Abstract
Mechanical loading during childhood and adolescence may yield skeletal benefits that persist beyond activity cessation and menarche. At 1 year pre- and 2 years post-menarche, non-dominant forearm areal bone mineral density (aBMD), bone mineral content (BMC) and projected area (area) were compared in gymnasts (n=9), ex-gymnasts (n=8) and non-gymnasts (n=13). At both observations, gymnasts and ex-gymnasts had higher forearm aBMD, BMC and area than non-gymnasts. gymnasts had higher post-menarcheal means than ex-gymnasts for all three parameters. Childhood mechanical loading yields skeletal advantages that persist at least 24 months after loading cessation and menarche. Continued post-menarcheal loading yields additional benefit.
Introduction
Evidence suggests that mechanical loading is osteogenic during childhood and adolescence. If skeletal benefits persist after activity cessation, adult bone structure and strength may be improved. However, most evidence demonstrating adult skeletal benefit from childhood and adolescent activity is retrospective in nature. Gymnastic activity has been examined extensively as a model of mechanical loading (2, 7, 8, 11, 15, 17, 18, 21, 22, 23, 25). This extreme model provides an ideal tool to assess maintenance of skeletal benefits for many reasons. First, gymnastics incorporates impact loads of up to 15 times body weight (20). It is unlikely that other activities will yield lasting skeletal improvements if persistent skeletal benefits cannot be detected after gymnastic loading. Second, many girls cease gymnastic participation during puberty, supplying cohorts for assessment of benefit persistence following childhood activity. Finally, because gymnastic activity loads the upper extremity in a manner that is not duplicated by other activities, the non-dominant forearm serves as a unique barometer for skeletal responses to mechanical loading via gymnastic activity (8).
Our group and others have shown increased bone accrual in girls who participate in gymnastics during the critical peri-pubertal years (2, 7, 11, 18, 21, 22). Comparisons of adult former gymnasts vs. non-gymnasts demonstrate 5-22% aBMD advantages attributed to prior gymnastic participation (2, 15, 17). However, there are no prospective longitudinal analyses demonstrating preservation of skeletal benefits from childhood gymnastic activity. The present study was designed to link post-menarcheal bone properties with childhood mechanical loading activity, prospectively evaluating cohorts of gymnasts, ex-gymnasts and non-gymnasts over a three-year circum-menarcheal period. For females, menarche is pivotal in bone accrual, with approximately half of adult bone mass acquired in four circum-menarcheal years (1, 4, 24). Using the non-dominant forearm as a model of gymnastic loading, we examined a subset of our cohort to evaluate whether mechanical loading during childhood and adolescence yields skeletal benefits that persist after activity cessation and beyond menarche.
Materials and Methods
The subjects of these analyses are a subset of a larger cohort (n=70) who were enrolled in an ongoing longitudinal study (25). Gymnasts and non-gymnasts were recruited from the local community and were matched for age and body size at enrollment. For the present analysis, in order to target the phase of peak bone accrual velocity, and to assure assessment across the same maturational phase, evaluation was limited to three peri-menarcheal years. Thus, only subjects who underwent two peri-menarcheal DXA scans, separated by an interval of approximately 36 months, are included, with one pre-menarcheal scan (approximately one year pre-menarche) and one post-menarcheal scan (approximately two years post-menarche). Subjects were classified as gymnasts (gym) if they participated in gymnastics over the two years prior to the first DXA scan and continued gymnastic participation until within two months of the post-menarcheal scan. ex-gymnasts (ex) were subjects who quit gymnastics prior to menarche and at least two years prior to the post-menarcheal DXA scan; they had participated in gymnastics over the two years prior to the pre-menarcheal scan. non-gymnasts (non) were subjects who had not participated in gymnastics for at least 3 years prior to the first DXA scan, or at any point thereafter. Subjects were not included unless they met these criteria for observation timing and gymnastic participation.
Subjects and their parents/guardians provided informed assent and consent using a document approved by the Institutional Review Board of our University, which also approved the study protocols. Areal bone mineral density (aBMD, g/cm2) and bone mineral content (BMC, g) of the distal third of the non-dominant forearm were assessed pre- and post-menarche using a Hologic QDR 4500W DXA scanner (Hologic Inc., Bedford, MA) and a standardized protocol. The coefficient of variation for this machine is 1% for both total body and forearm scans. Whole body scans yielded total body non-bone, fat free mass (FFM) and percentage of body mass as fat (%BF) (Hologic software, version 9.03D).
As previously described, subjects completed questionnaires to assess calcium intake and menarcheal status on a semi-annual basis (25). Mean calcium intake was calculated from semi-quantitative food frequency questionnaires for the one-year period prior to the first DXA scan and the three-year period between the first and second scans; these means were assessed as potential covariates of bone parameters. Gynecological age was computed as months since achievement of menarche. Standing height was measured semi-annually using wall-mounted rulers.
