Abstract
Background
One of the primary indications for reflux testing with multichannel intraluminal impedance with pH (pH-MII) is to correlate reflux events with symptoms such as cough. Adult and pediatric studies have shown, using cough as a model, that patient report of symptoms is inaccurate. Unfortunately, intraesophageal pressure recording (IEPR) to record coughs is more invasive which limits its utility in children. The primary aim of this study is to validate the use of acoustic cough recording (ACR) during pH-MII testing.
Methods
We recruited children undergoing pH-MII testing for the evaluation of cough. We simultaneously placed IEPR and pH-MII catheters as well as an acoustic recording (ACR) device in each patient. Each 24 hour ACR, pH-MII, and IEPR tracing was scored by blinded investigators. Sensitivities for each method of symptom recording were calculated.
Key Results
2698 coughs were detected in total; 1140 were patient reported (PR), 2425 were IEPR detected, and 2400 were ACR detected. The sensitivity of PR relative to ACR was 45.9% and the sensitivity of IEPR relative to ACR was 93.6%. There was strong inter-rater reliability (κ=0.78) for the identification of cough by ACR.
Conclusions and Inferences
Acoustic recording is a non-invasive, sensitive method of recording cough during pH-MII testing that is well suited for the pediatric population.
Keywords: Gastroesophageal reflux, impedance, cough
Introduction
The association between gastroesophageal reflux with atypical, extraesophageal symptoms such as cough, throat clearing and wheezing, has been debated in children. Recent randomized controlled trials and meta-analyses have failed to show a clear benefit of acid suppression for treatment of extraesophageal symptoms and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition recommends reflux testing prior to acid suppression therapy because of the associated costs and risks of acid suppression including gastrointestinal and respiratory infections (1–4). Determining which reflux test to perform is heavily debated as is the most important testing outcome (e.g. the amount of acid reflux, amount of non-acid reflux, the degree of symptom association with reflux events).
Because non-acid reflux is so common in children, multichannel intraluminal impedance testing (pH-MII) which measures both acid and non-acid reflux, has become one of the most commonly performed modes of reflux testing (5). Because there are limited papers describing the normal pH-MII values for reflux in children, gastroenterologists have relied on the temporal correlation of reflux events with symptoms rather than the total reflux burden during pH-MII testing (6). One of the key extraesophageal symptoms for which pH-MII testing is performed is chronic cough. To determine the reflux-cough correlation, patients must undergo reflux testing with a pH-MII catheter in the nose for 24 hours during which patients and/or their parents record symptoms for the entire 24-hour period. For patients with hundreds of symptoms per 24-hour period or for patients whose symptoms occur during sleep, symptom recording is especially challenging. Recently, we and others have shown that when using more objective measurement of cough detection such as intraesophageal pressure recording (IEPR), patients underreport 50%–90% of symptoms (7–9), and that many of the cough events attributed to reflux are, indeed, not associated with it. While IEPR offers a great advantage over pH-MII testing alone, the IEPR catheter requires a second nasal intubation or requires that 2 catheters to be placed simultaneously which increases discomfort and difficulty of placement in an unsedated child. Therefore, less invasive methods to detect cough are needed. One such method is acoustic recording (ACR) which involves the taping of microphones over the trachea and chest wall. The microphones record upper and lower airway sounds which can be correlated with reflux episodes detected by pH-MII. We hypothesized that ACR would be well tolerated in children and provide more accurate cough detection that patient report alone. It is the goal of this study to determine the sensitivity of ACR relative to other methods of cough detection, patient report (PR) and intraesophageal pressure recording (IEPR) (7–9).
Materials and Methods
This was a prospective study of patients, ages 4–18, undergoing pH-MII and endoscopy testing for the evaluation of chronic cough. Any patient presenting to Boston Children’s Hospital with a chief complaint of cough and who was undergoing endoscopy for the evaluation of reflux related extraesophageal symptoms with simultaneous pH-MII testing was approached for participation. If patients consented, an IEPR catheter and the ACR device were placed at the time of the endoscopy and pH-MII probe. This study was approved by the Boston Children’s Hospital Institutional Review Board, and informed consent was obtained from each family unit/patient.
pH-MII with IEPR
pH-MII was performed using standard techniques previously reported (10). The IEPR technique has been previously described (9). Briefly, a 4 channel esophageal pressure catheter (Sandhill Scientific) was placed at the time of the endoscopy and the pH-MII catheter placement. Both catheters were sutured together using absorbable sutures prior to placement, and the sutures were placed in an area of the catheter away from pressure or impedance transducers. None of the pressure sensors were in contact with the pH or MII sensors. Location of the catheter was confirmed using intraoperative fluoroscopy such that the distal pH sensor was located at the third vertebral angle above the diaphragm (11).
