Abstract
In plant-based medical systems, bitter tasting plants play a key role in managing dyspepsia. Yet when it comes to defining their mechanism of activity, herbalists and pharmacologists are split between two theories: one involves cephalic elicited vagal responses while the other comprises purely local responses. Recent studies indicate that bitters elicit a range of cephalic responses which alter postprandial gastric phase haemodynamics. Caffeine and regular coffee (Coffea arabica semen, L.) increase heart rate whereas gentian (Gentiana lutea radix, L.) and wormwood (Artemisia absinthium herba L.) increase tonus in the vascular resistance vessels. Following meals increased cardiac activity acts to support postprandial hyperaemia and maintain systemic blood pressure. The increased vascular tonus acts in parallel with the increased cardiac activity and in normal adults this additional pressor effect results in a reduced cardiac workload. The vascular response is a sympathetic reflex, evident after 5 minutes and dose dependent. Thus gentian and wormwood elicit cephalic responses which facilitate rather than stimulate digestive activity when postprandial hyperaemia is inadequate. Encapsulated caffeine elicits cardiovascular responses indicating that gastrointestinal bitter receptors are functionally active in humans. However, neither encapsulated gentian nor wormwood elicited cardiovascular responses during the gastric phase. These findings provide the platform for a new evidence-based paradigm.
1. Introduction
Bitter tasting herbs, commonly referred to as bitters, are used in many cultures [1–4] to support upper digestive activity; yet there is no consensus regarding a mechanism by which the chemosensory stimulation of taste receptors could enhance digestion. Results from our research group indicate that a novel mechanism is involved. Namely, some bitter tastants elicit a cephalic response increasing peripheral vascular resistance (PVR) [5]. During digestion, postprandial hyperaemia (PPH) places demands of the cardiovascular system (CVS) which are met by increased cardiac activity so as to prevent postprandial hypotension [6–10]. The increased PVR supports this cardiac activity and facilitates adequate PPH.
2. Theories of Bitter Activity
In the literature there are four models, two common and two minor, proposed to explain the effect of bitters on digestion.
CEPHALIC VAGAL REFLEX: stimulation of the oropharyngeal bitter receptors acts reflexively to increase saliva and vagal stimulation to the digestive organs.
LOCAL REFLEX: stimulation of both oropharyngeal and gastrointestinal bitter receptors acts locally to increase digestive secretions.
ALCOHOL: alcohol, rather than the bitter taste, improves digestion.
HYPERAEMIA: the major influence of bitters on digestion is improved blood circulation in the abdominal organs.
2.1. Cephalic Vagal Reflex
This longstanding model was reiterated in a 19th century pharmacology text: “the appetite is sharpened because the gustatory nerves are stimulated; this reflexively leads to dilation of the gastric vessels and to an increase in the gastric and salivary secretions” [11]. The later work of Pavlov, on the autonomic nerve system, was considered to support this model [12].
A more recent description of this model is as follows: “bitter stimuli pass primarily by way of the glossopharyngeal nerve to a special group of cells in the cerebral cortex. The taste is interpreted there as bitter, and causes stimuli to be forwarded through the vagus nerve to both the salivary gland and the stomach…. This stimulation of the digestive processes enhances the appetite” [13]. This model is supported by German E Commission [14] and several European Medical Agency Assessment Reports:
gentian (Gentiana lutea L.): “the long known action of bitters, which increase the secretion of gastric juice and bile due to the stimulation of gustatory nerves in the mouth” [15];
wormwood (Artemisia absinthium L.): “it is long known that the bitter constituents stimulate the gustatory nerves in the mouth and increase the secretion of gastric juice and bile, thereby promoting appetite and digestion” [16].
However, not all German pharmacologists agree [17]. In fact, generally pharmacologists are split on this issue with many agreeing [2, 18–25] and many disagreeing [17, 26–29]. The latter maintain that this model is unproven [29]. This difference of opinion results from the simple fact that the bitters have not been scientifically investigated [26]. A significant reason for this absence of research is the lack of investigative tools [30] to assess the levels of digestive secretions and more particularly the content of the secretions. Additionally, even if cephalic stimulation by bitters increased the production of digestive enzymes, it is the actual presence of food that stimulates enzyme secretion [31]. Thus studies would need to include both bitters and foods, a significant procedural complication.
Some pharmacologists claim that “bitter principles act reflexively on the cardiovascular system causing a decrease of heart rate and cardiac stroke volume” as evidence to support the model of bitters increasing vagal activity [32]. However these claims, based on an earlier study [33], have been shown to be fallacious, as the effect on heart rate and stroke volume for bitters added to water is no different than the effect of plain water on these parameters [34]. In contrast to the notion that digestion would benefit from enhanced parasympathetic activity [32], digestion is widely considered to be a sympathetic activity [35].
It has also been argued that bitters only affect those with impaired digestion [25, 32] yet no mechanism is suggested by which this selection process could occur. Also the question remains: if bitters increase digestive secretions, why do consumers of bitter aperitifs do not suffer side effects resulting from excess secretion of stomach acid, pancreatic juices, and gall?
2.2. Local Stimulation
This simple model asserts that the stimulation of bitter receptors acts locally to increase digestive secretions. This is certainly true for the oropharyngeal cavity as it is well known that bitter and sour tastants increase saliva production. Regarding the gastrointestinal tract, the discovery of bitter receptors in the gastrointestinal tract tissue [36] suggests that bitters may elicit chemosensory responses throughout the entire digestive system.
