Abstract
Child obesity continues to be a prevalent public health issue. This meta-analysis synthesized 17 studies investigating the association between levels of psychological stress experienced by mothers and the body mass index of their children. The overall standardized mean difference effect size was positive and significantly different from zero in cross-sectional d = 0.20 [k = 14, 95% Confidence Interval (CI): 0.06, 0.34] and longitudinal studies d = 0.18 (k = 5, 95% CI: 0.00, 0.351), and had significant heterogeneity in both [cross-sectional, Q(13) = 193.00, p < 0.001; longitudinal, Q(4) = 29.46, p < 0.001]. In longitudinal studies, effect sizes were larger when children also would have experienced the stressor, Q(6) = 4.68, p < 0.05, for toddlers than infants, Q(4) = 5.04, p < 0.05, and in higher quality studies, Q(4) = 14.58, p < 0.05. Results highlight the potential benefits of including a parent stress management component in childhood obesity prevention programs.
Keywords: maternal stress, child obesity, body mass index, stress
In 2007–2008, 9.5% of infants and toddlers in the United States and 16.9% of children aged 6 to 19 years were estimated to be obese 1. Child obesity prevention programs typically emphasize making changes to children’s diet and physical activity behaviors, and such programs have shown moderate success 2, 3. Although including child caretakers has been recommended for boosting obesity prevention program success, 4 targeting specific changes in mothers’ behaviors has not often been a focus of childhood obesity prevention programs. Programs that have targeted parenting practices, such as child-feeding strategies, rarely address issues such as parents’ depression, emotional distress, or anxiety 5. Yet parents of overweight and obese children report higher rates of negative emotions 6, 7. Growing evidence suggests that mothers’ psychological stress is associated with children’s decreased consumption of fruits, vegetables and high-calcium foods 8, as well as lower physical activity parenting, perceived lower importance of child physical activity, and higher child sedentary behavior 9, 10. These behaviors increase children’s risk for obesity or compromised nutritional status 5, 7, 11–17. Studies examining different facets of parental stress such as social, financial, and parenting stress show associations with increased rates of obesity in children 15, 17, 18. However, not all studies find a significant relationship between parental stress and child obesity risk.19–21 Conflicting findings underscore the need for conclusive, summative evidence.
Untested moderators such as type of maternal stress, child’s own experience of stress, and child age may account for the observed inconsistencies in the size and direction of the association between maternal stress and child obesity. In particular, mothers’ stress that is specifically tied to parenting may be associated with child obesity risk in ways that differ from other types of stress. Parenting stress is characterized by feelings of distress combined with a dysfunctional parent-child relationship and a difficult child. 22, 23 Parenting stress has been shown to interact with parenting behaviors, 24 but whether its effect on child obesity risk is stronger than that of generalized stress remains an open question. In addition, children’s experience of stress may exacerbate the effects of maternal stress on children’s obesity risk. In children, chronic stress repeatedly activates the hypothalamic-pituitary-adrenal axis (HPA) and release of stress hormones (e.g., glucocorticoids), which are associated with subsequent metabolic syndrome, including visceral adiposity, with particularly damaging effects during crucial stages of brain development 25–27. Stressors experienced by the child, such as maltreatment and abuse, have been associated with higher rates of concurrent and subsequent obesity 28, 29. Finally, child age may moderate the relationship between maternal stress and child obesity, with a smaller effect for older children. Although parent feeding practices play an important role in child eating behaviors, childcare and school settings have an increasingly strong influence as children spend more time away from home with age 30. Peers and media also contribute to child dietary consumption patterns 31, and media exposure may increase as children age. For infants, the introduction of solid foods creates variability in their diet, and consistent provision of healthy foods in appropriate quantities could be disrupted by maternal stress. Child age could be a proxy for these types of changes, reducing the effect of maternal stress on the incidence of child obesity risk for older children.
The current meta-analysis synthesized data from cross-sectional and longitudinal studies measuring the association between maternal stress and child obesity in order to estimate an overall effect size and test moderators of the effect. Data from cross-sectional studies were expected to provide evidence about whether there are concurrent, but not necessarily directional, associations between stress and obesity. Results from longitudinal studies were expected to shed light on whether maternal stress, especially coupled with children’s stress or present during critical periods of development, increased children’s subsequent obesity risk. Based on the existing evidence, we hypothesized that the effect size for maternal stress and child BMI would be (a) positive, (b) larger when children would have also experienced the stressor, and (c) smaller for older children.
Method
Sample of studies and inclusion criteria
Literature searches were conducted between February 5 and June 25 of 2014 using Google Scholar, Web of Science, PyscINFO, PsycEXTRA, ProQuest. Search terms and logic relations were: (maternal OR mother) AND (stress OR allostatic load OR stressor) AND “child BMI” OR “obesity” NOT prenatal NOT rat NOT "in utero"). Ancestral searches were conducted from reference sections of articles retrieved via database searches. Author websites were searched for unpublished or additional published results on the topic, and requests for unpublished data were sent to the listservs of the American Public Health Association and the Society for Behavioral Medicine. To be included in this review, studies had to (a) be conducted on a human population, (b) include mother-child dyads in which children were 18 years of age or younger, (c) measure stress that mothers experienced after the child’s birth, (d) report the relationship between maternal stress and a measure of child obesity (e.g., BMI z-score, BMI > 95th percentile, waist circumference), and (e) be a quantitative (vs. qualitative) study. Studies not reported in English were excluded.
