Abstract
Asthma occurs as a result of complex interactions of environmental and genetic factors. Clinical studies and animal models of asthma indicate offspring of allergic mothers have increased risk of development of allergies. Environmental factors including stress-induced corticosterone and vitamin E isoforms during pregnancy regulate the risk for offspring development of allergy. In this review, we discuss mechanisms for the development of allergic disease early in life, environmental factors that may impact the development of risk for allergic disease early in life, and how the variation in global prevalence of asthma may be explained, at least in part, by some environmental components.
Keywords: Allergy, Neonate, Fetus, Dendritic cells, Corticosterone, α-Tocopherol
Introduction
Asthma is a heterogeneous disease resulting from complex interactions of environmental and genetic factors [1, 2]. The World Health Organization reported that the prevalence of asthma from 1950 to the present has increased in countries regardless of whether they had high, intermediate, or low rates of asthma [3–6]. The rise in rates of asthma over a few decades [4–6] and the differences in rates among countries and in migrating populations suggest an important role of the local environment in the development of asthma. Therefore, it is critical to determine mechanisms for the development of allergy/asthma and identify environmental mediators that regulate the development of allergy in order to identify novel targets for intervention. Allergic disease often starts early in life in humans and animal models [7–15]. In this review, we discuss mechanisms for the development of allergic disease early in life and discuss environmental factors that impact the development of risk for allergic disease early in life.
Maternal Transfer of Risk of Allergy to Offspring
Some studies suggest that the development of allergen responsiveness may occur prenatally [16–18]. In reports examining human maternal and paternal asthma associations with the development of allergies in offspring, most associations are with maternal allergy/asthma [7, 19–26], suggesting that sensitization can occur prenatally or early postnatally. It is suggested that in utero and early exposures to environmental factors are critical for increased risk of allergic disease [27]. There is an association of higher risk of eczema, wheezing, and lower respiratory tract infections in early life with increases in human maternal and cord blood C-reactive protein, which is an acute phase protein produced during inflammation [28, 29]. A mouse model for maternal transfer of risk of allergy to offspring has been established [7–14]. This model reflects many of the parameters of development of allergic disease in humans including increased risk for development of allergies in offspring of allergic mothers. Moreover, as in humans, in this mouse model, the allergic responses of the offspring are not specific to the allergen of the mother.
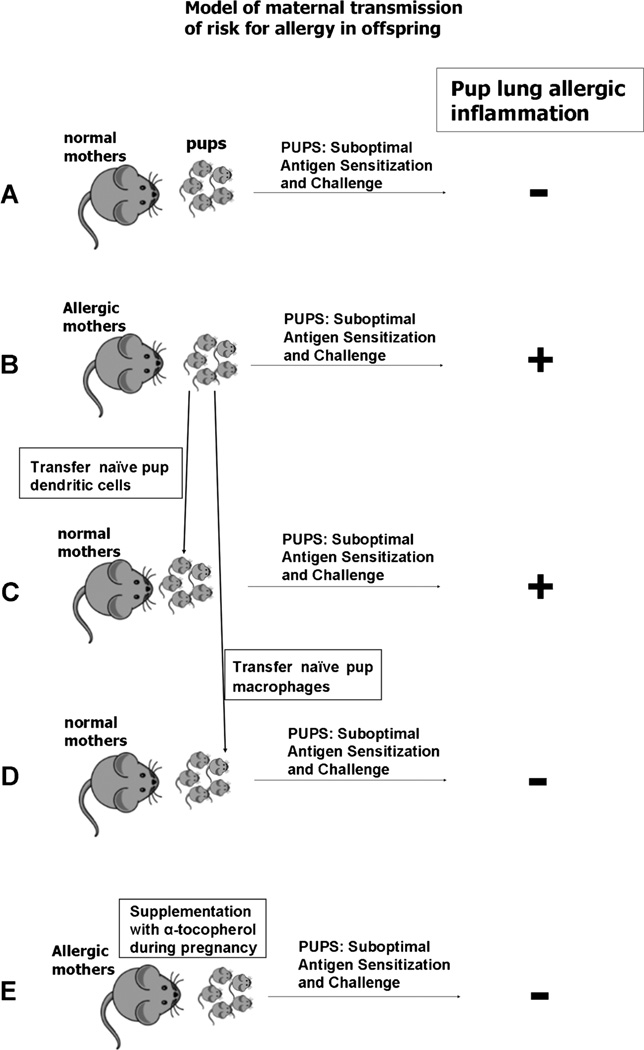
In the mouse model of maternal transfer of risk of allergy to offspring, allergy is induced in female mice by sensitizing with chicken egg ovalbumin (OVA)/alum on weeks 1 and 2 and then challenging with OVA three times on weeks 4, 8, and 12 [7–14]. After the last OVA challenge in week 12, these female mice are mated [7–14]. Therefore, the female mice have allergic lung inflammation during the first half of the pregnancy because it takes about 2 weeks for resolution of allergic lung inflammation, which is the majority of the 3 weeks of mouse gestation. Additional challenge with OVA during pregnancy is not necessary for induction of risk of allergy in the offspring [30]. To determine allergen responsiveness in the offspring, the offspring are treated with a suboptimal OVA protocol, such that the neonates receive only one instead of two OVA/alum treatments at postnatal day 3–5 and then starting 7 days later; the neonates are challenged with aerosolized OVA for three consecutive days [7–14]. Alternatively, the offspring are challenged with casein [30]. The offspring of these allergic mothers develop allergic lung inflammation and airway responsiveness whereas pups from non-allergic mothers do not develop inflammation in response to the allergen challenge [7–14] (Fig. 1a, b). Moreover, this ability of the offspring of allergic mothers to respond to allergen is sustained for up to 8 weeks of age in the mouse [9]. The magnitude of the offspring response to an initial allergen challenge declines in the offspring after 8 weeks [9]. Allergic responses are inhibited in the mother by anti- IL-4 antibody administration to the mothers at preconception and this maternal anti-IL-4 treatment blocks the development of responsiveness of offspring to suboptimal allergen [30]. These data suggest that an IL-4-dependent allergic response in the mother is involved in the transmission of risk to the offspring. However, IL-4 and IgE do not pass to the fetus from the mother [18, 31–33]. It was reported that antibody depletion of T cells in allergic mothers modulates the development of responsiveness of offspring to allergen [10]. In other studies, adoptive transfer of allergen-specific T cells from OVA TCR transgenic mice DO11.10 mice to females prior to mating results in offspring with responsiveness to suboptimal challenge of antigen [11]. These data suggest that maternal Th2 responses induce maternal signals that induce development of allergen responsiveness in offspring. Thus, female mice that are allergic before conception and develop a Th2 response during pregnancy produce offspring that have augmented responsiveness to suboptimal allergen challenge.
Fig. 1.
Model of maternal transmission of risk for allergy in offspring. Female mice are sensitized with chicken egg ovalbumin (OVA)/alum on weeks 1 and 2 and then challenging with OVA three times on weeks 4, 8, and 12 [7–14]. After the last OVA challenge in week 12, these female mice are mated [7–14]. To determine allergen responsiveness in the offspring, the offspring are treated with a suboptimal OVA protocol, such that the neonates receive only one instead of two OVA/alum treatments at postnatal day 3–5, and then starting 7 days later, the neonates are challenged with aerosolized OVA for three consecutive days [7–14]. a Normal mothers. b Allergic mothers. c Dendritic cells are isolated from the spleens of pups from allergic mothers before pup treatment with allergen. These dendritic cells are transferred to pups from non-allergic mothers. d Macrophages are isolated from the spleens of pups from allergic mothers before pup treatment with allergen. Macrophages are transferred to pups from non-allergic mothers. e Allergic mothers are supplemented with α-tocopherol at the time of mating
The responses of the offspring from allergic mothers are not specific to the allergen to which the mother responds. Uthoff et al. [18] reported that allergens can cross the placenta but that offspring are responsive to BLG whereas mothers were stimulated with OVA, suggesting that the process is antigen-independent. The antigen-independent maternal transfer of risk of allergy to offspring was also demonstrated by Hamada et al. [30]. In their report, offspring are responsive to casein whereas the mothers were sensitized and challenged at preconception with OVA [30]. An antigen-independent effect of maternal allergy on allergen responsiveness in pups has also been demonstrated in canines [34]. Similarly, in humans, children respond to different allergens than the allergic mother [7]. Thus, the offspring responses are not specific to the allergen that the mother responds to but instead, the offspring have an increased responsiveness to sensitization to allergens.
