Abstract
Objective
Computer-based interventions aimed at reducing college student drinking have shown positive effects. This paper compares differences in effects of computer-based personalized normative feedback (PNF) interventions based on delivery modality (in-person vs. remotely) across six previously evaluated studies with similar content.
Method
Three studies included evaluations of a computer-based PNF intervention where baseline and intervention procedures took place inside a laboratory setting; three separate studies included evaluations of the same intervention where participants completed the procedures remotely over the web. Thus, we tested for differences in intervention efficacy by delivery modality. Outcomes included drinks per week, drinking-related consequences, and the putative intervention mechanism, perceived drinking norms.
Results
Evidence from hierarchical linear models indicated that computer-based interventions are less effective at reducing drinking and related consequences when delivered remotely than when delivered in-person.
Conclusion
The advantages of interventions delivered remotely are not without cost. Suggestions for why remote computer-based interventions may be less effective are discussed.
Keywords: alcohol, interventions, delivery method, web-based, personalized normative feedback
Alcohol consumption in college is prevalent, with six in ten students reporting having been drunk in the past year and four in ten reporting having been drunk in the past month (Johnston, O’Malley, Bachman, & Schulenberg, 2012). Many students who drink experience negative alcohol-related consequences; 20% of college students report experiencing five or more different problems as a function of their drinking (Wechsler et al., 2002). Moreover, heavy drinking among college students can have a significant impact on academic performance, social relationships, and mental and physical health (Dunn et al., 2002; Geisner et al., 2004; Hingson, Edwards, Heeren, & Rosenbloom, 2009; Kaysen et al., 2006; Wechsler et al., 2000; Wechsler & Nelson, 2008).
Computer-delivered Interventions for Reducing Heavy Drinking
Significant efforts have identified efficacious individually-focused interventions for addressing problematic college drinking. In recent years, there has been an increase in the use of computer-delivered interventions targeting college student drinking. Several systematic reviews and meta-analyses have been conducted which focus on computer-delivered alcohol interventions (e.g., Bewick, Trusler, Mulhern, Barkham, & Hill, 2008; Carey, Scott-Sheldon, Elliott, Bolles, & Carey, 2009; Elliott, Carey, & Bolles, 2008; Portnoy, Scott-Sheldon, Johnson, & Carey, 2008; Rooke, Thorsteinsson, Karpin, Copelan, & Allsop, 2010; White et al., 2010). Reviews have generally found small but significant effects of these interventions, noting that effects largely depend on intervention content and comparison group.
Intervention Delivery Modality
There is great potential of computer-based interventions, which can be administered either in-person or remotely via the internet. Technology continues to advance, allowing for more flexibility and customization in the content and delivery of electronically-administered interventions (Cunningham, Kypri, & McCambridge, 2011; Cunningham, Khadjesari, Bewick, & Riper, 2010; Cunningham, Selby, Kypri, & Humphreys, 2006; Kypri, Saunders, & Gallagher, 2003; Walters & Neighbors, 2011; Walters, Miller, & Chiauzzi, 2005). As technology changes, it seems likely that telemedicine approaches and interactions among providers, caregivers, and patients will increasingly integrate computer interfaces. It is important to note that computer-delivered and web-based interventions are not synonymous. Computer-delivered interventions may occur in health care facilities, student affairs offices, or other research settings where participants receive the intervention on a computer at a designated location and often a designated time. Whereas increased effort is required to attend a session, distractions are typically minimized during the assessment and intervention. In contrast, remote interventions may occur on a computer or internet-capable device (e.g., tablet, smartphone) at a time and location chosen by the participant. Remote interventions provide increased flexibility, but are also accompanied by potential distractibility.
Some studies have examined differential efficacy of therapist-delivered brief alcohol interventions compared with computer-delivered interventions or interventions that include only printed feedback, with results supporting stronger efficacy for therapist-delivered interventions (e.g., Carey, Carey, Henson, Maisto, & DeMartini, 2011; Walters, Vader, Harris, Field, & Jouriles, 2009). A recent meta-analysis (Carey, Scott-Sheldon, Elliott, Garey, & Carey, 2012) reviewed studies examining in-person and computer-delivered interventions, although in-person and remote delivery methods were collapsed into the latter category. Results indicated that while participants in both kinds of interventions drank less and reported fewer problems at short-term follow-up, only participants in the in-person interventions continued to drink less at intermediate and long-term follow-ups. Direct comparisons between in-person and computer-delivered interventions favored those occurring in-person, but variability within computer-delivered interventions was considerable and authors noted the need for further research examining determinants of efficacy within computer-delivered interventions.
The current research extends the Carey et al. (2012) meta-analysis by evaluating whether efficacy of computer-delivered interventions differs according to the delivery modality (i.e., in-person or remote). We offer an examination of computer-delivered interventions for reducing college student drinking using a widely successful paradigm, personalized normative feedback (PNF). PNF was chosen for this research because it has been found efficacious as a stand-alone intervention (Larimer & Cronce, 2007), and has been delivered via computer both remotely and in-person.
