Abstract
Objective
Analysis of short- and long-term effects of rapid response across three different treatments for binge-eating disorder (BED).
Method
In a randomized clinical study comparing interpersonal psychotherapy (IPT), cognitive-behavioral guided self-help (CBTgsh), and behavioral weight loss (BWL) treatment in 205 adults meeting DSM-IV criteria for BED, the predictive value of rapid response, defined as ≥ 70% reduction in binge-eating by week four, was determined for remission from binge-eating and global eating disorder psychopathology at posttreatment, 6-, 12-, 18-, and 24-month follow-up.
Results
Rapid responders in CBTgsh, but not in IPT or BWL, showed significantly greater rates of remission from binge-eating than non-rapid responders, which was sustained over the long term. Rapid and non-rapid responders in IPT and rapid responders in CBTgsh showed a greater remission from binge-eating than non-rapid responders in CBTgsh and BWL. Rapid responders in CBTgsh showed greater remission from binge-eating than rapid responders in BWL. Although rapid responders in all treatments had lower global eating disorder psychopathology than non-rapid responders in the short term, rapid responders in CBTgsh and IPT were more improved than those in BWL and non-rapid responders in each treatment. Rapid responders in BWL did not differ from non-rapid responders in CBTgsh and IPT.
Conclusions
Rapid response is a treatment-specific positive prognostic indicator of sustained remission from binge-eating in CBTgsh. Regarding an evidence-based stepped care model, IPT, equally efficacious for rapid and non-rapid responders, could be investigated as a second-line treatment in case of non-rapid response to first-line CBTgsh.
Keywords: binge-eating disorder, rapid response, cognitive-behavioral therapy, self-help treatment, interpersonal psychotherapy, behavioral weight loss
Binge-eating disorder (BED), characterized by recurrent binge-eating that occurs in the absence of regular compensatory behaviors (American Psychiatric Association [APA], 2013), is associated with increased eating disorder and general psychopathology, psychiatric comorbidity, overweight and obesity, and impaired quality of life. Cognitive-behavioral therapy (CBT) and interpersonal psychotherapy (IPT) are considered standard specialty treatments for BED (Association of the Scientific Medical Societies [AWMF], 2011), leading to large and long-lasting improvements of binge-eating and associated psychopathology (Hilbert et al., 2012), while behavioral weight loss (BWL) treatment yields only moderate effects (Vocks et al., 2010). A recent randomized clinical study showed that both IPT and CBT in guided self-help format (CBTgsh) produced greater improvement of binge-eating over a two-year follow-up than BWL (Wilson, Wilfley, Agras, & Bryson, 2010). While patients with low psychopathology were as well-suited to CBTgsh as IPT, those with high psychopathology improved more with IPT.
Rapid response during the first weeks of treatment is presumably the most well-established predictor of treatment outcome of BED. Rapid response, typically defined as a 65–70% reduction in binge-eating over the first four weeks of treatment, predicted greater remission from binge-eating across various treatment approaches for binge-eating and obesity (e.g., CBT, CBTgsh, BWL, BWLgsh, dialectical behavior therapy [DBT]), with some evidence of stable effects up to one year post-treatment (Grilo, Masheb, & Wilson, 2006; Grilo & Masheb, 2007; Grilo, White, Wilson, Gueorguieva, & Masheb, 2012; Masheb & Grilo, 2007; Safer & Joyce, 2011; Zunker et al., 2010). Effects of rapid response on global eating disorder psychopathology were documented as well (Grilo et al., 2012; Masheb & Grilo, 2007). However, for specialist CBT only, rapid response did not predict these outcomes (Grilo et al., 2012). This study sought to examine the prognostic significance of rapid response for the two core clinical features of BED, binge-eating remission and eating disorder psychopathology over a longer, two-year period in a large randomized trial of CBTgsh, BWL, and for the first time, IPT. It was hypothesized that rapid responders would show a better outcome than non-rapid responders in CBTgsh and BWL, but not in IPT (analogous to specialist CBT); and that rapid responders in CBTgsh, and both rapid and non-rapid responders in IPT, would fare better than non-rapid responders in CBTgsh and patients in BWL.
