We have read the manuscript about codeine (3-methylmorphine) anaphylaxis by Hey-Soo Yoo et al.1 with great interest and would like to take the opportunity to raise some issues and communicate our experience. As recently reviewed, despite their frequent and ubiquitous use, genuine IgE-mediated allergy to opiates remains exceedingly rare. Also, correct diagnosis is not straightforward, mainly because of uncertainties associated with measurement of drug-specific IgE antibodies and skin testing.2 Actually, the key to correct diagnosis of opiate allergy lies in elucidating the clinical significance of positive specific IgE (sIgE) results and distinguishing skin test responsiveness resulting from direct histamine release from a true IgE-mediated activation of cutaneous mast cells. From investigations about morphine and pholcodine (3-[2-morpholinyl-ethyl] morphine)-reactive IgE antibodies it is clear that positive IgE results towards these compounds cannot be considered as a proof for opiate allergy. As a matter of fact, sIgE reactivity to opiates has been observed in up to 10% of the general population and over 80% of patients allergic to rocuronium.3,4,5 Mutatis mutandis, this observation applies to skin testing with these potent histamine releasers that, for years, have been used as a positive control in skin testing (for review2). In contrast, opiates seem not to trigger histamine release from human basophils,6,7,8 making these cells highly attractive as a complementary diagnostic instrument to discriminate non-immunologic hypersensitivity reactions from genuine allergy with an underlying IgE-mediated mechanism (for review2).
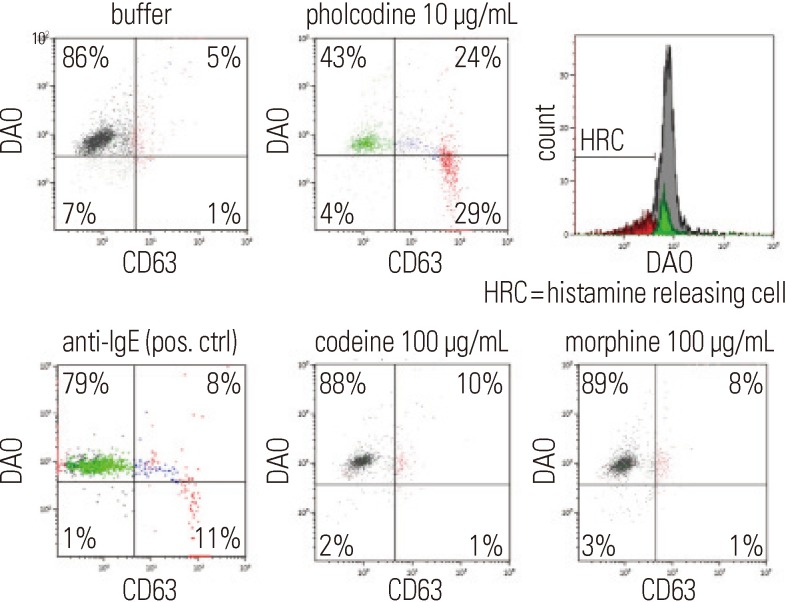
In their manuscript the authors describe a patient who suffered from anaphylaxis due to oral intake of codeine and document their diagnosis with a drug provocation and histamine release tests. However, due to the unavailability of codeine-sIgE tests, they were unable to establish a potential IgE-mediated mechanism. However, several points might be addressed here. First, measurement of pholcodine and morphine sIgE antibodies, that are readily available from Phadia Thermo Fisher Scientific, might have proven to be useful. As a matter of fact, these three opiates are structurally almost identical, except the substituent in position 3. At this position codeine has a methoxy group, morphine a hydroxyl group, and pholcodine a 2-morpholinoethyl group. Second, mutatis mutandis, the recommendation also applies to histamine release and drug provocation tests. Recently, we have described three patients with immediate hypersensitivity reactions to pholcodine in who measurement of drug-specific IgE and basophil activation tests (Figure) lead to the diagnosis of an IgE-mediated pholcodine allergy.9 Because these patients demonstrated a positive sIgE to morphine but negative basophil activation and provocation tests with the closely related structures morphine and pholcodine, the conclusion seems inescapable that the currently available quantification of opiate-sIgE tests should not be used to diagnose or predict clinical outcomes. Moreover, these observations seem to indicate the likelihood of antibody combining site heterogeneity with recognition at the fine structural level of features additional, and adjacent to, the position 3 substituent.