Personalized Normative Feedback (PNF)
One promising strategy in reducing college student drinking involves reducing overestimated descriptive drinking normative perceptions. Peer descriptive drinking norms are among the strongest influences on students’ personal drinking, stronger than the influence of parents, advisors, and faculty (Perkins, 2002). Given findings that students grossly overestimate the drinking of other students and that these normative perceptions are strongly predictive of drinking, reducing overestimated descriptive normative misperceptions has become a prominent focus of many college drinking intervention studies with considerable success (for reviews see Carey et al., 2007; Larimer & Cronce, 2007; Lewis & Neighbors, 2006; Miller et al., 2013; Walters & Neighbors, 2005). Furthermore, changes in perceived norms have been consistently found to mediate intervention efficacy (e.g., Lewis & Neighbors, 2007; Neighbors et al., 2004, 2006). Of interest to the current research is that a large randomized trial evaluating remote-delivered PNF found that repeated administration of gender-specific PNF had a significant effect over a two-year follow-up period, but the effect size was considerably smaller (d=.16) than previous in-lab studies (Neighbors et al., 2010).
Current Research
The potential advantages of remote computer-delivered interventions include relatively low cost due to reduced need for physical space and staff time, anonymity, and immediate and available access from any location with an internet connection (Cunningham et al., 2011). However, the overall advantages of remote computer-delivered interventions relative to in-person computer-delivered interventions cannot be considered independently from their relative effectiveness. Lower cost, wider reach, and greater flexibility are only valuable to the extent that they are not offset by relatively lower effectiveness. Thus, the purpose of the present research was to identify whether computer-delivered intervention efficacy differs by delivery modality. To address this question, we focused on six studies evaluating computer-delivered PNF, three of which were delivered in-person and three which were delivered remotely. Based on previous research, we tentatively expected larger effects for in-person delivery on drinking, alcohol-related consequences, and the putative intervention mechanism (i.e., changes in perceived norms).
Method
General PNF Procedure Overview
This research utilizes data from six studies, chosen based on consistency of presentation of the personalized normative feedback and type of control condition. All participants were undergraduate students who reported one or more heavy drinking event (5+/4+ drinks in one sitting for men/women, respectively) in the previous month. All procedures evaluate the same intervention: PNF using a typical student as the normative referent, compared to an assessment-only control. Overall, the studies are comparable with the exception that three of the studies (Studies 1–3) were delivered in-person and three (Studies 4–6) were delivered remotely. All studies were completed on a computer, took approximately 45 minutes to complete, and did not involve any therapist involvement. For in-person studies, staff interactions were limited to introductions, obtaining consent, and thanking participants upon completion. In-person participants completed the assessment and interventions in individual testing rooms.
All studies examine the baseline assessment with immediate provision of PNF and the follow-up assessments, which range from one month to two years, depending on the specifics of the study. The studies vary in the levels of complexity of their design, but only data for the PNF and assessment-only control conditions are included in the present analyses. Details surrounding each specific study and sample are described in Table 1. Follow-up completion rates did not differ for in-person (83%) versus remote (86%) interventions, χ2(1)=2.37, p=.124. Collateral reports were not obtained in any of the studies.
Table 1.
Sample characteristics and design for each of the six studies.
| Study | N | % Female | Age M(SD) | Race | BL DPW M(SD) | BL RAPI M(SD) | Authors | Compensation | Follow-up Interval |
|---|---|---|---|---|---|---|---|---|---|
|
In-Person Computer-delivered PNF Interventions
| |||||||||
| 1 | 252 | 59% | 18.53 (1.24) | 79.5% Caucasian 13.7% Asian 6.8% Other |
11.55 (9.37) | 7.25 (6.92) | Neighbors, Lewis, & Larimer, 2004 | Baseline: Extra credit 3-month: $15 6-month: $25 |
3-month (n=198) 6-month (n=207) |
| 2 | 214 | 56% | 19.67 (2.02) | 98.0% Caucasian 2.0% Other |
13.57 (11.74) | 7.87 (7.52) | Neighbors, Lewis, Bergstrom, & Larimer, 2006 | All timepoints: Extra credit | 2-month (n=185) |
| 3 | 117 | 56% | 20.10 (1.8) | 97.3% Caucasian 2.7% Other |
11.73 (9.68) | 5.26 (6.06) | Lewis & Neighbors, 2007 | All timepoints: Extra credit | 1-month (n=104) |
|
| |||||||||
|
Remote Computer-delivered PNF Interventions
| |||||||||
| 4 | 601 | 52% | 18.80 (4.53) | 95.1% Caucasian 0.7% Asian 4.2% Other |
5.53 (9.08) | 3.22 (6.69) | Grant U01AA014742 | All timepoints: $50 | 6-month (n=500) |
| 5 | 491 | 59% | 18.14 (.46) | 65.3% Caucasian 24.2% Asian 10.5% Other |
11.65 (10.81) | 6.91 (7.75) | Neighbors et al., 2010 | All timepoints: $25 | 6-month (n=454) 12-month (n=428) 18-month (n=411) 24-month (n=404) |
| 6 | 371 | 57% | 19.92 (1.30) | 75.7% Caucasian 24.3% Other |
11.48 (10.52) | 6.47 (7.43) | LaBrie et al., 2013 | Baseline: $25 Follow-ups: $30 |
1-month (n=307) 3-month (n=293) 6-month (n=283) |
Note.
