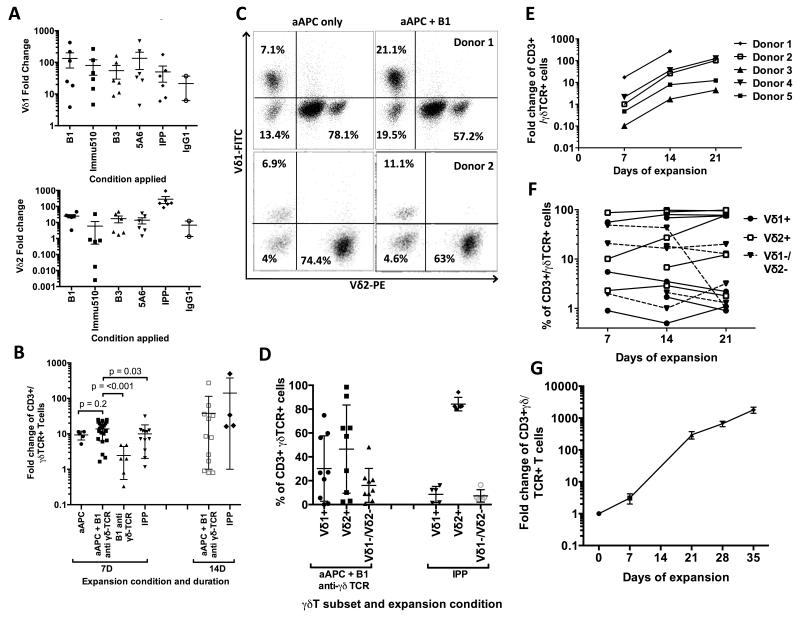
Figure 1. Expansion of diverse populations γδT cells from healthy donors and neuroblastoma patients.
Expansion of γδT cells from PBMC using immobilized anti-γδTCR antibody (A) and from pure preparations of γδT cells using aAPC, B1-coated aAPC, immobilised B1 or IPP (B). γδT subsets as revealed by flow cytometry after expansion are shown in (C) (representative of >6 donors), (D) and (F). γδT cells isolated from thawed healthy-donor PBMC varied in their expansion potential (E), whereas γδT cells isolated from fresh blood of neuroblastoma patients, taken at point of diagnosis, were more consistent (G). Error bars represent SEM and each data point represents an individual donor.
To effect more potent expansion of γδT cells in culture we made use of artificial antigen presenting cells (aAPC) that had been generated through engineering of the K562 erythroblastic leukaemia cell line to express co-stimulatory molecules (CD86, 41BB-L), membrane-bound IL-15 and the high affinity Fc receptor FcγRI (CD64) (22). Coating aAPC in murine anti-human stimulatory antibodies such as OKT3 anti-CD3 via CD32 is an effective means of expanding T cells (22). We demonstrated that B1-anti-γδTCR murine IgG1 mAb bound the aAPC (supplementary Figure 2). We compared the ability to expand γδT cells from adult blood of 1) irradiated aAPC coated with B1 mAb in the presence of added IL-2 and IL-21, 2) uncoated aAPC, or 3) IPP. After 7 days stimulation the combination of aAPC+B1 anti-γδTCR was significantly superior to IPP in terms of γδT cell fold change (Figure 1B). The addition of B1 anti-γδTCR to the aAPC did not at initial analysis lead to a significant improvement in γδT cell expansion (comparison of fold change by t-test yielded p=0.2), but if non-responders were eliminated (defined as fold change <3 within 7 days) the combination of aAPC+B1 was significantly better than aAPC alone (p=0.03). Our aim was to produce a balanced expansion of γδT cell subsets without the pressure towards Vδ2+ expansion associated with using phosphoantigens or aminobisphosphonates. Whilst non-antibody treated aAPC led to expansion of all γδT cell subsets, greater percentages of the rarer Vδ1+ and Vδ1negVδ2neg γδT subsets were obtained by combining aAPC with B1 anti-γδTCR (Figure 1C shows 2 representative donors) and there was a marked difference from the pattern seen following IPP expansion (Figure 1D). Whilst the expansion potential of γδT cells overall varied between donors (Figure 1E) the combination of aAPC+B1 anti-γδTCR generally maintained the relative proportions of each γδT cell subset during expansions from each donor over 3-weeks, allowing study of the entire γδT cell repertoire (Figure 1F). As is shown in Figure 1F, there was a high degree of variation in γδT cell repertoire between different donors; supplementary figure 3 shows representative data from three individuals before any expansion stimulus was applied..
γδT cell expansion from the blood of cancer patients has been reported to be problematic. In one study, γδT cells from 88% (14/16) healthy donors were expanded in vitro in response to IL-2 + pamidronate, whereas γδT cells from only 49% (20/41) cancer patients were successfully expanded following the same stimuli (23). We investigated the expansion potential of γδT cells from 10ml blood samples from newly diagnosed children with neuroblastoma. Over a 28-day expansion period using aAPC+B1, we achieved over 650-fold expansion of γδT cell numbers (mean fold change 665, 95% CI 410-920, n=4) (Figure 1G)
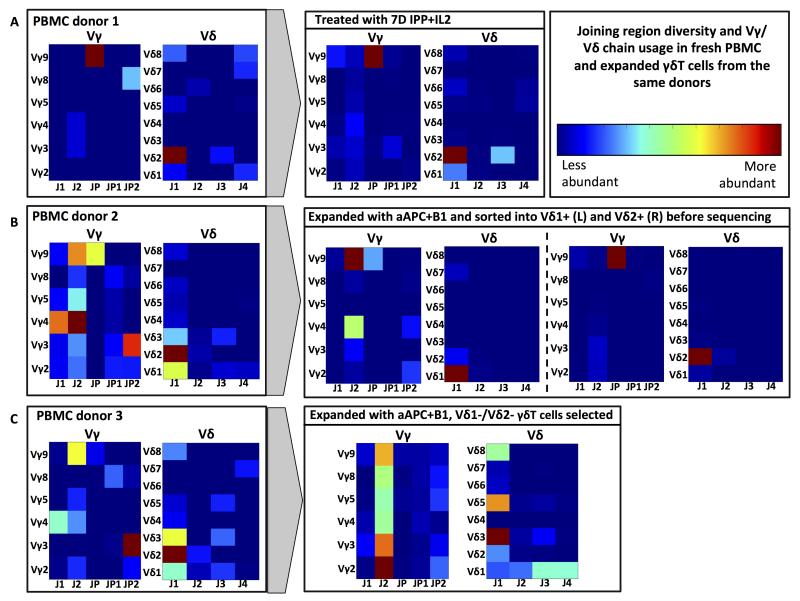
To obtain quantitative data on the repertoire of TCR gene usage in the expanded γδT cell subsets we flow-sorted the Vδ1+, Vδ2+ and Vδ1negVδ2neg populations from normal donors and performed next generation sequencing of T-cell receptor sequences. We compared these to γδT cells expanded using IPP, and also to the γδT cell repertoires found in unstimulated PBMCs from the same donors. The level of diversity in Vγ and Vδ chain usage of healthy donors was reduced following 7 days of stimulation with IPP, LCL and IL-2 (Figure 2A). Using this technique it is possible to determine the abundance of clones bearing distinct TCRγ or TCRδ chain rearrangements. We have shown the commonest hypervariable sequences of PBMC and expanded TCRδ chains in supplementary table 2. When γδT cells were expanded using aAPC+B1, and sorted into Vδ1+ and Vδ2+ populations we discovered high levels of gamma chain diversity within the Vδ1+ population, encompassing Vγ2+, Vγ3+ and Vγ9+ chain usage. There is even greater diversity within the Vδ1+ populations when the joining regions of the gamma chain are considered. Interestingly, the diversity of the Vδ2+ subset expanded from the same donor in the same way is much less than that of the Vδ1+ subset – almost all of the Vδ2+ cells were Vγ9Vγ2, using γJP and δJ1 (Figure 2B). Whilst there appears to have been some loss of diversity in the expansion of γδT cells from PBMC donor 2, this may be explained as the missing Vγ and Vδ populations fell in the Vδ1negVδ2neg population which is not shown. By characterising the γδT cell repertoire within the Vδ1negVδ2neg subset, we found that it contains γδT cells bearing the full range of Vγ chains (Vγ2-5, Vγ8-9) and a range of Vδ chains including Vδ3, Vδ5 and Vδ8. There was greater joining segment diversity in the Vδ chains than in the Vγ chains in this subset (Figure 2C). Whilst it is impossible to exclude the presence of some bias in the expansion technique using aAPC+B1, it is clearly less biased than expansion with IPP + LCL.