Maternal Effect on Offspring Dendritic Cells
Offspring from allergic mothers have increased allergic responsiveness to suboptimal allergen challenge and we and others report that the maternal effect alters offspring dendritic cells [7, 8, 35•, 36, 37]. Fedulov et al. [37] reported that the increased responsiveness of the offspring occurs through changes in pup dendritic cells but not in pup macrophages. In their studies, the transfer of splenic dendritic cells from non-challenged neonates of allergic mothers into neonates from non-allergic mothers confers increased allergic susceptibility in recipient neonates (Fig. 1c) [37]. In contrast, the transfer of macrophages from non-challenged neonates of allergic mothers into neonates from non-allergic mothers does not confer increased allergic susceptibility in recipient neonates (Fig. 1d) [37]. This is suggestive of a functional change in neonatal dendritic cells in offspring from allergic mothers. Changes in dendritic cells are consistent with the antigen-independent transfer of risk from allergic mothers to offspring in humans [7] and in animal models [8–14].
We reported that offspring of allergic mothers have an increase in a distinct subset of dendritic cells. The fetal livers from allergic mothers and the OVA-challenged pup lungs from offspring of allergic mothers had increased numbers of CD11b+ subsets of CD11c+ dendrititc cells [35•], a dendritic cell subset that is critical for generation of allergic responses [38•]. In contrast, in these tissues, there were no changes in CD11b− regulatory dendritic cells subsets, including plasmacytoid dendritic cells and CD103+ dendritic cells [35•]. Furthermore, Mikhaylova et al. [39•] reported that before antigen challenge of the pups, the dendritic cells of pups from allergic mothers had little transcriptional changes but extensive DNA methylation changes. Then, after allergen challenge, there were many transcriptional changes in the dendritic cells [39•]. These studies suggest that mediators, which do not confer allergen specificity, may be transferred from the mother to the offspring and these mediators regulate offspring dendritic cells and heighten the responsiveness of offspring to challenge with suboptimal doses of allergens.
Breast Milk and Offspring Allergy
There is a role of breast milk of allergic mice on the development of allergic responses in offspring in the model in Fig. 1b. However, the milk of allergic mothers is not necessary for the offspring allergic responses because the in utero maternal effects are sufficient for allergic responses by offspring of allergic mothers. This was demonstrated by cross-fostering the offspring. Briefly, pups from allergic mothers that are nursed by non-allergic mothers still have an allergic response to suboptimal challenge with OVA [32]. Therefore, maternal effects in utero mediate development of allergen responsiveness in offspring of allergic mothers [32]. Breast milk is sufficient, but not necessary, for maternal transmission of asthma risk in the offspring because when pups from non-allergic mothers are nursed by allergic mothers, the pups exhibit a response to suboptimal allergen challenge [32]. In this study, the breast milk from allergic and non-allergic mothers contained no detectable IFNγ, IL-2, IL-4, IL-5, IL-13, or TNFα, suggesting that other mediators increase the risk of offspring allergy through breast milk [32]. In clinical studies, it is reported that the mediators, omega-3 and omega-6 polyunsaturated fatty acids, in human milk associate with asthma and atopy but the mechanism is not known [40, 41]. Miyake et al. [42] reported that omega-3 fatty acids during pregnancy associate with lower infantile wheeze.
In other mouse models, the function of breast milk has been studied in female mothers that were not allergic at preconception. In these models, the non-allergic mother mice were exposed during pregnancy or lactation to allergen or an antigen tolerance protocol. This is in contrast to the clinical reports demonstrating that the risk for allergy in children has been associated with mothers with existing allergic disease before conception [7, 19–26]. Nevertheless, in mouse models where the mother was not allergic at preconception, but then exposed during pregnancy or lactation to allergen or an antigen tolerance protocol, there was protection of offspring responses to allergen sensitization/challenge. Briefly, it is reported that exposure of normal female mice during lactation to OVA results in transfer of antigen and TGFβ in milk, and this inhibited allergic inflammation in offspring treated later as adults (6–8 weeks old) with two sensitizations with OVA/alum and five OVA challenges [43]. These adult offspring also had elevated regulatory CD4+ T cells and the increase in T regulatory cells was dependent on milk TGFβ but not milk immunoglobulins [43]. In another approach, it was demonstrated that sensitization of females before mating and then extensive antigen challenges (10 OVA challenges) during lactation resulted in transfer of IgG immune complexes in the milk and induction of regulatory T cells and tolerance in the offspring when offspring were challenged with OVA at 6–8 weeks old; in this model, immune complexes but not TGFβ in the milk was required for tolerance [44]. Similar data were reported for allergic mothers and an offspring 60-day treatment protocol with subcutaneous OVA/alum, intraperitoneal OVA, and then five OVA challenges [45]. In summary, depending on timing, doses, and number of antigen challenges, factors in breast milk can contribute mediators that either increase or decrease offspring responses to allergen.
Maternal Exposure to Th2-Inducing Environmental Irritants Also Enhances Offspring Allergic Responses, Whereas Th1 Stimuli Reduce Offspring Allergic Responses
A maternal effect on offspring allergic responses has also been demonstrated for maternal exposure to environmental irritants. Maternal inhalation of titanium oxide or diesel exhaust particles during pregnancy increased responses of offspring to allergen challenge [46]. Also, skin sensitization to toluene diisocyanate (TDI) induces a Th2 response in the mother, and when the mother was mated after second dose of TDI, the offspring had increased allergic responses to suboptimal OVA [36].
It is also reported that a Th1 response in the mother may protect the offspring from developing allergic responses. When females are sensitized to dinitrochlorobenzene (DNCB), which induces a Th1 response, and then mated, the offspring do not develop an allergic response to suboptimal OVA [36]. Also, offspring are protected from the development of asthma by prenatal challenge of the mother with LPS, which induces a Th1 inflammation, an increase in IFNγ, and a decrease in IL-5 and IL-13 [47–50]. In addition, injection of non-allergic mothers with IFNγ on gestational day 6.5 protects against the development of allergic responses in offspring [51]. Fedolov et al. [52] demonstrated that treatment of the offspring from allergic mothers on postnatal day 4 with CpG oligonucleotides, a TLR9 agonist and Th1-type stimulant [53], protected the offspring from the development of allergic responses to suboptimal OVA using the model in Fig. 1a, b. Therefore, exposure of mothers, allergic mothers, or offspring from allergic mothers to Th1 stimuli inhibited the offspring response to allergen challenge.
Maternal Vitamins Regulate Offspring Allergic Responses
The prevalence of allergies has increased in just a few decades [4–6], suggesting that environmental factors likely impact allergies and asthma. Environmental factors that regulate allergy and asthma in the mother could then affect the risk of development of allergy and asthma in offspring. Exposure to environmental factors, such as chemical irritants or nutrients, during pregnancy has been associated with allergic disease in offspring [54, 55]. The data for vitamin D association with asthma and allergy is controversial in adults [56, 57] and in offspring [55–60]. Supplementation with higher levels of vitamin D during pregnancy or in cord blood has been associated with both a higher risk of allergy and with a lower risk of allergy in early infancy, but adequate vitamin D levels during pregnancy support fetal maturation [56, 57]. An environmental change over the past 40 years, which may contribute to elevating allergic responses, has been an increase in the d-γ-tocopherol isoform of vitamin E in the diet and in infant formulas [61–65].
