Abstract
Background:
The workplace is increasingly being used as a setting for health promotion and preventive health activities; not only to prevent occupational injury, but to assess and improve people's overall health.
Objective:
This study aims at developing and implementing a healthy workplace model in a software industry of Puducherry.
Methods:
Operations research was carried out in a purposively selected industry in Puducherry. The study was planned in four phases-baseline assessment and risk profiling, intervention, final evaluation and dissemination of results. Baseline evaluation of employees (n = 907) was done by a self-administered questionnaire to collect sociodemographic variables and risk factor profile using noncommunicable diseases (NCDs) LITE Proforma.
Results:
Healthy workplace committee comprising of several stakeholders was formed, and a formal launch of the health awareness campaign was organized. Broad themes for health education sessions and support activities were identified. Risk profiling of employees showed high levels of risk factors and morbidity-more than 15% were found to be hypertensive and around 55% were obese. Stress and back ache were reported by almost half of the respondents. Modifications in the workplace targeting physical and psychosocial work environment were suggested to the committee, as part of the initiative. This study has demonstrated the feasibility of developing and implementing a healthy workplace model in South India. This model can be replicated or adapted in other industries for health promotion and prevention of NCDs.
Conclusion:
Dedicated and concerted efforts of the management consistent with the requirements of safety, health and environment at work place with appropriate support from the health system can improve the quality of work and working life.
Keywords: Health promotion, healthy workplace, industry, noncommunicable diseases
INTRODUCTION
A healthy workplace is one in which workers and managers collaborate to use a continual improvement process to protect and promote the health, safety and well-being of all workers and the sustainability of the workplace.[1] This definition reflects how understanding of occupational health has evolved from an almost exclusive focus on the physical work environment to inclusion of psychosocial and personal health practice factors. The workplace is increasingly being used as a setting for health promotion and preventive health activities; not only to prevent occupational injury, but to assess and improve people's overall health.
In the past few decades, the nature of work in many organizations has been radically transformed due to growth in the use of information technology. While advancements in technology have minimized or eliminated some hazards at the workplace, new risks can emerge in their place which needs to be addressed.[2] High prevalence of risk factors and morbidity due to noncommunicable diseases (NCDs) has been reported among Indian industrial workers.[3,4]
Workers represent half the world's population and are the major contributors to economic and social development. Their health is determined not only by workplace hazards but also by social and individual factors and access to health services. Large gaps exist between and within countries with regard to the health status of workers, and only a small minority of the global workforce has access to occupational health services.
Globally, 2 million people die each year as a result of occupational accidents and work-related illnesses or injuries. Another 268 million nonfatal workplace accidents result in an average of three lost workdays per casualty, as well as 160 million new cases of work-related illness each year.[5] In 2000, selected occupational risk factors (risks for injuries, carcinogens, airborne particulates, ergonomic risks for back pain, and noise) were responsible worldwide for 37% of back pain, 16% of hearing loss, 13% of chronic obstructive pulmonary disease, 11% of asthma, 8% of injuries, 9% of lung cancer, 2% of leukemia, and about 100% of pneumoconioses and mesothelioma.[6]
Reducing employee health risks requires changes in job designs, workplace culture, organizational systems, management practices and most importantly, attitude of the employees and employers. Health camps for employees and traditional workplace health promotion programs focus narrowly on employee health. The private sector has a responsibility to ensure the health and to promote the health and well-being of employees, their families, and communities. This is being increasingly realized and facilitated as part of their corporate social responsibility.
The National Program for Prevention and Control of Diabetes, cardiovascular disease (CVD) and stroke has given a broad framework for healthy workplaces practices.[7] The healthy workplace model is built on the foundation of a healthy workplace committee (HWC) with three pillars of physical work environment, promoting healthy practices and psychosocial work environment. This calls for involvement of the District Health Mission, District Industry Centers and Directorates of Industry and Labor. However, since each organization is unique, the healthy workplace strategy must also be designed to fit the organization's culture, working conditions and employee characteristics. Very few studies are available in the Indian context which has implemented this strategy.[8] Hence, this study aims at developing and implementing a healthy workplace model in a software industry of Puducherry.
METHODS
Study setting
Puducherry has more than 7000 manufacturing and service units representing a cross-section of industries in seven well established industrial estates. A number of hardware and software companies function in this region. The oldest and largest of these firms was selected purposively for this study.
Study design
Operations research was designed and carried out in a selected software company during 2013–2014. Official permission for implementation of healthy workplace intervention was obtained from the company management. The study was approved by the Institute Scientific and Ethics Review board. Strategy for implementation of the healthy workplace model is presented in Figure 1.
Figure 1.
