Abstract
Background
The complex epidemic and significant diversity of HIV-1 strains in China pose serious challenges for surveillance and diagnostic assays, vaccine development and clinical management. There is a lack of HIV-1 isolates in current canonical HIV-1 subtype panels that can represent HIV-1 diversity in China; an HIV-1 subtype panel for China is urgently needed.
Methods
Blood samples were collected from HIV-1 infected patients participating in the drug-resistance surveillance program in China. The samples were isolated, cultured and stored as neat culture supernatant. The HIV-1 isolates were fully characterized. The panel was used to compare 2 viral load assays and 2 p24 assays as the examples of how this panel could be used.
Results
An HIV-1 subtype panel for China composed of 30 HIV-1 primary strains of four subtypes (B [including Thai-B], CRF01_AE, CRF07_BC and G) was established. The samples were isolated and cultured to a high-titer (106-109 copies/ml)/high-volume (40ml). The HIV-1 isolates were fully characterized by the final viral load, p24 concentration, gag-pol and envC2V3 sequencing, co-receptor prediction, determination of the four amino acids at the tip of the env V3-loop, glycosylation sites in the V3 loop and the drug-resistance mutations. The comparison of two p24 assays and two viral load assays on the isolates illustrated how this panel may be used for the evaluation of diagnostic assay performance. The Pearson value between p24 assays were 0.938. The viral load results showed excellent concordance and agreement for samples of Thai-B, but lower correlations for samples of CRF01_AE.
Conclusion
The current panel of 30 HIV-1 isolates served as a basis for the development of a comprehensive panel of fully characterized viral isolates, which could reflect the current dynamic and complex HIV-1 epidemic in China. This panel will be available to support HIV-1 research, assay evaluation, vaccine and drug development.
Introduction
It has been reported that the number of people living with HIV increased to 35 million (33.2 million–37.2 million) by the end of 2013 according to the United National Programme on HIV and AIDS (UNAIDS) [1]. Currently, the major source of the global pandemic is divided into four groups: M (Major), O (Outlier), N (Non-M and Non-O) and P. The M group includes nine major subtypes (i.e., A-D, F-H, J, and K), over 72 circulating recombinant forms (CRF), and numerous unique recombinant forms (URF). Their rapid evolution and comprehensive diversity make them a serious challenge for the maintenance of a reliable serological and nucleic acid test for blood screening, epidemiological surveillance, diagnosis, and clinical management of the infected persons. Differences between subtypes in HIV-1 RNA quantitation and determination, serological diagnostic and screening variations have been noted [2, 3]. Many HIV-1 nucleic acid tests or serological assays designed and tested based on subtype B virus have demonstrated an underestimation of some non-B subtypes [4–6]. Differences between subtypes in currently commercially available quantitative viral load tests have been reported [7–9]. Furthermore, viral diversity may also impact responses to antiretroviral therapies and vaccines [10–12]. Under these circumstances, a set of fully characterized viruses from HIV infections are needed to better represent current global HIV diversity and help control the worldwide HIV-1 epidemic through support of epidemiological testing, vaccines, and therapeutic efforts [13].
HIV-1 subtype B (Thailand’s variant of subtype B included), CRF01_AE, CRF07_BC and CRF08_BC are the major subtypes of HIV-1 strains circulating in China [14]. HIV-1 strains of subtype B from Thailand were transmitted to Yunnan province in the early 1990s. Strains of subtype C from India were transmitted to Yunnan soon after 1993 and these two subtypes caused the first wave of an HIV-1 epidemic in China among intravenous drug users (IDUs) in Yunnan province [15]. CRF07_BC and CRF08_BC were generated from subtypes B and C, and most likely originated in Yunnan [16–18]. CRF08_BC spread eastward to the southern coastal provinces around 1990 [16, 18], while CRF07_BC spread to northwestern China along a drug traffic route around 1993 [15, 18, 19]. Meanwhile, unregulated and unsanitary commercial plasma collection between the years 1992 and 1995 in Henan caused an HIV-1 subtype Thai-B infection epidemic in central China [20–22]. On the other hand, since HIV-1 CRF01_AE was first found among heterosexuals and IDUs in southern China around 1996–1997, this subtype of the virus spread through sexual routes to other provinces quickly and broadly [23–25]. Several new circulating recombinant forms generated from the subtypes circulating in China were found recently [26–32], such as CRF55_01B, which was a recombinant of CRF01_AE and Thai-B and was discovered from men having sex with men (MSM) in the year 2013 [26]; CRF57_BC, which was a recombinant of Thai-B and India C and was discovered in western Yunnan in China in 2014 [27]; and CRF61_BC, which was comprised of CRF07_BC and CRF08_BC and was identified in the heterosexual population in two different regions in China [29]. The diversity of HIV-1 is extensive in China.
In the U.S., a pilot program called the NIAID External Quality Assurance Program Oversight Laboratory (EQAPOL) established by the National Institutes of Health/National Institute of Allergy and Infectious Diseases (NIH/NIAID) in collaboration with other institutes throughout the world developed an HIV subtype panel that encompassed the genetic and geographic diversity currently present worldwide [13, 33]. This program has collected over 100 viral samples, but only 7 of them were isolated from HIV-1 infections in China [13].
To establish an HIV-1 subtype panel that represents the diversity of HIV-1 strains circulating in China, we collected 99 plasma specimens from HIV-1 infected individuals in 10 provinces of China through the HIV-1 drug-resistance surveillance program. Finally, we successfully obtained 30 HIV-1 isolates of different subtypes. The HIV-1 p24 antigen concentrations and viral loads of the isolates were evaluated. We also sequenced the three major structural genes: gag, pol and envC2V3 for subtype analysis, prediction of co-receptor usage, the four amino acids at the tip of the V3-loop and the glycosylation sites on envV3 sequence, as well as the drug-resistance mutations.
Materials and Methods
Patients and samples
Blood samples with the basic personal information of each patient were collected from HIV infected individuals who were participants in the HIV-1 drug-resistance surveillance program in 10 provinces of China (Guangxi, Guangdong, Sichuan, Henan, Xinjiang, Ningxia, Shanghai, Shandong, Beijing and Zhejiang). 10 ml of anticoagulated whole blood was obtained from each patient for virus isolation and expansion. The basic personal information of the patients showed that all the main routes of HIV-1 transmission were included among the cases (i.e., homosexual sex, heterosexual sex, blood donation, blood transfusion, intravenous drug using and occupational exposure).
All the samples were identified by HIV-1 antibody enzyme linked immunosorbent assay (ELISA) screening, HIV-1 p24 antigen testing and the Western blot to confirm the infection of HIV-1.
Isolation and expansion of primary HIV-1 strains
Peripheral blood mononuclear cells (PBMCs) from the blood samples were separated immediately after the collection, and they were co-cultured with PBMCs from healthy blood donors to separate and expand the virus in a three-step process: isolation, small-scale culture and large-scale culture.
For isolation, the healthy PBMCs were isolated from the blood of more than eight healthy blood donors by HISTOPAQUE-1077 (SIGMA). The isolated PBMCs were cultured in RPMI-1640 medium with 10% fetal bovine serum (FBS), 100 U/ml penicillin and 100 μg /ml streptomycin. The healthy PBMCs were stimulated by 5 μg/ml phytohemagglutinin (PHA) and 10 IU/ml interleukin-2 (IL-2) for three days. Then, the infected PBMCs were separated from the patients’ blood in the same way and cultured in RPMI1640 medium with FBS, penicillin, streptomycin and IL-2 but without PHA. The patient's PBMCs and activated healthy donor PBMCs were centrifuged at 250×g for 5 minutes, and then the PBMCs were re-suspended in RPMI-1640 medium to 2×106 cells/ml respectively. Infected and healthy PBMCs were mixed at a volume ratio of 1:1 into 24-well plates and were then co-cultured in a cell incubator containing 5% CO2 at 37°C. A total of 100 μl of supernatant was sampled every seven days to measure the concentration of p24 antigen to observe the growth of every HIV-1 strain, and one half of the initial volume of the cell supernatant was replaced by healthy donor cells to maintain a stable environment for virus growth. The cultures were continued for up to 28 days or until p24 results were greater than 2 pg/ml.
For small-scale culture, 4 ml of 2×106 cells/ml PBMCs from healthy donors were inoculated with 1 ml HIV-1 cell culture supernatant sampled at the end of the isolation, and the viruses were cultured for another 7 days until the 35th day or until the p24 results were greater than 10 pg/ml.
