Abstract
Background
Commercial or proprietary weight loss programs are popular obesity treatment options; however, their efficacy is unclear.
Purpose
To compare weight loss, adherence, and harms of commercial or proprietary weight loss programs to control/education or behavioral counseling among adults with overweight and obesity.
Data sources
MEDLINE and Cochrane Database of Systematic Reviews from inception to November 2014; references identified by programs
Study selection
Randomized controlled trials (RCT) of ≥12 weeks duration; prospective case series ≥12 months (harms only)
Data extraction
Two reviewers extracted information on study design, population characteristics, interventions, and mean % weight change, and assessed risk of bias.
Data synthesis
We included 39 RCTs. At 12 months, Weight Watchers’ participants achieved at least 2.6% greater weight loss than control/education. Jenny Craig resulted in at least 4.9% greater weight loss at 12 months as compared to both control/education and counseling. Nutrisystem participants achieved at least 3.8% greater weight loss at 3 months than control/education or counseling. Very-low-calorie programs (HMR, Medifast, Optifast) resulted in at least 4.0% greater short-term weight loss than counseling, but some attenuation of effect occurred beyond 6 months when reported. Atkins achieved 0.1–2.9% greater weight loss at 12 months than counseling. Results for SlimFast were mixed. We found limited evidence to evaluate adherence or harms for all programs and weight outcomes for other commercial programs.
Limitations
Many trials had short durations (<12 months), high attrition, and lacked blinding.
Conclusions
Clinicians could consider referring patients with overweight or obesity to Weight Watchers or Jenny Craig. Other popular programs such as NutriSystem show promising weight loss results; however, additional studies evaluating long-term outcomes are needed.
Primary funding source
None. Registered with PROSPERO (CRD42014007155).
Keywords: Weight reduction programs, commerce, obesity
Introduction
Two-thirds of U.S. adults are overweight or obese (1), and excess body weight increases the risk of hypertension and type 2 diabetes mellitus (2). Yet, losing weight can prevent the development or lead to improved control of these chronic conditions (3–4). Most Americans (63%) have seriously attempted to lose weight at some point in their lives, and 29% report currently trying to lose weight (5). In 2014, Americans were expected to spend $2.5 billion on commercial or proprietary weight loss services with Weight Watchers (45%), NutriSystem (14%), and Jenny Craig (13%) dominating the market share (6). Overall, weight loss services’ revenues were expected to increase by 3.2% in 2014 and continue to grow in coming years (6), as the industry anticipates increased referrals from clinicians given the provisions covering obesity screening in the 2010 Affordable Care Act (ACA).
Once fully implemented, the ACA will likely cover 25 million uninsured Americans through the exchanges – organizations that facilitate health insurance purchases – and Medicaid expansion (7). Americans who obtain health insurance through the exchanges receive coverage for all preventive services receiving grade A or B recommendations from the United States Preventive Services Task Forces (USPSTF)(8), including obesity screening and counseling. Using federal matching funds, the ACA also provides new incentives for states to cover all recommended USPSTF services for Medicaid beneficiaries, which previously had variable coverage of obesity services across states (9–10). The USPSTF-recommended obesity counseling interventions are high intensity and comprehensive – incorporating nutrition, physical activity, self-monitoring, goal setting, and group or individual sessions (11). While some commercial or proprietary weight loss programs also offer comprehensive programs of high intensity, insurance coverage for these programs varies by state or health insurance type. Some state Medicaid programs have piloted programs providing Weight Watchers for their beneficiaries (12–13).
A 2005 systematic review of commercial and proprietary weight loss programs’ efficacy concluded that Weight Watchers was the only program with demonstrated efficacy in achieving modest weight loss based on results from 3 randomized controlled trials (RCTs), one of which included only breast cancer survivors (14). Scant evidence existed for all other commercial weight loss programs. Since then, additional RCTs have been published examining a variety of weight loss programs. An updated review incorporating this new evidence may aid clinicians in determining the efficacy of commercial or proprietary weight loss programs. Our objective was to examine the weight loss benefits, adherence, and harms of commercial or proprietary weight loss programs as compared to control/education or behavioral counseling among individuals with overweight and obesity.
Methods
Identification and Selection of Weight Loss Programs
We generated a list of 141 commercial and proprietary weight loss programs through several sources: obesity experts, U.S. News and World Report rankings, and Internet searches (Google, Bing)(Supplemental Table 1). Using information provided on the programs’ websites, we characterized each program with respect to weight loss focus, dietary change, meal replacements, physical activity, behavioral/social support (e.g., coaching, online forum), delivery location (e.g., residential, online), medication/supplement use, and availability in the U.S. (information available from authors upon request).
We included programs that emphasized nutrition (dietary change and/or meal replacements) and behavioral counseling/social support components with or without physical activity, as dietary change and support are essential components in effective weight loss programs (15). We excluded programs that 1) did not focus on weight loss (e.g., wellness, food addiction), 2) promoted medications/supplements, 3) were not currently available across the U.S., or 4) were residential programs. Thirty-two commercial or proprietary weight loss programs met our criteria.
Protocol and Registration
We updated a 2005 systematic review (14). We developed a study protocol prior to data collection, which was registered and made publicly available online by the PROSPERO International prospective register of systematic reviews (CRD42014007155; http://www.crd.york.ac.uk/prospero/).
Data Sources and Search Strategy
We used three data sources to identify citations: MEDLINE, Cochrane Database of Systematic Reviews (CDSR), and the commercial or proprietary weight loss programs themselves.
We used the same strategy as the prior review (14) to search MEDLINE for articles published from October 2002 through November 2014, which allowed the recommended one-year overlap with the prior review (16). We screened all articles included in the prior review, which searched MEDLINE from inception through October 2003 (14). We also searched MEDLINE from inception through November 2014 combining the name of each included weight loss program with the terms weight loss and commercial or proprietary. We searched CDSR from inception to November 2014 using a similar search strategy as our MEDLINE search. Terms used in the MEDLINE and CDSR searches are listed in Supplemental Table 2. We reviewed the reference lists of each included article, relevant review articles, and related systematic reviews to cull additional citations for screening. Finally, we contacted all included weight loss programs to request bibliographies of published studies using their program and any unpublished trial results. We received responses from 11 of the 32 programs. In November 2014, we also reviewed each included weight loss program’s website and culled any scientific articles listed for screening.
Study Selection
Two study team members independently reviewed and screened articles against pre-specified inclusion and exclusion criteria (Supplemental Table 3). We included RCTs among overweight or obese adults that compared a commercial or propriety weight loss program to control/education or behavioral counseling. We defined the comparator as “control/education” if participants received no intervention, only printed materials, health education curriculum, or engaged in less than 3 sessions with a provider during the study period and as “behavioral counseling” if participants had 3 or more consultations with a provider. We included RCTs of 12 weeks duration or greater. We also assessed adverse events in prospective case series studies and RCTs without a relevant comparator arm that were at least 12 months in duration.
Data Extraction and Risk of Bias Assessment
Two team members serially extracted data on study design, setting, population characteristics, and intervention characteristics. Our primary weight outcome was mean percent weight change. Our secondary weight outcome was percent achieving a clinically significant weight loss of ≥5%. We considered long-term outcomes as ≥12 months. Investigator-defined outcomes included program adherence/engagement, serious adverse events, and attrition. Other adverse events included program withdrawal due to adverse events, biliary disorders, joint pain, alopecia, constipation, and eating disorders.
