Abstract
Systematic measurement of treatment preferences is needed to obtain well-informed preferences. Guided by a conceptualization of treatment preferences, a measure was developed to assess treatment acceptability and preference. The purpose of this study was to evaluate the psychometric properties of the Treatment Acceptability and Preferences (TAP) measure. The TAP measure contains a description of each treatment under evaluation, items to rate its acceptability, and questions about participants’ preferred treatment option. The items measuring treatment acceptability were internally consistent (alpha > .80) and demonstrated validity, evidenced by a one-factor structure and differences in the scores between participants with preferences for particular interventions. The TAP measure has the potential for the assessment of acceptability and preferences for various behavioral interventions.
Keywords: Preference, acceptability, measurement, reliability, validity, chronic insomnia, behavioral treatments, treatment attributes, clinical trial
Preferences for treatment are of clinical importance. They form a critical component of patient-centered care, in which health professionals inform patients about treatment options, assess patients’ preferences, and provide care that is consistent with patients’ preferences (Givens, Houston, van Vouheers, Ford, & Cooper, 2007; Sidani, Epstein & Miranda, 2006). Providing care in accordance with patients’ preferences contributes to patients’ engagement in and adherence to treatment, satisfaction with care, and consequently outcome achievement (Lang, 2005; Mills et al., 2006; Rowe et al., 2005). In addition, preferences for treatment are increasingly implicated as potential threats to internal and external validity in intervention research. They are posited as factors influencing enrollment in a study, participation in and adherence to the intervention under evaluation, attrition, and impact of the treatment on the outcomes (Howard & Thornicroft, 2006; Millat, Borie, & Fingerhut, 2005).
A large number of studies have been conducted to gain an understanding of treatment preferences. In descriptive-correlational studies researchers have investigated the relationships of socio-demographic (e.g., age) and clinical (e.g., severity of illness) characteristics to treatment preferences expressed by persons with physical problems such as breast cancer (e.g., Ananian et al., 2004; Jansen et al., 2001; Koedoot et al., 2003) and heart diseases (e.g., Janevic et al., 2003; Morrow, Weiner, Steinley, Young, & Murray, 2007), and psychological problems such as recurrent panic attacks (e.g., Hazlett-Stevens et al., 2002) and depression (e.g., Cooper et al., 2003; Gum et al., 2006). Researchers have been unable to identify a consistent set of factors that significantly predict preferences. In experimental studies researchers examined the effects of treatment preferences on recruitment and retention of participants, adherence to treatment, and achievement of outcomes (e.g., Adamson, Sellman, & Dore, 2005; Awad, Shapiro, Lund, & Feine, 2000; Klaber-Moffett et al., 2004; Macias et al., 2005). Similarly, the results have been inconsistent, indicating that preferences for treatment have either no or minimal influence on recruitment, attrition, adherence to treatment, and outcomes.
Although factors such as across-study differences in the clinical problem addressed and type of treatment offered could have contributed to the inconsistent findings, of more concern are the procedure followed and the items used to assess preferences. Bowling and Rowe (2005) stated that the results of these studies should be viewed with caution due to the non-standardized and non-rigorous methods used to elicit preferences. Montgomery and Fahey (2001) found that the measurement of treatment preferences varies across studies from self-report questionnaires to investigator-administered trade-off or utility assessment. Furthermore, the reliability and validity of the measures have not been reported. The resulting preferences expressed by study participants may not be well-informed and may not accurately represent their choice of treatment. There is a need for a systematic method to validly assess preferences for treatment across studies (Bowling & Rowe; Thomas, Croft, Paterson, Dziedzic, & Hay, 2004).
As part of a multi-site methodological study involving a partially randomized clinical trial (PRCT) or preference trial (Sidani, Epstein, & Moritz, 2003), we developed a systematic measure for assessing preferences for treatment. In the PRCT design, assessment of treatment preferences is done to guide allocation of participants to intervention groups. The systematic measure was designed in accordance with a conceptualization of preferences derived from relevant literature and with suggestions to obtain well-informed preferences. The sections of the measure are consistent with the literature regarding how to obtain well-informed preferences. The purpose of the sub-study reported here was to evaluate the psychometric properties (internal consistency reliability and validity) of the measure for assessing treatment preferences. We begin by reviewing pertinent literature on treatment preferences and preference measurement. We then describe the measure we developed, and the design and results of the sub-study.
Relevant Literature
The literature review is divided into two sections. In the first, we present the conceptualization of treatment preferences that guided the review of the literature on preference measurement and the design of our measure. In the second section, we critically review available preference measures.
Conceptualization of treatment preferences
As conceptualized in relevant literature, treatment preferences represent patients’ choices of treatment, that is, the treatment option patients want to receive to manage their presenting clinical problem (Stalmeier et al. 2007). Preferences reflect individuals’ understanding of the treatment options (Corrigan & Salzer, 2003; TenHave, Coyne, Salzer, & Katz, 2003; Wensig & Elwyn, 2003) and perception of treatment acceptability (Becker, Darius, & Schaumberg, 2007). Treatment acceptability refers to a favorable or positive attitude toward treatment options. The attitude is based on a careful consideration of the treatment attributes.
Treatment attributes are characteristics of interventions that individuals take into consideration when formulating their perceived acceptability of treatment, and hence their preferences. The attributes commonly found to shape treatment preferences are: appropriateness in addressing the presenting clinical problem, suitability to individual life style, convenience, and effectiveness in managing the clinical problem (Lambert et al., 2004; Miranda, 2004; Tacher, Morey, & Craighead, 2005). A treatment option is acceptable if perceived as reasonable and appropriate for managing the problem, non-intrusive, consistent with lifestyle, easy to apply, and effective (Tarrier, Liversidge, & Gregg, 2006).
This conceptualization of treatment preferences implies that individuals understand the treatment options presented and have considered their acceptability prior to expressing their preferences. Accordingly, a valid assessment of preferences requires three steps: presenting information on each treatment option offered to individuals to enhance their understanding of the options (Dwight-Johnson, Unutzer, Sherbourne, Tang, & Wells, 2001); assessing their perception of treatment attributes, which helps delineate the acceptability of the treatment options; and inquiring about their choice of treatment (Tarrier et al., 2006). The information on treatment options should conform with ethical standards applied to securing informed consent. Accordingly, the treatment options are described in terms of: nature of treatment (i.e., its purpose and components or activities comprising it), dose, schedule, mode of delivery, benefits (i.e., effectiveness in producing outcomes), and risks (i.e., discomfort or side effects experienced as a results of treatment), as recommended by Dwight-Johnson et al. (2001), E. Irwin, Arnold, Whelan, Reyno, and Cranton (1999), and Zoeller, Feeny, Cochran, and Pruitt (2003). This systematic assessment of treatment preferences contributes to patients being well informed about treatment options and therefore, in a position to validly express their choice of treatment.
