Abstract
Objective
This study aimed to assess three-dimensional changes in the temporomandibular joint positions and mandibular dimensions after correction of dental factors restricting mandibular growth in patients with Class II division 1 or division 2 malocclusion in the pubertal growth period.
Methods
This prospective clinical study included 14 patients each with Class II division 1 (group I) and Class II division 2 (group II) malocclusions. The quad-helix was used for maxillary expansion, while utility arches were used for intrusion (group I) or protrusion and intrusion (group II) of the maxillary incisors. After approximately 2 months of treatment, an adequate maxillary arch width and acceptable maxillary incisor inclination were obtained. The patients were followed for an average of 6 months. Intraoral and extraoral photographs, plaster models, and cone-beam computed tomography (CBCT) images were obtained before and after treatment. Lateral cephalometric and temporomandibular joint measurements were made from the CBCT images.
Results
The mandibular dimensions increased in both groups, although mandibular positional changes were also found in group II. There were no differences in the condylar position within the mandibular fossa or the condylar dimensions. The mandibular fossa depth and condylar positions were symmetrical at treatment initiation and completion.
Conclusions
Class II malocclusion can be partially corrected by achieving an ideal maxillary arch form, particularly in patients with Class II division 2 malocclusion. Restrictions of the mandible in the transverse or sagittal plane do not affect the temporomandibular joint positions in these patients because of the high adaptability of this joint.
Keywords: Computed tomography, Early treatment, Temporomandibular joint, Class II
INTRODUCTION
Class II malocclusion is a common clinical entity and is categorized into Class II division 1 and Class II division 2 malocclusions. The former is characterized by labially inclined maxillary incisors and an excessive overjet,1 while the latter is characterized by a Class II molar relationship with retroclined maxillary incisors.2 According to McNamara and Brudon,3 one of the most important causes of Class II malocclusion is maxillary constriction. Relative constriction of the maxilla leads to mandibular retrusion.4 Therefore, maxillary expansion in the early phase can lead to the forward positioning of the mandible during the retention period in patients with Class II malocclusion associated with maxillary constriction.3,5,6,7
Rapid palatal expansion appliances are commonly used in studies evaluating mandibular positional changes after maxillary expansion.4,6,8,9,10 However, Sayin and Türkkahraman11 recommended slow maxillary expansion rather than rapid maxillary expansion for the treatment of Class II division 1 malocclusion in the absence of skeletal constriction. One of the most effective appliances used for slow maxillary expansion is the quad-helix.12 In Class II division 2 malocclusion, the mandible is restricted by retroclined upper incisors.13,14 Therefore, incisor protrusion using utility arches is also necessary in addition to maxillary expansion using the quad-helix.12,15,16 In either case, the goal of treatment is to facilitate the spontaneous correction of Class II malocclusion by eliminating the factors restricting mandibular movement.
Spontaneous correction is generally achieved not through mandibular growth but through the elimination of occlusal interferences that enables the mandible to move forward to a more comfortable position.6,7,13,17 Mandibular growth is difficult to distinguish from mandibular positional changes without clear assessments of the temporomandibular joint and mandibular body. Therefore, the use of cone-beam computed tomography (CBCT) for temporomandibular joint imaging can provide better results.18,19,20,21 To the best of our knowledge, no studies have evaluated three-dimensional (3D) mandibular positional changes after the elimination of maxillary occlusal interferences in patients with Class II division 1 or division 2 malocclusion.
Therefore, this study aimed to investigate and compare 3D changes in the mandibular dimensions and temporomandibular joint positions in patients with Class II division 1 or division 2 malocclusion in the pubertal growth period after correction of the maxillary arch form using the quad-helix and utility arches.
MATERIALS AND METHODS
Patients in the pubertal growth period determined using the cervical vertebral maturation method22 who exhibited Class II division 1 or division 2 malocclusion with transverse maxillary deficiency were considered eligible for this pro spective clinical trial. On the basis of these criteria, 14 patients with Class II division 1 malocclusion (group I) and 14 with Class II division 2 malocclusion (group II) were recruited from the Department of Orthodontics, Faculty of Dentistry, Hacettepe University (Ankara, Turkey). Group I comprised eight girls and six boys and group II comprised six girls and eight boys. Ethical approval for this investigation was granted by the Hacettepe University Ethical Committee of Non-Invasive Clinical Research (institutional review board number: LUT 12/09-02). All of the patients and their guardians were informed and signed informed consent.
None of the patients had a unilateral or bilateral posterior crossbite, although transverse maxillary deficiency was evident during forward mandibular movement to achieve a Class I relationship. Minimal anterior crowding was present (0-3 mm). Group I patients showed a mean overjet of 8.2 ± 3.6 mm and a mean overbite of 2.5 ± 1.4 mm; the corresponding values in group II were 5.4 ± 1.7 mm and 4.4 ± 1.0 mm, respectively.
Intraoral and extraoral photographs and CBCT images were obtained for all patients at the beginning of treatment (T0) and after the follow-up period (T1). After recording initial impressions, quad-helix appliances were fabricated and activated up to one molar width before cementation. In the same appointment, the quad-helix was cemented, the maxillary incisors were bonded, and leveling utility arches were placed. After 5 weeks, intrusion or intrusion and protrusion utility arches were placed in groups I and II, respectively. Once an acceptable maxillary arch width, a U-shaped arch form, and an ideal incisor inclination were achieved, the patients were followed for an average of 6 months to assess mandibular adaptation. After this period, follow-up impressions were recorded (T1).
