Highlights
-
•
We describe a case of a 3 years old girl, with all features of Herlyn–Werner–Wunderlich syndrome (HWWS) who came to our attention for lower abdominal mass.
-
•
Only six cases are reported in Literature with early onset of this syndrome under 5 years.
-
•
The aim of this article is to share our experience and focus the attention on the importance of high level of suspicion of HWWS in neonatal period to early diagnosis and treatment.
-
•
The possible early presentation of this syndrome should be suspected in all neonates (females) with renal agenesia confirmed postnatally or with prenatal diagnosis.
-
•
An error of evaluation with planning of removal of mass, that can damage patients in term of chance for a successful reproductive outcome.
-
•
Our team consider HWWS as differential diagnosis in newborn with prenatal ultrasonography of a cystic mass behind the urinary bladder in the absence of a kidney and plan a pelvic ultrasound (with aim to identify an uterus, normal or dydhelfus, and presence or absence of pelvic mass), an examination under anesthesia and cisto-vaginoscopy, if it is necessary. A high level of suspicion, indeed, is the key to early diagnosis.
Keywords: Herlyn–Werner–Wunderlich syndrome, Congenital mullerian anomaly
Abstract
Herlyn–Werner–Wunderlich syndrome (HWWS) is a rare congenital mullerian anomaly consisting of uterus didelphys, hemivaginal septum, and unilateral renal agenesis [1,2]. Most authors reported cases of Herlyn–Werner–Wunderlich syndrome with prepuberal or postpuberal onset with cyclical abdominal pain and a vaginal mass (3–8). Only six cases are reported in Literature with early onset of this syndrome under 5 years (9–14). Our case is about 3 years old girl, with all the features of this syndrome who came to our attention for lower abdominal mass. The aim of this article is to share our experience and focus the attention on the importance of high level of suspicion of HWWS in neonatal period to early diagnosis and treatment. The possible early presentation of this syndrome should be suspected in all neonates (females) with renal agenesia confirmed postnatally or with prenatal diagnosis. It is common, in fact, an error of evaluation with planning of removal of mass, that can damage patients in term of chance for a successful reproductive outcome. For all these reasons, our team consider HWWS as differential diagnosis in newborn with prenatal ultrasonography of a cystic mass behind the urinary bladder in the absence of a kidney and plan a pelvic ultrasound (with aim to identify an uterus, normal or dydhelfus, and presence or absence of pelvic mass), an examination under anesthesia and cystoscopy and vaginoscopy, if it is necessary. A high level of suspicion, indeed, is the key to early diagnosis.
1. Introduction
Herlyn–Werner–Wunderlich syndrome (HWWS) is a rare congenital mullerian anomaly consisting of uterus didelphys, vaginal septum, and unilateral renal agenesis [1,2]. Most authors reported cases of Herlyn–Werner–Wunderlich syndrome with prepuberal or postpuberal onset with cyclical abdominal pain and a vaginal mass [3–8]. Only six cases are reported in Literature with early onset of this syndrome under 5 years [9–14]. Our case is about 3 years old girl, with all the features of this syndrome who came to our attention for lower abdominal mass. The aim of this article is to share our experience and focus the attention on the importance of high level of suspicion of HWWS in neonatal period to early diagnosis and treatment.
