Abstract
Urgent action is needed to reduce the harm caused by smoking. Product standards that reduce the addictiveness of cigarettes are now possible both in the U.S. and in countries party to the Framework Convention on Tobacco Control. Specifically, standards that required substantially reduced nicotine content in cigarettes could enable cessation in smokers and prevent future smoking among current non-smokers. Behavioral economics uses principles from the field of microeconomics to characterize how consumption of a reinforcer changes as a function of the unit price of that reinforcer (unit price = cost / reinforcer magnitude). A nicotine reduction policy might be considered an increase in the unit price of nicotine because smokers are paying more per unit of nicotine. This perspective allows principles from behavioral economics to be applied to nicotine reduction research questions, including how nicotine consumption, smoking behavior, use of other tobacco products, and use of other drugs of abuse are likely to be affected. This paper reviews the utility of this approach and evaluates the notion that a reduction in nicotine content is equivalent to a reduction in the reinforcement value of smoking—an assumption made by the unit price approach.
1. Introduction
The Family Smoking Prevention and Tobacco Control Act gives the FDA the authority to regulate cigarettes (US Congress, 2009). Included in the act is the authority to reduce the content of nicotine to any non-zero level, a strategy that has been suggested for reducing the prevalence of smoking (Benowitz and Henningfield, 1994, Benowitz and Henningfield, 2013, US Department of Health and Human Services, 2014). Similar standards could be set by countries party to the Framework Convention on Tobacco Control; Article 9 allows for guidelines on the regulation of the content and emissions of tobacco products. Recent studies support nicotine reduction as a promising approach by showing that substantial reductions in nicotine content can result in reduced toxicant exposure and, in some cases, a reduction in smoking behavior and dependence (Benowitz et al., 2012, Benowitz et al., 2007, Donny et al., 2007, Hatsukami et al., 2010a, Hatsukami et al., 2010b). Notably, required reductions in the nicotine content in cigarettes would differ from existing reduced yield cigarettes which yield less nicotine when smoked by a machine, but less so when smoked by humans (Hoffmann and Hoffmann, 2001).
1.1 Behavioral economics: A unique framework for nicotine reduction
Behavioral economics borrows principles from the field of microeconomics to describe how consumption of a reinforcer changes as the unit price of that reinforcer is manipulated (unit price = cost / reinforcer magnitude) (See Hursh and Roma, 2013 for a recent review and tutorial of the approach). A behavioral economics framework asserts that consumption of a reinforcer is related to the unit price of that reinforcer and the unit price of concurrently available reinforcers. Manipulations in unit price often take place through increases in cost (i.e., the numerator) such as increases in monetary value, effort, or time required obtaining the reinforcer (Hursh and Roma, 2013). An example of this approach is taxation, which has been reliably shown to drive down consumption (Chaloupka, Chaloupka and Warner, 1999). Importantly, a decrease in the magnitude of the reinforcer (i.e., the denominator) should be functionally equivalent to an increase in cost (Bickel et al., 1990) and may represent an underutilized approach to tobacco control. The relationship between cost and reinforcer magnitude is rather intuitive on the surface—if the price of a pack of cigarettes is doubled, the change in cigarette consumption should be the same as if the number of cigarettes in a pack were cut in half, because the price per cigarette (i.e., unit price) has been changed in the same way.
Decades of research suggest that the primary reason people smoke is to obtain nicotine (US Department of Health and Human Services, 1988, Stolerman and Jarvis, 1995). Hence, a reduction in nicotine content may be thought of as an increase in the unit price of nicotine. This perspective allows for the application of behavioral economics approaches to be applied to research questions related to potential product standards for nicotine (Donny et al., 2012). The purpose of the present paper is to describe how a behavioral economics framework might be used to advance research related to nicotine regulation, and discuss the implications of such a framework.
2. How will nicotine reduction affect nicotine consumption and smoking behavior?
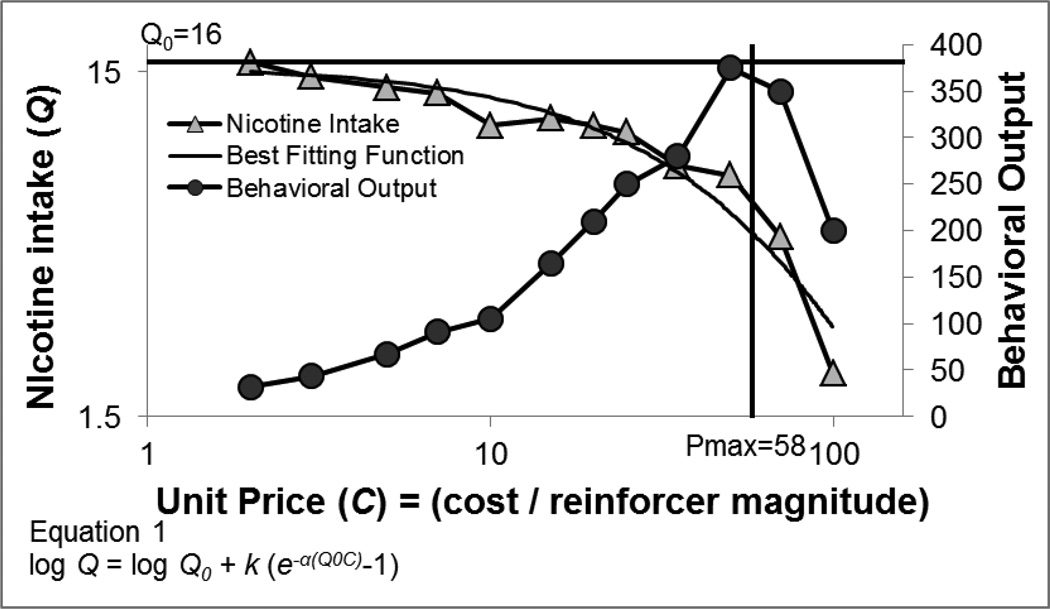
Behavioral economics uses demand curves to characterize changes in consumption of a reinforcer as a function of unit price (Hursh and Silberberg, 2008). An example of a demand curve and a curve showing corresponding changes in behavior can be seen in Figure 1. Assuming people smoke to obtain nicotine, a demand curve can be generated by using nicotine content as reinforcer magnitude to calculate unit price. However, changes in nicotine content may not translate easily into changes in nicotine intake (Figure 1), as intake will be influenced by changes in smoking behavior (e.g., cigarettes per day, puff volume). In a hypothetical nicotine reduction policy, nicotine content is reduced but other, potentially harmful, cigarette components, such as tar, remain unchanged. Thus, any increase in smoking behavior (i.e., any compensation) will likely result in a negative health impact. Nicotine intake can be measured through the use of biomarkers of nicotine exposure (e.g., cotinine, total nicotine equivalents). This approach should account for all the ways in which nicotine intake can change as a function of changes in smoking behavior. The behavioral output (Figure 1) required to achieve a given level of nicotine intake is best viewed as a composite measure of smoking behavior and should be closely related to total smoke exposure.