Two reviewers independently assessed the risk of bias for each included study using the Cochrane Collaboration’s tool (17). We designated a trial’s overall risk of bias (ROB) at a time point as “low” if the following were all low: selection bias based on inadequate generation of a randomized sequence, detection bias based on lack of outcome assessor blinding, and attrition bias. We designated the trial’s ROB as “high,” if any domain was high. If all domains were unclear, we labeled the trial as “unclear.” ROB was otherwise “moderate.” We characterized the ROB for each program’s body of evidence by examining the overall ROB for relevant trials. For each program, we rated the ROB across trials as “low,” if most studies were low; as “high,” if most trials were high; and otherwise as “moderate.”
Data Synthesis and Analysis
For all comparisons, we report the qualitative synthesis of data by calculating and displaying the between group mean differences with 95% CIs (if calculable) for individual RCTs grouped by comparison. We denote analysis type (intention-to-treat (ITT) or completers’) for each result reported. We did not perform meta-analyses given the trials’ heterogeneous study populations, varying analysis types, and failure to report variance estimates for difference-in-differences.
Results
Of the 4,212 citations evaluated, we included 45 trials reported in 62 articles (Supplemental Figure 1) that represent 11 programs out of the 32 eligible. Table 1 characterizes the components and costs of each program with an eligible study. Overall, participants’ mean age ranged from 37 to 57 years and the majority was female in most trials. Race varied across trials (Table 2). Most studies occurred in an urban setting and many received financial support from the commercial program that they were investigating. Supplemental Table 4 provides details on study and population characteristics and ROB ratings for each individual trial. Data on our secondary outcome of percent achieving ≥5% loss is displayed in Supplemental Figure 2.
Table 1.
Components and Costs of Included Commercial or Proprietary Weight Loss Programs with Eligible Randomized Controlled Trials
| Program | Intensity* | Nutrition | Physical Activity | Behavioral Strategies | Support | Monthly Costs† | USPSTF Criteria‡ |
|---|---|---|---|---|---|---|---|
| Weight Watchers | High | Low-calorie conventional foods s Points tracking |
Activity tracking | Self-monitoring | Group sessions Online coaching s Online community forum |
$43§ | Yes |
| Jenny Craig | High | Low-calorie meal replacements | Encourages increased activity | Goal setting s Self-monitoring |
One-on-one counseling | $570§ | Yes |
| Nutrisystem | High | Low-calorie meal replacements | Exercise plans | Self-monitoring | One-on-one counseling s Online community forum |
$280 | Yes |
| HMR | High | Very-low-calorie or low-calorie meal replacements | Encourages increased activity | Goal setting | Group sessions s Telephone coaching s Medically supervised |
$682 | Yes |
| Medifast | High | Very-low-calorie or low-calorie meal replacements | Encourages increased activity | Self-monitoring | One-on-one counseling s Online coaching |
$424 | Yes |
| Optifast | High | Very-low-calorie or low-calorie meal replacements | Encourages increased activity | Problem-solving | One-on-one counseling s Group support s Medically supervised |
$665§ | Yes |
| Atkins | Self-directed | Low-carbohydrate conventional foods or meal replacements | Encourages increased activity | Self-monitoring | Online community forum | $10 for book | No |
| Biggest Loser Club | Self-directed | Low-calorie meal plans | Exercise plans | Self-monitoring | Online community forum | $20 | No |
| eDiets | Self-directed | Low-calorie meal plans | Activity tracking | -- | Online nutrition support s Online community forum |
$10 | No |
| Lose It! | Self-directed | Calorie tracking | Activity tracking | Self-monitoring | Online community forum | Free | No |
| SlimFast | Self-directed | Low-calorie meal replacements | -- | Self-weighing | Online nutrition support s Coaching text messages |
$70 | No |
Information presented in this table was abstracted from program websites available December 2014 and from materials provided by some programs.
High intensity programs recommend more than 12 sessions per year; Low intensity programs recommend less than 12 sessions per year or are self-directed.
Costs data obtained from prices listed on program websites and/or prices quoted during telephone contact with program centers. Monthly costs may be estimated based on daily or weekly rates. Costs are rounded to the nearest dollar. Actual costs to patients may vary.
Assessment of whether program may potentially meet USPSTF criteria for intensive behavioral counseling for obesity; however, this assessment does not reflect actual coverage of these programs under these guidelines.
Some health insurance companies or employers offer discounts for this program. Program may also be eligible to use Flexible Spending Account, Health Reimbursement Account, or Health Savings Account to cover costs. Abbreviations: HMR – Health Management Resources.
Table 2.
Population Characteristics and Risk of Bias among Included Randomized Controlled Trials, by Program and Comparator
| Commercial Program | Comparator | RCTs, n (N eligible) | RCTs Urban* Location, n | Overall Baseline Population Characteristics | Risk of Bias† | RCTs with Commercial Program Support, n | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Range Study Duration, months | Range Mean Age, years | Range Women, % | Range White Patients, % | Range Black Patients, % | Range Mean BMI, kg/m2 | ||||||
| Market Leaders | |||||||||||
|
| |||||||||||
| Weight Watchers | Control/education | 6 (1,850) | 2‡ | 3–24 | 36–51 | 72–100 | 74–89‡ | 4–13‡ | 31–34‡ | High | 4 |
| Counseling | 2 (265) | 2 | 11–12 | 49–51 | 67–90 | 27–90 | 5–6† | 33–36 | Moderate | 1 | |
|
| |||||||||||
| Jenny Craig | Control/education | 1 (70) | 1 | 12 | 40–42 | 100 | 57 | 3–17 | 34 | Moderate | 1 |
| Counseling | 2 (669) | 2 | 12–24 | 44–57 | 47–100 | 68–82 | 3–11 | 34–36 | High | 2 | |
|
| |||||||||||
| NutriSystem | Control/education | 1 (69) | 1 | 3 | 52–53 | 68–74 | 37–44 | 44–60 | 39 | Moderate | 1 |
| Counseling | 2 (127) | 1 | 3–6 | 54–56 | 58–100 | 32–40‡ | 54–64‡ | 33–36 | High | 2 | |
|
| |||||||||||
| Very-Low-Calorie or Low-Calorie Meal Replacement Programs | |||||||||||
|
| |||||||||||
| HMR | Control/education | 3 (128) | 0 | 3–6 | 37–52 | 63–82 | 91–93‡ | NR | 32–35 | High | 3 |
| Counseling | 1 (38) | 1 | 6 | 45–51 | 75–78 | 91–94 | 6–9 | 35–36 | High | 0 | |
|
| |||||||||||
| Medifast | Control/education | 0 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Counseling | 1 (90) | NR | 9 | 43–45 | 33–76 | 42–60 | 36–56 | 38–39 | High | 1 | |
|
| |||||||||||
| Optifast | Control/education | 0 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Counseling | 4 (246) | 4 | 5–15 | 38–52 | 63–100 | 64‡ | 35‡ | 33–40 | High | 0 | |
|
| |||||||||||
| Self-Directed Programs | |||||||||||
|
| |||||||||||
| Atkins | Control/education | 1 (118) | NR | 12 | 41 | 74–75 | NR | NR | 31–32 | High | 0 |
| Counseling | 7 (1,026) | 3 | 5–24 | 40–54 | 9–100 | 14–79‡ | 3–66‡ | 31–37 | High | 3 | |
|
| |||||||||||
| Biggest Loser Club | Control/education | 1 (203) | NR | 3 | 42 | 58–59 | NR | NR | 32 | Low | 1 |
| Counseling | 0 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
|
| |||||||||||
| eDiets | Control/education | 0 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Counseling | 1 (47) | 1 | 12 | 43–44 | 100 | NR | NR | 33–34 | Unclear | 0 | |
|
| |||||||||||
| Lose It! | Control/education | 0 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Counseling | 1 (35) | 1 | 6 | 43–45 | 78–88 | NR | 41–72 | 34–35 | High | 0 | |
|
| |||||||||||
| SlimFast | Control/education | 4 (362) | 1‡ | 6–51 | 39–70 | 35–82‡ | 82–86‡ | 9–14‡ | 32–35 | High | 3 |
| Counseling | 4 (297) | 3 | 3–12 | 37–59 | 33–100‡ | NR | NR | 29–34 | High | 4 | |
Urban location defined as trial located in a city with a population >250,000.