CBCT was performed using the Iluma Cone Beam CT Scanner (3M IMTEC, Ardmore, OK, USA) at 3.8 mA, 120 kVp, and a 19 × 24 field of view. The patients were seated in a natural head posture and maximum dental intercuspation like most of the studies that evaluate the temporomandibular joint.18,19,20,21 From the CBCT images, lateral cephalometric and panoramic radiographs were created using Quick Ceph Studio (Quick Ceph System, San Diego, CA, USA). Cephalometric analyses were performed using these radiographs.
For temporomandibular joint measurements, the CBCT images were saved as Digital Imaging and Communications in Medicine files and processed in the OsiriX medical imaging software program (Open-Source, OsiriX Medical Imaging Software, www.osirix-viewer.com), as described by Leonardi et al.23 By determining the long axis of the condyle in the coronal and axial sections, a sagittal image (Figure 1) was constructed.
Figure 1. Anterior (1), superior (2), and posterior (3) joint spaces and the mandibular fossa depth (4) on a sagittal image of the right temporomandibular joint.
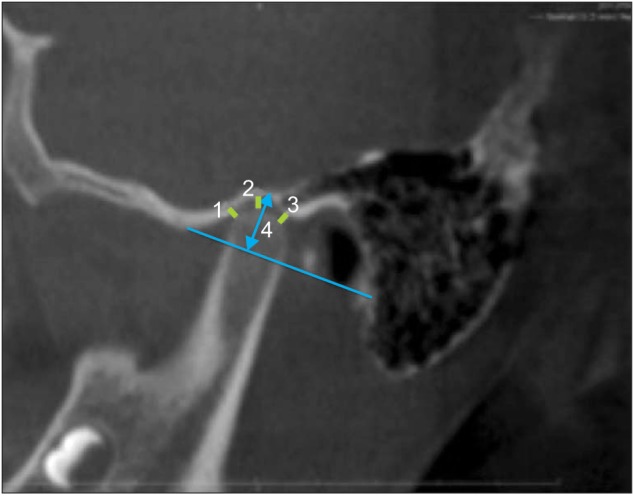
From the sagittal image, the following linear measurements were made (Figure 1).
Anterior joint space: the shortest distance between the most anterior point of the condyle and the posterior wall of the articular tubercle
Superior joint space: the shortest distance between the most superior point of the condyle and the deepest point of the mandibular fossa
Posterior joint space: the shortest distance between the most posterior point of the condyle and the posterior wall of the mandibular fossa
Depth of the mandibular fossa: distance between the deepest point of the mandibular fossa and the plane formed by the most inferior point of the articular tubercle to the most inferior point of the auditory meatus.
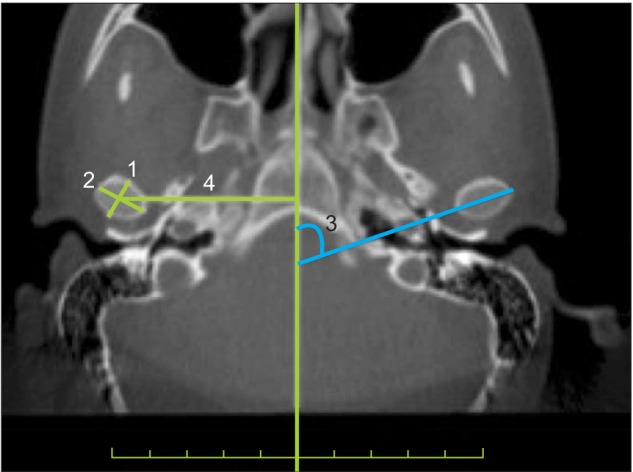
Subsequently, the midsagittal plane was determined in the coronal and sagittal sections as a plane perpendicular to the anterior nasal spine-posterior nasal spine line and an axial image was constructed. From the axial image, the following linear measurements were made (Figure 2): Greatest anteroposterior diameter of the mandibular condyle; greatest mediolateral diameter of the mandibular condyle; angle between the long axis of the mandibular condyle and the midsagittal plane; vertical distance from the geometric centers of the condyles to the midsagittal plane.
Figure 2. The greatest anteroposterior (1) and mediolateral (2) diameters of the mandibular condyle, vertical distance from the geometric centers of the condyles to the midsagittal plane (4), and the angle between the long axis of the mandibular condyle and the midsagittal plane (3) on an axial image of the temporomandibular joint.
Statistical analysis
Every measurement was made twice by the same blinded observer, with a 3-week interval between measurements. To assess the reproducibility of all measurements, intraclass correlation coefficients and 95% confidence intervals were determined (Table 1).
Table 1. ICC and 95% CI for pre- and post-treatment measurements to assess reproducibility in patients with Class II division 1 or division 2 malocclusion.