Critical review of preference measures
Although a large number of researchers investigated preferences for treatment in different patient populations, the reports of most studies include minimal details on the measurement of preferences. Where described, the measures differ across studies. In some studies, there was no clear indication that information about treatment options was presented to participants (e.g., Givens et al., 2007; Gum et al., 2006; Heit et al., 2003). If options were presented, the content and format for relaying the information were either not specified or did not conform to recommendations described above. Yet, the content and format for presenting information about treatment options influence participants’ perception of, and hence expressed preferences for treatment (Koedoot et al., 2003; Say & Thompson, 2003; Wragg, Robinson, & Lilford, 2000). For instance, Tarrier et al. (2006) suggested that providing information that compares attributes of the treatment options may affect participants’ perception of treatment acceptability.
Often, treatment preferences are assessed with a single question (e.g., Ananian et al., 2004; Morrow et al., 2007). Single questions do not capture the complex nature of preferences (Bowling & Rowe, 2005), and in particular acceptability of treatment options, raising questions about the accuracy of actual treatment choice. Capturing participants’ expressed choice should be based on careful consideration of the treatment options’ attributes. Further, the content of the single question varies across studies; the questions inquire about participants’ choice or preference of a treatment option (e.g., Fraenkel et al., 2007; Givens et al., 2007), agreement or willingness to receive the treatment (e.g., Hazlett-Stevens et al., 2002), or rank ordering of treatment options in order of preference (e.g., Becker et al., 2007; Tarrier et al., 2006). The extent to which the words and cognitive tasks (e. g., selection, rank ordering) comprising single questions are equivalent in eliciting preferences needs to be determined.
An increasing number of studies involve assessing participants’ perception of treatment acceptability. Two general types of measures are administered in such studies. The first consists of questionnaires requesting participants to rate each treatment option in relation to a set of attributes; a total score is computed as a function of the individual items’ scores to reflect participants’ perception of each option’s acceptability. The Credibility Scale and the Treatment Perceptions Questionnaire (TPQ) illustrate this type of questionnaire. The Credibility Scale captures the extent to which participants find the treatment descriptions to be credible (Becker et al., 2007). It involves rating each treatment option in terms of acceptability, suitability, tolerability, expectation of positive benefit, credibility, efficacy, appropriateness, reasonableness, justifiability, and discomfort (Tarrier et al., 2006). The TPQ requests participants to rate the options for acceptability, believability, and effectiveness (Deacon & Abramowitz, 2005; Morin, Gaulier, Barry, & Kowatch, 1992; Vincent & Lionberg, 2001). Although these questionnaires are simple and easy to use, some of the attributes included may overlap and may be interpreted differently by participants (e.g., credibility, reasonableness, justifiability). In addition, the treatment attribute of convenience, which has been found to influence preferences (e.g., Lambert et al., 2004), was omitted.
The second type of measure used to assess perception of treatment acceptability is derived from the trade-off technique for utility assessment. This technique is exemplified with the standard gamble, time trade-off, and conjoint analysis (also referred to as choice experiment; e.g., Fraenkel et al., 2007; Guenter et al., 2006; Schwartz, Merriman, Reed, & Hammes, 2004). Briefly, the standard gamble and time trade-off techniques require participants to weigh alternative treatment options in terms of a set of favorable (e.g., effectiveness, survival rate) and unfavorable (e.g., risks, side effects) attributes that are purposefully altered by the investigators and presented in hypothetical scenarios. Conjoint analysis is based on similar trade-offs, but the focus is on determining the importance of the attributes in influencing preferences. The application of these techniques within the context of research shows that they are difficult to administer. Participants reported cognitive fatigue and burden, and difficulty in deciding on the importance of attributes and on the trade-offs to make, which results in inconsistent responses across scenarios and a high rate of missing data (Feldman-Stewart & Brundage, 2004; Osoba et al., 2006; Sinnott, Joyce, & Barnett, 2007). In addition, the attributes manipulated across scenarios may not necessarily be the ones of most importance to participants. Further, scenarios with more favorable than unfavorable attributes tend to be preferred, potentially leading to biased expression of preferences (Douglas, Normand, Higginson, & Goodwin, 2005). Accordingly, these techniques are of limited feasibility and utility.
The measure we developed to assess treatment preferences is designed to address the limitations identified above. It presents balanced descriptions of treatment options, highlighting their benefits and risks. Comparisons among options are not presented in the descriptions to prevent any influence on patients’ perceptions, as suggested by Tarrier et al. (2006). The instrument contains items to measure participants’ perception of treatment acceptability, covering relevant attributes found to influence preferences, and global questions inquiring about the option of their preference.
Measure for Assessing Treatment Preferences
The Treatment Acceptability and Preferences (TAP) measure contains descriptions of treatment options, items assessing perception of treatment acceptability, and items inquiring about participants’ choice. The first section presents the description of a treatment option offered within the context of the study and the items for rating acceptability of this option. The second section presents the description of the other option and the items assessing its acceptability. The third section includes items inquiring about preferences. The following details the strategies for developing and the content of the sections comprising the TAP measure.
Description of treatment options
The procedure used to develop the information related to each treatment option offered within the context of the study is described in detail in Sidani et al. (2006). It consists of conducting an extensive review of the literature pertaining to each treatment option, critically appraising findings of studies that evaluated the treatment option, and synthesizing the results to estimate the effectiveness of the treatment options. A description of each treatment was generated from relevant conceptual, clinical, and empirical literature, as well as from the study trial protocol. The conceptual and clinical literature assisted in specifying the treatments’ purposes, components, and specific activities. The empirical literature identified the effectiveness or benefits, and risks or side effects of the treatments. The trial protocol guided the description of the treatment in terms of the therapist’s role, the dose and schedule for giving the treatments.
The information on each treatment option is described in clearly labeled sections covering: the name of the intervention, description of the purpose, components and activities, role of therapist, schedule (i.e., number of sessions, frequency and mode of delivering them), benefits (i.e., effectiveness of the intervention, based on empirical evidence), and risks or discomfort experienced as a result of treatment, for easy recognition. The treatment-related information is presented in non-technical, clear, and simple to understand terms at the sixth grade reading level, in an easy-to-read format using factual statements. Factual statements are necessary to minimize bias in provision of information and ensure subsequent preferences are based on facts about, not misconceptions of, the treatment (Say & Thomson, 2003; Walker, Vincent, Furer, Cox & Kjernisted, 1999). The description of each treatment is focused on information pertinent to the particular treatment; that is, no information is provided that compares any aspect of a treatment to that of another treatment included in the questionnaire.