Figure 2. Joining region diversity and Vγ/Vδ chain usage in fresh PBMC and expanded γδT cells from the same donors.
Heat maps demonstrating variable and joining gene segment usage, as revealed by next generation RNA sequencing, in gamma and delta chain T-cell receptors in PBMC populations of healthy donors, before and after expansion using IPP or aAPC+B1. Relative frequency of V and J pairings is shown in blue (low abundance), through to red (high abundance). PBMC donor 1 (A) demonstrates a dominance of Vγ9Vδ2, which is reinforced following a 7-day expansion with IPP and IL2. PBMC donor 2 (B) demonstrates more diversity prior to expansion using aAPC and B1 and there is greater gamma chain diversity in the Vδ1+ subset than in the Vδ2+ subset. In the Vδ1negVδ2neg population sorted from donor 3 (C) there is marked diversity in both delta and gamma chain joining segment and V segment usage in both PBMC and expanded cells.
γδT cell subsets have different differentiation phenotypes
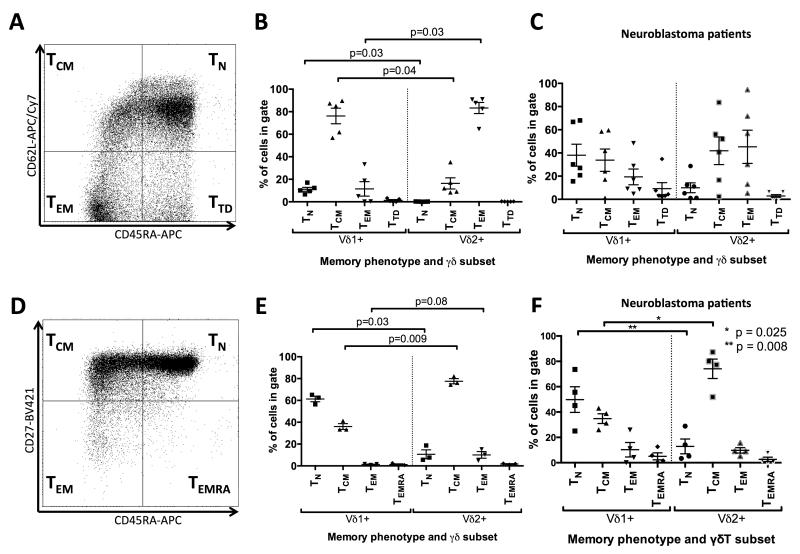
Whilst αβ memory phenotype has been studied in great detail, corresponding data on γδT cells is more limited and their memory phenotype is less well defined. Three memory phenotypes of γδT cells have been previously described, based on CD27 and CD45RA staining (CD45RA+/CD27+ naïve, CD45RA−/CD27+ central memory, CD45RA−/CD27− effector memory CD45RA+) (24). L-selectin (CD62L) can also be used as a memory marker. Similar to αβT cells, as Vδ2+ γδT cells become more differentiated from central memory (TCM) to effector memory (TEM) they down-regulate expression of L-selectin (CD62L) and CD27. Vδ1 memory phenotypes have been reported to show a similar pattern following antigen exposure, as demonstrated by the comparison of CMV+ and CMVneg individuals (25).
Figure 3A shows the distribution of differentiation phenotypes from a representative neuroblastoma patient, using CD62L and CD45RA as markers. Comparison of the CD62L/CD45RA phenotype between Vδ1+ and Vδ2+ T cells staining of PBMC taken from healthy donors and neuroblastoma patients (at point of diagnosis) yielded some consistent patterns but the variation between neuroblastoma patients was higher than that seen in healthy donors (Figure 3B & C), Vδ1+ γδT cells are less differentiated than Vδ2+ γδT cells, as reflected by lower numbers of CD45RA−/CD62L− (TEM) cells and higher numbers of CD62L+/CD45RA− (TCM) and CD62L+/CD45RA+ (TN). This was confirmed using CD27/CD45RA staining of PBMC – an example of which is shown in Figure 3D. Using this staining panel, the percentage of naïve (CD27+/CD45RA+) cells is significantly higher in the Vδ1+ population than in Vδ2+ cells, whereas the Vδ2+ subset contains significantly more central memory (CD27+/CD45RA−) cells (Figure 3E & F). Interestingly, γδT cells isolated from fresh blood of healthy donors (mean age 24, figure 3E) appeared to be less differentiated than those obtained from cryopreserved leucocyte cones provided by the National Blood Service (Figure 3B, adult donor ages unspecified). This may be related to donor age, but could also indicate an effect of cryopreservation on memory marker expression. The general trend of Vδ1+ γδT cells being significantly less differentiated remains in either sample type.
Figure 3. Memory phenotypes of un-stimulated γδT cells from healthy donors or neuroblastoma patients at the point of diagnosis.