BL = Baseline; DPW = Drinks per week; RAPI = Rutgers Alcohol Problems Index (alcohol-related consequences).
Measures
Drinks per week
The Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985) was used to assess quantity and frequency of alcohol consumption. Participants were asked to “Consider a typical week during the last three months. How much alcohol, on average (measured in number of drinks), do you drink on each day of a typical week?” Responses consisted of the typical number of drinks participants reported consuming on each day of the week. A weekly drinking variable was calculated by summing responses. The number of drinks per week has previously been shown to be a reliable index of alcohol use among college students relative to other drinking indices (Borsari, Neal, Collins, & Carey, 2001).
Alcohol-related consequences
A modified version of the Rutgers Alcohol Problems Index (RAPI; White & Labouvie, 1989) assessed how often 23 alcohol-related problems have occurred over the previous three months. The RAPI was modified to include two additional items (i.e., “drove after having two drinks” and “drove after having four drinks”). Response options for each item were on a 5-point scale (0=never; 1=1 to 2 times; 2=3 to 5 times; 3=6 to 10 times; 4=more than 10 times). Scores were calculated by summing the 25 items.
Perceived norms for drinks per week
Perceived descriptive norms were measured by the Drinking Norms Rating Form (DNRF; Baer et al., 1991). The DNRF measures perceived typical weekly drinking in which participants report the average number of standard drinks they think the typical student at their university consumes for each day of the week over the previous three months. Scores are summed for each day of the week and represent the average number of drinks perceived to be consumed by the typical student each week. The DNRF is a common measure of perceived drinking norms and has shown good concurrent and prospective validity (Neighbors, Dillard, Lewis, Bergstrom, & Neil, 2006).
Results
Baseline Differences
Baseline drinks per week and alcohol-related consequences are presented by study in Table 1. At baseline, participants who completed the survey in-person reported higher levels of drinks per week (M=12.33, SD=10.39) than participants who completed the survey remotely (M=9.16, SD=10.62), t(1995)=−6.15, p<.001. Similarly, in-person participants also reported more consequences at baseline (M=7.09, SD=7.04) than remote participants (M=5.37, SD=7.35), t(1990)=−4.80, p<.001. Thus, the respective baseline drinking variable was included as a covariate in all analyses.
Intervention Effects
Alcohol consumption (drinks per week)
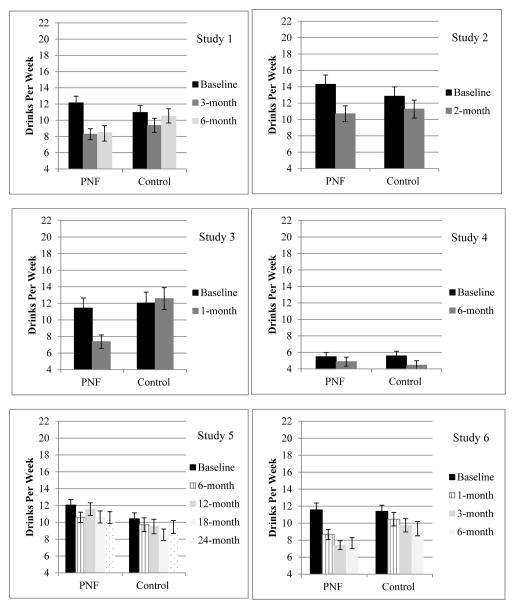
We were interested in evaluating drinks per week at the first follow-up as a function of intervention condition, controlling for baseline drinks per week. Means and standard errors for drinks per week across all studies are presented in Figure 1. Results with tests of significance and effect sizes are presented in Table 2. All three in-person computer-based interventions showed significant PNF intervention effects on reducing drinks per week. Only one remote intervention (Study 6) showed significant intervention effects.
Figure 1.
Means and standard errors for drinks per week for Studies 1–6.
Table 2.
Effect sizes (Cohen’s d) and test statistics for the intervention effect on drinking at the first follow-up across Studies 1–6 with weighted average effect sizes based on delivery modality.
| Outcome | Delivery Modality | Study | t | Effect Size (d) | CI (d) | Weighted Average |
|---|---|---|---|---|---|---|
| Drinks per week | In-person | 1 | −2.27* | −.33 | (−.61, −.04) | −.43 |
| 2 | −2.05* | −.30 | (−.60, −.01) | |||
| 3 | −4.26*** | −.85 | (−1.24, −.45) | |||
|
| ||||||
| Remote | 4 | 0.58 | .05 | (−.12, .23) | −.04 | |
| 5 | 0.08 | .01 | (−.18, .19) | |||
| 6 | −2.47* | −.28 | (−.51, −.06) | |||
|
| ||||||
| Alcohol-related consequences | In-person | 1 | −1.86† | −.27 | (−.55, .02) | −.23 |
| 2 | −1.64 | −.24 | (−.54, .05) | |||
| 3 | −0.69 | −.14 | (−.53, .26) | |||
|
| ||||||
| Remote | 4 | 1.20 | .11 | (−.06, .28) | .08 | |
| 5 | 1.47 | .14 | (−.05, .32) | |||
| 6 | −0.53 | −.06 | (−.29, .16) | |||
|
| ||||||
| Perceived norms for drinks per week | In-person | 1 | −4.20*** | −.61 | (−.89, −.32) | −.81 |
| 2 | −5.75*** | −.85 | (−1.15, −.56) | |||
| 3 | −5.53*** | −1.10 | (−1.50, −.71) | |||
|
| ||||||
| Remote | 4 | −3.53*** | −.32 | (−.43, −.14) | −.36 | |
| 5 | −3.33*** | −.31 | (−.50, −.13) | |||
| 6 | −4.18*** | −.49 | (−.73, −.26) | |||
Note.