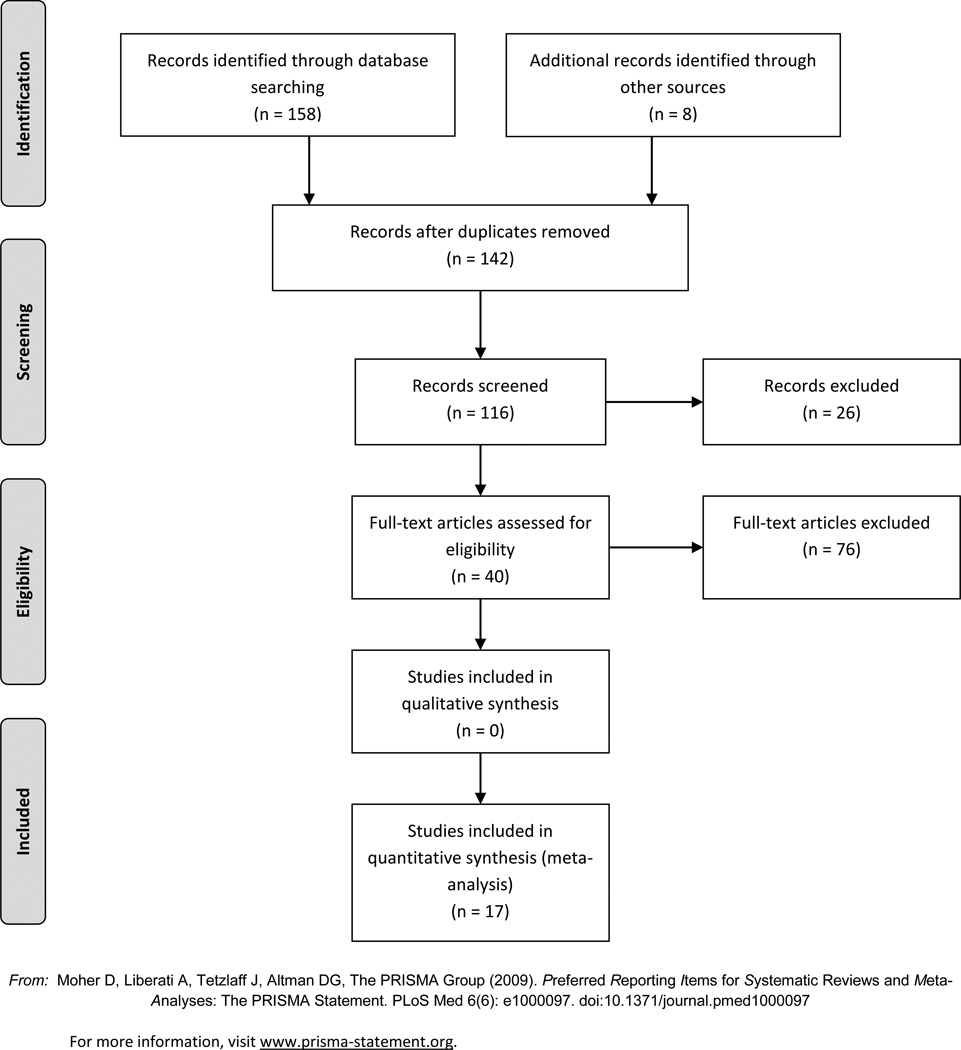
Database, ancestry searches, and personal communications returned 142 studies after removal of duplicates. Listserv requests returned zero. One study met screening criteria but was not included because it reported findings by categorizing children into “overweight” vs. “not overweight” based on adjusted relative weight over the 75th percentile according to the Department of Health Education and Welfare norms in 1979, which could not be compared to current BMI over the 95th percentile 32. Only one study was excluded because it used a measure of obesity that was not based on BMI or BMI z-score (i.e., waist-to-hip ratio)7. Two longitudinal studies used the same dataset (Fragile Families and Child Well-being Study; 17, 33 but calculated maternal stress exposure differently (exposure to intimate partner violence only vs. a composite score that included intimate partner violence, food insecurity, housing insecurity, maternal depressive symptoms, maternal substance use, and father’s incarceration). Effect sizes from those two studies were combined in the analysis. Two longitudinal studies used two different measures of “overall stress” (ex., composite stressors and perceived stress), 19, 34 which were combined to form one “overall stress” effect size per study.
Effect size estimation procedures
Odds ratios (OR), correlation coefficients, and regression coefficients were reported and retained for the meta-analysis. Odds ratios (OR) were retrieved directly from study results for both cross-sectional and longitudinal studies. ORs were converted into effect sizes and standard errors using ln-transformations, resulting in effect sizes comparable to standardized mean difference scores (d) 35. This method is provided in the Cochrane Handbook for Systematic Reviews of Interventions 36. A positive d indicated that higher maternal stress was associated with increased child obesity risk, whereas a negative d indicated that higher maternal stress was associated with reduced obesity risk. Effect sizes for correlations and regression coefficients, ds, and variance of ds were calculated according to the procedures outlined in Borenstein et al. 37.
Decision rules for lifting effect size information from study reports were as follows: When both Centers for Disease Control (CDC) and International Obesity Task Force (IOTF) cut-points were used to determine obesity status, CDC scores were retained to allow comparability with other studies 13. When ORs were given only for sub-groups (ex., gender), a summary OR was calculated using the overall summary effect procedures for fixed effects outlined in Borenstein (2011) 17. When ORs were presented at different levels of stress, we retained the comparison between high/chronic stress with low/no stress 17, 33. When a correlation or OR was tested but not reported as significant, it was assumed to be non-significant, and an effect size of 0 was imputed 38. In those cases, confidence intervals were calculated based on the assumption that equal numbers of participants would have fallen into each of the four cells of a 2×2 odds ratio table. Summary effect sizes were calculated with and without the imputed zero values, and the results are described below 38, 39. Studies were coded for the percentage of obese children in the sample and the presence of seven of the most common covariates reported by the included studies: race, marital status, age, socioeconomic status, education, general health, maternal obesity.
Coding for moderators
All coding and rating were performed by two authors independently, and initial agreement for each item ranged from 70% to 100%. All discrepancies were resolved through discussion. First, a code was created to reflect whether the maternal stress measure captured parenting stress specifically (Parenting Stress Index or subscale 14, 40–42, Swedish Parenting Stress questionnaire 18, 34) vs. an overall/composite measure of stress (cumulative maternal stressor index 11, cumulative social risk summary 17, Depression Anxiety Stress Scale 43, 44, General health questionnaire 19, Holmes and Raye Life Change Questionnaire 32, 39, intimate partner violence 33, Life event checklist + Swedish Parenting Stress Questionnaire + Quality of social support + Parental worries 34, Perceived Stress Scale 38, 45, Self-esteem + Brief symptom inventory + work stress + overall health + social support 13, Symptom Distress Checklist 19, Symptom Distress Checklist + Global Severity Index 46). Second, studies were coded for whether or not the child would most likely have experienced the same stress or stressor as the one captured by the maternal stress measure. Codes were assigned to indicate that children would have likely experienced the stress (cumulative maternal stressor, cumulative social risk index, Holmes and Raye Life Change questionnaire, intimate partner violence, Life event + SPSQ + quality of social support + parental worries, Parenting Stress Index, Swedish Parenting Stress Questionnaire). Studies that either controlled for child stress separately or used a maternal stress measure that reflected stress that the mother could have experienced outside the child’s realm were coded to reflect this (Depression Anxiety Stress Scale, General Health Questionnaire, Perceived Stress Scale, Self-esteem + Brief symptom inventory + work stress + overall health + social support, Symptom Distress Checklist, Symptom Checklist + Global Severity Index). Third, average child age when maternal stress was measured (“baseline” in longitudinal studies) was used as the indicator of child age.
Quality assessment
The Tool to Assess Risk of Bias in Cohort Studies was modified and used to evaluate study quality 47 (see supplement). One item assessed population representativeness, two items assessed risk of bias in stress and obesity measures, a fourth assessed self-selection bias, and a fifth assessed adjustment for baseline level of child weight/obesity (longitudinal only). Scoring options for each item ranged from 1 = High risk of bias to 4 = Low risk of bias. Higher scores indicated higher study quality.
Data analytic plan
Overall effect size, confidence intervals, and Q (standardized measure of heterogeneity within effect sizes) were calculated separately for cross-sectional and longitudinal studies using mixed-effects models. Mixed-effects models were used in the analysis. Comparisons across subgroups (e.g., parenting stress vs. overall stress) assumed a fixed variance across studies, indicating that the categories had a common meaning across studies. The variance within subgroups (e.g., parenting stress) was modeled as a random effect, indicating that effect sizes were randomly selected from multiple populations and did not necessarily reflect a single underlying mean value 37. Continuous moderators (i.e., child age, study quality) were tested using mixed-effects Method of Moments regression models. Analyses were conducted using Comprehensive Meta-Analysis Version 2 (2005) (http://www.meta-analysis.com/index.html).