Figure 1.
Example of demand curve plotting consumption as a function of unit price (triangles) and corresponding changes in behavior (circles). The demand curve plots nicotine consumption as a function of increases in unit price. Best fitting function for the demand curve using Equation 1 is plotted using solid line. In Equation 1, Q and C are consumption and unit price, respectively; k is a scaling parameter specifying the range of the dependent variable. Q0 is a free parameter estimating consumption if the reinforcer were free (graphically the y-intercept), and α is a free parameter describing sensitivity to increases in unit price (graphically rate of change in the slope). Pmax is the unit price at which demand switches from inelastic to elastic (plotted here as the Pmax estimated from Equation 1), and at this price, the maximum amount of behavioral output is observed.
An exponential equation, shown in Figure 1, can be used to describe demand curves (Hursh and Silberberg, 2008). Demand curves are typically downward sloping in that consumption (Q) decreases as the unit price of the reinforcer (C) is increased, suggesting that nicotine intake is likely to decrease as nicotine content is decreased. Across a range of low unit prices, decreases in nicotine intake are proportionally less than the increase in unit price and demand is referred to as inelastic. Decreases in nicotine intake as unit price is increased are less than might be predicted because smoking behavior, and consequently smoke exposure, increases (i.e., compensation). Across a range of higher unit prices, decreases in nicotine intake are proportionally greater than the increase in unit price and demand is referred to as elastic. In this case, decreases in nicotine intake are greater than might be predicted because smoking behavior decreases as unit price increases. The estimated unit price at which demand would switch between inelastic and elastic is termed Pmax, and at this unit price the predicted maximum amount of behavioral output (i.e., compensation), termed Omax, would be observed. Thus, when smoking behavior is plotted as a function of descending nicotine content, the function is likely to have an ascending and a descending limb, corresponding to the inelastic and elastic portions of a demand curve. For any level of smoking behavior (and smoke exposure) on the inelastic portion of the curve, there is a price that will produce equivalent smoking behavior on the elastic portion of the curve. Unit prices between these two prices result in compensation and unit prices outside of this range result in decreased exposure. Given one of these two unit prices and a complete demand curve, the corresponding unit price could be easily calculated. The two free parameters in Equation 1, Q0 and α, describe predicted nicotine intake when the reinforcer is free (graphically the y-intercept), and sensitivity to increases in unit price (graphically the rate of change in slope), respectively (Hursh and Silberberg, 2008). Data suggest that the typical relationship between unit price, intake, and behavioral output, is indeed likely to extend to changes in nicotine content (Bickel et al., 1991). DeGrandpre et al. (1992) reanalyzed 17 data sets from studies where nicotine yield was manipulated (e.g., through brand switching, shortened cigarettes), and found that nicotine intake adhered to typical demand curves.
Demand curves provide a more complete characterization of the relationship between changes in nicotine content and nicotine intake than traditional measures. Previous nicotine research has used a compensation index (CI) (Benowitz et al., 2012, Scherer, 1999, Grebenstein et al., 2013, Harris et al., 2011, Benowitz et al., 2005, Stephen et al., 1989). This approach has been frequently used to study differences in machine-measured nicotine yields between regular and light or ultralight cigarettes; however, the same concept can be applied to manipulations of nicotine content, when other features of product design are assumed to be constant:
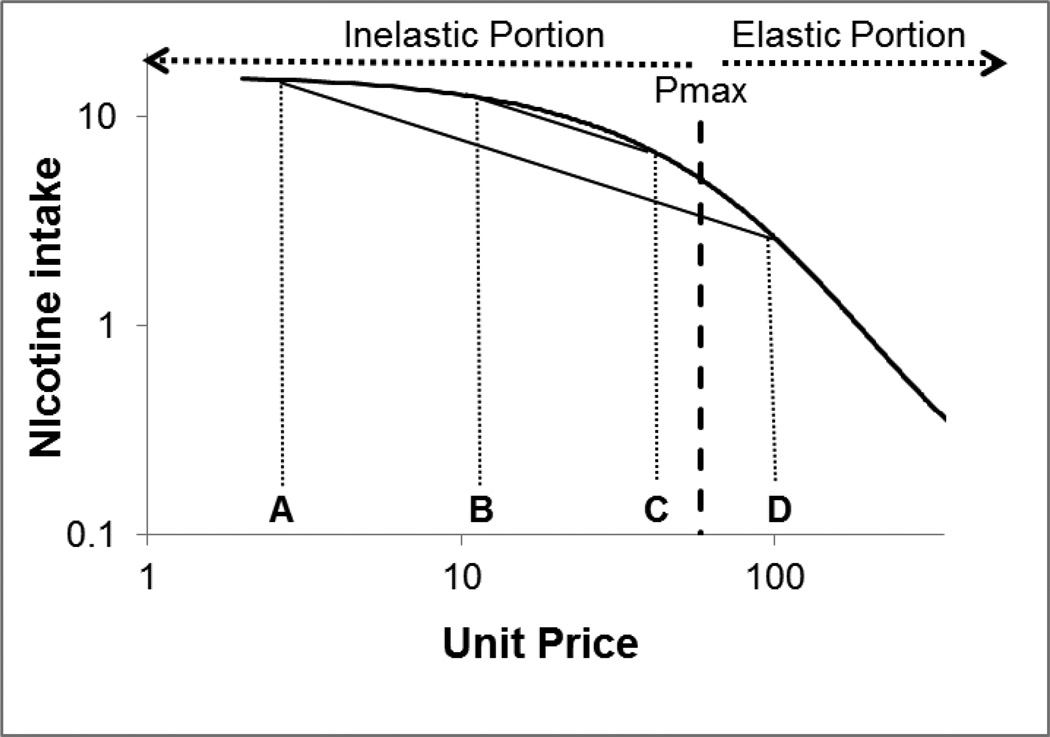
| (2) |
in which marker1 and marker2 refer to biomarkers for nicotine intake before and after nicotine reduction, respectively, and content1 and content2 refer to nicotine contents before and after nicotine reduction, respectively. The CI measure is related to demand curves because for any two points on a demand curve, the CI will correspond to the slope of a line connecting those two points on a demand curve. An example is shown in Figure 2. The CI between unit price A and unit price D would be the same as the CI between unit price B and unit price C, as the proportional change in intake as a function of change in price is the same. However, to say that behavior has been changed in the same way between each of the two sets of prices is misleading. A reduction in nicotine from unit price A to unit price D has shifted demand to the elastic portion of the demand curve, and further reductions in nicotine content will decrease smoking behavior. A reduction in nicotine from unit price B to unit price C has failed to shift demand to the elastic portion of the demand curve. Further reductions in nicotine content will result in increased smoking behavior. In fact, unit price C is nearing Pmax, the unit price that will result in the highest level of smoking behavior. Hence, although the CI is useful for summarizing compensatory change between any two points, it cannot capture the nature of the relationship or be used to predict what additional changes in content might do to behavior.
