Abstract
Purpose
To describe the processes and outcomes of developing and implementing a Continuity of Care Document (CCD), My Health Profile, as personal health record for persons living with HIV (PLWH) in an HIV/AIDS Special Needs Plan (SNP) in New York City.
Methods
Multiple qualitative and quantitative data sources were used to describe the processes and outcomes of implementing My Health Profile including focus groups, Audio Computer Assisted Self Interview (ACASI) surveys, administrative databases, chart abstraction, usage logs, and project management records. Qualitative data were thematically analyzed. Quantitative data analytic methods included descriptive and multivariate statistics. Data were triangulated and synthesized using the Reach, Efficacy/Effectiveness, Adoption, Implementation, Maintenance (RE-AIM) Framework.
Results
Reach
SNP members are predominantly African American or Hispanic/Latino and about one third are female. A larger proportion of African Americans and smaller proportions of Hispanics/Latinos and Whites were trained to use My Health Profile.
Efficacy/Effectiveness
CCDs were produced for 8,249 unique members and updated on a monthly basis, 509 members were trained to use My Health Profile. Total number of member logins for 112 active users was 1,808 and the longest duration of use was 1,008 days. There were no significant differences between users and non-users of My Health Profile in clinical outcomes, perceptions of the quality of medical care, or health service utilization.
Adoption
My Health Profile was well-matched to organizational mission, values, and priorities related to coordination of care for a high-risk population of PLWH.
Implementation
Pre-implementation focus group participants identified potential barriers to use of My Health Profile including functional and computer literacy, privacy and confidentiality concerns, potential reluctance to use technology, and cognitive challenges. Key strategies for addressing barriers included a dedicated bilingual coach for recruitment, training, and support; basic computer and My Health Profile training; transparent audit trail revealing clinician and case manager access of My Health Profile, time-limited passwords for sharing My Health Profile with others at the point of need, and emergency access mechanism.
Maintenance
My Health Profile was integrated into routine operational activities and its sustainability is facilitated by its foundation on standards for Health Information Exchange (HIE).
Conclusions
Although potential barriers exist to the use of PHRs such as My Health Profile, PLWH with complex medical needs, low socioeconomic status, and limited computer experience will use such tools when a sufficient level of user support is provided and privacy and confidentiality concerns are addressed.
Keywords: continuity of care, continuity of care record, continuity of care document, personal health record, HIV/AIDS, RE-AIM Framework
1. Introduction
By the end of 2011 the Centers for Disease Control and Prevention (CDC) estimated that 1.2 million individuals in the U.S. were infected and living with HIV [1]. As in other developed countries, the advent of modern antiretroviral therapy (ART) has resulted in the potential for people living with HIV (PLWH) to alter an almost uniformly progressive and fatal condition when untreated into a chronic medical illness that for many can be well managed and lead to near normal life expectancy [2, 3]. Unfortunately, nearly 40% of PLWH are either unengaged in care or poorly engaged in care at any specific point in time [4, 5], thereby compromising the ability to benefit from ART and other beneficial medical and care coordination efforts.
New York City is home to the oldest and largest HIV epidemic in the U.S. The current public health response comprises federal, state, and municipal programs each designed to address specific needs of PLWH, including access to care and medications, supportive services, care coordination, and public health surveillance. By 2003, in response to an evolving healthcare environment, the New York State Department of Health AIDS Institute had pioneered the development of HIV Special Needs Plans (SNPs) as a chronic HIV-specific Medicaid managed care plan [6]. SNPs were envisioned as a vehicle to provide complex care coordination and medical services to a population with rates of chemical dependency, mental health disorders, and other complex co-morbidities (Hepatitis C, tobacco use) many fold higher among PLWH than the general population [7, 8] and rates of care engagement below that necessary to obtain acceptable health outcomes.
Health Information Technology (HIT) has helped foster improved outcomes in clinical care, care coordination, and public health reporting and may hold promise as a means to improve overall care engagement. Initial HIT advancements have largely focused upon providing tools to clinicians, ancillary staff, and institutions to better manage laboratory reporting, clinical documentation, and medication administration [9–11]. More recently, the potential benefits of utilizing HIT to empower consumers, such as PLWH, to more vigorously participate in healthcare decisions and management have gathered momentum and are now widely seen as critical components of high quality healthcare delivery systems. Indeed, an important HIT objective of Healthy People 2020 focuses upon increasing the proportion of persons who use electronic personal health management tools, specifically the proportion of individuals who use the internet to keep track of personal health information, such as care received, test results, or upcoming medical appointments [12].
Continuity of Care Records (CCRs) [13] and the subsequent Continuity of Care Document (CCD) [14,15] standard have been widely cited as promising HIT tools designed to promote clinical care coordination across often segregated care sites and provider types through health information exchange (HIE). The initial CCR standard was developed by multiple stakeholders, including ASTM International, the Healthcare Information and Management Systems Society (HIMSS), the Massachusetts Medical Society, the American Academy of Family Physicians, and the American Academy of Pediatrics, as a highly structured, flexible, potentially interoperable health summary standard that was intended to be a ‘snapshot’ of core demographic, clinical, and care team information that could be used and updated during clinical encounters that may occur in the absence of a patient’s full medical record. The CCD standard is the outgrowth of a harmonization effort between ASTM International and Health Level Seven International (HL7) and specifies an implementation of CCR domains according to the semantics of HL7’s XML-based clinical document architecture (CDA) standard to produce a CCD. Ideally, a CCR or CCD could be used by patients to bridge gaps in medical records that exist in disparate sites of care due to the lack of any shared electronic health record (EHR), thereby ensuring that at least an important subset of critical clinical information exists at all points of care. The CCR and CCD standards specify a few required elements (e.g., patient identifying information, payers) and clinically important optional elements (e.g., practitioners, medications, laboratory results, family history). More broadly, CCR/CCD contents can be viewed as a limited form of a Personal Health Record (PHR), although by definition a ‘concise’ form rather then a ‘full’ PHR and without total control of information access by the patient.
