Abstract
BACKGROUND
The purpose of this study is to compare the compositions of federally-funded surgical research between 2003 and 2013, and to assess differences in funding trends between surgery and other medical specialties.
DATA SOURCES
The NIH RePORTER database was queried for grants within core surgical disciplines during 2003 and 2013. Funding was categorized by award type, methodology, and discipline. Application success rates for surgery and five non-surgical departments were trended over time.
RESULTS
Inflation-adjusted NIH funding for surgical research decreased 19% from $270M in 2003 to $219M in 2013, with a shift from R-awards to U-awards. Proportional funding to outcomes research almost tripled, while translational research diminished. Non-surgical departments have increased NIH application volume over the last 10 years; however, surgery’s application volume has been stagnant.
CONCLUSIONS
To preserve surgery’s role in innovative research, new efforts are needed to incentivize an increase in application volume.
Keywords: National Institutes of Health, Surgical research, research funding, academic surgery, mentorship, outcomes research
INTRODUCTION
Scholarly contributions to research are important measures of success in academic surgery, and the ability to obtain funding for such efforts is frequently considered for recruitment and promotion (1–4). As the largest public funding source for medical research world-wide, the National Institutes of Health (NIH) is universally recognized for its scientific rigor and role in academic advancement (5). The overall NIH budget increased dramatically from 1999–2003, however, it has not kept pace with inflation since that time. As a result, funding success rates have steadily decreased, such that only the top 10% of applications were awarded in 2013 (6, 7).
Historically, surgeon-scientists have lagged behind counterparts in other medical departments with regards to NIH funding, due in part to increasing clinical responsibilities (8, 9). As a result, the proportion of surgeons with NIH awards is only one-quarter that of non-surgeon physicians, and surgeons are under-represented in NIH study sections (10, 11). In order to expand surgery’s role in medical research, it would be sensible to examine how other medical specialties have compensated for the NIH’s budgetary decline. Furthermore, the impact of the depreciating NIH budget on individual surgical disciplines is uncertain, and contributions from growing fields such as health outcomes research are unclear. In order to take advantage of shifting trends, an assessment of the current landscape of funded surgical research is indicated.
The purpose of this study was two-fold. First, we assessed trends in NIH applications and success rates across major medical school departments in order to test the hypothesis that surgery has been affected disproportionately by the decrease in the NIH budget. Second, we examined the distribution of surgery research subjects and methodologies in 2003 and in 2013 to determine key areas of growth. Through these analyses, we hoped to propose strategies to promote future surgical research.
MATERIALS AND METHODS
The NIH RePORTER online database (Research Portfolio Online Reporting Tool, available at http://report.nih.gov) was queried for all research project grants within the United States and territories during the fiscal years of 2003 and 2013. Grants allocated to departments of surgery were selected through the “Department” search field. F- and T-awards were excluded as these represent resident and student training grants. Because the purpose of the study was to depict the landscape of surgery-related research, grants were included regardless of the advanced degree of the principal investigator (M.D., Ph.D., etc.). The exported data included summary descriptions of research, total costs, and information regarding principal investigators and research institutions. For comparative purposes, this identical process was used to query NIH support for the four best-funded clinical departments: internal medicine, psychiatry, pathology, and pediatrics, and the best-funded basic science department: microbiology. Additionally, application success rates for surgery and comparison departments were collected via the NIH database (12).
Research summary descriptions for surgery grants were reviewed by one of two study investigators (YH, BE). Each investigator reviewed grants from both datasets (2003 and 2013). Based on summary descriptions, each grant was categorized by surgical discipline. Departments of surgery in the United States vary in their inclusion of certain surgical specialties (neurosurgery, urology, obstetrics and gynecology, otolaryngology, ophthalmology). To be consistent across the study, only grants focusing on core surgical disciplines were included for analysis. For summary descriptions which were too broad for categorization, the principal investigator’s listed academic division was used as the surgical discipline. The surgical oncology discipline included cancer-related studies in any organ system. Research in undergraduate or graduate education and non-cancer research in the gastroenterology, endocrine, or hepatobiliary organ systems were included in the general surgery discipline. The research methodology for each grant was classified into the following categories: basic science, translational, clinical trial, outcomes, and operative technique. Basic science research was defined by a focus on core biological pathways, with no assessment of immediate therapeutic or diagnostic effect. Translational research included experiments aimed at addressing therapeutic or diagnostic needs for a specific human disease, including animal models of human pathology. Clinical trials were defined as hypothesis-driven human experiments targeting an existing medicine or procedure, while operative technique research was limited to novel surgical innovations. Finally, outcomes research included projects assessing institutional or multi-institutional outcomes of health care practices. Grant descriptions which incorporated several methodological categories were classified as translational research. To assess inter-rater agreement, 150 grants were evaluated by both reviewers. Inter-rater agreement was 0.85, with all differences in classification originating from the delineation between basic science and translational research.