The representative FACS plots (A, D) show the total T-cell population from a neuroblastoma patient. Memory phenotype of Vδ1 and Vδ2 γδT cells from healthy donors (B) and neuroblastoma patients (C) (n=6) using CD45RA and CD62L staining. Memory phenotype of Vδ1 and Vδ2 γδT cells using CD27 and CD45RA from a different set of healthy donors (E) and some of the same neuroblastoma patients (F) (n=4) is also shown. Error bars represent SEM.
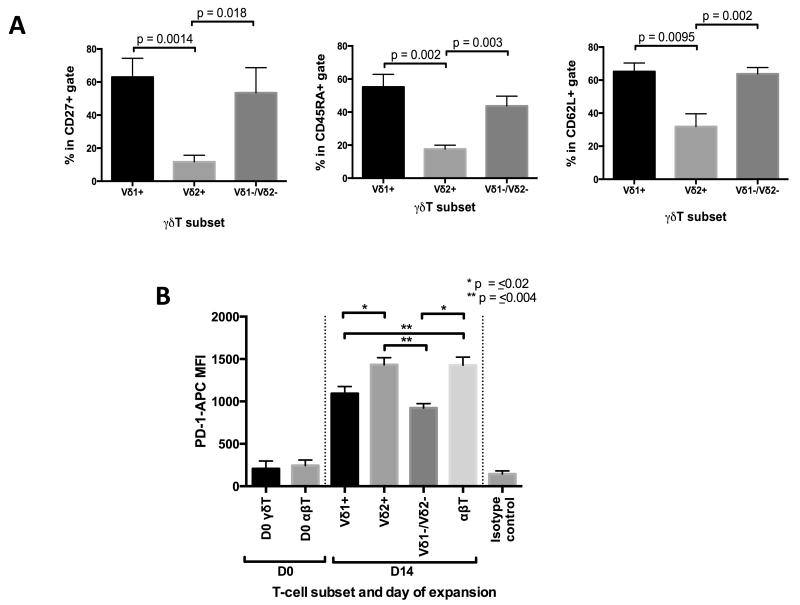
There are insufficient numbers of Vδ1negVδ2neg γδT cells to phenotype in peripheral blood but we were able to determine their memory phenotype following expansion with aAPC+B1 stimulation. Interestingly, following stimulation, Vδ1+ and Vδ1negVδ2neg γδT cells retain CD27, CD62L and CD45RA to significantly higher levels than Vδ2+ cells. (Figure 4A). The pattern of Vδ1+ γδT cells being less differentiated and Vδ2+ cells being more differentiated is preserved during and despite expansion. We hypothesised that this may be explained in terms of different degrees of antigen exposure and TCR stimulation. To explore this possibility, we evaluated expression of the death receptor PD1, which is regarded as a marker of T-cell exhaustion. Levels were comparable between un-stimulated αβT cells and γδT cells in PBMC. Following 14 days of weekly stimulation with aAPC+B1, expression of PD1 in Vδ1+ and Vδ1negVδ2neg γδT cells was significantly lower than that in Vδ2+ γδT cells or αβT cells from the same donors stimulated with weekly CD3/CD28 beads at the same time points. CD3/CD28 beads were used as a control because this repeated stimulus is a recognised means of inducing exhaustion in αβT cells (Figure 4B).
Figure 4. Memory and exhaustion markers in γδT cells after expansion with aAPC+B1.
(A) Expression of CD27, CD45RA and CD62L as measured by flow cytometry in Vδ1, Vδ2 and Vδ1negVδ2neg γδT cells following 28 days of expansion using aAPC+B1; data derived from 8 donors and error bars represent SEM. (B) Expression of the PD-1 in αβT cells and γδT cells from the same donors at baseline and after 14 days of expansion using weekly stimulation with either aAPC+B1 (γδT cells) or CD3/CD28 Dynabeads (αβT cells) data derived from 3 donors and error bars represent SEM. MFI= Mean fluorescence intensity
Differential cytotoxic function of γδT cell subsets
Vδ2+ γδT cells expanded using phosphoantigens or aminobisphosphonates will kill a variety of tumour cell lines in vitro, an effect which is augmented by the opsonisation of the target cell (1,2,6,7,26,27). Antibody dependent and independent cytotoxicity has been observed in several haematological and solid tumour models including CD20+ haematological malignancies, CD52+ lymphoma and HER2+ breast cancer lines. Nearly all neuroblastoma tumours express the ganglioside GD2, which has been successfully targeted with monoclonal antibodies ch14.18 and 3F8 in numerous clinical trials (16,28,29). In the absence of ch14.18 the innate antibody independent killing of GD2+ neuroblastoma cell lines (LAN1 or Kelly) by Vδ2+ cells expanded using IPP was minimal and significantly less than Vδ1+ γδT cells expanded using aAPC+B1 (Figure 5A). Non-transformed allogeneic PBMC were not killed (data not shown), indicating that this effect is not simply linked to an MHC-mismatch. For clarity, in this and subsequent cytotoxicity assays, E:T ratio of 10:1 is shown unless otherwise stated.
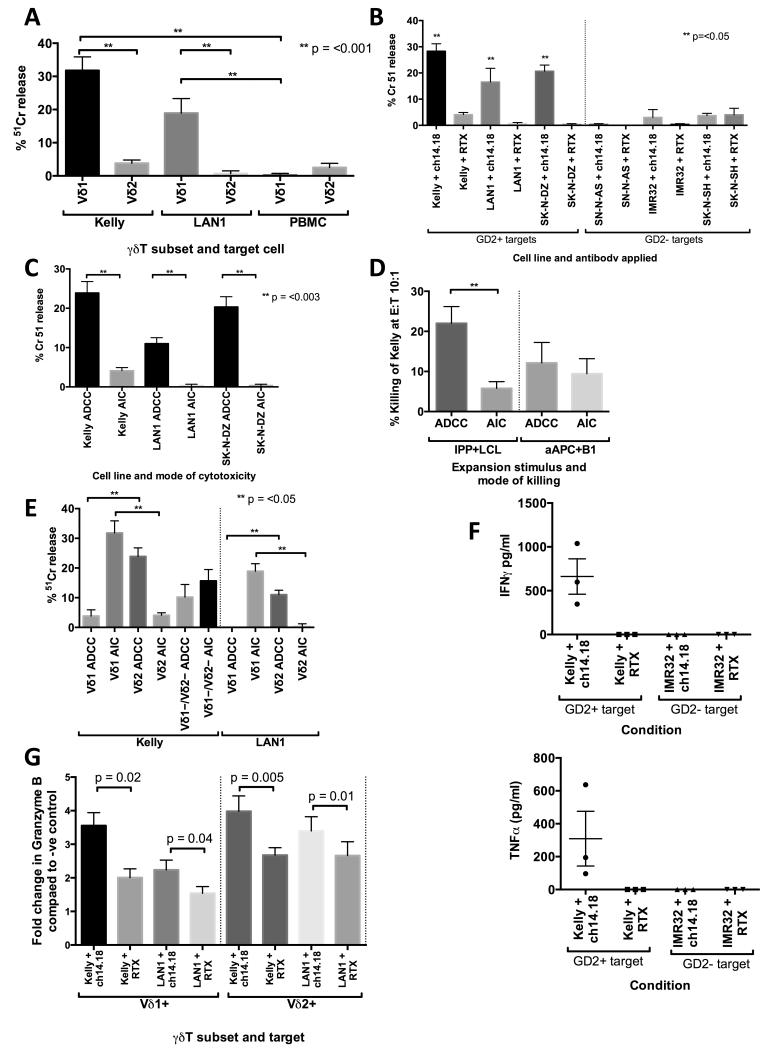
Figure 5. Differential cytotoxic profile of Vδ1, Vδ2 and Vδ1−/Vδ2− γδT cells against neuroblastoma cell lines.