2. Case report
A 3-years-old girl was admitted to our department with diagnosis of lower abdominal mass, that had made at other hospital, associated with 1 year history of lower abdominal pain. This pain had worsened in the last 5 months and it was sometimes associated with dysuria. On physical examination, a tender, mobile, and painless mass was palpated in the right lower abdomen. The external genitalia were normal in appearance, no alterations of external genitalia or hymen, but her vaginal mucosa appeared to bulge into the perineum. Routine urine and blood exams were normal. Abdominal and pelvis ultrasound (US) showed a cystic mass in the pelvic cavity measuring 3 × 5 cm, normal uterus, no visualized right kidney, suggesting its absence. MRI with contrast was performed and showed 2 communicating cystic masses in right lower abdomen and pelvis. The upper measured 6 × 2 cm and the lower 1.5 × 2.5 cm (Fig. 1). The lower was placed between bladder and rectum. Only right ovary was identified. The uterus appeared normal for age. The right kidney absence was confirmed. Transverse vaginal septum was identified. After discussion about differential diagnosis, we suspected HWWS syndrome and we planned an examination under anesthesia and cystoscopy and vaginoscopy. Cystoscopy showed normal bladder with absence of right hemitrigone and evidence of normal left ureteric orifice. Careful examination of genitalia revealed that a bulging of the vagina was a right transverse vaginal septum (Fig. 2). Intraoperative vaginoscopy by left orifice revealed a normal hemivagina, with cervix, and blind right hemivagina. A transhymenal resection of vaginal septum was performed with releasing of mucous (100 cc about) (Figs. 3 and 4). A final vaginoscopy showed unique vaginal cavity with double cervix. A 12F Foley catheter was placed in the bladder. The postoperative recovery was uneventful; bladder catheter was removed in third postoperative day. The child drained mucous from the vagina for about 20 days after surgery. One month postoperatively, follow-up ultrasound examination revealed absence of pelvic mass, not abdominal fluid, didelphys uterurus (not seen on the previous ultrasounds) and both ovaries. The child has been followed up for 1 year, she is healthy and symptom free. External genitalia are normal on physical examination. The plan is to follow up the child regularly until puberty in association with our gynecologist.
Fig.1.
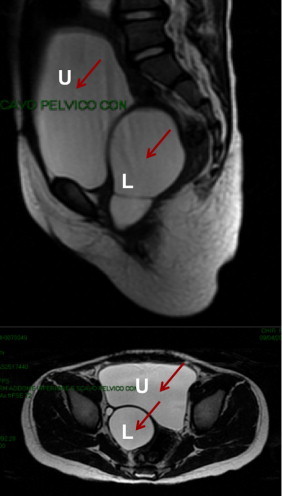
MRI showing two cysts. Upper (U) 6 × 2 cm and lower (L) 1.5 × 2.5 cm.
Fig. 2.
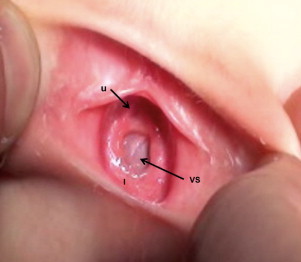
Physical examination of genitalia. U (urethra), I (hymen), VS (vaginal septum).
Fig. 3.
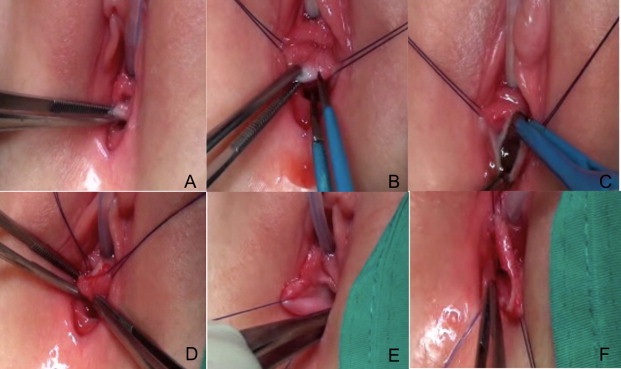
(A) Identification of transverse vaginal septum; (B) section by bipolar of vaginal septum; (C and D) evidence of spill of mucus (hydrocolpus); (E and F) evidence of left hemivagina (E) and right hemivagina (F).
Fig. 4.
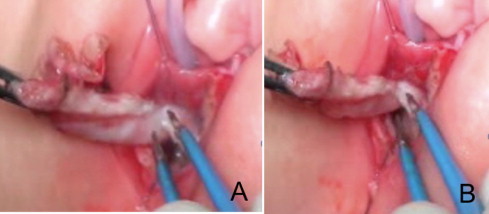
(A and B) Removal of vaginal septum.
3. Discussion
Herlyn–Werner–Wunderlich syndrome consists of unilateral renal agenesis, a blind vagina, and uterus didelphys.