The presence of functionally active gastrointestinal bitter receptors in humans has been established when it was demonstrated that encapsulated caffeine increased both arterial compliance and diastolic pressure [37]. Yet it remains to be demonstrated that sufficient receptor stimulation occurs in physiological situations, such as eating, when contact between the agonist and the receptor may be hindered by the presence of food. Additionally there is the problem of partial agonists and antagonists [38] whether using natural or isolated substances.
2.3. Alcohol
The American pharmacologist Tyler suggested that for aperitifs it was the alcohol rather than the tastants which were responsible for any improvements in digestion [13]. While various alcoholic beverages do delay gastric emptying [39–41], including aperitifs [42, 43], the amount of alcohol found in a single dose of bitters made from either fluid extracts or tinctures is minimal (0.5–1.5 mL) and unlikely to affect gastric emptying.
2.4. Hyperaemia
Both Hale White (1892) and Weiss (1988) have proposed that the bitters enhance blood circulation in the gut and thereby improve digestion. Hale White wrote that following the ingestion of bitters: “the appetite is sharpened because the gustatory nerves are stimulated; this reflexively leads to dilation of the gastric vessels” [11]. Similarly Weiss wrote “the appetite-inducing action of bitters is probably due to improved circulation in the abdominal organs” [18]. Furthermore, Weiss suggested that bitters increase sympathetic excitability over time and it was this repeated activation that produced a general tonic action.
This model is of interest because following studies in the 1980s and 1990s it was realised that the increased splanchnic circulation after eating, referred to as postprandial hyperaemia (PPH), is the limiting factor of the digestive process [6, 7, 9, 10]. PPH fuels the metabolic activity during digestion supplying nutrients for the following:
the production of digestive secretions;
the movement of chyme;
the absorption of nutrients;
the movement of nutrients away from the intestinal wall;
the removal of metabolic wastes.
PPH extends the systemic circulation, potentially reducing blood pressure (BP) and peripheral vascular resistance (PVR). To avoid hypotension cardiac activity increases, both heart rate [9] (HR) and cardiac contraction force (dP/dt) [5] increase, raising cardiac output (CO) and preventing a drop of BP and PVR [9]. An inadequate postprandial cardiac response leads to both digestive problems and postprandial hypotension [44]. Postprandial hypotension is a major problem amongst the elderly [45] and a predictor of all-cause mortality in the low-care elderly [46].
3. Experimental Findings
In studies using the bitters roasted coffee (Coffea arabica semen, L.) drinks, both regular (circa 130 mg caffeine) and decaffeinated, 133 mg encapsulated caffeine (BP) [37, 47], gentian (Gentiana lutea radix, L.) and wormwood (Artemisia absinthium herba, L.) [5], the impact of bitters was assessed on gastric phase haemodynamics.
There are three phases of digestion [31, 48] (Figure 1).
Cephalic phase where chewing, tasting, and swallowing stimulate neural processes to increase blood flow in the celiac artery.
Gastric phase where the presence of either food or fluids produces stomach extension. Stomach extension triggers mechanical receptors which elicits increases of the celiac blood flow. This period begins when food enters the stomach and extends to when gastric emptying starts, usually 15–30 minutes after ingestion has ceased. It is during this period when postprandial hypotension most commonly occurs [8].
Intestinal phase begins with gastric emptying and continues until the meal is fully digested. During this phase the blood flow in the superior mesenteric artery increases in a manner governed by the food composition. Maximum flow increase is greatest for carbohydrates and least for proteins with fats in the middle [49] although the total response may not vary between types of meals [50]. Neither water (room temperature or cold) nor sham feeding affects the mesenteric flow [49].
Figure 1.
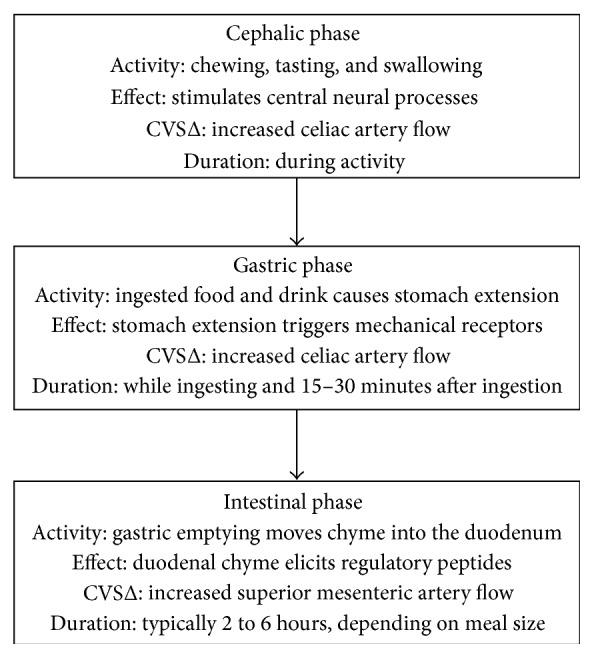
The three phases of digestion. CVSΔ: cardiovascular system change.
3.1. Coffee and Caffeine
Compared to control, encapsulated caffeine increased arterial compliance and diastolic BP in the 10–15 postingestion period, that is, just after the capsules opened [37]. As noted above, this finding indicates the presence of functionally active gastrointestinal bitter receptors in humans. In the later period 25–30 minutes, CVS changes were absent. The difference between the impacted CVS parameters in the two periods is likely due to the fact that caffeine, being rapidly and completely absorbed from the gut [51], is likely absent from the gut during the 25–30 minutes period. Notably there is no residual effect on the vasculature.