Publication bias
Two techniques were used to assess potential publication bias. First, Egger’s test provided a significance value for the test of asymmetry of funnel plots; two-tailed tests are reported 48. Asymmetrical funnel plots suggest publication bias especially if less precise, small-sample studies are more likely to show effects in the predicted direction than more precise, large-sample studies. Second, Duval and Tweedie’s Trim & Fill (random effects) procedure was used to estimate the number of missing studies that would need to be added to create a symmetrical distribution around the observed overall effect size 49, 50.
Results
Descriptive statistics
The search process resulted in 17 studies with 21 effect sizes (15 cross-sectional, 6 longitudinal) (see Figure 1). Most studies adjusted for marital status (59%), child age (65%) (by study design or statistical adjustment), SES (71%), maternal education (82%), and maternal obesity (88%). Effect sizes from studies that adjusted for covariates did not differ significantly from those that did not. Thus, adjusted and unadjusted effect sizes within studies were pooled, leaving a total of 19 independent effect sizes (14 cross-sectional, 5 longitudinal). The percent of child obesity in the cross-sectional and longitudinal samples was not significantly associated with the effect size.
Figure 1.
PRISMA 2009 Flow Diagram
Tables 1 and 2 show study characteristics and descriptive statistics. Children in the cross-sectional studies were elementary school age (M = 6.36 yrs., SD = 3.23) but were younger at baseline in longitudinal studies (M = 1.68 yrs., SD = 1.38), p < 0.01. Average rates of child obesity were 17.6% (SD = 18.27%) for children and 7.9% (SD = 7.47%) for infants and toddlers, comparable to U.S. estimates 1. Studies were relatively balanced on child gender and were conducted in 5 different countries (i.e., Australia, Brazil, Denmark, Sweden, and United States). Sample size ranged from 110 mother-child dyads to 21,121, with a mean of 2,462 (SD = 4,980).
Table 1.
Study characteristics
| Study name | Dataset | d | SE | Maternal stress | Published | Sample size |
Country | Avg. child age |
Avg. mat. age |
Child Stress |
% Child obesity |
BMI method |
% Male | Study quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Longitudinal | ||||||||||||||
| (Ajslev et al., 2010) | Danish National Birth Cohort | −0.002 | 0.010 | Stress | Yes | 21121 | Denmark | 7.00 | 30.69 | No | -- | Reported | -- | 2.800 |
| (Bergmeier et al., 2014) | Australian Research Council Discovery | 0.201 | 0.142 | Parenting stress | Yes | 201 | Australia | 3.92 | 36.11 | Yes | 3.0% | Assessed | 42.3% | 3.100 |
| (Boynton-Jarrett & Suglia, combined) | Fragile Families and Child Well-being Study | 0.266 | 0.084 | Stress | Yes | 1595 | USA | 5.00 | Yes | 16.5% | Assessed | 51.2% | 2.900 | |
| (Koch et al., 2008) | All Babies in Southeast Sweden-project | 0.523 | 0.124 | Stress | Yes | 5302 | Sweden | 5.00 | Yes | 4.2% | Assessed | 52.1% | 3.400 | |
| (Sowan & Stember, 2000) | Infant Growth Study | 0.000 | 0.080 | Stress | Yes | 630 | USA | 0.58 | Yes | 0.0% | Assessed | 54.0% | 2.800 | |
| Cross-sectional | ||||||||||||||
| (Bergmeier et al., 2014) | Australian Research Council Discovery | −0.040 | 0.141 | Parenting stress | Yes | 201 | Australia | 2.92 | 36.11 | Yes | 3.0% | Assessed | 42.3% | 3.125 |
| (Burdette et al., 2001) | Vermont Special Supplemental Nutrition Program | 0.000 | 0.315 | Stress | No | 150 | USA | No | -- | Assessed | -- | 3.375 | ||
| (Gemmill et al., 2013) | National Postnatal Depression Program | 0.873 | 0.174 | Stress | Yes | 159 | Australia | 4.82 | 37.00 | No | 10.1% | Reported | 45.3% | 2.625 |
| (Gibson et al., 2007) | Childhood Growth and Development Study | 0.020 | 0.110 | Stress | Yes | 329 | Australia | 9.51 | No | 12.2% | Assessed | -- | 3.750 | |
| (Gunderson et al., 2008) | National Health and Nutrition Examination Survey | 0.011 | 0.008 | Stress | Yes | 841 | USA | 8.30 | 32.32 | Yes | -- | Assessed | 54.4% | 3.000 |
| (Koch et al., 2008) | All Babies in Southeast Sweden-project | −0.006 | 0.119 | Parenting stress | Yes | 6603 | Sweden | 5.00 | Yes | 4.2% | Assessed | 52.1% | 3.500 | |
| (Koch et al., 2008) | All Babies in Southeast Sweden-project | 0.354 | 0.093 | Stress | Yes | 6106 | Sweden | 5.00 | Yes | 4.2% | Assessed | 52.1% | 3.625 | |
| (Ievers-Landis et al., 2008) | Cleveland Children’s Sleep and Health Study | −0.096 | 0.247 | Parenting stress | Yes | 819 | USA | 9.50 | Yes | 16.9% | Unknown | 51.0% | 3.000 | |
| (Lohman et al., 2009) | Welfare, Children, and Families: A Three-City Study | 0.037 | 0.031 | Stress | Yes | 1011 | USA | 38.32 | Yes | 20.0% | Assessed | 48.0% | 3.000 | |
| (McPhie et al., 2011) | Recruited for this study | 0.262 | 0.153 | Parenting stress | Yes | 175 | Australia | 2.83 | 35.69 | Yes | -- | Reported | 46.3% | 2.875 |
| (Rondó et al., 2013) | National Health Service (Sistema Unico de Saude) | −0.080 | 0.099 | Stress | Yes | 409 | Brazil | 6.50 | 30.70 | No | 4.2% | Assessed | 44.0% | 3.500 |
| (Stenhammar et al., 2010) | Child Public Health Unit in Uppsala County, Sweden | 0.850 | 0.069 | Parenting stress | Yes | 865 | Sweden | 3.00 | Yes | -- | Assessed | -- | 3.625 | |
| (Walton et al., 2014) | Parents and Tots Together | 0.003 | 0.298 | Parenting stress | No | 110 | USA | Yes | 48.5% | Unknown | -- | 3.750 | ||
| (Zeller et al., 2007) | Recruited for this study | 0.342 | 0.120 | Stress | Yes | 159 | USA | 12.59 | 40.53 | No | 52.3% | Assessed | 43.9% | 2.833 |
Table 2.