The association of renal agenesis with unilateral blind hemivagina was reported as Herlyn–Werner syndrome in 1971 [15], whereas the association of renal aplasia, bicornuate uterus with isolated hematocervix, and a simple vagina was reported by Wunderlich in 1976 [16]. This syndrome is a rare variant within the spectrum of mullerian duct anomalies. The most basic classification of mullerian ductal defects consists of (a) agenesis and hypoplasia, (b) defects of vertical fusion, and (c) defects of lateral fusion [8]. Indeed, HWWS may represent a failure of vertical and lateral fusion of mullerian structures. The actual incidence of mullerian anomalies is unknown. Patients with HWWS are usually asymptomatic until menarche when they present an hydrometrocolpos on the side of obstructed hemivagina producing a mass effect and pain. However, the diagnosis of HWWS may be delayed by several months because menstruation is often normal. Many authors [3–8], indeed, reported cases of HWWS in postpubertal adolescents or adult women where hematometrocolpos produces a more pronounced mass effect and pain with more complications. If this syndrome is suspected, the diagnosis is simply and it can be made by ultrasound and computed tomography and/or MRI of the abdomen and pelvis [17]. Resection of the vaginal septum is the treatment of choice for obstructive hemivagina. It can be made by abdominal approach through a Pfannenstiel incision or laparoscopy or by trans-hymenal approach [3–14,18]. In our opinion, the transhymenal approach is the best choice because it is efficent and simply to apply, reducing risks of abdominal surgery and with good esthetic results. However, a certain preoperative diagnosis must be present to perform it. The timing of diagnosis is an important goal for surgeon to avoid complications and preserve reproductive capacity. Laparoscopic approach should be reserved to cases of adolescent with suspicion of endometriosis that can be associated with HWWS [6]. Patients with this syndrome after treatment can have normal sexual relations and fertility is not compromised, even if the spontaneous abortion rate is high (40%) [19]. We decided to describe our case and share our experience based on the results of review of Literature. The largest series of HWWS are summarized in Table 1 [3–8], but all of these reported adolescent patients or prepuberal. We found only 6 cases of HWWS with onset under 5 years and their main features are shown in Table 2 [9–14]. Our case is the seventh “early” case of HWWS in Literature.
Table 1.
This table summarizes the largest series of HWWS.
| Series-n (references) |
Median age at presentation | Symptoms | Treatment |
|---|---|---|---|
| 13 [3] | 17.2 years | Severe pelvic pain, progressive dysmenorrhea, and irregularity in menses | 7 Vaginal septum excision and marsupialization |
| 4 Refused procedures | |||
| 2 Clinical follow-up | |||
| 39 [4] | 18.1 years | Dysmenorrhea | Surgical treatment |
| Cystic mass in vaginal wall | |||
| Abnormal vaginal discharge | |||
| 87 [5] | 20.7 years | Dysmenorrhea (94%), spotting (41%), chronic pelvic pain (24%), vaginal discharge (14%), dyspareunia (14%), fever (3%), and acute abdomen pain (2%) | Vaginal excision of obstructive septum ± isteroscopic metroplasty ± cervicoplasty |
| 70 [6] | 16.4 years | Dysmenorrhea | Vaginal septectomy |
| Intermittent mucopurulent discharge | |||
| Irregular vaginal hemorrhage | |||
| Endometriosis | |||
| Acute pelvic inflammation | |||
| 11 [7] | 13 years | Lower abdominal pain, progressive dysmenorrhoea, irregular menses, discharge of longstand-ing, partially clotted menstrual blood, menorrhagia, and acute abdominal pain | Surgical treatment of the haematocolpos/haematometrocol-pos |
| 12 [8] | 13 years | Menstrual irregularity 4 | All patients were treated by vaginal septectomy with marsupialization and drainage of the hematocolpos/hema-tometrocolpos |
| Abdominal pain 11 | One patient required a laparotomy and salpingectomy for pyosalpinx and intraabdominal abscess formation | ||
| Abdominal–pelvic mass 11 | |||
| Intraabdominal abscess 2 menstrual bleeding (n) 7 |
Table 2.