The development and deployment of electronic personal health management tools remain in their infancy and a number of high profile examples, such as Microsoft’s Health Vault and Google’s My Health Record, have recently been scaled back or are under internal review. However, meaningful use objectives for EHRs [16] include providing patients, upon request, with an electronic copy of their health information, an objective that can be facilitated through the development of a PHR based upon CCR/CCD standards. Thus, it is likely that adoption and use of PHRs, particularly those based upon CCR/CCD standards, is likely to expand as organizations and providers attempt to meet meaningful use standards and consumers seek access to their medical records across the care spectrum. Accessing clinical information across distinct clinical sites or geographic areas, such as New York City, ideally requires a PHR to be connected to a repository of health information or an HIE, a process that has been referred to as ‘tethering’ or ‘interconnecting’ [17]. Linking a PHR to a HIE, and thereby potentially pre-populating the PHR with data from multiple providers and organizations, has been viewed as an important HIT goal that might substantial increase the use of PHRs by consumers. Indeed, adoption rates of PHRs by consumers have varied significantly, generally in proportion to their perceived ease of use and burden of data entry [18]. Two prominent examples of PHR adoption are Kaiser Permanente’s (KP) HealthConnect and Britain’s National Health Service’s (NHS) Health Space. The rates of PHR adoption ranged from a low of 0.13% for the NHS’s Health Space to an impressive 28% for Kaiser Permanente’s HealthConnect, the latter representing one of the most successful examples of a broad PHR implementation project cited in the literature.
The purpose of this paper is describe the processes and outcomes of developing and implementing a CCD, My Health Profile, as a PHR for PLWH in an HIV/AIDS Special Needs Plan (SNP) in New York City.
2. Project Overview
In 2007, NYPS SelectHealth, an HIV/AIDS SNP operating in four of five boroughs in New York City, was awarded a grant from the Health Resources Services Administration (HRSA) Special Project of National Significance (SPNS) program. The NYPS SelectHealth project was intended to demonstrate the potential of HIT to improve the health care and care coordination of PLWH (i.e., members) and targeted three specific user groups, namely PLWH, care coordination personnel, and clinicians. The focus of this paper is My Health Profile, a CCD developed and deployed for use as a PHR by PLWH.
2.1 Premises and Rationale for My Health Profile
My Health Profile was developed based upon several important premises. First, targeted health and care coordination information could be organized as a CCD and accessed and used by PLWH through the My Health Profile interface across a geographic region via a standard Internet connection. Furthermore, the information in the CCD could be assembled from data that already existed in disparate electronic health records and administrative databases by employing HIE. An important early decision made in the design phase of the project was to align with HIT and HIE standards whenever possible. The rationale behind this decision included the benefits of leveraging development work in CCRs and the subsequent CCD standard by groups long dedicated to resolving the challenge of fractionated health information generally inaccessible at various points of clinical service provision, such as emergency departments and non-affiliated healthcare providers. Additionally, long-term maintenance of HIE was an important early project concern and sustainability and replicability were facilitated by adopting national standards of HIE and adapting to local, state, and national HIE networks as they evolved, such as regional health information organizations (RHIOs), and State and National Health Information Networks.
2.2 CCD/My Health Profile
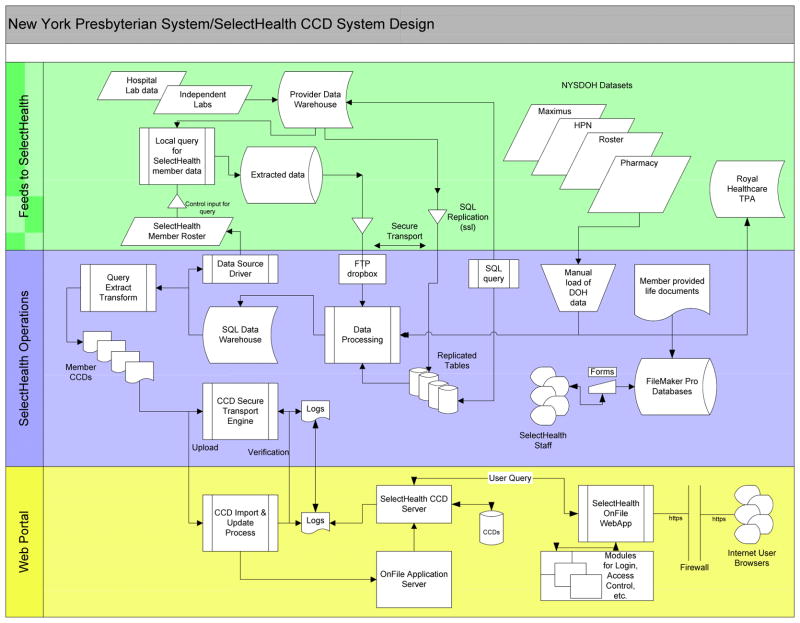
NYPS Select Health contracted with OnFile/American Medical File, Inc. to construct and host each CCD and pays a per member per month fee for this service. The CCD was populated with claims, demographic and clinical data. Each member had a CCD constructed, uploaded to a secure website, updated monthly, and made available to the member, participating care coordinators, and clinicians through a secure web interface. Figure 1 illustrates the initial information network that was developed and used to share information via a CCD to clinicians, case management agencies, and members.
Figure 1.