Methods
Participants
Individuals with BED (N = 205) were recruited through advertising and clinic referrals at two treatment sites (Rutgers University: 100, Washington University: 105). Ethical approval was granted by site-specific Institutional Review Boards. After a telephone screening, eligible participants were invited to a diagnostic visit during which informed consent was obtained and clinical interviews and self-report questionnaires were used in order to ascertain inclusion. Inclusion criteria were: age ≥ 18 years, 27.0 kg/m2 ≤ body mass index (BMI) ≤ 45.0 kg/m2, calculated from measured height and weight, and DSM-IV criteria for BED as established by the Eating Disorder Examination (EDE; Fairburn & Cooper, 1993). Exclusion criteria were: current psychosis, bipolar disorder, active suicidality, alcohol or drug dependence, medical conditions or treatments that would affect weight and/or ability to participate, and insufficient fluency in English. Further methodological detail is given in the main report (Wilson et al., 2010).
Treatments
All treatments were manualized and conducted individually over a 24-week period (see Wilson et al., 2010). BWL treatment was based on the NIDDK Diabetes Prevention Program’s manual (DPP Research Group, 2002) and consisted of 16 individual, weekly, 50-min sessions followed by four sessions at 2-week intervals. The treatment was delivered by master’s level therapists in clinical psychology or nutrition under bi-weekly supervision. CBTgsh, based on Fairburn’s book Overcoming Binge Eating (1995), offered ten, 25-min sessions with a therapist (first session: 1 hour). The first four sessions were weekly, the next two at 2-week intervals, and the last four at 4-week intervals. The treatment was delivered by graduate students without prior experience in CBTgsh or treatment of BED, receiving monthly supervision. IPT, adapted for BED (Wilfley, Frank, Welch, Spurrell, & Rounsaville, 1998), included 19, 50- to 60-min sessions over 24 weeks (first session: 2 hours). The first three sessions were scheduled during the first two weeks, followed by twelve weekly sessions, and ending with four sessions at 2-week intervals. The treatment was delivered by doctoral level therapists under weekly supervision.
Assessments
For this study, assessments at pretreatment, posttreatment, 6-, 12-, 18-, and 24-month follow-up were used. At all timepoints, the semi-structured eating disorder interview EDE (Fairburn & Cooper, 1993), with established reliability and validity, was administered to determine the number of objective binge-eating episodes over the past 28 days (OBEs, defined as consumption of an unusually large amount of food accompanied by a subjective experience of loss of control; APA, 2013). For primary outcome, remission from binge-eating was defined as full abstinence from OBEs (i.e., zero OBEs) in the past 28 days. For secondary outcome, the severity of eating disorder psychopathology was determined by the EDE global score (22 items; 0 to 6, with higher scores indicating greater severity). Interviewers were blind to treatment condition (see Wilson et al., 2010).
Data Analytic Plan
Definition of rapid response
According to Grilo et al. (2006), we initially tried to determine rapid response by calculating receiver operator characteristic (ROC) curves for the predictive value of within-treatment binge-eating (self-reported OBE frequency) regarding posttreatment remission from binge-eating (EDE-determined). We calculated ROC curves for percent change in OBEs and for the total percent change in OBEs over the first four weeks of treatment. Weekly area under the curve (AUC) was calculated and evaluated according to Cohen (small, AUC ≥ .556; medium, ≥ .638; large, ≥ .714). For predictive models, thresholds of AUC > .80 are considered acceptable (Wickens, 2002). The ROC analysis did not reveal any significant result (all ps > .05). AUCs were minimal [range: .493 (SE = .047) – .565 (SE = .046)]. As there was no empirical definition of rapid response possible based on this study’s data, we applied Grilo et al.’s empirically derived definition (2012) of rapid response as a reduction in binge-eating ≥ 70% by the fourth week of treatment for facilitation of comparisons between studies.