Most clinical studies on vitamin E include mixed forms of natural and synthetic tocopherols from supplementation or diet. Vitamin E consists of eight natural isomers, d-α-tocopherol; d-β-tocopherol; d-γ-tocopherol; d-δ-tocopherol; and d-α-, d-β-, d-γ-, and d-δ-tocotrienol. In addition, there are synthetic racemic forms of tocopherols. Of these forms, the two most abundant natural forms are d-α-tocopherol and d-γ-tocopherol. Plants synthesize the natural isoforms from tyrosine and chlorophyll [66]. Then, these tocols are consumed in the diet from plant lipids. Mammals do not interconvert the tocopherol isoforms. In the liver, d-α-tocopherol is preferentially transferred to lipoproteins by the liver α-tocopherol transfer protein, resulting in 10-fold higher tissue concentrations of α-tocopherol than γ-tocopherol [67–71]. In mechanistic studies, we demonstrated that α-tocopherol is an antagonist and γ-tocopherol is an agonist of endothelial cell PKCα during signals that mediate eosinophil recruitment [72]. In a mouse model of adult allergic lung inflammation to OVA that is characterized by high eosinophils and low neutrophils, we demonstrated that α-tocopherol and γ-tocopherol have opposing regulatory functions during inflammation [64, 65, 73]. Briefly, supplementing with γ-tocopherol elevated allergic responses in adult mice [65, 74]. Moreover, even at the 10-fold lower concentrations of γ-tocopherol than α-tocopherol, γ-tocopherol opposed the anti-inflammatory benefit of α-tocopherol in adult mouse allergic responses [65, 74]. The opposing functions of these two tocopherol isoforms have implications on interpretation of studies with mixed tocopherols as discussed in other reviews [57, 64, 75, 76]. Importantly, tocopherol isoform regulation of maternal allergy may influence the risk for development of allergy in offspring.
Consistent with animal models demonstrating opposing functions of α-tocopherol and γ-tocopherol with allergic inflammation and airway responsiveness, we reported that in a study with 4500 adult participants, increasing plasma concentrations of α-tocopherol associate with better lung function and increasing plasma concentrations of γ-tocopherol associate with lower lung function [77•]. Interestingly, countries with higher plasma levels of γ-tocopherol tend to have the highest prevalence rate of asthma [65, 78–83]. In the USA, the average plasma γ-tocopherol levels are two to five times higher than those of European and Asian countries whereas the average plasma α-tocopherol levels are about the same among these countries [83]. The plasma γ-tocopherol levels are high in the USA where the diet is rich in γ-tocopherol found in soy oil, corn oil, and canola oil [61–65]. In contrast, γ-tocopherol is low in olive oil and sunflower oil used in European countries [65, 83, 84]. The differences in outcomes from clinical reports on vitamin E and asthma in Europe and the USA may, in part, reflect the opposing functions of α-tocopherol and γ-tocopherol.
Tocopherol isoforms may influence development of allergies early in life. We demonstrated in a 20-year prospective study in the USA that by age 21, human plasma α-tocopherol associates with better lung spirometry and human plasma γ-tocopherol associates with worse lung spirometry [77•]. This suggests that during human development prior to age 21, tocopherols may have regulatory functions on responsiveness to allergen. It is reported by Allan et al. [55] that low maternal α-tocopherol associates with increased risk for doctor-diagnosed asthma in first 10 years of life [55]. Thus, the balance of α-tocopherol and γ-tocopherol in women regulates adult allergic responses [77•] and the balance of tocopherol isoforms in pregnant females may influence the development of risk of allergies in her children.
In mice, α-tocopherol supplementation of allergic female mice during pregnancy/lactation decreased neonate development of allergic lung inflammation in response to suboptimal allergen challenge (Fig. 1e) [35•]. In these studies, allergic responses to OVA were induced in adult female mice and then the females were mated while receiving α-tocopherol-supplemented diets (250 mg α-tocopherol/kg diet) or a basal α-tocopherol diet (45 mg α-tocopherol/kg diet) [35•]. A basal α-tocopherol diet is used as the control because adequate α-tocopherol levels are required for placental development [85, 86]. Then, the 3-day-old neonates received a suboptimal allergen sensitization with OVA/alum and OVA challenge on days 10–12 [35•]. α-Tocopherol is loaded in the liver onto lipoproteins that then enter circulation for delivery to peripheral tissues. The α-tocopherol-supplemented diet significantly increased liver α-tocopherol in the saline-treated mothers threefold as compared to basal diet controls The OVA treatment reduced the α-tocopherol tissue concentrations in the α-tocopherol-supplemented mothers, which is consistent with reduced α-tocopherol levels in asthmatics [87–90], suggesting that α-tocopherol supplementation may be especially necessary for asthmatic mothers. Maternal α-tocopherol supplementation increased pup liver α-tocopherol 2.5-fold [35•]. This α-tocopherol supplementation of allergic mothers during pregnancy/lactation resulted in a dose-dependent inhibition of lung eosinophils [35•] in the OVA-stimulated pups from allergic mothers as compared to OVA-challenged pups from non-allergic mothers (Fig. 1e) [35•]. There was no effect of treatments on pup weight, pup numbers, or pup gender distribution [35•]. OVA-treated pups from allergic mothers had increased serum IgE, but α-tocopherol supplementation did not alter the IgE [35•]. α-Tocopherol supplementation of allergic female mothers inhibited OVA-induced pup lung messenger RNA (mRNA) expression of cytokines that regulate allergic inflammation (IL-33 and IL-4) and chemokines for eosinophil recruitment (CCL11 and CCL24) [35•]. Therefore, α-tocopherol supplementation of allergic mothers inhibits allergic inflammation and cytokine/chemokine mediators of allergic inflammation in OVA-challenged pups from these allergic mothers. Studies are ongoing in our lab to determine mechanisms of γ-tocopherol regulation of maternal transfer of risk of allergy to offspring.
In studies to determine the regulatory effect of α-tocopherol in utero and in the milk, pups were cross-fostered at birth. Cross-fostering pups from allergic mothers with 250 mg α-tocopherol/kg diet to allergic mothers with basal diet (45 mg α-tocopherol/kg diet) indicated that α-tocopherol supplementation of the allergic mother during pregnancy was sufficient to inhibit the OVA-induced increase in neonate lung eosinophils [35•]. In addition, α-tocopherol supplementation during lactation reduced the allergic responses in the neonates [35•], suggesting a contribution of α-tocopherol after birth [35•]. In summary, α-tocopherol supplementation of allergic mothers during pregnancy was sufficient to reduce the development of allergic responses in the offspring.
α-Tocopherol supplementation starting at conception of a second pregnancy of allergic female mice also inhibits development of allergic lung inflammation in offspring. The offspring from allergic mothers that were supplemented with α-tocopherol at the time of the second mating had a >90 % inhibition of lung lavage eosinophils in the OVA-challenged pups [35•]. Moreover, in OVA-challenged pups from allergic mothers, α-tocopherol reduced lung mRNA expression of several mediators of allergic inflammation: the cytokines IL-4, IL-33, and TSLP and the chemokines CCL11 and CCL24 [35•]. This is consistent with α-tocopherol regulation of development of allergic inflammation. There were no effects of α-tocopherol on low levels of the Th1 cytokine IFNγ or the regulatory cytokine IL-10 [35•], indicating that α-tocopherol did not switch the response to OVA to a Th1 response.
It is reported that transfer of dendritic cells but not macrophages from pups from allergic mothers are sufficient for the development of the allergic responses in pups in response to suboptimal OVA challenge [37]. We reported that offspring from allergic mothers with a suboptimal OVA challenge have elevated numbers of distinct subsets of lung dendritic cells (CD11b+CD11c+ resident and alveolar dendritic cells) but there are no changes in numbers of CD11b−CD11c+ dendritic cells (plasmacytoid dendritic cells and CD103+ dendritic cells) in the pup lung [35•]. During development of gestational day 18 fetal livers of allergic mothers, there is an increase in dendritic cells of the phenotype of CD11b+CD11c+ resident dendritic cells [35•]. Therefore, there is an effect of maternal allergy on the development of dendritic cells in the fetus.