Risk of bias across studies rated as low, if most trials within that group were individually rated as overall low at the first reported time point. Risk of bias across studies rated as unclear, if most trials within that group were individually rated as overall unclear at the first reported time point. Risk of bias across studies rated as high, if most trials within that group were individually rated as overall high at the first reported time point. Otherwise, risk of bias across studies was rated as moderate.
Results from trials reporting this characteristic. Abbreviations: BMI – body mass index; HMR – Health Management Resources; NR – not reported; RCT – randomized controlled trial.
Leading Market Share Programs: Weight Watchers, Jenny Craig, Nutrisystem
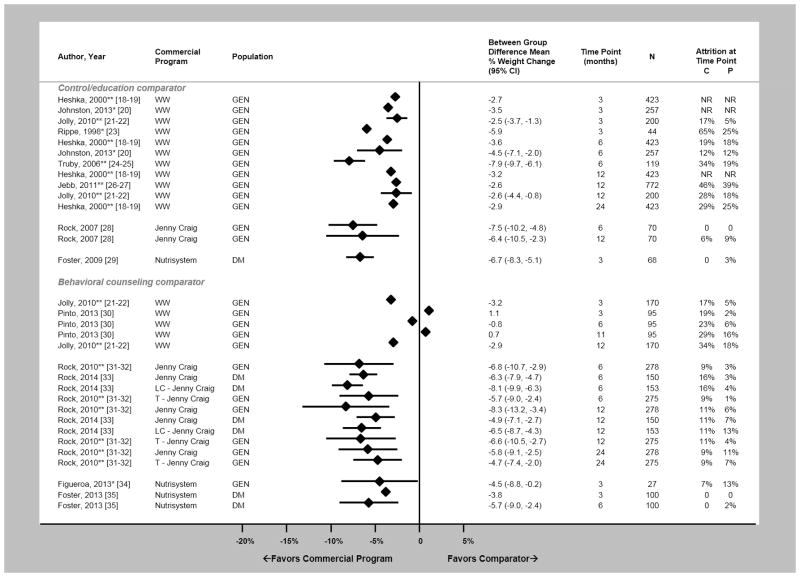
Six RCTs compared Weight Watchers to control/education (18–27) – two only reported completers’ analyses. As compared to control/education, Weight Watchers resulted in at least 2.6% greater weight loss at 12 months in ITT analyses (ROB: moderate)(Figure 1). Attrition was variable across trials. Adherence was reported variably (Supplemental Table 5). Three trials reported on serious adverse events – none occurred (18–19, 26–27,36)(Supplemental Table 6). Two RCTs compared Weight Watchers to behavioral counseling (21–22, 30). Results were mixed (Figure 1), which may be due to the difference in counseling providers – primary care provider (21–22) versus psychologist (30). Harms were not reported.
Figure 1.
Difference in mean percent weight change between commercial programs that dominate the market share (Weight Watchers; Jenny Craig; Nutrisystem) and comparators displayed by time point. Diamond size is standardized across trials and does not reflect sample size analyzed. Attrition reflects the percentage of participants unavailable for weight measurement at that time point in the trial. *Results from completers’ analysis. **Results reported in more than one article. Abbreviations: C – attrition reported in comparator arm at time point; DM – overweight or obese patients with diabetes mellitus; GEN – general population of patients with overweight and obesity; LC – low carbohydrate version of program; NR – not reported; P – attrition reported in commercial program arm at time point; T – telephone based program; WW – Weight Watchers.
One RCT compared Jenny Craig to control/education (28) and two RCTs compared Jenny Craig to behavioral counseling (31–33). Jenny Craig resulted in at least 4.9% greater weight loss at 12 months as compared to both control/education and counseling in ITT analyses (ROB: moderate and high, respectively)(Figure 1), regardless of program delivery (in person versus telephone), program version (traditional versus low-carbohydrate), or study population (general versus patients with diabetes). Attrition was less than 20% in all trials. Adherence was not reported and harms occurred rarely (Supplemental Table 6).
One RCT compared Nutrisystem to control/education (29) and two RCTs compared Nutrisystem to behavioral counseling (34–35) – one only reported completers’ analyses. Regardless of analysis type or study population, Nutrisystem resulted in at least 3.8% greater weight loss as compared to both control/education and counseling at 3 months (ROB: moderate and high, respectively)(Figure 1). No trials continued to 12 months. Attrition was less than 20% in all trials. Adherence was not reported and harms occurred rarely when reported (Supplemental Table 6).
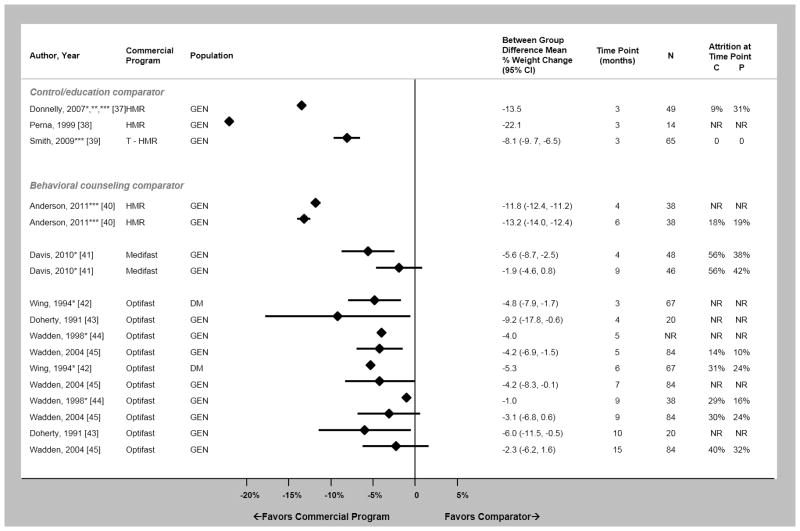
Very-Low-Calorie and Low-Calorie Programs: Health Management Resources (HMR), Medifast, Optifast
Three RCTs compared HMR to control/education (37–39) – one only reported completers’ analyses – and one RCT compared HMR to behavioral counseling (40). No trials continued to 12 months. At 3 months, HMR achieved more weight loss than control/education (ROB: high)(Figure 2). The magnitude was diminished when HMR was delivered remotely (39). HMR resulted in 13.2% greater weight loss than counseling at 6 months (ROB: high)(Figure 2). Attrition was variable when reported. Program adherence was high, when reported (Supplemental Table 5). HMR participants reported constipation (Supplemental Table 6)(46–47).
Figure 2.
Difference in mean percent weight change between commercial programs that use very-low-calorie or low calorie meal replacements (HMR; Medifast; Optifast) and comparators displayed by time point. Diamond size is standardized across trials and does not reflect sample size analyzed. Attrition reflects the percentage of participants unavailable for weight measurement at that time point in the trial. *Results from completers’ analysis. **Trial reported median percent difference in weight change rather than mean. ***Intervention was low-calorie (1200 to 1500 calories daily) during weight loss phase. Abbreviations: C – attrition reported in comparator arm at time point; DM – overweight or obese patients with diabetes mellitus; GEN – general population of patients with overweight and obesity; HMR – Health Management Resources; NR – not reported; P – attrition reported in commercial program arm at time point; T – telephone based program.