Prediction of treatment outcome
Analyses were performed by intent-to-treat and included all randomized participants. First, remission from binge-eating over follow-up (number of time points with remission) was compared in rapid and non-rapid responders in each treatment using an omnibus Kruskal-Wallis H test and pairwise T and χ2 tests for follow-up analyses. In cases of missing data on remission from binge-eating, baseline values were carried forward. To ensure robustness of the results, the analyses were repeated with missing data multiply imputed, creating five completed datasets via an iterative Markov Chain Monte Carlo method. Multiple imputation results were reported only if divergent from baseline value carried forward results. Effect sizes were displayed as r or φ (small, ≥ .10; medium, ≥ .30; large, ≥ .50). Second, for the global eating disorder psychopathology, a mixed linear model analysis of rapid response (rapid vs. non-rapid response; between-subjects), Rapid Response × Treatment (BWL, CBTgsh, IPT; between-subjects), Rapid Response × Time (baseline, posttreatment, 6-, 12-, 18-, 24-month follow-up; within-subjects), and Rapid Response × Treatment × Time was conducted. Participants were hierarchically nested within time and treated as a random factor. As hierarchical linear modeling allows data from participants with missing data at some, but not all, time points to remain in the analyses, data from all randomized participants were used without imputation. All analyses were performed with SPSS 20.0. A two-tailed significance level of α < 0.05 was applied to all statistical tests.
Results
Defining rapid response as a reduction in binge-eating ≥ 70% by the fourth week of treatment, rapid response was identified in 70.7% of study participants (145/205). Rapid response rates in BWL (73.4%; 47/64), CBTgsh (74.2%; 49/66), and IPT (65.3%; 49/75) did not differ [χ2(2, N = 205) = 1.68, p = .433, φ = .090].
Rapid Response and Remission from Binge-eating
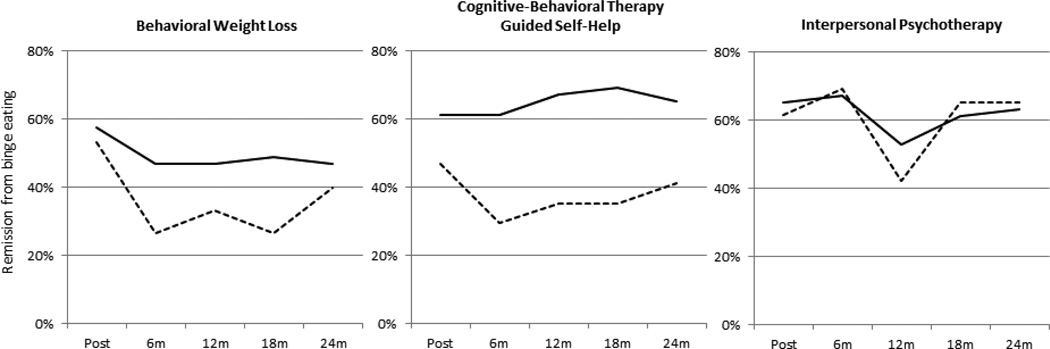
Following significance of the omnibus Kruskal-Wallis H test [H(5, N = 205) = 17.34, p = .004], pairwise comparisons revealed greater remission from binge-eating in rapid versus non-rapid responders in CBTgsh (p = .01), but not in IPT or BWL (both ps > .05) (Figure 1, Table S1). Rapid and non-rapid responders in IPT, and rapid responders in CBTgsh, showed a greater remission from binge-eating than non-rapid responders in CBTgsh and BWL (all ps < .05). Rapid responders in CBTgsh (p = .027) and, at a trend level, rapid responders in IPT (p = .061), showed greater remission from binge-eating than rapid responders in BWL. Regarding time course, rapid responders in CBTgsh showed significantly greater rates of remission from binge-eating at 6-, 12-, and 18-month follow-up, and at a trend level, at 24-month follow-up than non-rapid responders [posttreatment: χ2(1, N = 66) = 1.04, p = .309, φ = .125; 6 months χ2(1) = 5.13, p = .024, φ = .279; 12 months χ2(1) = 5.36, p = .021, φ = .285; 18 months χ2(1) = 6.15, p = .013, φ = .305; 24 months χ2(1) = 3.04, p = .081, φ = .215; small-to-medium effects]. Overall, the mean differences in rates of remission from binge-eating between rapid responders minus those from non-rapid responders were 27.3% in CBTgsh, 13.4% in BWL, and 1.3% in IPT (Figure 1).1
Figure 1.