(A) Antibody independent killing of GD2+ neuroblastoma cell lines by polyclonal populations of Vδ1+ and Vδ2+ γδT cells; n=11 for Kelly data; n= 3 for LAN1 data.. (B and C) Cytotoxicity of IPP expanded Vδ2+ cells is significantly enhanced by target opsonisation with ch14.18; raw data shown in B (n=3) and antibody dependent and independent components of killing shown in C (n=16 for Kelly and n= 3 for LAN1 and SKNAS) . (D) Comparative antibody dependent and independent killing of Kelly cells by Vδ2+ γδT cells expanded with IPP (n=9) or aAPC (n=7). (E) . Vδ1+, Vδ2+ and Vδ1negVδ2neg show different patterns of antibody dependent and independent cytotoxicity (n= between 5 and 11 for Kelly and n=3 or 4 for LAN1). (F) Interferon gamma and Tumor necrosis factor-alpha secretion as determine by cytokine bead array following co-culture of IPP expanded Vδ2+ with opsonized and non-opsonized Kelly cells (n=3). (G) Granzyme B in supernatant of expanded Vδ1+ and Vδ2+ γδT cells co-cultured with γδT cell sensitive GD2+ tumor cell lines Kelly and LAN1, expressed as fold change of –ve control (γδT cell insensitive cell line with irrelevant antibody)..
We then loaded the neuroblastoma cells with ch14.18 anti-GD2 antibody to determine if this would boost γδT cell cytotoxicity. In these and subsequent experiments, antibody dependent cytotoxicity (ADCC) was determined by subtracting the Antibody Independent Cytotoxicity (AIC) from total killing observed in the presence of antibody. The cytotoxicity of IPP expanded Vδ2+ γδT cells was significantly increased by target opsonisation. Moreover increased killing following addition of ch14.18 antibody was observed only against three GD2 positive and not three GD2 negative neuroblastoma cell lines. Therefore, Vδ2+ cytotoxicity following IPP expansion is predominantly antibody dependent (Figure 5B,C). However, the cytotoxicity of Vδ2+ γδT cells expanded with aAPC+B1 was not significantly increased by target opsonisation (p=0.07 at 10:1 E:T ratio), though this could be explained by the antibody independent killing of Vδ2+ cells expanded using this condition being slightly higher than those expanded with IPP (Figure 5D). In contrast, Vδ1+ γδT cells expanded with aAPC+B1 had significantly less ADCC but significantly more AIC against the cell lines tested, and Vδ1negVδ2neg γδT cells showed intermediate levels of both ADCC and AIC (Figure 5E). A full range of E:T ratios from 10:1 to 1.25:1 against the neuroblastoma cell line Kelly is shown in supplementary figure 4 and GD2 expression of neuroblastoma cell lines shown in supplementary figure 5. In line with the dependence on opsonised target cells for cytotoxic function, production of Th1 cytokines TNFα and IFNγ by IPP expanded Vδ2 γδT cells was only seen when the γδT cells were co-cultured with ch14.18 opsonised GD2+ neuroblastoma (Figure 5F). NKG2D expression in expanded Vδ2+ γδT cells was significantly higher than in Vδ1+ or Vδ1−/Vδ2− γδT cells despite identical durations of expansion (21 days) (supplementary figure 6A). Whilst both Vδ1+ and Vδ2+ γδT cells appeared to increase their production of Granzyme B in the presence of opsonised targets, the increase was more significant in the case of Vδ2+ cells (p= 0.005 and 0.01 vs. p = 0.02 and 0.04) (Figure 5G). In fact, expansion with aAPC+B1 appears to induce IFNγ and Granzyme B production in Vδ1+ and Vδ1negVδ2neg γδT cells which is not seen when Vδ2+ γδT cells are expanded with IPP+LCL, though all subtypes were capable of upregulating IFNγ and Granzyme B in response to stimulation with PMA/Ionomycin (supplementary figure 6B, representative of 3 donors). The difference is likely due to the increased level of stimulation provided by 41BB-L and CD86 on the aAPC. Staining for Nkp30 and FAS-L was negative in γδT cells co-cultured with aAPC or tumour cells, and also in those stimulated with PMA/Ionomycin (data not shown). Production of IL-1, IL-4, IL-6, IL-10, IL-13 and IL-17a by Vδ1+ or Vδ2+ γδT cells in the presence of opsonised or non-opsonised Kelly or LAN1 was insignificant (mean detected levels <1 pg/ul, n=3, data not shown).