Figure 2.
Hypothetical demand curve plotting nicotine consumption as a function of unit price. If changes in nicotine consumption were calculated using the traditional compensation index (CI, see text), CI would be the same between unit prices A and D as between unit prices B and C. However, the demand curve shows that the change from unit price A to unit price D has shifted demand to the elastic portion of the curve, and further increases in unit price will reduce behavior. The change from unit price B to unit price C has shifted demand close to Pmax, where the maximal behavioral output will be observed.
A “threshold” nicotine content has been theorized to exist for maintaining nicotine reinforcement and dependence (Sofuoglu and Lesage, 2012). Recent research has indicated that a machine-measured nicotine yield of 0.05 mg per cigarette may reliably reduce smoking behavior and dependence (Benowitz et al., 2012, Donny et al., 2007, Hatsukami et al., 2010a). From a behavioral economics perspective in which people smoke solely for nicotine, the “threshold” nicotine content for reinforcement might be thought of as the unit price that will suppress intake to zero (i.e., breakpoint). However, it is important to recognize that the content that produces this unit price will depend on the cost of cigarettes; therefore, the effectiveness of any regulatory policy reducing nicotine content will likely depend on the monetary cost of cigarettes being stable (or at least not decreasing). Furthermore, there is likely to be variability in this threshold unit price across individuals depending on economic circumstances and willingness to pay for cigarettes (e.g., if more nicotine dependent; see Section 4 for discussion of interindividual variability).
The demand curve approach to modeling changes in nicotine intake predicts that the relationship between nicotine content and nicotine intake will be exponential. Once nicotine intake has been tested at several nicotine contents, a demand curve could be created and the contents that will produce maximal compensation and the threshold for maintaining smoking behavior could be estimated. As of yet, no published studies have used demand curves to model changes in nicotine intake by producing high unit prices via reductions in the nicotine content of cigarettes. Hursh and Silberberg (2008) showed that Equation 1 is very robust by testing it across a variety of data sets using different reinforcers collected for a variety of purposes, giving some confidence in estimating nicotine intake at untested prices. Of course, it is always risky to make predictions about the relationship between two variables outside of the range of testing for the independent variable, but a demand curve can provide a useful estimation.
Critical nicotine contents (e.g., that produce Omax and breakpoint) may also be predicted using changes in smoking behavior as a result of monetary increases in cost. Actual cigarette prices have not varied across a wide range that includes high unit prices on the elastic portion of the demand curve, making estimation difficult. However, a tool that might be useful for estimating the unit price that suppresses intake to zero is the Cigarette Purchase Task (CPT) (Jacobs and Bickel, 1999). The CPT asks smokers to make predictions about how many cigarettes they would smoke if cigarettes were a variety of prices, and demand curves can be created from participants’ responses. In one study, participants completed the CPT and reported a mean breakpoint of $4.88/cigarette for their usual brand under conditions of deprivation (MacKillop et al., 2012). Assuming usual brand cigarettes yield approximately 0.8 mg of nicotine, and an average pack of cigarettes in the US is $6.36 (32 cents per cigarette) (World Lung Foundation and American Cancer Society, 2012) we can estimate the threshold nicotine yield to be approximately 0.05 mg, consistent with previous research indicating this machine-measured yield reduces use and dependence. Using the same strategy, we can use the mean price at which maximum compensation was estimated, of $3.79, to predict the yield that will produce maximal compensation to be approximately 0.07 mg. Possibly more important than the precise estimates is the observation that the difference between Pmax and breakpoint may be small (given the current cost of cigarettes) and that reducing nicotine well below the estimated threshold would likely minimize the risk of compensation. Of course, using data where the unit price for cigarettes was manipulated via increasing cost assumes that increasing cost and decreasing nicotine content are functionally equivalent across a range of unit prices which, to our knowledge, has not been tested.