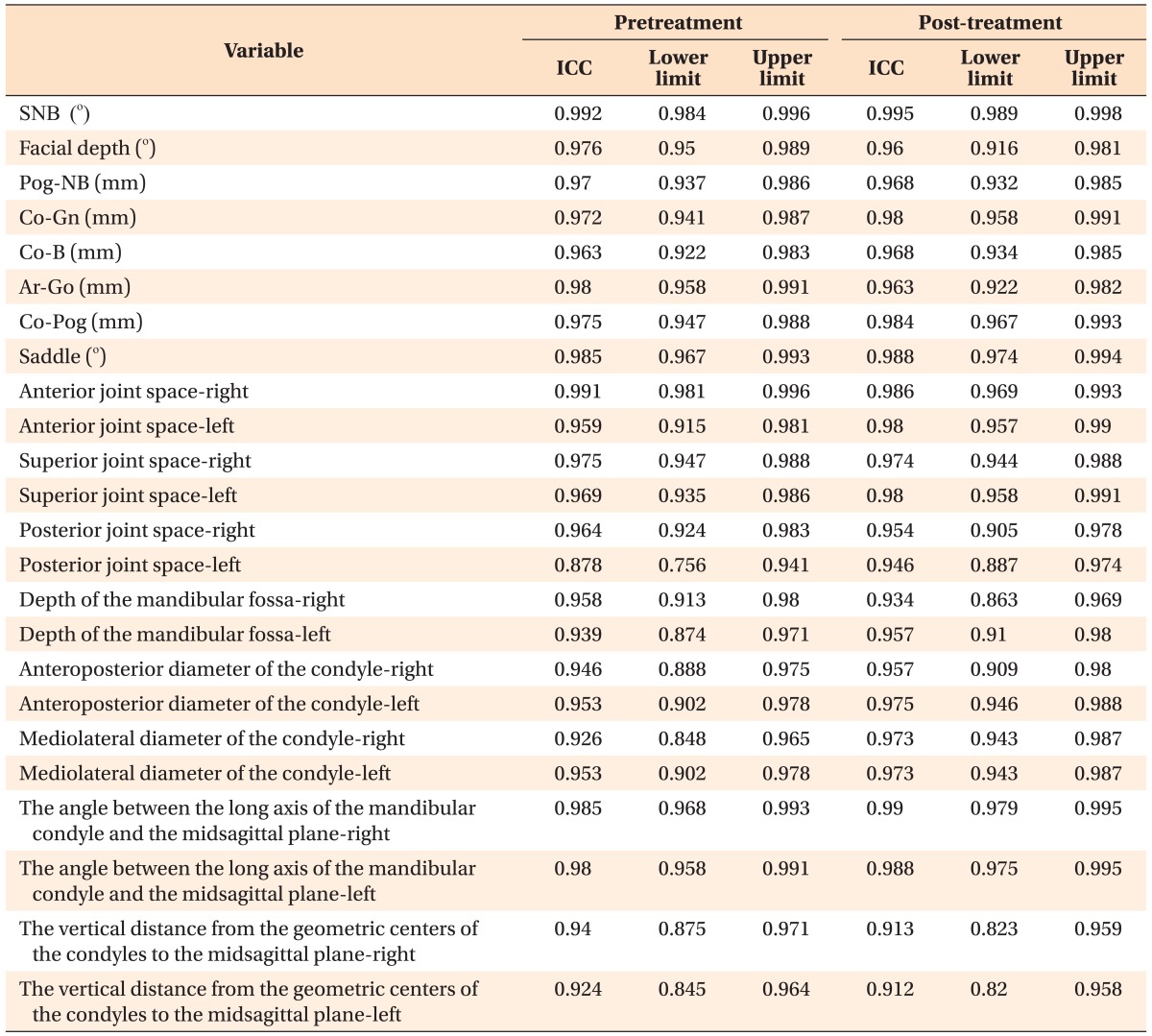
ICC, Intraclass Correlation Coefficient; CI, confidence interval; SNB, Sella-Nasion-B point angle; Pog-NB, distance from Pogonion to Nasion-B point perpendicular; Co-Gn, Condylion-Gnathion distance; Co-B, Condylion-B point distance; Ar-Go, Articulare-Gonion distance; Co-Pog, Condylion-Pogonion distance.
The data were analyzed using SPSS for Windows version 11.5 (SPSS Inc., Chicago IL, USA). The Shapiro-Wilks test was used to examine the distribution of constant variables. Descriptive statistics are shown as means ± standard deviations.
Significant differences in mean values between the two groups were assessed using Student's t-test. To determine statistically significant changes in the groups, the dependent t-test was used for the mean values.
A p-value of < 0.05 was considered statistically significant. To control for type 1 errors, Bonferroni correction was applied to all multiple comparisons.
RESULTS
The mean age at T0 was 11.2 ± 1.3 and 12 ± 0.9 years for the girls and boys, respectively, in group I and 10.9 ± 1.1 and 11.5 ± 1.3 years for the girls and boys, respectively, in group II. At the beginning of treatment, six and eight patients in group I were in the cervical stage (CS)2 and CS3 periods, respectively, while nine and five patients in group II were in the CS2 and CS3 periods, respectively.22 The mean treatment duration was 8 months in both groups. No statistically significant differences were observed in the mean age, cervical vertebral maturation stage, and mean treatment duration between the two groups (p < 0.05).
The cephalometric measurements of dentoskeletal changes in both groups and the significance of these measurements are shown in Table 2.
Table 2. Cephalometric measurements of dentoskeletal changes achieved by orthodontic treatment in patients with Class II division 1 or division 2 malocclusion.