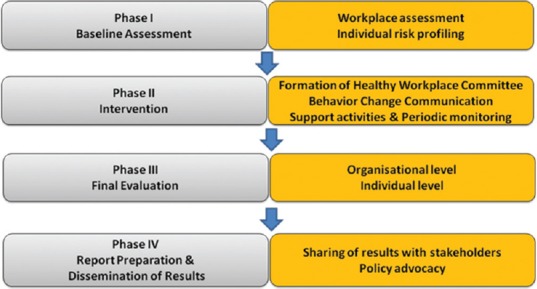
Strategic framework for implementation of the intervention
Details of the program
The study was planned in four phases-baseline assessment and risk profiling, intervention, final evaluation and dissemination of results. In the baseline assessment, all employees in the company were included in the study, after taking informed consent.
Baseline evaluation of employees was done by a self-administered questionnaire to collect sociodemographic variables and risk factor profile using NCDs LITE Proforma.[8] This was, followed by anthropometric measurements such as height, weight, body mass index and blood pressure recording. Measures were taken to ensure confidentiality of the data collected.
The intervention consisted of formation of HWC and intensive health promotion activities every month as per the theme decided, modifications in the organization and workplace, supportive activities, and periodic monitoring. Final evaluation would be done at the end of 1-year intervention to measure the risk factor levels, anthropometric and blood pressure measures.
RESULTS
Baseline assessment
Situation analysis of the workplace was done to collect the baseline information on existing policies for healthy workplace, to identify organizational strengths, weakness, opportunities, and threats. Workplace assessment focused on the physical work environment (canteen facilities, barriers for physical fitness like usage of lifts), healthy practices promotion strategies (no smoking policies, health education materials on display) and psychosocial work environment (stress management training, counseling, support services).
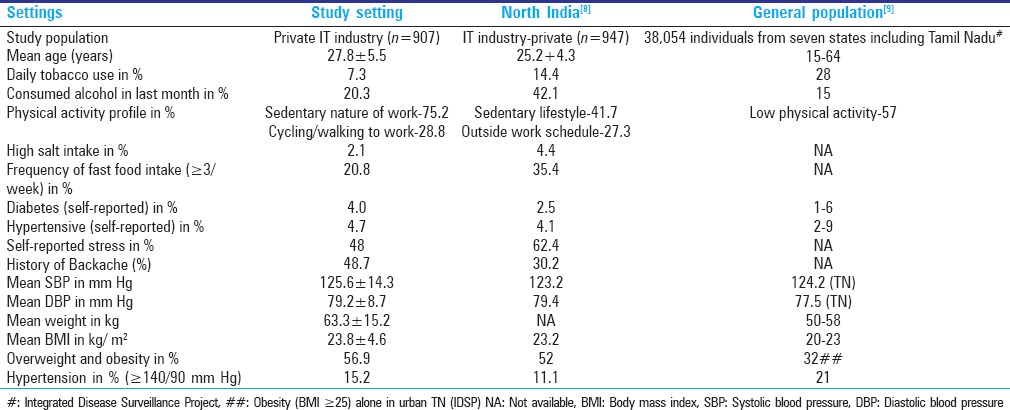
After obtaining consent, baseline evaluation was done for all employees, using a self-administered questionnaire and anthropometry. A total of 907 employees out of n participated in the baseline assessment. Findings from the baseline risk assessment were shared with the committee members and circulated among the staff through the intranet [Table 1]. Results were presented at the group level without disclosing the identity of individuals. However, individuals found to have a greater risk were encouraged to communicate with the investigators/medical team of the company and were referred to the tertiary hospital.
Table 1.
Comparison of baseline characteristics at the study setting, industrial population in North India and general population
Intervention
Formation of healthy workplace committee
Initial sensitization of stakeholders on emerging epidemic of NCDs in industrial settings was done by the investigators. It was proposed to form a core committee with key stakeholders such as top management, human resource (HR) managers, representatives from employees union, and academicians (investigators). Another sub-committee was planned with representative members from the various divisions in their organization. Available models for health promoting workplaces were discussed. Drafting of a healthy workplace promotion policy and action plan was agreed upon by all the members. After the preliminary liaison meet, members of both the committees were finalized. Strategy for healthy workplace policy was proposed, and plan of activities for behavior change communication, and organizational support was discussed.
Formal launch of the campaign
A competition was organized among the employees for developing logo for the campaign. This was evaluated by the core committee for creativity, applicability and content validity [Figure 2]. The healthy workplace initiative was formally launched in the presence of the HWC, the employees, and management. Several logistic issues (channel of dissemination, type of support activities, maximizing employee participation) and operational problems (impact of time, effect on production) were raised and discussed in the committee meetings.
Figure 2.

Logo developed for the campaign by the stakeholders
Behavior change communication
Broad themes for health education sessions were identified by the HWC, e.g. prevention of diseases such as diabetes, CVDs, stroke, cancer, musculoskeletal diseases. Based on the content and sequence, themes for each month were identified targeting a specific risk factor every month. Channels of communication were identified, and dissemination protocols were laid [Table 2].