This table summarizes all cases of HWWs, under 5 years old, who are reported in Literature.
| Patient (reference) | Age at presentation | Symptoms/history | Treatment |
|---|---|---|---|
| 1 [9] | 5 months | Acute urinary retention | Not known |
| 1 [10] | 3 years | Painless abdominal mass | Endoscopic incision and resection |
| She had a history of prior open drainage of a similar mass on day 1 of life and percutaneous drainage of a similar mass at age 1 year | |||
| 1 [11] | 4 years | History of abdominal pain of 1-year duration | Abdominal exploration through a Pfannenstiel |
| 1 [12] | Newborn | Prenatal diagnosis of a dilated left pelvic kidney and postnatal diagnosis of a uterus didelphys with a communication between the left hemiuterus and the fluid-filled structure | Trans-hymenal surgical resection |
| 1 [13] | Newborn | A reddish, prolapsed mass over the infant’s vaginal introitus | Trans-hymenal incision and catheter drainage |
| 1 [14] | Newborn | Prenatal sonography revealed the absence of the left kidney and a retrovesical cystic lesion suspected as hydrometrocolpos. Postnatal evaluation confirmed that the cystic lesion was a hydrocolpos associated with double uterus and blind hemivagina | Not known |
4. Conclusion
In conclusion, the main aim of this report is focusing the attention on the possible early presentation of this syndrome that should be suspected in all neonates (females) with renal agenesia confirmed postnatally or suspected prenatally. It is common, in fact, an error of evaluation with planning of removal of mass, that can damage patients in term of chance for a successful reproductive outcome. For all these reasons, our team considers HWWS as differential diagnosis in newborn with prenatal ultrasonography of a cystic mass behind the urinary bladder in the absence of a kidney and plan a pelvic ultrasound (with aim to identify an uterus, normal or didelphys, and presence or absence of pelvic mass), an examination under anesthesia and cystoscopy and vaginoscopy, if it is necessary. A high level of suspicion, indeed, is the key to early diagnosis.
Conflict of interests
The authors have no conflicts of interest to disclose. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
No funding was secured for this study.
Financial disclosure
The remaining authors have no financial relationships relevant to this article to disclose.
Authors contribution
All authors conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Dr. Angotti Rossella conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Dr Francesco Molinaro conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Dr. Bulotta Anna Lavinia conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Dr. Bindi Edoardo conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Dr. Elisa Cerchia conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Dr. Marina Sica conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Prof. Mario Messina conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
All are agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Consent
We have consent form from patient.
Guarantor
Rossella Angotti is the guarantor of this paper.
References
- 1.Karaca L., Pirimoglu B., Bayraktutan U., Ogul H., Oral A., Kantarci M. Herlyn–Werner–Wunderlich syndrome a very rare urogenital anomaly in a teenage girl. J. Emerg. Med. 2014;(December (8)) doi: 10.1016/j.jemermed.2014.09.064. pii: S0736-4679(14) 1108-1. [DOI] [PubMed] [Google Scholar]
- 2.Van Leerdam L.E., Beerendonk C.C., Klein W.M., Sir O. Herlyn–Werner–Wunderlich syndrome. Nederlands Tijdschrift Voor Geneeskunde. 2014;158(December):A7886. Dutch. [PubMed] [Google Scholar]
- 3.Yavuz A., Bora A., Kurdoğlu M., Goya C., Kurdoğlu Z., Beyazal M., Akdemir Z.J. Herlyn–Werner–Wunderlich syndrome merits of sonographic and magnetic resonance imaging for accurate diagnosis and patient management in 13 cases. Pediatr. Adolesc. Gynecol. 2014 doi: 10.1016/j.jpag.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Wang J., Zhu L., Lang J., Liu Z., Sun D., Leng J., Fan Q. Clinical characteristics and treatment of Herlyn–Werner–Wunderlich syndrome. Arch. Gynecol. Obstet. 2014;290(November (5)):947–950. doi: 10.1007/s00404-014-3286-5. [DOI] [PubMed] [Google Scholar]