NYPS SelectHealth HIE Network
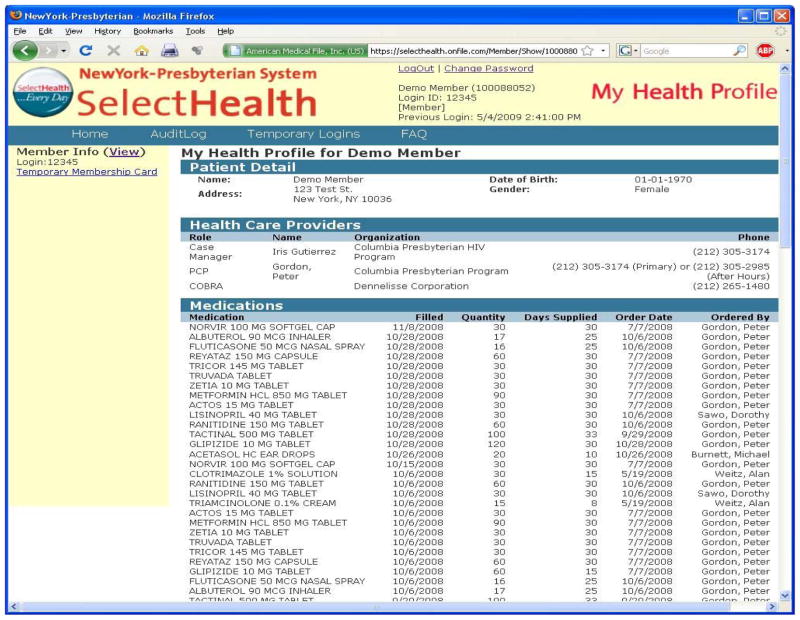
My Health Profile included the following sections and data:
Member Details: member name, address, gender, date of birth and phone number.
Healthcare and Care Coordination Providers: name of the primary care provider, their affiliation and phone number; name of each case manager, their affiliation and phone number.
Medications: most recent medications (up to 50) including name of medication, fill date, quantity, days supplied, ordered date and the name of the prescribing provider.
Results: most recent laboratory tests and key diagnostic tests from a core set of 26 predefined tests including test name, test date, count, percent, range, and results.
Payers: payer name, policy/coverage type, covered party ID, member status.
Document information: authored by, document id, title, description, effective date.
Figure 2 illustrates a CCD for a hypothetical patient similar to that used throughout the project period.
Figure 2.
Section of My Health Profile for a hypothetical patient
In terms of other My Health Profile features, members had the ability to generate and print time-delimited disposable passwords to allow access by others. In addition, members had the ability to view an integrated audit log which listed everyone who had accessed their My Health Profile and to print a PDF version of the CCD. They also had the option to carry an emergency access card which contained instructions for how emergency personnel could view their My Health Profile.
2.3 Introduction of My Health Profile to Members
Information about My Health Profile was presented to members upon plan enrollment and through quarterly member newsletters. Members were offered the opportunity to receive training on the use of the Internet and access to My Health Profile beginning in January, 2008 and continuing through the present time. Offers of training, available through a My Health Profile Community Coach, were made via print material during initial plan enrollment, via quarterly member newsletters, and through community outreach efforts at a variety of community based organizations and sites of clinical care. Available community free internet access points, such as local public libraries and community based organizations, were disseminated to the plan membership and promoted during training sessions with prospective My Health Profile users.
3. Methods
3.1. Samples and Data Sources
The samples are summarized in Table 1. The overall sample comprised all existing and new members of the HIV SNP since a CCD was constructed and updated monthly for each member. Multiple qualitative and quantitative data sources were used to evaluate My Health Profile (Table 2). We conducted five focus groups with members (n=35) to gather perceptions regarding challenges to managing health information and barriers and facilitators to use of a system such as My Health Profile prior to its implementation and two focus groups (n=15) post-implementation. At six month intervals cohorts of approximately 100 members completed Audio Computer Assisted Self Interview (ACASI) surveys that included questions related to demographics, medical history, medical care, continuity of care, other services, satisfaction with care, quality of life, trust, stigma, willingness to share personal health information, and computer literacy; 294 unique members completed at least one ACASI survey with a total of 418 ACASI surveys collected. Data from NYPS SelectHealth administrative databases and chart abstraction were used to gather clinical laboratory information (e.g., HIV viral load, CD4 counts) and service utilization from 350 unique members. My Health Profile use was captured through system log files. Data about implementation processes were gathered from project management records.
Table 1.
Characteristics of SelectHealth Membership and Study Samples
| Characteristics | Members** N=7080 |
My Health Profile
*** N=80 |
Focus Groups N=50 |
ACASI N= 294 |
Chart Abstraction N=350 |
|---|---|---|---|---|---|
|
| |||||
| n (%) | n (%) | n (%) | n (%) | n (%) | |
|
| |||||
| Gender | |||||
| Male | 4503(63.6) | 51(63.8) | 29(58.0) | 189(64.3) | 144(41.1) |
| Female | 2545(35.9) | 28(35.0) | 21(42.0) | 101(34.4) | 194(55.4) |
| Transgender | 29(.4) | 1(1.3) | 4(1.3) | 11(3.1) | |
| Unknown | 3(0) | ||||
|
| |||||
| Race | |||||
| African American/Black | 2699(38.1) | 39(48.8) | 40(80.0) | 234(56.0) | 165(47.1) |
| Asian | 23(.3) | 0(0) | 0(0) | 3(.7) | 3(.9) |
| Native Hawaiian/Pacific Islander | 2 (0) | 1(1.3) | 0(0) | 2(.5) | 2(.6) |
| Native American or Alaskan | 18(.3) | 3(3.88) | 0(0) | 8(1.9) | 0(0) |
| White/Caucasian | 2709(38.3) | 11(13.8) | 1(2.0) | 42(10.0) | 144(41.1) |
| Other/Not Specified* | 1629(23.0) | 26(32.5) | 9(18.0) | 127(30.4) | |
|
| |||||
| Ethnicity | |||||
| Hispanic/Latino | 2709(38.0) | 24(30.0) | 11(22.0) | 92(22.1) | NA |
| Non-Hispanic/Latino | 3450(49.0) | 56(70.0) | 39(78.0) | 324(77.9) | |
| Not Specified | 921(13.0) | ||||
|
| |||||
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
|
| |||||
| Age | 45.6(12.0) | 46.3(8.9) | NA | 46.8(9.1)) | 47.5(9.5) |
Most frequent response to Other was Hispanic/Latino,
Unique members January 2009 through August 31, 2011,
No significant differences between My Health Profile users and non-users.