Descriptive Statistics for Cross-sectional and Longitudinal Studies
| Cross-sectional | Longitudinal | ||||
|---|---|---|---|---|---|
| Item | M (SD) or N (%) | M (SD) or N (%) | t-test or χ2 |
||
| Stress | |||||
| Stress measure | -- | ||||
| Parenting stress | 6 | 42.86 | 1 | 20.00 | |
| Stress | 8 | 57.14 | 4 | 80.00 | |
| Child stress | -- | ||||
| No | 5 | 35.71 | 1 | 20.00 | |
| Yes | 9 | 64.29 | 4 | 80.00 | |
| Avg. child age at mat. stress measure | 6.36 | 3.23 | 1.68 | 1.38 | 4.06** |
| Sample characteristics | |||||
| Percent child obesity | 17.55 | 18.27 | 5.93 | 7.27 | 1.70 |
| Percent male | 47.94 | 4.20 | 49.90 | 5.20 | −0.67 |
| Mother’s average age | 35.81 | 3.38 | 33.40 | 3.83 | 0.80 |
| Avg. age child at obesity measure | 6.36 | 3.23 | 4.30 | 2.36 | 1.44 |
| Country of origin | -- | ||||
| Australia | 4 | 28.57 | 1 | 20.00 | |
| Brazil | 1 | 7.14 | 0 | 0.00 | |
| Denmark | 0 | 0 | 1 | 20.00 | |
| Sweden | 3 | 21.43 | 1 | 20.00 | |
| United States | 6 | 42.86 | 2 | 40.00 | |
| Methodological features | |||||
| Outcome Assessment type | -- | ||||
| Assessed | 10 | 71.43 | 4 | 80.00 | |
| Self-report | 2 | 14.29 | 1 | 20.00 | |
| Unknown | 2 | 14.29 | 0 | 0.00 | |
| Sample size | 1281.20 | 2174.70 | 5769.80 | 8813.90 | −1.13 |
| Publication year | 2009.40 | 3.52 | 2008.00 | 5.89 | 0.44 |
| Study quality | 3.26 | 0.38 | 3.00 | 0.26 | 1.69 |
< 0.01
too few studies to estimate significance values
Note: Satterthwaite t-test results are reported, which assume unequal variances
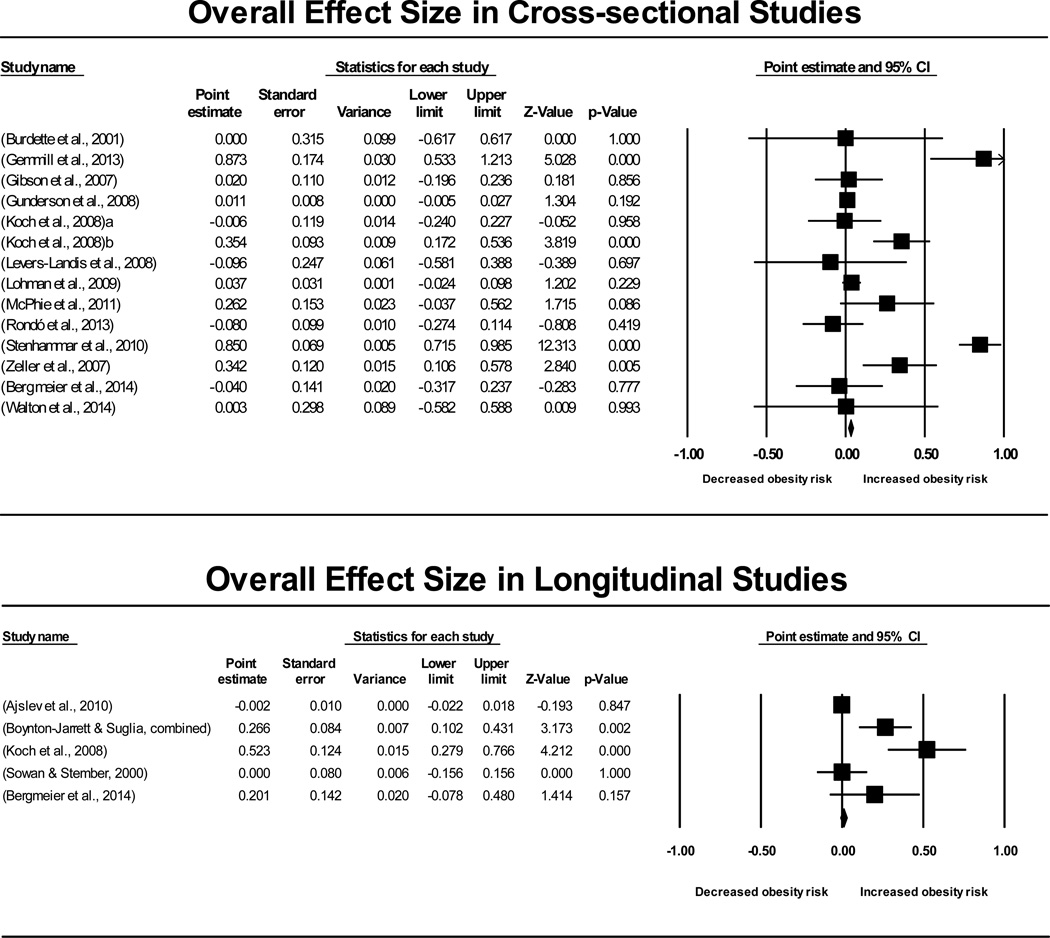
Overall Effect Size for Association between Maternal Stress and Child Obesity
For cross-sectional studies, the overall effect size between maternal stress and child obesity was positive and significantly different from zero, d = 0.20 (k = 14, 95% CI: 0.06, 0.34) and had significant heterogeneity, Q(13) = 193.00, p < .001 (see Table 3). The overall effect size was not changed by excluding the imputed effect size of 0 for one study 38, d = 0.20 (k = 13, 95% CI: 0.06, 0.35, p = 0.006, Q(12) = 192.99, p < .001. For longitudinal studies, the overall effect size between maternal stress and child obesity was marginally significant, d = 0.18 (k = 5, 95% CI: 0.00, 0.35, p = 0.05) and had significant heterogeneity, Q(4) = 29.46, p < .001.
Table 3.
Effect Sizes by Moderator for Cross-sectional and Longitudinal Studies
| Cross-sectional | Longitudinal | |||||
|---|---|---|---|---|---|---|
| Effect size estimate | Effect size estimate | |||||
| Moderator | k | Q | d or slope (95% CI) | k | Q | d or slope (95% CI) |
| Overall effect | 14 | 193.00** | 0.196** (0.056 / 0.337) | 5 | 29.461** | 0.176‡ (0.000 / 0.351) |
| Stress measure | 0.022 | 0.026 | ||||
| Parenting stress | 6 | 0.181 (−0.236 / 0.598) | 1 | 0.201 (−0.078 / 0.480) | ||
| Overall stress | 8 | 0.148** (0.038 / 0.258) | 4 | 0.173 (−0.026 / 0.371) | ||
| Child stress | 0.74 | 4.679* | ||||
| No | 5 | 0.232 (−0.086 / 0.550) | 3 | −0.002 (−0.022 / 0.018) | ||
| Yes | 9 | 0.182* (0.008 / 0.355) | 4 | 0.237* (0.021 / 0.453) | ||
| Child age^ | 11 | 1.162 | −0.034 (−0.096 / 0.028) | 5 | 5.037* | 0.110* (0.014 / 0.206) |
| Study quality | 14 | 0.224 | −0.090 (−0.461 / 0.282) | 5 | 14.581* | 0.858** (0.418 / 1.298) |
p < 0.01,
p < 0.05,
p = 0.05
Child age at maternal stress measure
Putative moderators of the association between maternal stress and child obesity
The comparison between types of stress (parenting versus overall) did not reach significance for the cross-sectional, Q(1) = 0.02, p = .881, or longitudinal studies, Q(1) = 0.026, p = .871.
For cross-sectional studies, the comparison between children who would have experienced stress versus those who would not was not significant, Q(1) = 0.74, k = 14, p = .785, indicating that the relationship between maternal stress and child obesity is relatively constant across levels of child stress. However, the comparison was significant in longitudinal studies, Q(1) = 4.68, p = 0.031 reflecting that the effect size was larger for children who would have experienced stress, d = 0.24, k = 4, 95% CI: 0.02, 0.45, than those who would not, d = 0.00, k = 3, 95% CI: −0.02, 0.02.