Acoustic Recording (ACR) Device
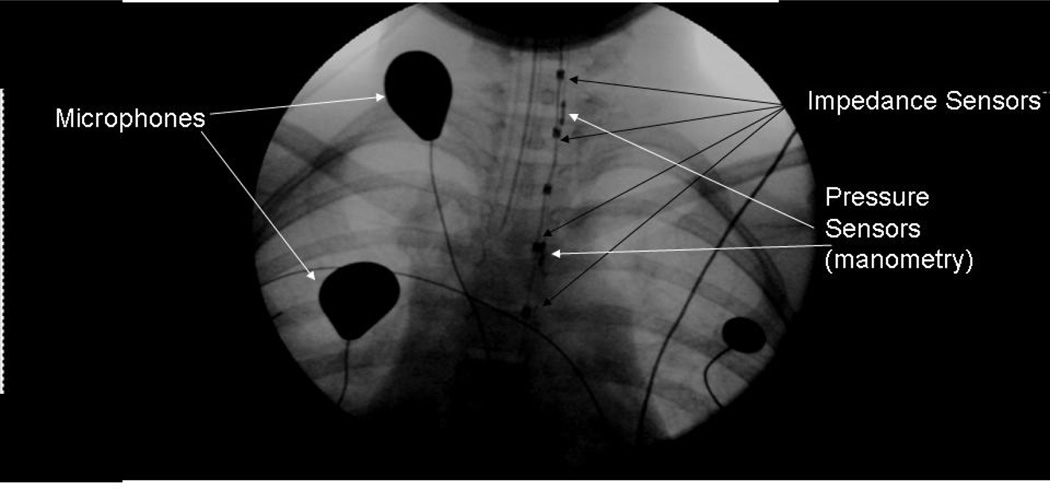
While under anesthesia, 3 microphones and acoustic recording device (Sandhill Scientific) were placed on the patient. Once microphone was taped over the trachea, one was taped over the right chest wall in the area of the 2nd intercostal space, and one was clipped to the patient’s clothing. The first microphone measured upper airway sounds, the second measured lower airway sounds, and the third measured ambient noises such the coughs and sounds from family members could be differentiated from patient coughs. Fluoroscopy imaging of the pH-MII and the IEPR catheters as well as the tracheal and chest wall microphones are shown in Figure 1.
Figure 1.
Fluoroscopy image of pH-MII and IEPR catheters and ACR microphones
pH-MII, IEPR, and ACR occurred for a minimum of 20 hours and patient/parents recorded cough on a log, using the clock on the pH-MII recording device upon which symptoms correlation was based. Prior to placement in the patient, the clocks on the pH-MII, IEPR and ACR were synchronized within 1 second of each other. The ACR device and the pH-MII were also synchronized by sound and electrical signaling between devices.