The treatment options investigated in our study entailed behavioral interventions for the management of chronic insomnia. The first option was sleep education and hygiene (SEH), which consists of providing basic knowledge about sleep processes and functions, and supportive strategies that can be performed to promote sleep (Epstein & Bootzin, 2002). This intervention was offered in a booklet format, and participants could read the booklet at their convenience and apply the strategies to promote sleep on their own. The second option was stimulus control instructions (SCI), which involves activities to perform and avoid around bedtime, with the aim of assisting persons with insomnia to re-associate the bed and bedroom with falling asleep or back to sleep (Bootzin & Epstein, 2000). The third option was sleep restriction therapy (SRT), which limits sleep to a specific time by restricting the amount of time spent in bed based on the person’s baseline sleep assessment (Wohlgemuth & Edinger, 2000). The fourth option was multi-component intervention (MCI), which was comprised of SEH, SCI, and SRT. The last three interventions (i.e., SCI, SRT, and MCI) were offered in four group sessions and two individual telephone sessions led by a trained therapist.
The investigators of three systemic reviews found that the SCI, SRT, and MCI are more effective than the SEH in managing chronic insomnia. SEH is considered as a minimal treatment (M. R. Irwin, Cole, & Nicasso, 2006; Morin, Culbert, & Schwartz, 1994; Morin et al., 2006). Figure 1 illustrates the information on one of the behavioral interventions (SRT) offered in the study and presented in the TAP measure.
Figure 1.
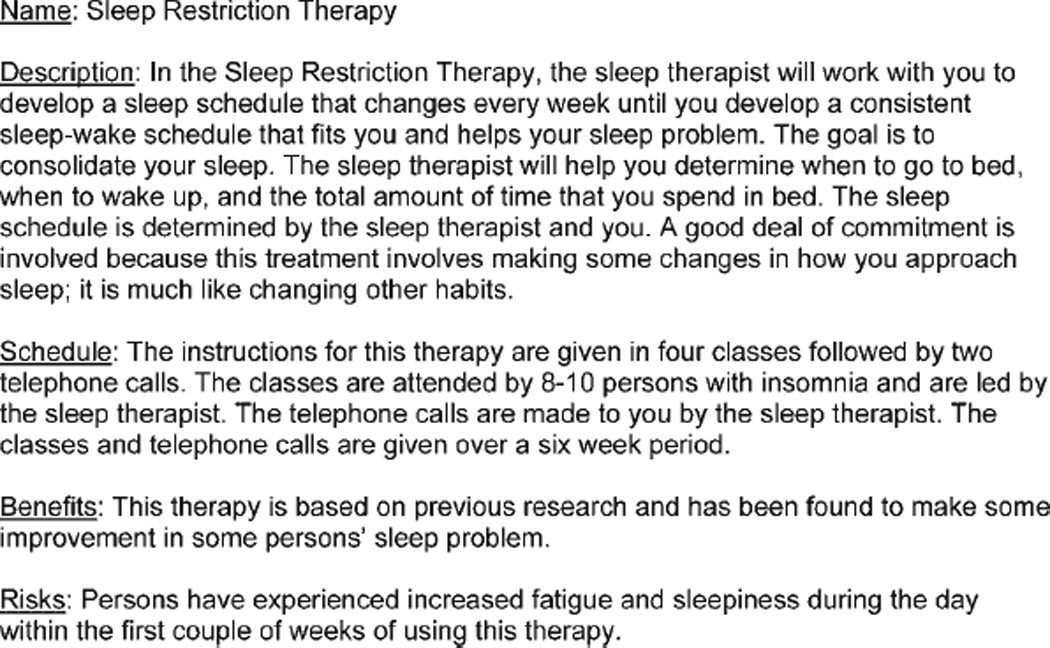
Description of a treatment option.
Items measuring perception of treatment acceptability and preferences
The content of the items we developed to measure participants’ perception of treatment acceptability was consistent with the definition of acceptability and encompassed the treatment attributes found to shape preferences, as described earlier. The specific attributes included in the TAP measure were: (a) appropriateness, that is, the treatment option seems logical in addressing insomnia; (b) suitability to individual life style; (c) effectiveness in managing insomnia; and (d) convenience, which was operationalized as willingness to apply and adhere to the treatment. Discomfort or side effects, assessed in other measures of acceptability, were not mentioned frequently as factors contributing to preferences, which is consistent with findings indicating that patients are willing to accept aggressive treatments, trading side effects for effectiveness (Jansen et al., 2001; Koedoot et al., 2003).
The items are presented immediately following the description of a treatment option. Participants are instructed to rate the option in terms of the four attributes (appropriateness, suitability, effectiveness, and willingness to comply). Each attribute was reflected in an individual item for a total of four items. The ratings were given on a 5-point scale ranging from not at all (0) to very much (4); thus, higher scores indicate perception that the treatment option is appropriate, suitable, and effective, and participants are willing to adhere to it. A total scale score is computed as the mean of the four items’ scores to reflect level of perceived treatment acceptability. The possible range for the total scale score is 0 to 4, with high score reflecting high acceptability.
Two items were generated to elicit treatment preferences. The first item requests participants to state whether or not they had a preference (yes – no) for either of the two treatment options they rated. The second item asks participants with a preference to indicate which option is their choice. The latter item is consistent with single items used in previous research (e.g., Givens et al., 2007).
Research Methods
The data analyzed to test the psychometric properties of the TAP measure were obtained from a multi-site methodological study (Sidani et al., 2003). The overall goal of the study was to determine the utility of the PRCT in maintaining the validity and enhancing the clinical relevance of findings in intervention evaluation research. The PRCT involved inquiring about participants’ preferences for the treatment options under evaluation and accounting for these preferences when allocating participants to the treatment options. Consistent with this design, we assessed eligible participants’ preferences for the treatment options, using the measure we developed, at pre-test prior to treatment assignment. Participants expressing a preference for a particular treatment option were allocated to the option of their choice; those with no preference were randomly assigned to treatment options as described by Sidani et al., (2003) and TenHave et al. (2003), and illustrated with Coward’s (2002) study.