Table 2.
Plan for modules for health education among the employees
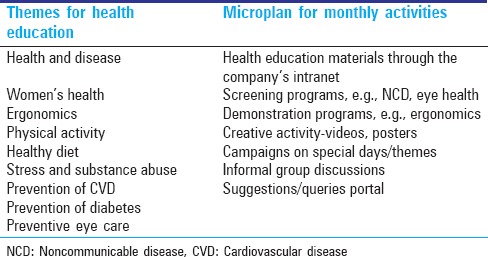
Health education materials were developed by subject experts with adequate illustrations and practical advices and examples. A total of 22–25 sub-topics were developed in this manner for the theme identified for each month. These were disseminated through their intranet portal for accessed by the employees on a daily basis. The content was also summarized in the local language (Tamil) as well for better reach among the employees. Health promotion materials such as banners, posters and pamphlets focusing on these themes were developed and put up on prominent places in the workplace.
Support activities
Demonstration programs have been organized on ergonomics, targeting prevention of work-related musculoskeletal disorders. Multiple sessions were planned in such a way that all employees belonging to different shifts were benefitted. Moreover, these were done at the respective floors and close to their workstations for the greater benefit to the employees and avoid disruption of the regular functioning of the company. Volunteers have been identified for each division and floor wise, in order to facilitate group discussions and support behavior change. Monthly meetings would be organized with the employees for health promotion on lifestyle changes such as smoking cessation, regular physical activity, healthy diet (fruits, vegetables, fibers intake), reduction of alcohol consumption and high salt intake. Eye camps and other screening programs have been planned.
Modifications in the workplace
Based on the workplace assessment measures were suggested to increase the access and reach of the campaign. With regards to the physical work environment, canteen facilities were reviewed, and suggestions were given to increase vegetable content and provide fruit options in the staff canteen. Need for a gymnasium or fitness center within the campus was emphasized. Alternately, formation of walking groups was also suggested to facilitate group dynamics and behavior change. Favorable measures have been taken by the management, and this was well received by the employees. Healthy practices promotion strategies were adequately enforced with respect to tobacco cessation and no-smoking policies. However, other NCD risk factors would be addressed as part of the monthly campaigns. Psychosocial work environment was taken care of by the HRs division of the company. It was decided to offer capacity building programs for the executives with regards to certain areas like stress management training and counseling.
Periodic monitoring
The committee met every 3 months to identify key intervention areas, plan strategies, and periodic review of activities. Microplan of activities for the subsequent month is developed. Feedback is obtained from members of different departments/units.
Final evaluation
At the end of 1-year intervention, the overall effectiveness of the project will be assessed both at the individual level and organizational level. At the end of the intervention period, the feasibility of the project and effectiveness will be shared with the management, employees and other industries.
DISCUSSION
This study has revealed that it is feasible to develop a healthy workplace model in industrial settings. There are several factors which facilitated successful program implementation.
HWC is the prime mover that takes the planning, coordinating and monitoring role in this program. It is essential to offer training programs for senior and mid-level management to carry out this role effectively, even with minimal external support
Support from management at all levels is essential to engage in discussions in creating health and enabling environments. Orchestrating systemic change toward workplace health promotion requires clarity of vision, strong commitment, cooperation, and involvement
Support from staff by way of cooperation, participation, volunteering and setting examples by leading are various dimensions of their involvement
Tracking the results for employees, the organization, and the community is another crucial component of such programs. Demonstration of change and the facilitating and inhibiting factors sets a process which aims for continual improvement.
High levels of risk factors and morbidity as in other studies among industrial population was noted in this study. Baseline risk assessment showed that more than 15% and around 55% of the employees were found to be hypertensive and obese during the baseline survey. Stress and back ache were reported by almost half of the respondents. This situation requires modifications in the workplace targeting physical and psychosocial work environment and health promotion, in order to prevent the consequences of NCDs and ill health in this young working group. The strategy on occupational health for all, endorsed by the World Health Assembly of 1995, emphasized the importance of primary prevention and encouraged countries to establish national policies and programs for occupational health, with guidance and support from WHO and International Labor Organization. This was, followed by the Global Plan of Action on Workers Health (GPA 2008–2017) with the objectives of devising and implementing policy instruments on workers' health, protecting and promoting health at the workplace, improving access to occupational health services, providing evidence for action and practice and incorporating workers' health into other policies.[10] In the Indian context, occupational health has received more focus with the announcement of the National Policy on Safety, Health, and Environment at Work Place by the Ministry of Labor and Employment, in 2009.[2]
This health promoting workplace model is sustainable with minimal technical expertise and support, as there is a strong commitment from the management. There is a need for capacity building programs to train the HR personnel of such companies to support such programs. The employees' participation can be increased when the health promotion activities cater to a wide audience on topics covering various issues. An integrated model encompassing communicable, and NCDs, including women and child health and other topics aimed at improving health literacy will be greatly beneficial to them.