Total costs of grants allocated in fiscal year 2003 were adjusted to 2013 equivalent dollars using an inflation adjustment factor of 1.27 (13). Summary statistics for mean and total allocations are provided by award activity and award type. Proportional contributions to total NIH surgery research funding were calculated based on research methodology and discipline. To determine trends in average funding per grant, the Wilcoxon rank sum test was used to compare allocations between 2003 and 2013 in order to account for nonparametric data distributions.
RESULTS
In total, 1025 grants in core surgical disciplines met inclusion criteria and underwent review: 613 from 2003 and 512 from 2013. Total adjusted NIH funding to surgical research diminished 19.1% from $270.4M in 2003 to $218.7M in 2013. Geographic distribution of NIH funding by state in 2003 and in 2013 is provided within Supplemental Materials.
Allocations to departments of surgery by research activity and award type are presented in Table 1. Funding for research projects (R-awards) underwent the largest decrease (-38%), including a 39% decrease in R01 awards ($152.2M to $92.8M). Allocations for cooperative agreements (U-awards) increased 23%, making up 28% of total surgery research funding in 2013. K-awards—representing mentored research among young physician-scientists—saw a 33% decrease, with notable drops in several major surgical disciplines (Table 2). Additional data on award activities subdivided by surgical discipline are available in the Supplemental Materials. Non-competitive renewals (Type 5) dominated funding within both datasets, and new grants (Type 1) comprised 17% of funding for both periods. Notably, allocations to competitive renewals (Type 2) have diminished by 66%.
Table 1.
National Institutes of Health grants awarded to departments of surgery
| 2003a | 2013 | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| N | Total $M (%) | Median $K | N | Total $M (%) | Median $K | % Change (N) | % Change (Total $) | |
| Total Awards | 613 | 270.4 | 344.4 | 512 | 218.7 | 304.6 | −16.5% | −19.1% |
| Activity | ||||||||
| R | 454 | 173.3 (64%) | 367.6 | 343 | 108.1 (49%) | 307.5 | −24.40% | −37.60% |
| K | 82 | 13.1 (5%) | 159.9 | 57 | 8.8 (4%) | 133.9 | −30.50% | −32.80% |
| U | 48 | 50.1 (19%) | 340.4 | 81 | 61.7 (28%) | 477.5 | +68.80% | +23.20% |
| P | 27 | 33.7 (12%) | 1349.3 | 28 | 35.5 (16%) | 1218.5 | +3.70% | +5.30% |
| Award Typeb | ||||||||
| 1 | 115 | 44.8 (17%) | 344.8 | 82 | 37.3 (17%) | 309.6 | −28.70% | −16.70% |
| 2 | 42 | 22.3 (8%) | 408.4 | 17 | 7.5 (3%) | 380.8 | −59.50% | −66.40% |
| 3 | 31 | 3.9 (1%) | 61.8 | 37 | 5.1 (2%) | 75 | +19.40% | +30.80% |
| 4 | 3 | 1.5 (1%) | 496.7 | 1 | 0.3 (<1%) | 280.6 | −66.70% | −80% |
| 5 | 401 | 190.6 (70%) | 342.3 | 367 | 163.6 (75%) | 309.3 | −8.50% | −14.20% |
| 7 | 19 | 6.1 (2%) | 298.9 | 8 | 4.8 (2%) | 307.3 | −57.90% | −21.30% |
| 8 | 2 | 1.2 (<1%) | 601.4 | 0 | 0 | 0 | - | - |
| Institutec | ||||||||
| NCI | 137 | 66.8 (25%) | 335.4 | 137 | 54.9 (25%) | 285.7 | 0% | −17.90% |
| NHLBI | 135 | 62.4 (23%) | 390.9 | 121 | 44.3 (20%) | 361.8 | −10.40% | −29.10% |
| NIAID | 54 | 32.3 (12%) | 361.7 | 41 | 30.0 (14%) | 358.3 | −24.10% | −7.00% |
| NIDDK | 136 | 48.6 (18%) | 293.4 | 95 | 36.7 (17%) | 314.2 | −30.10% | −24.50% |
| NIGMS | 89 | 35.4 (13%) | 350.2 | 39 | 14.5 (7%) | 287 | −56.20% | −59.00% |
| Other | 62 | 24.9 (9%) | 250.4 | 79 | 38.3 (18%) | 292.3 | +27.40% | −53.90% |
Allocations in 2003 adjusted for inflation (x1.266)
Application Types: Type 1—new; Type 2—competing continuation; Type 3—competing revision/supplement; Type 4—extension; Type 5—non-competing continuation; Type 7—change in institution; Type 8—change in awarding institute
Institutes: NCI–National Cancer Institute; NHLBI—National Heart, Lung, and Blood Institute; NIAID—National Institute of Allergy and Infectious Diseases; NIDDK—National Institute of Diabetes and Digestive and Kidney Diseases; NIGMS—National Institute of General Medical Sciences
Table 2.