Compared to the room temperature control, hot preparations of regular coffee and decaffeinated espressos (67 mL) increased HR immediately after ingestion [37]. This is expected as hot water is known to increase HR [52]. Additionally, for the regular coffee, HR increases continued to the 30-minute mark (Figure 2). A follow-up study [47] reported that decaffeinated coffee with addition of caffeine produces similar results to caffeine.
Figure 2.
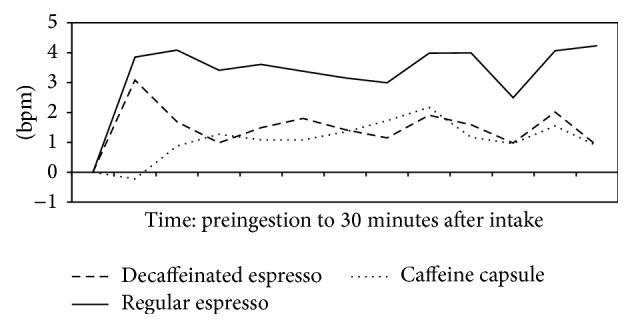
Postingestion changes in heart rate minus placebo postingestion changes. bpm: beats per minute.
The increase in HR, without changes in dP/dt, PVR, or baroreceptor sensitivity, suggests that the caffeine is eliciting vagal withdrawal, that is, reducing the vagal brake on the autonomic nerve system, for at least 30 minutes after the ingestion of regular coffee.
These findings indicate that the bitter compound caffeine is likely the active substance in regular coffee eliciting HR increases. In contrast the quinides, responsible for coffee's bitter taste, elicited no CVS responses. This variation indicates that dissimilar bitters may elicit different responses and so the hedonistic quality of bitterness is not an indicator of particular cephalic chemosensory responses.
The contrasting findings, that the chemosensory stimulation of oropharyngeal receptors by caffeine elicits increased HR while the chemosensory stimulation of gastrointestinal receptors by caffeine elicits increased AC, can be explained by the varying neural connections of the oropharyngeal and the gastrointestinal receptors. The oropharyngeal receptors have neural connections terminating in the rostral area of the nucleus tractus solitarius, whereas the gastrointestinal receptors have neural connections terminating in the caudal area of the nucleus tractus solitarius. Alternatively as caffeine is an agonist for 5 bitter receptors (hTAS2R: 7, 10, 14, 43, and 46) [53] it may be stimulating different receptors or constellations of receptors in the different tissues. Either way, the differing CVS responses indicate it cannot be assumed that a response elicited by a bitter agonist in one tissue can predict the response to the same agonist in another tissue.
3.2. Gentian and Wormwood
Gentian and wormwood are some of the most commonly used bitters in Europe [18, 29] and monographs of both drugs have recently been prepared by the European Medical Agency [15, 16, 54, 55]. The impact of these drugs on gastric phase haemodynamics was investigated in two parts.
In the first part, 100 mL room temperature water and capsules containing 1000 mg plant material were compared with placebo control during the 10–15-minute postingestion period, that is, just after the capsules opened. In contrast to the caffeine capsules, neither gentian nor wormwood altered CVS parameters.
In the second part, 1 mL of fluid extracts (40% alcohol) prepared from 500 mg and 1500 mg of both drugs was administered in 100 mL room temperature water. Compared to the control, both drugs elicited CVS changes in the 5–10-minute postingestion period. However, to fully appreciate the impact of the drugs it is necessary to recognise the impact of the control. The control elicited increases in dP/dt resulting in increased SV, systolic BP, and diastolic BP (see Table 1). The reduced HR is likely also the result of the increased dP/dt. The increased BP will decrease HR via the baroreflex activity [56]. With gentian and wormwood fluid preparations, the larger doses of both drugs and to lesser degree the smaller dose of gentian increased PVR or vascular tonus. This led to a reduction of cardiac activity (decreased SV and CO) without altering BP, presumably via baroreflex activity. Hence by increasing the vascular tone the bitters are complimenting the cardiac activity, which is compensating for the PPH. The net effect of the increased vascular tone is a reduction in cardiac workload. As these changes were observed for the fluids but not the capsules, it can be concluded that the gentian and wormwood are increasing PVR by eliciting cephalic chemosensory reflex responses.
Table 1.
Cardiovascular changes in the gastric phase of digestion.
| Condition | HR | dP/dt | SV | CO | PVR | AC | S.BP | D.BP |
|---|---|---|---|---|---|---|---|---|
| Control | ↓∧ | ↑∧∧ | ↑# | 0 | 0 | 0 | ↑∧∧ | ↑∧∧ |
| G500 | 0 | 0 | ↓∗ | ↓∗ | ↑† | 0 | 0 | 0 |
| G1500 | 0 | 0 | ↓∗ | ↓∗∗ | ↑∗∗ | 0 | 0 | 0 |
| W500 | 0 | 0 | ↓∗∗ | ↓∗∗ | ↑∗∗ | 0 | 0 | 0 |
| W1500 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
HR: heart rate, dP/dt: contraction force, SV: stroke volume, CO: cardiac output, PVR: peripheral vascular resistance, AC: arterial compliance, S.BP: systolic blood pressure, D.DP: diastolic blood pressure, G500: gentian 500 mg, G1500: gentian 1500 mg, W500: wormwood 500 mg, W1500: wormwood 1500 mg. ↑: increase, and ↓: decrease; #0.05 ≤ p < 0.010, ∧ p < 0.05, ∧∧ p < 0.001 pre-post ingestion comparisons for the control condition; †0.05 ≤ p < 0.010, ∗ p < 0.05, ∗∗ p < 0.001 placebo-controlled pre-post ingestion comparisons.