The increase in the numbers of dendritic cell subsets in offspring of allergic mothers is regulated by α-tocopherol. Maternal supplementation with α-tocopherol significantly reduces the OVA-stimulated pup lung numbers of CD11b+ subsets of CD11c+ dendritic cells, including resident dendritic cells, myeloid dendritic cells, and CD11b+ alveolar dendritic cells, without altering CD11b− subsets of CD11c+ dendritic cells, including plasmacytoid dendritic cells, CD103+ dendritic cells, CD11b− alveolar dendritic cells, and alveolar macrophages [35•]. Interestingly, α-tocopherol supplementation does not completely deplete CD11b+ dendritic cells, but instead, α-tocopherol supplementation of allergic mothers reduces the numbers of pup CD11b+ dendritic cells to the numbers of these dendritic cells in pups from non-allergic mothers [35•]. For all dendritic cell subsets, the mean fluorescence intensity (MFI) for MHCII, CD80, and CD86 was not different among the groups [35•]. In the fetus on gestational day 18, α-tocopherol supplementation of allergic mothers reduces the number of fetal liver CD11b+ subsets of CD11c+ dendritic cells, including those of the phenotype of myeloid dendritic cells and phenotype of resident DCs without altering MFI for MHCII, CD80, or CD86 [35•]. The fetal liver CD11b− subsets of CD11c+ dendritic cells are not altered by maternal supplementation of α-tocopherol [35•]. We also demonstrated a direct effect of tocopherols on bone marrow dendritic cell differentiation in vitro. Bone marrow from 10-day-old mouse neonates from non-allergic mothers with basal diet was incubated with GM-CSF for 8 days in vitro in the presence of α-tocopherol. In these cultures, α-tocopherol reduces the number of CD45+CD11b+CD11c+ dendritic cells and the number of cells with resident dendritic cell phenotype (CD45+CD11b+CD11c+Ly6c-MHC- dendritic cells) without affecting the percent of viable cells in the culture [35•], indicating that α-tocopherol regulates differentiation of bone marrow cells to dendritic cells. Whether the inhibition of offspring risk for allergic responsiveness by maternal supplementation with α-tocopherol is through regulation by a maternal transplacental mediator or by the offspring response to the maternal mediator is not known and is under investigation in our laboratory. These studies of tocopherol isoform regulation impacts our understanding of mechanisms of regulation of dendritic cells by environmental factors during the development of allergies, the design of clinical studies with tocopherol isforms, and, perhaps, risk for allergic disease in future generations.
Transplacental Mediators and Development of Allergic Disease
It is not known whether transplacental cytokines influence the maternal effect on the offspring development of allergic responses. Th2 cytokines (IL-4, IL-5, and IL-13) are elevated in the placenta but transplacental crossing of these cytokines has not been demonstrated [91–93]. It is reported that only 2 % of maternal GM-CSF crosses the human placenta in ex vivo perfusate studies [94]. Whether maternal GM-CSF increases risk of offspring for allergic responses is not known. Understanding mechanisms of maternal transfer of risk for allergy to offspring and mechanisms for regulation of this risk will have an impact on limiting the development of allergic disease early in life.
One endogenous transplacental maternal mediator in mice has been reported to be sufficient to induce the increased responsiveness in the offspring to suboptimal OVA challenge [95•]. This mediator is low-level maternal corticosterone [95•]. In adult mice and rats, OVA sensitization and challenge increases stress [96–101] and increases endogenous serum corticosterone [102, 103]. Moreover, it is reported that symptoms of stress/anxiety are commonly associated with allergy/asthma in adult mice and in humans [104–108]. In addition, it is reported that stress in adult 4-week-old mice exacerbates OVA-induced allergic responses and this stress-induced effect is blocked by pretreatment with a glucocorticoid receptor antagonist [103]. When maternal corticosterone is elevated during pregnancy, the maternal cortisol can cross the placenta and affect fetal cortisol levels [109, 110]. Others reported that maternal corticosterone crosses the placenta to the fetus and is a strong inducer of Th2 responses [111, 112]. Cortisol is also present in human breast milk [113] and has the potential to affect allergic responses in neonates. Consistent with the mechanistic studies in mouse models, in pregnant asthmatic women without treatment for asthma, a deficiency in the placenta of a cortisol-metabolizing enzyme 11 beta-hydroxysteroid dehydrogenase 2 leads to increased fetal cortisol and low birth weight which is predictive of lower lung function later in life [114, 115].
In mice, it has been demonstrated that subjecting pregnant female mice to stress increases endogenous corticosterone, increases offspring allergic responses to suboptimal allergen, and increases airway responsiveness after suboptimal allergen challenge [95•, 109]. Furthermore, glucocorticoid during pregnancy is sufficient for allergic responses in offspring because administration of a low dose of glucocorticoid to non-allergic mothers on day 15 of gestation increases off-spring allergic responsiveness to suboptimal allergen challenge [95•]. In addition, when these mothers are subjected to stress and treated during pregnancy with an inhibitor of endogenous corticosterone synthesis, there is a reduction in the allergic response by the offspring [95•]. Therefore, elevated corticosterone in allergic pregnant mice may be a mediator that is transferred from the mother to the fetus or in the breast milk to the neonate, resulting in enhanced responses of off-spring to suboptimal allergen challenge. This mechanism is consistent with the antigen-independent transfer of risk from mother to offspring [30, 34].
Conclusion
The development of allergic disease often begins in utero or early in life and environmental factors impact the development of risk for allergic disease. Animal models and clinical studies indicate that the development of increased risk for allergies in offspring of allergic mothers may occur in utero. In animal models, this occurs by in utero regulation of distinct dendritic cell subsets that are able to transfer risk to naïve offspring. One maternal factor transferred from allergic or Th2 stressed mothers to the fetus or transferred to the offspring in breast milk is low levels of corticosterone. The development of allergic responses and distinct dendritic cell subsets in offspring from allergic mothers is blocked by maternal supplementation with the α-tocopherol isoform of vitamin E. Understanding the epidemiology, biology, and regulation of asthma inception by environmental factors will lead to approaches to reduce the development of allergy and asthma. The marked differences in rates of disease across the world, changes over short periods, and changes with migrating populations mean that asthma and allergic diseases are not inevitable consequences of a genetic predisposition. This is important, as the ability to modify diet and lifestyle means that lower rates of these diseases can be attained without medications or sophisticated medical infrastructures and can be achieved worldwide.
Acknowledgments
Sources of Support This study was supported by National Institutes of Health Grant R01 AT004837 (J.M.C-M).
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest Dr. Cook-Mills has a patent pre-application, Compositions and Methods for the Treatment of Natal and Prenatal Conditions with Alpha-Tocopherol Pending.