Weekly hours of gymnastics and other physical activities were recorded semi-annually by interview; this instrument has been validated in our gymnasts, comparing the questionnaire against coaching staff logs, with correlations ranging from R=0.93 for 1-month to R=0.97 for 12-month comparisons of mean hrs/wk (p<0.0001, unpublished data). These reports were used to generate annual means for hours per week (h/wk) of participation in organized physical activities. Gymnastic activity alone was quantified for gym, and for ex (prior to cessation of gymnastics), as this was the primary independent variable. For non, all organized physical activities were quantified; similarly, after cessation of gymnastic training all organized physical activities were quantified for ex. Means excluded aquatic activities, as this non-impact, non-weight-bearing activity is not considered to be osteogenic. Two annual means were computed: one for the year prior to the pre-menarcheal scan and one for the year preceding the post-menarcheal scan. For each subject, the difference between these means was calculated to yield an index of change in physical activity, with a positive value indicating an increase in activity and a negative value indicating a decrease in activity.
Statistical Analyses
All variables were screened for normality; as no significant skewness or kurtosis was observed for any variable distribution, ANOVA, ANCOVA and Pearson correlations were used in analyses. Between-group differences in all independent variables (height, FFM, calcium intake, gynecological age, etc.) were compared (ANOVA); results are reported as means and standard deviations with the significance level set at p<0.05. Activity group differences in bone outcomes (forearm aBMD, BMC and projected area) were assessed using repeated measures ANOVA. Due to the known positive influence of physical maturity and body size on skeletal properties, post-menarcheal gynecological age and height were included as covariates. Correlations screened calcium intake as a potential covariate of bone outcomes.
Adjusted means were compared for gym, ex and non, evaluating loading effects for: the pre-menarcheal scan; the post-menarcheal scan; and group-specific circum-menarcheal rate of change (group x time interaction term). Adjusted means and standard errors are presented graphically (Figures 2-4). For this preliminary analysis of a subset of our cohort, we report effect sizes rather than significance levels (Cohen's “d”, where 0.15 = small effect, 0.40 = medium effect, 0.75 = large effect). This procedure indicates likelihood of a “meaningful” difference between groups, while preserving the experimental alpha risk for the final analysis (5). Large effects are likely to indicate meaningful differences, whereas small or negligible effects are unlikely to signify meaningful group differences of clinical importance.
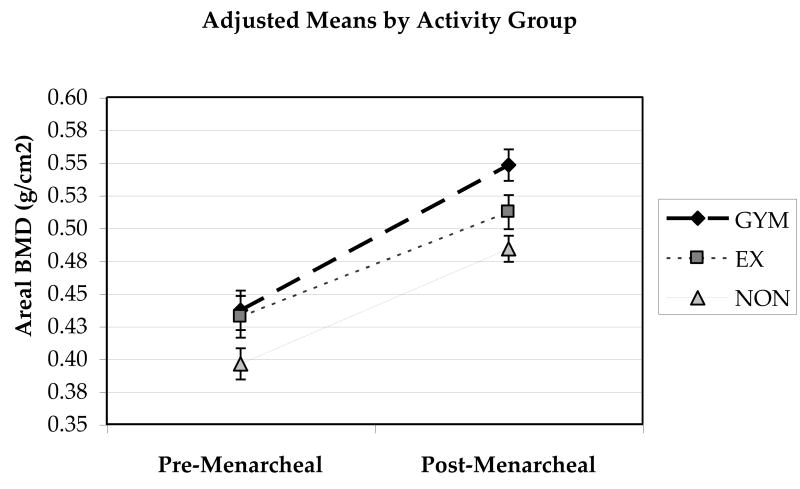
Figure 2.
Forearm areal BMD (g/cm2) is depicted for gym, ex and non groups. Pre- and post-menarcheal group means and standard errors are adjusted for gynecological age and height.
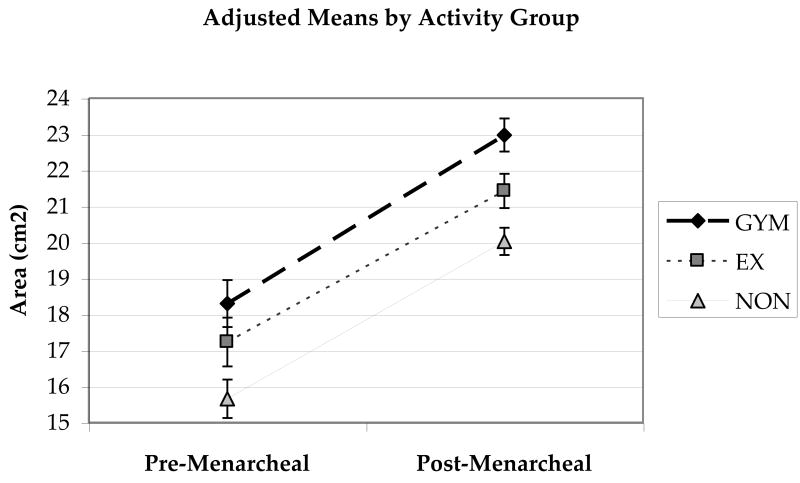
Figure 4.