4. Methodological Considerations
Whether designing or assessing studies on the impact of tastants on CVS, there are physiological, perceptual, statistical, and parameter recording issues which need to be considered. Firstly the impact of swallowing dominates the initial minutes of postingestion period. Secondly, a high intensity tastant may produce a startle [57] or alerting [58] reaction which may last up to 5 minutes (Figure 3). Instances in the literature where startle reactions may have occurred include the effects of quinine sulphate on the CVS [59] and gastric emptying [60, 61]. Thirdly, the necessity of a control condition to assess interventions in nonpathological populations is critical [62], and in particular comparisons to baseline are inappropriate [63]. Due to the inherent difficulty in blinding the presentation of tastants, between-participant designs are often preferable to within-participant designs. Fourthly, combining measures from both the gastric- and intestinal phases produces uninterpretable results because the two phases are physiologically distinct. Lastly applying repeated measures ANOVA to a series of nonindependent measures is incorrect. Repeated measures ANOVA is only valid when applied to measures obtained from independent readings, such as the same test group tested with multiple treatments on separate occasions. Thus it is inappropriate to use this analysis technique for serial measurements such as readings at 30, 60, and 90 minutes from the same test session, unless independence can be demonstrated. For serial measurements the statistically legitimate procedure is to produce summary measures from the readings prior to analysis [64, 65]. This is a surprising common mistake and a review of 125 publications reported that post hoc t-tests and repeated measure ANOVAs were incorrectly applied in 56% and 52% of cases, respectively [66]. CVS studies failing to report dP/dt measures can be considered incomplete while short-term changes of heart rate variability scores are misleading unless dP/dt can be shown to be fixed [67].
Figure 3.
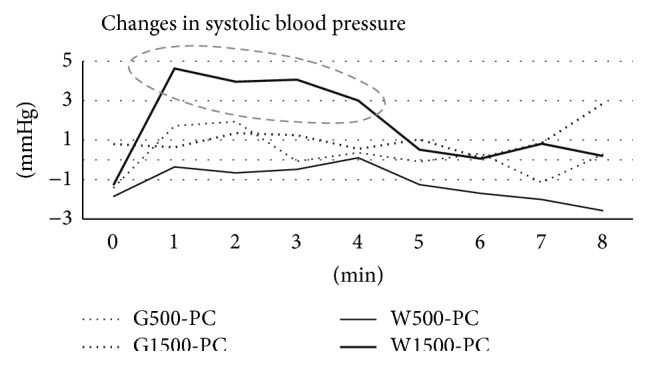
Postingestion placebo-controlled changes from baseline for systolic blood pressure following the intake of four bitter preparations. The sharp increase in blood pressure (broken ellipse) for W1500 during the first minute and extending to 5 minutes is likely the result of a startle or alerting response to the tastant. G500: extract produced from 500 mg gentian, G1500: extract produced from 1500 mg gentian, W500: extract produced from 500 mg wormwood, W1500: extract produced from 1500 mg wormwood, PC: placebo control.
5. Discussion
The studies outlined above provide a platform on which we can build a new evidence-based model, on the impact of bitters on humans, grounded on a physiological mechanism.
Some bitter tastants elicit cephalic reflex autonomic and CVS responses whereas others appear not to, such as the quinides in coffee. Consequently there is no universal bitter effect [25], as different bitters elicit a range of cephalic responses, or even none at all.
Some bitter tastants elicit cephalic responses increasing HR, the mechanism of which is likely due to vagal withdrawal for example, caffeine. This is consistent with caffeine's reputation as a human activator, although the chemosensory pathway is novel. It is even possible that at the dose of circa 130 mg this response occurs without hedonistic recognition [68]. Despite altering postprandial haemodynamics, it remains to be determined whether the increased HR affects PPH. Currently the mechanism by which regular coffee [69], but decaffeinated coffee [70], increases gastric emptying is unknown but may involve cephalic responses.
Some bitter tastants elicit cephalic responses increasing PVR, namely, gentian and wormwood. This change in postprandial haemodynamics is likely to impact inadequate PPH by increasing BP in situations where the cardiac output is insufficient. Thus this type of bitter assists digestion, rather than stimulating digestion as suggested by many authors [17, 32]. In fact, these bitters can be described as eupeptics (from Greek eu: well and pepis: digestion) promoting gastric juice secretion and facilitating digestion [27]. By implication, this finding suggests that bitters which elicit increased PVR may be of use in cardiac disorders, particularly those involving digestion such as postprandial angina [44, 46]. This finding also helps us to understand why these bitters help those with poor digestion but do not affect those with normal digestion [25, 29, 32].