Data on treatment preferences were gathered in the two sites that implemented the PRCT. The behavioral interventions for the management of chronic insomnia were vehicles for testing the utility of the PRCT design. The specific treatment options were the SEH and MCI in site 1, and the SCI and SRT in site 2. All participants rated the two options offered within their respective site and indicated their preferences, using the TAP measure. These data were included in the sub-study evaluating the psychometric properties of the TAP measure. The analysis was conducted on the data obtained for each treatment option separately, as was also done by Tarrier et al. (2006).
Sample
Study participants were persons with chronic insomnia. The eligibility criteria were: (a) community-dwelling, non-institutionalized adults 21 years of age or older, (b) able to read and write English, (c) having complaints of insomnia evidenced by sleep onset latency and/or time awake after sleep onset of 30 minutes or more per night, for a minimum of 3 nights per week, for 3 month duration or more, ascertained with a 14-day daily sleep diary and Insomnia Severity Index completed at baseline. Persons with sleep apnea (self-reported), cognitive impairment ascertained by the Mini-Mental State Exam (MMSE) score < 27, or psychological impairment evidenced by Brief Symptom Inventory (BSI) Global Severity Index T score > 50 were excluded. Cognitive and/or psychological impairment could interfere with participants’ perception of, engagement in, and adherence to the behavioral interventions for managing insomnia. The MMSE and BSI are well established screening instruments (Derogatis & Melisaratos, 1983; Folstein, Folstein, & McHugh, 1975). The Insomnia Severity Index demonstrated acceptable internal consistency reliability and validity (Bastien, Vallières, & Morin, 2001).
Persons with chronic insomnia were recruited through advertisement in local newspapers and newsletters, and by distributing flyers and brochures to community health centers and clinics. The number of eligible participants who completed the measure for assessing treatment preferences was 198 in site 1 and 233 in site 2, for a total of 431. The within-site sample size was adequate for testing the psychometric properties of the measure, based on the rule of 10 cases per item (Streiner & Norman, 2003). The number of items comprising the measure was 4 and of cases needed for the analysis was 40.
The 431 participants who completed the treatment preference measure were middle aged adults, with a mean age of 51 years (± 16). Most were White (80%), married (44%) women (66%). On average, they had 16 years (± 4) of education. Most were employed on a part-time (17%) or full-time (46%) basis; the remaining participants were students (4%) or retired (33%).
Procedure
The study protocol was approved by the Institutional Review Board at the participating institution at each site. Data were collected over a six year period (2001 – 2007). Eligible participants who provided written, informed consent attended a meeting with the research assistant (RA) at the study research office. During the meeting, the participant completed the screening measures (MMSE and BSI), and the RA administered the TAP measure following six steps. First, the RA informed the participant that two treatment options were under investigation and there was an interest in learning about his or her perception of each treatment. Second, the RA read the description of the first treatment option. The RA was instructed to read the description slowly, clearly, and in an unbiased manner, in order to facilitate understanding. Third, the RA explained that the participant was to respond to the items comprising the TAP section measuring treatment acceptability in relation to the option just described. Fourth, the RA read the items and corresponding response options and circled the response option selected by the participant. Fifth, the RA repeated the four steps as they relate to the second treatment option offered at the site. Last, the RA administered the two items of the TAP inquiring about the participant’s preference.
Data Analysis
Descriptive statistics were used to examine the distribution and measures of central tendency and dispersion for the characteristics of the participants and the individual item and total scale scores on the measure of treatment preferences. The psychometric properties were tested separately for each treatment option offered within the sites. The internal consistency reliability of the four items assessing treatment acceptability was determined by examining their item-to-total correlations and estimating the Cronbach’s alpha coefficient. Item-to-total correlation coefficients equal or greater than .30 and alpha coefficients equal or greater than .70 were criteria indicative of acceptable reliability for newly developed measures (Streiner & Norman, 2003).
Validity was examined with three strategies. First, the factorial structure of the four items measuring acceptability was explored using separate responses pertaining to each treatment option within the sites. The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and the Bartlett’s test of sphericity were applied to evaluate the suitability of the data for factor analysis. Consistent with the conceptualization of acceptability described earlier, a one-factor solution was anticipated; the single factor was hypothesized to reflect unidimensionality of treatment acceptability. Accordingly, principal axis factoring was used for factor extraction. The extraction of one factor with similar magnitudes of factor loadings (> .30) would provide evidence of the invariance of the factor structure across treatment options (Teel & Verran, 1991). The second strategy for evaluating validity consisted of examining differences in the means of the total scores on the TAP measure, for the two treatment options rated by participants within each site. These differences were examined with paired t-tests. Significant within-group differences were anticipated to indicate that on average, participants with a preference discriminated among the two treatment options in terms of their acceptability. The third strategy for documenting validity involved comparison of the total scale scores for each treatment option between participants who did and those who did not express a preference for this particular option. Independent sample t-tests were used in this analysis. For instance, for participants in site 1 who rated both the SEH and the MCI, the total scale score reflecting perception of acceptability of the SEH were compared between participants who indicated preference for this option and those who did not. Significant between-group differences in the scores imply that the mean acceptability score for participants who expressed a preference for a treatment option is higher than the mean score for those who did not express a preference for that option. Effect sizes, computed as the standardized groups’ mean difference, were estimated to detect the magnitude of the between-group difference.
Results
Characteristics of Participants
Participants reported experiencing a combination of insomnia types, including difficulty falling asleep and/or difficulty staying asleep. Specifically, they indicated having severe levels of difficulty falling asleep (41%) and difficulty staying asleep (60%). The total score on the Insomnia Severity Index ranged between 4 and 28, with a mean of 17.29 (± 4.24), indicating insomnia of moderate severity.
Preferences for Interventions
Of the 198 participants in site 1, 158 (80%) indicated a preference for a treatment option offered at the site, and 40 (20%) had no preference. Of those with a preference, 122 (77%) selected the MCI and 36 (23%) the SEH. Of the 233 participants in site 2, 220 (94.4%) expressed a preference, and 13 (5.6%) did not express a preference. One hundred and twenty one (55%) participants with a preference selected the SCI, and 99 (45%) selected the SRT as the treatment of their choice.
Perceived Acceptability of Treatment Options
The mean ratings of the four treatment attributes and of the overall acceptability (i.e., total scale score) for each treatment option offered are presented in Table 1. In site 1, all 198 participants rated the SEH and the MCI. In general, they perceived the MCI as more acceptable than the SEH. In site 2, the 233 participants rated the SCI and the SRT, and most viewed the SCI as slightly more acceptable than the SRT.
Table 1.