Figure. Representative plot CD63 appearance and histamine release in response to buffer, anti-IgE as a positive control, pholcodine 10 µg/mL (top), and the structurally almost similar opiates codeine 100 mg/mL and morphine 100 µg/mL (both bottom) (From9: with permission). Intracellular histamine and its release is analyzed flow cytometrically by an enzyme affinity method using the histaminase diamine oxidase (DAO) conjugated to laser-excitable fluorochromes.10.
ACKNOWLEDGMENTS
Didier Ebo is a Senior Clinical Researcher of the Research Foundation Flanders (FWO: 1800614N). Vito Sabato is a Clinical Researcher of the Research Foundation Flanders (FWO: 1700614N).
Footnotes
There are no financial or other issues that might lead to conflict of interest.
References
- 1.Yoo HS, Yang EM, Kim MA, Hwang SH, Shin YS, Ye YM, Nahm DH, Park HS. A case of codeine induced anaphylaxis via oral route. Allergy Asthma Immunol Res. 2014;6:95–97. doi: 10.4168/aair.2014.6.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baldo BA. Cross-reactive antigens for natural IgE antibodies: allergens with the potential to transform a dormant to an active allergic response? Clin Exp Allergy. 2012;42:810–813. doi: 10.1111/j.1365-2222.2012.03994.x. [DOI] [PubMed] [Google Scholar]
- 3.Fisher MM, Baldo BA. Immunoassays in the diagnosis of anaphylaxis to neuromuscular blocking drugs: the value of morphine for the detection of IgE antibodies in allergic subjects. Anaesth Intensive Care. 2000;28:167–170. doi: 10.1177/0310057X0002800207. [DOI] [PubMed] [Google Scholar]
- 4.Ebo DG, Venemalm L, Bridts CH, Degerbeck F, Hagberg H, De Clerck LS, Stevens WJ. Immunoglobulin E antibodies to rocuronium: a new diagnostic tool. Anesthesiology. 2007;107:253–259. doi: 10.1097/01.anes.0000270735.40872.f2. [DOI] [PubMed] [Google Scholar]
- 5.Laroche D, Chollet-Martin S, Léturgie P, Malzac L, Vergnaud MC, Neukirch C, Venemalm L, Guéant JL, Roland PN. Evaluation of a new routine diagnostic test for immunoglobulin e sensitization to neuromuscular blocking agents. Anesthesiology. 2011;114:91–97. doi: 10.1097/ALN.0b013e31820164d2. [DOI] [PubMed] [Google Scholar]
- 6.Swerts S, Van Gasse A, Leysen J, Faber M, Sabato V, Bridts CH, Jorens PG, De Clerck LS, Ebo DG. Allergy to illicit drugs and narcotics. Clin Exp Allergy. 2014;44:307–318. doi: 10.1111/cea.12177. [DOI] [PubMed] [Google Scholar]
- 7.Withington DE, Patrick JA, Reynolds F. Histamine release by morphine and diamorphine in man. Anaesthesia. 1993;48:26–29. doi: 10.1111/j.1365-2044.1993.tb06785.x. [DOI] [PubMed] [Google Scholar]
- 8.Ebertz JM, Hermens JM, McMillan JC, Uno H, Hirshman C, Hanifin JM. Functional differences between human cutaneous mast cells and basophils: a comparison of morphine-induced histamine release. Agents Actions. 1986;18:455–462. doi: 10.1007/BF01964946. [DOI] [PubMed] [Google Scholar]
- 9.Leysen J, De Witte L, Sabato V, Faber M, Hagendorens M, Bridts C, De Clerck L, Ebo D. IgE-mediated allergy to pholcodine and cross-reactivity to neuromuscular blocking agents: lessons from flow cytometry. Cytometry B Clin Cytom. 2013;84:65–70. doi: 10.1002/cyto.b.21074. [DOI] [PubMed] [Google Scholar]
- 10.Ebo DG, Bridts CH, Mertens CH, Hagendorens MM, Stevens WJ, De Clerck LS. Analyzing histamine release by flow cytometry (HistaFlow): a novel instrument to study the degranulation patterns of basophils. J Immunol Methods. 2012;375:30–38. doi: 10.1016/j.jim.2011.09.003. [DOI] [PubMed] [Google Scholar]