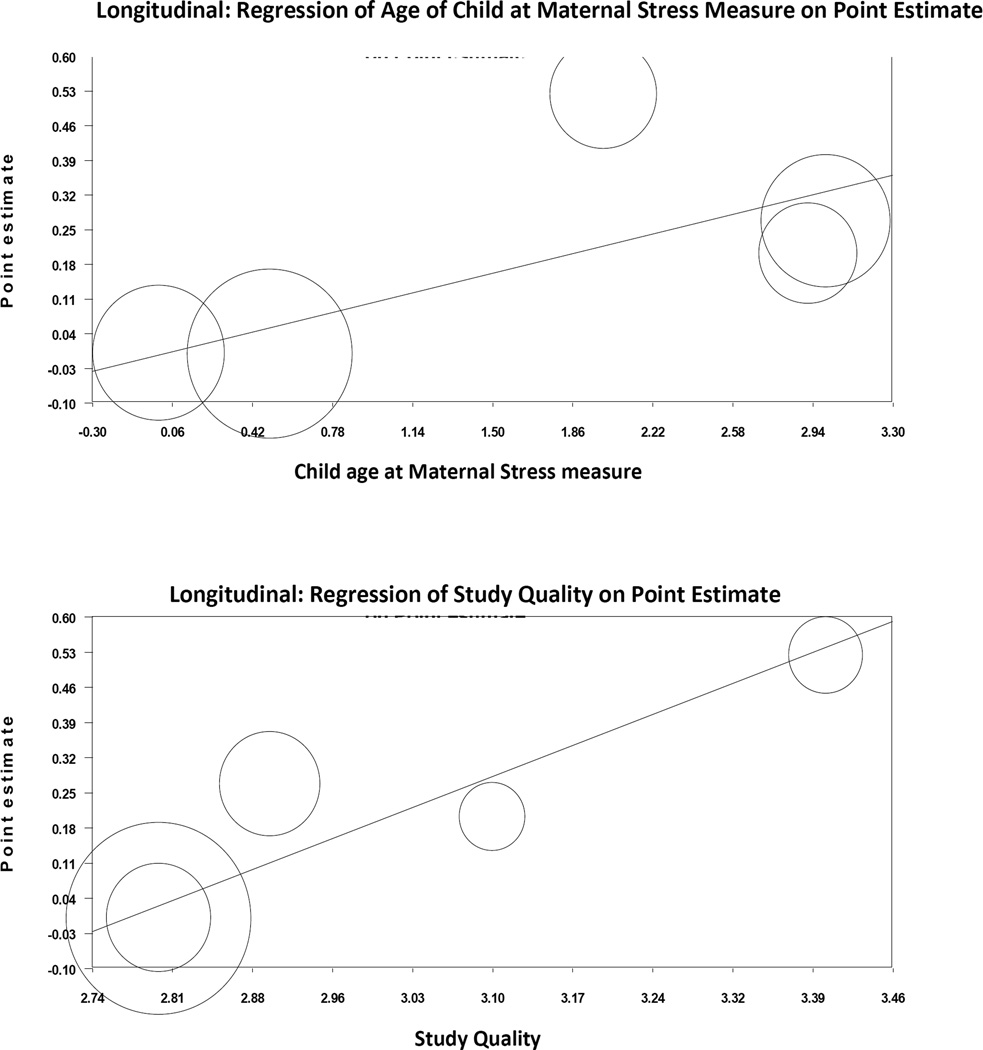
In cross-sectional studies, child age at maternal stress assessment was not significantly associated with effect size (B = −0.03, k = 11, 95% CI: −0.10, 0.03), Q(1) = 1.16, p = 0.281, suggesting that the effect size was relatively constant for children aged 3 – 13 years (3 studies did not provide sufficient information). However, in longitudinal studies, which had an age range of 0 – 3 years at baseline, older age at baseline was associated with a larger effect size (B = 0.11, k = 5, 95% CI: 0.01, 0.21), Q(1) = 5.04, p = 0.025 (see Figure 3).
Figure 3.
Regression of Effect Size on Age of Child at Maternal Stress Measure and Study Quality in Longitudinal Studies
Study quality
Study quality was not significantly associated with effect size in cross-sectional studies (B = −0.09, k = 14, 95 % CI: −0.46, 0.28), Q(1) = 0.22, p = 0.636 but was associated with a larger effect size in longitudinal studies (B = 0.86, k = 5, 95% CI: 0.42, 1.30), Q(1) = 14.58, p < 0.001 (see Figure 3), indicating that higher quality studies had larger effect sizes.
Publication Bias
For cross-sectional studies, the Egger’s regression test was not significant, t(12) = 1.72, p = 0.112, suggesting a symmetrical funnel plot and no publication bias. Similarly, Duval and Tweedie’s technique estimated that no missing studies would be required to create a symmetrical distribution, also indicating no bias. The pattern was similar for longitudinal studies. Neither Egger’s test, t(3) = 2.38, p = 0.097, nor Duval and Tweedie’s technique indicated publication bias.
Discussion
As child obesity continues to be a public health problem, discovering parental factors that influence obesity risk provides new targets for intervention and prevention. Results of this meta-analysis indicate that maternal stress may be one such factor. Across study designs, children were at greater risk of obesity when mothers experienced stress. For longitudinal studies, higher study quality was associated with larger effect sizes, supporting the validity of the results.
Our results support theoretical predictions that maternal stress may reduce proactive obesity-related parenting practices 13, 51, 52 or affect weight gain through changes in maternal or child mental health. According to household production theories and family stress theory, maternal stress could change parenting behavior, such as meal preparation or transportation to organized sports, in ways that ultimately increase obesity risk. 8–10, 13, 51 Maternal stress may also reduce parent sensitivity or disrupt bonds of secure attachment formation, decreasing children’s ability to learn self-regulation skills, such as control of eating behavior. 52, 53 While no other studies, to our knowledge, have systematically examined maternal stress in this way, one review found that chronic maternal depression was linked to greater risk for child overweight.54 Thus, our study extends previous work to paint a fuller picture of the “family ecology”54 that might identify higher risk children. Obesity prevention programs and policies aimed at parents and families may want to consider the important influence of maternal stress.
Children’s own experience of stress seemed to exacerbate the association between maternal stress and subsequent higher child obesity risk. This finding fits with previous research confirming a positive association between chronic stress and obesity in children, although studies have been mixed regarding longitudinal effects 55. Children’s experience of chronic stress could increase energy intake, decrease physical activity, or stimulate visceral fat accumulation through elevated cortisol secretion 55, 56. Among adolescents, stress-related eating has been shown to co-occur with other unhealthful habits, such as inadequate sleep or high-calorie/low-nutrient food consumption 57. Child stress may interact with other stressors to decrease physical activity, such as family financial strain 10 or natural disasters 58. This finding brings to light the possibility that maternal stress is only a risk factor for subsequent child obesity risk when the child also experiences stress. The two main types of child stress that appeared in the current review were environmental/external stressors and mother-child dysfunctional relationship. Stress that mothers experienced outside of those domains, such as work-related difficulties, did not heighten child risk of obesity. However, in the cross-sectional studies, this was not the case. On a cross-sectional basis, child risk was equally high whether or not the children would have experienced the stress(or). Combined, these findings indicate that maternal stress identifies concurrent child obesity risk but not subsequent risk, unless the stressor also affects the child. Combined, these findings indicate that maternal stress identifies concurrent child obesity risk but not subsequent risk, unless the stressor also affects the child. This discovery should be tested in subsequent studies but suggests that policy-makers and program designers focused on primary prevention consider addressing both mother's and children's stress.