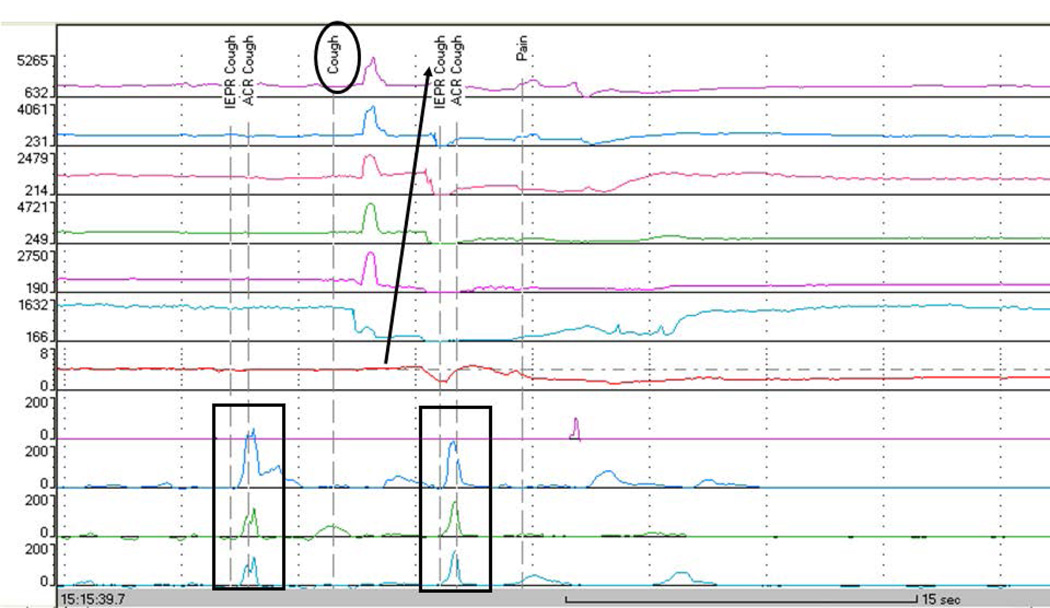
After study completion, the pH-MII and IEPR studies were blindly analyzed by one of the authors (RR) both for reflux and the presence of high pressure, simultaneous, intraesophageal pressure spikes signifying cough (Figure 2). 24-hour ACR sounds were reviewed by a single listener (NH) and for any sound that was not a clear cough, a second listener (JA) blindly reviewed the sounds in question. Only those sounds which both listeners agreed upon were included as coughs. To determine the degree of inter-rater reliability for cough identification using ACR, we chose 20 sound clips, each 30 second, with a variety of sounds made by each of the patients. Six blinded listeners scored the sound clips for the presence or absence of cough.
Figure 2.
Tracing of an acid reflux event (Arrow, retrograde drops in impedance) preceded by and concurrent with IEPR and ACR cough events. Note the IEPR spikes during cough (Rectangle). Also note that the patient reports a single cough (Oval).
After the manual analysis of the pH-MII tracings, the patient/parent reported coughs and the ACR coughs were added to the pH-MII/IEPR tracings. ACR coughs were added by using the elapsed time from the start of the study to determine the location of the ACR on the pH-MII tracings. Coughs detected by any method that were separated by less than 1 second were considered part of the same cough burst for the purposes of symptom-reflux associations. To determine the esophageal pressures seen during cough episodes, we randomly chose 120 coughs and measured the peak pressure amplitude (mm Hg) generated during each cough episode.
Reflux-cough associations
The symptom index using each technique was defined as the number of symptoms associated with reflux/total number of symptoms and was considered positive if it is >50% (12). The symptom sensitivity index was defined as the total number of reflux episodes associated with symptoms/total number of reflux episodes and was considered positive if it is >10% (13). The SAP was considered abnormal if it was greater than 95% (14). In this study, we used a standard 2 minute window before and after a cough when considering if reflux was associated with the cough (13, 15). However, we also recorded the exact time from reflux to cough and from cough to reflux for each cough detected. Definitions for reflux by pH-MII have been previously described (10).
Statistics
Based on our prior study in which we compared IEPR to patient reported cough, we assumed a minimum average difference of 10 coughs per patient between the patient-reported coughs and the ACR coughs. We anticipated that we would need to recruit 10 patients to give us greater than 90% power to reject the null hypothesis that there is no difference between the two techniques (patient report and ACR). The Type I error probability associated with this test of this null hypothesis was 0.05. Results are expressed as medians (ranges) and, when clinically relevant, the 95% of the data was also included. We compared proportions using chi-square analyses. Paired t tests were used to compare the differences in symptom indices within patients. To determine agreement of cough between 6 blinded listeners, Fleiss’ kappa statistic was calculated.