A minimum dose of bitters is essential to elicit cephalic responses, for example, wormwood, and the magnitude of a response is dose dependent for example, gentian. Additionally, the hedonist perception of bitterness is not an indicator of a cephalic response. This finding contradicts the view that bitters only need to be tasted to be therapeutically active [25]. Furthermore the finding suggests that drop doses, such as 5–10 drops of 1 : 5 tinctures, recommended by some authors [25], are likely to be ineffective. Rather these findings provide evidence for the single doses, prepared from 1000 mg gentian or 1000 mg wormwood, recommended by the German E Commission [14] and the European Medical Agency monographs [54, 55].
The onset of increased HR and PVR is circa 5 minutes. This contrasts with the view that cephalic responses are slow [25] and therefore bitters should be taken 15–30 minutes prior to eating [2, 25]. Thus there appears to be little reason not to take bitters directly before, during, or even after a meal. It has been proposed that the cephalic response is limited to 30 minutes [27]; this remains to be established and ideally would require a study incorporating a meal. In the above studies with gentian and wormwood, several participants spontaneously reported that the bitter taste remained for in excess of 30 minutes. Other authors note that a bitter aftertaste may be present hours and even days after exposure [71]. Two publications report bitter combinations improving gastroparesis (inadequate gastric emptying) in pathological groups [72, 73]. Despite the limitations of these studies, the results suggest that the effect of these combinations is continuing well into the intestinal phase of digestion. Whether these combinations are increasing PPH or working directly on the gastric emptying process is unclear, but it is plausible that improving reduced PPH would encourage normal gastric emptying.
The fast onset suggests that in acute, and even some chronic, conditions dosage could be repeated at 30-minute intervals or even more often when required. Although the European Medical Agency monograph limits the use of wormwood [55], due to the thujone content, the accompanying Assessment Report notes an absence of thujone in percolated fluid extracts (30% alcohol) [16]. This report has also been criticised as basing recommendations on outdated animal studies and producing overly conservative conclusion regarding thujone [74]. Modern toxicity research indicates that it would take between 2 and 20 cups of wormwood tea to reach the maximum acceptable daily intake level [74] assuming that wormwood tea extracts 100% of the thujone in the dried herb [16]. There are no similar limitations for gentian [54].
The finding that encapsulated caffeine elicited gastric CVS responses indicates that tastants in the gastrointestinal tract are capable of rapidly eliciting systemic responses. The mechanism for caffeine responses is likely via vagal connections with neural relays in the CVS section of the nucleus tractus solitarius. This possible mechanism is supported by recent work indicating that more neural relays exist in taste transduction than previously realised [75]. The fact that secondary plant metabolites in the gastrointestinal are capable of eliciting autonomic and CVS responses indicates how exposed our homeostatic and circulatory systems are to dietary compounds as well as other substances formed in the gut either during digestion of foods or by the microbiota.
6. Conclusions
It is now possible to categorise bitters into functional subgroups rather than chemical subgroups based on mechanism of action. The eupeptics, gentian, and wormwood elicit cephalic responses via the sympathetic system, increasing peripheral vascular resistance. There is no evidence that either of these eupeptics enhance vagal transmissions, even if heart rate decreases. The increased cardiac activity in response to postprandial hyperaemia is complimented by the enhanced vascular tonus. This reduces the load on the heart and so the eupeptics may have therapeutic uses outside of their digestive usage, particularly regarding postprandial cardiac insufficiency. Although encapsulated gentian and wormwood did not elicit responses during the gastric phase of digestion, they may elicit responses during the intestines-phase of digestion. Gentian and wormwood may be used, both to prevent dyspepsia and to relieve dyspepsia, in fluid doses containing circa 1000 mg of the dried drug. In chronic conditions, during which the digestive organs have experienced a period of insufficient blood flow or ischaemia, both local and systemic tonic effects can be expected to result from the improved splanchnic blood flow. These eupeptics have a fast onset and dosage can be repeated as required. The low toxicity favours a user-regulated regime of administration.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Williamson E. M. Major Herbs of Ayurveda. Edinburgh, UK: Churchill Livingstone; 2002. [Google Scholar]