Forearm projected area (cm2) is depicted for gym, ex and non groups. Pre- and post-menarcheal group means and standard errors are adjusted for gynecological age and height.
Results
Subjects included 9 gym, 8 ex, and 13 non. Subject characteristics are presented in Table 1. Age at menarche was similar in the three groups (non= 12.7 ± 0.9 yrs; ex= 13.0 ± 0.8 yrs; gym= 13.2 ± 0.9 yrs, NS). The interval between observations was 37.6 ± 1.9 mos (range 32.7-41.1 mos) and was similar in the three groups (p=0.11). The majority of ex-gymnasts (88%) continued to participate in gymnastics for variable intervals after the pre-menarcheal scan, but did not participate in gymnastics after menarche (mean gynecological age at cessation −6.3 ± 6.0 mos, range −20.4 to −0.5 mos). On average, ex-gymnasts received their post-menarcheal scan 30.0 ± 6.8 mos after cessation of gymnastics (range 24.7 to 45.3 mos). No subjects reported oligomenorrhea or amenorrhea, although some reported variability in cycle length consistent with early post-menarcheal development (non= 4, ex=1, gym= 2). All subjects denied the use of oral contraceptives or other modifiers/regulators of reproductive hormones throughout the course of the study.
Table 1. Subject Characteristics and Bone Outcomes by Activity Group.
| Variable | (units) | Non-Gymnasts (n=13) | Ex-Gymnasts (n=8) | Gymnasts (n=9) | |
|---|---|---|---|---|---|
| Pre-menarcheal | Age | (years) | 11.6 ± 1.0 | 11.8 ± 0.7 | 12.0 ± 0.9 |
| Gynecological Age | (months) | -13.8 ± 2.6 | -15.0 ± 4.2 | -15.2 ± 3.1 | |
| Height | (cm) | 149.6 ± 6.6 | 146.2 ± 6.9 | 145.8 ± 6.0 | |
| FFM | (kg) | 28.9 ± 3.5 | 27.4 ± 5.1 | 30.0 ± 4.8 | |
| Body Fat | (%) | 22.7 ± 6.6 | 20.6 ± 3.7 | 18.1 ± 4.8 | |
| Calcium intake, 1yr | (mg/day) | 919.8 ± 434.4 | 994.0 ± 394.0 | 1063.6 ± 463.8 | |
| Organized Activity | (hrs/wk) ¥ | 3.2 ± 3.4 | 10.4 ± 2.4 (gym) B | 15.1 ± 6.8 (gym) AB | |
| Age started gym | (yrs) | - | 7.5 ± 1.8 | 5.9 ± 1.8 | |
| Post-Menarcheal | Age | (years) | 14.7 ± 1.1 | 15.1 ± 0.7 | 15.1 ± 0.9 |
| Gynecologic Age | (months) | 23.4 ± 3.6 | 23.8 ± 3.5 | 22.1 ± 3.9 | |
| Height | (cm) | 162.3 ± 5.0 | 161.7 ± 6.7 | 159.0 ± 6.6 | |
| FFM | (kg) | 37.9 ± 2.0 | 38.2 ± 3.5 | 40.8 ± 3.3 | |
| Body Fat | (%) ¥ | 23.2 ± 4.1 | 25.1 ± 3.9 | 20.0 ± 3.2 A | |
| Calcium intake, 3 yr | (mg/day) | 760.5 ± 392.8 | 986.2 ± 343.4 | 1033.2 ± 369.3 | |
| Organized Activity | (hrs/wk) ¥ | 6.0 ± 3.0 | 5.3 ± 3.1 | 15.2 ± 6.5 (gym) AB |
Means and standard deviations for subject characteristics and unadjusted bone outcomes are presented for each activity group; FFM = total body, non-bone fat-free mass
denotes significant differences between groups by ANOVA (p<0.05)
indicates significantly different mean vs. Ex-gymnasts
indicates significantly different mean vs. Non-gymnasts
For all groups, physical activity exposure was carefully assessed for the year prior to both pre-menarcheal and post-menarcheal scans. At the time of the pre-menarcheal scan, active gymnasts (includes both gym and ex groups) averaged 12.9 ± 5.6 h/wk of gymnastic activity over the preceding year (range=4.0 to 23.0 h/wk). Mean h/wk for the ex group was lower than for the gym group (p<0.05, see Table 1). At the post-menarcheal observation, active gymnasts (gym group only) averaged 15.2 ± 6.5 h/wk of gymnastic activity over the preceding year (range 6.8-22.6 h/wk), and 12.9 ± 5.6 h/wk (range 4.7- 20.6 h/wk), on average, over the preceding three years.