Mean (SD) Ratings of Treatment Options Within Sites
| Attribute Rated | Site 1 (n = 198) |
Site 2 (n = 233) |
||
|---|---|---|---|---|
| SEH | MCI | SCI | SRT | |
| Suitability | 1.76 (1.10) | 2.38 (0.95) | 2.45 (1.09) | 2.29 (1.22) |
| Appropriateness | 1.95 (1.05) | 2.52 (0.93) | 2.99 (0.93) | 2.81 (1.07) |
| Effectiveness | 1.44 (0.90) | 1.96 (0.84) | 2.23 (0.98) | 2.24 (1.07) |
| Willingness to adhere | 2.60 (1.15) | 3.01 (1.02) | 3.20 (1.01) | 2.87 (1.30) |
| Total scale (acceptability) | 1.96 (0.89) | 2.47 (0.74) | 2.72 (0.84) | 2.55 (0.99) |
Legend: SD: standard deviation; n: number of cases; SEH: sleep education and hygiene; MCI: multi-component intervention; SCI: stimulus control instructions; SRT: sleep restriction therapy
Internal Consistency Reliability
Data obtained from 198 participants who rated the SEH and the MCI, and 233 participants who rated the SCI and SRT were included in this analysis. The four items measuring acceptability of each treatment option offered in this study were internally consistent. The item-total correlation coefficients can be found in Table 2. They all exceeded the .30 criterion. The Cronbach’s alpha coefficient was .86 for the SEH, .80 for the MCI, .84 for the SCI, and .87 for the SRT.
Table 2.
Item-Total Correlation And Factor Loadings For Items Assessing Acceptability
| Item | Item-total correlation | Factor loading | ||||||
|---|---|---|---|---|---|---|---|---|
| SEH | MCI | SCI | SRT | SEH | MCI | SCI | SRT | |
| n | 198 | 198 | 233 | 233 | 198 | 198 | 233 | 233 |
| Suitability | .80 | .68 | .68 | .80 | .90 | .78 | .76 | .89 |
| Appropriateness | .82 | .71 | .71 | .70 | .91 | .84 | .79 | .75 |
| Effectiveness | .64 | .47 | .67 | .72 | .69 | .52 | .75 | .79 |
| Willingness to comply | .59 | .62 | .67 | .69 | .63 | .70 | .75 | .75 |
Legend: n: number of cases; SEH: sleep education and hygiene; MCI: multi-component intervention; SCI: stimulus control instructions; SRT: sleep restriction therapy
Factorial Structure
The results of the factor analysis (Table 2) supported those of internal consistency reliability. For the SEH intervention (rated by n = 198), the data met the assumptions for factor analysis (KMO value = .79, test of sphericity p < .05). One factor was extracted (eigen value = 2.54), accounting for 63% of the variance in the items’ responses. The factor loadings were larger than .60. For the MCI (rated by n = 198), the KMO value was .73 and the p-value associated with the test of sphericity was < .05. One factor was extracted (eigen value = 2.09), accounting for 52% of the variance. All items loaded > .50 on the factor. The assumptions for factor analysis were met for the SCI and the SRT interventions which were both rated by 233 participants (KMO value = .82 and .81, respectively; p-value for sphericitiy test < .05). Similarly, one factor was extracted, with eigen values of 2.34 for the SCI and 2.57 for the SRT, accounting for 58% and 64% of the variance, respectively. The factor loadings were greater or equal to .70. The pattern of findings supported the invariance of the factor structure. The four items capture a common unidimensional concept that of treatment acceptability as hypothesized.
Comparison of Acceptability Scores Between Participants with Preference
The data for this analysis included the responses of the 158 participants in site 1 and 220 participants in site 2 who expressed a preference for one of the treatment options. Table 3 presents the mean acceptability score for participants who had a preference for the specific treatment options offered at each site. In site 1, participants who identified a preference for the MCI had a higher mean acceptability score for this intervention than those who did not have a preference for this intervention (t[59] = 5.33, p < .01; df adjusted for unequal variance). The effect size was 1.02. Similarly, those with a preference for the SHE had higher acceptability score than those who did not prefer this treatment option (t[94] = 7.34, p < .01). The effect size was −1.09. The same pattern of findings was observed in site 2 (Table 4). Participants with an expressed preference for the SCI had a higher acceptability score for this treatment option (t[178] = 2.70, p < .01; effect size = 0.36) and those with a preference for the SRT had a higher acceptability score for this treatment option (t[216] = 9.53, p < .01; effect size = −1.25) than those who did not.
Table 3.
Mean (SD) Acceptability Scores For Participants With Preferences For Specific Treatment Options In Site 1
| Treatment Rated | Treatment of Preference | |
|---|---|---|
| MCI (n = 122) |
SEH (n = 36) |
|
| MCI | 2.63 (.65) | 1.91 (.81) |
| SEH | 1.73 (.86) | 2.62 (.63) |
Legend: SD: standard deviation; n: number of cases; SEH: sleep education and hygiene; MCI: multi-component intervention
Table 4.
Mean (SD) Acceptability Scores For Participants With Preferences For Specific Treatment Options In Site 2
| Treatment Rated | Treatment of Preference | |
|---|---|---|
| SCI (n = 121) |
SRT (n = 99) |
|
| SCI | 2.86 (.71) | 2.56 (.95) |
| SRT | 2.09 (.98) | 3.14 (.65) |
Legend: SD: standard deviation; n: number of cases; SCI: stimulus control instructions; SRT: sleep restriction therapy
Comparisons of Acceptability Scores for Treatment Options
This comparison used paired t-tests to identify differences in ratings given by participants who completed the TAP measure, to the treatment options at each site. In site 1, the mean total acceptability score for the MCI (Table 1) was significantly higher than the mean total acceptability score for the SEH (t[197] = 6.41, p < .01). The effect size was 0.69, implying that the difference in the means was of a moderate magnitude. In site 2, a statistically significant difference (t[232] = 2.26, p < .05) was found in the mean total acceptability scores for the two treatments rated (Table 1). The effect size was 0.20, suggesting that the difference in acceptability of the SCI and SRT was of a small magnitude.
Discussion
The results indicate that the majority (≥ 80%) of participants did have preferences for behavioral interventions for managing chronic insomnia. This finding is consistent with reports of studies of preferences for treatment in persons presenting with various physical and psychological conditions such as pain (e.g., Thomas et al., 2004), angina (Rowe et al., 2005), psoriasis (Fortune, Richards, Griffiths, & Main, 2004), insomnia (Vincent & Lionberg, 2001) and depression (Gum et al., 2006). Across studies, the majority (60 – 100%) of participants have expressed a clear preference for a particular treatment option.