Table 2.
Methods and Data Sources by RE-AIM Dimensions
| RE-AIM Dimension/Study Questions | Methods/Data Sources |
|---|---|
| Reach: The absolute number, proportion, and representativeness of participants in a given program. | |
| What percentage of the primary target population began program? | SH administrative data: # trained, # My Health Profile users |
| Were participants representative of target population? | Comparison of My Health Profile users with non-users |
| Efficacy/Effectiveness: The impact of the program on important outcomes. | |
| Did program achieve primary outcomes? | SH administrative data: # CCDs |
| How did the program affect secondary outcomes? | ACASI data |
| Did it produce unintended adverse consequences? | Project management data, focus groups |
| Did it produce unintended positive consequences? | Project management data, focus groups |
| What did the program cost as implemented? | Addressed in multi-site evaluation |
| Adoption: The absolute number, proportion, and representativeness of settings and staff willing to offer a program. | |
| Did low-resource organizations serving high-risk populations implement the program? | SelectHealth membership data |
| Did program help the organization address its primary mission? | SelectHealth document review and project team discussion |
| Is program consistent with organizational values and priorities? | SelectHealth document review and project team discussion |
| Implementation: At the setting level, includes consistency of delivery and predisposing and enabling factors. | |
| Were program components delivered as intended? | Project management and My Health Profile use data |
| What barriers to implementation (predisposing factors at individual, setting/ organizational levels) were identified and how were they addressed? | Focus groups, ACASI data |
| What enabling (facilitating) factors were/are required to support the program? | Focus groups, project management data |
| Maintenance: The extent to which a program or policy becomes part of the routine organizational practices/policies. | |
| Did organization sustain the program over time? | Project management data |
| How did the program evolve? | Project management data |
| What reinforcing factors were/are required to maintain the program? | Project management data |
3.2. Theoretical Framework
The RE-AIM Framework was used to guide the project evaluation and synthesize My Health Profile processes and outcomes. The RE-AIM Framework was initially developed to enhance the replicability and generalizability of behavioral studies by examining and reporting study aspects beyond efficacy [19]. Bakken and Ruland extended the framework to facilitate its application to clinical informatics innovations involve behaviors of system users (e.g., clinicians, patients) [20]. Definitions of RE-AIM dimensions are provided in Table 2. Although all dimensions are relevant to My Health Profile, Implementation was a particularly important dimension; thus, findings related to implementation are given more attention.
3.3. Data Analysis
This paper includes both previously published data and new data. For previously published data, the reader is referred to the primary publication for methodological details. More information is provided regarding analysis of new data. Qualitative data were thematically analyzed per methods detailed in [21]. Quantitative data were summarized with descriptive statistics. Where relevant, we also conducted correlational and multivariate analyses. After individual analyses were completed, we synthesized previously published results– noted by associated citations – and new results according to the dimensions of the RE-AIM Framework.
4. Results
4.1 Reach
The assessment of Reach focuses on the absolute number, proportion, and representativeness of participants in a given program. SelectHealth membership grew from approximately 600 to more than 6,000 by the project’s end with a total of 8,249 unique members during the course of the project including the development phase. The demographic characteristics of SelectHealth members, My Health Profile users, focus group participants, ACASI respondents, and charts selected for abstraction are displayed in Table 1. Members are predominantly African American or Hispanic/Latino and about one third are female.
During the initial phase of the project, 15% of the membership was trained to My Health Profile. The proportion dramatically decreased as the membership rapidly expanded. In total 509 members trained, i.e, began the program. Fifty-seven percent of those trained also participated in ACASI, thus allowing comparison between the majority of those trained and the overall membership on key demographic characteristics. As compared to the SelectHealth membership, a larger proportion of African Americans and smaller proportions of Hispanics/Latinos and Whites were trained. There were no differences in gender and those trained were slightly older than the overall membership 46.8(9.1) vs. 45.6(12.0).
In terms of comparisons between overall SelectHealth membership and those participating in one or more evaluation activity, for focus group participants, ACASI respondents, and charts selected for abstraction, African Americans and females were over-represented as compared to SelectHealth members for the key project implementation period of January 1, 2009–August 31, 2011 (Table 1).
4.2 Efficacy/Effectiveness
The efficacy/effectiveness dimension examines impact on important primary and secondary outcomes and also considers unintended consequences. The primary outcome related to the implementation of My Health Profile was access to critical healthcare information at the point of need including clinical settings, case management agencies, and members’ homes or other access points. Although a CCD was produced for each SelectHealth member on a monthly basis for a total of 138,532 CCDs, for this dimension member we conceptualized access as actual use of My Health Profile rather than availability. Defining My Health Profile use as > 1 login and >1 day of logins to remove those who did not use the system beyond the training session, the number of users was 112 – 22% of those trained. As of January 23, 2012 the total number of member logins was 1,808 and the longest duration of use was 1,008 days. As shown in Figure 3, the number of user logins ranged from 2 to >100 with most users falling into the category of 2–10 uses.
Figure 3. My Health Profile.