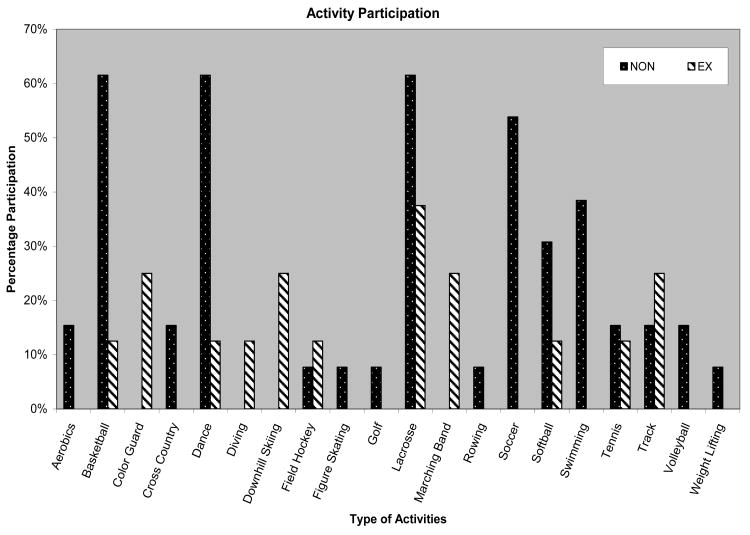
For ex-gymnasts, by the time of the post-menarcheal scan, annual mean physical activity level had decreased for the group and for each individual, even with substitution of other activities for gymnastics (change= -5.1 h/wk, range= -13.8 to −1.6 h/wk). Ex-gymnasts participated in a variety of activities after discontinuing gymnastics; in general, their activities for the interval between ceasing gymnastics and the post-menarcheal DXA scan were similar to those of non-gymnasts (Figure 1). For non-gymnasts, 11 of 13 individuals increased activity between scans, resulting in an increase in the mean physical activity level for the group (change= +2.8 h/wk, range= -2.7 to +6.5 h/wk). The pre- to post-menarche change in annual mean physical activity differed significantly for non-gymnasts (increased activity) vs. ex-gymnasts (decreased activity), ANOVA p=0.01.
Figure 1.
Physical activity participation between the 1st and 2nd DXA scans is depicted for NON-GYMNAST and EX-GYMNAST groups. The percentage of subjects who engaged in each activity is shown separately for each group. Many subjects participated in multiple activities.
Group means did not differ for age, gynecological age (months from menarche), height, fat free mass (FFM), or percent body fat (% fat) at the time of the pre-menarcheal DXA scan (p>0.05)(Table 1). However, at the time of the post-menarcheal scan, gymnasts had lower percent fat than ex-gymnasts (p<0.03). There was no clear, positive correlation between average calcium intake and bone outcomes at either measurement date; accordingly, calcium intake was not included as a covariate in repeated measures ANOVA.
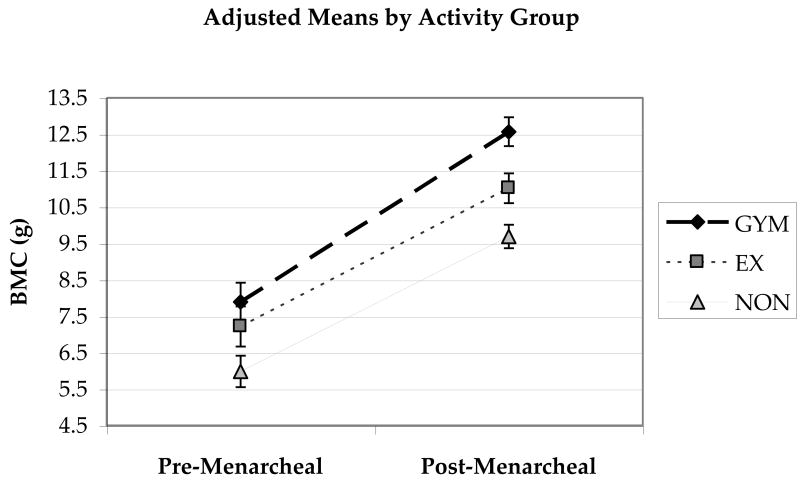
At the pre-menarcheal observation, gymnasts and ex-gymnasts had higher mean forearm aBMD than non-gymnasts, with large effect sizes for both comparisons (Cohen's d=0.98, 0.86, respectively); the effect size for the difference between gymnasts and ex-gymnasts (active gymnasts at the time of the pre-menarcheal observation) was negligible (Cohen's d=0.01)(Figure 2). Forearm BMC means were also higher for gymnast and ex-gymnast groups compared to non-gymnasts, with large effect sizes for the two comparisons (Cohen's d=1.28, 0.83)(Figure 3). Mean forearm BMC was greater in gymnast than ex-gymnast groups (medium effect, Cohen's d=0.46). Similarly, forearm projected area means were greater for gymnasts and ex-gymnasts than for non-gymnasts (large effect sizes, Cohen's d= 1.45; 0.86)(Figure 4); projected area for the gymnast group was larger than for the ex-gymnast group (medium effect, Cohen's d= 0.59).
Figure 3.
Forearm BMC (g) is depicted for gym, ex and non groups. Pre- and post-menarcheal group means and standard errors are adjusted for gynecological age and height.