Human and Animal Rights and Informed Consent This article does not contain any studies with human subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
- 1.Martinez FD. Genes, environments, development and asthma: a reappraisal. Eur Respir J. 2007;29:179–184. doi: 10.1183/09031936.00087906. [DOI] [PubMed] [Google Scholar]
- 2.Martinez FD, Vercelli D. Asthma. Lancet. 2013;382:1360–1372. doi: 10.1016/S0140-6736(13)61536-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bousquet J, Bousquet PJ, Godard P, Daures JP. The public health implications of asthma. Bull World Health Organ. 2005;83:548–554. [PMC free article] [PubMed] [Google Scholar]
- 4.Vollmer WM, Osborne ML, Buist AS. 20-year trends in the prevalence of asthma and chronic airflow obstruction in an HMO. Am J Respir Crit Care Med. 1998;157:1079–1084. doi: 10.1164/ajrccm.157.4.9704140. [DOI] [PubMed] [Google Scholar]
- 5.Friebele E. The attack of asthma. Environ Health Perspect. 1996;104:22–25. doi: 10.1289/ehp.9610422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Schayck CP, Smit HA. The prevalence of asthma in children: a reversing trend. Eur Respir J. 2005;26:647–650. doi: 10.1183/09031936.05.00019805. [DOI] [PubMed] [Google Scholar]
- 7.Lim RH, Kobzik L. Maternal transmission of asthma risk. Am J Reprod Immunol. 2009;61:1–10. doi: 10.1111/j.1600-0897.2008.00671.x. [DOI] [PubMed] [Google Scholar]
- 8.Hamada K, et al. Allergen-independent maternal transmission of asthma susceptibility. J Immunol. 2003;170:1683–1689. doi: 10.4049/jimmunol.170.4.1683. [DOI] [PubMed] [Google Scholar]
- 9.Fedulov AV, Leme AS, Kobzik L. Duration of allergic susceptibility in maternal transmission of asthma risk. Am J Reprod Immunol. 2007;58:120–128. doi: 10.1111/j.1600-0897.2007.00496.x. [DOI] [PubMed] [Google Scholar]
- 10.Hubeau C, Apostolou I, Kobzik L. Targeting of CD25 and glucocorticoid-induced TNF receptor family-related gene-expressing T cells differentially modulates asthma risk in offspring of asthmatic and normal mother mice. J Immunol. 2007;178:1477–1487. doi: 10.4049/jimmunol.178.3.1477. [DOI] [PubMed] [Google Scholar]
- 11.Hubeau C, Apostolou I, Kobzik L. Adoptively transferred allergen-specific T cells cause maternal transmission of asthma risk. Am J Pathol. 2006;168:1931–1939. doi: 10.2353/ajpath.2006.051231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herz U, et al. Allergic sensitization and allergen exposure during pregnancy favor the development of atopy in the neonate. Int Arch Allergy Immunol. 2001;124:193–196. doi: 10.1159/000053708. [DOI] [PubMed] [Google Scholar]
- 13.Herz U, et al. Prenatal sensitization in a mouse model. Am J Respir Crit Care Med. 2000;162:S62–S65. doi: 10.1164/ajrccm.162.supplement_2.ras-1. [DOI] [PubMed] [Google Scholar]
- 14.Jarrett E, Hall E. Selective suppression of IgE antibody responsiveness by maternal influence. Nature. 1979;280:145–147. doi: 10.1038/280145a0. [DOI] [PubMed] [Google Scholar]
- 15.Wark PA, Murphy V, Mattes J. The interaction between mother and fetus and the development of allergic asthma. Expert Rev Respir Med. 2014;8:57–66. doi: 10.1586/17476348.2014.848795. [DOI] [PubMed] [Google Scholar]
- 16.Blumer N, Herz U, Wegmann M, Renz H. Prenatal lipopolysaccharide-exposure prevents allergic sensitization and airway inflammation, but not airway responsiveness in a murine model of experimental asthma. Clin Exp Allergy. 2005;35:397–402. doi: 10.1111/j.1365-2222.2005.02184.x. [DOI] [PubMed] [Google Scholar]
- 17.Devereux G, Barker RN, Seaton A. Antenatal determinants of neonatal immune responses to allergens. Clin Exp Allergy. 2002;32:43–50. doi: 10.1046/j.0022-0477.2001.01267.x. [DOI] [PubMed] [Google Scholar]
- 18.Uthoff H, et al. Critical role of preconceptional immunization for protective and nonpathological specific immunity in murine neonates. J Immunol. 2003;171:3485–3492. doi: 10.4049/jimmunol.171.7.3485. [DOI] [PubMed] [Google Scholar]
- 19.Kurukulaaratchy RJ, Waterhouse L, Matthews SM, Arshad SH. Are influences during pregnancy associated with wheezing phenotypes during the first decade of life? Acta Paediatr. 2005;94:553–558. doi: 10.1111/j.1651-2227.2005.tb01938.x. [DOI] [PubMed] [Google Scholar]
- 20.Celedon JC, et al. Exposure to cat allergen, maternal history of asthma, and wheezing in first 5 years of life. Lancet. 2002;360:781–782. doi: 10.1016/S0140-6736(02)09906-3. [DOI] [PubMed] [Google Scholar]
- 21.Kurukulaaratchy RJ, Matthews S, Waterhouse L, Arshad SH. Factors influencing symptom expression in children with bronchial hyperresponsiveness at 10 years of age. J Allergy Clin Immunol. 2003;112:311–316. doi: 10.1067/mai.2003.1623. [DOI] [PubMed] [Google Scholar]
- 22.Latzin P, et al. Prospectively assessed incidence, severity, and determinants of respiratory symptoms in the first year of life. Pediatr Pulmonol. 2007;42:41–50. doi: 10.1002/ppul.20542. [DOI] [PubMed] [Google Scholar]
- 23.Martinez FD, et al. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 1995;332:133–138. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 24.Litonjua AA, Carey VJ, Burge HA, Weiss ST, Gold DR. Parental history and the risk for childhood asthma. Does mother confer more risk than father? Am J Respir Crit Care Med. 1998;158:176–181. doi: 10.1164/ajrccm.158.1.9710014. [DOI] [PubMed] [Google Scholar]
- 25.Lim RH, Kobzik L, Dahl M. Risk for asthma in offspring of asthmatic mothers versus fathers: a meta-analysis. PLoS One. 2010;5:e10134. doi: 10.1371/journal.pone.0010134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Folsgaard NV, et al. Neonatal cytokine profile in the airway mucosal lining fluid is skewed by maternal atopy. Am J Respir Crit Care Med. 2012;185:275–280. doi: 10.1164/rccm.201108-1471OC. [DOI] [PubMed] [Google Scholar]
- 27.Bousquet J, et al. MeDALL (Mechanisms of the Development of ALLergy): an integrated approach from phenotypes to systems medicine. Allergy. 2011;66:596–604. doi: 10.1111/j.1398-9995.2010.02534.x. [DOI] [PubMed] [Google Scholar]
- 28.Sonnenschein-van der Voort AM, et al. Influence of maternal and cord blood C-reactive protein on childhood respiratory symptoms and eczema. Pediatr Allergy Immunol. 2013;24:469–475. doi: 10.1111/pai.12094. [DOI] [PubMed] [Google Scholar]
- 29.Giwercman C, et al. Increased risk of eczema but reduced risk of early wheezy disorder from exclusive breast-feeding in high-risk infants. J Allergy Clin Immunol. 2010;125:866–871. doi: 10.1016/j.jaci.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 30.Hamada K, et al. Allergen-independent maternal transmission of asthma susceptibility. J Immunol. 2003;170:1683–1689. doi: 10.4049/jimmunol.170.4.1683. [DOI] [PubMed] [Google Scholar]
- 31.Lim RH, Kobzik L. Transplacental passage of interleukins 4 and 13? PLoS One. 2009;4:e4660. doi: 10.1371/journal.pone.0004660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leme AS, et al. Role of breast milk in a mouse model of maternal transmission of asthma susceptibility. J Immunol. 2006;176:762–769. doi: 10.4049/jimmunol.176.2.762. [DOI] [PubMed] [Google Scholar]
- 33.Hsu P, Nanan R. Foetal immune programming: hormones, cytokines, microbes and regulatory T cells. J Reprod Immunol. 2014;104–105:2–7. doi: 10.1016/j.jri.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 34.Barrett EG, Rudolph K, Bowen LE, Bice DE. Parental allergic status influences the risk of developing allergic sensitization and an asthmatic-like phenotype in canine offspring. Immunology. 2003;110:493–500. doi: 10.1111/j.1365-2567.2003.01757.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Abdala-Valencia H, Berdnikovs S, Soveg F, Cook-Mills JM. Alpha-tocopherol supplementation of allergic female mice inhibits development of CD11c+CD11b+ dendritic cells in utero and allergic inflammation in neonates. Am J Physiol Lung Cell Mol Physiol. 2014;307:L482–L496. doi: 10.1152/ajplung.00132.2014. In this report using a mouse model, it was demonstrated that offspring of allergic mothers have an increase in numbers of distinct subsets of dendritic cells. The increase in numbers of these dendritic cell subsets in the fetal liver and pup lung of offspring of allergic mothers was blocked by supplementation of the allergic mother at the time of pregnancy with the vitamin E isoform α-tocopherol. In addition, α-tocopherol directly regulated bone marrow differentiation of these dendritic cell subsets in vitro.