Temporal expression of Fcγ Receptors with expansion in γδT subsets
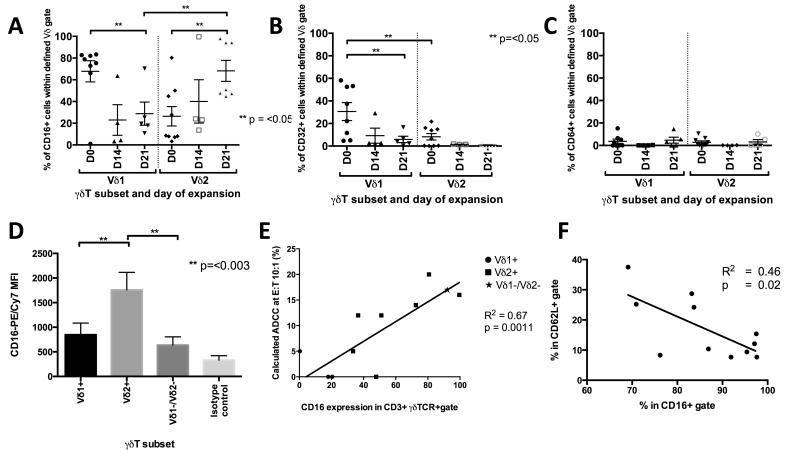
IgG antibodies can recruit effector cells for cytotoxicity or phagocytosis of opsonised targets through engagement and cross linking of the low affinity Fcγ Receptors FcγRII (CD32) or FcγRIII (CD16) or the high affinity receptor FcγRI (CD64). To investigate the mechanism of γδT cell ADCC we compared the Fcγ receptor expression of Vδ1+ and Vδ2+ γδT cells as they were expanded. Vδ1+ γδT cells demonstrated significantly greater surface expression of CD16 and CD32 than unexpanded Vδ2+ cells, (Figures 6A and 6B) whilst CD64 expression was very low (Figure 6C). Over a 3 week expansion CD32 expression fell in both subsets (Figure 6B). In contrast, in Vδ1+ cells, CD16 expression decreased significantly by day 21, whilst Vδ2+ CD16 expression rose to levels significantly greater than baseline, and also to significantly greater than that of Vδ1+ cells from the same donors at the same timepoints (Figure 6A). Whilst CD16 expression on Vδ1+ cells falls, it persists at a low level even after 21 days of expansion and is also seen at low levels in the Vδ1negVδ2neg subset (Figure 6D). CD16 expression in expanded γδT cells showed a highly significant positive correlation with their ability to exert ADCC against opsonised GD2+ neuroblastoma (R2 = 0.67, p=0.0011, Figure 6E). It has previously been reported that the more differentiated subsets of Vδ2+ γδT cells have greater expression of CD16 (30), a finding that is in keeping with our observations. CD62L loss is a recognised marker of T-cell differentiation, and there is an inverse relationship between the expression of CD62L and that of CD16 in expanding Vδ2+ cells (Figure 6F).
Figure 6. FcγR staining correlates with cytotoxicity and differentiation phenotype.
Expression of Fcγ receptors CD16 (A), CD32 (B) and CD64 (C) in Vδ1+ and Vδ2+ γδT cells over a 3 week expansion period (data from 6-7 donors). (D) Mean fluorescence intensity of CD16 surface staining from sorted populations (n=7). (E) CD16 expression correlates with the ability of γδT cells to exert ADCC and (F), in Vδ2+ cells CD16 is inversely correlated with CD62L expression.
Discussion
γδT cells have been recognized as multifaceted effector cells for immunotherapy of cancer. Their tumoricidal properties include targeting cells in an MHC-independent manner by differentiating between healthy and transformed cells (31) and expanding from peripheral blood in response to engagement of their TCR. Previous studies of cancer immunotherapy using γδT cells have either enriched Vγ9Vδ2+ numbers in patients through administration of aminobisphosphonates (32) or have expanded this population of cells ex vivo before adoptive transfer (33,34). A limitation in the field has been the lack of protocols for expansion of subsets other than Vγ9Vδ2+, and lack of understanding of the tumoricidal properties of these cells. Hence our demonstration of expansion and killing properties of the non-Vδ2 subset raises new prospects for translation into clinical studies.
We chose to use neuroblastoma as a model system for evaluation of γδT cell immunotherapy. Neuroblastoma immune evasion mechanisms include production of soluble NKG2D ligands sMICA and sMICB (35) and low expression of MHC (36) which protect the tumour against MHC-dependent killing by CD8+ T cells and NKG2D-bearing NK cells. Moreover neuroblastoma is amenable to immunotherapy as demonstrated by significant clinical benefit to patients treated with ch14.18 anti-GD2 monoclonal antibody (16,28,29), and sensitivity of neuroblastoma cells to killing by Vγ9Vδ2+ γδT cells (31).
We have shown that γδT subsets undergo unbiased expansion to clinically useful numbers from blood donors or neuroblastoma patients using anti-γδTCR antibody-coated artificial Antigen Presenting Cells. This degree of expansion is comparable with that using bisphosphonates or their metabolic products (37,38). Previous studies have shown activities of γδT cells against haematological malignancies (2,7). renal cell carcinoma (32,39), non-small cell lung cancer (33), osteosarcoma (40) and prostate cancer (41), and tumoricidal properties of non-Vδ2 γδT cells (21,37,42,43). Using aAPC expansion we have generated Vδ1, Vδ2 and Vδ1negVδ2neg populations with distinctive properties.
Phosphoantigen activated or expanded Vδ2+ γδT cells have previously been shown to exert effective ADCC with lymphoma (2,7) and breast cancer (6,26) and variable innate killing activity against neuroblastoma cells (31). In our hands IPP expanded Vδ2+ δ2 cells have little innate cytotoxicity against allogeneic neuroblastoma cell lines but marked ADCC, associated with release of Th1 cytokines IFNγ and TNFα. In contrast, Vδ2+ cells expanded with aAPC+B1 had greater innate killing, but their capacity for ADCC was reduced. It might be that this differential polarisation in the two different culture conditions is independent of TCR signalling and results from alternate signals. An alternate hypothesis is that IPP and the B1 antibody preferentially expand γδT cells with different Vδ2 TCR chains and associated with different killing properties. In favour of this we note that some of the Vδ2 cells have non Vγ9 pairings (Figure 2). Similarly, Vδ1 cells consistently show greater antibody independent killing supporting the notion that different TCR are associated with different killing properties. Further studies are required to determine the mechanisms of innate killing. Importantly, there is a strong correlation between CD16 expression and ADCC; whereas γδT bearing a non-δ2 chain lose CD16 and ADCC properties as they expand, δ2 TCR positive cells retain relatively bright CD16 expression and remain ADCC competent. Whether this polarization of phenotype is due to qualitative or quantitative difference in signalling through the TCR remains an open question. A possible explanation for lack of antibody independent killing of neuroblastoma by Vδ2 cells relates to the production of soluble NKG2D ligands sMICA, sMICB and ULPB1-6 by neuroblastoma cells, which can block the NKG2D receptor (35,44). There are significantly higher levels of NKG2D on expanded Vδ2+ γδT cells (supplementary Figure 5) which may make them particularly susceptible to suppression by soluble NKG2D ligands.
This is the first demonstration of the cytotoxicity of Vδ1+ and Vδ1negVδ2neg γδT cells against neuroblastoma and it offers an alternative to NK cells for generation of large bulk populations of innate killer cells for adoptive transfer. The Vδ1negVδ2neg cells are a heterogeneous population and maybe not surprisingly their cytotoxicity shows both antibody dependent and independent elements, with a (non significant) tendency towards innate killing. Future studies will require single cell sequencing or expansion of clones of Vδ1negVδ2neg, as well as the more conventional Vδ1 and Vδ2 containing populations, to define the different Vγ/Vδ pairings, and to study the functional significance of each pairing. We propose that expanded Vγ9Vδ2+ cells will have the most potential clinical benefit in combination with a tumor antigen specific therapeutic antibody such as rituximab, herceptin or anti-GD2. However in bulk expansions, the more modest innate cytotoxicity of aAPC+B1 expanded Vδ2+ could be combined with the much more potent cytotoxicity of Vδ1+ and Vδ1negVδ2neg γδT cells.