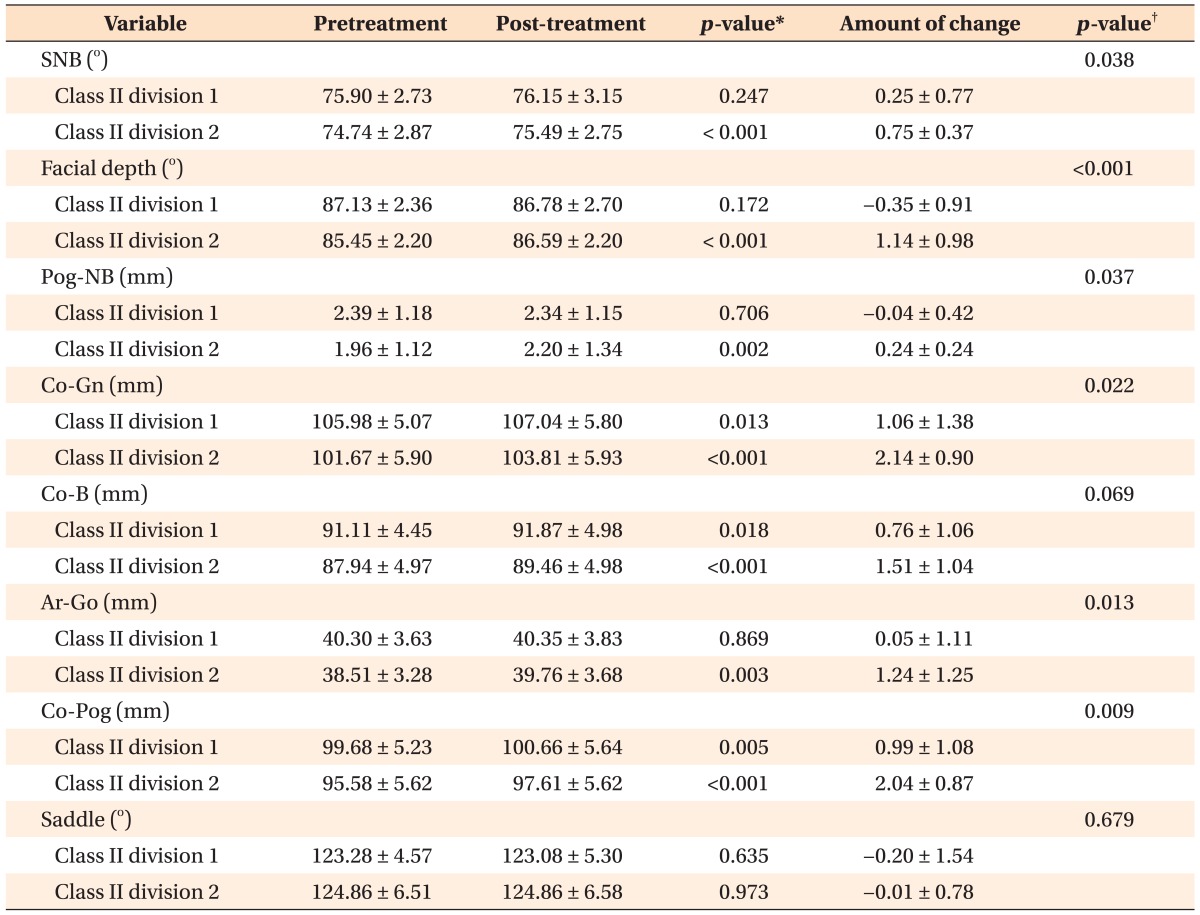
Values are presented as mean ± standard deviation.
SNB, Sella-Nasion-B point angle; Pog-NB, Distance from Pogonion to Nasion-B point perpendicular; Co-Gn, Condylion-Gnathion distance; Co-B, Condylion-B point distance; Ar-Go, Articulare-Gonion distance; Co-Pog, Condylion-Pogonion distance.
*For comparison of pre- and post-treatment measurements within groups, p < 0.025 according to Bonferroni correction was considered statistically significant.
†For comparison of treatment effects between groups, p < 0.05 was considered statistically significant.
In both groups, the Condylion-Gnathion distance (Co-Gn), Condylion-B point distance (Co-B), and Condylion-Pogonion distance (Co-Pog) distances increased significantly (p < 0.05). However, in group II, Sella-Nasion-B point angle (SNB) and the facial depth angles as well as the Distance from Pogonion to Nasion-B point perpendicular (Pog-NB) and Articulare-Gonion distance (Ar-Go) distances also increased significantly (p < 0.05).
The results of the temporomandibular joint measurements and the significance of the changes are shown in Tables 3, 4, and 5. In both groups, the anterior, superior, and posterior joint spaces and the anteroposterior and mediolateral condylar measurements did not show significant changes after treatment (p > 0.025). At T0 and T1, there were no statistically significant differences between groups in the mandibular joint depth, the angle between the long axis of the mandibular condylar process and the midsagittal plane, and the vertical distance from the geometric centers of the condyles to the midsagittal plane (p > 0.0125). Moreover, there was no difference in any evaluated parameter between the right and left temporomandibular joints in both groups (p > 0.0125).
Table 3. Pre- and post-treatment TMJ measurements in patients with Class II division 1 or division 2 malocclusion.