p < .10
p < .05
p < .01
p < .001
Hierarchical linear modeling (HLM; Raudenbush, 2004) was also used to comprehensively evaluate the effects of in-person versus web-delivered PNF. Data from all timepoints for all studies were included in the analysis. This included one follow-up timepoint in Studies 2–4, two follow-up timepoints in Study 1, three follow-up time-points in Study 6, and four follow-up timepoints in Study 5, yielding 4513 timepoints and 2046 individuals. Individuals (Level 1) were nested within study (Level 2). The number of drinks per week at follow-up was specified as the Level-1 outcome. Baseline drinks per week, length of time since baseline, and condition were specified as Level-1 covariates. Study was included as a Level-2 covariate, and the in-lab versus remote delivery modality variable was included as a Level-2 predictor of the Level-1 condition slope.
Estimates and respective tests are presented in Table 3. Results from main effects indicated a significant intervention effect across all six studies, t(1952)=−2.04, p=.041. However, this was contingent upon a significant cross-level interaction indicating that the intervention effect varied as a function of delivery modality, t(1951)=−2.70, p=.007, suggesting that the intervention showed stronger effects when delivered in-person. Thus, results suggested that across six studies using the same intervention, in-person feedback was more effective than remote feedback in reducing drinks per week.
Table 3.
HLM results for delivery modality as a moderator of PNF efficacy on outcomes.
| Outcome | Step | Effect | b | SE(b) | t | p |
|---|---|---|---|---|---|---|
| Drinks per week | 1 | Baseline Drinks per Week | .584 | .017 | 33.39 | <.001 |
| Time | −.008 | .020 | −.38 | .702 | ||
| Feedback | −.734 | .359 | −2.04 | .041 | ||
| 2 | Modality × Feedback | −2.185 | .811 | −2.70 | .007 | |
|
| ||||||
| Alcohol-related consequences | 1 | Baseline RAPI | .555 | .028 | 20.09 | <.001 |
| Baseline Drinks per Week | .094 | .019 | 4.96 | <.001 | ||
| Time | −.009 | .020 | −.46 | .646 | ||
| Feedback | .406 | .342 | 1.19 | .236 | ||
| 2 | Modality × Feedback | −1.749 | .769 | −2.28 | .023 | |
|
| ||||||
| Perceived norms for drinks per week | 1 | Baseline Perceived Norms | .298 | .017 | 17.87 | <.001 |
| Time | −.110 | .021 | −5.24 | <.001 | ||
| Feedback | −2.943 | .361 | −8.15 | <.001 | ||
| 2 | Modality × Feedback | −1.231 | .819 | −1.50 | .133 | |
Note. Step 1 indicates a model with only main effects entered, whereas Step 2 indicates a full model with main effects and the delivery modality × feedback interaction.
Alcohol-related consequences
We were also interested in whether similar differences might be evident for alcohol-related negative consequences, controlling for consumption (drinks per week). As can be seen in Table 2, although there were no significant differences at first follow-up on consequences in any of the studies, one of the in-person studies (Study 1) showed a marginal intervention effect. Effect sizes for the in-person studies ranged from d=−.14 to −.27, whereas effect sizes for the remote studies ranged from d=−.06 to .14.
The same HLM analysis approach was used in predicting alcohol-related consequences. Estimates and respective tests are presented in Table 3. Consistent with drinks per week, a significant cross-level interaction between condition and delivery approach emerged, suggesting that intervention effects on alcohol-related problems were stronger for in-person versus remotely-delivered interventions, t(1649)=−2.28, p=.023.