The systematic measure for assessing participants’ acceptability and preferences for treatment that was developed and used in this multi-site study was well received by participants. Participants did not report difficulty understanding the treatment options as described in the measure or responding to the four items measuring treatment acceptability and the two items assessing treatment preferences.
The four items demonstrated internal consistency reliability and factorial validity, implying that they accurately captured the hypothesized concept of treatment acceptability. The items represent attributes of treatments that participants take into consideration when formulating their preferences and selecting a particular treatment option. Participants tend to prefer treatments that are perceived as appropriate, suitable, effective, convenient, and with minimal side effects (Rowe et al., 2005). Investigating participants’ perception of these attributes prior to eliciting their preferences provides a means to systematically guide their treatment selection. Participants were required to carefully consider the combination of these attributes relative to each option offered in order to determine its acceptability and to base their choice of treatment on their perception of treatment acceptability. This strategy facilitates comprehensive assessment of the complex nature of preferences (Bowling & Rowe, 2005), as conceptualized for this study.
The four items showed discriminate validity in that they captured varying levels of acceptability expressed by the same individual to different treatments. This was evidenced by differences in the acceptability scores for the treatment options offered at the two sites. In site 1, the MCI on average, was viewed as more acceptable than the SEH. This was anticipated, as the content and format for delivering the SEH, as described in the measure, reflected minimal treatment (Morin et al., 1994). In contrast, the magnitude of the difference in the level of perceived acceptability of the SCI and SRT offered in site 2, was small. This difference can be explained by the fact that these two treatment options were described as effective and were equally attractive to participants (Morin et al., 1994).
The level of treatment acceptability was related to treatment preferences, where participants with a preference for a treatment option had higher acceptability scores for that option than the other option. This pattern of findings supports the validity of the items and implies that participants do, indeed, consider these treatment attributes when selecting their treatment of preference.
Although the TAP measure is reliable and valid, its application is limited in assessing acceptability and preferences for educational and behavioral treatments with minimal risks or side effects. The importance of the latter attributes, particularly if the side effects are severe, in influencing acceptability and preferences for these types of treatments is not clear and should be investigated in future research.
The TAP measure we developed provides a systematic, reliable and valid instrument for assessing treatment acceptability and preference. The measure can be applied to the assessment of acceptability and preference of other interventions that demonstrate effectiveness in managing different clinical problems. The measure has been adapted and is currently being used to assess acceptability and preferences for educational and behavioral interventions for HIV prevention (Miranda, 2008), and for insomnia treatment acceptability and preferences of Iraq and Afghanistan combat veterans (Epstein, Babcock-Parziale, & Haynes, 2008). The administration of the measure will contribute to a comprehensive and accurate assessment of treatment acceptability and preferences, which will improve the validity of conclusions of studies investigating determinants of preferences and/or the impact of treatment preferences on enrollment, participation in and adherence to the treatment, attrition, and effectiveness of the treatment in achieving the outcomes. The utility of the instrument for assessing acceptability and preferences for treatment in day-to-day practice should be investigated in future work. The TAP measure could guide assessment of patients’ preferences for intervention, which is a core component of patient-centered care.
Acknowledgments
Funding: National Institutes of Health – National Institute of Nursing Research (NR05075). Partially supported by resources provided by the Phoenix Veterans Affairs Health Care System
Contributor Information
Souraya Sidani, School of Nursing, Ryerson University, Toronto, Ontario.
Dana R. Epstein, Nursing Service / Research, Phoenix Veterans Affairs Health Care System, Phoenix, Arizona.
Richard R. Bootzin, Department of Psychology, University of Arizona, Tucson, Arizona.
Patricia Moritz, School of Nursing, University of Colorado Health Sciences Center, Denver, Colorado.
Joyal Miranda, Nursing, University of Toronto, Toronto, Ontario.
References
- Adamson SJ, Sellman DJ, Dore GM. Therapy preference and treatment outcome in clients with mild to moderate alcohol dependence. Drug & Alcohol Review. 2005;24:209–216. doi: 10.1080/09595230500167502. [DOI] [PubMed] [Google Scholar]
- Ananian P, Houvenaeghel G, Protiere C, Rouanet P, Arnaud S, Moatti JP, et al. Determinants of patients’ choice of reconstruction with mastectomy for primary breast cancer. Annals of Surgical Oncology. 2004;11:762–771. doi: 10.1245/ASO.2004.11.027. [DOI] [PubMed] [Google Scholar]
- Awad MA, Shapiro SH, Lund JP, Feine JS. Determinants of patients’ treatment preferences in a clinical trial. Community Dental & Oral Epidemiology. 2000;28:119–125. doi: 10.1034/j.1600-0528.2000.028002119.x. [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Becker CB, Darius E, Schaumberg K. An analog study of patient preferences for exposure versus alternative treatments of posttraumatic stress disorder. Behaviour Research & Therapy. 2007;45:2861–2873. doi: 10.1016/j.brat.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Bootzin RR, Epstein DR. Stimulus control instructions. In: Lichstein KL, Morin CM, editors. Treatment of late-life insomnia. Thousand Oaks, CA: Sage; 2000. pp. 167–184. [Google Scholar]
- Bowling A, Rowe G. “You decide doctor”. What do patient preference arms in clinical trials really mean? Journal of Epidemiology & Community Health. 2005;59:914–915. doi: 10.1136/jech.2005.035261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, et al. The acceptability of treatment of depression among African-American, Hispanic and White primary care patients. Medical Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Salzer MS. The conflict between random assignment and treatment preference: Implications for internal validity. Evaluation & Program Planning. 2003;26:109–121. doi: 10.1016/S0149-7189(03)00014-4. [DOI] [PubMed] [Google Scholar]