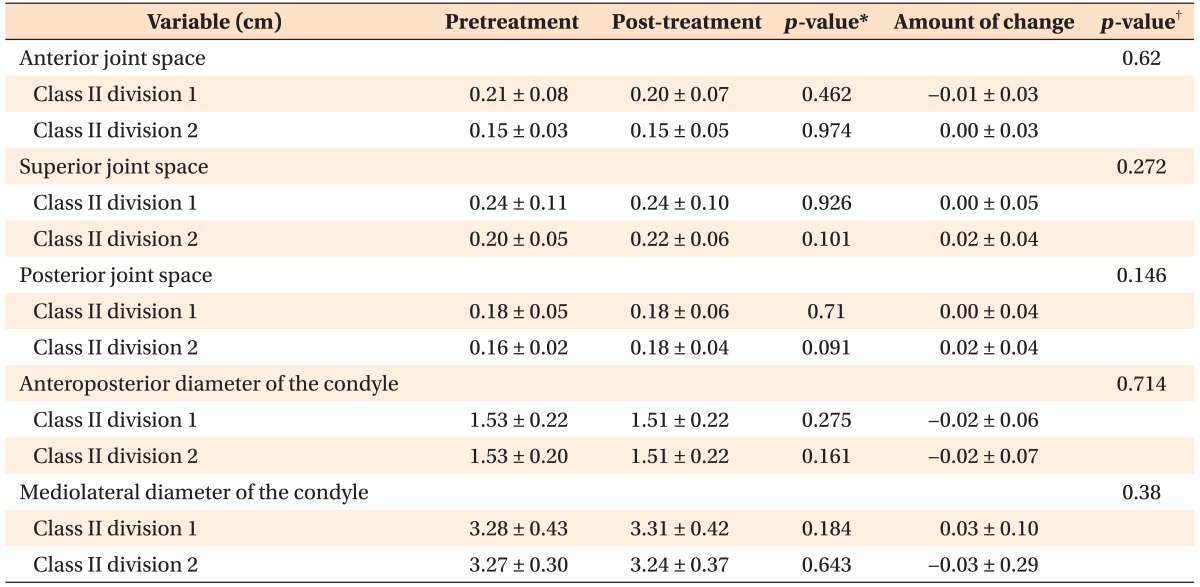
Values are presented as mean ± standard deviation.
TMJ, Temporomandibular joint.
*For comparison of pre- and post-treatment measurements within groups, p < 0.025 according to Bonferroni correction was considered statistically significant.
†For comparison of treatment effects between groups, p < 0.05 was considered statistically significant.
Table 4. Pretreatment measurements for the right and left TMJ in patients with Class II division 1 or 2 malocclusion.
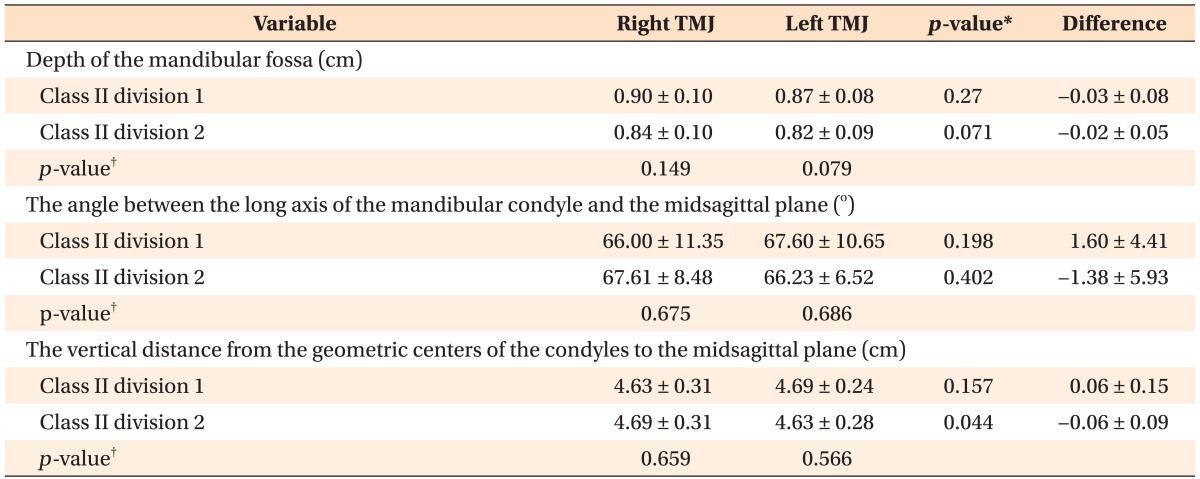
Values are presented as mean ± standard deviation.
TMJ, Temporomandibular joint.
*For comparison of pretreatment measurements for the right and left TMJ within groups, p < 0.0125 according to Bonferroni correction was considered statistically significant.
†For comparison of pretreatment measurements for the right and left TMJ between groups, p < 0.0125 according to Bonferroni correction was considered statistically significant.
Table 5. Post-treatment measurements for the right and left TMJ in patients with Class II division 1 or 2 malocclusion.