Results
Cough detection
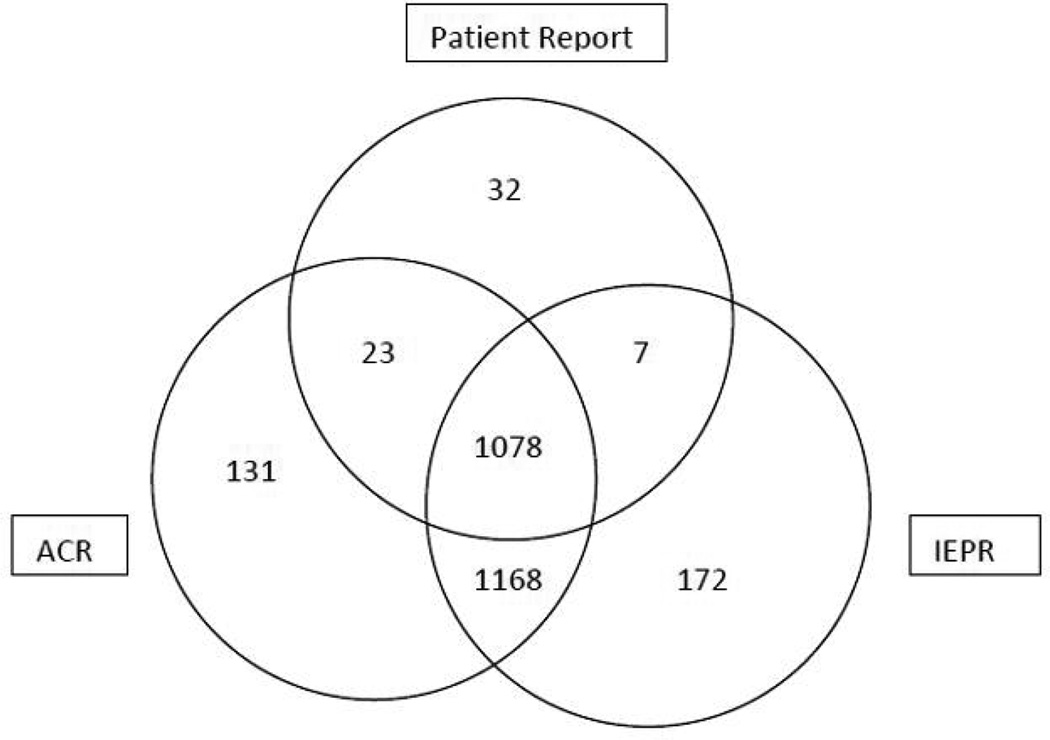
ACR was well tolerated; there were no adverse events to microphone use other than discomfort with tape removal over the microphone in 2 of the patients. 2611 total coughs were detected in 10 patients; 2425 were detected by IEPR, 2400 were detected by acoustic cough recording, and 1140 were patient reported. The frequency of coughs per patient is shown in Table 1. The overlap in detection between the three devices is shown in Figure 3. The sensitivity of each of the devices is shown in Table 2; ACR is as sensitive as IEPR and both devices were more sensitive than patient report. To compare IEPR coughs assuming the gold standard is patient report, we created a logistic model with random effects per patient to account for the multiple observations per patient, the AUC is calculated to be 0.880 (0.867, 0.893). To compare ACR coughs assuming the gold standard is patient report, after adjusting the model to account for the multiple observations per patient, the AUC is calculated to be 0.882 (0.869, 0.895). To compare ACR coughs assuming the gold standard is IEPR, after adjusting the model to account for the multiple observations per patient, the AUC is calculated to be 0.777 (0.744, 0.811).
Table 1.
Patient characteristics (reflux burden, cough frequency, and symptom indices).
| Total Reflux |
Coughs by PR |
Coughs by IEPR |
Coughs by ACR |
SI by PR |
SI by IEPR |
SI by ACR |
SSI by PR |
SSI by IEPR |
SSI by ACR |
SAP by PR |
SAP by IEPR |
SAP by ACR |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | 75 | 670 | 751 | 781 | 48 | 49 | 48 | 100 | 100 | 100 | 100 | 100 | 100 |
| Patient 2 | 23 | 12 | 45 | 37 | 0 | 22 | 27 | 0 | 57 | 43 | 0 | 84 | 90 |
| Patient 3 | 39 | 68 | 205 | 184 | 22 | 19 | 17 | 28 | 100 | 82 | 63 | 84 | 78 |
| Patient 4 | 67 | 112 | 171 | 145 | 59 | 53 | 55 | 100 | 100 | 100 | 100 | 100 | 100 |
| Patient 5 | 20 | 15 | 113 | 133 | 27 | 9 | 7 | 2 | 50 | 45 | 68 | 61 | 75 |
| Patient 6 | 18 | 150 | 157 | 179 | 21 | 21 | 22 | 100 | 100 | 100 | 99 | 100 | 100 |
| Patient 7 | 78 | 8 | 278 | 292 | 56 | 26 | 24 | 5 | 87 | 91 | 85 | 91 | 91 |
| Patient 8 | 306 | 27 | 107 | 97 | 66 | 66 | 63 | 6 | 24 | 21 | 97 | 0 | 29 |
| Patient 9 | 4 | 3 | 21 | 12 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Patient 10 | 24 | 75 | 577 | 540 | 22 | 22 | 29 | 71 | 100 | 100 | 0 | 99 | 99 |
SI= Symptom Index (%)
SSI= Symptom Sensitivity Index (%)
SAP=Symptom Association Probability (%)
PR= Patient Report
IEPR= Intraesophageal Pressure Recording
ACR= Acoustic Cough Recording
Figure 3.