3. How is a nicotine reduction policy related to the consumption of other reinforcers?
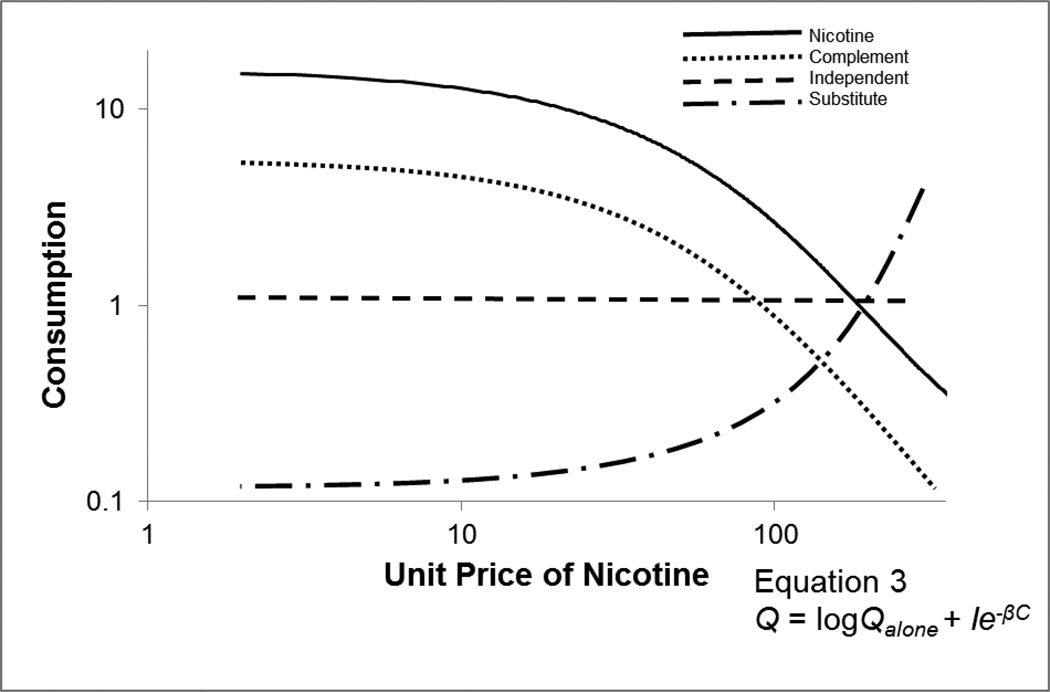
The effect of unit price of concurrently available reinforcers on consumption is termed cross-price elasticity (see Hursh & Roma, 2013 for a review). Cross-price elasticity is important for a nicotine-reduction policy because as nicotine is reduced, consumption of other reinforcers (e.g., other tobacco products, other drugs of abuse) could change. Conversely, the unit price of each of these reinforcers may affect the impact of a nicotine reduction policy. Cross-price demand curves, which plot consumption of a second, fixed-price commodity as a function of the unit price of the primary, variable-priced commodity, can be used to characterize the relationship between the unit price of nicotine and the unit price of other reinforcers. Commodities can be classified as either being substitutes, complements, or independents, depending on whether consumption of the commodity increases, decreases, or is unchanged by increasing the unit price of nicotine, respectively (see Figure 3). An extension of Equation 1 (shown in Figure 3) can be used to fit cross-price demand curves, and to characterize the nature (e.g., substitute, complement, independent) and intensity of the relationship between the two reinforcers.
Figure 3.
Hypothetical demand curve for nicotine (solid line) and cross-price demand curves for a hypothetical substitute (dots and dashes), complement (dots), and independent (dashes). Equation 3 can be used to characterize any cross-price demand curve, and is an extension of the exponential demand equation (Equation 1). Qalone is the maximum level of consumption for the fixed-price commodity when the price of the primary commodity is infinity, I is the interaction constant, β is the sensitivity of fixedprice commodity consumption to the price of the variable-priced commodity, and C is the unit price of the primary commodity. The sign of the interaction constant indicates whether the fixed-price commodity is functioning as a substitute (negative), complement (positive), or independent (a β value of 0).
To the extent that smoking is driven by nicotine, other nicotine-containing products are likely to substitute for cigarettes as the unit price of cigarettes is increased. Shifts in use from cigarettes to other tobacco products may result in reduced harm, especially if those products are non-combustible. For example, electronic nicotine delivery devices (e-cigarettes) are rising in popularity (Abrams, 2014), and these products may be especially strong substitutes because they also provide a similar behavioral experience to cigarettes. The tobacco marketplace is changing at an alarming rate, and the development of effective substitutes for cigarettes continues to increase. These changes may cause demand for cigarettes to become more elastic.
Other drugs of abuse represent another important class of reinforcers to characterize because the public health impact of a nicotine reduction policy is likely to be affected by the change in consumption of various drugs. Previous research has shown that consumption of coffee decreases as the unit price of cigarettes increases (i.e., caffeine is a complement to cigarettes (Bickel et al., 1992)). Likewise, increasing cigarette taxes decreases alcohol and marijuana consumption (Lee, 2007, Dee, 1999, Chaloupka et al., 1999, Pacula, 1998, Farrelly et al., 2001), suggesting that consumption of alcohol and marijuana may decrease following nicotine reduction.
Researchers should aim to characterize the nature and intensity of the relationship between nicotine and other reinforcers by creating cross-price demand curves. Some human laboratory studies have utilized a task in which smokers make an effortful response to receive access to either cigarettes or another product (Bickel et al., 1992, Bickel and Madden, 1999, Johnson and Bickel, 2003, Johnson et al., 2004). The unit price of cigarettes can be raised in the presence of other products, so that the interactions between the unit prices of products can be considered.
Behavioral economics research has also shown that the elasticity of one reinforcer can be shifted by the availability of other reinforcers (Hursh and Roma, 2013), suggesting that the availability and unit price of other reinforcers may affect the impact of a nicotine reduction policy. Researchers will need to test these relationships both by manipulating the unit price of nicotine and by manipulating the unit price of other reinforcers because the symmetry of cross-price elasticity cannot be assumed (Bickel et al., 1992).The availability of other nicotine delivery products, discussed above, is especially likely to affect a nicotine reduction policy, but changes in the availability or unit price of other drugs of abuse may also change the impact of a nicotine reduction policy. For example, the recent legalization of marijuana in some US states may increase cigarette smoking if the complementary relationship between marijuana and cigarettes is symmetrical. Furthermore, people smoke cigarettes under a variety of conditions, including under the influence of other drugs or medications, and these drugs may alter sensitivity to nicotine. Therefore, it is important to examine the elasticity of demand for cigarettes within the broader pharmacological context in which people smoke cigarettes.