For large scale culture, 1 ml of cell supernatant from the small-scale culture were put into 39 ml of 1×106cells/ml PBMCs, and cultured for another 7 days or until the p24 antigen results were greater than 25 pg/ml.
The cell suspensions were centrifuged at 800×g for 5 minutes and the supernatant was aliquoted into 1.5 ml centrifuge tubes at 1 ml/tube and stored in liquid nitrogen (-196°C).
HIV-1 gag, pol, envC2V3 and full-length genome amplification and sequencing
The full-length of gag and pol were amplified and sequenced and then spliced together as a complete genetic region for subtyping. The C2V3 region of env was also amplified and sequenced.
Viral RNA from the culture supernatant was extracted with a QIAamp Viral RNA Mini Kit and served as the template for amplification. The 1,502 bp full length gag gene (HXB2: 790–2292), 3,011 bp full length pol gene (HXB2: 2,085–5,096) and 520 bp envC2V3 (HXB2: 7021–7541) fragments were amplified according to reference [34]. The full-length gag and pol genes were connected together as a complete genetic region (HXB2: 790–5,096) for subtyping.
Phylogenetic analysis and subtype identification
In order to identify the subtypes of the isolated strains, we regarded the gag-pol fragment as the target sequence. A neighbor-joining tree of these target sequences and reference strains (subtypes A–D, F–H, J, K and most kinds of circulating recombinant forms were included) was constructed by MEGA5.1 with bootstrap 1000. Virus samples that were unidentified in the gag-pol fragment were uploaded to REGA (http://jose.med.kuleuven.ac.be/genotypetool/html/subtypinghiv.html) and NCBI HIV Subtyping. Recombinants and incomplete gag-pol sequences of the recombinants were analyzed using the jumping profile hidden Markov model (jpHMM) tool provided at www.hiv.lanl.gov (http://jphmm.gobics.de/).
In order to identify the diversity of CRF01_AE isolates in our program, we performed phylogenetic analysis for the CRF01_AE isolates in our panel in particular by using the full-length sequences of the gene pol from the isolates, together with the HIV-1 CRF01_AE sequences used in Yi Feng and Xiang He’s study [35]. A neighbor-joining tree was constructed by MEGA5.1 with bootstrap 1000.
The prediction of co-receptor usage, the four amino acids at the tip of the V3-loop and the glycosylation sites by envV3
The genotype prediction of co-receptor usage of the HIV-1 isolates based on the envV3 sequence information was predicted with two online software programs: a Web-based genotypic algorithm—WebPSSM (http://intra.mullins.microbiol.washington.edu/webpssm/) and Geno2Pheno (G2P) prediction, which is based on the bioinformatics prediction tool that uses the V3 sequence plus additional host-specific features to select false positive rates (FPR) at 1%, 2.5%, 5%, 15%, and 20%. The FPR represents the percentage of all samples that are X4-incapable will be predicted as X4-capable viruses, and FPR at 2.5% was used in this program; http://coreceptor.geno2pheno.org/index.php. We translated the nucleotide sequence of the V3 loop into the corresponding amino acid sequence using software Gene Cutter provided by the Los Alamos HIV database (http://www.hiv.lanl.gov/content/sequence/GENE_CUTTER/cutter.html), and the top four amino acids at the tip of the V3-loop of each HIV-1 isolate. In addition, the glycosylation sites on the V3-loop were predicted by online prediction software N-GlycoSite (http://www.hiv.lanl.gov/content/sequence/GLYCOSITE/glycosite.html).
The determination of viral drug resistance mutations
We submitted the full-length pol gene (2,085 bp–5,096 bp) to the Stanford University Network HIV-1 database (http://hivdb.stanfrod.edu/hiv/) after amplification and sequencing to determine drug resistance mutations and tolerance of various antiviral drugs of the HIV-1 isolates.
Measurement of HIV-1 isolate p24 concentration and viral load after isolation and expansion
We detected p24 antigen and measured the viral load to evaluate the correlation and agreement between the two indicators.
P24 antigen was quantified using a BioMerieux VIDAS HIV p24 II assay and one domestic p24 test assay. For the samples that were beyond the upper limits (400 pg/ml for the VIDAS HIV p24 II assay and 80 pg/ml for the domestic p24 test assay), the RPMI-1640 medium with 10% FBS was used for dilution in the performance of both of the assays.
The viral loads of all the 30 samples in the panel were measured using two commercial kits according to the manufacturers’ instructions: the automated Roche Cobas AmpliPrep/Cobas TaqMan HIV-1 test version 2.0 assay (CAP/CTM v2.0 assay) and Nuclisens HIV-1 EasyQ version 2.0 assay (EasyQ v2.0 assay). For the samples that were beyond the upper limits (5,757,126 IU/ml for EasyQ v2.0 assay and 17,000,000 IU/ml for the CAP/CTM v2.0 assay [36]), HIV-1-negative plasma was used to dilute the culture supernatant of the isolates in the performance of the two assays.
To compare the performance of the CAP/CTM v2.0 assay with that of the EasyQ v2.0 assay, all HIV-1 viral load values (expressed as copies/ml) were converted to IU/ml, and then into log IU/ml values for statistical analysis [36]. The correlation coefficient (R) of Pearson test was used to assess the strength of the linear association and the Bland-Altman method was used to assess the level of agreement between the paired measurements [37].
Statistical analysis
The mean differences and standard deviations (SD) were calculated using SPSS 22.0 software to compare the performance of the 2 viral load measurement assays. The Pearson correlation coefficient (R) was used to assess the strength of the linear association between the log-transformed levels in the positive samples measured by the two viral load assays and between the p24 concentration values tested by the two p24 assays. The Bland-Altman method was used to assess the level of agreement between the paired measurements using MedCalc 14.8.1.0 software [37]. The linear association between the p24 concentrations measured by the BioMerieux VIDAS HIV p24 II assay and the HIV-1 viral loads measured by a Roche Cobas AmpliPrep/Cobas TaqMan HIV-1 test version 2.0 assay (CAP/CTM v2.0 assay) had also been evaluated.
Ethical statement
The study has been ethically approved by the Ethical Board of the Beijing Institute of Microbiology and Epidemiology. Blood samples were collected from the patients participated in the drug-resistance surveillance program in China. The written informed consents were obtained from all the participants and the data were analyzed anonymously. The informed consent process has also been approved by the Ethical Board of the Beijing Institute of Microbiology and Epidemiology.
Results
Virus isolation and expansion
After seven times of isolation and expansion in different years, the p24 concentrations of 30 isolates were greater than 25 pg/ml. As for the 30 HIV-1 primary strains that were isolated and expanded successfully, strains from each of the 10 provinces in China still existed; i.e., Guangxi (n = 4), Guangdong (n = 5), Sichuan (n = 1), Henan (n = 11), Xinjiang (n = 1), Ningxia (n = 1), Shanghai (n = 1), Shandong (n = 4), Beijing (n = 1) and Zhejiang (n = 1). The basic personal information of the cases is summarized in Table 1.
Table 1. Basic information on the 30 HIV-1 samples.
| Sample ID | Gender a | Infection route | Area of origin | Year | Treatment b |
|---|---|---|---|---|---|
| HN2002024 | M | Blood transfusion | Henan | 2002 | Y |
| GX2005002 | M | Heterosexual sex | Guangxi | 2005 | N |
| GX2005016 | M | Blood transfusion | Guangxi | 2005 | N |
| GD2005003 | M | Blood transfusion | Guangdong | 2005 | Y |
| GD2005004 | M | Heterosexual sex | Guangdong | 2005 | Y |
| GD2005006 | M | Heterosexual sex | Guangdong | 2005 | N |
| GD2005025 | M | intravenous drug using | Guangdong | 2005 | N |
| GD2005028 | F | Blood transfusion | Guangdong | 2005 | N |
| NX2005012 | M | Blood transfusion | Ningxia | 2005 | N |
| GX2006183 | M | Unclear | Guangxi | 2006 | Y |
| GX2006185 | F | Heterosexual sex | Guangxi | 2006 | Y |
| BJ2006001 | M | Heterosexual sex | Beijing | 2006 | Y |
| SD2006001 | M | Blood transfusion | Shandong | 2006 | Y |
| ZJ2006001 | F | Blood transfusion | Zhejiang | 2006 | Y |
| SH2007052 | M | Heterosexual sex | Shanghai | 2007 | Unknown |
| SC2009001 | M | Occupational Exposure | Sichuan | 2009 | Y |
| SX2010001 | M | Blood transfusion | Shanxi | 2010 | Y |
| SD2010001 | M | Homosexual sex | Shandong | 2010 | N |
| HN2010001 | M | Blood donation | Henan | 2010 | N |
| HN2010002 | M | Blood donation | Henan | 2010 | N |
| BJ2010001 | M | Homosexual sex | Beijing | 2010 | N |
| HN2010003 | F | Blood transfusion | Henan | 2010 | N |
| HN2010004 | F | Blood donation | Henan | 2010 | N |
| BJ2010002 | M | Homosexual sex | Beijing | 2010 | N |
| XJ2010001 | M | Homosexual sex | Xinjiang | 2010 | N |
| HN2010005 | F | Blood donation | Henan | 2010 | N |
| BJ2010003 | M | Homosexual sex | Beijing | 2010 | N |
| SD2013001 | M | Homosexual sex | Shandong | 2013 | N |
| SD2013005 | M | Homosexual sex | Shandong | 2013 | N |
| SD2013008 | M | Homosexual sex | Shandong | 2013 | N |
a: “M” represents for male and “F” represents for female.
b: “Y” represents for treated and “N” represents for treated naive.