Rates of remission from binge-eating over follow-up by rapid response and treatment. Rapid response indicated by solid lines; non-rapid response by dotted lines. Rapid response defined as a reduction in binge-eating ≥ 70% by the fourth week of treatment. Remission from binge-eating defined as zero episodes of binge-eating over the past 28 days using the Eating Disorder Examination. Posttreatment, 6-, 12-, 18-, and 24-month follow-up assessments.
Rapid Response and Global Eating Disorder Psychopathology
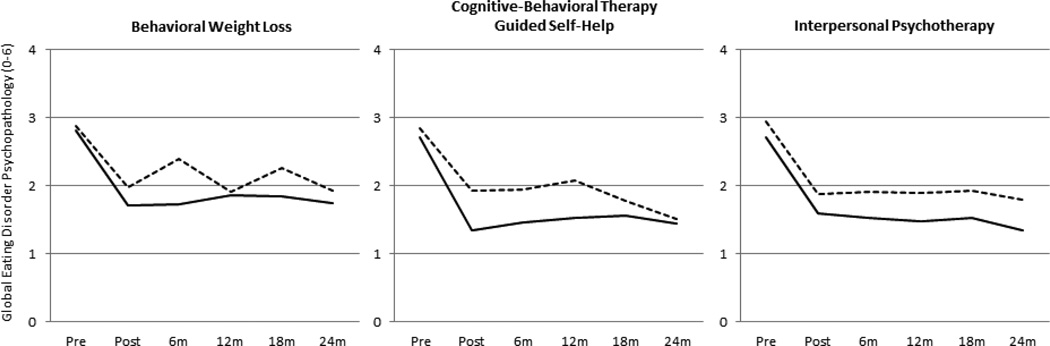
The mixed linear model analysis of the global EDE score revealed variations by rapid response [F(1, 909) = 21.72, p < .001], modified by interactions with treatment [F(4, 917) = 4.03, p = .003] and time [F(10, 297) = 29.61, p < .001]. The three-way interaction was not significant [F(20, 301) = 0.36, p = .996]. According to follow-up tests, rapid responders in each treatment condition had lower global eating disorder psychopathology than non-rapid responders (all ps < .05), which amounted on average to 0.35 EDE units less (Figure 2, Table S2). Across treatments, rapid response effects on global eating disorder psychopathology were observed from posttreatment through 6-month follow-up (both ps < .05) and, at a trend level, at 12- and 18-month follow-up (both ps < .10), but were no longer significant at 24-month follow-up (p > .10). Rapid responders in CBTgsh and IPT achieved lower eating disorder psychopathology than those in BWL and than non-rapid responders in each treatment (all ps < .05). Rapid responders in BWL did not differ from non-rapid responders in CBTgsh and IPT, and there were no differences by treatment in non-rapid responders (all ps > .05).
Figure 2.
Global eating disorder psychopathology over follow-up by rapid response and treatment. Rapid response indicated by solid lines; non-rapid response by dotted lines. Rapid response defined as a reduction in binge-eating ≥ 70% by the fourth week of treatment. Global eating disorder psychopathology assessed as the Global Score of the Eating Disorder Examination (0–6, with higher scores indicating greater severity). Pretreatment, posttreatment, 6-, 12-, 18-, and 24-month follow-up assessments.
Discussion
Based on a large randomized clinical trial of BED, this study examined the short- and long-term prognostic significance of rapid response, defined as a reduction in binge-eating ≥ 70% by the fourth week of treatment, in BWL, CBTgsh, and for the first time, IPT. We found evidence for a treatment-specific predictive value of rapid response. Rapid responders in CBTgsh showed significantly greater rates of remission from binge-eating than non-rapid responders, 6 to 18 months following treatment. This rapid response effect amounted to a 27.3% greater rate of remission from binge-eating and can thus be considered clinically relevant. In contrast, rates of remission in IPT and BWL did not differ significantly by rapid response. Rapid and non-rapid responders in IPT, and rapid responders in CBTgsh, revealed a greater remission from binge-eating than non-rapid responders in CBTgsh and BWL. In addition, rapid responders in CBTgsh showed a greater remission than those in BWL.