- 2.Kemper F. H. ESCOP Monographs. The Scientific Foundation for the Herbal Medicinal Products. 2nd. Stuttgart, Germany: Thieme; 2003. [Google Scholar]
- 3.Ministry-of-Health-Labour-and-Wefare. Japanese Pharmacopoeia. Toyko, Japan: Ministry-of-Health-Labour-and-Wefare; 2006. [Google Scholar]
- 4.Olivier D. K., van Wyk B.-E. Bitterness values for traditional tonic plants of southern Africa. Journal of Ethnopharmacology. 2013;147(3):676–679. doi: 10.1016/j.jep.2013.03.059. [DOI] [PubMed] [Google Scholar]
- 5.McMullen M. K., Whitehouse J. M., Whitton P. A., Towell A. Bitter tastants alter gastric-phase postprandial haemodynamics. Journal of Ethnopharmacology. 2014;154(3):719–727. doi: 10.1016/j.jep.2014.04.041. [DOI] [PubMed] [Google Scholar]
- 6.Avasthi P. S., Greene E. R., Voyles W. F. Noninvasive doppler assessment of human postprandial renal blood flow and cardiac output. The American Journal of Physiology—Renal Fluid and Electrolyte Physiology. 1987;252(6):F1167–F1174. doi: 10.1152/ajprenal.1987.252.6.F1167. [DOI] [PubMed] [Google Scholar]
- 7.Sidery M. B., MacDonald I. A., Cowley A. J., Fullwood L. J. Cardiovascular responses to high-fat and high-carbohydrate meals in young subjects. American Journal of Physiology—Heart and Circulatory Physiology. 1991;261(5):H1430–H1436. doi: 10.1152/ajpheart.1991.261.5.H1430. [DOI] [PubMed] [Google Scholar]
- 8.Lipsitz L. A., Ryan S. M., Parker J. A., Freeman R., Wei J. Y., Goldberger A. L. Hemodynamic and autonomic nervous system responses to mixed meal ingestion in healthy young and old subjects and dysautonomic patients with postprandial hypotension. Circulation. 1993;87(2):391–400. doi: 10.1161/01.cir.87.2.391. [DOI] [PubMed] [Google Scholar]
- 9.Sidery M. B., MacDonald I. A. The effect of meal size on the cardiovascular responses to food ingestion. British Journal of Nutrition. 1994;71(6):835–848. doi: 10.1079/bjn19940190. [DOI] [PubMed] [Google Scholar]
- 10.Kearney M. T., Cowley A. J., MacDonald I. A. The cardiovascular responses to feeding in man. Experimental Physiology. 1995;80(5):683–700. doi: 10.1113/expphysiol.1995.sp003878. [DOI] [PubMed] [Google Scholar]
- 11.Hale White W. Materia Medica, Pharmacy, Pharmacology and Therapeutics. 1st. London, UK: J. & A. Churchill; 1892. [Google Scholar]
- 12.Hale-White W. Materia Medica: Pharmacy, Pharmacology and Therapeutics. 17th. London, UK: J. & A. Churchill; 1920. [Google Scholar]
- 13.Robbers J., Tyler V. E. Tyler's Herbs of Choice. Binghamton, NY, USA: The Hawthorn Press; 1999. [Google Scholar]
- 14.Blumenthal M. The Complete German E Monographs. Austin, Tex, USA: American Botanical Council; 1998. [Google Scholar]
- 15.Knöss W., Stolte F. Assessment Report on Gentiana lutea L., Radix. London, UK: European Medicines Agency; 2009. [Google Scholar]
- 16.Koch J. Assessment Report on Artemisia absinthium L., Herba. London, UK: European Medicines Agency; 2009. [Google Scholar]
- 17.Kraft K., Hobbs C. Pocket Guide to Herbal Medicine. Stuttgart, Germany: Georg Thieme; 2004. [DOI] [Google Scholar]
- 18.Weiss R. F. Herbal Medicine. 6th. Gothenburg, Sweden: AB Arcanum; 1988. [Google Scholar]
- 19.Bradley P. R. British Herbal Compendium. Bournemouth, UK: British Herbal Medicine Association; 1992. [Google Scholar]
- 20.Bruneton J. Pharmacognosy. Phytochemistry of Medicinal Plants. Paris, France: Lavoisier; 1999. [Google Scholar]
- 21.Sandberg F., Corrigan D. Natural Remedies: Their Origins and Uses. London, UK: Taylor and Thomas; 2001. [Google Scholar]
- 22.Brendler T., Joerg G., Jaenicke C. Herbal Remedies. 4th. Berlin, Germany: Medpharm Scientific Publishers; 2003. [Google Scholar]
- 23.van Wyk B.-E., Wink M. Medicial Plants of the World. Portland, Ore, USA: Timber Press; 2004. [Google Scholar]
- 24.Wichtl M. Herbal Drugs and Phytopharmaceuticals. 3rd. Stuttgart, Germany: Medpharm; 2004. [Google Scholar]
- 25.Mills S., Bone K. Principles and Practice of Phytotherapy: Modern Herbal Medicine. 2nd. Edinburgh, UK: Churchill Livingstone; 2013. [Google Scholar]
- 26.Laurence D. R., Bennett P. N., Brown M. J. Clinical Pharmacology. 8th. New York, NY, USA: Churchill Livingstone; 1997. [Google Scholar]
- 27.Capasso F., Gaginella T. S., Grandolin G., Izzo A. A. Phytotherapy. A Quick Reference to Herbal Medicine. Berlin, Germany: Springer; 2003. [Google Scholar]
- 28.Barnes J., Anderson L. A., Phillipson J. D. Herbal Medicines. 3rd. London, UK: Pharmaceutical Press; 2007. [Google Scholar]
- 29.Heinrich M., Barnes J., Gibbons S., Williamson E. M. Fundamentals of Pharmacognosy and Phytotherapy. 2nd. Edinburgh, UK: Churchill Livingstone; 2012. [Google Scholar]
- 30.Furness J. B. The Enteric Nervous System. Malden, Mass, USA: Blackwell Publishing; 2006. [Google Scholar]
- 31.Hall J. E. Guyton and Hall: Textbook of Medical Physiolgy. 12th. Philadelphia, Pa, USA: Elsevier Sanders; 2011. [Google Scholar]
- 32.Schulz V., Hänsel R., Tyler V. E. Rational Phytotherapy. A Reference Guide for Physicians and Pharmacists. 5th. Berlin, Germany: Springer; 2004. [Google Scholar]
