Abstract
BACKGROUND
Epstein Barr Virus (EBV) is a ubiquitous herpes virus that persists lifelong in normal humans by colonizing memory B cells. Infection during childhood is usually asymptomatic. Isolated gallbladder wall thickening or hydrops have been reported in patients with EBV infectious mononucleosis. However, acute acalculous cholecystitis is an atypical clinical presentation of primary EBV infection. We present a teenager with acute cholecystitis associated with EBV acute infection. Acute acalculous cholecystitis accounts for 2–15% of all cases of acute cholecystitis. Few cases of acute cholecystitis have been reported during the course of primary EBV infection.
PRESENTATION OF CASE
A 15-year-old female who came to the JDCH ER complaining of 3 days history of mild diffuse abdominal pain associated with two episodes of emesis. She also reports headache as well as a mild cough and low grade subjective fever. Blood test results showed mild leukocytosis with significant elevation in the lymphocytes (59%), High alkaline phosphatase (221 U/I), AST (191 U/I), ALT(221 U/I) and bilirubin (Total 1.8 and direct 1.5). Abdominal US showed a contracted gallbladder with wall thickness and pericholecystic fluid. During hospital stay number 2–3 laboratory work up show a trending up in the bilirubin levels. MRCP was ordered and no abdnormalities were found. At this point Hospital stay number 3 EBV acute infection was suspected. Serum serological studies were subsequently diagnostic for this viral disease. Management was conservative and the patient was discharged asymptomatic on hospital day number six.
Keywords: Epstein Barr Virus, Acute cholecystitis, Childhood, Mononucleosis, Acalculous cholecystitis
1. Background
Epstein Barr Virus (EBV) is a ubiquitous herpes virus that persists lifelong in normal humans by colonizing memory B cells. Infection during childhood is usually asymptomatic, whereas it presents as typical infectious mononucleosis in about 50% of adolescents and young adults.1,2 Isolated gallbladder wall thickening or hydrops have been reported in patients with EBV infectious mononucleosis. However, acute acalculous cholecystitis is an atypical clinical presentation of primary EBV infection.2,3 We present a teenager with acute cholecystitis associated with EBV acute infection successfully treated with medical management.
Acute acalculous cholecystitis accounts for 2–15% of all cases of acute cholecystitis. It is most commonly associated with trauma, recent surgery, shock, burns, sepsis, critical illness, total parental nutrition and prolonged fasting.1,4 Only 13 cases of acute cholecystitis have been reported during the course of primary EBV infection, of these cases, 12 were in female patients with ages ranging from 18 to 53 years old. Of those only one requires surgical intervention.1
2. Case report
A 15-year-old female without significant past medical history came to the JDCH emergency room complaining of 3 days history of mild diffuse abdominal pain mainly in the epigastric region, constant, cramping/sharp, 7/10 in intensity associated with two episodes of non-bilious, non-bloody emesis. She also reports headache as well as a mild cough and low grade subjective fever. Blood test results showed mild elevated white blood cells count (10.95 × 10) with significant elevation in the lymphocytes (59%), High serum concentration of alkaline phosphatase (221 U/I), aspartate aminotransferase (191 U/I), alanine aminotransferase(221 U/I) and bilirubin (Total 1.8 and direct 1.5). Abdominal ultrasound showed a contracted gallbladder with wall thickness (19 mm) with pericholecystic fluid. Normal common bile duct (Figs. 1 and 2). CT imaging revealed similar findings with marked pericholecystic fluid. No visceromegaly. Moderate free fluid in the pelvis (Fig. 3). During hospital stay number 2–3 laboratory work up show a trending up in the bilirubin levels up to (Total 2.3 μmol/L and Direct 1.8 μmol/L). MRCP was ordered to rule out biliary obstruction and no choledocholithiasis nor intra or extra hepatobiliary duct dilation was found. No gallstone seen. At this point Hospital stay number 3 Epstein–Barr Virus (EBV) acute infection was suspected. Serum serological studies were subsequently diagnostic for this viral disease (both heterophile antibody test and IgM against EBV capsid antigen). There was no evidence of other coexisting infectious disease. Management was conservative and the patient was discharged asymptomatic on hospital day number six.
Fig. 1.

Abdominal ultrasound.
Fig. 2.

Abdominal ultrasound.
Fig. 3.
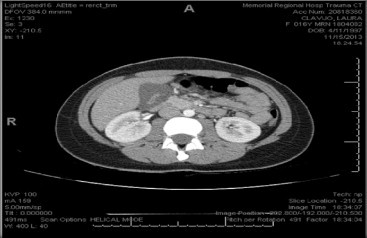
MRCP.
3. Discussion
EBV is known to be one of the causes of infectious hepatitis. Mild transient elevation in the serum aminotransferases have been previously reported and mild jaundice is described in approximately 5% of the cases, possibly caused by cholestasis or maybe by virus-induced hemolysis.1,5 The association between EBV infection and ACC has been previously reported, but it was described as an uncommon event.4
AAC is an inflammatory process of the gallbladder in the absence of gallstones. The disease is rare in childhood and most cases occur during the course of infectious diseases. Other etiologies included major cardiac or abdominal surgery, burns and prolonged parental nutrition. Criteria such as gallbladder wall thickening of over 3 mm, distention of the gallbladder, localized tenderness and pericolecystic fluid and sludge have been used for the diagnosis of ACC. The combination of two or more of the above criteria, in the appropriate clinical setting, is considering being diagnostic. Taking in consideration the sporadic presentation off ACC, the etiologic pattern and clinical spectrum of the disease in childhood have not been well established.1,6–8
Sixteen cases of ACC associated with isolated primary EBV infection have been described. Four of those in the pediatric population. In all reports, ACC subsided during the regression of the EBV infection without needing of surgical intervention.1–9 Our new patient presented with the clinical picture of Acute Cholecystitis and possible biliary obstructive pattern. Serologic test confirmed the primary EBV infection. ACC has an excellent prognosis, subsiding gradually during the regression of the infectious mononucleosis, as happened in most of the previous reported cases in the literature.