Phylogenetic analysis and subtype identification
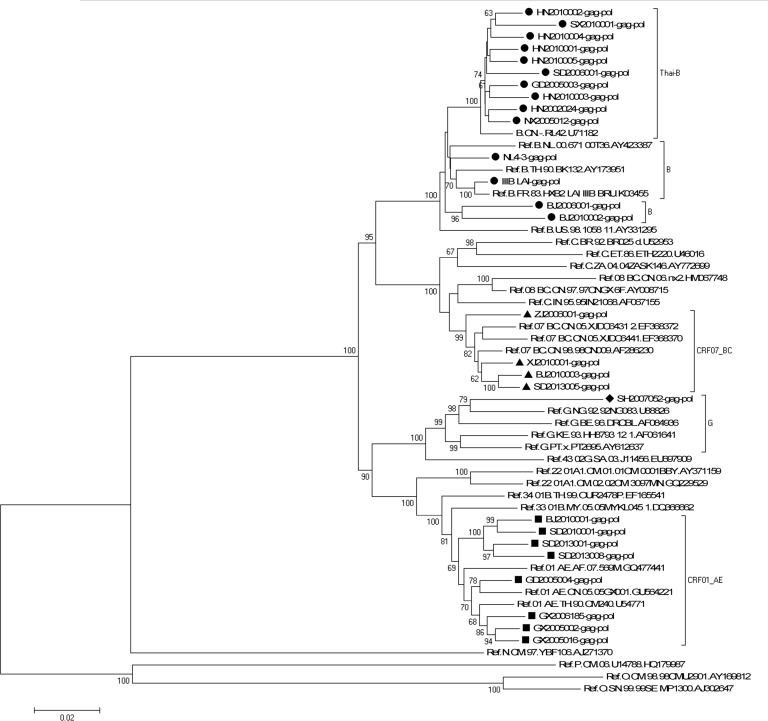
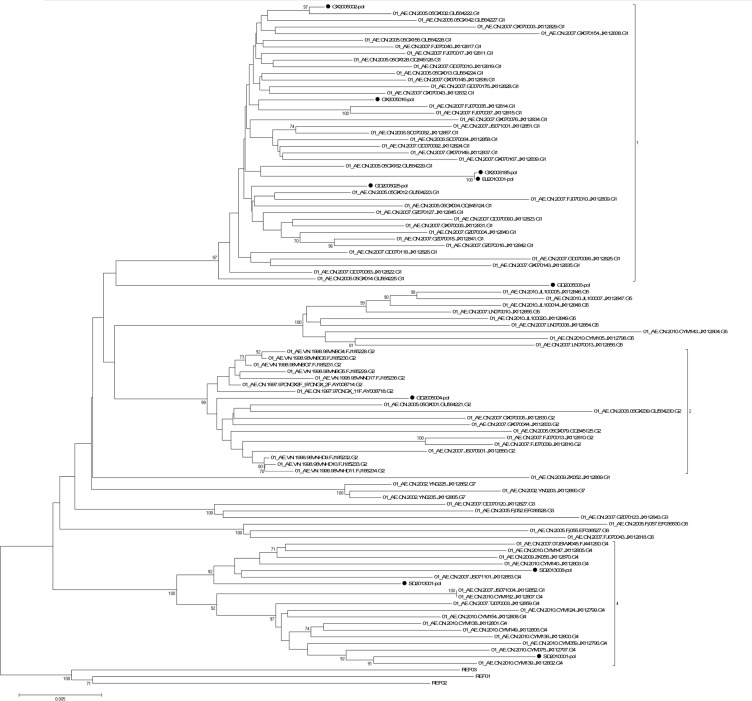
A neighbor-joining tree was constructed to determinate the subtype of each isolate based on 25 full-length gag-pol genetic region sequences of the isolates in our program (all the gag-pol sequences are available from the Los Alamos Databases and their accession numbers of GenBank are KP178421-KP178445) (GD2005006, GD2005025 and GD2005028 failed in gag amplification; GX2006183, SC2009001 failed in pol amplification) and 30 standard subtype reference sequences from the Los Alamos HIV sequence database (the reference sequence of subtype Thai-B: B.CN-RL42.U71182 was included) (Fig 1). Subtypes of five other strains (GD2005006, GD2005025, GD2005028, GX2006183 and SC2009001) were designated and identified by REGA Viral Subtyping and the NCBI HIV Subtyping tool based on their gene gag sequences (GX2006183-gag: KP178446; SC2009001-gag: KP178447) or gene pol sequences (GD2005006-pol: KP178448; GD2005025-pol: KP178449; GD2005028-pol: KP178450). Subtyping assessment results revealed that our panel included four subtypes currently (i.e., B, CRF01_AE, CRF07_BC and G). Thirteen of the 30 samples from this analysis were subtype B (11 strains of Thai-B were included), twelve were subtype CRF01_AE, four were subtype CRF07_BC, and one was subtype G, which was an exceptional subtype in China (Table 2). A neighbor-joining tree of 10 full-length pol gene sequences of all 11 CRF01_AE isolates (GX2006183 failed in pol amplification) in our program and 93 CRF01_AE full-length pol gene sequences in Yi Feng and Xiang He’s study as the reference sequences was constructed to identify the diversity of the CRF01_AE isolates in our panel (Fig 2). In Yi Feng and Xiang He’s study, seven distinct phylogenetic clusters of CRF01_AE were identified. The CRF01_AE isolates in our study were found in three of the seven clusters shown in Fig 2.
Fig 1. Phylogenetic analysis of characterized HIV-1 gag-pol gene sequences.
The tree was midpoint rooted. Horizontal branch lengths are drawn to scale (the scale bar represents 0.02 nucleotide substitution per site). Bracket separation is for clarity only. Numbers at the nodes indicate the bootstraps in which the cluster to the right was supported by 60% and higher. Markers in different shapes at the ends of the horizontal branch represent different subtypes to which the sequences belong. Triangle represents the subtype CRF07_BC, square represents the subtype CRF01_AE, rhombus represents the subtype G, and circle represents the subtype B (B represented by black round while Thai-B represented by dark red circle).