At the post-menarcheal observation, gymnasts and ex-gymnasts had higher mean forearm aBMD than non-gymnasts, with large effect sizes (Cohen's d=1.86, 0.81, respectively); in addition, gymnasts had higher mean aBMD than ex-gymnasts (large effect size, Cohen's d=1.05)(Figure 2). Mean forearm BMC was also higher for gymnast and ex-gymnast groups than for non-gymnasts, with extremely large effect sizes (Cohen's d=2.61, 1.20)(Figure 3). Additionally, forearm BMC was greater in gymnasts than ex-gymnasts (large effect, Cohen's d=1.41). Forearm projected area was larger for the gymnast group than for both ex-gymnast and non-gymnast groups, with very large effects, (Cohen's d=1.21; 2.31, respectively) and ex-gymnast area was also greater than non-gymnast area (large effect, Cohen's d= 1.09)(Figure 4).
The interaction term, activity group x time, demonstrated large effects for aBMD and BMC (Cohen's d=0.86; 0.76), suggesting different between-group rates for growth in these variables (as depicted in Figures 2 and 3). In contrast, for forearm projected area, the interaction term effect size was small, indicating similar growth rates (Cohen's d= 0.26)(Figure 4).
Discussion
This three-year longitudinal analysis suggests post-menarcheal preservation of skeletal benefits in female ex-gymnasts who quit gymnastics before menarche. These ex-gymnasts maintained higher forearm BMC (14%), projected area (7%), and aBMD (6%) relative to non-gymnasts two years after menarche, despite having quit gymnastics an average of 2.5 years before the post-menarcheal scan. Although differentials were even greater prior to menarche and before retirement (pre-menarcheal BMC 21%, projected area 10%, aBMD 10%), at the post-menarcheal scan, ex-gymnasts maintained approximately two-thirds of their pre-menarcheal advantages over non-gymnasts. These findings provide preliminary evidence that substantial skeletal benefits are attributable to childhood activity and persist after activity cessation, beyond peri- and post-menarcheal growth.
To our knowledge, only one other group has published work evaluating retention of skeletal benefits from previous childhood activity (10, 12, 13). In pre-pubertal children (mean age 7.7 yrs) who had participated in a seven-month randomized, controlled high-impact loading intervention, Fuchs et al. reported retention of statistically significant gains in BMC and bone area at the proximal femur after seven months of detraining (10). Jumpers' total hip BMC advantage diminished from 5.4% immediately post-intervention, to 3.6% seven months later (67% retention of skeletal advantage). In a seven-year follow-up, jumpers maintained a 1.4% advantage in total hip BMC (26% retention of skeletal advantage) (12). Although this difference does not exceed DXA measurement error, longitudinal consistency of the jumpers' advantages in seven measurements over seven years provides compelling evidence for benefit persistence. These investigators attribute the gradual dissipation of benefits to interactions between growth, physical activity, diet and genetic predisposition over the subsequent period of extensive growth, overwhelming effects of the brief intervention (12). Retention of skeletal benefits at the total body, lumbar spine, femoral neck and total hip were reproduced in a separate cohort of children, three years after an identical intervention (13). In comparison to their jumpers, our post-menarcheal ex-gymnasts maintained 65-69% of their pre-menarcheal skeletal advantages more than two years after cessation of gymnastic loading. While our study does not assess significance, the large effect sizes suggest that meaningful benefits have been retained through peri-menarcheal growth, despite de-training during this phase of maximal bone accrual.
Previous studies evaluated adult former gymnasts, seeking indirect evidence of persistent benefits from gymnastic participation during youth. In a small, longitudinal study, mature former collegiate gymnasts (age 24.2 ± 1.7 yrs.), who began training four years before menarche, maintained aBMD advantages over non-gymnasts for at least one year post-retirement (total body 5%; femoral neck 16%)(17). In separate cross-sectional studies, Bass et al. and Kirchner et al. demonstrated greater aBMD in adult former gymnasts than non-gymnasts, with mean percentage differences of 6-22% at the lumbar spine and proximal femur (2, 15). A follow-up evaluation of Kirchner's ex-gymnasts and non-gymnasts nine years later, at a mean of 24 years post-retirement, demonstrated maintenance of gymnasts' aBMD advantages at total body and regional sites (8-14%) (23). Ex-gymnast arm aBMD advantages ranged from 9-14% for all three cross-sectional studies. These percent advantages are greater than the post-menarcheal forearm aBMD advantage noted for our ex (retired from gymnastics prior to menarche (6%)), and similar to the advantage noted for our gym (who remained active throughout adolescence) (13%).
Studies that evaluate adult former gymnasts infer skeletal benefit from participation in gymnastics throughout growth and suggest that benefits are maintained when gymnastics is stopped after skeletal growth is complete. However, they do not address the result of mechanical loading when exposure is limited to childhood or adolescence. By evaluating ex-gymnasts who quit their sport before menarche and completion of skeletal growth, the present study provides prospective evidence for post-menarcheal maintenance of skeletal benefits attributed to pre-menarcheal activity. Additional study is necessary to determine whether these benefits persist through adulthood.