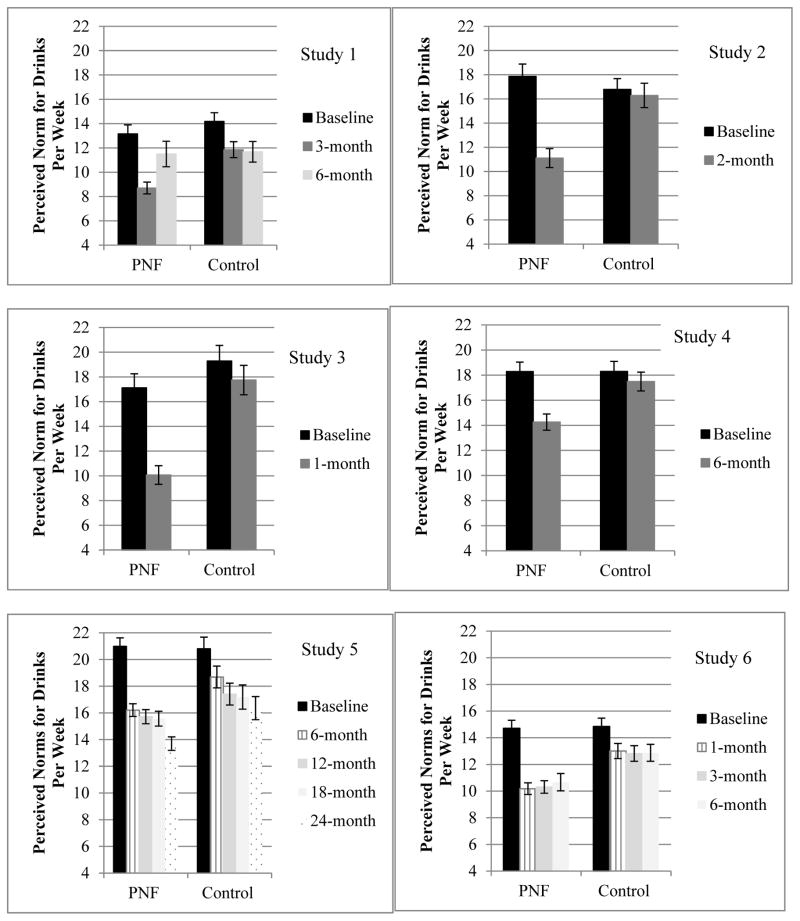
Perceived drinking norms
A final question of interest was to evaluate the putative PNF mediator (perceived norms for drinks per week) at follow-up as a function of intervention controlling for baseline perceived norms. Means and standard errors across all studies are presented in Figure 2. Results with tests of significance and effect sizes for the intervention at first follow-up are provided in Table 2. The PNF group reported lower perceived drinking norms at first follow-up in all six studies (p<.001).
Figure 2.
Means and standard errors for perceived norms for drinks per week for Studies 1–6.
HLM was again used to evaluate the effects of in-person versus remote PNF on perceived norms for drinks per week. Estimates and respective tests are presented in Table 3. Results from main effects indicated an overall feedback effect showing decreased perceived norms in the PNF group, t(1915)=−8.15, p<.001. However, the cross-level interaction between condition and delivery approach was not significant, t(1914)=−1.50, p=.133. Thus, results suggested that remote web-based feedback was not less effective than in-person feedback in reductions of perceived drinking norms.
Discussion
Recent studies evaluating college drinking interventions have become increasingly nuanced. For example, research has begun to consider dismantling of therapist-delivered interventions versus feedback only (Walters, Vader, Harris, Field, & Jouriles, 2009) as well as relative efficacy of specific feedback components (e.g., Martens, Smith, & Murphy, 2013). However, no previous research to date has specifically compared efficacy of the same intervention based on whether it was completed in-lab or remotely. Our results suggested that remote computer-delivered feedback was less effective than in-person computer-delivered feedback in reducing drinking and related consequences. Although the ability to reach many individuals electronically and virtually considerably reduces the costs associated with the provision of individually-tailored feedback interventions (Cunningham, 2009; Walters & Neighbors, 2011), our results suggest that college students who complete an intervention remotely may have a different experience than those who complete an identical intervention in person.
As suggested in Neighbors et al. (2010), several factors may contribute to the relatively lower efficacy of remote computer-based interventions. In remote interventions, students might be more distracted by competing attentional demands (e.g., other open computer applications like Facebook or email, television, other people talking, interruption by roommates), which are reduced in in-person interventions (Cunningham et al., 2011; Walters & Neighbors, 2011). Relatedly, a monitoring effect may be occurring, whereby students who are being monitored in a research setting, even if not closely, are more conscientious and diligent in processing all of the information provided. This would be similar to research showing assessment reactivity effects (Clifford & Maisto, 2000; Clifford, Maisto, & Davis, 2007; Kypri, Langley, Saunders, & Cashell-Smith, 2006; Maisto, Clifford, & Davis, 2007). Of additional note is the possibility of a selection effect, such that students who are less motivated are unwilling to attend an in-person intervention but are willing to complete it remotely. Finally, it is possible that participants who attend an in-person session may experience higher levels of trust and rapport with the research staff through interactions with them (Elliot et al., 2008; Taylor & Luce, 2003). Although the staff is not providing any in-person treatment, this increased rapport may indirectly affect participants’ willingness to pay attention and trust the intervention content. The present research was not designed to specifically evaluate these factors, but to empirically evaluate whether a remote feedback-based intervention is in fact less efficacious than the same intervention delivered in-person. Subsequent research could focus on identifying the relative factors responsible for this effect and determining whether factors undermining remote interventions might be attenuated or altered to bolster the effects.