Distribution of K-awards in 2013 versus 2003
| 2003a | 2013 | |||
|---|---|---|---|---|
|
| ||||
| N | Total ($M) | N | Total ($M) | |
| General | 16 | 2.54 | 4 | 0.56 |
| Cardiothoracic | 9 | 1.48 | 10 | 1.31 |
| Pediatric | 7 | 1.00 | 2 | 0.25 |
| Surgical Oncology | 19 | 3.52 | 10 | 2.58 |
| Transplant | 5 | 0.74 | 8 | 1.06 |
| Trauma/Crit Care | 13 | 1.96 | 6 | 0.70 |
| Vascular | 12 | 1.74 | 9 | 1.26 |
Allocations in 2003 adjusted for inflation (x1.266)
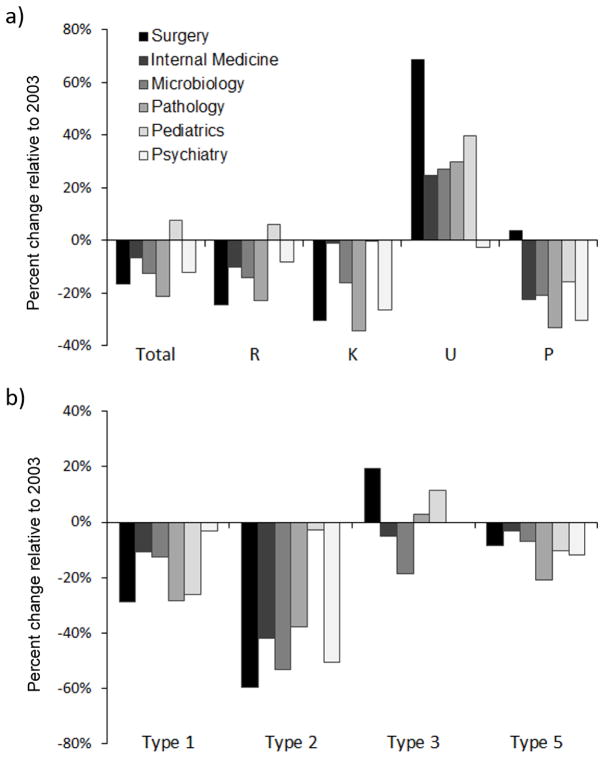
Comparisons between surgery and the other five studied departments in NIH research are provided in Figure 1. Over the 2003–2013 period, surgery’s relative decrease in total number of research awards was second only to pathology. Surgery’s decreases in R-award activity, Type 1 awards, and Type 2 awards were the most severe of all comparison departments, and its decrease in K-awards was second-most. On the other hand, surgery enjoyed the greatest relative increases in U-awards and Type 3 awards (competitive revisions). Additional data on total funding amount and average grant size for non-surgical departments are available in Supplemental Materials.
Figure 1.
Relative change in award number between years 2003 and 2013 across medical departments, by award activity (a) and award type (b).