It is striking that following stimulation with the pan-γδTCR antibody and aAPC, Vδ2+ cells develop a more differentiated phenotype than Vδ1+ or Vδ1negVδ2neg cells. There are several possible explanations. Firstly, the differences may reflect greater differentiation in the starting populations. This could be explained in terms of a relatively greater frequency of exposure to the ligands of the Vγ9Vδ2 TCR compared with the (largely unknown) ligands of Vδ1+ or Vδ1negVδ2neg TCRs. Secondly there might be a quantitatively greater stimulus to the cells associated with engagement of the Vγ9Vδ2 TCR compared with alternate stimuli. Finally, engagement of the Vγ9Vδ2 TCR might result in qualitatively different signalling and a specific drive towards a more differentiated phenotype. Distinguishing these different explanations will require detailed studies of TCR ligand effects and intracellular signalling. The preservation of relatively un-differentiated non-Vδ2 subsets of γδT cells, with a less exhausted phenotype is potentially exciting, as these cells have characteristics associated with efficacious cellular therapy products.
The differentiation state of T cells has important implications for their efficacy in cellular therapy. It is recognized that adoptive cell therapy using less differentiated CD8+ cells is more efficacious (45), a finding that may also be true in the case of γδT cells. Phenotyping using CD27, CD45RA and CD62L is commonly used to determine the memory phenotype of αβT cells and has also been used for the same purpose in both Vδ2+ and Vδ1+ cells (24,25,38). Using these, we have shown that Vδ1+ γδT cells from neuroblastoma patients at the point of diagnosis are significantly less differentiated than Vδ2+ γδT cells from the same blood samples, a finding which is also seen in healthy adult donors. Following 28 days of expansion, Vδ1+ and Vδ1negVδ2neg γδT cells express a less differentiated state. Vδ2+ γδT cells are uniformly CD27low/CD62Llow/CD45RAlow, falling into the effector memory subset. Interestingly, in contrast to the findings of Angelini and colleagues (30), expanded Vδ2+, which are predominantly CD27−/CD45RA−, also express CD16. Hence, in expanded bulk populations using antibody B1 coated aAPC, there are cells of central memory phenotype expected to provide longevity following adoptive transfer, and cells primed for ADCC which will provide additional anti-tumor efficacy.
T-cell exhaustion refers to a state induced by chronic antigen exposure and characterized by a decline in T-cell function – specifically a loss of ability to lyse target cells and produce cytokines such as IFNγ and TNFα (46,47). CTLA4 and PD-1 are inhibitory receptors associated with hyper-stimulated T cells which provide important immunological checkpoints to immune activation (48). We chose to measure PD-1 as a representative marker of hyper-stimulation/exhaustion. PD-1 expression by Vδ1+ and Vδ1negVδ2neg γδT cells was significantly lower than that seen in Vδ2+ γδT cells in the same samples. This finding suggests Vδ1+ and Vδ1negVδ2neg γδT cells might be more favorable in adoptive transfer, a hypothesis that requires testing in clinical studies. Importantly interaction between PD-1 and PDL-1 is a recognized immune escape mechanism of many tumours (49).
In summary we have identified a novel approach for unbiased expansion of γδT cells from peripheral blood of cancer patients. Artificial antigen presenting cells are readily available for translation into GMP manufacturing. Unlike previous expansion studies favoring Vδ2 cell expansion, our method will also expand Vδ1+ and Vδ1negVδ2neg γδT cells, which have a more favorable innate killing and memory phenotype. Adoptive transfer of a bulk population of expanded cells bearing a broad repertoire of γδTCR may allow both innate killing and ADCC function to be exploited. Combined with the antigen presenting function of γδT cells this may prove to be an optimal adoptive cell therapy approach for cancer.
Supplementary Material
Statement of translational relevance.
Gamma delta T cells comprise less than 5% of peripheral blood T lymphocytes in most populations. Any strategies to exploit them in cancer therapy adoptive transfer must therefore involve large scale ex vivo expansions. Previous studies have employed aminobisphosphonates or functional equivalents to expand the Vγ9Vδ2 lineage, but strategies to expand γδT cells bearing other receptors have not been developed as clinical applications. Here we show that artificial antigen presenting cells that can be used within GMP protocols, can result in the unbiased expansion of a wide range of repertoires, The Vδ1 lineage and the Vδ1negVδ2neg lineage in the expanded populations are less differentiated and show potent antibody independent cytotoxicity against neuroblastoma cells. This demonstration of robust expansion and cytotoxicity of polyclonal gamma delta T cells supports translation of the technology into adoptive transfer clinical trials.