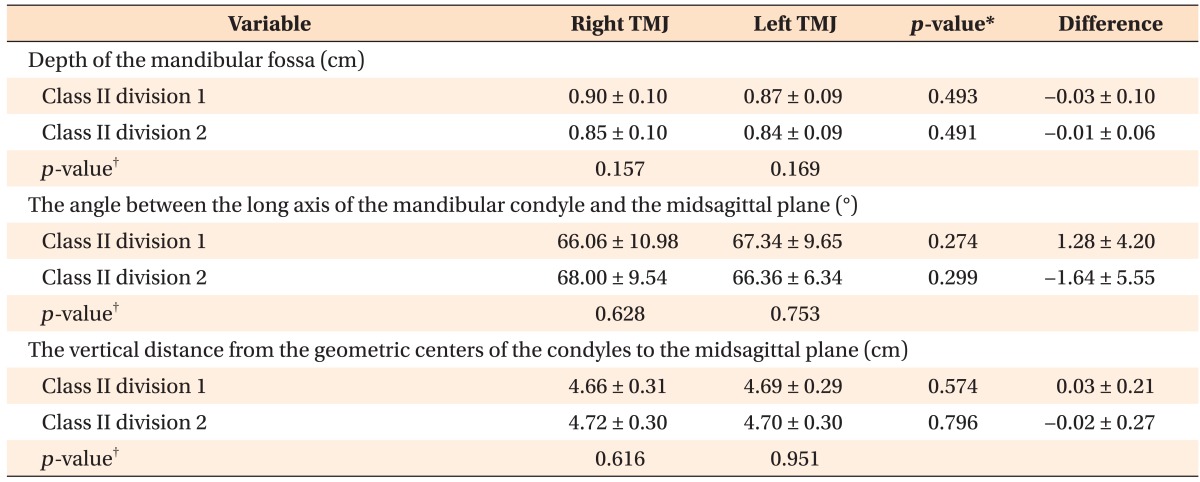
TMJ, temporomandibular joint.
*For comparison of post-treatment measurements for the right and left TMJ within groups, p < 0.0125 according to Bonferroni correction was considered statistically significant.
†For comparison of post-treatment measurements for the right and left TMJ between groups, p < 0.0125 according to Bonferroni correction was considered statistically significant.
DISCUSSION
A few studies18,23 have evaluated 3D changes in the temporomandibular joint positions after orthodontic treatment using CBCT, although none of them evaluated positional changes after the elimination of occlusal interferences in patients with Class II division 1 or division 2 malocclusion. The current study conducted 3D assessments of changes in the temporomandibular joint positions after the elimination of occlusal interferences for free mandibular movement in the transverse and sagittal planes in patients with Class II division 1 or division 2 malocclusion. This study did not use a control group for ethical reasons, although the patients in both groups were in the same cervical vertebral maturation stage.
Guest et al.8 compared 50 patients with a mixed dentition who were treated by acrylic-splinted rapid maxillary expansion with a control group of 50 subjects. The Co-Gn distance showed a mean increase of 1.3 mm in the treated group relative to the control values, with a statistically significant difference. In the present study, the increase in the Co-Gn, Co-B, and Co-Pog distances was statistically significant in both groups. However, in group II, SNB and the facial depth angles as well as the Pog-NB and Ar-Go distances also showed statistically significant increases, indicating that in patients with Class II division 2 malocclusion, the elimination of maxillary interferences may lead to a greater increase in the mandibular dimensions.
Timmons17 concluded that the mandibular position could change with cracking of the occlusal locks. Cleall and BeGole16 suggested that protrusion of retruded maxillary incisors could lead to changes in mandibular closure in patients with Class II division 2 malocclusion. In the present study, mandibular dimensional changes were achieved by establishing an ideal maxillary dental arch form, particularly in patients with Class II division 2 malocclusion.
The saddle angle did not change in both groups, indicating no changes in the temporomandibular joint positions. Moreover, measurements of the temporomandibular joint showed no statistically significant changes in the anterior, superior, and posterior joint spaces and the anteroposterior and mediolateral distances of the condyle between T0 and T1. Aras et al.24 used the Forsus™ (3M Unitek Co., Monrovia, CA, USA) fatigue resistant device in 29 Class II patients in the pubertal peak period for 9 months and evaluated the temporomandibular joint positions using magnetic resonance imaging (MRI). Although the mandibular dimensions increased significantly, no changes were observed in the temporomandibular joint positions. The authors concluded that the changes in the mandible could be related to the appositional growth of the condyle and glenoid fossa. To identify remodeling using MRI, images should be obtained more frequently. In the present study, CBCT records were obtained 6 months after maxillary arch correction. Therefore, condylar remodeling could have been the reason for the unchanged temporomandibular joint positions.
Ruf and Pancherz25 treated 15 patients with Class II malocclusion using the Herbst appliance and performed MRI before, 6-12 weeks after, and at the end of treatment. On the 6-12-week images, 20 of 30 condyles showed signs of remodeling at the posterior and superior borders, and 22 of the joints showed glenoid fossa remodeling. However, on comparison of pre- and post-treatment MRI findings, no statistically significant differences were observed in the position of the condyle in the glenoid fossa. The study concluded that MRI should be performed more frequently to appreciate glenoid fossa and condylar remodeling.