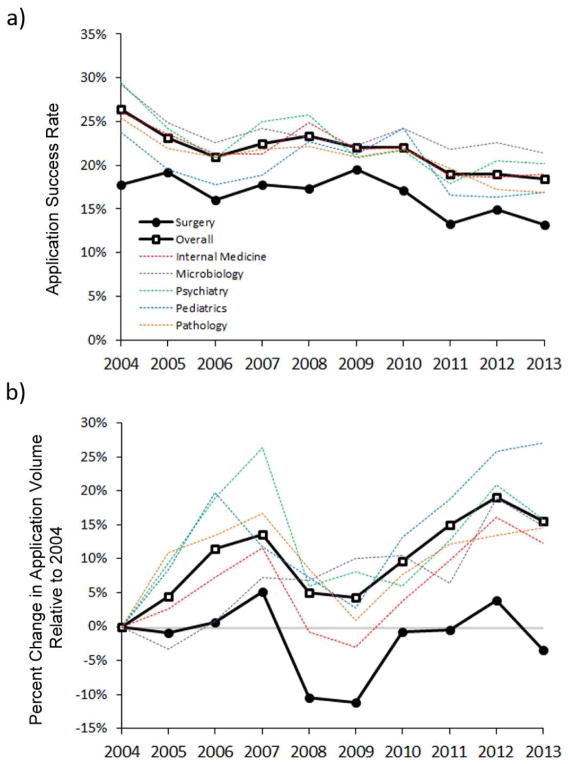
Trends in success rate and application volume are available through the NIH for the years 2004 through 2013. Surgeons have traditionally had a lower application success rate than non-surgeons (10). This relationship held true as success rates decreased across the NIH overall (Figure 2). However, over this 10-year period, each of the non-surgical departments have had a compensatory increase in application volume. Indeed, the NIH as a whole received 15% more applications in 2013 than in 2004. On the other hand, surgery’s application volume has been stagnant over the same period, such that the number of applications submitted by departments of surgery in 2013 was actually lower than in 2004 (Figure 2).
Figure 2.
Trends in award success rate (a) and application volume (b) within surgery and five top-funded non-surgical departments between years 2004 and 2013.
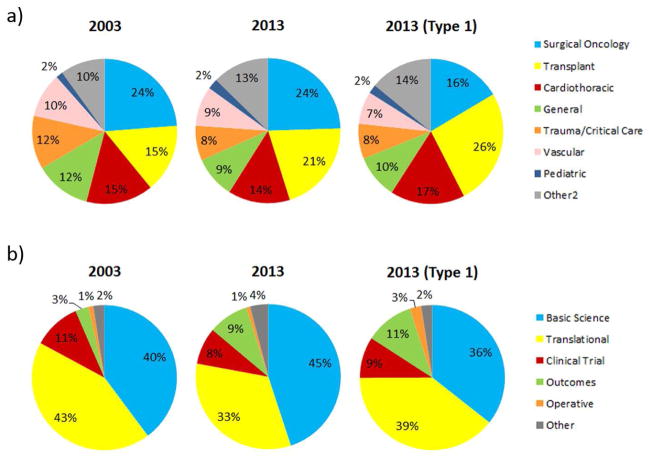
Proportional contributions to total surgical funding by research methodology and discipline are shown in Figure 3. Surgical oncology was the largest recipient of funding in both fiscal years. Transplant surgery has expanded rapidly, receiving 21% of funds in 2013, including 26% of Type 1 allocations. This growth was largely driven by an increase in U-awards, which comprised 36% (27/75) of transplant grants in 2013, compared to only 12% (54/437) of non-transplant grants (p < 0.001). Transplant U-awards averaged $908K each, while other transplant awards averaged only $429K each (p = 0.004). An emerging contributor to general surgery is endocrine research. Funding in this area increased greater than 4.5-fold by 2013 and comprised 6% of all surgery Type 1 allocations. Laboratory-based research—basic science or translational—comprised 83% of total research funds in 2003 and 78% in 2013. Outcomes research has expanded, increasing from 3% to 9% of total research funds, including 11% of Type 1 allocations.
Figure 3.
Relative distribution of National Institutes of Health funding allocations to surgery, by surgical discipline (a) and research methodology (b).