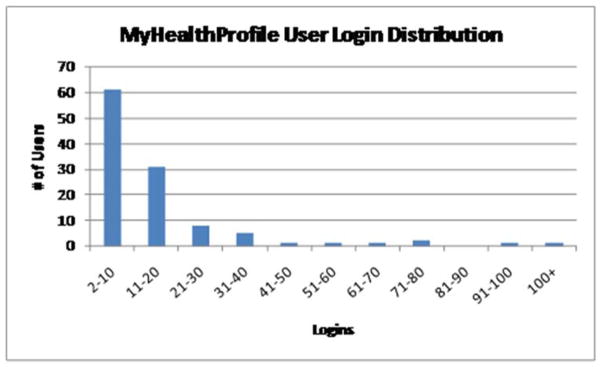
User Login Distribution (n=112)
We examined potential differences between users and non-users of My Health Profile on demographic characteristics collected through ACASI. Chi-squared analysis and independent sample t-tests showed no significant differences in demographics characteristics among My Health Profile users (n=80) and those who were trained, but did not subsequently use My Health Profile (n=214). In a binary logistic regression, those who had previously used the Internet were 2.7 times more likely (95% confidence interval=1.1–7.1) to use My Health Profile. There were no significant differences between those who used it daily versus less frequently. In terms of secondary outcomes, we compared 39 users and 43 non-users of My Health Profile who completed at least two ACASI surveys approximately 6–12 months apart. There were no significant differences in clinical outcomes such as self-report of skipping ART (p=.068) or having an undetectable viral load (p=.398). There were also no significant differences in perceptions of the quality of medical care (p=.192), one or more visits to the emergency department (p=.132), and one or more hospitalizations (p=.182).
There were several unintended positive consequences. Post-implementation focus group data and members’ reports to project personnel indicated that access to their data via My Health Profile had several positive behavioral effects. For instance, several users reported that viewing data that they did not understand motivated them to seek additional information about their health on the web. In addition, multiple users indicated how empowered they felt by having access to their healthcare data.
4.3 Adoption
Adoption addresses whether low-resource organizations serving high-risk populations participated in the program and the fit with organizational mission and priorities.. In this instance, a single organization, NYPS SelectHealth developed and adopted My Health Profile. As an HIV SNP, it serves a Medicaid population of primarily racial and ethnic minorities considered to be at high risk for poor health outcomes. NYPS SelectHealth leadership conceptualized the CCD including its My Health Profile member view in the context of its organizational mission and priorities that focus on providing members with both the kind of care and tools that can help them to improve their health and quality of life. In particular, My Health Profile supports the organizational mission and priority for coordinated care for PLWH.
4.4 Implementation
Implementation in RE-AIM takes into consideration consistency of delivery (i.e., were components delivered as intended) and predisposing and enabling factors for program delivery. For My Health Profile program components included creation of the CCDs and training of members to use My Health Profile. In regards to the former,138,532 CCDs were produced for 8,249 unique SelectHealth members during the project period. A much smaller proportion of members (n=509) were trained to use My Health Profile over the project period. During the initial project period when SelectHealth membership was approximately 600, 15% of the membership was trained. Although training efforts continued, the percentage of members trained decreased as membership grew to > 6,000 in latter project years.
In regards to predisposing and enabling factors for use of My Health Profile, member focus group participants identified perceived barriers and facilitators to use of such a system prior to My Health Profile implementation. Key findings are summarized here and detailed results provided in [18]. Barriers included functional and computer literacy, privacy and confidentiality concerns, potential reluctance to use technology, and cognitive challenges (e.g., remembering password). Despite recognition of potential barriers, participants were predominantly and enthusiastically positive about the usefulness of such a system to improve coordination of care and other services. Moreover, they suggested several facilitators that would enable use such as general computer training, training specific to use of My Health Profile, effective marketing of My Health Profile that makes it clear that use is additive rather than a replacement for current services, and personal support from another family member with more computer skills. In addition, post-implementation focus group participants suggested that another significant facilitator for use was a special member Emergency Card that could be provided to allow data access in critical situations, e.g., if the patient was taken to an emergency department.
The potential barrier of privacy and confidentiality concerns identified in the focus groups was also explored using ACASI data as reported in detail in [22]. In brief, we assessed the attitudes of a sample of SelectHealth members (n=93) who had not yet used My Health Profile towards electronic storage and sharing of their personal health information. Most (84%) were willing to share their personal health information with clinicians involved in their care; fewer (39%) were willing to share personal health information with non-clinical staff. Willingness to share PHI with their clinician, other clinicians, and non-clinical staff was positively associated with trust of clinicians to provide high-quality care and perceptions of their clinician’s willingness to spend time with patients.
Multiple strategies were used to address perceived barriers to My Health Profile. A critical strategy employed was a bilingual coach dedicated to recruitment, training, and user support. ACASI data collection was used as an opportunity to encourage members to activate their My Health Profile account because participation in ACASI was often perceived as empowering even to those who had limited prior interaction with computers. To address concerns regarding basic computer literacy, introduction to computer sessions were offered on a regular basis in several locations. In addition, training specific to My Health Profile was given in conjunction with account creation. The coach and other project personnel were routinely available to handle issues related to My Health Profile use (e.g., forgotten password), reinforce training, and provide other assistance as needed. Post-implementation focus group participants confirmed the importance of the coach and the impact of their personal relationship with the coach on their motivation and ability to use My Health Profile.
In addition, a key component of reducing concerns related to privacy and confidentiality of data in the CCD including the My Health Profile view was an audit trail. This allowed the users to see who had viewed their data. In terms of security, CCD data were stored behind the SelectHealth firewall and My Health Profile was password protected.
4.5 Maintenance
Maintenance is the extent to which a program or policy becomes part of the routine organizational practices/policies and includes evolution over time and reinforcing factors. NYPS SelectHealth has integrated the creation of CCDs and use of My Health Profile into its operational activities. Four hundred members, 78.6% of the 509 individuals trained, have active accounts. The remainder is no longer with SelectHealth. The system evolved over time from the initial version on the OnFile platform. During the fourth year of the project, a second generation PHR, My Health Profile Plus, was developed and included a change in data source to include Regional Health Information Organization (RHIO) data and a change in user interface and functions including data entry. This version is not the focus of this report but the enhanced RHIO network is the foundation for the next iteration, which is underway and focuses upon creating a user interface for those with low health literacy levels. The primary reinforcing factors for maintenance are continued organizational commitment and the use of HIE standards.