- 5.Fedele L., Motta F., Frontino G., Restelli E., Bianchi S. Double uterus with obstructed hemivagina and ipsilateral renal agenesis: pelvic anatomic variants in 87 cases. Hum. Reprod. 2013;28(June (6)):1580–1583. doi: 10.1093/humrep/det081. [DOI] [PubMed] [Google Scholar]
- 6.Zhu L., Lang J., Tong J. Clinical characteristics of 70 patients with Herlyn–Werner–Wunderlich syndrome. Int. J. Gynaecol. Obstet. 2013;121(May (2)):173–175. doi: 10.1016/j.ijgo.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 7.Cinzia O.M., Lucchetti C., Schingo P.M.S. Herlyn–Werner–Wunderlich syndrome uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr. Radiol. 2007;37(7):657–665. doi: 10.1007/s00247-007-0497-y. [DOI] [PubMed] [Google Scholar]
- 8.Gholoum S., Puligandla P.S., Hui T. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn–Werner–Wunderlich syndrome) J. Pediatr. Surg. 2006;41:987–992. doi: 10.1016/j.jpedsurg.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Pansini L. Acute urinary retention due to didelphys uterus associated with an obstructed hemivagina in a 5-month-old infant. J. Pediatr. Surg. 1988;23:984–985. doi: 10.1016/s0022-3468(88)80402-0. [DOI] [PubMed] [Google Scholar]
- 10.Roth M., Mingin G., Dharamsi N., Psooy K., Koyle M. Endoscopic ablation of longitudinal vaginal septa in prepubertal girls a minimally invasive alternative to open resection. J. Pediatr. Urol. 2010;6(October (5)):464–468. doi: 10.1016/j.jpurol.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Sanghvi Y., Shastri P., Mane S.B., Dhende N.P. Prepubertal presentation of Herlyn–Werner–Wunderlich syndrome a case report. J. Pediatr. Surg. 2011;46(June (6)):1277–1280. doi: 10.1016/j.jpedsurg.2011.02.067. [DOI] [PubMed] [Google Scholar]
- 12.Vivier P.H., Liard A., Beurdeley M., Brasseur-Daudruy M., Cellier C., Le Dosseur P., Dacher J.N. Uterus didelphys hemihydrocolpos and empty ipsilateral lumbar fossa in a newborn girl: involuted dysplastic kidney rather than renal agenesis. Pediatr. Radiol. 2011;41(September (9)):1205–1207. doi: 10.1007/s00247-011-2046-y. [DOI] [PubMed] [Google Scholar]
- 13.Wu T.H., Wu T.T., Ng Y.Y., Ng S.C., Su P.H., Chen J.Y., Chen S.J. Herlyn–Werner–Wunderlich syndrome consisting of uterine didelphys, obstructed hemivagina and ipsilateral renal agenesis in a newborn. Pediatr. Neonatol. 2012;53(February (1)):68–71. doi: 10.1016/j.pedneo.2011.11.014. Epub 2012 January 24. [DOI] [PubMed] [Google Scholar]
- 14.Han B.H., Park S.B., Lee Y.J., Lee K.S., Lee Y.K. Uterus didelphys with blind hemivagina and ipsilateral renal agenesis (Herlyn–Werner–Wunderlich syndrome) suspected on the presence of hydrocolpos on prenatal sonography. J. Clin. Ultrasound. 2013;41(July–August (6)):380–382. doi: 10.1002/jcu.21950. [DOI] [PubMed] [Google Scholar]
- 15.Herlyn U., Werner H. Simultaneous occurrence of an open Gartner-duct cyst: a homolateral aplasia of the kidney and a double uterus as a typical syndrome of abnormalities. Geburtshife Frauenheikd. 1971;31:340–347. [PubMed] [Google Scholar]
- 16.Wunderlich M. Unusual form of genital malformation with aplasia of the right kidney. Zentralbl Gynakol. 1976;98:559–562. [PubMed] [Google Scholar]
- 17.Tanaka Y.O., Kurosaki Y., Kobayashi T. Uterus didelphys associated with obstructed hemvagina and ipsilateral renal agenesis: MR findings in seven cases. Abdom. Imaging. 1998;23:437–441. doi: 10.1007/s002619900375. [DOI] [PubMed] [Google Scholar]
- 18.Dorais J., Milroy C., Hammoud A., Chaudhari A., Gurtcheff S., Peterson C.M. Conservative treatment of a Herlyn–Werner–Wunderlich müllerian anomaly variant noncommunicating hemiuterus with Gartner duct pseudocyst. J. Minim. Invasive Gynecol. 2011;18(March–April (2)):262–266. doi: 10.1016/j.jmig.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Propst A.M., Hill J.A., III Anatomic factors associated with recurrent pregnancy loss. Semin. Reprod. Med. 2000;18:341–350. doi: 10.1055/s-2000-13723. [DOI] [PubMed] [Google Scholar]