References
- 1.Himoudi N, Morgenstern DA, Yan M, Vernay B, Saraiva L, Wu Y, et al. Human γδT Lymphocytes Are Licensed for Professional Antigen Presentation by Interaction with Opsonized Target Cells. The Journal of Immunology. 2012;188:1708–16. doi: 10.4049/jimmunol.1102654. [DOI] [PubMed] [Google Scholar]
- 2.Gertner-Dardenne J, Bonnafous C, Bezombes C, Capietto AH, Scaglione V, Ingoure S, et al. Bromohydrin pyrophosphate enhances antibody-dependent cell-mediated cytotoxicity induced by therapeutic antibodies. Blood. 2009;113:4875–84. doi: 10.1182/blood-2008-08-172296. [DOI] [PubMed] [Google Scholar]
- 3.Brandes M, Willimann K, Moser B. Professional antigen-presentation function by human gammadelta T Cells. Science. 2005;309:264–8. doi: 10.1126/science.1110267. [DOI] [PubMed] [Google Scholar]
- 4.Wu Y, Wu W, Wong WM, Ward E, Thrasher AJ, Goldblatt D, et al. Human γδ T Cells: A Lymphoid Lineage Cell Capable of Professional Phagocytosis. The Journal of Immunology. 2009;183:5622–9. doi: 10.4049/jimmunol.0901772. [DOI] [PubMed] [Google Scholar]
- 5.Morgan GJ, Davies FE, Gregory WM, Cocks K, Bell SE, Szubert AJ, et al. First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomised controlled trial. Lancet. 2010;376:1989–99. doi: 10.1016/S0140-6736(10)62051-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tokuyama H, Hagi T, Mattarollo SR, Morley J, Wang Q, Fai-So H, et al. Vγ9Vδ2 T cell cytotoxicity against tumor cells is enhanced by monoclonal antibody drugs—Rituximab and trastuzumab. Int J Cancer. 2008;122:2526–34. doi: 10.1002/ijc.23365. [DOI] [PubMed] [Google Scholar]
- 7.Braza MS, Klein B, Fiol G, Rossi JF. γδT-cell killing of primary follicular lymphoma cells is dramatically potentiated by GA101, a type II glycoengineered anti-CD20 monoclonal antibody. Haematologica. 2011;96:400–7. doi: 10.3324/haematol.2010.029520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Rosa SC, Andrus JP, Perfetto SP, Mantovani JJ, Herzenberg LA, Herzenberg LA, et al. Ontogeny of gamma delta T cells in humans. J Immunol. 2004;172:1637–45. doi: 10.4049/jimmunol.172.3.1637. [DOI] [PubMed] [Google Scholar]
- 9.Hviid L, Akanmori BD, Loizon S, Kurtzhals JA, Ricke CH, Lim A, et al. High frequency of circulating gamma delta T cells with dominance of the v(delta)1 subset in a healthy population. Int Immunol. 2000;12:797–805. doi: 10.1093/intimm/12.6.797. [DOI] [PubMed] [Google Scholar]
- 10.Déchanet J, Merville P, Bergé F, Bone-Mane G, Taupin JL, Michel P, et al. Major expansion of gammadelta T lymphocytes following cytomegalovirus infection in kidney allograft recipients. J Infect Dis. 1999;179:1–8. doi: 10.1086/314568. [DOI] [PubMed] [Google Scholar]
- 11.Zhao J, Huang J, Chen H, Cui L, He W. Vdelta1 T cell receptor binds specifically to MHC I chain related A: molecular and biochemical evidences. Biochem Biophys Res Commun. 2006;339:232–40. doi: 10.1016/j.bbrc.2005.10.198. [DOI] [PubMed] [Google Scholar]
- 12.Spada FM, Grant EP, Peters PJ, Sugita M, Melián A, Leslie DS, et al. Self-recognition of CD1 by gamma/delta T cells: implications for innate immunity. J Exp Med. 2000;191:937–48. doi: 10.1084/jem.191.6.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vantourout P, Hayday A. Six-of-the-best: unique contributions of γδ T cells to immunology. Nat Rev Immunol. 2013;13:88–100. doi: 10.1038/nri3384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maeurer MJ, Martin D, Walter W, Liu K, Zitvogel L, Halusczcak K, et al. Human intestinal Vdelta1+ lymphocytes recognize tumor cells of epithelial origin. J Exp Med. 1996;183:1681–96. doi: 10.1084/jem.183.4.1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Devaud C, Rousseau B, Netzer S, Pitard V, Paroissin C, Khairallah C, et al. Anti-metastatic potential of human Vδ1(+) γδ T cells in an orthotopic mouse xenograft model of colon carcinoma. Cancer Immunol Immunother. 2013 doi: 10.1007/s00262-013-1402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu AL, Gilman AL, Ozkaynak MF, London WB, Kreissman SG, Chen HX, et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N Engl J Med. 2010;363:1324–34. doi: 10.1056/NEJMoa0911123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogbomo H, Hahn A, Geiler J, Michaelis M, Doerr HW, Cinatl J. NK sensitivity of neuroblastoma cells determined by a highly sensitive coupled luminescent method. Biochem Biophys Res Commun. 2006;339:375–9. doi: 10.1016/j.bbrc.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 18.Lefranc M-P, Giudicelli V, Ginestoux C, Jabado-Michaloud J, Folch G, Bellahcene F, et al. IMGT, the international ImMunoGeneTics information system. Nucleic Acids Res. 2009;37:D1006–12. doi: 10.1093/nar/gkn838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Magoč T, Salzberg SL. FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics. 2011;27:2957–63. doi: 10.1093/bioinformatics/btr507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas N, Heather J, Ndifon W, Shawe-Taylor J, Chain B. Decombinator: a tool for fast, efficient gene assignment in T-cell receptor sequences using a finite state machine. Bioinformatics. 2013;29:542–50. doi: 10.1093/bioinformatics/btt004. [DOI] [PubMed] [Google Scholar]
- 21.Zhou J, Kang N, Cui L, Ba D, He W. Anti-γδ TCR antibody-expanded γδ T cells: a better choice for the adoptive immunotherapy of lymphoid malignancies. Cell Mol Immunol. 2011;9:34–44. doi: 10.1038/cmi.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suhoski MM, Golovina TN, Aqui NA, Tai VC, Varela-Rohena A, Milone MC, et al. Engineering artificial antigen-presenting cells to express a diverse array of co-stimulatory molecules. Mol Ther. 2007;15:981–8. doi: 10.1038/mt.sj.6300134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilhelm M. T cells for immune therapy of patients with lymphoid malignancies. Blood. 2003;102:200–6. doi: 10.1182/blood-2002-12-3665. [DOI] [PubMed] [Google Scholar]
- 24.Dieli F, Poccia F, Lipp M, Sireci G, Caccamo N, Di Sano C, et al. Differentiation of Effector/Memory V 2 T Cells and Migratory Routes in Lymph Nodes or Inflammatory Sites. Journal of Experimental Medicine. 2003;198:391–7. doi: 10.1084/jem.20030235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pitard V, Roumanes D, Lafarge X, Couzi L, Garrigue I, Lafon M-E, et al. Long-term expansion of effector/memory Vdelta2-gammadelta T cells is a specific blood signature of CMV infection. Blood. 2008;112:1317–24. doi: 10.1182/blood-2008-01-136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Capietto AH, Martinet L, Fournie JJ. Stimulated T Cells Increase the In Vivo Efficacy of Trastuzumab in HER-2+ Breast Cancer. The Journal of Immunology. 2011;187:1031–8. doi: 10.4049/jimmunol.1100681. [DOI] [PubMed] [Google Scholar]