Demonstrating the treatment-specificity of rapid response for CBTgsh, the results extend previous short-term findings on rapid response and suggestions of a treatment-specific time course in individual CBTgsh (Grilo & Masheb, 2007; Masheb & Grilo, 2007). The absence of differences between rapid and non-rapid responders in IPT, however, is inconsistent with effects in other specialist treatments, such as CBT leading to short-term rapid response (Grilo et al., 2012) and DBT leading to short- and long-term rapid response (Safer & Joyce, 2011). Unlike IPT, which was offered individually, CBT and DBT were conducted in groups. Therapists in individual treatment may be better able to prevent adverse effects of non-rapid response than those in group treatment possibly due to greater intensity or treatment personalization. In line with this interpretation, individual BWL did not produce a significant rapid response effect whereas group BWL did (Grilo et al., 2012). CBTgsh, although individual, was the least intense treatment in this study, potentially explaining its rapid response effect. For BWL and CBTgsh, rates of rapid response were higher than in previous studies (BWL: 73.4% vs. 47% [Grilo et al., 2012]; CBTgsh: 74.2% vs. 42% to 62.2% [Grilo & Masheb, 2007; Masheb & Grilo, 2007]). For IPT, they were comparable or higher (65.3% vs. 67% [CBT; Grilo et al., 2012] or 56% [DBT; Safer & Joyce, 2011]). This could also be related to the individual format (BWL, IPT) or more extended individual treatment (CBTgsh).
The pattern for global eating disorder psychopathology was similar to that of binge-eating remission: In all treatments, rapid responders had lower global eating disorder psychopathology than non-rapid responders, with rapid responders in CBTgsh and IPT showing more improvement than those in BWL and more than non-rapid responders in each treatment. Rapid responders in BWL did not differ from non-rapid responders in CBTgsh and IPT. The fact that rapid responders in all treatment conditions had lower global eating disorder psychopathology than non-rapid responders, especially at posttreatment and 6-month follow-up, and, at a trend level, at 12- and 18-month follow-up, is generally consistent with most of the literature (Grilo et al., 2012; Masheb & Grilo, 2007; Safer & Joyce, 2011).
An important difference between this and previous studies is that Grilo and colleagues used daily self-monitoring of binge-eating that was reviewed by therapists at each session (Grilo et al., 2006; Grilo & Masheb, 2007; Grilo et al., 2012; Masheb & Grilo, 2007), while this study used retrospective recall of binge-eating during the previous week of treatment to define rapid response. This may explain why an empirical threshold for the within-treatment reduction of binge-eating was not derived based on this study’s data, and the overall rapid response effects were small when applying the criterion of a reduction in binge-eating ≥ 70%. Another study that used binge recall diaries also found a relatively small effect size of prediction and no evidence for a rapid response effect when using the same criterion (Zunker et al., 2010). In general, retrospective recall, e.g., as performed in the self-report form of the EDE, has been found to have acceptable convergence with interview (EDE) and self-monitoring, especially to assess OBEs (Grilo, Masheb, & Wilson, 2001). Self-monitoring reviewed by therapists, as done by Grilo and colleagues, may have increased validity further, although this assessment was not “blinded” and was thus confounded with treatment. In contrast, self-monitoring by patients did not lead to satisfactory sensitivity and specificity when empirically defining rapid response (Safer et al., 2011). Thus, the definition of rapid response likely depends on measurement. Further research is necessary on the reliable measurement of binge-eating during treatment.