One RCT reported completers’ analyses comparing Medifast to behavioral counseling (41). Medifast achieved a 5.6% greater weight loss than counseling at 4 months (ROB: high). The difference was not statistically significant at 9 months (Figure 2). Attrition was high (38–56%). Adherence was not reported and no serious harms occurred (Supplemental Table 6).
Four RCTs compared Optifast with behavioral counseling (42–45) – two reported completers’ analyses only. Optifast resulted in 4.2–9.2% greater weight loss than counseling at 4–5 months in ITT analyses (ROB: moderate)(Figure 2). Only one trial continued beyond 12 months, which reported no statistically significant difference. Attrition was variable when reported, and adherence was not reported. Two prospective case series studies reported less than 1% of Optifast participants experienced death (48–49). Cholecystectomy, constipation, or alopecia rarely occurred (Supplemental Table 6)(49–50).
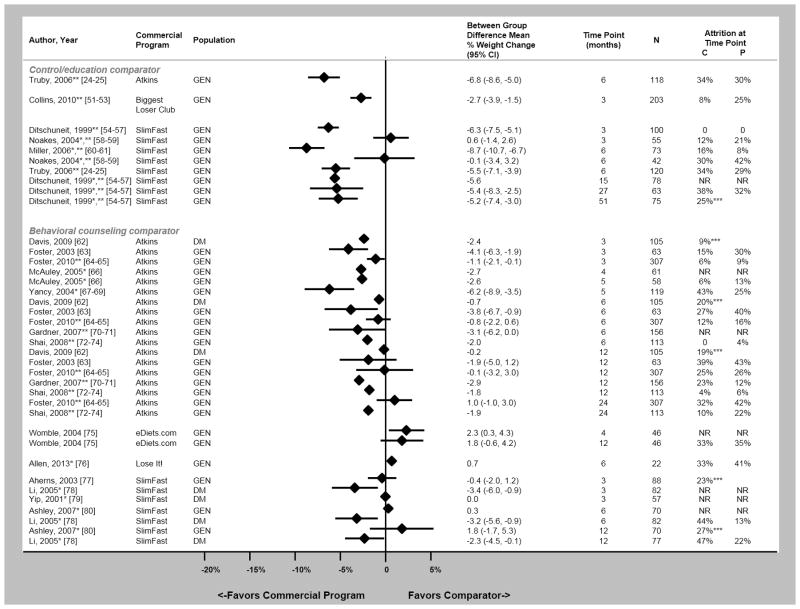
Self-Directed Programs: Atkins, Biggest Loser Club, eDiets, Lose It!, SlimFast
One RCT compared Atkins to control/education (24–25). Atkins resulted in 6.8% greater weight loss than control/education at 6 months (ROB: high)(Figure 3). Seven RCTs compared Atkins to behavioral counseling (62–74) – one reporting completers’ analyses only. As compared to behavioral counseling, Atkins achieved 0.1–2.9% greater weight loss at 12 months in ITT analyses (ROB: moderate)(Figure 3). Adherence was not reported and Atkins’ participants reported constipation (Supplemental Table 6).
Figure 3.
Difference in mean percent weight change between self-directed commercial programs (Atkins; Biggest Loser Club; eDiets; Lose It!, SlimFast) and comparators displayed by time point. Diamond size is standardized across trials and does not reflect sample size analyzed. Attrition reflects the percentage of participants unavailable for weight measurement at that time point in the trial. Panel C displays the results for. *Results from completers’ analysis. **Results reported in more than one article. ***Value represents overall attrition at time point. Abbreviations: C – attrition reported in comparator arm at time point; DM – overweight or obese patients with diabetes mellitus; GEN – general population of patients with overweight and obesity; NR – not reported; P – attrition reported in commercial program arm at time point.
Three RCTs evaluated Internet-based programs – Biggest Loser Club, eDiets, and Lose It! One RCT reported that Biggest Loser Club achieved 2.7% greater weight loss than control/education at 3 months (ROB: low)(Figure 3)(51–53). One RCT demonstrated no statistically significant difference between eDiets and counseling at 12 months (ROB: high)(Figure 3)(75). One RCT reported that Lose It! achieved similar weight loss to counseling at 3 months in completers’ analysis (ROB: high)(Figure 3)(76). Attrition was high and program adherence variable when reported (Supplemental Table 5). No trial reported harms.
Four RCTs compared SlimFast to control/education (24–25,54–61) – two reported completers’ analyses. Results were mixed (Figure 3). One RCT that showed no between group difference provided free food to both control and intervention arms (58–59), which may explain the different results as compared to other trials. Four RCTs compared SlimFast to behavioral counseling (77–80) – three only reported completers’ analyses. Results were again mixed (Figure 3), although most trials showed minimal between group differences. Attrition and adherence were variable, when reported (Supplemental Table 5). Harms were not reported.
Discussion
Overall, the literature base examining commercial weight loss programs has expanded since the prior 2005 review (14). We identified 13 RCTs evaluating commercial weight loss programs that currently occupy a majority of the U.S. market share: Weight Watchers, NutriSystem, and Jenny Craig. We found 9 RCTs evaluating very-low-calorie programs and 18 RCTs examining self-directed programs. We identified no RCTs for the 21 other programs that met our inclusion criteria; therefore, additional studies are still needed.
Given provisions in the ACA covering obesity screening, clinicians may be increasingly prompted to consider referring patients to commercial programs. Recent weight management guidelines from the American Heart Association (AHA)/American College of Cardiology (ACC)/The Obesity Society (TOS) recommend that clinicians refer patients with overweight and obesity to high intensity programs (15). However, these guidelines do not provide recommendations regarding commercial weight loss programs. A recent review comparing the efficacy of different diet types found that low carbohydrate and low fat diets resulted in the greatest weight losses at 6- and 12-months (81). This meta-analysis categorized several commercial programs into groups focused on dietary composition. They reported results for individual programs as a secondary analysis; however, several programs in the commercial marketplace were not included in this study (e.g., Optifast, SlimFast, Lose It!). Our study compliments this prior work by providing a comprehensive representation of available commercial programs. Overall, our results may help clinicians critically evaluate all commercial programs, which we outline below by program type.
Currently, three programs dominate the weight loss services industry – Weight Watchers, Jenny Craig and Nutrisystem (6). These three programs are high intensity, and two rely on low-calorie meal replacements. Our findings show that Weight Watchers’ participants consistently lose more weight than control/education participants, which they sustain beyond 12 months. While we conclude that Weight Watchers has weight loss efficacy, it is unclear whether Weight Watchers is superior to behavioral counseling. Jenny Craig participants consistently had a greater sustained weight loss as compared to both control/education and counseling participants, including among patients with diabetes mellitus. We identified Weight Watchers as one of the lowest cost programs, which has previously been shown to be the most cost-effective weight management strategy as compared to other commercial programs and medications (82). Jenny Craig is more expensive than Weight Watchers, although Jenny Craig includes the cost of food (meal replacements) where Weight Watchers estimates do not. Given these findings, it may be reasonable for clinicians to refer patients to Weight Watchers or Jenny Craig, especially if they lack the time, training, or ancillary staff to deliver behavioral counseling in their practices. Clinicians should note our moderate to high ROB ratings for these trials. Finally, Nutrisystem demonstrates better short-term weight loss than control/education and behavioral counseling; however, we identified no long-term trial results. We conclude that Nutrisystem shows promise, but the lack of long-term RCTs prohibits definitive conclusions.
