Highlights
-
•
Squamous cell carcinoma arising from an epidermal cyst is rare.
-
•
The most frequently affected region is the head and neck. In contrast, involvement of the fingers is extremely rare.
-
•
The clinical symptoms of squamous cell carcinoma arising from an epidermal cyst can mimic those of an infected epidermal cyst.
-
•
The current report facilitates awareness of such disease.
Abbreviations: MRI, magnetic resonance imaging; CRP, C-reactive protein
Keywords: Squamous cell carcinoma, Epidermal cyst, Thumb
Abstract
Introduction
Squamous cell carcinoma arising from an epidermal cyst is rare, and the most frequently affected region is the head and neck.
Presentation of case
A 41-year-old man noticed swelling and a small ulceration in the thumb pulp. A lesion with a 2-cm diameter was simply resected based on a diagnosis of infected epidermal cyst. Pathological diagnosis of the resected material was squamous cell carcinoma arising from an epidermal cyst. Consequent amputation was performed.
Discussion and conclusion
The clinical symptoms of squamous cell carcinoma arising from an epidermal cyst can mimic those of an infected epidermal cyst. The current report facilitates awareness of such disease.
1. Introduction
Epidermal cysts are common lesions, and are characterized by a lining composed of squamous epithelium [1]. Squamous cell carcinoma arising from an epidermal cyst is rare. The reported frequency of squamous cell carcinoma arising from epidermal cysts ranges from 0.011 to 0.045% [2,3]. The most frequently affected region is the head and neck, which represents 40% of cases [3]. In contrast, involvement of the fingers is extremely rare. Herein, we report a case of squamous cell carcinoma arising from an epidermal cyst in the thumb.
2. Case report
A 41-year-old man had noticed swelling on the right thumb pulp 2 weeks before, and was referred to our hospital. A small ulceration was observed on the radial side of the thumb. Plain radiographs showed osteolysis at the flexor side on the distal phalanx. Periosteal reaction was not observed in the lesion (Fig. 1A and B). No laboratory data abnormalities were detected, except for a slight elevation of the inflammatory marker C-reactive protein (CRP) (1.4 mg/dL). Magnetic resonance imaging (MRI) revealed that the lesion measured 2 cm in longitudinal diameter. The lesion displayed low signal intensity on T1-weighted images (Fig. 1C) and heterogeneous low to moderate signal intensity on T2-weighted images (Fig. 1D). Gadolinium enhancement was absent inside the lesion on T1-weighted fat-suppression images (Fig. 1E). Based upon the diagnosis of an infected epidermal cyst, an oral antibiotic was administered for 1 week, and the swelling decreased. After the medication was stopped, the swelling reappeared. Consequent intravenous antibiotic medication was moderately effective. Resection of the lesion was performed. During surgery, the structure of the cystic wall was determined to be vague, and the margin to the surrounding tissue was unclear. Whitish material consisting of an epidermal cyst and granulated tissue-like material was observed in the interior of the lesion. The lesion was resected completely macroscopically. Pathological findings of the resected material showed a squamous epithelium-lined epidermal cyst (Fig. 2A). In addition, atypical keratinized cells consisting of squamous cell carcinoma were also observed (Fig. 2B and C). Based on the diagnosis of squamous cell carcinoma, disarticulation at the distal interphalangeal joint was performed.
Fig. 1.
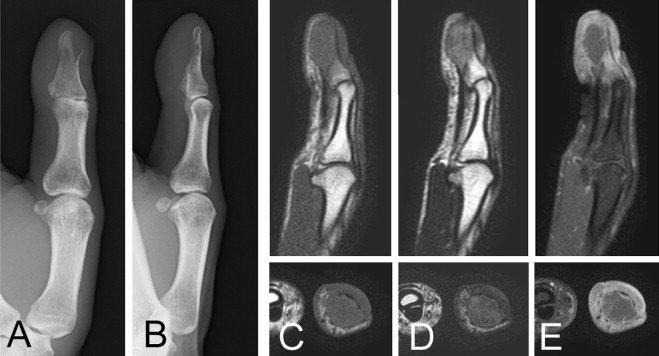
Plain radiographs show that the cortical bone of the distal phalanx has disappeared at the flexor side, and the remaining bone is thinned (A and B). MRI images display low signal intensity on T1-weighted images (C), and heterogeneous low to moderate signal intensity on T2-weighted images (D). No gadolinium enhancement is observed inside of the lesion (E).
Fig. 2.
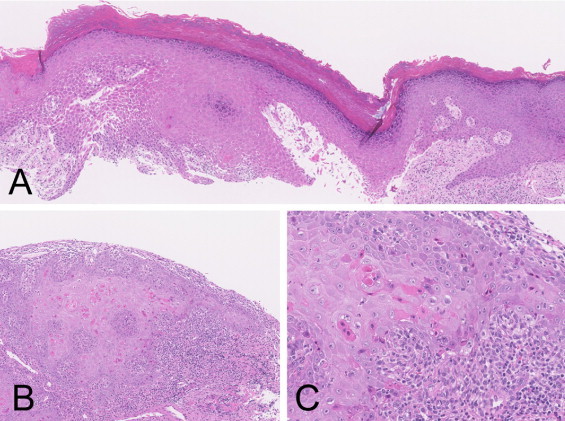
The cystic lesion shows an epidermal cyst with keratinized epithelium (A). Atypical keratinized cells are also seen, suggesting squamous cell carcinoma (B and C).