Overlap of cough detection based on acoustic recording (ACR), intraesophageal pressure recording (IEPR) and patient report.
Table 2.
Differences in the sensitivity of cough detection depending on the gold standard used.
| Patient Report relative to ACR | 45.9% |
| ACR relative to IEPR | 92.6% |
| IEPR relative to ACR | 93.6% |
| Patient Report relative to IEPR | 45.4% |
We randomly chose 120 coughs measured by IEPR that were identified by patients and found that the median pressure using IEPR were 161 mm Hg, range 20–365 mm Hg. For the 20 representative coughs scored by 6 blinded listeners, there was a Fleiss kappa statistic of 0.78.
Gastroesophageal reflux and its relationship to cough
The total numbers of reflux events per patient are shown in Table 1. There was a median of 32 reflux episodes (range: 4–306) per study detected, of which 7 were acid (range: 0–57), 19 were non-acid (range: 1–303) and 12 were pH-only episodes (range: 0–32). The median % time pH was <4 was 2.7% (range: 0–15).
Of the 2611 coughs, 856 coughs were associated with a reflux episode. 436 (51%) of reflux events came before the cough and 522 (61%) of reflux events came after the cough. The median time from reflux to cough was 10 seconds (95%: 1 min 37 seconds) and the median time from cough to reflux was 23 seconds (95%: 1 min 41 seconds, p=0.001). There was no significant difference in the median bolus clearance time of reflux events that proceed cough (9 seconds, 95%: 163 seconds) versus reflux episodes that follow cough (10 seconds, 95%: 44 seconds, p=0.2).
There was a significant difference in the median bolus clearance time in the proximal most channel for reflux events that proceed cough (0.6 seconds, 95%: 52 seconds) versus reflux episodes that followed cough (3 seconds, 95%: 40 seconds, p=0.001). There was a significant relationship between reflux events reaching the proximal most sensor and patient reported cough (p=0.008). There was no relationship between full column reflux and ACR or IEPR cough suggesting that, when improved cough detection is used, the relationship between full column events and cough is not significant (p=1.0 for ACR, p=0.3 for IEPR).
There was a significant difference between the SI determined by ACR and patient report (p=0.02) and the SI determined by IEPR and patient report (p=0.02). One out of the ten patients would have an abnormal SI by patient report which was in the normal range (<50%) by ACR and IEPR. None of the patients had an abnormal SI by IEPR or ACR but not by patient report.
There were significant differences between the SSI determined by ACR and patient report (p=0.02) and the SSI determined by IEPR and patient report (p=0.02). There was no significant difference between the SSI determined by ACR and IRPR (p=0.1). Two out of the 10 patients would have a normal SSI by patient report but an abnormal SSI by ACR and IEPR. None of the patients were considered to have an abnormal SSI by patient report but not by IEPR or ACR.
There were no significant differences between the SAP determined by any of the three methods (p>0.2). One patient had a positive SAP by patient report that would be negative by IEPR and ACR and one patient had a positive SAP using IEPR and ACR that would have been negative by patient report.
All of the patients with a positive SI, SSI and SAP by IEPR had a positive index by ACR. The distribution of indices per patient and method are shown in Table 1.
Discussion
This is the first study in pediatrics or adults to compare ACR to IEPR during 24-hour pH-MII testing and we have clearly shown that IEPR and ACR are equally as sensitive to detect cough but ACR is a much less invasive alternative which is of great benefit in pediatrics.