We examined three programs that promote weight loss through very-low-calorie meal replacements with calories typically ranging from 800 to 1000 daily and low-calorie meal replacements with calories typically ranging from 1000 to 1500 daily (HMR, Medifast, and Optifast). These programs achieve superior short-term weight loss outcomes than control/education and behavioral counseling. However, it is unclear whether they result in sustained, long-term weight losses, as differences between counseling and Medifast or Optifast were attenuated after 6 months (41,44–45). Clinicians should note our high ROB ratings for most of these trials. Many studies examining these programs were retrospective or short-term prospective case series, and therefore, did not meet our eligibility criteria. Very-low-calorie approaches may also have some risks, such as gallstones requiring cholecystectomy (49–50). Prior studies have found risk of gallstones to be three times greater with very-low-calorie diets (VLCD) than a low-calorie approach (83). In addition, high program costs may make these programs unaffordable for many patients. Current AHA/ACC/TOS recommendations encourage providers to refer to VLCD only in limited circumstances under close medical supervision within a high-intensity lifestyle intervention (15).
We also examined 5 self-directed programs – all of which currently offer support through the Internet. Of these programs, Atkins showed greater short-term weight loss than control/education or counseling. A recent meta-analysis reported that Atkins-like programs resulted in greater weight losses at 6- and 12-months as compared to no diet (81). Our review included fewer Atkins trials then this meta-analysis, as they incorporated trials of Atkins and low-carbohydrate approaches similar to Atkins. While Atkins appears promising, we interpret these findings cautiously as the delivery of Atkins in many trials included in the prior meta-analysis and in this study may be different from the typical patient experience. For example, trials often relied upon registered dieticians to deliver counseling and dietary guidance on Atkins. SlimFast may help patients achieve greater weight loss than control/education, but does not appear to differ substantially from behavioral counseling. Given that most SlimFast RCTs only reported completers’ analyses, we consider these findings preliminary. Some SlimFast trials also incorporated counseling sessions as a part of the intervention, which likely differs from the typical patient experience. Clinicians should note our high ROB ratings for both Atkins and SlimFast trials. Finally, the three exclusively Internet-based programs – Biggest Loser Club, eDiets, and Lose It! – may achieve superior short-term weight loss than control/education, but do not appear to differ from counseling. Similarly, recent weight management guidelines have reported lower weight loss efficacy of online comprehensive programs as compared to similar programs delivered in-person (15). Despite some limitations, it should be noted that we typically identified the self-directed options as the most affordable options.
While our results have implications for clinical practice, we also believe that this evaluation is critical to policymakers, health insurers and employers. The ACA is likely to increase obesity screening, and therefore, it is critical to have an actionable plan that addresses weight management. Health insurers and employers may want to consider providing benefits coverage or incentives of reduced program fees for commercial programs with strong evidence of effectiveness to beneficiaries and employees. Based on our findings, we would identify Weight Watchers and Jenny Craig for consideration for such benefits coverage. Similarly, Medicaid administrations may also want to consider covering these programs for their beneficiaries, which some states have already done (12–13).
This systematic review has limitations. We forgo weight loss outcomes reported in prospective case series studies due to the high risk of selection bias. We limited the scope to weight loss programs currently available in the U.S.; however, many of the included programs are available worldwide. Other studies have examined weight loss programs in the United Kingdom (84). Our program eligibility criteria also excluded some popular programs like Ornish and Zone, as Ornish does not focus on weight loss and Zone offers no behavioral/social support. These programs’ weight loss results have been well characterized previously (81). For several commercial programs (e.g., South Beach, Ideal Protein), their publications failed to meet our eligibility criteria, and therefore, are not included in this review. Finally, we do not report any head-to-head comparisons of commercial programs.
We also identified limitations within the literature base. Some programs only had results for short-term trials, which may be of little value to clinicians trying to determine whether a program can be effective in achieving long-term weight loss. Internal validity of many trials was weak due to high or unequal attrition and inadequate handling of missing data given the use of last-observation-carried-forward intention-to-treat or completers’ analyses. In many trials, study staff assisted in program retention and trials often covered the costs of these programs for participants. Therefore, the study results are likely better than can be expected in a “real world” setting, as a prior study of one commercial program reported retention of only 7% at 12 months (85). Studies often failed to report adherence/engagement or adverse outcomes. When described, program adherence was reported differently across trials, making comparability across studies challenging. Finally, trials frequently lacked blinding by participant and study personnel and for not reporting the blinding of outcome assessors, raising the possibility of biased results.
Overall, we found consistent evidence supporting the long-term efficacy of Weight Watchers and Jenny Craig, while NutriSystem may require 12-month or 24-month RCTs reporting ITT analyses before we can be confident of the long-term effect. Very low-calorie dietary approaches can achieve substantial short-term weight losses; however, enthusiasm is limited due to potential risks and the lack of evidence supporting sustained long-term weight losses. Additional RCTs are needed to investigate the efficacy of SlimFast and Internet-based commercial weight loss programs, which are increasingly popular. Clinicians might consider prioritizing referral only for those commercial programs that have a substantial body of evidence demonstrating a consistent, long-term effect.
Supplementary Material
Supplemental Figure 1. Summary of evidence search and selection. *We also excluded trials with ineligible study designs (retrospective case series, RCT<12 weeks duration, etc) or ineligible programs (not available in the US, etc). **Ineligible commercial programs include those that use medications or supplements, modified specifically for the study, unavailable in the U.S., or available only to special populations like active duty military or veterans. ***Other trials include prospective case series or randomized controlled trials without an eligible comparator arm of 12 months or greater duration that reported harms outcomes. Abbreviations: CDSR – Cochrane Database of Systematic Reviews; RCT – randomized controlled trial.
Supplemental Figure 2. Difference in percentage of group achieving at least 5% weight loss between the commercial program and the comparator displayed by time point. Diamond size is standardized across trials and does not reflect sample size analyzed. *Results from completers’ analysis. **Results reported in more than one article. Abbreviations: DM – overweight or obese patients with diabetes mellitus; GEN – general population of patients with overweight and obesity; HMR – Health Management Resources; T – telephone based program; WW – Weight Watchers.
Acknowledgments
Grant Support
RSD was supported by the Johns Hopkins medical student summer research program. DKJ was supported by the Medical Student Research Program in Diabetes at JHU-UMD Diabetes Research Center from the National Institute of Diabetes and Digestive and Kidney Diseases (P30DK079637). SNB was supported by a career development award from the National Heart, Lung, and Blood Institute (1K01HL096409). KAG was supported by a career development award from the National Heart, Lung, and Blood Institute (K23HL116601).
Footnotes
The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298(17):2028–37. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 3.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289(16):2083–93. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 4.Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–86. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saad L. To lose weight, Americans rely more on dieting than exercise. [September 27, 2014];Gallup Poll Social Series: Health and Healthcare. 2011 Accessed at http://www.gallup.com/poll/150986/Lose-Weight-Americans-Rely-Dieting-Exercise.aspx on.
- 6.IBIS World. [August 25, 2014];Weight loss services in the U.S. industry market research report. 2014 Jun; Accessed at http://clients1.ibisworld.com/reports/us/industry/default.aspx?entid=1719 on.
- 7.Congressional Budget Office. [December 17, 2014];Updated estimates of the insurance coverage provisions of the Affordable Care Act. 2014 Feb; Accessed at http://www.cbo.gov/sites/default/files/cbofiles/attachments/45010-breakout-AppendixB.pdf on.
- 8.Sebelius K. [December 6, 2014];Report to congress on preventive services and obesity-related services available to Medicaid enrollees. 2014 Accessed at http://www.medicaid.gov/medicaid-chip-program-information/by-topics/quality-of-care/downloads/rtc-preventive-obesity-related-services2014.pdf on.
- 9.Lee JS, Sheer JLO, Lopez N, Rosenbaum S. Coverage of Obesity Treatment: A state-by-state analysis of Medicaid and State Insurance Laws. Public Health Reports. 2010;125(4):596–604. doi: 10.1177/003335491012500415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaiser Commission on Medicaid and the Uninsured. [December 6, 2014];Coverage of Preventive Services for Adults in Medicaid. 2012 Sep; Accessed at http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8359.pdf on.