Skeletal benefits in our ex-gymnast cohort are attributable to pre-menarcheal loading. These girls had been active gymnasts during childhood (7.2 ± 1.6 yrs. of age) but had quit an average of 6.7 mos. pre-menarche (none continued beyond menarche). The importance of pre-menarcheal loading is also corroborated by a three-year mixed longitudinal study that evaluated bone accrual in 8-17 year old gymnasts (n=45) and non-gymnasts (n=54) (22). After adjustment for height and weight using multilevel modeling, their gymnasts had 24-51% higher BMC and 13-28% higher aBMD compared to non-gymnasts. For axial and total body bone variables, the greatest percentage differences were found at peak height velocity (PHV). For arm BMC and aBMD, the greatest percentage differential occurred at the earliest biological age (3 yrs prior to PHV). As PHV generally occurs about one year pre-menarche, these differentials support our conclusion that pre-menarcheal activity is paramount in enhancing bone accrual. However, their gymnasts' absolute arm BMC advantages continued to increase annually, through the third year post-PHV (22). This trend suggests further benefit from continued gymnastics participation. Similarly, our gymnast vs. ex-gymnast comparisons suggest an additive benefit from continued peri- and post-menarcheal loading: gymnast forearm aBMD and BMC advantages were greater at the post- vs. pre-menarcheal measurement (aBMD: pre= 1%, post= 7%; BMC: pre= 9%, post= 14%).
To reduce potential confounding effects of loading via daily life and other non-gymnastic activities, our analyses used the non-dominant forearm as a barometer of gymnastic loading. At this site, the magnitude of non-gymnastic loading is likely to be markedly lower than gymnastic loading. Nonetheless, to account for non-gymnastic loading, we reported participation in organized, non-gymnastic activity for ex and non over the focal peri-menarcheal interval (Figure 1). Both groups participated in a variety of osteogenic activities, including some that may have yielded low-level, bilateral forearm loads (basketball, lacrosse, field hockey and softball). For ex-gymnasts, organized activity participation dropped after gymnastic cessation, whereas non-gymnasts increased activity over the peri-menarcheal interval. We did not assess non-organized activity (free play), but it is unlikely that this un-quantified loading differed between groups of this age. Thus, it is unlikely that “other” activities are responsible for the post-menarcheal skeletal advantages attributed to pre-menarcheal gymnastic loading. Finally, several non-gymnasts had a history of recreational gymnastics participation during early childhood, but they had quit gymnastics more than three years prior to the pre-menarcheal DXA scan. Accordingly, early gymnastic participation may have increased bone parameter means for the non group; therefore, our ex vs. non comparisons may actually underestimate retention of benefits in ex-gymnasts.
Because DXA assesses bone in two dimensions and does not measure internal architecture, it has been criticized as a tool for measuring the growing skeleton. Nonetheless, DXA is frequently employed in growth studies due to ease of use, low radiation dose, applicability to axial and appendicular sites and wide availability. We have included aBMD, BMC and projected area in our results to allow comparison with other pediatric studies. BMC provides a simple assessment of bone mass, but it does not account for bone distribution or size. Projected area indicates bone size, but only in one dimension (medial-lateral). Areal BMD provides an indicator of overall bone mass, but this parameter does not specifically characterize geometry or density. Finally, fan beam DXA parameters can be problematic, as elevation off the table by the soft tissue envelope introduces a systematic error in bone outcomes. Although this error is particularly pronounced at axial sites (lumbar spine and femoral neck), the soft-tissue envelope at the forearm is minimal, decreasing the influence of fan beam error (6). Furthermore, the validity of our DXA measures is supported by strong agreement between pQCT and DXA indices for the radius in a similar post-menarcheal cohort (9).
This preliminary study is strengthened by its design; bone accrual was evaluated in girls of similar gynecological ages over a similar maturational period. Study inclusion was based upon the chance timing of menarche relative to prospectively obtained annual DXA scans, generating no systematic bias for inclusion or exclusion of subjects within the total cohort. Critically, differences in menarcheal age were not detected between gymnasts, ex-gymnasts and non-gymnasts, and, as a group, our gymnasts did not exhibit delayed menarche, as is frequently associated with gymnastics participation. Thus, confounding maturational differences were minimized.
Although self-selection bias for activity group membership cannot be ruled out, work by Laing et al. suggested that gymnastic-related skeletal advantages are not solely attributable to this phenomenon (19). They compared pre-pubertal gymnasts vs. non-gymnasts and detected no baseline advantage in bone measures at training initiation. At follow-up, they observed a slight BMC advantage in gymnasts after two years of training, suggesting that gymnasts' skeletal advantages are attributable to loading rather than self-selection (19).