4. Is nicotine content related to the reinforcer value of cigarettes?
A decrease in nicotine content may only be thought of as an increase in unit price if reinforcement value is closely related to nicotine content. Many theories of tobacco dependence place importance on nicotine as the primary source of value for smoking behavior, as either a positive or a negative reinforcer. In rodent self-administration experiments, rats will make more responses to earn higher doses of nicotine (Chaudhri et al., 2007, Donny et al., 1999), indicating that the value of nicotine as a primary reinforcer is related to dose of nicotine. Nicotine also increases cognitive performance, and researchers have suggested this may be a motivation for smoking (Evans and Drobes, 2009). Nicotine functions as a negative reinforcer by relieving withdrawal in dependent smokers (Baker et al., 2004), and relieving symptoms of anhedonia (Spring et al., 2008, Leventhal et al., 2009). However, the dose-response curves for the various positive and negative reinforcement functions of nicotine may be different. As nicotine content is decreased, the value of nicotine may change differently for each of these functions. This perspective emphasizes the need to understand whether even low nicotine content cigarettes maintain important functions that could reinforce behavior, especially in some individuals (e.g., depressed, cognitively impaired, etc…).
Furthermore, reinforcement value for the various functions of nicotine is almost surely not constant within an individual. Following the implementation of a nicotine reduction policy, physical dependence is likely to decrease, suggesting that value derived from withdrawal suppression will decrease. Additionally, the value of nicotine may not be constant within a single day. The first cigarette of the day may function to relieve withdrawal and/or have a more potent stimulating effect (e.g., due to overnight recovery from tachyphylaxis), providing more value to the first cigarette than other cigarettes. Likewise, the cognitive enhancement function of nicotine or the relief of anhedonia may be more relevant in certain contexts than others. The behavioral economics framework summarizes changes in nicotine consumption over longer periods of time, so variations in value throughout the day are averaged on a demand curve which could lead to inaccurate predictions if some effects become more or less important determinants of use when nicotine is reduced. However, behavioral economics has been used for a wide variety of reinforcers, including food, which likely also changes in value at various time-points since the last meal.
Smokers also obtain value from smoking other than from nicotine. Very low nicotine content cigarettes will substitute for nicotine containing cigarettes, at least in the short term (Donny and Jones, 2009, Johnson and Bickel, 2003, Johnson et al., 2004), and have actually been shown to function as a better substitute for nicotine-containing cigarettes than nicotine gum (Johnson et al., 2004), indicating that sources other than nicotine are important in maintaining smoking behavior. If the reinforcement value attributable to sources besides nicotine is constant across nicotine contents, contexts, and time, this additional value would just be added into the equation for unit price:
| (4) |
Any additional value not attributable to nicotine will reduce the unit price, translating to elevated consumption, and increased smoke exposure. As nicotine is reduced, the proportion of reinforcement value not attributable to nicotine will increase, making the increase in unit price smaller than estimated if all value were attributable to nicotine. Once nicotine content approaches zero, the residual value will be the sum of all value not attributable to nicotine.
Reinforcement value for smoking that is not attributable to nicotine may come from a variety of sources. A large portion of the value of cigarettes not attributable to nicotine is likely a result of conditioning. Cues reinstate drug seeking better than nicotine itself (LeSage et al., 2004), and promote relapse in abstinent smokers (Shiffman et al., 1996). Another theory of dependence argues that smoking may have become an automated behavior in dependent smokers, suggesting that behavior would be insensitive to a change in value (Tiffany, 1990). A long term effect of automaticity seems unlikely given that some research has already shown that low enough contents of nicotine will decrease smoking behavior (Hatsukami et al., 2010a, Donny et al., 2007). Additionally, although poorly understood (Hoffman and Evans, 2013), non-nicotine cigarette smoke constituents may have reinforcing value on their own or may interact with the reinforcing potential of nicotine (Bardo et al., 1999, Belluzzi et al., 2005, Clemens et al., 2009, Guillem et al., 2005, Villegier et al., 2007). Importantly, the FDA has the authority to regulate the content of any cigarette constituent (US Congress, 2009), allowing for the regulation of these reinforcing constituents if they also contribute to value.
Reinforcement value attributable to environmental stimuli is likely to change over time following the implementation of a nicotine reduction policy as cues are paired with very small amounts of nicotine, which theoretically will produce extinction. However, the timeline for extinction is unknown and may depend on many factors such as the strength of training for each cue. Additionally, the extinction of cues may be context dependent (Bouton et al., 2006, Wing and Shoaib, 2008). If the total reinforcement value not attributable to nicotine is context dependent, unit price, and the rate of smoking and nicotine consumption, will also be context dependent.
The reinforcement value of cigarettes is likely to vary across individuals, making it an important research area. Still, it is important to acknowledge that while a nicotine reduction policy may improve public health, it may not improve the health of all individuals. Some individual factors that might be critical include sex, metabolic rate, pharmacological history, racial/ethnic group, genetics, age, SES, geographical location, and psychiatric comorbidities (Hatsukami et al., 2010b). Several large studies are currently underway to examine a substantial nicotine reduction in populations that might be at risk including those with mood disorders, drug abusers, and women of childbearing age. The CPT may be a cost-effective and efficient method for assessing sensitivity to increases in unit price. However, if a large portion of reinforcement value for smoking is not attributable to nicotine, the CPT would not provide an adequate prediction of response to nicotine reduction.
Relatedly, the precise motives for smoking may vary between subpopulations of individuals. Some evidence suggests that a higher proportion of the value of a cigarette may be attributed to nicotine for males than for females (Perkins, 2009), indicating that women will be less sensitive to decreases in content. Another line of research suggests that although all individuals learn about cues in their environment, the degree to which those cues become “wanted” may be a trait to the individual (Flagel et al., 2009). For these individuals, a high proportion of reinforcement value for smoking is attributable to environmental cues paired with smoking.
5. Conclusions
An FDA policy reducing the nicotine content in cigarettes may dramatically improve public health. A behavioral economics framework provides several tools for researchers interested in a nicotine reduction policy. Demand curves and cross-price demand curves can be used to characterize changes in consumption of these reinforcers as a function of unit price. Research in which the unit price of cigarettes is manipulated through increases in cost may be useful for making predictions regarding nicotine reduction. Therefore, the CPT and data collected from increases in cigarette taxation may be important resources for individuals interested in nicotine reduction.
Nicotine consumption is likely to be related to unit price through an exponential function, meaning that smokers will compensate for decreases in nicotine content across a range of contents, reach a peak level of compensation, and further reductions in nicotine will reduce smoking behavior. Demand curves can be used to make predictions regarding the exact range of contents that will produce compensation, and the content that is likely to suppress nicotine consumption to zero.