Clinically, the results may inform a model of evidence-based stepped care to be further investigated, according to which CBTgsh (AWMF, 2011), rather than BWL (Grilo et al., 2012), represents a low-cost, low-intensity, first-line treatment, and IPT, equally efficacious for rapid and non-rapid responders, (or another evidence-based treatment) represents an alternative specialist approach in case of non-rapid response. Grilo et al. (2012) had recommended BWL as first-line treatment because of superior binge-eating remission in BWL rapid responders versus non-rapid responders and of superior weight loss outcome in BWL than in CBT. This was, however, not the focus of our study. This brief report concentrated on the core clinical features of BED, i.e. binge-eating remission and the associated global eating disorder psychopathology. Based on this study’s results, monitoring rapid response may offer the advantage of identifying CBTgsh patients early who are not likely to benefit from this treatment in order to offer an alternative treatment. This monitoring could be conducted in addition to evaluating pretreatment moderators such as eating disorder psychopathology and self-esteem (Wilson et al., 2010) that showed no significant overlap with rapid response. Generally, pretreatment patient characteristics of rapid response have proven elusive (Grilo et al., 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007; Safer & Joyce, 2011; Zunker et al., 2010). An examination of associated within-treatment changes could offer further insight into proximal predictors or correlates of rapid response in BED.
Regarding a potential matching of non-rapid responders to alternative treatments, it is important to note that neither in this nor prior studies was the effect size of rapid response sufficiently high to justify its use as an algorithm for evidence-based clinical decision-making. Ecological momentary assessment for concurrent recording of binge-eating, smartphone- or Internet-based measurement, and training and instructions on self-monitoring may provide research avenues to increase the diagnostic validity of rapid response for individual treatment decisions. Finally, future research should determine interventions suited to achieve and improve early therapeutic gains, for example, the use of CBTgsh tailored to binge-eating in BED, the inclusion of novel interventions (e.g., cue exposure), and the identification of the optimal dose, type, and training of guidance for enhanced rapid response.
Supplementary Material
Public Health Significance Statements.
This study provides evidence for rapid response as a treatment-specific positive prognostic indicator of long-term remission in cognitive-behavioral guided self-help (CBTgsh), a low-intensity, low-cost treatment for binge-eating disorder.
In contrast, interpersonal psychotherapy (IPT), a specialty treatment, was comparably efficacious for both rapid and non-rapid responders, while non-rapid responders in CBTgsh and rapid and non-rapid responders in behavioral weight loss treatment showed the lowest remission rates.
Monitoring rapid response can provide guidance regarding a switch from a low-intensity treatment (e.g., CBTgsh) to a more intensive intervention (e.g., IPT) in order to promote successful outcome in binge-eating disorder.
Acknowledgments
This research was supported by National Institute of Mental Health research grants R01063863 (Agras), R01064153 (Wilfley), K24070446 (Wilfley), and R01063862 (Wilson), and by grant 01EO1001 from the German Federal Ministry of Education and Research (Hilbert).
Footnotes
An additional analysis served to evaluate the association between rapid response and the psychopathological moderator identified in the main report (Wilson et al., 2010). The moderator of global eating disorder psychopathology/self-esteem indicated that CBTgsh was as well-suited as IPT for patients with high global eating disorder psychopathology and high self-esteem or for those with low global eating disorder psychopathology, while IPT was superior for patients with high global eating disorder psychopathology and low self-esteem. BWL patients fared worse if they had low self-esteem, especially in combination with high global eating disorder psychopathology, than if they had high self-esteem. φ coefficients on the association between rapid response and the moderator variables were low and non-significant (median-split variables; self-esteem and EDE global score: φ = .143; self-esteem: φ = .107; EDE global score: φ = .089; all ps > .05).
Contributor Information
Anja Hilbert, University of Leipzig Medical Center.
Thomas Hildebrandt, Icahn School of Medicine at Mount Sinai.