This meta-analysis also revealed that toddlers may be more susceptible to the effects of maternal stress on obesity than infants. Results from longitudinal studies indicated that the effect of maternal stress on child obesity was stronger when the stressor occurred during the toddler years than infancy. Yet across the ages of 3 – 13 years, as found in the cross-sectional studies, the effect size was relatively consistent. Different age ranges in the cross-sectional and longitudinal studies likely account for these different results. Maternal stress may have little effect on the composition of the child’s nutritional intake if it is experienced before children have transitioned to solid foods only; but the wider variety of foods and greater time and preparation required for feeding solid foods may introduce variability into feeding practices that could be disrupted by stress and lead to excess weight gain. For older children, the impact of maternal stress may be diluted by a larger network of social influences and food environments.
Previous theory and research suggested a link between prenatal maternal stress and subsequent child obesity risk59, 60 but this meta-analysis is, to our knowledge, the first to synthesize results from maternal stress during infancy and childhood, finding higher risk from toddlerhood through adolescence. Given that eating preferences and self-regulatory ability can be established in childhood,61, 62 and that weight tends to track across development, childhood is an important target for prevention.63 Infancy may be a relatively lower-risk time because the content of the child’s diet is consistent (i.e., breast milk or formula). Preventing and treating maternal stress when children are toddler-age may be the most strategic intervention point for maternal stress-based policies and programs.
Various mechanisms may help explain the effect of maternal stress on child obesity, such as changes in obesity-related parenting practices, child internalizing symptoms, or increased maternal depression.9, 51, 64–66 Stressed mothers may be more likely to disengage from proactive physical activity parenting or healthy meal planning, resulting in higher fast-food consumption or altered feeding practices 9, 51, 15, 64. Parenting stress might also increase child internalizing symptoms (ex., depression, anxiety) 66, which have been associated with adolescent obesity 67, 68, weight gain as children age 69, and impaired adolescent weight loss 70 possibly due to changes in health behaviors, psychiatric medication, or sociobiological factors affecting both symptoms and weight 68. Chronic maternal stress could precipitate or exacerbate maternal depression, interact with parenting styles and increase child overweight 65, 71–73, 74. However, a post-hoc analysis conducted with the current data did not find a significant difference between measures of maternal stress that included mental health ratings, such as depression or anxiety, and those without (results not reported). Future research is needed to investigate how mental health may influence stress, interact with parenting practices or affect child internalizing symptomatology.
One limitation of the present research is that most of our studies were conducted in developed countries, potentially limiting global generalizability. One study conducted in a developing country found that maternal stress was associated with lower child obesity risk 45, and another found that the effect of poverty – a stressor – on child obesity risk differed by country 75. Possibly, maternal stress lowers mothers’ ability to protect children from environmental pressures, such as the marketing of unhealthy food products,76 pushing children toward obesity in countries where food is abundant but toward malnutrition in nutritionally impoverished areas. A post-hoc analysis with the current cross-sectional data suggested that SES may moderate the effect, with no effect among low-income populations (in developed countries) and a positive effect in the general population. However, the trend did not reach significance (p = 0.09, k = 14, results not reported), and there were a small number of effect sizes from low-income populations (n = 3). Finally, the relatively small number of studies included in the overall meta-analysis, especially longitudinal, underscores the need for additional research.
Conclusions and future research
Across study designs, children whose mothers who experienced stress were at greater risk for obesity. Longitudinal studies are needed to test changes over time, the mechanisms of transmission, establish the temporal order of the effect (i.e., maternal stress leads to child obesity), and assess whether reciprocal relationships occur across time. Some studies have begun to test mediators, such as child feeding practices 43, but effects on child weight are not consistent 20, and additional work is needed to clarify disparate findings. Intervention studies are needed to examine potential causal effects of maternal stress reduction on decreasing child obesity risk. Many studies, including this one, operate under the hypothesis that parenting behaviors increase child risk, but the causal arrow could run in the opposite direction, with the diagnosis of an obese child heightening parent stress or altering parenting behaviors. Additional research is needed that uses consistent measures of maternal stress (e.g., Cohen’s Perceived Stress scale) and alternative methods of assessment such as ecological momentary assessment77, salivary cortisol78, waist-to-height ratios79, or dual energy X-ray absorptiometry (DEXA)80 scans to clarify whether differences exist that are not identified using less sophisticated technology. In conclusion, mothers who experience higher perceived stress or are exposed to more stressors may have children at greater risk for obesity. Although additional basic and intervention research is needed, the potential remains that child obesity prevention programs may be improved by minimizing the negative effects of maternal stress on child obesity risk.
Supplementary Material
Figure 2.
Overall Effect Size Estimates for Cross-sectional and Longitudinal Studies
Acknowledgements
This work was supported by the National Institutes of Health Cancer Control and Epidemiology Research Training Grant 5 T32 CA 009492 (Pentz, PI); American Cancer Society 118283-MRSGT-10-012-01-CPPB (Dunton, PI); National Heart, Lung, and Blood Institute 1R01HL119255 (Dunton, PI) and National Heart, Lung, and Blood Institute 1R21HL108018 (Dunton, Intille, PIs).
Conflict of interest statement
Authors have received funding from the American Cancer Institute and National Institutes of Health during the conduct of the study.