- Coward DD. Partial randomized design in a support group intervention study. Western Journal of Nursing Research. 2002;24:406–421. doi: 10.1177/01945902024004008. [DOI] [PubMed] [Google Scholar]
- Deacon BJ, Abramowitz JS. Patients’ perceptions of pharmacological and cognitive-behavioral treatments for anxiety disorders. Behavior therapy. 2005;36:139–145. doi: 10.1016/j.brat.2006.04.010. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An Introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Douglas HR, Normand CE, Higginson IJ, Goodwin DM. A new approach to eliciting patients’ preferences for palliative day care: The choice experiment method. Journal of Pain & Symptom Management. 2005;29:435–445. doi: 10.1016/j.jpainsymman.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, Unutzer J, Sherbourne C, Tang L, Wells KB. Can quality improvement programs for depression in primary care address patient preferences for treatment? Medical Care. 2001;39:934–944. doi: 10.1097/00005650-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Epstein DR, Babcock-Parziale JL, Haynes PL. Insomnia treatment preferences of Operation Enduring Freedom/Operation Iraqi Freedom Veterans: Preliminary findings. Sleep. 2008;31:A241. [Google Scholar]
- Epstein DR, Bootzin RR. Insomnia. Nursing Clinics of North America. 2002;37:611–631. doi: 10.1016/s0029-6465(02)00028-2. [DOI] [PubMed] [Google Scholar]
- Feldman-Stewart D, Brundage MD. Challenges for designing and implementing decision aids. Patient Education & Counseling. 2004;54:265–273. doi: 10.1016/j.pec.2003.09.007. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fortune DG, Richards HL, Griffiths CE, Main CJ. Targeting cognitive-behavior therapy to patients’ implicit model of psoriasis: results from a patient preference controlled trial. British Journal of Clinical Psychology. 2004;43:65–82. doi: 10.1348/014466504772812977. [DOI] [PubMed] [Google Scholar]
- Fraenkel L, Gulanski B, Wittnik D. Patient willingness to take teriparatide. Patient Education & Counseling. 2007;65:237–244. doi: 10.1016/j.pec.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Givens JL, Houston TK, Van Voorhees BW, Ford DE, Cooper LA. Ethnicity and preferences for depression treatment. General Hospital Psychiatry. 2007;29:182–191. doi: 10.1016/j.genhosppsych.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Guentner K, Hoffman LA, Happ MB, Kim Y, Dabbs AD, Mendelsohn AB, et al. Preferences for mechanical ventilation among survivors of prolonged mechanical ventilation and tracheostomy. American Journal of Critical Care. 2006;15:65–77. [PubMed] [Google Scholar]
- Gum AM, Arean PA, Hunkeler E, Tang L, Katon W, Hitchcock P, et al. Depression treatment preferences in older primary care patients. The Gerontologist. 2006;4:14–22. doi: 10.1093/geront/46.1.14. [DOI] [PubMed] [Google Scholar]
- Hazlett-Stevens H, Craske MG, Roy-Byrne PP, Sherbourne CD, Stein MB, Bystritsky A. Predictors of willingness to consider medication and psychosocial treatment for panic disorder in primary care patients. General Hospital Psychiatry. 2002;24:316–321. doi: 10.1016/s0163-8343(02)00204-9. [DOI] [PubMed] [Google Scholar]
- Heit M, Rosenquist C, Culligan P, Graham C, Murphy M, Shott S. Predicting treatment choice for patients with pelvic organ prolapse. The American College of Obstetrics & Gynecology. 2003;101:1279–1284. doi: 10.1016/s0029-7844(03)00359-4. [DOI] [PubMed] [Google Scholar]
- Howard L, Thornicroft G. Patient preference and randomized controlled trials in mental health research. British Journal of Psychiatry. 2006;188:303–304. doi: 10.1192/bjp.188.4.303. [DOI] [PubMed] [Google Scholar]
- Irwin E, Arnold A, Whelan TJ, Reyno LM, Cranton P. Offering a choice between two adjuvant chemotherapy regimens: a pilot study to develop a decision aid for women with breast cancer. Patient Education & Counseling. 1999;37:283–291. doi: 10.1016/s0738-3991(98)00117-7. [DOI] [PubMed] [Google Scholar]
- Irwin MR, Cole JC, Nicassio PM, Smith MT, Perlis ML. Comparative meta-analysis of behavioral interventions for insomnia and their efficiency in middle-aged adults and in older adults 55+ years of age. Health Psychology. 2006;25:3–19. doi: 10.1037/0278-6133.25.1.3. [DOI] [PubMed] [Google Scholar]
- Janevic MR, Janz NK, Dodge JA, Lin X, Pan W, Sinco BR, et al. The role of choice in health education intervention trials: a review and case study. Social Science & Medicine. 2003;56:1581–1594. doi: 10.1016/s0277-9536(02)00158-2. [DOI] [PubMed] [Google Scholar]
- Jansen SJ, Kievit J, Nooij MA, de Haes JC, Overpelt IM, van Slooten H, et al. Patients’ preferences for adjuvant chemotherapy in early-stage breast cancer: is treatment worthwhile? British Journal of Cancer. 2001;84:1577–1585. doi: 10.1054/bjoc.2001.1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaber-Moffett JA, Jackson DA, Richmond S, Hahn S, Coulton S, Farrin A, et al. Randomised trial of a brief physiotherapy intervention compared with usual physiotherapy for neck pain patients: outcomes and patients’ preference. British Medical Journal. 2004;330:75. doi: 10.1136/bmj.38286.493206.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koedoot CG, de Haan RJ, Stiggelbout AM, Stalmeier PFM, de Graeff A, Bakker PJM, et al. Palliative chemotherapy or best supportive care? A prospective study explaining patients’ treatment preference and choice. British Journal of Cancer. 2003;89:2219–2226. doi: 10.1038/sj.bjc.6601445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert N, Rowe G, Bowling A, Ebrahim S, Laurence M, Dalrymple J, et al. Reasons underpinning patients’ preferences for various angina treatments. Health Expectations. 2004;6:246–256. doi: 10.1111/j.1369-7625.2004.00282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ. Mental health treatment preferences of primary care patients. Journal of Behavioral Medicine. 2005;28:581–586. doi: 10.1007/s10865-005-9019-2. [DOI] [PubMed] [Google Scholar]
- Macias C, Barreira P, Hargreaves W, Bickman L, Fisher W, Aronson E. Impact of referral source and study applicants’ preference for randomly assigned service on research enrollment, service engagement, and evaluative outcomes. American Journal of Psychiatry. 2005;162:781–787. doi: 10.1176/appi.ajp.162.4.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millat B, Borie F, Fingerhut A. Patients’ preference and randomization: new paradigm of evidence-based clinical research. World Journal of Surgery. 2005;29:596–600. doi: 10.1007/s00268-005-7920-z. [DOI] [PubMed] [Google Scholar]