We have also shown that ACR is as sensitive as IEPR, but most importantly, it is significantly more comfortable and well tolerated. While most pH-MII probes are placed in the outpatient setting without sedation, the placement of 2 nasal catheters (pH-MII and IEPR catheters) can cause increased discomfort such that, at our institution, the two catheters are placed with sedation or general anesthesia. ACR, which only relies on 2 stickers with microphones placed on the chest and neck and one clipped to the clothing, is therefore feasible in any patient with chronic cough getting reflux testing in the outpatient setting.
While ACR definitely increased cough detection by more than 100% over patient report alone, the average symptom index per patient did not change regardless of the technique used (ACR, IEPR, patient report). The reason for this is that, with the more sensitive devices ACR and IEPR, both the numerator (number of coughs associated with reflux) and denominator (total number of coughs) increase proportionally relative to patient report. Therefore, while ACR definitely increased total symptom detection, it also increased the detection of reflux-associated coughs. There were, however, differences in the SSI as determined by patient report relative to IEPR and ACR. The reason for these differences is the numerator (the number of reflux events associated with symptoms) was higher with ACR and IEPR but the denominator (the total number of reflux episodes) was constant. Based on our data, 10–20% of patients would have a change in diagnosis based on symptom indices when ACR is used instead of patient report.
The importance of having an accurate, non-invasive method to detect cough will hopefully improve the accuracy of diagnosing reflux-related cough. Multiple studies have failed to show a consistent relationship between reflux by 24-hour reflux testing and cough and therapeutic trials of acid suppression therapy have failed to show consistent cough improvement (1, 2, 16–18). This inconsistent relationship between reflux and cough may because of several reasons: (1) early studies did not use pH-MII so relationships between non-acid reflux and cough may have been missed, (2) acid suppression does not significantly reduce the amount of total reflux episodes so a treatment effect would not be seen, or (3) the therapeutic trials stratified patients based on a positive symptom correlation based on patient report which, we know from this study, is inaccurate. ACR should overcome this final limitation by improving symptom identification.
Acoustic cough recording with pH-MII has been performed in 2 adult studies. In the first adult study of 21 patients undergoing ACR with pH-MII, the authors found that ACR detected four times the amount of coughs than standard patient reporting (although this study did not compare ACR to IEPR) (19). In our study, we found that ACR detected two times the amount of coughs relative to patient report. One explanation for the higher rate patient reported cough in our pediatric series is that there are often three or four people (the patient, two parents, and a nurse) recording symptoms so the number of symptoms missed by all of the providers is lower than if the patient alone were recording symptoms.
The second study using ACR to determine the temporal relationship between cough and reflux detected by pH-MII in 71 adults found that reflux was as likely to occur after a cough as before the cough which was similar to the findings in our study (20). Furthermore, Smith et al propose cutting the symptom-reflux association window down to 10 seconds based on the biological plausibility that reflux should not cause cough several minutes after reflux resolution, Interestingly, the median time to cough occurrence after a reflux episode in our study was 10 seconds. While we can conclude in our study that majority of reflux-cough episodes occur within 1 min and 40 seconds, we cannot yet conclude that the symptom window should be reduced without a therapeutic outcome trial to validate an ideal window. However, ACR presents a critical first step in this process; we can now non-invasively identify coughs with a high sensitivity and the next necessary step, an intervention trial stratified based on symptom association using ACR, is needed.
One of the biggest critiques of ACR is that it is difficult to differentiate sounds such as throat clearing from cough. One hope was that IEPR should be able to differentiate throat clearing from cough, as throat clearing might have lower intraesophageal pressures. In a study of 10 adults who simulated cough and throat clearing during simultaneous high resolution manometry and ACR, cough and throat clearing during acoustic recording were confused between 6–8% of the time though these could be differentiated by differences in median intraesophageal pressures, as throat clearing had lower intraesophageal pressures (median 27 mmHg) versus cough (median 54 mmHg, p=0.001) (21). Our study has shown that there is a wide range of intraesophageal pressures in pediatric patients who cough and interestingly, our esophageal pressures during cough are higher than reported in this adult study suggesting that actual coughs, rather than simulated coughs, may have different esophageal pressures. The implications of this wide pressure range during IEPR is that measuring esophageal pressure spikes alone may not be adequate to differentiate cough from other sounds and that ACR may be necessary to clarify sound differences.