5. Discussion
Many PLWH have high rates of complex medical co-morbidities, live amidst endemic poverty, and struggle with low health literacy. Collectively, these challenges, and others, often thwart the potential positive health benefits of universal access to antiretroviral therapy and basic clinical care. Multiple strategies to mitigate these factors and address ongoing barriers to care engagement have been proposed, including the provision of electronic personal health management tools to help manage overall care, increase health literacy, and promote self-efficacy [23]. Personal health records, especially those that are connected, or “tethered” to health information exchanges and offer easy access to consumers, have been cited as a potentially important HIT intervention to mitigate barriers engendered by fragmented healthcare systems. Indeed a large number of national and international health care redesign efforts and HIT policy initiatives have focused upon the evolution of PHR technology as a critical important component of a suite of HIT tools necessary to achieve high-quality health outcomes on a population level. However, concerns with regard to consumer acceptance and use, especially with regard to safety-net populations with often low health literacy levels, unstable housing, and limited access to the Internet and other digital tools, have been raised as potentially important barriers to PHR adoption [24–27] although only a limited number of studies have evaluated the impact of these barriers on PHR acceptance and use [27, 28].
The current report adds to the body of evidence that suggests PLWH, in this study a high-risk population with high levels of complex comorbidities, endemic poverty, modest educational levels, minimal experience with HIT, and limited access to the Internet, will accept and use a simplified PHR, a CCD, designed to foster improved clinical care and care coordination at rates comparable to more affluent, educated, and IT experienced healthcare consumers [29–30] when strategies addressing basic computer and PHR-specific training needs, Internet access, and privacy and security concerns are included as part of implementation efforts.
PHR acceptance and use in this high-risk population appears, however, to be sensitive to a number of important factors. Notably, while the percentage of plan members who received My Health Profile training and subsequently used the PHR approached 15% during the 2nd and 3rd years of the project, rapid growth in plan membership in subsequent years led to an overall decline in the percentage of total My Health Profile users as project training and support resources did not increase commensurably to match the volume of new members during the period of rapid plan growth. As expected, prior Internet experience was associated with use, but My Health Profile uptake occurred in both existing and new users of the Internet. In fact, participation in ACASI data collection itself proved to be an important motivator of use among those with limited computer experience. Furthermore, results from pre-implementation focus groups strongly supported general computer/Internet and My Health Profile training as important facilitators of My Health Profile acceptance and use.
Project training and support resources were provided by a number of SelectHealth’s permanent member services staff but the role of a dedicated My Health Profile community coach was critical to the project’s overall success and specifically with efforts during the implementation phase to promote My Health Profile use. In addition, the community coach greatly augmented efforts to promote effective strategies to extend and strengthen the reach of the initiative throughout the plan membership by ensuring that training materials, program promotional events, and informational mailings where delivered in a culturally-competent context and carefully attuned to the health literacy level of the target audience in general. Collectively, these ‘human touch’ measures proved an essential component of the My Health Profile project as illustrated by the decline in the percentage of members trained when the plan size grew rapidly during the later years of the project. These findings underscore the need for budgeting adequate human resources in addition to technology when wide-scale HIT projects are undertaken in high-risk populations.
PLWH assessed in this study also reported high levels of trust in their care providers and willingness to share personal health information with clinicians involved with their care. The fact that My Health Profile use did not vary by age, race, ethnicity, or gender suggests that further research is needed to explore other types of predictors of use.
Using ACASI data, we did not find significant differences between users and non-users of My Health Profile on secondary outcomes such as self-report of skipping ART, having an undetectable viral load, perceptions of the quality of medical care or healthcare service utilization (emergency department visit or hospitalization). The lack of differences may be due to low statistical power because of the small sample size in the analysis (n=82) or the relatively short duration of use between the two measurements (6–12 months). Moreover, only 43 of 112 My Health Profile users were in the analysis; two high-volume users with 22 and 39 logins were excluded because they only had one measure. Recall bias due to self-report is also a consideration. Despite these limitations, it is of note that the measure most proximal to PLWH behavior – skipping ART – was closest to the typical statistical criterion of .05 for level of significance.
The study also underscores the importance of utilizing an evaluative framework designed to capture not just the efficacy of the intervention but the fuller story of complex, real-world HIT project implementations. As previously noted evaluation frameworks such as RE-AIM expand the dimensions of evaluation and help better capture important HIT implementation facilitating and impeding factors. In this study, RE-AIM was particularly useful as a strategies for triangulating findings across the variety of data sources.
Finally, results from this study support the position that consumers perceive potential benefit from being able to directly access their clinical and care coordination information. My Health Profile users and other study participants were largely from underserved, socioeconomically marginalized communities that have not been thoroughly studied with regard to their views regarding PHI sharing, interest in directly accessing personal health information, or understanding the barriers and facilitating factors related to acceptance and use of PHRs. The need for such consumer access and engagement with HIT tools like My Health Profile appear to be great. For example, SelectHealth Emergency Department utilization data revealed that more than 50% of ED visits occur at institutions other than where a member’s primary care was provided (unpublished data). This finding coupled with the substantial barriers emergency department clinicians report accessing critical clinical information on patients from both within and without their respective institutions [31, 32] underscore the criticality of direct patient access to PHRs populated with HIE data as potentially an important initiative to pursue.
The study findings, however, must be interpreted in the context of several limitations. First, the study was limited to a single SNP and a single system, My Health Profile. Second, the rapid and significant growth in SelectHealth membership without an increase in project resources may underestimate the potential for acceptance and use. Third, the findings may be different for other high-risk PLWH not represented in the study sample.