Cross-price demand curves can be used to characterize the relationship between nicotine reduction and use of other products (including nicotine replacement therapy, and other drugs of abuse). These demand curves could be created from rodent self-administration paradigms, human laboratory studies, or data from cigarette taxation. Other tobacco products are likely to be imperfect substitutes for cigarettes, meaning their consumption is likely to increase as nicotine is reduced. The availability of other reinforcers, as well as the pharmacological context in which people smoke, is likely to affect a nicotine reduction policy.
A regulatory policy decreasing the nicotine content of cigarettes hinges on the idea that the primary motive for smoking is nicotine. A behavioral economics approach also assumes the nicotine content of cigarettes is related to the reinforcement value for smoking. There is already a great deal of evidence that nicotine is related to reinforcement value (US Department of Health and Human Services, 1988, US Department of Health and Human Services, 2014). However, there is likely variability in the degree to which individuals are influenced by changes in nicotine content, and it is important to identify individuals for whom nicotine is not the primary reinforcer. Nicotine may be related to reinforcement value only within a range of contents, and it is within this range of contents that behavioral economics will have the most utility.
The present paper has highlighted several important nicotine reduction research questions and described how the behavioral economic framework could be used to address them. This paper is not meant to be an exhaustive review of all behavioral economic applications to nicotine reduction. There are likely many other research questions for which this perspective could be useful. For example Hursh and Roma (14) have discussed how behavioral economics could be used to understand an illicit drug market. If a nicotine reduction policy is implemented, a black market for nicotine-containing cigarettes is likely to be a concern. Researchers interested in nicotine reduction can benefit from using a behavioral economics framework to think about these types of questions, design their experiments, and analyze their data.
Highlights.
Behavioral economics could be used by nicotine reduction researchers.
Smoking may increase at some nicotine contents and decrease at lower contents.
Behavioral economics could characterize changes in use of other reinforcers.
A behavioral economics approach assumes people smoke to obtain nicotine.
Acknowledgments
The authors would like to thank committee members Dr. Michael Sayette and Dr. Saul Shiffman for their comments on that version.
Funding
This publication was supported by the National Institute on Drug Abuse and FDA Center for Tobacco Products (CTP) (U54 DA031659 awarded to E.C.D.). The funding source had no other role other than financial support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
A previous draft of this manuscript served as a specialty paper presented by the first author in partial fulfillment of a doctoral degree.
Conflict of Interest
Dr. Hatsukami was funded by Nabi Biopharmaceuticals and NIDA to be a site for a nicotine immunotherapy trial. Tracy Smith, Dr. Sved, and Dr. Donny have no conflicts to report.
Contributor Information
Tracy T. Smith, Department of Psychology, University of Pittsburgh
Alan F. Sved, Departments of Neuroscience and Psychology, University of Pittsburgh
Dorothy K. Hatsukami, Department of Psychiatry, University of Minnesota
Eric C. Donny, Department of Psychology, University of Pittsburgh
Bibliographic References
- Abrams DB. Promise and peril of e-cigarettes: can disruptive technology make cigarettes obsolete? JAMA. 2014;311:135–136. doi: 10.1001/jama.2013.285347. [DOI] [PubMed] [Google Scholar]
- Baker TB, Brandon TH, Chassin L. Motivational influences on cigarette smoking. Annu Rev Psychol. 2004;55:463–491. doi: 10.1146/annurev.psych.55.090902.142054. [DOI] [PubMed] [Google Scholar]
- Bardo MT, Green TA, Crooks PA, Dwoskin LP. Nornicotine is self-administered intravenously by rats. Psychopharmacology (Berl) 1999;146:290–296. doi: 10.1007/s002130051119. [DOI] [PubMed] [Google Scholar]
- Belluzzi JD, Wang R, Leslie FM. Acetaldehyde enhances acquisition of nicotine self-administration in adolescent rats. Neuropsychopharmacology. 2005;30:705–712. doi: 10.1038/sj.npp.1300586. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Dains KM, Hall SM, Stewart S, Wilson M, Dempsey D, Jacob p., 3RD Smoking behavior and exposure to tobacco toxicants during 6 months of smoking progressively reduced nicotine content cigarettes. Cancer Epidemiol Biomarkers Prev. 2012;21:761–769. doi: 10.1158/1055-9965.EPI-11-0644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL, Hall SM, Stewart S, Wilson M, Dempsey D, Jacob p., 3RD Nicotine and carcinogen exposure with smoking of progressively reduced nicotine content cigarette. Cancer Epidemiol Biomarkers Prev. 2007;16:2479–2485. doi: 10.1158/1055-9965.EPI-07-0393. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Henningfield JE. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N Engl J Med. 1994;331:123–125. doi: 10.1056/NEJM199407143310212. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Henningfield JE. Reducing the nicotine content to make cigarettes less addictive. Tob Control. 2013;22(Suppl 1):i14–i17. doi: 10.1136/tobaccocontrol-2012-050860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL, Jacob p, 3RD, Bernert JT, Wilson M, Wang L, Allen F, Dempsey D. Carcinogen exposure during short-term switching from regular to "light" cigarettes. Cancer Epidemiol Biomarkers Prev. 2005;14:1376–1383. doi: 10.1158/1055-9965.EPI-04-0667. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Degrandpre RJ, Higgins ST, Hughes JR. Behavioral economics of drug self-administration. I. Functional equivalence of response requirement and drug dose. Life Sci. 1990;47:1501–1510. doi: 10.1016/0024-3205(90)90178-t. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Degrandpre RJ, Hughes JR, Higgins ST. Behavioral economics of drug self-administration. II. A unit-price analysis of cigarette smoking. J Exp Anal Behav. 1991;55:145–154. doi: 10.1901/jeab.1991.55-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Hughes JR, Degrandpre RJ, Higgins ST, Rizzuto P. Behavioral economics of drug self-administration. IV. The effects of response requirement on the consumption of and interaction between concurrently available coffee and cigarettes. Psychopharmacology (Berl) 1992;107:211–216. doi: 10.1007/BF02245139. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Madden GJ. A comparison of measures of relative reinforcing efficacy and behavioral economics: cigarettes and money in smokers. Behav Pharmacol. 1999;10:627–637. doi: 10.1097/00008877-199911000-00009. [DOI] [PubMed] [Google Scholar]