Table 2. Characterization of expanded viruses.
| Sample ID | Infection route | Area of collection | HIV-1 subtype | CD4+T-cells (cells/μl) in plasma | VIDAS HIV p24 II (pg/ml) a | Domestic HIV-1 p24 assay(pg/ml) a | NucliSENS EasyQ HIV-1 v2.0(million copies/ml) a | COBAS Taqman v 2.0(million copies/ml) a | Coreceptor predicted by Webpssm | Coreceptor predicted by Geno 2 Pheno (FPR 2.5%) | The top 4 peptides of V3 | Number of glycosylation sites in V3 loop | Drug-resistant mutations |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GX2005002 | Heterosexual sex | Guangxi | CRF01_AE | 43 | 14800 | 6168 | 330 | 252 | X4/R5 | X4/R5 | GPGR | 10 | NRTI: K70KT |
| GX2005016 | Blood transfusion | Guangxi | CRF01_AE | 137 | 345 | 74 | 0.0068 | 1.07 | X4/R5 | X4/R5 | GPGR | 8 | None |
| GX2006183 | Unclear | Guangxi | CRF01_AE | 293 | 680 | 166 | 0.4 | 0.892 | X4/R5 | X4/R5 | GLGH | 11 | None |
| GX2006185 | Heterosexual sex | Guangxi | CRF01_AE | 114 | 371 | 173 | 0.15 | 0.747 | X4/R5 | X4/R5 | GPGH | 9 | None |
| GD2005003 | Blood transfusion | Guangdong | B | 8 | 11900 | 6664 | 1300 | 152 | R5 | X4/R5 | GPGR | 10 | None |
| GD2005004 | Heterosexual sex | Guangdong | CRF01_AE | 3 | 1472 | 498 | 4.3 | 8.15 | X4/R5 | X4/R5 | GPGH | 9 | None |
| GD2005006 | Heterosexual sex | Guangdong | CRF01_AE | 2 | 8630 | 2372 | 170 | 127 | X4/R5 | X4/R5 | GPGQ | 11 | None |
| GD2005025 | intravenous drug using | Guangdong | CRF01_AE | 10 | 622 | 270 | 0.32 | 1.51 | R5 | R5 | GPGQ | 9 | PI: K20KT, D30DE, V32EV, M46MR |
| GD2005028 | Blood transfusion | Guangdong | B | 36 | 86 | 28 | 2.5 | 1.16 | R5 | R5 | GPGR | 10 | PI: V82FIV* |
| SC2009001 | Occupational Exposure | Sichuan | CRF01_AE | 503 | 1390 | 498 | 9 | 10 | X4/R5 | X4/R5 | GPGR | 9 | None |
| SX2010001 | Blood transfusion | Shanxi | B | 76 | 14000 | 5742 | 170 | 203 | R5 | R5 | GPGR | 13 | NRTI: M41L*, M184V*, L210W*, T215Y*, K219KN; NNRTI: K103N*, M230L* |
| SD2010001 | Homosexual sex | Shandong | CRF01_AE | 1187 | 22170 | 7806 | 43 | 173 | R5 | R5 | GPGQ | 10 | None |
| HN2010001 | Blood donation | Henan | B | 265 | 595 | 314 | 8.8 | 4.24 | R5 | R5 | GQGR | 13 | None |
| HN2010002 | Blood donation | Henan | B | 432 | 14100 | 5609 | 130 | 251 | R5 | R5 | GQGR | 11 | PI: A71T |
| BJ2010001 | Homosexual sex | Henan | CRF01_AE | 1179 | 3576 | 909 | 13 | 28 | R5 | R5 | GPGQ | 10 | None |
| HN2010003 | Blood trasfusion | Henan | B | 312 | 7440 | 3766 | 180 | 140 | R5 | R5 | GQGR | 13 | None |
| HN2010004 | Blood donation | Henan | B | 219 | 3370 | 1289 | 32 | 43.9 | R5 | R5 | GPGQ | 13 | INI: L68V |
| BJ2010002 | Homosexual sex | Henan | B | 1187 | 101000 | 92819 | 5100 | 2010 | R5 | R5 | GWGR | 10 | PI: A71T; INI: A128T |
| XJ2010001 | Homosexual sex | Xinjiang | CRF07_BC | 1333 | 18500 | 7331 | 1700 | 1170 | R5 | R5 | GPGQ | 9 | PI: Q58E |
| HN2010005 | Blood donation | Henan | B | 248 | 18900 | 12021 | 860 | 359 | R5 | R5 | GPGR | 9 | None |
| BJ2010003 | Homosexual sex | Henan | CRF07_BC | 1528 | 2630 | 554 | 250 | 101 | R5 | R5 | GPGQ | 12 | INI: H51HQ |
| NX2005012 | Blood transfusion | Ningxia | B | 21 | 237 | 65 | 5.8 | 2.12 | R5 | R5 | GQGR | 11 | INI: L68V |
| SH2007052 | Heterosexual sex | Shanghai | G | ND | 363 | 50 | 0.66 | 0.823 | R5 | R5 | APGQ | 10 | None |
| HN2002024 | Blood trasfusion | Henan | B | ND | 80000 | 128722 | 1700 | 618 | X4/R5 | X4/R5 | GPGR | 10 | PI: I54M*, L23IL, A71V |
| SD2013001 | Homosexual sex | Shandong | CRF01_AE | 197 | 2575 | 1047 | 0.2 | 22.7 | X4/R5 | R5 | GPGQ | 11 | INI: P145PS, S153FS |
| SD2013005 | Homosexual sex | Shandong | CRF07_BC | 715 | 107 | 46 | 14 | 3.11 | R5 | R5 | GPGQ | 10 | None |
| SD2013008 | Homosexual sex | Shandong | CRF01_AE | 486 | 21500 | 11583 | 40 | 254 | X4/R5 | X4/R5 | GPGQ | 8 | None |
| BJ2006001 | Heterosexual sex | Beijing | B | 40 | 1500 | 866 | 4.6 | 2.49 | X4/R5 | X4/R5 | GRGR | 12 | NRTI: M41L*, L210W*, T215F*; NNRTI: A98G, K103N*, V179E*, Y181C*, G190A*; PI: L63P, V77I |
| SD2006001 | Blood trasfusion | Shandong | B | 74 | 1600 | 409 | 5.8 | 2.78 | X4/R5 | X4/R5 | GPGR | 13 | NRTI: M184V*; NNRTI: K103N*; PI: L63P, A71T, V77I, I93L |
| ZJ2006001 | Blood transfusion | Zhejiang | CRF07_BC | 38 | 4060 | 1488 | 9.9 | 17 | Unknown | Unknown | Unknown | Unknown | NRTI: K65R*, T69D, K219R; NNRTI: V106M*, Y181C*; PI: L63P, I93L, L10X |
| IIIB_LAI(Ref) | Unknown | France | B | Unknown | 79000 | 43925 | 2600 | 708 | X4/R5 | X4/R5 | GPGR | 11 | None |
| NL4-3(Ref) | Recombinant | France | B | Unknown | 78000 | 44829 | 2200 | 686 | X4/R5 | X4/R5 | GPGR | 12 | IN: V151I |
ND: Not done, envC2V3 PCR was negative.
a: Samples for p24 antigen tests(VIDAS HIV p24 II and the domestic HIV-1 p24 assay) and viral load tests(NucliSENS EasyQ HIV-1 v2.0 and COBAS Taqman v 2.0) are culture supernatant of the isolates after expansion.
*: NRTI/NNRTI/PI/INI Major drug-resistance mutations. Mutations without “*” are minor resistance mutations, accessory mutations or single nucleotide polymorphisms (SNP).
Ref: Reference virus. IIIB_LAI and NL4-3 are reference virus with clear background information and high replication capacity but are not primary isolates.
The expanded virus was characterized in terms of infection route, area of origin, CD4+T cells concentration in blood sample, viral RNA concentration (Roche TaqMan v2.0 and BioMerieux NucliSENS EasyQ HIV-1 v2.0), p24 concentration (BioMerieux VIDAS HIV p24 II and One domestic HIV-1 p24 antigen assay), coreceptor usage (Webpssm and Geno 2 Pheno (FPR 2.5%)), the four identical residues at the tip of v3 loop, number of glycosylation sites in v3-loop, and drug-resistance mutations in pol.
Fig 2. Neighbor-joining tree of HIV-1 CRF01_AE pol gene sequences.
The phylogenetic tree was constructed with HIV-1 full-length gene pol sequences. Horizontal branch lengths are drawn to scale (the scale bar represents 0.005 nucleotide substitution per site). The numbers “1”, “2”, and “4” marked on the bracket separation are clusters that correspond to the clusters in Yi Feng and Xiang He’s study. Numbers at the nodes indicate the bootstraps in which the cluster to the right was supported by 70% and higher. The red circles at the ends of the horizontal branch represent the HIV-1 CRF01_AE samples in our panel. The three reference sequences at the root of the neighbor-joining tree were HIV-1 CRF01_AE sequences from Central Africa. The accession numbers of the three references in the Los Alamos HIV Database are Ref.01_AE.CF.1990.90CF11697.AF197340, Ref.01_AE.CF.1990.90CF4071.AF197341 and Ref.01_AE.CF.1990.90CR402_CAR_E_4003.U51188.