One possible limitation of this study is we have a small sample size. Because this study was powered based on the number of anticipated coughs necessary for a sensitivity analysis, the actual number of patients is small so generalizations about reflux-cough mechanisms are limited. However we have almost 3000 cough episodes, a sample size that allows for ample validation of the different techniques used. In this study, however, we echo previous findings that reflux-cough and cough-reflux sequences occur with equal frequency and that the SI does not vary based on the technology used but the SSI does vary (9). To determine true associations between reflux and cough by ACR, a larger pediatric patient population is needed.
A second limitation is that there may be a bias towards more reflux associated coughs in our patients as these patients were referred to a gastroenterologist for the evaluation of reflux-related cough. Nevertheless, the number of patients with a positive symptom association, regardless of the index used, was low so we feel this bias was minimal. Because of our small sample size, we recognize that we cannot draw any conclusions about the frequency of reflux related coughs on a population level however we do want to highlight that the success of finding a cough-reflux correlation does depend on the method of cough detection (patient report, IEPR and ACR).
In summary, ACR has a sensitivity that is equivalent to IEPR and significantly improves the detection of cough in children undergoing pH-MII testing, and allows a better characterization of its relationship with reflux. Studies are now needed to determine if this increased detection improves therapeutic outcomes but clearly relying on symptom reporting by patients is flawed and clinical decision making based on patient report alone should be done with caution.
Key Messages.
Adult and pediatric studies have shown, using cough as a model, that patient report of symptoms is inaccurate. Intraesophageal pressure recording (IEPR), while more sensitive to detect cough, requires placement of a second catheter and therefore placement is uncomfortable and requires anesthesia, therefore limiting its utility in children. In this study, we found that acoustic cough recording (ACR), a non-invasive way to measure cough, is a sensitive tool for cough detection; we found that the sensitivity of patient detected coughs relative to ACR was 46% and the sensitivity of ACR to IEPR was 93%.
Acknowledgements
Funding, and Disclosures: This work was supported through NIH K23 DK073713-05 (RR) 1R03DK089146-02 (RR), and Translational Research Program Junior Investigator Award (RR).
Abbreviations
- pH-MII
Multichannel intraluminal impedance with pH
- SI
Symptom Index
- SSI
Symptom Sensitivity Index
- ACR
acoustic recording
- IRPR
intraesophageal pressure recording
- PR
Patient report
Footnotes
Contributions:
RR conceptualized and designed the study, recruited patients, drafted the initial manuscript, and approved the final manuscript.
JA recruited patients, assisted with data entry, listened to the acoustic recordings, critically reviewed the manuscript, and approved the final manuscript.
NH assisted with data entry, listened to the acoustic recordings, critically reviewed the manuscript, and approved the final manuscript.
HL assisted in the statistical analyses and approved of the final manuscript.
UK assisted with patient recruitment, critically reviewed the manuscript, and approved the final manuscript.
References
- 1.Holbrook JT, Wise RA, Gold BD, et al. Lansoprazole for children with poorly controlled asthma: a randomized controlled trial. JAMA. 2012;307:373–381. doi: 10.1001/jama.2011.2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mastronarde JG, Anthonisen NR, Castro M, et al. Efficacy of esomeprazole for treatment of poorly controlled asthma. N Engl J Med. 2009;360:1487–1499. doi: 10.1056/NEJMoa0806290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canani RB, Cirillo P, Roggero P, et al. Therapy with gastric acidity inhibitors increases the risk of acute gastroenteritis and community-acquired pneumonia in children. Pediatrics. 2006;117:e817–e820. doi: 10.1542/peds.2005-1655. [DOI] [PubMed] [Google Scholar]
- 4.Rudolph CD, Mazur LJ, Liptak GS, et al. Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 2001;32(Suppl 2):S1–S31. doi: 10.1097/00005176-200100002-00001. [DOI] [PubMed] [Google Scholar]