While this article can provide a preliminary answer to the question of whether PNF delivery modality impacts intervention efficacy, there are several limitations that need to be addressed with future research to comprehensively answer this question. First, this research compared effects across samples and studies with different characteristics and procedures. The samples for all three in-person studies were from psychology subject pools, whereas the samples for all three remote studies were from the larger undergraduate student body. Psychology students are demographically similar to the larger student bodies on each campus; however, this cannot be ruled out as a source of selection bias. Second, there were a few other differences in the in-person and remote studies. Participants in the in-person studies received extra credit for part or all of their participation, whereas remote participants were paid at each timepoint. Although baseline drinking was comparable in four of the six studies, one of the remote studies had significantly lower drinking and one of the in-person studies had somewhat higher drinking. Further, the length of follow-ups for the in-person interventions was generally shorter than for the remote interventions. Thus, it may not be the case that remote interventions are not effective, but instead that they are not effective for very long (i.e., more than one month).
The finding that both delivery modalities produced reductions in perceived norms suggests that participants were at least partially attending to the remote interventions. It would have been more convincing if the face-to-face interventions reduced the perceived norms more than the remote interventions, which would have indicated that the participants adjusted their estimates to a greater extent. Unfortunately, this cannot be confirmed with the current data due to the timing of follow-ups for the studies (i.e., the three remote studies included one study with a one-month follow-up showing significant effects and two studies with follow-ups beginning at six months showing nonsignificant effects). Thus, similar to the point raised above, it is a possibility that remote interventions are effective, but only for a limited period of time. In light of research showing that these intervention effects decay over time (Carey et al., 2012), it would be helpful to further examine remote versus in-person differences using studies with better matched samples and study procedures.
In conclusion, brief computer-delivered remote interventions have several advantages over in-person interventions, including reduced cost and participant burden, greater reach, and potentially higher appeal to potential college student participants (Cunningham et al., 2011; Elliot et al., 2008; Gray & Klein, 2006; Ybarra & Suman, 2008). Given that computer-delivered alcohol interventions may be particularly beneficial for groups less likely to seek traditional alcohol-related services (e.g., young adults, at-risk drinkers; White et al., 2010) and the considerable amount of variability within computer-delivered interventions (Carey et al., 2012), delivery modality is an important factor influencing effect sizes. We believe that this research is a step toward improving understanding of the factors associated with treatment delivery and response from both clinical and cost-effectiveness perspectives. The present research provides evidence that computer-delivered interventions for college students may be more effective when conducted in-person than remotely over the internet. Furthermore, the relatively large difference in effect sizes suggests that this is not a trivial issue. The practical advantages of remote delivery are not without cost, and transfer of empirically-supported lab-based interventions to remote delivery should be done thoughtfully and with additional evaluation.
Public Health Relevance.
This research highlights the importance of intervention delivery method for computer-delivered brief alcohol interventions. Results across six studies provide evidence of better outcomes for personalized normative feedback delivered in-person over remote delivery.
Acknowledgments
Preparation of this article was supported by National Institute on Alcohol Abuse and Alcoholism Grants F31AA020442 and R01AA014576.
References
- Baer JS, Stacy A, Larimer M. Biases in the perception of drinking norms among college students. Journal of Studies on Alcohol. 1991;52:580–586. doi: 10.15288/jsa.1991.52.580. [DOI] [PubMed] [Google Scholar]
- Bewick BM, Trusler K, Mulhern B, Barkham M, Hill AJ. The feasibility and effectiveness of a web-based personalised feedback and social norms alcohol intervention in UK university students: A randomised control trial. Addictive Behaviors. 2008;33:1192–1198. doi: 10.1016/j.addbeh.2008.05.002. [DOI] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology. 2000;68(4):728–733. [PubMed] [Google Scholar]
- Borsari B, Carey KB. Descriptive and injunctive norms in college drinking: A meta-analytic integration. Journal of Studies on Alcohol. 2003;64:331–341. doi: 10.15288/jsa.2003.64.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Peer influences on college drinking: A review of the research. Journal of Substance Abuse. 2001;13:391–424. doi: 10.1016/s0899-3289(01)00098-0. [DOI] [PubMed] [Google Scholar]