- 36.Lim RH, Arredouani MS, Fedulov A, Kobzik L, Hubeau C. Maternal allergic contact dermatitis causes increased asthma risk in offspring. Respir Res. 2007;8:56. doi: 10.1186/1465-9921-8-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fedulov AV, Kobzik L. Allergy risk is mediated by dendritic cells with congenital epigenetic changes. Am J Respir Cell Mol Biol. 2011;44:285–292. doi: 10.1165/rcmb.2009-0400OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Williams JW. Transcription factor IRF4 drives dendritic cells to promote Th2 differentiation. Nat Commun. 2013;4:2990. doi: 10.1038/ncomms3990. There are many subsets of dendritic cells in the lung. In this report, they demonstrated that lung IRF4+ dendritic cell subsets drive the Th2 response in mice.
- 39. Mikhaylova L, Zhang Y, Kobzik L, Fedulov AV. Link between epigenomic alterations and genome-wide aberrant transcriptional response to allergen in dendritic cells conveying maternal asthma risk. PLoS One. 2013;8:e70387. doi: 10.1371/journal.pone.0070387. The offspring of allergic mothers have an elevated risk of developing allergic responses in humans and animal models. This increased risk of developing allergic responses in offspring of allergic mothers is mediated by changes in offspring dendritic cells. In this report, they identified epigenomic changes in dendritic cells of offspring of allergic mice.
- 40.Stoney RM, et al. Maternal breast milk long-chain n-3 fatty acids are associated with increased risk of atopy in breastfed infants. Clin Exp Allergy. 2004;34:194–200. doi: 10.1111/j.1365-2222.2004.01852.x. [DOI] [PubMed] [Google Scholar]
- 41.Reichardt P, et al. Fatty acids in colostrum from mothers of children at high risk of atopy in relation to clinical and laboratory signs of allergy in the first year of life. Allergy. 2004;59:394–400. doi: 10.1111/j.1398-9995.2003.00429.x. [DOI] [PubMed] [Google Scholar]
- 42.Miyake Y, Okubo H, Sasaki S, Tanaka K, Hirota Y. Maternal dietary patterns during pregnancy and risk of wheeze and eczema in Japanese infants aged 16–24 months: the Osaka Maternal and Child Health Study. Pediatr Allergy Immunol. 2011;22:734–741. doi: 10.1111/j.1399-3038.2011.01176.x. [DOI] [PubMed] [Google Scholar]
- 43.Verhasselt V, et al. Breast milk-mediated transfer of an antigen induces tolerance and protection from allergic asthma. Nat Med. 2008;14:170–175. doi: 10.1038/nm1718. [DOI] [PubMed] [Google Scholar]
- 44.Mosconi E, et al. Breast milk immune complexes are potent inducers of oral tolerance in neonates and prevent asthma development. Mucosal Immunol. 2010;3:461–474. doi: 10.1038/mi.2010.23. [DOI] [PubMed] [Google Scholar]
- 45.Muniz BP, et al. Tolerogenic microenvironment in neonatal period induced by maternal immunization with ovalbumin. Immunobiology. 2014;219:377–384. doi: 10.1016/j.imbio.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 46.Fedulov AV, et al. Pulmonary exposure to particles during pregnancy causes increased neonatal asthma susceptibility. Am J Respir Cell Mol Biol. 2008;38:57–67. doi: 10.1165/rcmb.2007-0124OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gerhold K, et al. Prenatal initiation of endotoxin airway exposure prevents subsequent allergen-induced sensitization and airway inflammation in mice. J Allergy Clin Immunol. 2006;118:666–673. doi: 10.1016/j.jaci.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 48.Gerhold K, Bluemchen K, Franke A, Stock P, Hamelmann E. Exposure to endotoxin and allergen in early life and its effect on allergen sensitization in mice. J Allergy Clin Immunol. 2003;112:389–396. doi: 10.1067/mai.2003.1646. [DOI] [PubMed] [Google Scholar]
- 49.Tulic MK, Knight DA, Holt PG, Sly PD. Lipopolysaccharide inhibits the late-phase response to allergen by altering nitric oxide synthase activity and interleukin-10. Am J Respir Cell Mol Biol. 2001;24:640–646. doi: 10.1165/ajrcmb.24.5.4265. [DOI] [PubMed] [Google Scholar]
- 50.Gerhold K, et al. Endotoxins prevent murine IgE production, T(H)2 immune responses, and development of airway eosinophilia but not airway hyperreactivity. J Allergy Clin Immunol. 2002;110:110–116. doi: 10.1067/mai.2002.125831. [DOI] [PubMed] [Google Scholar]
- 51.Lima C, et al. Modulation of the induction of lung and airway allergy in the offspring of IFN-gamma-treated mother mice. J Immunol. 2005;175:3554–3559. doi: 10.4049/jimmunol.175.6.3554. [DOI] [PubMed] [Google Scholar]
- 52.Fedulov A, Silverman E, Xiang Y, Leme A, Kobzik L. Immunostimulatory CpG oligonucleotides abrogate allergic susceptibility in a murine model of maternal asthma transmission. J Immunol. 2005;175:4292–4300. doi: 10.4049/jimmunol.175.7.4292. [DOI] [PubMed] [Google Scholar]
- 53.de Brito CA, et al. CpG-induced Th1-type response in the downmodulation of early development of allergy and inhibition of B7 expression on T cells of newborn mice. J Clin Immunol. 2010;30:280–291. doi: 10.1007/s10875-009-9358-9. [DOI] [PubMed] [Google Scholar]
- 54.Netting MJ, Middleton PF, Makrides M. Does maternal diet during pregnancy and lactation affect outcomes in offspring? A systematic review of food-based approaches Nutrition. 2014;30:1225–1241. doi: 10.1016/j.nut.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 55.Allan KM, et al. Maternal vitamin D and E intakes during pregnancy are associated with asthma in children. Eur Respir J. 2014;30:erj01022–erj02014. doi: 10.1183/09031936.00102214. [DOI] [PubMed] [Google Scholar]
- 56.Junge KM, Lehmann I, Borte M. Can vitamin D intake during pregnancy affect the risk of allergy in children? Expert Rev Clin Immunol. 2013;9:699–701. doi: 10.1586/1744666X.2013.816481. [DOI] [PubMed] [Google Scholar]
- 57.Cook-Mills JM, Avila PC. Vitamin E and D regulation of allergic asthma immunopathogenesis. Int Immunopharmacol. 2014;29:007. doi: 10.1016/j.intimp.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Camargo CA, Jr, et al. Maternal intake of vitamin D during pregnancy and risk of recurrent wheeze in children at 3 y of age. Am J Clin Nutr. 2007;85:788–795. doi: 10.1093/ajcn/85.3.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Beigelman A, et al. The association between vitamin D status and the rate of exacerbations requiring oral corticosteroids in preschool children with recurrent wheezing. J Allergy Clin Immunol. 2014;133:1489–1492. doi: 10.1016/j.jaci.2014.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chawes BL, et al. Cord blood 25(OH)-vitamin D deficiency and childhood asthma, allergy and eczema: the COPSAC2000 birth cohort study. PLoS One. 2014;9:e99856. doi: 10.1371/journal.pone.0099856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Uauy R, et al. Safety and efficacy of omega-3 fatty acids in the nutrition of very low birth weight infants: soy oil and marine oil supplementation of formula. J Pediatr. 1994;124:612–620. doi: 10.1016/s0022-3476(05)83144-0. [DOI] [PubMed] [Google Scholar]
- 62.Boyle FG, Yuhas RJ, Lien EL. Red blood cell and tissue phospholipid fatty acid profiles of weanling rats fed infant formula fat blends containing soy and/or corn oil. Ann Nutr Metab. 1996;40:234–242. doi: 10.1159/000177927. [DOI] [PubMed] [Google Scholar]
- 63.Nelson SE, Rogers RR, Frantz JA, Ziegler EE. Palm olein in infant formula: absorption of fat and minerals by normal infants. Am J Clin Nutr. 1996;64:291–296. doi: 10.1093/ajcn/64.3.291. [DOI] [PubMed] [Google Scholar]
- 64.Cook-Mills JM, McCary CA. Isoforms of vitamin E differentially regulate inflammation. Endocr Metab Immune Disord Drug Targets. 2010;10:348–366. doi: 10.2174/1871530311006040348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Berdnikovs S, et al. Isoforms of vitamin E have opposing immunoregulatory functions during inflammation by regulating leukocyte recruitment. J Immunol. 2009;182:4395–4405. doi: 10.4049/jimmunol.0803659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hunter SC, Cahoon EB. Enhancing vitamin E in oilseeds: unraveling tocopherol and tocotrienol biosynthesis. Lipids. 2007;42:97–108. doi: 10.1007/s11745-007-3028-6. [DOI] [PubMed] [Google Scholar]