Average total cost per grant was calculated for each research methodology and surgical discipline, and data from the two fiscal years were compared using the Wilcoxon rank sum test (Table 3). Average allocation per grant significantly decreased for surgical research overall, from $344.4K in 2003 to $304.6K in 2013 (p = 0.010). A significant decrease in per-grant value was noted for basic science research (−10.1%, p = .004) and research in trauma and critical care (−17.7%, p = .002). Grants provided to transplant and pediatric surgery increased in value, however, these trends were not significant.
Table 3.
Median grant allocations in 2013 versus 2003
| 2003a | 2013 | % Change Value | p-valueb | |||
|---|---|---|---|---|---|---|
|
| ||||||
| N | Median ($K) | N | Median ($K) | |||
| Total | 613 | 344.4 | 512 | 304.6 | −11.5% | .010 |
| Type: | ||||||
| Basic Science | 299 | 339.3 | 263 | 304.9 | −10.1% | .004 |
| Translational | 257 | 358.3 | 135 | 334.2 | −6.7% | .627 |
| Clinical Trials | 17 | 408.1 | 31 | 321.9 | −21.1% | .144 |
| Outcomes | 18 | 267.8 | 50 | 233.7 | −12.7% | .928 |
| Operative | 8 | 354.7 | 5 | 290.5 | −18.1% | .721 |
| Disciplines: | ||||||
| General | 101 | 346.3 | 66 | 293.9 | −15.1% | .091 |
| Cardiothoracic | 91 | 369.6 | 83 | 361.8 | −2.1% | .288 |
| Pediatric | 14 | 167.8 | 11 | 281.2 | +67.6% | .405 |
| Surgical Oncology | 131 | 318.8 | 126 | 289.1 | −9.3% | .052 |
| Transplant | 97 | 335.6 | 75 | 353.2 | +5.2% | .129 |
| Trauma/Crit Care | 83 | 348.9 | 50 | 287.0 | −17.7% | .002 |
| Vascular | 54 | 391.0 | 47 | 342.8 | −12.3% | .062 |
Allocations in 2003 adjusted for inflation (x1.266)
p-value compares average allocations in 2003 versus 2013 using the Wilcoxon rank sum test
DISCUSSION
There has been a reduction in inflation-adjusted surgical funding between the years 2003 and 2013 that is more severe than the overall contraction in the NIH budget. Surgical research has experienced a reduction in R- and K-awards with a concurrent increase in U-awards, suggesting a movement from single-investigator projects toward multi-institutional endeavors. Embedded within overall stagnant trends are several emerging areas of academic growth.
The years 2013 and 2003 represent landmarks in research policymaking. The NIH budget doubled between 1999 to 2003, a period characterized by an unprecedented increase in federal grant applications (14). Since that time, inflation has gradually eroded the purchasing power of the NIH. As a result, application success rates have decreased dramatically, particularly among first-time (Type 1) submissions (6). In 2009, the American Recovery and Reinvestment Act infused over $8 billion into the NIH, boosting research over the following 2 years. However, residual impact from this measure within 2013 data is likely to be minimal. After a $1.55 billion reduction due to sequestration, the adjusted NIH budget in 2013 was the lowest in 13 years (7, 15).
In the years preceding 2003, the proportion of NIH funding dedicated to surgery was largely stable (11). However, work by Mann and colleagues showed that surgeons had begun to lag behind non-surgical counterparts in research participation by 2008, largely due to a lower application rate (10). Our data reveal that this disparity has enlarged since 2008–2009. There has been an increase of 15–20% in application rates across the five top research departments between 2004–2013, while surgery’s application rate has decreased about 4%. This trend may be explained in part by expanding workforces in departments of internal medicine and infectious disease (16). However, other non-surgical specialties such as pediatrics and psychiatry have had relatively stable workforces, yet have had substantial increases in application volume. Equally concerning is the fact that application success rates for departments of surgery have persistently remained lower than non-surgical counterparts. Encouragingly, this gap has narrowed compared to 2004. Surgeons comprise a comparative minority within NIH review sections; thus, it has been suggested that surgeon-scientists may suffer from negative bias in the review process (17). Finally, increasing clinical demands have promoted perceptions in both the surgeon and non-surgeon communities that it is progressively more challenging for surgeon-scientists to produce high-volume, rigorous research.