The prediction of co-receptor usage, the four amino acids at the tip of the V3-loop and the glycosylation sites by envV3 sequences of each isolate
The predominant co-receptor usage of each of the virus isolates was determined based on genotype analysis by two online software programs: WebPSSM and Geno2Pheno (G2P) prediction (Table 2). Twenty-nine envC2V3 sequences (KP178451-KP178479) of the thirty samples were amplified successfully. Fifteen of the thirty samples tested exhibited a CCR5 phenotype while fourteen of the thirty samples test exhibited a CXCR4/CCR5 phenotype in both assays (the envC2V3 amplification of ZJ2006001 was negative). However, the predictions for GD2005003 and SD2013001 were opposite according to the two assays (Table 2). The four amino acids at the tip of the V3-loop and the number of glycosylation sites on the V3-loop for each isolate are shown in Table 2.
The determination of viral drug resistance mutations
Online tools at the Stanford University HIV-1 database (http://hivdb.stanfrod.edu/hiv/) were used to determine the drug-resistance mutations in the full-length sequences of the gene pol of each isolate. Their tolerance for each kind of antiviral drug related to the mutations were also predicted to consummate the fully characterization of the isolates (Table 2).
Statistical analysis of the p24 concentrations and viral loads of the HIV-1 isolates
P24 antigen concentrations were quantified using a BioMerieux VIDAS HIV p24 II assay and a domestic p24 test assay. No isolates were below the lower limits of the assays (3.0 pg/ml for the VIDAS HIV p24 II assay and 5.0 pg/ml for the domestic p24 test assay). The results of the p24 concentration test by the BioMerieux VIDAS HIV p24 II assay ranged from 86.1 pg/ml to 1.01×105 pg/ml. The results of the p24 concentration test by the domestic p24 test assay ranged from 28.3 pg/ml to 1.29×105 pg/ml (Table 2). The viral loads were measured by the Cobas AmpliPrep/Cobas TaqMan HIV-1 test version 2.0(CAP/CTM v2.0, Roche) and the NucliSens EasyQ HIV-1 version 2.0 (EasyQ v2.0, BioMerieux). No isolates were below the lower limits of the assays (5.747 IU/ml for the EasyQ v2.0 assay and 34 IU/ml for the CAP/CTM v2.0 assay). The viral load test by CAP/CTM v2.0 ranged from 7.47×105 copies/ml to 2.01×109 pg/ml. The viral load test with the EasyQ v2.0 ranged from 6.8×103 copies/ml to 5.1×109 copies/ml (Table 2).
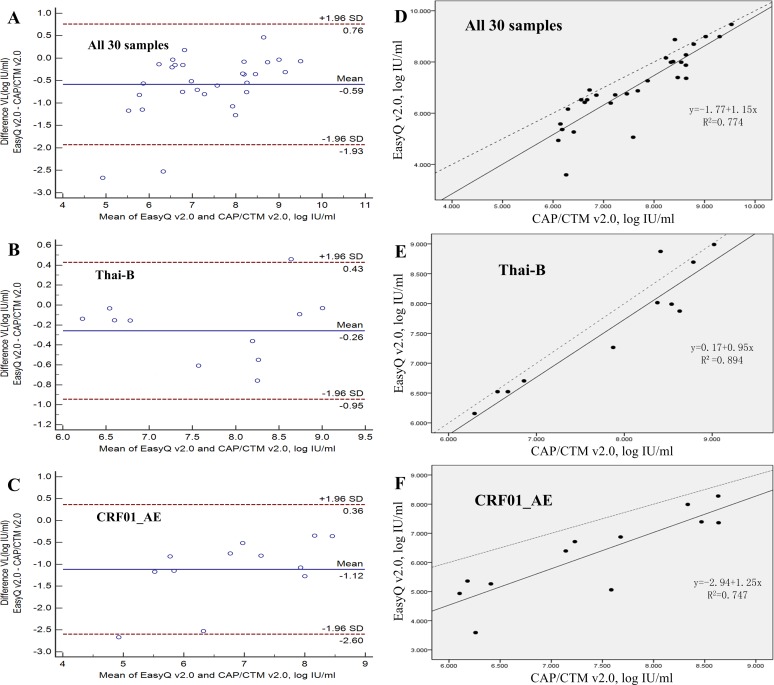
As for the two assays providing viral load tests, according to the results of the performance, EasyQ v2.0 showed a significant linear correlation (R = 0.880, p<0.001) and high agreement (93.33%, 28/30) with CAP/CTM v2.0 for all 30 samples (Table 3 and Fig 3A). The regression equation used for fitting was: EasyQ v2.0 = -1.77+1.15×CAP/CTM V2.0 (Fig 3D). The mean difference between the quantitative values measured by EasyQ v2.0 and CAP/CTM v2.0 was 0.587 log IU/ml (SD = 0.687; Table 3). For the different subtype isolates (subtype Thai-B and subtype CRF01_AE, Table 3), a significant linear correlation (R = 0.946 for subtype Thai-B, p <0.001; R = 0.864 for subtype CRF01_AE, p<0.001; Table 3) and high agreement (90.91% for Thai-B and 91.67% for CRF01_AE; Fig 3) were observed. The mean difference between the values measured by EasyQ v2.0 and CAP/CTM v2.0 was 0.260 log IU/ml (SD = 0.350) for subtype Thai-B (p = 0.260) and 1.120 log IU/ml (SD = 0.756) for subtype CRF01_AE (p<0.001). The number of samples with the quantitative differences between EasyQ v2.0 and CAP/CTM v2.0 exceeded 0.5 log IU/ml varied from each subtype: three samples (27.27%) for subtype Thai-B and 10 samples (83.33%) for subtype CRF01_AE. Furthermore, six subtype CRF01_AE samples showed quantitative differences of >1 log IU/ml, while no samples of Thai-B showed quantitative differences of >1 log IU/ml (Table 3).
Table 3. Comparison of the EasyQ v2.0 and CAP/CTM v2.0 using samples belonging to different clades.
| Paired t-test | Pearson correlation test | Bland-Altman model | Outliers(n[%]) | |||||
|---|---|---|---|---|---|---|---|---|
| n | Difference in viral load(log IU/ml) a | Sig b | R value c [p-value] | Limits of agreement | Agreement(n/N[%]) | >0.5 log IU/ml | >1 log IU/ml | |
| Total | 30 | 0.587±0.687 | <0.001 | 0.880[<0.001] | -1.93,0.76 | 28[93.33] | 15[50.00] | 6[20.00] |
| Thai-B | 11 | 0.260±0.350 | 0.026 | 0.946[<0.001] | -0.95,0.43 | 10[90.91] | 3[27.27] | 0[0] |
| CRF01_AE | 12 | 1.120±0.756 | <0.001 | 0.864[<0.001] | -2.60,0.36 | 11[91.67] | 10[83.33] | 6[50.00] |
EasyQ v2.0: NucliSens EasyQ HIV-1 version 2.0; CAP/CTMv2.0: Cobas AmpliPrep/Cobas TaqMan HIV-1 test version 2.0.
a: Values are expressed as mean±SD.
b: Significance calculated using paired t-test (p-values).
c: Correlation coefficient (R value) calculated using Pearson correlation test.
Fig 3. Agreement and linear relationship between the Cobas AmpliPrep/Cobas TaqMan HIV-1 test version 2.0 (CAP/CTM v2.0) and the NucliSens EasyQ HIV-1 version 2.0 (EasyQ v2.0) calculated using the Bland-Altman model.
(A) Agreement between EasyQ v2.0 and CAP/CTM v2.0 when used to measure all 30 samples in the panel. (B) Agreement between EasyQ v2.0 and CAP/CTM v2.0 when used to measure 11 clade Thai-B samples in the panel. (C) Agreement between EasyQ v2.0 and CAP/CTM v2.0 when used to measure 12 clade CRF01_AE samples in the panel. For A, B and C, solid horizontal lines indicate the mean values, and dashed horizontal lines indicate the +1.96SD and _1.96SD values. (D) The linear relationship between the CAP/CTM v2.0 and EasyQ v2.0 when used to measure all 30 samples. (E) The linear relationship between the CAP/CTM v2.0 and EasyQ v2.0 when used to measure 11 clade Thai-B samples. (F) The linear relationship between the CAP/CTM v2.0 and EasyQ v2.0 when used to measure 12 clade CRF01_AE samples. For D, E and F, solid line represents the fitted regression line and the dashed line represents the equality line.