- Bouton ME, Garcia-gutierrez A, Zilski J, Moody EW. Extinction in multiple contexts does not necessarily make extinction less vulnerable to relapse. Behav Res Ther. 2006;44:983–994. doi: 10.1016/j.brat.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Chaloupka F, Warner KE. The economics of smoking. NBER Working Paper No. 7047. 1999 [Google Scholar]
- Chaloupka FJ. How effective are taxes in Reducing Tobacco Consumption? [Google Scholar]
- Chaloupka FJ, Pacula RL, Farrelly MC, Johnston LD, O'malley PM, Bray JW. Do higher cigarette prices encourage youth to use marijuana? NBER Working Paper No. 6939. 1999 [Google Scholar]
- Chaudhri N, Caggiula AR, Donny EC, Booth S, Gharib M, Craven L, Palmatier MI, Liu X, Sved AF. Self-administered and noncontingent nicotine enhance reinforced operant responding in rats: impact of nicotine dose and reinforcement schedule. Psychopharmacology (Berl) 2007;190:353–362. doi: 10.1007/s00213-006-0454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemens KJ, Caille S, Stinus L, Cador M. The addition of five minor tobacco alkaloids increases nicotine-induced hyperactivity, sensitization and intravenous self-administration in rats. Int J Neuropsychopharmacol. 2009;12:1355–1366. doi: 10.1017/S1461145709000273. [DOI] [PubMed] [Google Scholar]
- Conklin CA, Tiffany ST. Applying extinction research and theory to cue-exposure addiction treatments. Addiction. 2002;97:155–167. doi: 10.1046/j.1360-0443.2002.00014.x. [DOI] [PubMed] [Google Scholar]
- Dee TS. The complementarity of teen smoking and drinking. J Health Econ. 1999;18:769–793. doi: 10.1016/s0167-6296(99)00018-1. [DOI] [PubMed] [Google Scholar]
- Degrandpre RJ, Bickel WK, Hughes JR, Higgins ST. Behavioral economics of drug self-administration. III. A reanalysis of the nicotine regulation hypothesis. Psychopharmacology (Berl) 1992;108:1–10. doi: 10.1007/BF02245277. [DOI] [PubMed] [Google Scholar]
- Donny EC, Caggiula AR, Mielke MM, Booth S, Gharib MA, Hoffman A, Maldovan V, Shupenko C, Mccallum SE. Nicotine self-administration in rats on a progressive ratio schedule of reinforcement. Psychopharmacology (Berl) 1999;147:135–142. doi: 10.1007/s002130051153. [DOI] [PubMed] [Google Scholar]
- Donny EC, Houtsmuller E, Stitzer ML. Smoking in the absence of nicotine: behavioral, subjective and physiological effects over 11 days. Addiction. 2007;102:324–334. doi: 10.1111/j.1360-0443.2006.01670.x. [DOI] [PubMed] [Google Scholar]
- Donny EC, Jones M. Prolonged exposure to denicotinized cigarettes with or without transdermal nicotine. Drug Alcohol Depend. 2009;104:23–33. doi: 10.1016/j.drugalcdep.2009.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donny EC, Taylor TG, Lesage MG, Levin M, Buffalari DM, Joel D, Sved AF. Impact of Tobacco Regulation on Animal Research: New Perspectives and Opportunities. Nicotine Tob Res. 2012 doi: 10.1093/ntr/nts162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DE, Drobes DJ. Nicotine self-medication of cognitive-attentional processing. Addict Biol. 2009;14:32–42. doi: 10.1111/j.1369-1600.2008.00130.x. [DOI] [PubMed] [Google Scholar]
- Farrelly MC, Bray JW, Zarkin GA, Wendling BW. The joint demand for cigarettes and marijuana: evidence from the National Household Surveys on Drug Abuse. J Health Econ. 2001;20:51–68. doi: 10.1016/s0167-6296(00)00067-9. [DOI] [PubMed] [Google Scholar]
- Flagel SB, Akil H, Robinson TE. Individual differences in the attribution of incentive salience to reward-related cues: Implications for addiction. Neuropharmacology. 2009;56(Suppl 1):139–148. doi: 10.1016/j.neuropharm.2008.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grebenstein P, Burroughs D, Zhang Y, Lesage MG. Sex differences in nicotine self-administration in rats during progressive unit dose reduction: implications for nicotine regulation policy. Pharmacol Biochem Behav. 2013:114–115. 70–81. doi: 10.1016/j.pbb.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillem K, Vouillac C, Azar MR, Parsons LH, Koob GF, Cador M, Stinus L. Monoamine oxidase inhibition dramatically increases the motivation to self-administer nicotine in rats. J Neurosci. 2005;25:8593–8600. doi: 10.1523/JNEUROSCI.2139-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AC, Pentel PR, Burroughs D, Staley MD, Lesage MG. A lack of association between severity of nicotine withdrawal and individual differences in compensatory nicotine self-administration in rats. Psychopharmacology (Berl) 2011;217:153–166. doi: 10.1007/s00213-011-2273-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami DK, Kotlyar M, Hertsgaard LA, Zhang Y, Carmella SG, Jensen JA, Allen SS, Shields PG, Murphy SE, Stepanov I, Hecht SS. Reduced nicotine content cigarettes: effects on toxicant exposure, dependence and cessation. Addiction. 2010a;105:343–355. doi: 10.1111/j.1360-0443.2009.02780.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami DK, Perkins KA, Lesage MG, Ashley DL, Henningfield JE, Benowitz NL, Backinger CL, Zeller M. Nicotine reduction revisited: science and future directions. Tob Control. 2010b;19:e1–e10. doi: 10.1136/tc.2009.035584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman AC, Evans SE. Abuse potential of non-nicotine tobacco smoke components: acetaldehyde, nornicotine, cotinine, and anabasine. Nicotine Tob Res. 2013;15:622–632. doi: 10.1093/ntr/nts192. [DOI] [PubMed] [Google Scholar]