Nevertheless, supporting the ability of consumers to connect directly to their personal health information aggregated at sites of care has long been seen as an important adjunct to consumer empowerment, care coordination, and improved health outcomes [30,33,34]. Interestingly, despite widespread calls for the development of such systems as part of regional, state, and national HIE implementation few descriptions of functioning PHRs tethered to HIEs have been reported. In an effort to address this lagging component of the national HIT agenda, the Health IT Policy Committee of the Office for the National Coordinator (ONC) for Health Information Technology recently rearticulated their Consumer e-Health Program Mission, namely “to empower consumers to be partners in their health through information technology”. The Committee further stated a suggested strategic approach that included:
Access: Give consumers easier access to their personal health information. Make “real” what is already required by law.
Action: Support the development of tools and services that help consumers to take action using their electronic health information.
Attitude: Support the evolution in expectations regarding access to and use of health information to engage more fully in health.
PLWH, and other high-risk populations, are perhaps uniquely positioned to benefit most from direct access to their personal health information as associated barriers regarding access to care, housing instability, and an often revolving door of healthcare providers, potentiate the problems associated with already fragmented and overly complex healthcare delivery systems. SelectHealth’s My Health Profile, and other forms of PHRs tethered to HIEs, are perhaps the ideal mechanism to ensure that essential health information, or ‘actionable information’, is available at the right time and right place [35]. Given the relative restive pace of inter-institutional HIE, advancement of a consumer-centric model of health information aggregation, access, and control is critical.
Study findings suggest that PLWH will adopt and utilize PHRs that broadly support the sharing of personal health information when care is taken to address privacy and security concerns, and that such projects are sustainable when aligned with organizational priorities. Collectively these findings support the position advocated by the Office for the National Coordinator for Health Information Technology’s Policy Committee calling for greater vigor in establishing consumer access to PHI, better HIT tools to facilitate access, and the seeking of a ‘pledge’ from data holders to commit to make health information easily accessible electronically to individuals.
Summary points.
What is already known on the topic?
PHRs are becoming increasingly available to consumers
Rates of adoption are often low despite general perception of usefulness by consumers
High-risk populations often suffer fragmented healthcare delivery and advances in HIT may represent an important opportunity to address this complex problem
What this study added to our knowledge?
People Living with HIV (PLWH) are largely willing to share PHI via a HIE when security and privacy concerns are sufficiently addressed
A population of PLWH, a group typified by endemic poverty and modest health literacy, will adopt a limited PHR at rates similar to more affluent and educated populations when training and ongoing support is provided
Capturing important HIT project implementation characteristics critical for understanding determinants of success may require novel mixed methods evaluative approaches and an integrative evaluation framework
Acknowledgments
The authors would like to acknowledge the many consumers, case managers, and clinicians who graciously volunteered their time to participate in focus groups, interviews, and ACASI sessions. In addition, a number of individuals assisted in organizing and conducting the project and evaluation. Special thanks to Paul Teixeira for his contributions to studying willingness to share PHI and Tom Moore and Gil Kuperman for providing leadership and technical assistance regarding RHIO and My Health Profile plus integration efforts and development.
The implementation and evaluation of NewYork Presbyterian System SelectHealth’s Continuity of Care Record Demonstration Project is funded through a Human Resources and Services Administration Special Projects of National Significance Grant (H97HA08483).
Footnotes
Authors’ contributions
Peter Gordon, MD: (1a) the conception and design of the study (Principal Investigator); (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Eli Camhi, MSSW: (1a) the conception and design of the study (Co-principal Investigator); (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Ron Hesse: (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Michelle Odlum, MPH, MS, EdD: (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Rebecca Schnall, RN, PhD: (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Martha Rodriguez, BA: (1b) acquisition of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Esmerlin Valdez: (1b) acquisition of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval
Suzanne Bakken, RN, DNSc: (1a) the conception and design of the study (Evaluation Director); (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Conflict of interest statement
None
References
- 1.Centers for Disease Control and Prevention. HIV in the United States. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [updated 2011; cited 2012 January 25]; Available from: http://www.cdc.gov/hiv/resources/factsheets/PDF/us.pdf. [Google Scholar]
- 2.Nakagawa F, Lodwick RK, Smith CJ, Smith R, Cambiano V, Lundgren JD, et al. Projected life expectancy of people with HIV according to timing of diagnosis. AIDS. 2012;26(3):335–343. doi: 10.1097/QAD.0b013e32834dcec9. [DOI] [PubMed] [Google Scholar]
- 3.May MT, Ingle SM. Life expectancy of HIV-positive adults: a review. Sex Health. 2011;8(4):526–533. doi: 10.1071/SH11046. [DOI] [PubMed] [Google Scholar]
- 4.Dombrowski JC, Kent JB, Buskin SE, Stekler JD, Golden MR. Population-based metrics for the timing of HIV diagnosis, engagement in HIV care, and virologic suppression. AIDS. 2012;26(1):77–86. doi: 10.1097/QAD.0b013e32834dcee9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feldman I, Cruz H, DeLorenzo J, Hidalgo J, Plavin H, Whitaker J. Developing a managed care delivery system in New York State for Medicaid recipients with HIV. Am J Manag Care. 1999;5(11):1457–1465. [PubMed] [Google Scholar]