Progressive changes have occurred in the surgical research landscape. Our data corroborate recent work showing declines in K08’s and R01’s awarded to physicians across all medical fields (18). The fact that there has been a concurrent increase in surgery U-awards suggest that surgeon-scientists unable to attain a first-time R01 award should not only revise an existing application (19), but also seek out collaborators for multi-institutional efforts. Furthermore, despite the fact that grants through the Agency for Healthcare Research and Quality (AHRQ) were not included in our dataset, expansion in outcomes-based research was readily apparent. Including AHRQ allocations would likely further magnify this evolving area of investigation.
Surgical oncology, transplant, and cardiothoracic surgery have traditionally dominated core surgical research, and there are no indications that their prominence will change in the near future. Transplant stands out as a persistently expanding entity, due at least in part to a high prevalence of U-awards which on average garner more federal support than R-awards. There has been a relative contraction in general surgery research, from 101 awards in 2003 to 66 in 2013. Research disciplines within our dataset were categorized by grant summary descriptions rather than investigator training. Nevertheless, as the academic surgical workforce becomes increasingly specialized (20), so too may the scope of surgical research.
Although decreasing in absolute number, Type 1 allocations—indicative of new projects—have contributed a constant percentage to overall funding between 2003 and 2013. In contrast, Type 2 allocations—indicative of competitive renewals—have fallen precipitously. In 2007, the NIH adopted policy changes aimed at increasing the percentage of research awards allocated to new investigators (21). Designed to complement future innovation, these strategies may have negatively impacted the preservation of established research. Other contributing factors may include a progressive shift toward shorter research projects or a reluctance to renew research in the face of mounting clinical demands. Importantly, NIH’s new investigator policies pertain only to R01’s, and do not apply to training grants such as K-awards. Recent publications have shown trends toward diminishing K-award funding within transplant, endocrine, and cardiothoracic surgery, with clinical responsibilities cited as the primary barrier to research (22–25). Our data corroborate these findings by noting a one-third reduction in K-awards over the last decade, a decline surpassed among clinical departments only by pathology.
In light of these findings, a broad reexamination of the research paradigm is indicated. Traditional valuation of surgical research is based on internal measures of productivity and innovation, institutional dominance of the research “market share”, and potential for competitive advantages in clinical practice (26). Key within this system are young investigators, who provide the seeds for future innovation. The optimal method for cultivating this population is unclear. Most surgery chairpersons do not judge publication rate to be the most important indicator of research success in residency (27). However, the number of articles published in residency is associated with future funding success (28–30). Because surgery residents typically conduct dedicated research three or more years before entering practice, topics addressed during these fellowships may be obsolete by the time they apply for K-awards (11). What remains relevant, however, are the abilities to pose meaningful questions, think critically, and write compellingly. Therefore, these are the skill sets that should receive the greatest focus during training.
Patronage must not terminate with residency. Surgery departments should assign to each new faculty member one or more research mentors who are eager to teach the research process, particularly with regards to writing manuscripts and grant applications. In an era in which procedure-related financial compensation is ever more stringent, expanding operative case volume is frequently the primary means by which surgeons can maintain consistent earnings. Furthermore, resident work-hour restrictions have led to an increase in clinical responsibilities among faculty, thereby reducing time available for research (31). In addition to mentorship, our results stress the need to incentivize faculty to submit grant applications. Such incentives may take the form of protected time or salary support for the application process itself. As departmental earnings continue to contract, however, provision of these short-term subsidies will require conviction that such investments will be rewarded in the long-run by research innovation.
This study has several limitations. Trends in research across specialties outside of core surgical disciplines were not assessed. Exclusion of these areas was necessary to ensure a reliable dataset. Nevertheless, reporting research productivity using specialty academic society rosters would be a worthwhile pursuit. Second, several surgical disciplines had small numbers of grants within each fiscal year. Thus, comparisons regarding changes in average grant value within these disciplines may be underpowered. Finally, by searching only for grants awarded through the NIH, contributions through organizations such as the Centers for Disease Control and Prevention, the Patient Centered Outcomes Research Institute (PCORI), and the AHRQ were excluded. Given the growth in outcomes studies, surgery’s roles within AHRQ and PCORI are deserving of prospective study. However, with a combined budget less than 3% that of the NIH (32), the expected impact of AHRQ and PCORI grants to data within this study is relatively minor. Other sources of funding not examined in this study include funding through the Department of Defense and research foundations such as the Gates Foundation, American Cancer Society, and American Heart Association.