In the present study, functional treatment methods were not employed. However, after eliminating the factors restricting mandibular movement in the transverse and sagittal planes, changes in the mandible and temporomandibular joints were assessed and compared between patients with Class II division 1 and those with Class II division 2 malocclusion. The results revealed statistically significant increases in the mandibular dimensions with forward movement of the mandible in the latter, but not in the former. These changes could be related to condylar and glenoid fossa remodeling after the mandibular positional changes. However, to confirm this hypothesis and rule out the changes related to physiological growth, further studies assessing temporomandibular joint images at more frequent intervals are necessary. In the present study, CBCT images were obtained 6 months after achieving the ideal maxillary arch shape. This minimum time interval was accepted to rule out the changes related to physiological growth; furthermore, a minimum 6-month period is necessary for the adaptation of the masticatory muscles to the changing functional demands.26,27,28,29
The temporomandibular joint is highly adaptable and remodels in response to varying functional demands. Vitral et al.18 treated a patient with a functional unilateral posterior crossbite using rapid maxillary expansion and observed adaptation and remodeling of the condyle on CBCT images obtained 7 months after treatment. Leonardi et al.23 evaluated the condyle-fossa relationship before and after rapid maxillary expansion in patients with a functional posterior crossbite and compared the findings with those for a control group of 13 subjects. At the beginning of treatment, there were no statistically significant differences in the anterior, superior, and posterior joint spaces between the sides with and without a crossbite. After rapid maxillary expansion, the superior and the posterior joint spaces increased significantly on the side with a crossbite, while only the superior joint space increased on the contralateral side. These results are not in accordance with those of the present study. However, in the above-mentioned study, the patients had a functional crossbite before treatment; this could have affected the initial joint positions. Symmetrical joint positions seen before the treatment could be due to the adaptation of the temporomandibular joint. The final impressions were recorded only 18 days after treatment, which may have been too early for the joints to adapt to the new position of the mandible. In the present study, although some mandibular dimensional changes were observed because of possible temporomandibular joint adaptation after 6 months, the mandibular positional changes were not in accordance with the temporomandibular joint positional changes, indicating that the temporomandibular joint positions do not change, irrespective of mandibular restriction in the transverse or sagittal plane. Therefore, the ideal temporomandibular joint positions can be established in both conditions.
In the present study, no statistically significant differences were found in the mandibular fossa depth, angle between the long axis of the mandibular condyle and the midsagittal plane, and vertical distance from the geometric centers of the condyles to the midsagittal plane between the right and left temporomandibular joints at the beginning and end of treatment; this was consistent with the findings in most previous studies.19,21,23
CONCLUSION
The following conclusions were drawn after treating patients with Class II division 1 or division 2 malocclusion to achieve the ideal maxillary arch form in this study.
The mandibular dimensions significantly increased in both groups after treatment. However, the increase in mandibular dimensions and the mandibular positional changes were significantly greater in patients with Class II division 2 malocclusion than in patients with Class II division 1 malocclusion. Nevertheless, a Class II relationship can be corrected to some extent through the achievement of an ideal maxillary arch form.
In both groups, there were no statistically significant changes in the anterior, superior, and posterior joint spaces and the anteroposterior and mediolateral condylar widths after treatment, indicating that restrictions of the mandible in the transverse or sagittal plane do not affect the temporomandibular joint positions because of the high adaptability of this joint.
At the beginning and end of treatment, there were no statistically significant differences in the mandibular fossa depth, angle between the long axis of the mandibular condyle and the midsagittal plane, and vertical distance from the geometric centers of the condyles to the midsagittal plane between the right and left temporomandibular joints. So this treatment didn't lead to asymmetrical positioning of the temporomandibular joint.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Bishara SE. Class II Malocclusions: Diagnostic and clinical considerations with and without treatment. Semin Orthod. 2006;12:11–24. [Google Scholar]
- 2.Yousefian J, Trimble D, Folkman G. A new look at the treatment of Class II Division 2 malocclusions. Am J Orthod Dentofacial Orthop. 2006;130:771–778. doi: 10.1016/j.ajodo.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 3.McNamara JA, Brudon WL. Orthodontic and orthopedic treatment in the mixed dentition. Ann Arbor, Mi: Needham Press; 1993. p. 365. [Google Scholar]
- 4.Gianelly AA Boston University School of Dental Medicine. Rapid palatal expansion in the absence of crossbites: added value? Am J Orthod Dentofacial Orthop. 2003;124:362–365. doi: 10.1016/s0889-5406(03)00568-7. [DOI] [PubMed] [Google Scholar]