An air tourniquet was used during the curettage and the amputation. A combination of a brachial plexus block and general anesthesia has been used for these surgical procedures. No recurrence or metastasis was observed during 3 years of follow-up care after the amputation.
3. Discussion
The current case is consistent with an epidermal cyst with malignant transformation to squamous cell carcinoma. A previous review described 19 cases of squamous cell carcinoma arising from epidermal cysts. The series consisted of 13 men and 6 women, ranging in age from 21 to 80 years old (mean, 43.2 years old) [3]. The lesion size ranged from 1.5 to 13 cm (mean, 5.7 cm). The head and neck are the most affected sites (42.1% of cases) [3]. With respect to fingers and thumbs, only one case in the index finger has been reported [3]. Metastasis was observed in 3 of the 19 cases [3].
Malignant transformation is characterized by a long duration: the duration to malignant changes of lesions ranged from 2 to 480 months (mean, 101 months) [3–5]. The mechanism underlying malignant transformation in an epidermal cyst is not clear [6,7]. However, chronic irritation and actinic damage have been proposed as contributing factors. The present patient is a laborer, and the affected site was the thumb. Therefore, chronic irritation and actinic damage are possible causes of malignant transformation. The patient did not notice the lesion until malignant transformation had occurred; the preexisting epidermal cyst in the thumb pulp appeared to be too small to be noticed.
The preoperative diagnosis of the current case was an infected epidermal cyst based upon clinical appearance and MRI findings. MRI is useful for assessing the overall tumor and the association with the neighboring tissues. A pre-operative MRI is considered necessary for resection of a tumor involving the finger or thumb. In the current case gadolinium enhancement MRI was useful to confirm the cystic nature of the mass. However, a similar appearance between infected epidermal cysts and malignant transformed epidermal cysts has been previously reported [4]. Therefore, histological confirmation is required for resected epidermal cysts, particularly for suspected infected epidermal cysts, to exclude malignant transformation. In cases in which malignant transformation of epidermal cyst is diagnosed, additional resection is necessary. It is proposed that margins of 4–6 mm for resection are required based on the treatment of cutaneous squamous cell carcinoma [7]. In the current case, after the diagnosis of a squamous cell carcinoma in the curetted material had been established, the MRI was repeated to assess the residual lesion and the inflammatory findings due to the curettage, and the level of amputation required.
4. Conclusion
In summary, squamous cell carcinoma arising from an epidermoid is rare. The most frequently affected region is the head and neck. The current reported thumb case is extremely rare with respect to location. The clinical symptoms mimic that of an infected epidermal cyst. The current report facilitates awareness of such disease.
Conflict of interest
None declared.
Funding
None.
Ethical approval
Because of the case report, the ethics committee was not held.
Authors contribution
Akio Sakamoto: study design, data collections, data analysis and writing.
Eisuke Shiba and Masanori Hisaoka are pathologists for the diagnosis the lesion.
Consent
A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Guarantor
Akio Sakamoto accepts the full responsibility for the article.
References
- 1.Enzinger F.M., Weiss S.W. CV Mosby; St. Louis: 2008. Soft Tissue Tumors. [Google Scholar]
- 2.Chiu M.Y., Ho S.T. Squamous cell carcinoma arising from an epidermal cyst. Hong Kong Med. J. 2007;13:482–484. [PubMed] [Google Scholar]
- 3.Antón-Badiola I., San Miguel-Fraile P., Peteiro-Cancelo A., Ortiz-Rey J.A. Squamous cell carcinoma arising on an epidermal inclusion cyst: a case presentation and review of the literature. Actas Dermosifiliogr. 2010;101:349–353. [PubMed] [Google Scholar]
- 4.Cappello Z.J., Kasdan M.L., Augenstein A.C., Shaheen S.P. Squamous cell carcinoma in an epidermoid cyst. Eplasty. 2013;26:44. [PMC free article] [PubMed] [Google Scholar]
- 5.Lin C.Y., Jwo S.C. Squamous cell carcinoma arising in an epidermal inclusion cyst. Chang Gung Med. J. 2002;25:279–282. [PubMed] [Google Scholar]
- 6.Tokunaga M., Toya M., Endo Y., Fujisawa A., Tanioka M., Kato M., Miyachi Y. A case of an undifferentiated squamous cell carcinoma arising from an epidermal cyst. Case Rep. Dermatol. Med. 2013;2013:469516. doi: 10.1155/2013/469516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shabbir A., Loss L., Bogner P., Zeitouni N.C. Squamous cell carcinoma developing from an epidermoid cyst of the ear. Dermatol. Surg. 2011;37:700–703. doi: 10.1111/j.1524-4725.2011.01977.x. [DOI] [PubMed] [Google Scholar]