CONCLUSIONS
Although the recent decline in surgical funding does outpace non-surgical fields, the difference is not vast. Within this environment are categories of research that continue to thrive, such as cooperative efforts and investigations in transplant and endocrine surgery. Outcomes research is expanding, and should be further developed along with health services and education research. However, over 70% of NIH funding continues to support laboratory-based research (translational and basic). The continued success of surgeons in garnering support for these research areas is a testament to the viability of academic surgical careers in laboratory-based science. To ensure that NIH funding continues to support important surgical innovation, training programs must refocus attention toward mentorship of junior investigators and incentivizing the grant application process.
Supplementary Material
Supplemental Table 1: Distribution of common award activities across surgical disciplines in 2003 and 2013.
Supplemental Table 2: National Institutes of Health grants awarded to top five research departments
Geographic distribution of National Institutes of Health funding to departments of surgery
BRIEF SUMMARY.
Between 2003 and 2013, NIH research funding to core disciplines in departments of surgery has diminished by one fifth in inflation-adjusted dollars. Volume of NIH applications from departments of surgery is consistently lower than from non-surgical departments. To improve the research outlook for academic surgeons, young investigators must be effectively incentivized to increase the rate of NIH grant applications.
Acknowledgments
Source of Funding: Funding support is provided by National Institutes of Health (NIH) T32 CA163177 (to YH, TN, and BE). All other authors report no conflicts of interest.
ABBREVIATIONS
- NIH
National Institutes of Health
- AHRQ
Agency for Healthcare Research and Quality
- PCORI
Patient-centered Outcomes Research Institute
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Yinin Hu, Email: yh9b@virginia.edu.
Brandy L. Edwards, Email: BLE4N@hscmail.mcc.virginia.edu.
Kendall D. Brooks, Email: kdb9fj@virginia.edu.
Timothy Newhook, Email: TN8D@hscmail.mcc.virginia.edu.
References
- 1.Addona T, Polcino M, Silver L, Taub PJ. Leadership trends in plastic surgery. Plast Reconstr Surg. 2009;123:750–753. doi: 10.1097/PRS.0b013e318197ed20. [DOI] [PubMed] [Google Scholar]
- 2.Colaco M, Svider PF, Mauro KM, Eloy JA, Jackson-Rosario I. Is there a relationship between national institutes of health funding and research impact on academic urology? J Urol. 2013;190:999–1003. doi: 10.1016/j.juro.2013.02.3186. [DOI] [PubMed] [Google Scholar]
- 3.Sanfey H. Promotion to professor: A career development resource. Am J Surg. 2010;200:554–557. doi: 10.1016/j.amjsurg.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Sanfey H, Gantt NL. Career development resource: Academic career in surgical education. Am J Surg. 2012;204:126–129. doi: 10.1016/j.amjsurg.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Kotchen TA, Lindquist T, Malik K, Ehrenfeld E. NIH peer review of grant applications for clinical research. JAMA. 2004;291:836–843. doi: 10.1001/jama.291.7.836. [DOI] [PubMed] [Google Scholar]
- 6.Mandel HG, Vesell ES. Declines in funding of NIH R01 research grants. Science. 2006;313:1387–1388. doi: 10.1126/science.313.5792.1387b. [DOI] [PubMed] [Google Scholar]
- 7.LaBeaud AD, McKeating H. The largest drought in american history: Funding for science is drying up. PLoS Negl Trop Dis. 2013;7:e2351. doi: 10.1371/journal.pntd.0002351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Debas HT. Impact of the health care crisis on surgery: Perspective of the dean. Arch Surg. 2001;136:158–160. doi: 10.1001/archsurg.136.2.158. [DOI] [PubMed] [Google Scholar]
- 9.Winslow ER, Bowman MC, Klingensmith ME. Surgeon workhours in the era of limited resident workhours. J Am Coll Surg. 2004;198:111–117. doi: 10.1016/j.jamcollsurg.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 10.Mann M, Tendulkar A, Birger N, Howard C, Ratcliffe MB. National institutes of health funding for surgical research. Ann Surg. 2008;247:217–221. doi: 10.1097/SLA.0b013e3181568e26. [DOI] [PubMed] [Google Scholar]