- 11.United States Preventive Services Task Force. [December 6, 2014];Obesity in Adults: Screening and Management. 2012 Jun; Accessed at http://www.uspreventiveservicestaskforce.org/uspstf/uspsobes.htm on.
- 12.Mitchell NA, Ellison MC, Hill JO, Tsai AG. Evaluation of the effectiveness of making Weight Watchers available to Tennessee Medicaid (TennCare) recipients. J Gen Intern Med. 2013;28(1):12–7. doi: 10.1007/s11606-012-2083-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bleich SN, Herring BJ. Medicaid coverage for weight loss counseling may make ‘cents’. J Gen Intern Med. 2013;28(1):3–5. doi: 10.1007/s11606-012-2201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsai AG, Wadden TA. Systematic Review: An Evaluation of Major Commercial Weight Loss Programs in the United States. Ann Intern Med. 2005;142(1):56–66. doi: 10.7326/0003-4819-142-1-200501040-00012. [DOI] [PubMed] [Google Scholar]
- 15.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS Guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 Suppl 2):S102–38. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsertsvadze A, Maglione M, Chou R, Garritty C, Coleman C, Lux L, et al. AHRQ Publication No. 11-EHC057-EF. Rockville, MD: Agency for Healthcare Research and Quality; Jul, 2011. Updating Comparative Effectiveness Reviews: Current Efforts in AHRQ’s Effective Health Care Program. Methods Guide for Comparative Effectiveness Reviews. [PubMed] [Google Scholar]
- 17.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. [October 1, 2013];The Cochrane Collaboration. 2011 Accessed at www.cochrane-handbook.org on.
- 18.Heshka S, Greenway F, Anderson JW, Atkinson RL, Hill JO, Phinney SD, et al. Self-help weight loss versus a structured commercial program after 26 weeks: a randomized controlled study. Am J Med. 2000;109(4):282–7. doi: 10.1016/s0002-9343(00)00494-0. [DOI] [PubMed] [Google Scholar]
- 19.Heshka S, Anderson JW, Atkinson RL, Greenway FL, Hill JO, Phinney SD, et al. Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA. 2003;289(14):1792–8. doi: 10.1001/jama.289.14.1792. [DOI] [PubMed] [Google Scholar]
- 20.Johnston CA, Rost S, Miller-Kovach K, Moreno JP, Foreyt JP. A randomized controlled trial of a community-based behavioral counseling program. Am J Med. 2013;126(12):1143.e19–24. doi: 10.1016/j.amjmed.2013.04.025. [DOI] [PubMed] [Google Scholar]
- 21.Jolly K, Daley A, Adab R, Lewis A, Denley J, Beach J, et al. A randomized controlled trial to compare a range of commercial or primary care led weight reduction programmes with a minimal intervention control for weight loss in obesity: the Lighten Up trial. BMC Public Health. 2010;10:439. doi: 10.1186/1471-2458-10-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jolly K, Lewis A, Beach J, Denley J, Adab P, Deeks JJ, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: Lighten Up randomized controlled trial. BMJ. 2011;343:d6500. doi: 10.1136/bmj.d6500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rippe JM, Price JM, Hess SA, Kline G, DeMers KA, Damitz S. Improved psychological well-being, quality of life, and health practices in moderately overweight women participating in a 12-weeks structured weight loss program. Obes Res. 1998;6(3):208–18. doi: 10.1002/j.1550-8528.1998.tb00339.x. [DOI] [PubMed] [Google Scholar]
- 24.Truby H, Baic S, DeLooy A, Fox KR, Livingstone MB, Logan CM, et al. Randomised controlled trial of four commercial weight loss programmes in the UK: initial findings from the BBC “diet trials. BMJ. 2006;322(7553):1309–11. doi: 10.1136/bmj.38833.411204.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morgan LM, Griffin BA, Millward DJ, DeLooy A, Fox KR, Baic S, et al. Comparison of the effects of four commercially available weight-loss programmes on lipid-based cardiovascular risk factors. Public Health Nutr. 2008;12(6):799–807. doi: 10.1017/S1368980008003236. [DOI] [PubMed] [Google Scholar]
- 26.Jebb SA, Ahern AL, Olson AD, Aston LM, Holzapfel C, Stoll J, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomized controlled trial. Lancet. 2011;378(9801):1485–92. doi: 10.1016/S0140-6736(11)61344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker CG, Holzapfel C, Loos RJ, Mander AP, Kloop N, Illig T, et al. Genetic predisposition to an adverse lipid profile limits the improvement in total cholesterol in response to weight loss. Obesity (Silver Spring) 2013;21(12):2589–95. doi: 10.1002/oby.20328. [DOI] [PubMed] [Google Scholar]
- 28.Rock CL, Pakiz B, Flatt SW, Quintana EL. Randomized trial of a multifaceted commercial weight loss program. Obesity (Silver Spring) 2007;15(4):939–49. doi: 10.1038/oby.2007.614. [DOI] [PubMed] [Google Scholar]
- 29.Foster GD, Borradaile KE, Vander Veur SS, Leh Shantz K, Dilks RJ, Goldbacher EM, et al. The effects of a commercially available weight loss program among obese patients with type 2 diabetes: a randomized study. Postgrad Med. 2009;121(5):113–8. doi: 10.3810/pgm.2009.09.2046. [DOI] [PubMed] [Google Scholar]
- 30.Pinto AM, Fava JL, Hoffman DA, Wing RR. Combining behavioral weight loss treatment and a commercial program: a randomized clinical trial. Obesity (Silver Spring) 2013;21(4):673–80. doi: 10.1002/oby.20044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rock CL, Flatt SW, Sherwood NE, Karanja N, Pakiz B, Thomson CA. Effect of a free prepared meal and incentivized weight loss program on weight loss and weight loss maintenance in obesity and overweight women: a randomized controlled trial. JAMA. 2010;304(16):1803–11. doi: 10.1001/jama.2010.1503. [DOI] [PubMed] [Google Scholar]
- 32.Dow CA, Thomson CA, Flatt SW, Sherwood NE, Pakiz B, Rock CL. Predictors of improvement in cardiometabolic risk factors with weight loss in women. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rock CL, Flatt SW, Pakiz B, Taylor KS, Leone AF, Brelje K, et al. Weight loss, glycemic control, and cardiovascular disease risk factors in response to differential diet composition in a weight loss program in type 2 diabetes: a randomized controlled trial. Diabetes Care. 2014;37(6):1573–80. doi: 10.2337/dc13-2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Figueroa A, Vicil F, Sanchez-Gomes MA, Wong A, Ormsbee MJ, Hooshmand S, et al. Effects of diet and/or low-intensity resistance exercise training on arterial stiffness, adiposity, and lean mass in obese postmenopausal women. Am J Hypertension. 2013;26(3):416–23. doi: 10.1093/ajh/hps050. [DOI] [PubMed] [Google Scholar]
- 35.Foster GD, Wadden TA, Lagrotte CA, Vander Veur SS, Hesson LA, Homko CJ, et al. A randomized comparison of a commercially available portion-controlled weight-loss intervention with a diabetes self-management education program. Nutr Diabetes. 2013;3:e63. doi: 10.1038/nutd.2013.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dansinger ML, Gleason JA, Griffith JL, Sleker HP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA. 2005;293(1):45–53. doi: 10.1001/jama.293.1.43. [DOI] [PubMed] [Google Scholar]