Although this study was limited by a comparatively small sample size, ex-gymnast vs. non-gymnast forearm aBMD, area and BMC comparisons yielded large effect sizes for differences between ex-gymnasts and non-gymnasts at both pre- and post-menarcheal time points. Without considering the effect of covariates, this result indicates minimum required cell sizes of n=24, 16, and 40 (respectively) to achieve at least 80% power for detection of significant differences between ex-gymnasts and non-gymnasts in future peri-menarcheal studies. Our two-observation design assesses between-group differences in net bone gain only; additional scans at cessation of gymnastic activity and at more frequent intervals might have generated a more complex picture of bone growth, particularly for the ex group. As seven of eight ex-gymnasts continued gymnastics between the pre-menarcheal scan and menarche, these girls may have experienced an additional period of accelerated bone growth between scans (prior to retirement) and/or a phase of detraining-related bone loss or zero net gain (after retirement). Accordingly, future studies will include a larger number of participants and use multilevel modeling, thereby increasing statistical power and allowing evaluation of gymnastic exposure timing and detraining effects.
Our results provide preliminary evidence that skeletal benefits attributed to mechanical loading during growth persist through the early post-menarcheal years, even after osteogenic activity is discontinued. This analysis focuses on the forearm as a model of mechanical loading via gymnastic activity; additional study is necessary for evaluation of region- and tissue-specific skeletal adaptation and maintenance. Prolonged follow-up of this cohort is necessary to determine whether benefits are maintained to adulthood.
Acknowledgments
Funding for the current study was provided by: NIH/NIAMS, the Orthopedic Research and Education Foundation and SUNY Upstate Medical University. This work was made possible through the efforts of many individuals who participated in subject measurement and data management over the years. The authors would particularly like to acknowledge the assistance of Christina Morganti, Moira Davenport, Susan Hemingway, Cathy Riley, Paula Rosenbaum and Kay Bruening. Of course, we are most grateful for the continued dedication of our subjects and their parents.
Footnotes
The authors are subject to no conflicts of interest.
Contributor Information
Tamara A. Scerpella, SUNY Upstate Medical University
Jodi N. Dowthwaite, SUNY Upstate Medical University
Nicole M. Gero, SUNY Upstate Medical University
Jill A. Kanaley, University ot Missouri
Robert J. Ploutz-Snyder, NASA — Johnson Space Center
References
- 1.Bailey DA. The Saskatchewan pediatric bone mineral accrual study: bone mineral acquisition during the growing years. Int J Sports Med. 1997;18:S191–4. doi: 10.1055/s-2007-972713. [DOI] [PubMed] [Google Scholar]
- 2.Bass S, Pearce G, Bradney M, Hendrich E, Delmas PD, Harding A, Seeman E. Exercise before puberty may confer residual benefits in bone density in adulthood: studies in active prepubertal and retired female gymnasts. J Bone Miner Res. 1998;13(3):500–7. doi: 10.1359/jbmr.1998.13.3.500. [DOI] [PubMed] [Google Scholar]
- 3.Bass SL, Saxon L, Daly RM, Turner CH, Robling AG, Seeman E, Stuckey S. The effect of mechanical loading on the size and shape of bone in pre-, peri- and post-pubertal girls: A study in tennis players. J Bone Miner Res. 2002;17(12):2274–2280. doi: 10.1359/jbmr.2002.17.12.2274. [DOI] [PubMed] [Google Scholar]
- 4.Cadogan J, Blumsohn A, Barker ME, Eastell R. A longitudinal study of bone gain in pubertal girls: anthropometric and biochemical correlates. J Bone Miner Res. 1998;13:1602–1612. doi: 10.1359/jbmr.1998.13.10.1602. [DOI] [PubMed] [Google Scholar]
- 5.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale (NJ): Lawrence Erlbaum Associates; 1988. p. 532. [Google Scholar]
- 6.Cole JH, Scerpella TA, van der Meulen MCH. Fan-beam densitometry of the growing skeleton: are we measuring what we think we are? J Clin Densitometry. 2005;8:57–64. doi: 10.1385/jcd:8:1:057. [DOI] [PubMed] [Google Scholar]
- 7.Courteix D, Lespessailles E, Jaffre C, Obert P, Benhamou CL. Bone mineral acquisition and somatic development in highly trained girl gymnasts. Acta Paediatr. 1999;88:803–808. doi: 10.1080/08035259950168694. [DOI] [PubMed] [Google Scholar]