- 11.Rangel SJ, Efron B, Moss RL. Recent trends in national institutes of health funding of surgical research. Ann Surg. 2002;236:277–86. doi: 10.1097/00000658-200209000-00004. discussion 286–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institutes of Health. Funding: Success rates. 2014;2014 [Google Scholar]
- 13.Bureau of Labor Statistics. CPI inflation calculator. 2014;2014 [Google Scholar]
- 14.National Institutes of Health. The NIH almanac. 2014;2014 [Google Scholar]
- 15.FASEB. Federal funding for biomedical and related life sciences research: FY 2015. 2014 [Google Scholar]
- 16.Association of American Medical Colleges. 2012 physician specialty data book. 2012 [Google Scholar]
- 17.Agnew B. New NIH procedures to shield clinicians from grants bias. The Scientist. 1998;12:1–14. [Google Scholar]
- 18.Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: Continuing challenges in the 21st century. FASEB J. 2014;28:1049–1058. doi: 10.1096/fj.13-241687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mandel HG, Vesell ES. NIH budget grows, but not R01 success rates. Science. 2001;294:54–57. doi: 10.1126/science.294.5540.54. [DOI] [PubMed] [Google Scholar]
- 20.American College of Surgeons Health Policy Research Institute. The surgical workforce in the united states: Profile and recent trends. 2010 [Google Scholar]
- 21.National Institutes of Health. New and early stage investigator policies. 2014;2014 [Google Scholar]
- 22.Englesbe MJ, Sung RS, Segev DL. Young transplant surgeons and NIH funding. Am J Transplant. 2011;11:245–252. doi: 10.1111/j.1600-6143.2010.03314.x. [DOI] [PubMed] [Google Scholar]
- 23.Englesbe MJ, Lynch RJ, Sung RS, Segev DL. Time-trends in publication productivity of young transplant surgeons in the united states. Am J Transplant. 2012;12:772–778. doi: 10.1111/j.1600-6143.2011.03878.x. [DOI] [PubMed] [Google Scholar]
- 24.Adler JT, Chen H. Is endocrine surgery research dying? Am J Transl Res. 2010;2:129–134. [PMC free article] [PubMed] [Google Scholar]
- 25.Ratcliffe MB, Howard C, Mann M, del Nido P. National institutes of health funding for cardiothoracic surgical research. J Thorac Cardiovasc Surg. 2008;136:392–7. doi: 10.1016/j.jtcvs.2008.04.009. discussion 398–9. [DOI] [PubMed] [Google Scholar]
- 26.Souba WW, Wilmore DW. Judging surgical research: How should we evaluate performance and measure value? Ann Surg. 2000;232:32–41. doi: 10.1097/00000658-200007000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Souba WW, Tanabe KK, Gadd MA, Smith BL, Bushman MS. Attitudes and opinions toward surgical research. A survey of surgical residents and their chairpersons. Ann Surg. 1996;223:377–383. doi: 10.1097/00000658-199604000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lessin MS, Klein MD. Does research during general surgery residency correlate with academic pursuits after pediatric surgery residency? J Pediatr Surg. 1995;30:1310–1313. doi: 10.1016/0022-3468(95)90492-1. [DOI] [PubMed] [Google Scholar]
- 29.Robertson CM, Klingensmith ME, Coopersmith CM. Long-term outcomes of performing a postdoctoral research fellowship during general surgery residency. Ann Surg. 2007;245:516–523. doi: 10.1097/01.sla.0000245468.98852.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orandi BJ, Blackburn S, Henke PK. Surgical mentors' and mentees' productivity from 1993 to 2006. Am J Surg. 2011;201:260–265. doi: 10.1016/j.amjsurg.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 31.Jamal MH, Rousseau MC, Hanna WC, Doi SA, Meterissian S, Snell L. Effect of the ACGME duty hours restrictions on surgical residents and faculty: A systematic review. Acad Med. 2011;86:34–42. doi: 10.1097/ACM.0b013e3181ffb264. [DOI] [PubMed] [Google Scholar]
- 32.Agency for Healthcare Research and Quality. Overview of AHRQ budget request by portfolio: Congressional justification, fiscal year 2013. FY 2013 Congressional Justification. 2012 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1: Distribution of common award activities across surgical disciplines in 2003 and 2013.
Supplemental Table 2: National Institutes of Health grants awarded to top five research departments
Geographic distribution of National Institutes of Health funding to departments of surgery