- 67.Wolf G. How an increased intake of alpha-tocopherol can suppress the bioavailability of gamma-tocopherol. Nutr Rev. 2006;64:295–299. doi: 10.1111/j.1753-4887.2006.tb00213.x. [DOI] [PubMed] [Google Scholar]
- 68.Leonard SW, Terasawa Y, Farese RV, Jr, Traber MG. Incorporation of deuterated RRR- or all-rac-alpha-tocopherol in plasma and tissues of alpha-tocopherol transfer protein-null mice. Am J Clin Nutr. 2002;75:555–560. doi: 10.1093/ajcn/75.3.555. [DOI] [PubMed] [Google Scholar]
- 69.Brigelius-Flohe R, Traber MG. Vitamin E: function and metabolism. FASEB J. 1999;13:1145–1155. [PubMed] [Google Scholar]
- 70.Podda M, Weber C, Traber MG, Packer L. Simultaneous determination of tissue tocopherols, tocotrienols, ubiquinols, and ubiquinones. J Lipid Res. 1996;37:893–901. [PubMed] [Google Scholar]
- 71.Traber MG, Kayden HJ. Preferential incorporation of alpha-tocopherol vs gamma-tocopherol in human lipoproteins. Am J Clin Nutr. 1989;49:517–526. doi: 10.1093/ajcn/49.3.517. [DOI] [PubMed] [Google Scholar]
- 72.McCary CA, et al. Vitamin E isoforms directly bind PKCalpha and differentially regulate activation of PKCalpha. Biochem J. 2012;441:189–198. doi: 10.1042/BJ20111318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McCary CA, Abdala-Valencia H, Berdnikovs S, Cook-Mills JM. Supplemental and highly elevated tocopherol doses differentially regulate allergic inflammation: reversibility of alpha-tocopherol and gamma-tocopherol’s effects. J Immunol. 2011;186:3674–3685. doi: 10.4049/jimmunol.1003037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cook-Mills JM, Marchese M, Abdala-Valencia H. Vascular cell adhesion molecule-1 expression and signaling during disease: regulation by reactive oxygen species and antioxidants. Antioxid Redox Signal. 2011;15:1607–1638. doi: 10.1089/ars.2010.3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cook-Mills JM, Marchese ME, Abdala-Valencia H. Vascular cell adhesion molecule-1 expression and signaling during disease: regulation by reactive oxygen species and antioxidants. Antioxid Redox Signal. 2011;15:1607–1638. doi: 10.1089/ars.2010.3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cook-Mills JM. In: Eosinophils in health and disease. J J, Rosenberg Lee HF, editors. Elsevier; 2012. pp. 139–153. [Google Scholar]
- 77. Marchese ME. The vitamin E isoforms alpha-tocopherol and gamma-tocopherol have opposite associations with spirometric parameters: the CARDIA study. Respir Res. 2014;15:31. doi: 10.1186/1465-9921-15-31. The prevalence of allergies has increased in just a few decades suggesting that environmental factors likely impact allergies and asthma. In this report, it is demonstrated in a 20-year prospective study with 4500 individuals in the USA that, by age 21, human plasma α-tocopherol associates with better lung spirometry and human plasma γ-tocopherol associates with worse lung spirometry. Thus, the balance of α-tocopherol and γ-tocopherol regulates adult allergic responses. Regulation of allergies and asthma in women has the potential to influence the development of risk of allergies in her children.
- 78.Tabak C, et al. Dietary factors and pulmonary function: a cross sectional study in middle aged men from three European countries. Thorax. 1999;54:1021–1026. doi: 10.1136/thx.54.11.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Smit HA, Grievink L, Tabak C. Dietary influences on chronic obstructive lung disease and asthma: a review of the epidemiological evidence. Proc Nutr Soc. 1999;58:309–319. doi: 10.1017/s0029665199000427. [DOI] [PubMed] [Google Scholar]
- 80.Weiss ST. Diet as a risk factor for asthma. Ciba Fndn Symp. 1997;206:244–257. [PubMed] [Google Scholar]
- 81.Troisi RJ, et al. A prospective study of diet and adult-onset asthma. Am J Respir Crit Care Med. 1995;151:1401–1408. doi: 10.1164/ajrccm.151.5.7735592. [DOI] [PubMed] [Google Scholar]
- 82.Dow L, et al. Does dietary intake of vitamins C and E influence lung function in older people? Am J Respir Crit Care Med. 1996;154:1401–1404. doi: 10.1164/ajrccm.154.5.8912755. [DOI] [PubMed] [Google Scholar]
- 83.Wagner KH, Kamal-Eldin A, Elmadfa I. Gamma-tocopherol—an underestimated vitamin? Ann Nutr Metab. 2004;48:169–188. doi: 10.1159/000079555. [DOI] [PubMed] [Google Scholar]
- 84.Jiang Q, Christen S, Shigenaga MK, Ames BN. Gamma-tocopherol, the major form of vitamin E in the US diet, deserves more attention. Am J Clin Nutr. 2001;74:714–722. doi: 10.1093/ajcn/74.6.714. [DOI] [PubMed] [Google Scholar]
- 85.Muller-Schmehl K, et al. Localization of alpha-tocopherol transfer protein in trophoblast, fetal capillaries’ endothelium and amnion epithelium of human term placenta. Free Radic Res. 2004;38:413–420. doi: 10.1080/10715760310001659611. [DOI] [PubMed] [Google Scholar]
- 86.Jishage K, et al. Vitamin E is essential for mouse placentation but not for embryonic development itself. Biol Reprod. 2005;73:983–987. doi: 10.1095/biolreprod.105.043018. [DOI] [PubMed] [Google Scholar]
- 87.Kalayci O, Besler T, Kilinc K, Sekerel BE, Saraclar Y. Serum levels of antioxidant vitamins (alpha tocopherol, beta carotene, and ascorbic acid) in children with bronchial asthma. Turk J Peds. 2000;42:17–21. [PubMed] [Google Scholar]
- 88.Kelly FJ, Mudway I, Blomberg A, Frew A, Sandstrom T. Altered lung antioxidant status in patients with mild asthma. Lancet. 1999;354:482–483. doi: 10.1016/S0140-6736(99)01812-7. [DOI] [PubMed] [Google Scholar]
- 89.Shvedova AA, Kisin ER, Kagan VE, Karol MH. Increased lipid peroxidation and decreased antioxidants in lungs of guinea pigs following an allergic pulmonary response. Tox Appl Pharm. 1995;132:72–81. doi: 10.1006/taap.1995.1088. [DOI] [PubMed] [Google Scholar]
- 90.Schunemann HJ, et al. The relation of serum levels of antioxidant vitamins C and E, retinol and carotenoids with pulmonary function in the general population. Am J Respir Crit Care Med. 2001;163:1246–1255. doi: 10.1164/ajrccm.163.5.2007135. [DOI] [PubMed] [Google Scholar]
- 91.Zourbas S, Dubanchet S, Martal J, Chaouat G. Localization of pro-inflammatory (IL-12, IL-15) and anti-inflammatory (IL-11, IL-13) cytokines at the foetomaternal interface during murine pregnancy. Clin Exp Immunol. 2001;126:519–528. doi: 10.1046/j.1365-2249.2001.01607.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ostojic S, et al. Demonstration of the presence of IL-16, IL-17 and IL-18 at the murine fetomaternal interface during murine pregnancy. Am J Reprod Immunol. 2003;49:101–112. doi: 10.1034/j.1600-0897.2003.01150.x. [DOI] [PubMed] [Google Scholar]
- 93.Bowen JM, Chamley L, Mitchell MD, Keelan JA. Cytokines of the placenta and extra-placental membranes: biosynthesis, secretion and roles in establishment of pregnancy in women. Placenta. 2002;23:239–256. doi: 10.1053/plac.2001.0781. [DOI] [PubMed] [Google Scholar]
- 94.Gregor H, et al. The passage of granulocyte-macrophage colony-stimulating factor across the human placenta perfused in vitro. J Soc Gynecol Investig. 1999;6:307–310. doi: 10.1016/s1071-5576(99)00042-8. [DOI] [PubMed] [Google Scholar]
- 95. Lim R, Fedulov AV, Kobzik L. Maternal stress during pregnancy increases neonatal allergy susceptibility: role of glucocorticoids. Am J Physiol Lung Cell Mol Physiol. 2014;307:L141–L148. doi: 10.1152/ajplung.00250.2013. Maternal factors that are transferred from allergic mothers to offspring for the increased risk of allergy in the offspring were not known. In this report, they demonstrated in mice that maternal corticosterone is sufficient to increase the risk of allergic responses in offspring.