- 33.Glatzel H. Influence of bitter tonics on heart stroke volume, heart beat frequenccy and blood pressure. Planta Medica. 1968;16(1):82–94. doi: 10.1055/s-0028-1099884. [DOI] [PubMed] [Google Scholar]
- 34.McMullen M. K. Evidence does not support the suggestion that gustatory exposure to bitter tastants reduces cardiac activity. Journal of Ethnopharmacology. 2013;149(3):838–839. doi: 10.1016/j.jep.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 35.van Baak M. A. Meal-induced activation of the sympathetic nervous system and its cardiovascular and thermogenic effects in man. Physiology and Behavior. 2008;94(2):178–186. doi: 10.1016/j.physbeh.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 36.Wu S. V., Rozengurt N., Yang M., Young S. H., Sinnett-Smith J., Rozengurt E. Expression of bitter taste receptors of the T2R family in the gastrointestinal tract and enteroendocrine STC-1 cells. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(4):2392–2397. doi: 10.1073/pnas.042617699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMullen M. K., Whitehouse J. M., Shine G., Whitton P. A., Towell A. The immediate and short-term chemosensory impacts of coffee and caffeine on cardiovascular activity. Food and Function. 2011;2(9):547–554. doi: 10.1039/c1fo10102a. [DOI] [PubMed] [Google Scholar]
- 38.Brockhoff A., Behrens M., Roudnitzky N., Appendino G., Avonto C., Meyerhof W. Receptor agonism and antagonism of dietary bitter compounds. Journal of Neuroscience. 2011;31(41):14775–14872. doi: 10.1523/jneurosci.2923-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Franke A., Teyssen S., Harder H., Singer M. V. Effect of ethanol and some alcoholic beverages on gastric emptying in humans. Scandinavian Journal of Gastroenterology. 2004;39(7):638–644. doi: 10.1080/00365520410005009. [DOI] [PubMed] [Google Scholar]
- 40.Franke A., Nakchbandi I. A., Schneider A., Harder H., Singer M. V. The effect of ethanol and alcoholic beverages on gastric emptying of solid meals in humans. Alcohol and Alcoholism. 2005;40(3):187–193. doi: 10.1093/alcalc/agh138. [DOI] [PubMed] [Google Scholar]
- 41.Kasicka-Jonderko A., Jonderko K., Bożek M., Kamińska M., Mgłosiek P. Potent inhibitory effect of alcoholic beverages upon gastrointestinal passage of food and gallbladder emptying. Journal of Gastroenterology. 2013;48(12):1311–1323. doi: 10.1007/s00535-013-0752-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Inamori M., Iida H., Endo H., et al. Aperitif effects on gastric emptying: a crossover study using continuous real-time 13C breath test (BreathID System) Digestive Diseases and Sciences. 2009;54(4):816–818. doi: 10.1007/s10620-008-0427-3. [DOI] [PubMed] [Google Scholar]
- 43.Heinrich H., Goetze O., Menne D., et al. Effect on gastric function and symptoms of drinking wine, black tea, or schnapps with a Swiss cheese fondue: randomised controlled crossover trial. British Medical Journal. 2010;341(7786) doi: 10.1136/bmj.c6731.c6731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Luciano G. L., Brennan M. J., Rothberg M. B. Postprandial hypotension. The American Journal of Medicine. 2010;123(3):281.e1–281.e6. doi: 10.1016/j.amjmed.2009.06.026. [DOI] [PubMed] [Google Scholar]
- 45.Vloet L. C. M., Pel-Little R. E., Jansen P. A. F., Jansen R. W. M. M. High prevalence of postprandial and orthostatic hypotension among geriatric patients admitted to Dutch hospitals. The Journals of Gerontology, Series A, Biological Sciences and Medical Sciences. 2005;60(10):1271–1277. doi: 10.1093/gerona/60.10.1271. [DOI] [PubMed] [Google Scholar]
- 46.Fisher A. A., Davis M. W., Srikusalanukul W., Budge M. M. Postprandial hypotension predicts all-cause mortality in older, low-level care residents. Journal of the American Geriatrics Society. 2005;53(8):1313–1320. doi: 10.1111/j.1532-5415.2005.53415.x. [DOI] [PubMed] [Google Scholar]
- 47.McMullen M. K., Whitehouse J. M., Shine G., Whitton P. A., Towell A. Caffeine in hot drinks elicits cephalic phase responses involving cardiac activity. Food & Function. 2012;3(9):931–940. doi: 10.1039/c2fo00002d. [DOI] [PubMed] [Google Scholar]
- 48.Trahair L. G., Horowitz M., Jones K. L. Postprandial hypotension: a systematic review. Journal of the American Medical Directors Association. 2014;15(6):394–409. doi: 10.1016/j.jamda.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 49.Qamar M. I., Read A. E. Effects of ingestion of carbohydrate, fat, protein, and water on the mesenteric blood flow in man. Scandinavian Journal of Gastroenterology. 1988;23(1):26–30. doi: 10.3109/00365528809093842. [DOI] [PubMed] [Google Scholar]
- 50.Sauder K. A., Johnston E. R., Skulas-Ray A. C., Campbell T. S., West S. G. Effect of meal content on heart rate variability and cardiovascular reactivity to mental stress. Psychophysiology. 2012;49(4):470–477. doi: 10.1111/j.1469-8986.2011.01335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blanchard J., Sawers S. J. A. The absolute bioavailability of caffeine in man. European Journal of Clinical Pharmacology. 1983;24(1):93–98. doi: 10.1007/bf00613933. [DOI] [PubMed] [Google Scholar]