- 27.Chen Z, Freedman MS. CD16+ gammadelta T cells mediate antibody dependent cellular cytotoxicity: potential mechanism in the pathogenesis of multiple sclerosis. Clin Immunol. 2008;128:219–27. doi: 10.1016/j.clim.2008.03.513. [DOI] [PubMed] [Google Scholar]
- 28.Cheung N-KV, Cheung IY, Kushner BH, Ostrovnaya I, Chamberlain E, Kramer K, et al. Murine anti-GD2 monoclonal antibody 3F8 combined with granulocyte-macrophage colony-stimulating factor and 13-cis-retinoic acid in high-risk patients with stage 4 neuroblastoma in first remission. Journal of Clinical Oncology. 2012;30:3264–70. doi: 10.1200/JCO.2011.41.3807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simon T, Hero B, Faldum A, Handgretinger R, Schrappe M, Niethammer D, et al. Consolidation Treatment With Chimeric Anti-GD2-Antibody ch14.18 in Children Older Than 1 Year With Metastatic Neuroblastoma. Journal of Clinical Oncology. 2004;22:3549–57. doi: 10.1200/JCO.2004.08.143. [DOI] [PubMed] [Google Scholar]
- 30.Angelini DF. FcγRIII discriminates between 2 subsets of V 9V 2 effector cells with different responses and activation pathways. Blood. 2004;104:1801–7. doi: 10.1182/blood-2004-01-0331. [DOI] [PubMed] [Google Scholar]
- 31.Chargui J, Combaret V, Scaglione V, Iacono I, Péri V, Valteau-Couanet D, et al. Bromohydrin pyrophosphate-stimulated Vgamma9delta2 T cells expanded ex vivo from patients with poor-prognosis neuroblastoma lyse autologous primary tumor cells. J Immunother. 2010;33:591–8. doi: 10.1097/CJI.0b013e3181dda207. [DOI] [PubMed] [Google Scholar]
- 32.Lang JM, Kaikobad MR, Wallace M, Staab MJ, Horvath DL, Wilding G, et al. Pilot trial of interleukin-2 and zoledronic acid to augment γδ T cells as treatment for patients with refractory renal cell carcinoma. Cancer Immunol Immunother. 2011;60:1447–60. doi: 10.1007/s00262-011-1049-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakajima J, Murakawa T, Fukami T, Goto S, Kaneko T, Yoshida Y, et al. A phase I study of adoptive immunotherapy for recurrent non-small-cell lung cancer patients with autologous γδ T cells. European Journal of Cardio-Thoracic Surgery. 2010;37:1191–7. doi: 10.1016/j.ejcts.2009.11.051. [DOI] [PubMed] [Google Scholar]
- 34.Fournié J-J, Sicard H, Poupot M, Bezombes C, Blanc A, Romagné F, et al. What lessons can be learned from γδ T cell-based cancer immunotherapy trials? Cell Mol Immunol. 2012:1–7. doi: 10.1038/cmi.2012.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Raffaghello L, Prigione I, Airoldi I, Camoriano M, Morandi F, Bocca P, et al. Mechanisms of immune evasion of human neuroblastoma. Cancer Letters. 2005;228:155–61. doi: 10.1016/j.canlet.2004.11.064. [DOI] [PubMed] [Google Scholar]
- 36.Wölfl M, Jungbluth AA, Garrido F, Cabrera T, Meyen-Southard S, Spitz R, et al. Expression of MHC class I, MHC class II, and cancer germline antigens in neuroblastoma. Cancer Immunol Immunother. 2005;54:400–6. doi: 10.1007/s00262-004-0603-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deniger DC, Switzer K, Mi T, Maiti S, Hurton L, Singh H, et al. Bispecific T-cells Expressing Polyclonal Repertoire of Endogenous γδ T-cell Receptors and Introduced CD19-specific Chimeric Antigen Receptor. Mol Ther. 2013;21:638–47. doi: 10.1038/mt.2012.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Siegers GM, Ribot EJ, Keating A, Foster PJ. Extensive expansion of primary human gamma delta T cells generates cytotoxic effector memory cells that can be labeled with Feraheme for cellular MRI. Cancer Immunol Immunother. 2012 doi: 10.1007/s00262-012-1353-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kobayashi H, Tanaka Y, Yagi J, Osaka Y, Nakazawa H, Uchiyama T, et al. Safety profile and anti-tumor effects of adoptive immunotherapy using gamma-delta T cells against advanced renal cell carcinoma: a pilot study. Cancer Immunol Immunother. 2007;56:469–76. doi: 10.1007/s00262-006-0199-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li Z. Potential of human γδ T cells for immunotherapy of osteosarcoma. Mol Biol Rep. 2013;40:427–37. doi: 10.1007/s11033-012-2077-y. [DOI] [PubMed] [Google Scholar]
- 41.Dieli F, Vermijlen D, Fulfaro F, Caccamo N, Meraviglia S, Cicero G, et al. Targeting human {gamma}delta} T cells with zoledronate and interleukin-2 for immunotherapy of hormone-refractory prostate cancer. Cancer Research. 2007;67:7450–7. doi: 10.1158/0008-5472.CAN-07-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siegers GM, Dhamko H, Wang X-H, Mathieson AM, Kosaka Y, Felizardo TC, et al. Human Vδ1 γδ T cells expanded from peripheral blood exhibit specific cytotoxicity against B-cell chronic lymphocytic leukemia-derived cells. Cytotherapy. 2011;13:753–64. doi: 10.3109/14653249.2011.553595. [DOI] [PubMed] [Google Scholar]
- 43.Hua F, Kang N, Gao Y-A, Cui L-X, Ba D-N, He W. Potential regulatory role of in vitro-expanded Vδ1 T cells from human peripheral blood. Immunol Res. 2013;56:172–80. doi: 10.1007/s12026-013-8390-2. [DOI] [PubMed] [Google Scholar]
- 44.Raffaghello L, Prigione I, Airoldi I, Camoriano M, Levreri I, Gambini C, et al. Neoplasia (New York, NY) Vol. 6. Neoplasia Press; 2004. Downregulation and/or Release of NKG2D Ligands as Immune Evasion Strategy of Human Neuroblastoma; p. 558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Klebanoff CA, Gattinoni L, Restifo NP. Sorting through subsets: which T-cell populations mediate highly effective adoptive immunotherapy? J Immunother. 2012;35:651–60. doi: 10.1097/CJI.0b013e31827806e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zinselmeyer BH, Heydari S, Sacristán C, Nayak D, Cammer M, Herz J, et al. PD-1 promotes immune exhaustion by inducing antiviral T cell motility paralysis. Journal of Experimental Medicine. 2013;210:757–74. doi: 10.1084/jem.20121416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wherry EJ, Blattman JN, Murali-Krishna K, van der Most R, Ahmed R. Viral persistence alters CD8 T-cell immunodominance and tissue distribution and results in distinct stages of functional impairment. J Virol. 2003;77:4911–27. doi: 10.1128/JVI.77.8.4911-4927.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wherry EJ, Ha S-J, Kaech SM, Haining WN, Sarkar S, Kalia V, et al. Molecular signature of CD8+ T cell exhaustion during chronic viral infection. Immunity. 2007;27:670–84. doi: 10.1016/j.immuni.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 49.Hamid O, Robert C, Daud A, Hodi FS, Hwu W-J, Kefford R, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369:134–44. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.