- Hoffmann D, Hoffmann I. The changing cigarette: Chemical studies and bioassays. In: Institute NC, editor. Risks associated with smoking cigarettes with low machine-measured yields of tar and nicotine. 13 ed. Bethesda, MD: USDHHS, NIH, NCI; 2001. [Google Scholar]
- Hursh SR, Roma PG. Behavioral economics and empirical public policy. J Exp Anal Behav. 2013;99:98–124. doi: 10.1002/jeab.7. [DOI] [PubMed] [Google Scholar]
- Hursh SR, Silberberg A. Economic demand and essential value. Psychol Rev. 2008;115:186–198. doi: 10.1037/0033-295X.115.1.186. [DOI] [PubMed] [Google Scholar]
- Jacobs EA, Bickel WK. Modeling drug consumption in the clinical via simulation procedures: Demand for heroin and cigarettes in opiod-dependent outpatients. Experimental and Clinical Psychopharmacology. 1999;7:412–426. doi: 10.1037//1064-1297.7.4.412. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. The behavioral economics of cigarette smoking: The concurrent presence of a substitute and an independent reinforcer. Behav Pharmacol. 2003;14:137–144. doi: 10.1097/00008877-200303000-00005. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK, Kirshenbaum AP. Substitutes for tobacco smoking: a behavioral economic analysis of nicotine gum, Denicotinized cigarettes, and nicotine-containing cigarettes. Drug Alcohol Depend. 2004;74:253–264. doi: 10.1016/j.drugalcdep.2003.12.012. [DOI] [PubMed] [Google Scholar]
- Lee JM. The synergistic effect of cigarette taxes on the consumption of cigarettes, alcohol and betel nuts. BMC Public Health. 2007;7:121. doi: 10.1186/1471-2458-7-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesage MG, Burroughs D, Dufek M, Keyler DE, Pentel PR. Reinstatement of nicotine self-administration in rats by presentation of nicotine-paired stimuli, but not nicotine priming. Pharmacol Biochem Behav. 2004;79:507–513. doi: 10.1016/j.pbb.2004.09.002. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Waters AJ, Kahler CW, Ray LA, Sussman S. Relations between anhedonia and smoking motivation. Nicotine Tob Res. 2009;11:1047–1054. doi: 10.1093/ntr/ntp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackillop J, Brown CL, Stojek MK, Murphy CM, Sweet L, Niaura RS. Behavioral economic analysis of withdrawal- and cue-elicited craving for tobacco: an initial investigation. Nicotine Tob Res. 2012;14:1426–1434. doi: 10.1093/ntr/nts006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markou A, Paterson NE. Multiple motivational forces contribute to nicotine dependence. In: Bevins RA, Caggiula AR, editors. Nebraska Symposium on Motivation: The Motivational Impact of Nicotine and its Role in Tobacco Use. New York, NY: Springer Science + Business Media; 2009. [DOI] [PubMed] [Google Scholar]
- Pacula RL. Does increasing the beer tax reduce marijuana consumption? J Health Econ. 1998;17:557–585. doi: 10.1016/s0167-6296(97)00039-8. [DOI] [PubMed] [Google Scholar]
- Perkins KA. Sex differences in nicotine reinforcement and reward: influences on the persistence of tobacco smoking. Nebr Symp Motiv. 2009;55:143–169. doi: 10.1007/978-0-387-78748-0_9. [DOI] [PubMed] [Google Scholar]
- Reduced nicotine cigarettes in smokers with mood and anxiety disorders. ClinicalTrials.gov Identifier: NCT01928758. http://clinicaltrials.gov/ct2/show/NCT01928758.
- Scherer G. Smoking behaviour and compensation: a review of the literature. Psychopharmacology (Berl) 1999;145:1–20. doi: 10.1007/s002130051027. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: within-subjects analysis of real-time reports. J Consult Clin Psychol. 1996;64:366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- Sofuoglu M, Lesage MG. The reinforcement threshold for nicotine as a target for tobacco control. Drug Alcohol Depend. 2012;125:1–7. doi: 10.1016/j.drugalcdep.2012.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spring B, Cook JW, Appelhans B, Maloney A, Richmond M, Vaughn J, Vanderveen J, Hedeker D. Nicotine effects on affective response in depression-prone smokers. Psychopharmacology (Berl) 2008;196:461–471. doi: 10.1007/s00213-007-0977-7. [DOI] [PubMed] [Google Scholar]
- Stephen A, Frost C, Thompson S, Wald N. Estimating the extent of compensatory smoking. In: Wald N, Fruggatt P, editors. Nicotine, smoking, and the low tar programme. London: Oxford Medical Publishing; 1989. [Google Scholar]
- Stolerman IP, Jarvis MJ. The scientific case that nicotine is addictive. Psychopharmacology (Berl) 1995;117:2–10. doi: 10.1007/BF02245088. Discussion 14–20. [DOI] [PubMed] [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- US congress. Family smoking prevention and tobacco control act. 2009 [Google Scholar]
- US Department of Health and Human Services. Office of the surgeon general dhhs publication No. (CDC): 88-8406.0 The health consequences of smoking: nicotine addiction: a report of the surgeon general. Center for Health Promotion and Education. Office on Smoking and Health United States. Public Health Service. 1988 [Google Scholar]
- US Department of Health and Human services. The Health Consequences of Smoking--50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: US department of health and human services, centeres for disease control and prevention, national center for chronic disease prevention and health promotion, office on smoking and health; 2014. [Google Scholar]
- Vermont Center on Tobacco Regulatory Science. Grant Number: P50-DA-036114-01 [Google Scholar]
- Villegier AS, Lotfipour S, Mcquown SC, Belluzzi JD, Leslie FM. Tranylcypromine enhancement of nicotine self-administration. Neuropharmacology. 2007;52:1415–1425. doi: 10.1016/j.neuropharm.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Wing VC, Shoaib M. Contextual stimuli modulate extinction and reinstatement in rodents self-administering intravenous nicotine. Psychopharmacology (Berl) 2008;200:357–365. doi: 10.1007/s00213-008-1211-y. [DOI] [PubMed] [Google Scholar]
- World Lung Foundation and American Cancer Society. The Tobacco Atlas. Fourth Edition. Atlanta, GA: Bookhouse group, inc.; 2012. [Google Scholar]