- 52.Quinlan P. T., Lane J., Aspinall L. Effects of hot tea, coffee and water ingestion on physiological responses and mood: the role of caffeine, water and beverage type. Psychopharmacology. 1997;134(2):164–173. doi: 10.1007/s002130050438. [DOI] [PubMed] [Google Scholar]
- 53.Meyerhof W., Batram C., Kuhn C., et al. The molecular receptive ranges of human TAS2R bitter taste receptors. Chemical Senses. 2009;35(2):157–170. doi: 10.1093/chemse/bjp092. [DOI] [PubMed] [Google Scholar]
- 54.Knöss W., Stolte F. Community Herbal Monograph on Gentian lutea L., Radix. London, UK: European Medicines Agency; 2009. [Google Scholar]
- 55.Koch J. Community Herbal Monograph on Artemisia absinthium L., herba. London, UK: European Medicines Agency; 2009. [Google Scholar]
- 56.Levick J. R. An Introduction to Cardiovascular Physiology. 5th. London, UK: Arnold; 2010. [Google Scholar]
- 57.Bradley M. M., Lang P. J. Emotion and motivation. In: Cacioppo J. T., Tassinary L. G., Berntson G. G., editors. Handbook of Psychophysiology. New York, NY, USA: Cambridge University Press; 2007. pp. 581–607. [Google Scholar]
- 58.Marshall J. M. Cardiovascular changes associated with behavioural alerting. In: Jordan D., Marshall J., editors. Cardiovascular Regulation. London, UK: Portland Press; 1995. pp. 37–59. [Google Scholar]
- 59.Rousmans S., Robin O., Dittmar A., Vernet-Maury E. Autonomic nervous system responses associated with primary tastes. Chemical Senses. 2000;25(6):709–718. doi: 10.1093/chemse/25.6.709. [DOI] [PubMed] [Google Scholar]
- 60.Wicks D., Wright J., Rayment P., Spiller R. Impact of bitter taste on gastric motility. European Journal of Gastroenterology and Hepatology. 2005;17(9):961–965. doi: 10.1097/00042737-200509000-00012. [DOI] [PubMed] [Google Scholar]
- 61.McLaren L., Jones G. C. Quinine sulphate. Practical Diabetes International. 2010;27(9):413–414. doi: 10.1002/pdi.1536. [DOI] [Google Scholar]
- 62.Bland M. An Introduction to Medical Statistics. 3rd. Oxford, UK: Oxford University Press; 2000. [Google Scholar]
- 63.Bland J. M., Altman D. G. Comparisons against baseline within randomised groups are often used and can be highly misleading. Trials. 2011;12, article 264 doi: 10.1186/1745-6215-12-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matthews J. N. S., Altman D. G., Campbell M. J., Royston P. Analysis of serial measurements in medical research. British Medical Journal. 1990;300(6719):230–235. doi: 10.1136/bmj.300.6719.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Matthews J. N. S. Summary measures analysis of longitudinal data. In: Armitage P., Colton T., editors. Encyclopedia of Biostatistics. London, UK: Wiley-Blackwell; 2005. p. p. 6100. [Google Scholar]
- 66.Burke D. A., Whittemore S. R., Magnuson D. S. K. Consequences of common data analysis inaccuracies in CNS trauma injury basic research. Journal of Neurotrauma. 2013;30(10):797–805. doi: 10.1089/neu.2012.2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McMullen M. K. Oops! who forgot to measure cardiac contraction force (dP/dt)? Austin Journal of Pharmacology and Therapeutics. 2014;2(11):1–4. [Google Scholar]
- 68.Keast R. S. J., Riddell L. J. Caffeine as a flavor additive in soft-drinks. Appetite. 2007;49(1):255–259. doi: 10.1016/j.appet.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 69.Akimoto K., Inamori M., Iida H., et al. Does postprandial coffee intake enhance gastric emptying?: a crossover study using continuous real time 13C breath test (BreathID system) Hepato-Gastroenterology. 2009;56(91-92):918–920. [PubMed] [Google Scholar]
- 70.Schubert M. M., Grant G., Horner K., et al. Coffee for morning hunger pangs. An examination of coffee and caffeine on appetite, gastric emptying, and energy intake. Appetite. 2014;83:317–326. doi: 10.1016/j.appet.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 71.Meilgaard M. C., Civille G. V., Carr B. T. Sensory Evaluation Techniques. Roco Raton, Fla, USA: CRC Press; 2007. [Google Scholar]
- 72.Tian J.-X., Li M., Liao J.-Q., Liu W.-K., Tong X.-L. Xiangshaliujunzi Decoction for the treatment of diabetic gastroparesis: a systematic review. World Journal of Gastroenterology. 2014;20(2):561–568. doi: 10.3748/wjg.v20.i2.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Doi H., Sakakibara R., Sato M., et al. Dietary herb extract rikkunshi-to ameliorates gastroparesis in Parkinson's disease: a pilot study. European Neurology. 2014;71(3-4):193–195. doi: 10.1159/000355608. [DOI] [PubMed] [Google Scholar]
- 74.Lachenmeier D. W., Uebelacker M. Risk assessment of thujone in foods and medicines containing sage and wormwood—evidence for a need of regulatory changes? Regulatory Toxicology and Pharmacology. 2010;58(3):437–443. doi: 10.1016/j.yrtph.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 75.Matsumoto I. Gustatory neural pathways revealed by genetic tracing from taste receptor cells. Bioscience, Biotechnology and Biochemistry. 2013;77(7):1359–1362. doi: 10.1271/bbb.130117. [DOI] [PMC free article] [PubMed] [Google Scholar]