Continuous enhancement of community awareness regarding safety, health, and environment at workplace is also useful. Evidence building on the action through such research cum demonstration projects is important to advocate for policy change in the relevant areas. Dissemination of these findings can be encouraging to other companies to set up a similar mechanism in their workplaces, ultimately aiming toward increased productivity. This model can be presented to the Confederation of Indian Industry (CII), industrial bodies and other stakeholders for opening potential avenues for widespread implementation. This is already being adopted in our setting, partly by the local chapters of CII. It may not be feasible to implement the entire model across settings due to resource constraints, logistic issues and applicability and many other reasons. However, a stepwise approach of core, expanded and optional modules can be further developed.
At the national level, a multi-disciplinary approach with the active involvement of all stakeholders needs to be adopted, and measures to improve the prevailing occupational safety and health in the country need to be implemented.[11] Developing appropriate standards and codes of practices, enabling legislation and effective enforcement machinery are requisite measures by the government targeting workers' safety, health and environment. Encouraging employers to set up suitable health, safety management system and adopt “corporate social responsibility” and due recognition by accreditation, financial and nonfinancial incentives would be a great impetus for the companies and have a major impact on work performance and productivity.
CONCLUSION
Our study has demonstrated the feasibility of developing and implementing a Healthy Workplace Model in South India. This model can be replicated or adapted in other industries for health promotion and prevention of NCDs. Dedicated and concerted efforts of the management consistent with the requirements of safety, health and environment at work place with appropriate support from the health system can improve the quality of work and working life.
ACKNOWLEDGMENT
The authors would like to acknowledge the presence and contribution made by Dr. KC Premarajan, Dr. Sonali Sarkar from Department of PSM, JIPMER, during the first stakeholders meeting.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization. Healthy Workplaces: A Model for Action: For Employers, Workers, Policymakers and Practitioners. 2010. [Last cited on 2014 Jun 23]. Available from: http://www.who.int/occupational_health/publications/healthy_workplaces_model.pdf .
- 2.National Policy on Safety, Health and Environment at Work Place. [Last cited on 2014 Jun 24]. Available from: http://www.ilo.org/wcmsp5/groups/public/--asia/--ro.bangkok/--sro-bangkok/documents/policy/wcms_182422.pdf .
- 3.Reddy KS, Prabhakaran D, Chaturvedi V, Jeemon P, Thankappan KR, Ramakrishnan L, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. 2006;84:461–9. doi: 10.2471/blt.05.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohan V, Deepa M, Farooq S, Prabhakaran D, Reddy KS. Surveillance for risk factors of cardiovascular disease among an industrial population in southern India. Natl Med J India. 2008;21:8–13. [PubMed] [Google Scholar]
- 5.International Labour Organization. Facts on Safety at Work. 2005. Apr, [Last cited on 2014 Jun 23]. Available from: http://www.ilo.org/wcmsp5/groups/public/--dgreports/--dcomm/documents/publication/wcms_067574.pdf .
- 6.Fingerhut M, Nelson DI, Driscoll T, Concha-Barrientos M, Steenland K, Punnett L, et al. The contribution of occupational risks to the global burden of disease: Summary and next steps. Med Lav. 2006;97:313–21. [PubMed] [Google Scholar]
- 7.National Programme for Prevention and Control of Diabetes, Cardiovascular Disease and Stroke. [Last cited on 2014 Jun 24]. Available from: http://www.searo.who.int/india/topics/cardiovascular_diseases/NCD_Resources_COMBINED_MANUAL_for_medical_officer.pdf .
- 8.Thakur JS, Bains P, Kar SS, Wadhwa S, Moirangthem P, Kumar R, et al. Integrated healthy workplace model: An experience from North Indian industry. Indian J Occup Environ Med. 2012;16:108–13. doi: 10.4103/0019-5278.111750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Indian Council of Medical Research. IDSP Non Communicable Disease Risk Factors Survey Phase-I Report. 2007-08. [Last cited on 2014 Sep 15]. Available from: http://www.icmr.nic.in/final/IDSP-NCD%20Reports/Summary.pdf .
- 10.World Health Organisation. About Occupational Health. WHO. [Last cited on 2014 Jun 23]. Available from: http://www.who.int/occupational_health/about/en/
- 11.Report of the Working Group on Occupational Safety and Health. [Last cited on 2014 Jun 24]. Available from: http://www.ilo.org/wcmsp5/groups/public/--ed_protect/--protrav/--safework/documents/policy/wcms_211795.pdf .