- 37.Donnelly JE, Smith BK, Dunn L, Mayo MM, Jacobsen DJ, Stewart EE, et al. Comparison of a phone vs clinic approach to achieve 10% weight loss. Int J Obesity. 2007;31(8):1270–6. doi: 10.1038/sj.ijo.0803568. [DOI] [PubMed] [Google Scholar]
- 38.Perna F, Bryner R, Donley D, Kolar M, Hornsby G, Sauers J, et al. Effect of diet and exercise on quality of life and fitness parameters among obese individuals. J Exercise Physiology Online. 1992;2(2) [Google Scholar]
- 39.Smith BK, Van Walleghen EL, Cook-Wiens G, Martin RN, Curry CR, Sullivan DK, et al. Comparison of two self-directed weight loss interventions: limited weekly support vs. no outside support. Obes Res Clin Pract. 2009;3(3):I–IV. doi: 10.1016/j.orcp.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 40.Anderson JW, Reynolds R, Bush HM, Rinsky JL, Washnock C. Effect of a behavioral/nutritional intervention program on weight loss in obese adults: a randomized controlled trial. Postgrad Med. 2011;123(5):205–13. doi: 10.3810/pgm.2011.09.2476. [DOI] [PubMed] [Google Scholar]
- 41.Davis LM, Coleman C, Kiel J, Rampolla J, Hutchisen T, Ford L, et al. Efficacy of a meal replacement diet plan compared to a food-based diet plan after a period of weight loss and weight maintenance: a randomized controlled trial. Nutr J. 2010;9:11. doi: 10.1186/1475-2891-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wing RR, Blair E, Marcus M, Epstein LH, Harvey J. Year-long weight loss treatment for obese patients with type II diabetes: dose including an intermittent very-low-calorie diet improve outcome? Am J Med. 1994;97(4):354–62. doi: 10.1016/0002-9343(94)90302-6. [DOI] [PubMed] [Google Scholar]
- 43.Doherty JU, Wadden TA, Zuk L, Letizia KA, Foster GD, Day SC. Long-term evaluation of cardiac function in obese patients treated with a very-low-calorie diet: a controlled clinical study of patients without underlying cardiac disease. Am J Clin Nutr. 1991;53(4):854–8. doi: 10.1093/ajcn/53.4.854. [DOI] [PubMed] [Google Scholar]
- 44.Wadden TA, Considine RV, Foster GD, Anderson DA, Sarwer DB, Caro JS. Short- and long-term changes in serum leptin dieting obese women: effects of caloric restriction and weight loss. J Clin Endocrinol Metab. 1998;83(1):214–8. doi: 10.1210/jcem.83.1.4494. [DOI] [PubMed] [Google Scholar]
- 45.Wadden TA, Foster GD, Sarwer DB, Anderson DA, Gladis M, Sanderson RS, et al. Dieting and the development of eating disorders in obese women: results of a randomized controlled trial. Am J Clin Nutr. 2004;80(3):560–8. doi: 10.1093/ajcn/80.3.560. [DOI] [PubMed] [Google Scholar]
- 46.Anderson JW, Hamilton CC, Crown-Weber E, Riddlemoser M, Gustafson NJ. Safety and effectiveness of a multidisciplinary very-low-calorie diet program for selected obese individuals. J Am Diet Assoc. 1991;91(12):1582. [PubMed] [Google Scholar]
- 47.Anderson JW, Brinkman-Kaplan V, Hamilton CC, Logan JE, Collins RW, Gustafson NJ. Food-containing hypocaloric diets are as effective as liquid-supplement diets for obese individuals with NIDDM. Diabetes Care. 1994;17(6):602–4. doi: 10.2337/diacare.17.6.602. [DOI] [PubMed] [Google Scholar]
- 48.Kirschner MA, Schneider G, Ertel N, Cortes G. Supplemented starvation: a successful method for control of major obesity. J Med Soc N J. 1979;76(3):175–9. [PubMed] [Google Scholar]
- 49.Bischoff SC, Damms-Machado A, Betz C, Herpertz S, Legenbauer R, Low T, et al. Multicenter evaluation of an interdisciplinary 52-week weight loss program for obesity with regard to body weight, comorbidities and quality of life -- a prospective study. Int J Obes (Lond) 2012;36(4):614–24. doi: 10.1038/ijo.2011.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wadden TA, Foster GD, Letizia KA, Stenkard AJ. A multicenter evaluation of a proprietary weight reduction program for the treatment of marked obesity. Arch Intern Med. 1992;152(5):961–6. [PubMed] [Google Scholar]
- 51.Collins CE, Morgan PJ, Jones P, Fletcher K, Martin J, Aguiar EJ, et al. Evaluation of a commercial web-based weight loss and weight loss maintenance program in overweight and obese adults: a randomized controlled trial. BMC Public Health. 2010;10:669. doi: 10.1186/1471-2458-10-669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Collins CE, Morgan PJ, Jones P, Fletcher K, Martin J, Aguiar EJ, et al. A 12-week commercial web-based weight-loss program for overweight and obese adults: randomized controlled trial comparing basic versus enhanced features. J Med Internet Res. 2012;14(2):e57. doi: 10.2196/jmir.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hutchesson MJ, Collins CE, Morgan PJ, Watson JF, Guest M, Callister R. Changes to dietary intake during a 12-week commercial web-based weight loss program: a randomized controlled trial. Eur J Clin Nutr. 2014;68(1):64–70. doi: 10.1038/ejcn.2013.194. [DOI] [PubMed] [Google Scholar]
- 54.Ditschuneit HH, Flechtner-Mors M, Johnson TD, Adler G. Metabolic and weight-loss effects of a long-term dietary intervention in obese patients. Am J Clin Nutr. 1999;69(2):198–204. doi: 10.1093/ajcn/69.2.198. [DOI] [PubMed] [Google Scholar]
- 55.Fletchtner-Mors M, Ditschuneit HH, Johnson TD, et al. Metabolic and weight loss effects of long-term dietary intervention in obese patients: four-year results. Obes Res. 2000;8(5):399–402. doi: 10.1038/oby.2000.48. [DOI] [PubMed] [Google Scholar]
- 56.Ditschuneit HH, Flechtner-Mors M. Value of structured ieals for weight management: risk factors and long-term weight maintenance. Obes Res. 2001;9 (Suppl 4):284S–9S. doi: 10.1038/oby.2001.132. [DOI] [PubMed] [Google Scholar]
- 57.Ditschuneit HH, Frier HI, Flechtner-Mors M. Lipoprotein responses to weight loss and weight maintenance in high-risk obese subjects. Eur J Clin Nutr. 2002;56(3):264–70. doi: 10.1038/sj.ejcn.1601375. [DOI] [PubMed] [Google Scholar]
- 58.Noakes M, Foster PR, Keogh JB, Clifton PM. Meal replacements are as effective as structured weight-loss diets for treating obesity in adults with features of metabolic syndrome. J Nutr. 2004;134(8):1894–9. doi: 10.1093/jn/134.8.1894. [DOI] [PubMed] [Google Scholar]
- 59.Clifton PM, Keogh JB, Foster PR, Noakes M. Effect of weight loss on inflammatory and endothelial markers and FMD using two low-fat diets. Int J Obesity. 2005;29(12):1445–51. doi: 10.1038/sj.ijo.0803039. [DOI] [PubMed] [Google Scholar]
- 60.Miller GD, Nicklas BJ, Davis C, Loeser RF, Lenchik L, Messier SP. Intensive weight loss program improves physical function in older obese adults with knee osteoarthritis. Obesity (Silver Spring) 2006;14(7):1219–30. doi: 10.1038/oby.2006.139. [DOI] [PubMed] [Google Scholar]
- 61.Miller GD. Improved nutrient intake in older obese adults undergoing a structured diet and exercise intentional weight loss program. J Nutr Health Aging. 2010;14(6):461–6. doi: 10.1007/s12603-010-0100-3. [DOI] [PubMed] [Google Scholar]
- 62.Davis NJ, Tomuta N, Schechter C, Isasi CR, Segal-Isaacson CJ, Stein D, et al. Comparative study of the effects of a 1-year dietary intervention of a low-carbohydrate diet versus a low-fat diet on weight and glycemic control in type 2 diabetes. Diabetes Care. 2009;32(7):1147–52. doi: 10.2337/dc08-2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med. 2003;348:2082–90. doi: 10.1056/NEJMoa022207. [DOI] [PubMed] [Google Scholar]