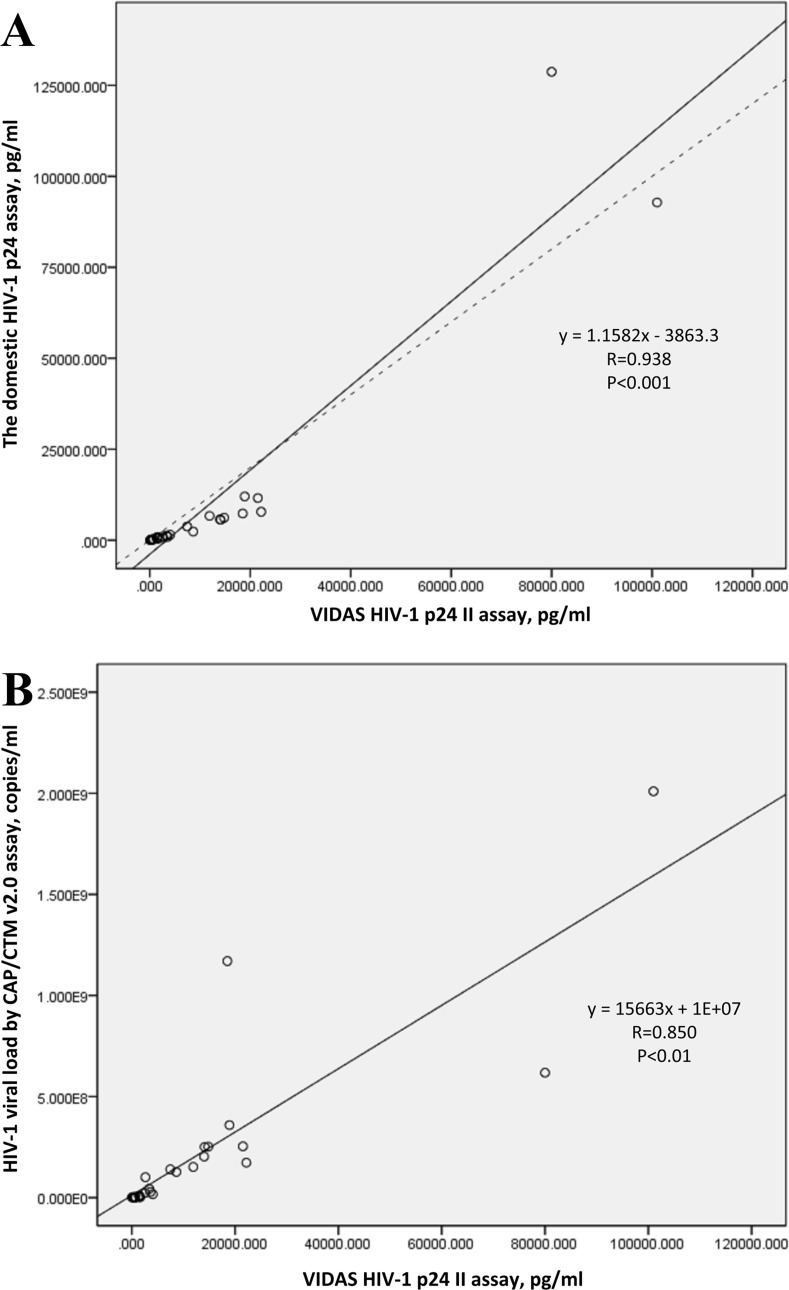
As for the two assays of p24 antigen tests, the Pearson correlation coefficient for the two HIV-1 P24 antigen assay based on all 30 samples in the panel was 0.938 (p<0.01). The correlation coefficient for the p24 concentrations tested by the BioMerieux VIDAS HIV p24 II assay and the viral loads tested by the Roche COBAS Taqman version 2.0 assay based on all the 30 isolates was 0.850 (p<0.01; Fig 4).
Fig 4. The linear relationship between the two assays of HIV-1 p24 measurement and the linear relationship between p24 antigen concentration and HIV-1 viral load based on the values of all 30 samples.
(A) The linear relationship between the BioMerieux VIDAS HIV p24 II assay and the domestic HIV-1 p24 assay when used to measure all 30 samples. Solid line represents the fitted regression line and the dashed line represents the equality line. (B) The linear relationship between HIV-1 p24 antigen concentration and viral load based on all 30 isolates, tested by BioMerieux VIDAS HIV p24 II and Roche COBAS Taqman version 2.0, respectively. Solid line represents the fitted regression line.
Discussion
With the diversity of HIV-1 increasing, HIV-1 isolates of each subtype spread broader and faster around the world. The EQAPOL program was established by the NIH/NIAID and other cooperative institutions and their efforts were aimed at the development of an HIV subtype panel that encompassed the genetic and geographic diversity currently present worldwide. Accordingly, we developed an HIV-1 isolate panel that can represent the diversity of HIV-1 strains circulating in China. This panel will help with the evaluation of HIV surveillance or diagnostic assays and research on HIV vaccines or antiviral drugs in China [13]. In our study, blood samples from HIV infected people in China were collected from 2002 to 2013. 30 HIV-1 primary strains of high-titer and high-volume were obtained successfully. These isolates were all well preserved in liquid nitrogen and can be used as the standard substances or samples in evaluation of HIV-1 assays, antiviral drug screening or vaccine development conveniently. The subtypes of these isolates not only include China’s frequent subtype B, CRF01_AEand CRF07_BC, but also a strain of subtype G which was infrequent in China was isolated from a plasma sample from Shanghai. Shown by Yi Feng and Xiang He’s research, the CRF01_AE epidemic in China is remarkably complex [35]. In their study, seven distinct phylogenetic clusters of CRF01_AE were identified. The CRF01_AE isolates in our study were found in three of the seven clusters shown in Fig 2, which means the CRF01_AE isolates in our panel can represent the current complex diversity of this subtype to some extent. We amplified and sequenced the fundamental genes; i.e., gag, pol, envC2V3 for each isolate. The co-recepter usage, glycosylation sites, four residues at the tip of the v3-loop for each isolate, also the drug-resistance mutations on gene pol were predicted to consummate the characterization of the isolates in this panel. This accurate and comprehensive characterization will make the panel convenient to use in the future.
The comparison of the p24 or viral load assays on the isolates illustrated how this panel may be used for evaluation of HIV-1 diagnostic assay performance. For example, according to Fig 3, compared with CAP/CTM v2.0, the EasyQ v2.0 showed a greater variation in the values measured for CRF01_AE samples than those for Thai-B samples. By Bland-Altman analysis, we could see that the distance between the mean values of the different results from the two assays in the viral loads of subtype CRF01_AE samples, which are shown as solid horizontal lines in Fig 3C, and the origin, which is shown as the zero point in Fig 3C (1.120), were much farther than that of Thai-B samples (0.260; Fig 3B). Furthermore, the proportion of subtype Thai-B samples showing quantitative differences between the two assays >0.5 log IU/ml or 1 log IU/ml was significantly lower than that for subtype CRF01_AE (Table 3). These data suggest higher levels of agreement between these two assays when measuring Thai-B samples than for CRF01_AE samples. A similar conclusion was shown in Sihong Xu’s study [36]. Higher values measured by CAP/CTM v2.0 may because of the fact that CAP/CTM v2.0 reduces under-quantification of the HIV-1 viral load by using two dual-labeled hybridization probes targeting both the gag and LTR regions, while EasyQ v2.0 targeted the HIV-1 gag gene only. The performance of the automated extractor of CAP/CTM v2.0 may also contribute to the higher values and stable performance of CAP/CTM v2.0. The lower agreement between the two assays when measuring subtype CRF01_AE samples may also due to different hybridization probes, which indicates that the probe targets in the sequence may not be conservative enough in subtype Thai-B and CRF01_AE, and at least one of the assays under-quantified the viral loads of subtype CRF01_AE samples. To face this problem, it is strongly suggested that the same version of the same viral load assay be used consistently during clinical treatment. Much more importantly, the genetic diversity of HIV-1 (including the genetic variability within HIV-1 strains of the same subtype) must be taken into account when designing primers and probes for HIV-1 viral load assays. Another example is the two different results for co-receptor usage prediction of GD2005003 and SD2013001 (Table 2) may be caused by the different calculation principles of the two software programs; i.e., Geno2pheno and PSSM, or the different FPR values chosen for Geno2pheno.
The entry of HIV-1 into host cells is mediated by interactions between the virus envelope (i.e., env) glycoprotein (gp120/gp41) and host-cell receptor [38]. The third hypervariable region 3 (V3) of the HIV-1 gp120 protein consists of 35 amino acids and plays an important role in viral infection by promoting the interaction between the virus and its co-receptor in the host cell membrane [39]. N-glycan represent approximately 50% of the molecular mass of gp120 and serves as a potential antigenic determinant and a shield against immune recognition [40]. It is convinced that HIV-1 escape from neutralizing antibodies through the extensive variability of the viral envelope glycoproteins, especially gp120 while the four amino acids at the tip of the V3 loop are subjected to strong purifying selection pressure due to their functional importance [41, 42]. Therefore, using the consensus sequence on envC2V3 to predict the co-receptor usage of each isolate, glycosylation sites on the v3-loop and identification of the four residues at the tip of the V3 loop is necessary for infection relevant experiments and studies.