- 7.Tesoriero J, Gieryic S, Carrascal A, Lavigne H. Smoking among HIVpPositive New Yorkers: prevalence, frequency, and opportunities for cessation. AIDS and Behavior. 2010;14(4):824–835. doi: 10.1007/s10461-008-9449-2. [DOI] [PubMed] [Google Scholar]
- 8.Verucchi G, Calza L, Manfredi R, Chiodo F. Human immunodeficiency virus and hepatitis C virus coinfection: epidemiology, natural history, therapeutic options and clinical management. Infection. 2004;32(1):33–46. doi: 10.1007/s15010-004-3063-7. [DOI] [PubMed] [Google Scholar]
- 9.Hayrinen K, Saranto K, Nykanen P. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform. 2008;77(5):291–304. doi: 10.1016/j.ijmedinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Appari A, Carian EK, Johnson ME, Anthony DL. Medication administration quality and health information technology: a national study of US hospitals. J Am Med Inform Assoc. 2012;19(3):360–367. doi: 10.1136/amiajnl-2011-000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazarus R, Klompas M, Campion FX, McNabb SJ, Hou X, Daniel J, et al. Electronic support for public health: validated case finding and reporting for notifiable diseases using electronic medical data. J Am Med Inform Assoc. 2009;16(1):18–24. doi: 10.1197/jamia.M2848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Healthy People 2020. Washington, DC: US Department of Health and Human Services; 2011. [updated 2011; cited 2012 January 26]; Available from: http://healthypeople.gov/2020/topicsobjectives2020/default.aspx. [Google Scholar]
- 13.Kibbe DC, Phillips RL, Jr, Green LA. The continuity of care record. Am Fam Physician. 2004;70(7):1220, 1222–1223. [PubMed] [Google Scholar]
- 14.Dolin RH, Giannone G, Schadow G. Enabling joint commission medication reconciliation objectives with the HL7 / ASTM Continuity of Care Document standard. AMIA Annu. Symp. Proc.; 2007; pp. 186–190. [PMC free article] [PubMed] [Google Scholar]
- 15.Ferranti JM, Musser RC, Kawamoto K, Hammond WE. The clinical document architecture and the continuity of care record: a critical analysis. J Am Med Inform Assoc. 2006;13(3):245–252. doi: 10.1197/jamia.M1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 17.Tang PC, Lee TH. Your doctor’s office or the Internet? Two paths to personal health recores. N Engl J Med. 2009;360(13):1276–1278. doi: 10.1056/NEJMp0810264. [DOI] [PubMed] [Google Scholar]
- 18.Silvestre AL, Sue VM, Allen JY. If you build it, will they come? The Kaiser Permanente model of online health care. Health Aff (Milwood) 2009;28(2):334–344. doi: 10.1377/hlthaff.28.2.334. [DOI] [PubMed] [Google Scholar]
- 19.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bakken S, Ruland CM. Translating clinical informatics interventions into routine clinical care: how can the RE-AIM framework help? J Am Med Inform Assoc. 2009;16(6):889–97. doi: 10.1197/jamia.M3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Odlum M, Gordon P, Camhi E, Schnall R, Teixeira P. Perceptions of predisposing, enabling, and reinforcing factors impacting the use of a Continuity of Care Document in special needs PLWH. Journal of Healthcare for the Poor and Underserved. 2012;23(4):1457–1476. doi: 10.1353/hpu.2012.0172. [DOI] [PubMed] [Google Scholar]
- 22.Teixeira PA, Gordon P, Camhi E, Bakken S. HIV patients’ willingness to share personal health information electronically. Patient Educ Couns. 2011;84(2):e9–12. doi: 10.1016/j.pec.2010.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kahn JS, Aulakh V, Bosworth A. What it takes: charactertistics of the ideal personal health record. Health Aff (Milwood) 2009;28(2):369–376. doi: 10.1377/hlthaff.28.2.369. [DOI] [PubMed] [Google Scholar]
- 24.Lober WB, Zierler B, Herbaugh A, Shinstrom SE, Stolyar A, Kim EH, et al. Barriers to the use of a personal health record by an elderly population. AMIA Annu. Symp. Proc.; 2006; pp. 514–8. [PMC free article] [PubMed] [Google Scholar]
- 25.Wen KY, Kreps G, Zhu F, Miller S. Consumers’ perceptions about and use of the internet for personal health records and health information exchange: analysis of the 2007 Health Information National Trends Survey. J Med Internet Res. 2010;12(4):e73. doi: 10.2196/jmir.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weitzman ER, Kaci L, Quinn M, Mandl KD. Helping high-risk youth move through high-risk periods: personally controlled health records for improving social and health care transitions. J Diabetes Sci Technol. 2011;5(1):47–54. doi: 10.1177/193229681100500107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. BMJ. 2010;341:c5814. doi: 10.1136/bmj.c5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Curtis J, Cheng S, Rose K, Tsai O. Promoting adoption, usability, and research for personal health records in Canada: the MyChart experience. Healthc Manage Forum. 2011;24(3):149–54. doi: 10.1016/j.hcmf.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 29.Undem T. Consumers and Health Information Technology: A National Survey. Oakland, CA: California HealthCare Foundation; 2010. Contract No.: Document Number|. [Google Scholar]
- 30.Patel VN, Dhopeshwarkar RV, Edwards A, Barron Y, Likourezos A, Burd L, et al. Low-income, ethnically diverse consumers’ perspective on health information exchange and personal health records. Inform Health Soc Care. 2011;36(4):233–252. doi: 10.3109/17538157.2011.554930. [DOI] [PubMed] [Google Scholar]
- 31.Baumlin KM, Genes N, Landman A, Shapiro JS, Taylor T, Janiak B. Electronic collaboration: using technology to solve old problems of quality care. Acad Emerg Med. 2010;17(12):1312–1321. doi: 10.1111/j.1553-2712.2010.00933.x. [DOI] [PubMed] [Google Scholar]
- 32.Finnell JT, Overhage JM, Grannis S. All Health Care is Not Local: An Evaluation of the Distribution of Emergency Department Care Delivered in Indiana. AMIA Annu. Symp. Proc.; 2011; pp. 409–416. [PMC free article] [PubMed] [Google Scholar]
- 33.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–6. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krist AH, Peele E, Woolf SH, Rothemich SF, Loomis JF, Longo DR, et al. Designing a patient-centered personal health record to promote preventive care. BMC Med Inform Decis Mak. 2011;11:73. doi: 10.1186/1472-6947-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Health IT Policy Committee. Consumer e-Health Program Update and Strategy Discussion. Office of the National Coordinator for Health Information Techology; 2011. Contract No.: Document Number|. [Google Scholar]