- 8.Dowthwaite JN, Flowers PPE, Spadaro JA, Scerpella TA. Bone geometry, density and strength indices of the distal radius reflect loading via childhood gymnastic activity. J Clin Densitom. 2007;10(1):65–75. doi: 10.1016/j.jocd.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dowthwaite JN, Hickman RM, Kanaley JA, Ploutz-Snyder RJ, Spadaro JA, Scerpella TA. Distal radius strength: A comparison of DXA-derived vs. pQCT-measured parameters in adolescent females. J Clin Densitom. 2009;12(1):42–53. doi: 10.1016/j.jocd.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Fuchs RK, Snow CM. Gains in hip bone mass from high-impact training are maintained: A randomized controlled trial in children. J Pediatr. 2002;141(3):357–62. doi: 10.1067/mpd.2002.127275. [DOI] [PubMed] [Google Scholar]
- 11.Gero N, Cole J, Kanaley J, van der Meulen M, Scerpella T. Increased bone accrual in premenarcheal gymnasts: A longitudinal study. Ped Ex Sci. 2005;17:43–45. [Google Scholar]
- 12.Gunter KB, Baxter-Jones ADG, Mirwald RL, Almstedt H, Fuchs RK, Durski S, Snow C. Impact Exercise Increases BMC During Growth: An 8-Year Longitudinal Study. J Bone Miner Res. 2008;23(7):986–993. doi: 10.1359/JBMR.071201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gunter KB, Baxter-Jones ADG, Mirwald RL, Almstedt H, Fuller A, Durski S, Snow C. Jump starting skeletal health: A 4-year longitudinal study assessing the effects of jumping on skeletal development in pre and circum pubertal children. Bone. 2008;42:710–718. doi: 10.1016/j.bone.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Kannus P, Haapasalo H, Sankelo M, Sievanen H, Pasanen M, Heinonen A, Oja P, Vuori I. Effect of starting age of physical activity on bone mass in the dominant arm of tennis and squash players. Ann Intern Med. 1995;123(1):27–31. doi: 10.7326/0003-4819-123-1-199507010-00003. [DOI] [PubMed] [Google Scholar]
- 15.Kirchner EM, Lewis RD, O'Connor PJ. Effect of past gymnastics participation on adult bone mass. J Appl Physiol. 1996;80(1):226–32. doi: 10.1152/jappl.1996.80.1.226. [DOI] [PubMed] [Google Scholar]
- 16.Kontulainen S, Sievanen H, Kannus P, Pasanen M, Vuori I. Effect of long-term impact-loading on mass, size, and estimated strength of humerus and radius of female racquet-sports players: a peripheral quantitative computed tomography study between young and old starters and controls. J Bone Miner Res. 2003;18(2):352–9. doi: 10.1359/jbmr.2003.18.2.352. [DOI] [PubMed] [Google Scholar]
- 17.Kudlac J, Nichols DL, Sanborn CF, DiMarco NM. Impact of detraining on bone loss in former collegiate female gymnasts. Calcif Tissue Int. 2004;75:482–87. doi: 10.1007/s00223-004-0228-4. [DOI] [PubMed] [Google Scholar]
- 18.Laing EM, Massoni JA, Nickols-Richardson SM, Modlesky CM, O'Connor PJ, Lewis RD. A prospective study of bone mass and body composition in female adolescent gymnasts. J Pediatr. 2002;141:211–216. doi: 10.1067/mpd.2002.126599. [DOI] [PubMed] [Google Scholar]
- 19.Laing EM, Wilson AR, Modlesky CM, O'Connor PJ, Hall DB, Lewis RD. Initial years of recreational artistic gymnastics training improves lumbar spine bone mineral accrual in 4- to 8- year-old females. J Bone Miner Res. 2005;20(3):509–19. doi: 10.1359/JBMR.041127. [DOI] [PubMed] [Google Scholar]
- 20.McNitt-Gray JL, Hester DM, Mathiyakom W, Munkasy BA. Mechanical demand and multijoint control during landing depend on orientation of the body segments relative to the reaction force. J Biomech. 2001;34:1471–1482. doi: 10.1016/s0021-9290(01)00110-5. [DOI] [PubMed] [Google Scholar]
- 21.Nickols-Richardson SM, O'Connor PJ, Shapses SA, Lewis RD. Longitudinal bone mineral density changes in female child artistic gymnasts. J Bone Miner Res. 1999;14(6):994–1002. doi: 10.1359/jbmr.1999.14.6.994. [DOI] [PubMed] [Google Scholar]
- 22.Nurmi-Lawton JA, Baxter-Jones AD, Mirwald RL, Bishop JA, Taylor P, Cooper C, New SA. Evidence of sustained skeletal benefits from impact-loading exercise in young females: a 3-year longitudinal study. J Bone Miner Res. 2004;19(2):314–22. doi: 10.1359/JBMR.0301222. [DOI] [PubMed] [Google Scholar]
- 23.Pollock NK, Laing EM, Modlesky CM, O'Connor PJ, Lewis RD. Former college artistic gymnasts maintain higher BMD: a nine-year follow-up. Osteoporosis Int. 2006;17(11):1691–1697. doi: 10.1007/s00198-006-0181-3. [DOI] [PubMed] [Google Scholar]
- 24.Sabatier JP, Guaydier-Souquieres G, Benmalek A, Marcelli C. Evolution of lumbar bone mineral content during adolescence and adulthood: a longitudinal study in 395 healthy females 10-24 years of age and 206 premenopausal women. Osteoporos Int. 1999;9:476–82. doi: 10.1007/s001980050173. [DOI] [PubMed] [Google Scholar]
- 25.Scerpella TA, Davenport M, Morganti CM, Kanaley JA, Johnson LM. Dose related association of impact activity and bone mineral density in pre-pubertal girls. Calcif Tissue Int. 2003;72:24–31. doi: 10.1007/s00223-001-1131-x. [DOI] [PubMed] [Google Scholar]