W. Stewart Agras, Stanford University School of Medicine.
Denise E. Wilfley, Washington University School of Medicine
G. Terence Wilson, The State University of New Jersey.
References
- American Psychiatric Association. DSM-5: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Association of the Scientific Medical Societies [Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften, AWMF] [Retrieved May 16, 2013];Leitlinie „Diagnostik und Therapie von Essstörungen“. 2011 from http://www.awmf.org/leitlinien/detail/ll/051-026.html. [Google Scholar]
- Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. http://dx.doi.org/10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment, and treatment. 12th ed. New York, NY: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Grilo CM, Masheb RM. Rapid response predicts binge eating and weight loss in binge eating disorder: findings from a controlled trial of orlistat with guided self-help cognitive behavioral therapy. Behaviour Research and Therapy. 2007;45(11):2537–2550. doi: 10.1016/j.brat.2007.05.010. http://dx.doi.org/10.1016/j.brat.2007.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69(2):317–322. doi: 10.1037//0022-006x.69.2.317. http://dx.doi.org/10.1037/0022-006X.69.2.317. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. Rapid response to treatment for binge eating disorder. Journal of Consulting and Clinical Psychology. 2006;74(3):602–613. doi: 10.1037/0022-006X.74.3.602. http://dx.doi.org/10.1037/0022-006X.74.3.602. [DOI] [PubMed] [Google Scholar]
- Grilo CM, White MA, Wilson GT, Gueorguieva R, Masheb RM. Rapid response predicts 12-month post-treatment outcomes in binge-eating disorder: Theoretical and clinical implications. Psychological Medicine. 2012;42(4):807–817. doi: 10.1017/S0033291711001875. http://dx.doi.org/10.1017/s0033291711001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A, Bishop ME, Stein RI, Tanofsky-Kraff M, Swenson AK, Welch RR, Wilfley DE. Long-term efficacy of psychological treatments for binge eating disorder. British Journal of Psychiatry. 2012;200(3):232–237. doi: 10.1192/bjp.bp.110.089664. http://dx.doi.org/10.1192/bjp.bp.110.089664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacovino JM, Gredysa DM, Altman M, Wilfley DE, editors. Psychological treatments for binge eating disorder. Current Psychiatry Reports. 2012;14(4):432–446. doi: 10.1007/s11920-012-0277-8. http://dx.doi.org/10.1007/s11920-012-0277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM, editors. Rapid response predicts treatment outcomes in binge eating disorder: implications for stepped care. Journal of Consulting and Clinical Psychology. 2007;75(4):639–644. doi: 10.1037/0022-006X.75.4.639. http://dx.doi.org/10.1037/0022-006X.75.4.639. [DOI] [PubMed] [Google Scholar]
- Safer DL, Joyce EE, editors. Does rapid response to two group psychotherapies for binge eating disorder predict abstinence? Behaviour Research and Therapy. 2011;49(5):339–345. doi: 10.1016/j.brat.2011.03.001. http://dx.doi.org/10.1016/j.brat.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vocks S, Tuschen-Caffier B, Pietrowsky R, Rustenbach SJ, Kersting A, Herpertz S. Meta-analysis of the effectiveness of psychological and pharmacological treatments for binge eating disorder. International Journal of Eating Disorders. 2010;43(3):205–217. doi: 10.1002/eat.20696. http://dx.doi.org/10.1002/eat.20696. [DOI] [PubMed] [Google Scholar]
- Wickens TD. Elementary signal detection theory. New York, NY: Oxford University Press; 2002. [Google Scholar]
- Wilfley DE, Frank MA, Welch R, Spurrell EB, Rounsaville BJ. Adapting interpersonal psychotherapy to a group format (IPT-G) for binge eating disorder: Toward a model for adapting empirically supported treatments. Psychotherapy Research. 1998;8(4):379–391. http://dx.doi.org/10.1080/10503309812331332477. [Google Scholar]
- Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Archives of General Psychiatry. 2010;67(1):94–101. doi: 10.1001/archgenpsychiatry.2009.170. http://dx.doi.org/10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zunker C, Peterson CB, Cao L, Mitchell JE, Wonderlich SA, Crow S, Crosby RD. A receiver operator characteristics analysis of treatment outcome in binge eating disorder to identify patterns of rapid response. Behaviour Research and Therapy. 2010;48(12):1227–1231. doi: 10.1016/j.brat.2010.08.007. http://dx.doi.org/10.1016/j.brat.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.