- Borsari B, Neal DJ, Collins SE, Carey KB. Differential utility of three indexes of risky drinking for predicting alcohol problems in college students. Psychology of Addictive Behaviors. 2001;15:321–324. doi: 10.1037/0893-164X.15.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Henson JM, Maisto SA, DeMartini KS. Brief alcohol interventions for mandated college students: Comparison of face-to-face counseling and computer-delivered interventions. Addiction. 2011;106:528–537. doi: 10.1111/j.1360-0443.2010.03193.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, Maisto SA. Which heavy drinking college students benefit from a brief motivational intervention? Journal of Consulting and Clinical Psychology. 2007;75:663–669. doi: 10.1037/0022-006X.75.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Bolles JR, Carey MP. Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction. 2009;104:1807–1819. doi: 10.1111/j.1360-0443.2009.02691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LJ, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clinical Psychology Review. 2012;32:690–703. doi: 10.1016/j.cpr.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA. Subject reactivity effects and alcohol treatment outcome research. Journal of Studies on Alcohol and Drugs. 2000;61:787–793. doi: 10.15288/jsa.2000.61.787. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA, Davis CM. Alcohol treatment research assessment exposure subject reactivity effects: Part I. Alcohol use and related consequences. Journal of Studies on Alcohol and Drugs. 2007;68:519–528. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- Collins R, Parks GA, Marlatt G. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cunningham JA. Internet evidence-based treatments. In: Miller P, editor. Evidence Based Addiction Treatment. Elsevier; Amsterdam, the Netherlands: 2009. pp. 379–397. [Google Scholar]
- Cunningham JA, Kypri K, McCambridge J. The use of emerging technologies in alcohol treatment. Alcohol Research and Health. 2011;33:320–326. [PMC free article] [PubMed] [Google Scholar]
- Cunningham JT, Khadjesari Z, Bewick BM, Riper H. Internet-based interventions for problem drinkers: From efficacy trials to implementation. Drug and Alcohol Review. 2010;29:617–622. doi: 10.1111/j.1465-3362.2010.00201.x. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Selby PL, Kypri K, Humphreys KN. Access to the Internet among drinkers, smokers and illicit drug users: Is it a barrier to the provision of interventions on the World Wide Web? Informatics for Health and Social Care. 2006;31:53–58. doi: 10.1080/14639230600562816. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Wild TC, Cordingley J, van Mierlo T, Humphreys K. A randomized controlled trial of an internet-based intervention for alcohol abusers. Addiction. 2009;104:2023–2032. doi: 10.1111/j.1360-0443.2009.02726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA, McNeely M. Computer-enhanced primary care practitioner advice for high-risk college drinkers in a student primary health-care setting. Cognitive & Behavioral Practice. 2000;7:82–100. [Google Scholar]
- Dunn EC, Larimer ME, Neighbors C. Alcohol and drug-related negative consequences in college students with bulimia nervosa and binge eating disorder. International Journal of Eating Disorders. 2002;32:171–178. doi: 10.1002/eat.10075. [DOI] [PubMed] [Google Scholar]
- Elliot JC, Carey KB, Bolles JR. Computer-based interventions for college drinking: A qualitative review. Addictive Behaviors. 2008;33:994–1005. doi: 10.1016/j.addbeh.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner I, Larimer ME, Neighbors C. The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addictive Behaviors. 2004;29:843–848. doi: 10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Edwards EM, Heeren T, Rosenbloom D. Age of drinking onset and injuries, motor vehicle crashes, and physical fights after drinking and when not drinking. Alcoholism: Clinical and Experimental Research. 2009;33:783–790. doi: 10.1111/j.1530-0277.2009.00896.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2011. Volume II: College students and adults ages 19–50. Ann Arbor: Institute for Social Research, The University of Michigan; 2012. p. 314. [Google Scholar]
- Kaysen D, Neighbors C, Martell J, Fossos N, Larimer ME. Incapacitated rape and alcohol use: A prospective analysis. Addictive Behaviors. 2006;31:1820–1832. doi: 10.1016/j.addbeh.2005.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadjesari Z, Murray E, Hewitt C, Hartley S, Godfrey C. Can stand-alone compute-based interventions reduce alcohol consumption? A systematic review. Addiction. 2011;106:267–282. doi: 10.1111/j.1360-0443.2010.03214.x. [DOI] [PubMed] [Google Scholar]
- Knight JR, Wechsler H, Kuo M, Seibring M, Weitzman ER, Schuckit MA. Alcohol abuse and dependence among U.S. college students. Journal of Studies on Alcohol. 2002;63:263–270. doi: 10.15288/jsa.2002.63.263. [DOI] [PubMed] [Google Scholar]
- Kypri K, Saunders JB, Gallagher SJ. Acceptability of various brief intervention approaches for hazardous drinking among university students. Alcohol and Alcoholism. 2003;38:626–628. doi: 10.1093/alcalc/agg121. [DOI] [PubMed] [Google Scholar]
- Kypri K, Sitharthan T, Cunningham JA, Kavanagh DJ, Dean JI. Innovative approaches to intervention for problem drinking. Current Opinion in Psychiatry. 2005;18:29–234. doi: 10.1097/01.yco.0000165591.75681.ab. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Lewis MA, Atkins DC, Neighbors C, Zheng C, Kenney SR, Larimer ME. RCT of web-based personalized normative feedback for college drinking prevention: Are typical student norms good enough? Journal of Consulting and Clinical Psychology. 2013;81:1074–1086. doi: 10.1037/a0034087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999–2006. Addictive Behaviors. 2007;32:2439–2468. doi: 10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Kaysen DL, Lee CM, Kilmer JR, Lewis MA, Dillworth T, Montoya HD, Neighbors C. Evaluating level of specificity of normative referents in relation to personal drinking behavior. Journal of Studies on Alcohol and Drugs. 2009;(Suppl 16):115–21. doi: 10.15288/jsads.2009.s16.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C. Social norms approaches using descriptive drinking norms education: A review of the research on personalized normative feedback. Journal of American College Health. 2006;54:213–218. doi: 10.3200/JACH.54.4.213-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C. Optimizing personalized normative feedback: The use of gender-specific referents. Journal of Studies on Alcohol and Drugs. 2007;68:228–237. doi: 10.15288/jsad.2007.68.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Davis CM. Alcohol treatment research assessment exposure subject reactivity effects: Part II. Treatment engagement and involvement. Journal of Studies on Alcohol and Drugs. 2007;68:529–533. doi: 10.15288/jsad.2007.68.529. [DOI] [PubMed] [Google Scholar]