- Mills N, Metcalfe C, Ronsmans C, Davis M, Lane JA, Sterne JAC, et al. A comparison of socio-demographic and psychological factors between patients consenting to randomisation and those selecting treatment (the ProtecT study) Contemporary Clinical Trials. 2006;27:413–419. doi: 10.1016/j.cct.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Miranda J. An exploration of participants’ treatment preferences in a partial RCT. Canadian Journal of Nursing Research. 2004;36(3):100–114. [PubMed] [Google Scholar]
- Miranda J. Patient preferences for HIV prevention interventions; Poster session, XVII International AIDS Conference; Mexico City, Mexico. 2008. Aug, [Google Scholar]
- Montgomery AA, Fahey T. How do patients’ treatment preferences compare with those of clinicians? Quality in Health Care. 2001;10(Suppl1):i39–i43. doi: 10.1136/qhc.0100039... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia: Update of the recent evidence (1998–2004) Sleep. 2006;29:1398–1414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- Morin CM, Culbert JP, Schwartz SM. Nonpharmacological interventions for insomnia: a meta-analysis of treatment efficacy. American Journal of Psychiatry. 1994;151:1172–1180. doi: 10.1176/ajp.151.8.1172. [DOI] [PubMed] [Google Scholar]
- Morin CM, Gaulier B, Barry T, Kowatch RA. Patients’ acceptance of psychological and pharmacological therapies for insomnia. Sleep. 1992;15:302–305. doi: 10.1093/sleep/15.4.302. [DOI] [PubMed] [Google Scholar]
- Morrow DG, Weiner M, Steinley D, Young J, Murray MD. Patient's health literacy and experience with instructions: Influence preferences for heart failure medication instructions. Journal of Aging & Health. 2007;19:575–593. doi: 10.1177/0898264307304448. [DOI] [PubMed] [Google Scholar]
- Osoba D, Hsu MA, Copley-Merriman C, Coombs J, Johnson FR, Hauber B, et al. Stated preferences of patients with cancer for health-related quality-of-life (HRQOL) domains during treatment. Quality of Life Research. 2006;15:273–283. doi: 10.1007/s11136-005-0580-5. [DOI] [PubMed] [Google Scholar]
- Rowe G, Lambert N, Bowling A, Ebrahim S, Wakeling I, Thomson R. Assessing patients’ preferences for treatment for angina using a modified repertory grid method. Social Science & Medicine. 2005;60:2585–2595. doi: 10.1016/j.socscimed.2004.10.019. [DOI] [PubMed] [Google Scholar]
- Say RE, Thomson R. The importance of patient preferences in treatment Decisions-challenges for doctors. British Medical Journal. 2003;327:542–545. doi: 10.1136/bmj.327.7414.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz CE, Merriman MP, Reed GW, Hammes BJ. Measuring patient treatment preferences in end-of-life care research: Applications for advance care planning interventions and response shift research. Journal of Palliative Medicine. 2004;7:233–245. doi: 10.1089/109662104773709350. [DOI] [PubMed] [Google Scholar]
- Sidani S, Epstein D, Miranda J. Eliciting patient treatment preferences: A strategy to integrate evidence-based and patient-centered care. Worldviews on Evidence-Based Nursing. 2006;3:116–123. doi: 10.1111/j.1741-6787.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- Sidani S, Epstein DR, Mortiz P. An alternative paradigm for clinical nursing research: an exemplar. Research in Nursing & Health. 2003;26:244–255. doi: 10.1002/nur.10086. [DOI] [PubMed] [Google Scholar]
- Sinnott PL, Joyce VR, Barnett PG. Preference measurement in economic analysis. Guidebook. Menlo Park, CA: VA Palo Alto, Health Economics Resource Center; 2007. [Google Scholar]
- Stalmeier PF, van Tol-Geerdink JJ, van Lin EN, Schimmel E, Huizenga H, van Daal WA, et al. Doctors' and patient's preferences for participation and treatment in curative prostate cancer radiotherapy. Journal of Clinical Oncology. 2007;25:3096–3100. doi: 10.1200/JCO.2006.07.4955. [DOI] [PubMed] [Google Scholar]
- Streiner DL, Norman GR. Health measurement scales. A practical guide to their development and use. 3rd ed. Oxford, UK: Oxford University Press; 2003. [Google Scholar]
- Tacher JA, Morey E, Craighead WE. Using patient characteristics and attitudinal data to identify depression treatment preference groups: A latent-class model. Depression and Anxiety. 2005;21:47–54. doi: 10.1002/da.20057. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Liversidge T, Gregg L. The acceptability and preference for the psychological treatment of PTSD. Behavior Research & Therapy. 2006;44:1643–1656. doi: 10.1016/j.brat.2005.11.012. [DOI] [PubMed] [Google Scholar]
- Teel C, Verran JA. Factor comparison across studies. Research in Nursing & Health. 1991;14:67–72. doi: 10.1002/nur.4770140110. [DOI] [PubMed] [Google Scholar]
- TenHave TR, Coyne J, Salzer M, Katz I. Research to improve the simple randomized clinical trial. General Hospital Psychiatry. 2003;25:115–123. doi: 10.1016/s0163-8343(02)00275-x. [DOI] [PubMed] [Google Scholar]
- Thomas E, Croft PR, Paterson SM, Dziedzic K, Hay EM. What influences participants’ treatment preference and can it influence outcome? Results from a primary care-based randomized trial for shoulder pain. British Journal of General Practice. 2004;54:93–96. [PMC free article] [PubMed] [Google Scholar]
- Vincent N, Lionberg C. Treatment preference and patient satisfaction in chronic insomnia. Sleep. 2001;24:411–417. doi: 10.1093/sleep/24.4.411. [DOI] [PubMed] [Google Scholar]
- Walker J, Vincent N, Furer P, Cox B, Kjernisted K. Treatment preference in hypochondriasis. Journal of Behavioral Therapy & Experimental Psychiatry. 1999;30:251–258. doi: 10.1016/s0005-7916(99)00027-0. [DOI] [PubMed] [Google Scholar]
- Wensig M, Elwyn G. Methods for incorporating patients’ views in health care. British Medical Journal. 2003;326:877–879. doi: 10.1136/bmj.326.7394.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohlgemuth WK, Edinger JD. Sleep restriction therapy. In: Lichstein KL, Morin CM, editors. Treatment of late-life insomnia. Thousand Oaks, CA: Sage; 2000. pp. 147–166. [Google Scholar]
- Wragg JA, Robinson EJ, Lilford RJ. Information presentation and decisions to enter clinical trials: A hypothetical trial of hormone replacement therapy. Social Science & Medicine. 2000;51:453–462. doi: 10.1016/s0277-9536(99)00477-3. [DOI] [PubMed] [Google Scholar]
- Zoeller LA, Feeny NC, Cochran B, Pruitt L. Treatment choice for PTSD. Behaviour Research & Therapy. 2003;41:879–886. doi: 10.1016/s0005-7967(02)00100-6. [DOI] [PubMed] [Google Scholar]