In conclusion, by isolating, expanding, sequencing and analyzing the HIV-1 strains from blood samples of HIV-1 infected persons, our study produced a panel of HIV-1 primary strains of a variety of HIV-1 subtypes circulating in China with clear and complete fundamental sequences and biological features. Our program will continue to collect HIV-1 strains for more subtypes to develop a more comprehensive panel that can represent the diversity, the current dynamic and complex epidemic of HIV-1 more completely and accurately. Especially for samples of CRF08_BC, because it is one of the frequent subtypes circulating in China besides CRF07_BC, CRF01_AE and B. Also, more effort should be spent on the isolation of viruses from the acute/early stage of infection to analyze the transmitted or early founder viruses. This is an important step in achieving a molecular understanding of HIV-1 transmission and for potentially developing an effective HIV/AIDS vaccine since direct analysis of HIV-1 at or near the moment of transmission is practically impossible [43]. In our study, we created a basic protocol and standard for sample collection, inclusion and analysis by developing the panel. Under the circumstance of high variable HIV-1 strains of each subtype spread throughout the world, the creation of this panel will not only serves as the standard for assays, vaccines and drugs development andevaluation, but also as the samples for diversity related HIV-1 research to help improve the current situation when many researches on HIV-1 diversity still stay on the genome sequence level. By offering HIV-1 isolates isolated from blood samples directly, researches based on the panel will have high simulation and high reproducibility when compared with researches based on infectious clones of the viruses. In this way, our panel may also play a role in antiviral drug screening and vaccine development.
Acknowledgments
We would like to thank all the participants for their contributions and cooperation, as well as the local CDCs for sample provision.
Data Availability
All sequence files are available from the Los Alamos HIV Database or the GenBank (accession number(s) KP178420-KP178479). All other relevant data are within the paper.
Funding Statement
This study was supported by the National Science and Technology Special Projects on Major Infectious Diseases (Grant No. 2012ZX10001-002). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.UNAIDS, 2014. 2014 Gap report from UNAIDS. Available: http://www.unaids.org/en/resources /campaigns/2014/2014gapreport/gapreport
- 2. Sezgin E, Hendrickson SL, Jabs DA, Van Natta ML, Lewis RA, Troyer JL, et al. Effect of host genetics on incidence of HIV neuroretinal disorder in patients with AIDS. J Acquir Immune Defic Syndr. 2010;54(4):343–51. Epub 2010/06/10. 10.1097/QAI.0b013e3181deaf4d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Buonaguro L, Tornesello ML, Buonaguro FM. Human immunodeficiency virus type 1 subtype distribution in the worldwide epidemic: pathogenetic and therapeutic implications. Journal of virology. 2007;81(19):10209–19. Epub 2007/07/20. 10.1128/jvi.00872-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Church D, Gregson D, Lloyd T, Klein M, Beckthold B, Laupland K, et al. Comparison of the RealTime HIV-1, COBAS TaqMan 48 v1.0, Easy Q v1.2, and Versant v3.0 assays for determination of HIV-1 viral loads in a cohort of Canadian patients with diverse HIV subtype infections. J Clin Microbiol. 2011;49(1):118–24. Epub 2010/11/19. 10.1128/jcm.00685-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kline NE, Schwarzwald H, Kline MW. False negative DNA polymerase chain reaction in an infant with subtype C human immunodeficiency virus 1 infection. Pediatr Infect Dis J. 2002;21(9):885–6. Epub 2002/10/17. . [DOI] [PubMed] [Google Scholar]
- 6. Obaro SK, Losikoff P, Harwell J, Pugatch D. Failure of serial human immunodeficiency virus type 1 DNA polymerase chain reactions to identify human immunodeficiency virus type 1 clade A/G. Pediatr Infect Dis J. 2005;24(2):183–4. Epub 2005/02/11. . [DOI] [PubMed] [Google Scholar]
- 7. Henquell C, Jacomet C, Antoniotti O, Chaib A, Regagnon C, Brunet S, et al. Difficulties in diagnosing group o human immunodeficiency virus type 1 acute primary infection. J Clin Microbiol. 2008;46(7):2453–6. Epub 2008/05/16. 10.1128/jcm.02217-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Foglieni B, Candotti D, Guarnori I, Raffaele L, Berzuini A, Spreafico M, et al. A cluster of human immunodeficiency virus Type 1 recombinant form escaping detection by commercial genomic amplification assays. Transfusion. 2011;51(4):719–30. Epub 2010/11/23. 10.1111/j.1537-2995.2010.02942.x . [DOI] [PubMed] [Google Scholar]
- 9. Nubling CM, Heiden M, Chudy M, Kress J, Seitz R, Keller-Stanislawski B, et al. Experience of mandatory nucleic acid test (NAT) screening across all blood organizations in Germany: NAT yield versus breakthrough transmissions. Transfusion. 2009;49(9):1850–8. Epub 2009/05/21. 10.1111/j.1537-2995.2009.02212.x . [DOI] [PubMed] [Google Scholar]
- 10. Taylor BS, Hammer SM. The challenge of HIV-1 subtype diversity. N Engl J Med. 2008;359(18):1965–6. Epub 2008/10/31. 10.1056/NEJMc086373 . [DOI] [PubMed] [Google Scholar]
- 11. Ntemgwa M, Gill MJ, Brenner BG, Moisi D, Wainberg MA. Discrepancies in assignment of subtype/recombinant forms by genotyping programs for HIV type 1 drug resistance testing may falsely predict superinfection. AIDS Res Hum Retroviruses. 2008;24(7):995–1002. Epub 2008/07/03. 10.1089/aid.2008.0064 . [DOI] [PubMed] [Google Scholar]
- 12. Snoeck J, Kantor R, Shafer RW, Van Laethem K, Deforche K, Carvalho AP, et al. Discordances between interpretation algorithms for genotypic resistance to protease and reverse transcriptase inhibitors of human immunodeficiency virus are subtype dependent. Antimicrob Agents Chemother. 2006;50(2):694–701. Epub 2006/01/27. 10.1128/aac.50.2.694-701.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sanchez AM, DeMarco CT, Hora B, Keinonen S, Chen Y, Brinkley C, et al. Development of a contemporary globally diverse HIV viral panel by the EQAPOL program. J Immunol Methods. 2014;409:117–30. Epub 2014/01/23. 10.1016/j.jim.2014.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. He X, Xing H, Ruan Y, Hong K, Cheng C, Hu Y, et al. A comprehensive mapping of HIV-1 genotypes in various risk groups and regions across China based on a nationwide molecular epidemiologic survey. PLoS One. 2012;7(10):e47289 Epub 2012/10/12. 10.1371/journal.pone.0047289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guan Y, Chen J, Shao Y, Zhao Q, Zeng Y, Zhang J, et al. [Subtype and sequence analysis of the C2-V3 region of gp120 genes among human immunodeficiency virus infected IDUs in Ruili epidemic area of Yunnan Province of China]. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi. 1997;11(1):8–12. Epub 1997/03/01. . [PubMed] [Google Scholar]