Footnotes
The authors declare no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of High Body Mass Index in US Children and Adolescents, 2007–2008. Jama-Journal of the American Medical Association. 2010 Jan;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Flynn MAT, McNeil DA, Maloff B, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with 'best practice' recommendations. Obesity Reviews. 2006 Feb;7:7–66. doi: 10.1111/j.1467-789X.2006.00242.x. [DOI] [PubMed] [Google Scholar]
- 3.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews. 2011;(12) doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Han JC, Lawlor DA, Kimm SYS. Childhood obesity. Lancet. 2010 May;375(9727):1737–1748. doi: 10.1016/S0140-6736(10)60171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell GL, Farrow C, Haycraft E, Meyer C. Parental influences on children's eating behaviour and characteristics of successful parent-focussed interventions. Appetite. 2013 Jan;60:85–94. doi: 10.1016/j.appet.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 6.McConley RL, Mrug S, Gilliland MJ, et al. Mediators of maternal depression and family structure on child BMI: Parenting quality and risk factors for child overweight. Obesity. 2012;19(2):345–352. doi: 10.1038/oby.2010.177. [DOI] [PubMed] [Google Scholar]
- 7.Kozyrskyj AL, Zeng Y, Colman I, et al. Maternal distress in early life predicts the waist-to-hip ratio in schoolchildren. Journal of Developmental Origins of Health and Disease. 2011 Apr;2(2):72–80. doi: 10.1017/S2040174410000723. [DOI] [PubMed] [Google Scholar]
- 8.Park H, Walton-Moss B. Parenting Style, Parenting Stress, and Children's Health-Related Behaviors. Journal of Developmental and Behavioral Pediatrics. 2012 Jul-Aug;33(6):495–503. doi: 10.1097/DBP.0b013e318258bdb8. [DOI] [PubMed] [Google Scholar]
- 9.Lampard AM, Jurkowski JM, Lawson HA, Davison KK. Family Ecological Predictors of Physical Activity Parenting in Low-Income Families. Behavioral Medicine. 2013 Oct;39(4):97–103. doi: 10.1080/08964289.2013.802215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lundahl A, Nelson TD, Van Dyk TR, West T. Psychosocial Stressors and Health Behaviors: Examining Sleep, Sedentary Behaviors, and Physical Activity in a Low-Income Pediatric Sample. Clinical Pediatrics. 2013 Aug;52(8):721–729. doi: 10.1177/0009922813482179. [DOI] [PubMed] [Google Scholar]
- 11.Gundersen C, Lohman BJ, Garasky S, Stewart S, Eisenmann J. Food security, maternal stressors, and overweight among low-income US children: Results from the National Health and Nutrition Examination Survey (1999–2002) Pediatrics. 2008 Sep;122(3):E529–E540. doi: 10.1542/peds.2008-0556. [DOI] [PubMed] [Google Scholar]
- 12.Li JO, Olsen J, Vestergaard M, Obel C, Baker JL, Sorensen TIA. Prenatal Stress Exposure Related to Maternal Bereavement and Risk of Childhood Overweight. Plos One. 2010 Jul;5(7) doi: 10.1371/journal.pone.0011896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lohman BJ, Stewart S, Gundersen C, Garasky S, Eisenmann JC. Adolescent Overweight and Obesity: Links to Food Insecurity and Individual, Maternal, and Family Stressors. Journal of Adolescent Health. 2009 Sep;45(3):230–237. doi: 10.1016/j.jadohealth.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 14.McPhie S, Skouteris H, McCabe M, et al. Maternal correlates of preschool child eating behaviours and body mass index: A cross-sectional study. International Journal of Pediatric Obesity. 2011;6(5–6):476–480. doi: 10.3109/17477166.2011.598937. [DOI] [PubMed] [Google Scholar]
- 15.Parks EP, Kumanyika S, Moore RH, Stettler N, Wrotniak BH, Kazak A. Influence of Stress in Parents on Child Obesity and Related Behaviors. Pediatrics. 2012 Nov;130(5):E1096–E1104. doi: 10.1542/peds.2012-0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stenhammar C, Olsson GM, Bahmanyar S, et al. Family stress and BMI in young children. Acta Paediatrica. 2010 Aug;99(8):1205–1212. doi: 10.1111/j.1651-2227.2010.01776.x. [DOI] [PubMed] [Google Scholar]
- 17.Suglia SF, Duarte CS, Chambers EC, Boynton-Jarrett R. Cumulative social risk and obesity in early childhood. Pediatrics. 2012;129(5):e1173–e1179. doi: 10.1542/peds.2011-2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stenhammar C, Olsson G, Bahmanyar S, et al. Family stress and BMI in young children. Acta paediatrica. 2010 Aug;99(8):1205–1212. doi: 10.1111/j.1651-2227.2010.01776.x. [DOI] [PubMed] [Google Scholar]
- 19.Ajslev TA, Andersen CS, Ingstrup KG, Nohr EA, Sorensen TIA. Maternal Postpartum Distress and Childhood Overweight. Plos One. 2010 Jun;5(6) doi: 10.1371/journal.pone.0011136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McPhie S, Skouteris H, Fuller-Tyszkiewicz M, et al. Maternal predictors of preschool child-eating behaviours, food intake and body mass index: A prospective study. Early Child Development and Care. 2012;182(8):999–1014. [Google Scholar]
- 21.Moens E, Braet C, Bosnians G, Rosseel Y. Unfavourable family characteristics and their associations with childhood obesity: A cross-sectional study. European Eating Disorders Review. 2009;17(4):315–323. doi: 10.1002/erv.940. [DOI] [PubMed] [Google Scholar]
- 22.Abidin RR. Parenting Stress Index, Third Edition: Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- 23.Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the Parenting Stress Index-Short Form. Journal of Clinical Child and Adolescent Psychology. 2006 Jun;35(2):302–312. doi: 10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- 24.Anthony LG, Anthony BJ, Glanville DN, Naiman DQ, Waanders C, Shaffer S. The relationships between parenting stress, parenting behaviour and preschoolers' social competence and behaviour problems in the classroom. Infant and Child Development. 2005 Jun;14(2):133–154. [Google Scholar]
- 25.Pervanidou P, Chrousos GP. Stress and obesity/metabolic syndrome in childhood and adolescence. International Journal of Pediatric Obesity. 2011 Sep;6:21–28. doi: 10.3109/17477166.2011.615996. [DOI] [PubMed] [Google Scholar]
- 26.Rosmond R. Role of stress in the pathogenesis of the metabolic syndrome. Psychoneuroendocrinology. 2005;30(1):1–10. doi: 10.1016/j.psyneuen.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Charmandari E, Kino T, Souvatzoglou E, Chrousos GP. Pediatric stress: hormonal mediators and human development. Hormone Research in Paediatrics. 2003;59(4):161–179. doi: 10.1159/000069325. [DOI] [PubMed] [Google Scholar]
- 28.Alvarez J, Pavao J, Baumrind N, Kimerling R. The relationship between child abuse and adult obesity among California women. American Journal of Preventive Medicine. 2007 Jul;33(1):28–33. doi: 10.1016/j.amepre.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 29.Whitaker RC, Phillips SA, Orzol SA, Burdette HL. The association between maltreatment and obesity among preschool children. Child Abuse & Neglect. 2007 Nov-Dec;31(11–12):1187–1199. doi: 10.1016/j.chiabu.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Birch L, Savage JS, Ventura A. Influences on the development of children's eating behaviours: from infancy to adolescence. Canadian journal of dietetic practice and research: a publication of Dietitians of Canada= Revue canadienne de la pratique et de la recherche en dietetique: une publication des Dietetistes du Canada. 2007;68(1):s1. [PMC free article] [PubMed] [Google Scholar]
- 31.Cullen KW, Baranowski T, Rittenberry L, Olvera N. Social-environmental influences on children's diets: results from focus groups with African-, Euro- and Mexican-American children and their parents. Health Education Research. 2000 Oct;15(5):581–590. doi: 10.1093/her/15.5.581. [DOI] [PubMed] [Google Scholar]
- 32.Hanson CL, Klesges RC, Eck LH, Cigrang JA, Carle DL. Family relations, coping styles, stress, and cardiovascular disease risk factors among children and their parents. Family Systems Medicine. 1990;8(4):387. [Google Scholar]