- 96.Costa-Pinto FA, Basso AS, Britto LR, Malucelli BE, Russo M. Avoidance behavior and neural correlates of allergen exposure in a murine model of asthma. Brain Behav Immun. 2005;19:52–60. doi: 10.1016/j.bbi.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 97.Costa-Pinto FA, et al. Neural correlates of IgE-mediated allergy. Ann N YAcad Sci. 2006;1088:116–131. doi: 10.1196/annals.1366.028. [DOI] [PubMed] [Google Scholar]
- 98.Portela Cde P, Massoco Cde O, de Lima WT, Palermo-Neto J. Stress-induced increment on total bronchoalveolar cell count in OVA-sensitized rats. Physiol Behav. 2001;72:415–420. doi: 10.1016/s0031-9384(00)00429-7. [DOI] [PubMed] [Google Scholar]
- 99.Portela CP, et al. Effects of stress and neuropeptides on airway responses in ovalbumin-sensitized rats. Neuroimmunomodulation. 2007;14:105–111. doi: 10.1159/000107765. [DOI] [PubMed] [Google Scholar]
- 100.Portela Cde P, Tiberio Ide F, Leick-Maldonado EA, Martins MA, Palermo-Neto J. Effects of diazepam and stress on lung inflammatory response in OVA-sensitized rats. Am J Physiol Lung Cell Mol Physiol. 2002;282:L1289–L1295. doi: 10.1152/ajplung.00352.2001. [DOI] [PubMed] [Google Scholar]
- 101.Tonelli LH, et al. Allergic rhinitis induces anxiety-like behavior and altered social interaction in rodents. Brain Behav Immun. 2009;23:784–793. doi: 10.1016/j.bbi.2009.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lu Y, et al. Effects of stress in early life on immune functions in rats with asthma and the effects of music therapy Early-life psychological stress exacerbates adult mouse asthma via the hypothalamus-pituitary-adrenal axis. J Asthma. 2010;47:526–531. doi: 10.3109/02770901003801964. [DOI] [PubMed] [Google Scholar]
- 103.Chida Y, Sudo N, Sonoda J, Hiramoto T, Kubo C. Early-life psychological stress exacerbates adult mouse asthma via the hypothalamus-pituitary-adrenal axis. Am J Respir Crit Care Med. 2007;175:316–322. doi: 10.1164/rccm.200607-898OC. [DOI] [PubMed] [Google Scholar]
- 104.Strine TW, et al. Depression and anxiety in the United States: findings from the 2006 Behavioral Risk Factor Surveillance System. Psychiatr Serv. 2008;59:1383–1390. doi: 10.1176/ps.2008.59.12.1383. [DOI] [PubMed] [Google Scholar]
- 105.Cheung TK, et al. Gastroesophageal reflux disease is associated with poor asthma control, quality of life, and psychological status in Chinese asthma patients. Chest. 2009;135:1181–1185. doi: 10.1378/chest.08-1702. [DOI] [PubMed] [Google Scholar]
- 106.Sansone RA, Sansone LA. Asthma: wheezing, woes, and worries. Psychiatry. 2008;5:48–52. [PMC free article] [PubMed] [Google Scholar]
- 107.Di Marco F, et al. Close correlation between anxiety, depression, and asthma control. Respir Med. 2010;104:22–28. doi: 10.1016/j.rmed.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 108.Cordina M, Fenech AG, Vassallo J, Cacciottolo JM. Anxiety and the management of asthma in an adult outpatient population. Ther Adv Respir Dis. 2009;3:227–233. doi: 10.1177/1753465809347038. [DOI] [PubMed] [Google Scholar]
- 109.von Hertzen LC. Maternal stress and T-cell differentiation of the developing immune system: possible implications for the development of asthma and atopy. J Allergy Clin Immunol. 2002;109:923–928. doi: 10.1067/mai.2002.124776. [DOI] [PubMed] [Google Scholar]
- 110.Huang CC, Shih MC, Hsu NC, Chien Y, Chung BC. Fetal glucocorticoid synthesis is required for development of fetal adrenal medulla and hypothalamus feedback suppression. Endocrinology. 2012;153:4749–4756. doi: 10.1210/en.2012-1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Norbiato G, Bevilacqua M, Vago T, Clerici M. Glucocorticoids and Th-1, Th-2 type cytokines in rheumatoid arthritis, osteoarthritis, asthma, atopic dermatitis and AIDS. Clin Exp Rheumatol. 1997;15:315–323. [PubMed] [Google Scholar]
- 112.Ramirez F, Fowell DJ, Puklavec M, Simmonds S, Mason D. Glucocorticoids promote a TH2 cytokine response by CD4+ T cells in vitro. J Immunol. 1996;156:2406–2412. [PubMed] [Google Scholar]
- 113.Groer MW, Humenick S, Hill PD. Characterizations and psychoneuroimmunologic implications of secretory immunoglobulin A and cortisol in preterm and term breast milk. J Perinat Neonatal Nurs. 1994;7:42–51. doi: 10.1097/00005237-199403000-00005. [DOI] [PubMed] [Google Scholar]
- 114.Murphy VE, et al. Reduced 11beta-hydroxysteroid dehydrogenase type 2 activity is associated with decreased birth weight centile in pregnancies complicated by asthma. J Clin Endocrinol Metab. 2002;87:1660–1668. doi: 10.1210/jcem.87.4.8377. [DOI] [PubMed] [Google Scholar]
- 115.Murphy VE, et al. Maternal asthma is associated with reduced female fetal growth. Am J Respir Crit Care Med. 2003;168:1317–1323. doi: 10.1164/rccm.200303-374OC. [DOI] [PubMed] [Google Scholar]