- 64.Foster GD, Wyatt HR, Hill JO, Makris AP, Rosenbaum DL, Brill C, et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: a randomized trial. Ann Intern Med. 2010;153:147–57. doi: 10.1059/0003-4819-153-3-201008030-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Friedman AN, Ogden LG, Foster GD, Klein S, Stein R, Miller B, et al. Comparative effects of low-carbohydrate high-protein versus low-fat diets on the kidney. Clin J Am Soc Nephrol. 2012;7:1103–11. doi: 10.2215/CJN.11741111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McAuley KA, Hopkins CM, Smith KJ, McLay RT, Williams SM, Taylor RW, et al. Comparison of high-fat and high-protein diets with a high-carbohydrate diet in insulin-resistant obese women. Diabetologia. 2005;48:8–18. doi: 10.1007/s00125-004-1603-4. [DOI] [PubMed] [Google Scholar]
- 67.Yancy WS, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia. Ann Intern Med. 2004;140:769–77. doi: 10.7326/0003-4819-140-10-200405180-00006. [DOI] [PubMed] [Google Scholar]
- 68.Westman EC, Yancy WS, Olsen MK, Dudley T, Guyton JR. Effect of a low-carbohydrate, ketogenic diet program compared to a low-fat diet on fasting lipoprotein subclasses. Int J Cardiol. 2006;110(2):212–6. doi: 10.1016/j.ijcard.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 69.Yancy WS, Almirall D, Maciejewski ML, Kolotkin RL, McDuffie JR, Westman EC. Effects of two weight-loss diets on health-related quality of life. Qual Life Res. 2009;18(3):281–9. doi: 10.1007/s11136-009-9444-8. [DOI] [PubMed] [Google Scholar]
- 70.Gardner CD, Kiazand A, Alhassan S, Kim S, Stafford RS, Balise RR, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: The A to Z weight loss study: a randomized controlled trial. JAMA. 2007;297:969–77. doi: 10.1001/jama.297.9.969. [DOI] [PubMed] [Google Scholar]
- 71.Moore SD, King AC, Kiernan M, Gardner CD. Outcome expectations and realization as predictors of weight regain among dieters. Eat Behav. 2011;12(1):60–3. doi: 10.1016/j.eatbeh.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenber I, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359:229–41. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 73.Greenberg I, Stampfer MJ, Schwarzfuchs D, Shai I. Adherence and success in long-term weight loss diets: the dietary intervention randomized controlled trial (DIRECT) J Am Coll Nutr. 2009;28:159–68. doi: 10.1080/07315724.2009.10719767. [DOI] [PubMed] [Google Scholar]
- 74.Tirosh A, Golan R, Harman-Boehm I, Henkin Y, Schwarzfuchs D, Rudich A, et al. Renal function following three distinct weight loss dietary strategies during 2 years of a randomized controlled trial. Diabetes Care. 2013;36(8):2225–32. doi: 10.2337/dc12-1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Womble LG, Wadden TA, McGuckin BG, Sargent SL, Rothman RA, Krauthamer-Ewing ES. A randomized controlled trial of a commercial Internet weight loss program. Obes Res. 2004;12(6):1011–8. doi: 10.1038/oby.2004.124. [DOI] [PubMed] [Google Scholar]
- 76.Allen JK, Stephens J, Dennison Himmelfarb CR, Stewart KJ, Hauck S. Randomized controlled pilot study testing use of smartphone technology for obesity treatment. J Obes. 2013;2013:151597. doi: 10.1155/2013/151597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ahrens RA, Hower M, Best AM. Effects of weight reduction interventions by community pharmacists. J Am Pharm Assoc. 2003;43(5):583–9. doi: 10.1331/154434503322452210. [DOI] [PubMed] [Google Scholar]
- 78.Li Z, Hong K, Saltsman P, DeShields S, Bellman M, Thames G, et al. Long-term efficacy of soy-based meal replacements vs an individualize diet plan in obese type II DM patients: relative effects on weight loss, metabolic parameters, and C-reactive protein. Eur J Clin Nutr. 2005;59(3):411–8. doi: 10.1038/sj.ejcn.1602089. [DOI] [PubMed] [Google Scholar]
- 79.Yip I, Go VL, DeShields S, Saltsman P, Bellman M, Thames G, et al. Liquid meal replacements and glycemic control in obese type 2 diabetes patients. Obes Res. 2001;9 (Suppl 4):341S–7S. doi: 10.1038/oby.2001.140. [DOI] [PubMed] [Google Scholar]
- 80.Ashley JM, Herzog H, Clodfeler S, Bovee V, Schrage J, Piritsos C. Nutrient adequacy during weight loss interventions: a randomized study in women comparing the dietary intake in a meal replacement group with a traditional food group. Nutr J. 2007;6:12. doi: 10.1186/1475-2891-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Johnston BC, Kanters S, Bandayrel K, Wu P, Naji F, Siemieniuk RA, et al. Comparison of weight loss among named diet programs in overweight and obese adults: a meta-analysis. JAMA. 2014;312(9):923–33. doi: 10.1001/jama.2014.10397. [DOI] [PubMed] [Google Scholar]
- 82.Finkelstein EA, Kruger E. Meta- and cost-effectiveness analysis of commercial weight loss strategies. Obesity (Silver Spring) 2014;22(9):1942–51. doi: 10.1002/oby.20824. [DOI] [PubMed] [Google Scholar]
- 83.Johansson K, Sundstrom J, Marcus C, Hemmingsson E, Neovius M. Risk of symptomatic gallstones and cholecystectomy after a very-low-calorie diet or low-calorie diet in a commercial weight loss program: 1-year matched cohort study. Int J Obes (Lond) 2014;38(2):279–84. doi: 10.1038/ijo.2013.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Madigan CD, Daley AJ, Lewis AL, Jolly K, Aveyard P. Which weight-loss programmes are as effective as Weight Watchers?: non-inferiority analysis. Br J Gen Pract. 2014;64(620):e128–36. doi: 10.3399/bjgp14X677491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Finley CE, Barlow CE, Greenway FL, Rock CL, Blair SN. Retention rates and weight loss in a commercial weight loss program. Int J Obes (Lond) 2007;31(2):292–8. doi: 10.1038/sj.ijo.0803395. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Summary of evidence search and selection. *We also excluded trials with ineligible study designs (retrospective case series, RCT<12 weeks duration, etc) or ineligible programs (not available in the US, etc). **Ineligible commercial programs include those that use medications or supplements, modified specifically for the study, unavailable in the U.S., or available only to special populations like active duty military or veterans. ***Other trials include prospective case series or randomized controlled trials without an eligible comparator arm of 12 months or greater duration that reported harms outcomes. Abbreviations: CDSR – Cochrane Database of Systematic Reviews; RCT – randomized controlled trial.
Supplemental Figure 2. Difference in percentage of group achieving at least 5% weight loss between the commercial program and the comparator displayed by time point. Diamond size is standardized across trials and does not reflect sample size analyzed. *Results from completers’ analysis. **Results reported in more than one article. Abbreviations: DM – overweight or obese patients with diabetes mellitus; GEN – general population of patients with overweight and obesity; HMR – Health Management Resources; T – telephone based program; WW – Weight Watchers.