- 16. Piyasirisilp S, McCutchan FE, Carr JK, Sanders-Buell E, Liu W, Chen J, et al. A recent outbreak of human immunodeficiency virus type 1 infection in southern China was initiated by two highly homogeneous, geographically separated strains, circulating recombinant form AE and a novel BC recombinant. Journal of virology. 2000;74(23):11286–95. Epub 2000/11/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Su L, Graf M, Zhang Y, von Briesen H, Xing H, Kostler J, et al. Characterization of a virtually full-length human immunodeficiency virus type 1 genome of a prevalent intersubtype (C/B') recombinant strain in China. Journal of virology. 2000;74(23):11367–76. Epub 2000/11/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tee KK, Pybus OG, Li XJ, Han X, Shang H, Kamarulzaman A, et al. Temporal and spatial dynamics of human immunodeficiency virus type 1 circulating recombinant forms 08_BC and 07_BC in Asia. Journal of virology. 2008;82(18):9206–15. Epub 2008/07/04. 10.1128/jvi.00399-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Qin G, Shao Y, Liu G. [Subtype and sequence analysis of the C2-V3 region of gp120 genes among HIV-1 strains in Sichuan province]. Zhonghua Liu Xing Bing Xue Za Zhi. 1998;19(1):39–42. Epub 1999/05/14. . [PubMed] [Google Scholar]
- 20. Li YW, Shao YM, Luo XG. [Subtype and sequence analysis of the C2-V3 region of gp120 genes among HIV-1 strains in Hubei province]. Zhonghua Liu Xing Bing Xue Za Zhi. 1997;18(4):217–9. Epub 1997/08/01. . [PubMed] [Google Scholar]
- 21. Xu JQ, Wang JJ, Han LF, Xu C, Ruan YH, Xu ZH, et al. Epidemiology, clinical and laboratory characteristics of currently alive HIV-1 infected former blood donors naive to antiretroviral therapy in Anhui Province, China. Chin Med J (Engl). 2006;119(23):1941–8. Epub 2007/01/04. . [PubMed] [Google Scholar]
- 22. Wang FX, Zhou H, Ling H, Zhou HZ, Liu WH, Shao YM, et al. Subtype and sequence analysis of HIV-1 strains in Heilongjiang Province. Chin Med J (Engl). 2007;120(22):2006–10. Epub 2007/12/11. . [PubMed] [Google Scholar]
- 23. Chen J, Young NL, Subbarao S, Warachit P, Saguanwongse S, Wongsheree S, et al. HIV type 1 subtypes in Guangxi Province, China, 1996. AIDS Res Hum Retroviruses. 1999;15(1):81–4. Epub 1999/02/19. 10.1089/088922299311754 . [DOI] [PubMed] [Google Scholar]
- 24. Yu XF, Chen J, Shao Y, Beyrer C, Liu B, Wang Z, et al. Emerging HIV infections with distinct subtypes of HIV-1 infection among injection drug users from geographically separate locations in Guangxi Province, China. J Acquir Immune Defic Syndr. 1999;22(2):180–8. Epub 2000/06/08. . [DOI] [PubMed] [Google Scholar]
- 25. Xing H, Liang H, Wan ZY, Chen X, Wei M, Ma PF, et al. [Distribution of recombinant human immunodeficiency virus type-1 CRF01_AE strains in China and its sequence variations in the env V3-C3 region]. Zhonghua Yu Fang Yi Xue Za Zhi. 2004;38(5):300–4. Epub 2004/10/23. . [PubMed] [Google Scholar]
- 26. Han X, An M, Zhang W, Cai W, Chen X, Takebe Y, et al. Genome Sequences of a Novel HIV-1 Circulating Recombinant Form, CRF55_01B, Identified in China. Genome Announc. 2013;1(1). Epub 2013/02/14. 10.1128/genomeA.00050-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wei H, Liu Y, Feng Y, Hsi J, Xing H, He X, et al. Genome sequence of a novel HIV-1 circulating recombinant form (CRF57_BC) identified from Yunnan, China. AIDS Res Hum Retroviruses. 2014;30(4):384–8. Epub 2013/11/12. 10.1089/aid.2013.0228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gao L, Hanson MN, Balakrishnan M, Boyer PL, Roques BP, Hughes SH, et al. Apparent defects in processive DNA synthesis, strand transfer, and primer elongation of Met-184 mutants of HIV-1 reverse transcriptase derive solely from a dNTP utilization defect. J Biol Chem. 2008;283(14):9196–205. Epub 2008/01/26. M710148200 [pii] 10.1074/jbc.M710148200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Li X, Ning C, He X, Yang Y, Li F, Xing H, et al. Genome Sequences of a Novel HIV-1 Circulating Recombinant Form (CRF61_BC) Identified among Heterosexuals in China. Genome Announc. 2013;1(3). Epub 2013/07/03. 10.1128/genomeA.00326-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wei H, His J, Feng Y, Xing H, He X, Liao L, et al. Identification of a novel HIV-1 circulating recombinant form (CRF62_BC) in western Yunnan of China. AIDS Res Hum Retroviruses. 2014;30(4):380–3. Epub 2013/10/30. 10.1089/aid.2013.0235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hsi J, Wei H, Xing H, Feng Y, He X, Liao L, et al. Genome sequence of a Novel HIV-1 circulating recombinant form (CRF64_BC) identified from Yunnan, China. AIDS Res Hum Retroviruses. 2014;30(4):389–93. Epub 2013/11/12. 10.1089/aid.2013.0234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Feng Y, Wei H, Hsi J, Xing H, He X, Liao L, et al. Identification of a novel HIV Type 1 circulating recombinant form (CRF65_cpx) composed of CRF01_AE and subtypes B and C in Western Yunnan, China. AIDS Res Hum Retroviruses. 2014;30(6):598–602. Epub 2013/11/28. 10.1089/aid.2013.0233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Manak M, Sina S, Anekella B, Hewlett I, Sanders-Buell E, Ragupathy V, et al. Pilot studies for development of an HIV subtype panel for surveillance of global diversity. AIDS Res Hum Retroviruses. 2012;28(6):594–606. Epub 2011/12/14. 10.1089/aid.2011.0271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Liu W, Liang Sj Fau—Yang J-y, Yang Jy Fau—Li J-j, Li Jj Fau—Wang B, Wang B Fau—Chen L-l, Chen Ll Fau—Li L, et al. [Distribution of HIV-1 subtypes in Guangxi Zhuang Autonomous Region, 2008–2009]. (0254–6450 (Print)). [PubMed] [Google Scholar]
- 35. Feng Y, He X, Hsi JH, Li F, Li X, Wang Q, et al. The rapidly expanding CRF01_AE epidemic in China is driven by multiple lineages of HIV-1 viruses introduced in the 1990s. AIDS (London, England). 2013;27(11):1793–802. Epub 2013/06/29. 10.1097/QAD.0b013e328360db2d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Xu S, Song A, Nie J, Li X, Meng S, Zhang C, et al. Comparison between the automated Roche Cobas AmpliPrep/Cobas TaqMan HIV-1 test version 2.0 assay and its version 1 and Nuclisens HIV-1 EasyQ version 2.0 assays when measuring diverse HIV-1 genotypes in China. J Clin Virol. 2012;53(1):33–7. Epub 2011/11/05. 10.1016/j.jcv.2011.10.001 . [DOI] [PubMed] [Google Scholar]
- 37. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10. Epub 1986/02/08. . [PubMed] [Google Scholar]
- 38. Weissenhorn W, Dessen A, Harrison SC, Skehel JJ, Wiley DC. Atomic structure of the ectodomain from HIV-1 gp41. Nature. 1997;387(6631):426–30. Epub 1997/05/22. 10.1038/387426a0 . [DOI] [PubMed] [Google Scholar]
- 39. Hwang SS, Boyle TJ, Lyerly HK, Cullen BR. Identification of the envelope V3 loop as the primary determinant of cell tropism in HIV-1. Science (New York, NY). 1991;253(5015):71–4. Epub 1991/07/05. . [DOI] [PubMed] [Google Scholar]
- 40. Zhu X, Borchers C, Bienstock RJ, Tomer KB. Mass spectrometric characterization of the glycosylation pattern of HIV-gp120 expressed in CHO cells. Biochemistry. 2000;39(37):11194–204. Epub 2000/09/14. . [DOI] [PubMed] [Google Scholar]
- 41. Kwong PD, Doyle ML, Casper DJ, Cicala C, Leavitt SA, Majeed S, et al. HIV-1 evades antibody-mediated neutralization through conformational masking of receptor-binding sites. Nature. 2002;420(6916):678–82. Epub 2002/12/13. 10.1038/nature01188 . [DOI] [PubMed] [Google Scholar]
- 42. Liu Y, Curlin ME, Diem K, Zhao H, Ghosh AK, Zhu H, et al. Env length and N-linked glycosylation following transmission of human immunodeficiency virus Type 1 subtype B viruses. Virology. 2008;374(2):229–33. Epub 2008/03/04. 10.1016/j.virol.2008.01.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Keele BF, Giorgi EE, Salazar-Gonzalez JF, Decker JM, Pham KT, Salazar MG, et al. Identification and characterization of transmitted and early founder virus envelopes in primary HIV-1 infection. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(21):7552–7. Epub 2008/05/21. 10.1073/pnas.0802203105 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All sequence files are available from the Los Alamos HIV Database or the GenBank (accession number(s) KP178420-KP178479). All other relevant data are within the paper.