- 5.Reichenbach E, Bruückl H, Taatz H. Kieferorthopädische klinik und therapie. Leipzig: J.A. Barth; 1971. p. 248. [Google Scholar]
- 6.Lima Filho RM, Lima AC, de Oliveira Ruellas AC. Spontaneous correction of Class II malocclusion after rapid palatal expansion. Angle Orthod. 2003;73:745–752. doi: 10.1043/0003-3219(2003)073<0745:SCOCIM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Marshall SD, Southard KA, Southard TE. Early transverse treatment. Semin Orthod. 2005;11:130–139. [Google Scholar]
- 8.Guest SS, McNamara JA, Jr, Baccetti T, Franchi L. Improving Class II malocclusion as a side-effect of rapid maxillary expansion: a prospective clinical study. Am J Orthod Dentofacial Orthop. 2010;138:582–591. doi: 10.1016/j.ajodo.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 9.Volk T, Sadowsky C, Begole EA, Boice P. Rapid palatal expansion for spontaneous Class II correction. Am J Orthod Dentofacial Orthop. 2010;137:310–315. doi: 10.1016/j.ajodo.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 10.McNamara JA., Jr Early intervention in the transverse dimension: is it worth the effort? Am J Orthod Dentofacial Orthop. 2002;121:572–574. doi: 10.1067/mod.2002.124167. [DOI] [PubMed] [Google Scholar]
- 11.Sayin MO, Türkkahraman H. Malocclusion and crowding in an orthodontically referred Turkish population. Angle Orthod. 2004;74:635–639. doi: 10.1043/0003-3219(2004)074<0635:MACIAO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Ricketts RM. Bioprogressive therapy. Denver, CO: Rocky Mountain/Orthodontics; 1979. p. 141. [Google Scholar]
- 13.Pancherz H, Zieber K, Hoyer B. Cephalometric characteristics of Class II division 1 and Class II division 2 malocclusions: a comparative study in children. Angle Orthod. 1997;67:111–120. doi: 10.1043/0003-3219(1997)067<0111:CCOCID>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Hedges R. A cephalometric evaluation of class II, Division 2. Angle Orthod. 1958;28:191–197. [Google Scholar]
- 15.Sabri R. Treatment of a Class II Division 2 malocclusion with space reopening for a single-tooth implant. Am J Orthod Dentofacial Orthop. 2001;119:135–142. doi: 10.1067/mod.2001.112116. [DOI] [PubMed] [Google Scholar]
- 16.Cleall JF, BeGole EA. Diagnosis and treatment of class II division 2 malocclusion. Angle Orthod. 1982;52:38–60. doi: 10.1043/0003-3219(1982)052<0038:DATOCI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Timmons LS. Induced change in the anteroposterior relationship of the jaws. Angle Orthod. 1972;42:245–251. doi: 10.1043/0003-3219(1972)042<0245:ICITAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Vitral RW, Fraga MR, de Oliveira RS, de Andrade Vitral JC. Temporomandibular joint alterations after correction of a unilateral posterior crossbite in a mixed-dentition patient: a computed tomography study. Am J Orthod Dentofacial Orthop. 2007;132:395–399. doi: 10.1016/j.ajodo.2005.12.033. [DOI] [PubMed] [Google Scholar]
- 19.Rodrigues AF, Fraga MR, Vitral RW. Computed tomography evaluation of the temporomandibular joint in Class I malocclusion patients: condylar symmetry and condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2009;136:192–198. doi: 10.1016/j.ajodo.2007.07.032. [DOI] [PubMed] [Google Scholar]
- 20.Vitral RW, Telles Cde S. Computed tomography evaluation of temporomandibular joint alterations in class II Division 1 subdivision patients: condylar symmetry. Am J Orthod Dentofacial Orthop. 2002;121:369–375. doi: 10.1067/mod.2002.121664. [DOI] [PubMed] [Google Scholar]
- 21.Vitral RW, Telles Cde S, Fraga MR, de Oliveira RS, Tanaka OM. Computed tomography evaluation of temporomandibular joint alterations in patients with class II division 1 subdivision malocclusions: condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2004;126:48–52. doi: 10.1016/j.ajodo.2003.06.012. [DOI] [PubMed] [Google Scholar]
- 22.Hassel B, Farman AG. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofacial Orthop. 1995;107:58–66. doi: 10.1016/s0889-5406(95)70157-5. [DOI] [PubMed] [Google Scholar]
- 23.Leonardi R, Caltabiano M, Cavallini C, Sicurezza E, Barbato E, Spampinato C, et al. Condyle fossa relationship associated with functional posterior crossbite, before and after rapid maxillary expansion. Angle Orthod. 2012;82:1040–1046. doi: 10.2319/112211-725.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aras A, Ada E, Saracoğlu H, Gezer NS, Aras I. Comparison of treatments with the Forsus fatigue resistant device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2011;140:616–625. doi: 10.1016/j.ajodo.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 25.Ruf S, Pancherz H. Temporomandibular joint growth adaptation in Herbst treatment: a prospective magnetic resonance imaging and cephalometric roentgenographic study. Eur J Orthod. 1998;20:375–388. doi: 10.1093/ejo/20.4.375. [DOI] [PubMed] [Google Scholar]
- 26.Grünheid T, Langenbach GE, Korfage JA, Zentner A, van Eijden TM. The adaptive response of jaw muscles to varying functional demands. Eur J Orthod. 2009;31:596–612. doi: 10.1093/ejo/cjp093. [DOI] [PubMed] [Google Scholar]
- 27.Du X, Hägg U. Muscular adaptation to gradual advancement of the mandible. Angle Orthod. 2003;73:525–531. doi: 10.1043/0003-3219(2003)073<0525:MATGAO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Aggarwal P, Kharbanda OP, Mathur R, Duggal R, Parkash H. Muscle response to the twin-block appliance: an electromyographic study of the masseter and anterior temporal muscles. Am J Orthod Dentofacial Orthop. 1999;116:405–414. doi: 10.1016/S0889-5406(99)70225-8. [DOI] [PubMed] [Google Scholar]
- 29.Sood S, Kharbanda OP, Duggal R, Sood M, Gulati S. Muscle response during treatment of Class II Division 1 malocclusion with Forsus Fatigue Resistant Device. J Clin Pediatr Dent. 2011;35:331–338. doi: 10.17796/jcpd.35.3.5v86511u4h1mw144. [DOI] [PubMed] [Google Scholar]