The exact pathogenesis of ACC remains uncertain, the main cause is thought to be bile stasis and increased lithogenicity of bile, resulting in gallbladder inflammation. Recently in the literature EBV-induced hepatitis has been recognized as an important cause of cholestasis.9 Our patient had cholestatic hepatitis due to confirmed EBV infection. Therefore the previous cases presented and our case supports the role of bile stasis in the pathogenesis of ACC, and also may suggest a possible role for acute EBV-infection as a possible role inducing cholestasis.
The presence of Gilbert's syndrome in patients with cholestasis of infectious origin (EBV-infection) could also play a role in the development of gallbladder abnormalities. The incidence of Gilbert's syndrome may contribute in the pathogenesis of ACC in children with EBV infection.10
Guala et al., who studied selected hospitalized pediatric patients, reported that EBV might impair liver function mostly in individuals homozygous or heterozygous for the UGT1A1*28 mutation. They also reported that a more severe clinical course of EBV infection could be expected as a consequence of this genetic variation. Hepatic involvement and the subsequent cholestasis during EBV infection are seen more often in individuals with Gilbert's syndrome.10,11
In the review of the literature 17 cases (including the present report) of EBV-associated ACC were collected. All cases were described between 2007 and 2013. In general all patients showed similar clinical manifestations. Hyperbilirubinemia and moderate transaminase level elevation were the most common associated laboratory findings. Ultrasound findings of wall thickening were between 6 and 15 mm. Only one patient (21 years old) reported in 2009 by Hagel et al. underwent cholecystectomy as a definite treatment.
4. Conclusion
Acute acalculous cholecystitis (ACC) may occur during the course of EBV infection in the pediatric population. Most of the cases reported were treated with medical management. First time diagnosis may be challenging; clinical and hematological parameters of viral infection are helpful in forming diagnostic suspicious. EBV infection need to be considered early in the differential diagnosis of ultrasound findings of ACC.
Conflict of interest
None.
Funding
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contribution
Literature review: Jesus Hidalgo. Writing: Jesus Hidalgo, Fuad Alkhoury and Diego Diaz. Reviewing: Diego Diaz.
Key learning points
Key Learning Points We ask that you provide concise bullet points that clearly state the key learning points from your work.
-
•
Acute acalculous cholecystitis
-
•
Mononucleosis
-
•
Epstein Barr virus
-
•
Gallbladder
-
•
Ultrasound
References
- 1.Valentina B., Antoluigi A. Epstein–Barr virus-associated with acute acalculous cholecystitis in adult. Am J Case Rep. 2012;13:153–156. doi: 10.12659/AJCR.883245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Macsween K.F., Crawford D.H. Epstein–Barr virus recent advances. Lancet Infect Dis. 2003;3:131–140. doi: 10.1016/s1473-3099(03)00543-7. [DOI] [PubMed] [Google Scholar]
- 3.Lagona E., Sharifi, Voutsioti A., Mavri A., Markouri M., Attilakos A. Epstein Barr virus infectious mononucleosis associated with acute acalculous cholecystitis. Infection. 2007;35:118–119. doi: 10.1007/s15010-007-6115-y. [DOI] [PubMed] [Google Scholar]
- 4.O’Donovan N., Fitzgerald E. Gallbladder wall thickening in infectious mononucleosis: an ominous sign. Postgrad Med J. 1996;72:299–300. doi: 10.1136/pgmj.72.847.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeson H.B. Acute complications of Epstein Barr virus infectious mononucleosis. Curr Opin Pediatr. 2000;12:263–268. doi: 10.1097/00008480-200006000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Tsakayannis D., Kozakewich H.P., Lilleli C.W. Acalculous cholecystitis in children. J Pediatr Surg. 1996;31:127–131. doi: 10.1016/s0022-3468(96)90334-6. [DOI] [PubMed] [Google Scholar]
- 7.Mendez S., Aguillar D., Chavez T. Hepatic manifestation of Epstein viral infection. Ann Hepatol. 2005;4:205–209. [PubMed] [Google Scholar]
- 8.Jimenez S., Perez P., Leal L., Herrerías G. Lethal liver failure in an elderly patient with hepatitis B superinfected with Epstein Barr virus. Eur Gastroenterol Hepatol. 2002;14:1283–1284. doi: 10.1097/00042737-200211000-00021. [DOI] [PubMed] [Google Scholar]; (b) Miguel C., Jose Caviedes, Guillermo D., Cesar P. Epstein Barr virus acute cholecystitis. BMJ Case Rep. 2012:1–2. doi: 10.1136/bcr.02.2012.5744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiara I., Lucia A., Giovanni D., Maria F: Acute acalculous cholecystitis during the course of primary Epstein Barr virus infection: a new case and a review of the literature. Int J Infect Dis. 2008;12:391–395. doi: 10.1016/j.ijid.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Achilleas A., Alexia P., George H. Acute acalculous cholecystitis in children with Epstein Barr virus infection: a role for Gilbert's syndrome? Int J Infect Dis. 2009;13:161–164. doi: 10.1016/j.ijid.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Guala A., Campra D., Marinel L.I.l. Are Gilbert's syndrome and liver involvement genetically linked in infectious mononucleosis? Pediatr Infect Dis J. 2003;22:1110–1111. doi: 10.1097/01.inf.0000101789.93016.d9. [DOI] [PubMed] [Google Scholar]