- Martens MP, Smith AE, Murphy JG. The efficacy of single-component brief motivational interventions among at-risk college drinkers. Journal of Consulting and Clinical Psychology. 2013;81:691–701. doi: 10.1037/a0032235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M, Leffingwell T, Claborn K, Meier E, Walters S, Neighbors C. Personalized feedback interventions for college alcohol misuse: An update of Walters & Neighbors (2005) Psychology of Addictive Behaviors. 2013;27:909–920. doi: 10.1037/a0031174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Dillard AJ, Lewis MA, Bergstrom RL, Neil TA. Normative Misperceptions and Temporal Precedence of Perceived Norms and Drinking. Journal of Studies on Alcohol. 2006;67:290–299. doi: 10.15288/jsa.2006.67.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Fossos N, Woods BA, Fabiano P, Sledge M, Frost D. Social anxiety as a moderator of the relationship between perceived norms and drinking. Journal of Studies on Alcohol and Drugs. 2007;68:91–96. doi: 10.15288/jsad.2007.68.91. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: Efficacy of a computer-delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72:434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Lewis MA, Atkins DC, Jensen MM, Walter T, Fossos N, Lee CM, Larimer ME. Efficacy of web-based personalized normative feedback: A two-year randomized controlled trial. Journal of Consulting and Clinical Psychology. 2010;78:898–911. doi: 10.1037/a0020766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Lewis MA, Bergstrom RL, Larimer ME. Being controlled by normative influences: Self-determination as a moderator of a normative feedback alcohol intervention. Health Psychology. 2006;25:571–579. doi: 10.1037/0278-6133.25.5.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins H. Social norms and the prevention of alcohol misuse in collegiate contexts. Journal of Studies on Alcohol. 2002;(SUPPL 14):164–172. doi: 10.15288/jsas.2002.s14.164. [DOI] [PubMed] [Google Scholar]
- Perkins H, Berkowitz AD. Perceiving the community norms of alcohol use among students: Some research implications for campus alcohol education programming. International Journal of the Addictions. 1986;21:961–976. doi: 10.3109/10826088609077249. [DOI] [PubMed] [Google Scholar]
- Perkins H, Meilman PW, Leichliter JS, Cashin JR, Presley CA. Misperceptions of the norms for the frequency of alcohol and other drug use on college campuses. Journal of American College Health. 1999;47:253–258. doi: 10.1080/07448489909595656. [DOI] [PubMed] [Google Scholar]
- Portnoy DB, Scott-Sheldon LAJ, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: A meta analysis of 75 randomized controlled trials, 1988 to 2007. Preventive Medicine. 2008;47:3–16. doi: 10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prentice DA, Miller DT. Pluralistic ignorance and alcohol use on campus: Some consequences of misperceiving the social norm. Journal of Personality and Social Psychology. 1993;64:243–256. doi: 10.1037//0022-3514.64.2.243. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW. HLM 6: Hierarchical linear and nonlinear modeling. Scientific Software International; 2004. [Google Scholar]
- Rooke S, Thorsteinsson E, Karpin A, Copeland J, Allsop D. Computer-delivered interventions for alcohol and tobacco use: A meta-analysis. Addiction. 2010;105:1381–1390. doi: 10.1111/j.1360-0443.2010.02975.x. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Luce KH. Computer- and internet- based psychotherapy interventions. Current Directions in Psychological Science. 2003;12:18–22. [Google Scholar]
- Walters ST, Neighbors C. Feedback interventions for college alcohol misuse: What, why and for whom? Addictive Behaviors. 2005;30:1168–1182. doi: 10.1016/j.addbeh.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Neighbors C. College prevention: A view of present (and future) Web-based approaches. Alcohol Research: Current Reviews. 2011;34:222–224. [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Miller E, Chiauzzi E. Wired for wellness: e-Interventions for addressing college drinking. Journal of Substance Abuse Treatment. 2005;29:139–145. doi: 10.1016/j.jsat.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Dismantling motivational interviewing and feedback for college drinkers: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77:64–73. doi: 10.1037/a0014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol and Drugs. 2008;69:481–490. doi: 10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall G, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college: A national survey of students at 140 campuses. JAMA: Journal of the American Medical Association. 1994;272:1672–1677. [PubMed] [Google Scholar]
- Wechsler H, Lee J, Kuo M, Lee H. College binge drinking in the 1990s: A continuing problem: Results of the Harvard School of Public Health 1999 College Alcohol Study. Journal of American College Health. 2000;48:199–210. doi: 10.1080/07448480009599305. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001. Journal of American College Health. 2002;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- White A, Kavanagh D, Stallman H, Klein B, Kay-Lambkin F, Proudfoot J, Young R. Online alcohol interventions: A systematic review. Journal of Medical Internet Research. 2010;12:160–171. doi: 10.2196/jmir.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ybarra M, Suman M. Reasons, assessments and actions taken: Sex and age differences in uses of Internet health information. Health Education Research. 2008;23:512–552. doi: 10.1093/her/cyl062. [DOI] [PubMed] [Google Scholar]