- 5.Vandenplas Y, Salvatore S, Devreker T, Hauser B. Gastro-oesophageal reflux disease: oesophageal impedance versus pH monitoring. Acta Paediatr. 2007;96:956–962. doi: 10.1111/j.1651-2227.2007.00306.x. [DOI] [PubMed] [Google Scholar]
- 6.Rosen R, Furuta G, Fritz J, Donovan K, Nurko S. Role of acid and nonacid reflux in children with eosinophilic esophagitis compared with patients with gastroesophageal reflux and control patients. J Pediatr Gastroenterol Nutr. 2008;46:520–523. doi: 10.1097/MPG.0b013e318158600c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blondeau K, Mertens V, Dupont L, et al. The relationship between gastroesophageal reflux and cough in children with chronic unexplained cough using combined impedance-pH-manometry recordings. Pediatr Pulmonol. 2010 doi: 10.1002/ppul.21365. [DOI] [PubMed] [Google Scholar]
- 8.Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, impedance monitoring. Gut. 2005;54:449–454. doi: 10.1136/gut.2004.055418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosen R, Amirault J, Giligan E, Khatwa U, Nurko S. Intraesophageal Pressure Recording Improves The Detection of Cough During Multichannel Intraluminal Impedance Testing (pH-MII) in Children. J Pediatr Gastroenterol Nutr. 2013 doi: 10.1097/MPG.0b013e3182a80059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosen R, Nurko S. The importance of multichannel intraluminal impedance in the evaluation of children with persistent respiratory symptoms. Am J Gastroenterol. 2004;99:2452–2458. doi: 10.1111/j.1572-0241.2004.40268.x. [DOI] [PubMed] [Google Scholar]
- 11.Vandenplas Y, Rudolph CD, Di Lorenzo C, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) J Pediatr Gastroenterol Nutr. 2009;49:498–547. doi: 10.1097/MPG.0b013e3181b7f563. [DOI] [PubMed] [Google Scholar]
- 12.Wiener GJ, Richter JE, Copper JB, Wu WC, Castell DO. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am J Gastroenterol. 1988;83:358–361. [PubMed] [Google Scholar]
- 13.Breumelhof R, Smout AJ. The symptom sensitivity index: a valuable additional parameter in 24-hour esophageal pH recording. Am J Gastroenterol. 1991;86:160–164. [PubMed] [Google Scholar]
- 14.Weusten BL, Roelofs JM, Akkermans LM, Van Berge-Henegouwen GP, Smout AJ. The symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology. 1994;107:1741–1745. doi: 10.1016/0016-5085(94)90815-x. [DOI] [PubMed] [Google Scholar]
- 15.Omari TI, Schwarzer A, vanWijk MP, et al. Optimisation of the reflux-symptom association statistics for use in infants being investigated by 24-hour pH impedance. J Pediatr Gastroenterol Nutr. 2011;52:408–413. doi: 10.1097/MPG.0b013e3181f474c7. [DOI] [PubMed] [Google Scholar]
- 16.Chang AB, Lasserson TJ, Kiljander TO, Connor FL, Gaffney JT, Garske LA. Systematic review and meta-analysis of randomised controlled trials of gastro-oesophageal reflux interventions for chronic cough associated with gastro-oesophageal reflux. BMJ. 2006;332:11–17. doi: 10.1136/bmj.38677.559005.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gatta L, Vaira D, Sorrenti G, Zucchini S, Sama C, Vakil N. Meta-analysis: the efficacy of proton pump inhibitors for laryngeal symptoms attributed to gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2007;25:385–392. doi: 10.1111/j.1365-2036.2006.03213.x. [DOI] [PubMed] [Google Scholar]
- 18.Orenstein SR, Hassall E, Furmaga-Jablonska W, Atkinson S, Raanan M. Multicenter, double-blind, randomized, placebo-controlled trial assessing the efficacy and safety of proton pump inhibitor lansoprazole in infants with symptoms of gastroesophageal reflux disease. J Pediatr. 2009;154:514–520. e514. doi: 10.1016/j.jpeds.2008.09.054. [DOI] [PubMed] [Google Scholar]
- 19.Kavitt RT, Higginbotham T, Slaughter JC, et al. Symptom reports are not reliable during ambulatory reflux monitoring. Am J Gastroenterol. 2012;107:1826–1832. doi: 10.1038/ajg.2012.342. [DOI] [PubMed] [Google Scholar]
- 20.Smith JA, Decalmer S, Kelsall A, et al. Acoustic cough-reflux associations in chronic cough: potential triggers and mechanisms. Gastroenterology. 2010;139:754–762. doi: 10.1053/j.gastro.2010.06.050. [DOI] [PubMed] [Google Scholar]
- 21.Xiao Y, Carson D, Boris L, et al. The acoustic cough monitoring and manometric profile of cough and throat clearing. Dis Esophagus. 2013 doi: 10.1111/dote.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]