- 33.Boynton-Jarrett R, Fargnoli J, Suglia SF, Zuckerman B, Wright RJ. Association between maternal intimate partner violence and incident obesity in preschool-aged children: results from the Fragile Families and Child Well-being Study. Archives of pediatrics & adolescent medicine. 2010;164(6):540. doi: 10.1001/archpediatrics.2010.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Koch FS, Sepa A, Ludvigsson J. Psychological Stress and Obesity. Journal of Pediatrics. 2008;153(6):839–844. doi: 10.1016/j.jpeds.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 35.Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics in medicine. 2000;19(22):3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::aid-sim784>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 36.Schünemann HJ, Oxman AD, Vist GE, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Wiley-Blackwell; 2008. Interpreting results and drawing conclusions; pp. 359–387. [Google Scholar]
- 37.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Wiley; 2011. [Google Scholar]
- 38.Burdette HL, Whitaker RC, Harvey-Berino J. Television viewing and outdoor time in low-income preschool children: Relationship to depression, perceived stress, and BMI in their mothers. Obesity Research. 2001 Sep;9:59S–59S. [Google Scholar]
- 39.Sowan N, Stember ML. Parental risk factors for infant obesity. MCN: The American Journal of Maternal/Child Nursing. 2000;25(5):234–240. doi: 10.1097/00005721-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Bergmeier H, Skouteris H, Horwood S, Hooley M, Richardson B. Child temperament and maternal predictors of preschool children’s eating and body mass index. A prospective study. Appetite. 2014;74:125–132. doi: 10.1016/j.appet.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 41.Ievers-Landis CE, Storfer-Isser A, Rosen C, Johnson NL, Redline S. Relationship of sleep parameters, child psychological functioning, and parenting stress to obesity status among preadolescent children. Journal of Developmental and Behavioral Pediatrics. 2008 Aug;29(4):243–252. doi: 10.1097/DBP.0b013e31816d923d. [DOI] [PubMed] [Google Scholar]
- 42.Walton K, Simpson JR, Darlington GJH. Parenting Stress: A Cross-Sectional Analysis of Associations with Childhood Obesity and Related Behaviours. 2014 doi: 10.1186/1471-2431-14-244. unpublished. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gemmill AW, Worotniuk T, Holt CJ, Skouteris HJM. Maternal psychological factors and controlled child feeding practices in relation to child body mass index. Child Obesity. 2013;9(4) doi: 10.1089/chi.2012.0135. Epub ahead of print 2013 Jun 2019. [DOI] [PubMed] [Google Scholar]
- 44.Gibson LY, Byrne SM, Davis EA, Blair E, Jacoby P, Zubrick SR. The role of family and maternal factors in childhood obesity. Medical Journal of Australia. 2007 Jun;186(11):591–595. doi: 10.5694/j.1326-5377.2007.tb01061.x. [DOI] [PubMed] [Google Scholar]
- 45.Rondo PHC, Ferreira RF, Nogueira F, Ribeiro MCN, Lobert H, Artes R. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. European Journal of Clinical Nutrition. 2003 Feb;57(2):266–272. doi: 10.1038/sj.ejcn.1601526. [DOI] [PubMed] [Google Scholar]
- 46.Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, Davies W. Controlled study of critical parent and family factors in the obesigenic environment. Obesity. 2007;15(1):126–126. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- 47.de Moraes VY, Godin K, dos Santos JBG, Faloppa F, Bhandari M, Belloti JC. Influence of compensation status on time off work after carpal tunnel release and rotator cuff surgery: a meta-analysis. Patient safety in surgery. 2013;7(1):1. doi: 10.1186/1754-9493-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000 Jun;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 50.Hunter JE, Schmidt FL. Methods of meta-analysis: Correcting error and bias in research findings. Sage; 2004. [Google Scholar]
- 51.McCurdy K, Gorman KS, Metallinos-Katsaras E. From Poverty to Food Insecurity and Child Overweight: A Family Stress Approach. Child Development Perspectives. 2010 Aug;4(2):144–151. [Google Scholar]
- 52.Anderson SE, Gooze RA, Lemeshow S, Whitaker RC. Quality of early maternal-child relationship and risk of adolescent obesity. Pediatrics. 2012;129(1):132–140. doi: 10.1542/peds.2011-0972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Anderson SE, Whitaker RC. Attachment Security and Obesity in US Preschool-Aged Children. Archives of Pediatrics & Adolescent Medicine. 2011 Mar;165(3):235–242. doi: 10.1001/archpediatrics.2010.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lampard AM, Franckle RL, Davison KK. Maternal depression and childhood obesity: A systematic review. Preventive Medicine. 2014 Feb;59:60–67. doi: 10.1016/j.ypmed.2013.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wilson SM, Sato AF. Stress and Paediatric Obesity: What We Know and Where To Go. Chemphyschem. 2014 Apr;15(5):91–102. doi: 10.1002/smi.2501. [DOI] [PubMed] [Google Scholar]
- 56.De Vriendt T, Moreno LA, De Henauw S. Chronic stress and obesity in adolescents: Scientific evidence and methodological issues for epidemiological research. Nutrition Metabolism and Cardiovascular Diseases. 2009 Sep;19(7):511–519. doi: 10.1016/j.numecd.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 57.Jaaskelainen A, Nevanpera N, Remes J, Rahkonen F, Jarvelin MR, Laitinen J. Stress-related eating, obesity and associated behavioural traits in adolescents: a prospective population-based cohort study. Bmc Public Health. 2014 Apr;:14. doi: 10.1186/1471-2458-14-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lai BS, La Greca AM, Llabre MM. Children's Sedentary Activity After Hurricane Exposure. Psychological Trauma-Theory Research Practice and Policy. 2014 May;6(3):280–289. [Google Scholar]
- 59.Entringer S, Buss C, Wadhwa PD. Prenatal stress and developmental programming of human health and disease risk: concepts and integration of empirical findings. Current Opinion in Endocrinology Diabetes and Obesity. 2010 Dec;17(6):507–516. doi: 10.1097/MED.0b013e3283405921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schuurmans C, Kurrasch DM. Neurodevelopmental consequences of maternal distress: what do we really know? Clinical Genetics. 2013 Feb;83(2):108–117. doi: 10.1111/cge.12049. [DOI] [PubMed] [Google Scholar]
- 61.Cashdan E. A sensitive period for learning about food. Human Nature. 1994;5(3):279–291. doi: 10.1007/BF02692155. [DOI] [PubMed] [Google Scholar]
- 62.Schwartz C, Scholtens P, Lalanne A, Weenen H, Nicklaus S. Development of healthy eating habits early in life. Review of recent evidence and selected guidelines. Appetite. 2011 Dec;57(3):796–807. doi: 10.1016/j.appet.2011.05.316. [DOI] [PubMed] [Google Scholar]
- 63.Dietz WH, Gortmaker SL. Preventing obesity in children and adolescents. Annual Review of Public Health. 2001;22:337–353. doi: 10.1146/annurev.publhealth.22.1.337. [DOI] [PubMed] [Google Scholar]
- 64.Hurley KM, Black MM, Papas MA, Canfield LE. Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. Journal of Nutrition. 2008 Apr;138(4):799–805. doi: 10.1093/jn/138.4.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Duarte CS, Shen S, Wu P, Must A. Maternal depression and child BMI: longitudinal findings from a US sample. Pediatric Obesity. 2012 Apr;7(2):124–133. doi: 10.1111/j.2047-6310.2011.00012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rodriguez CM. Association Between Independent Reports of Maternal Parenting Stress and Children's Internalizing Symptomatology. Journal of Child and Family Studies. 2011 Oct;20(5):631–639. [Google Scholar]
- 67.Halfon N, Larson K, Slusser W. Associations Between Obesity and Comorbid Mental Health, Developmental, and Physical Health Conditions in a Nationally Representative Sample of US Children Aged 10 to 17. Academic Pediatrics. 2013 Jan-Feb;13(1):6–13. doi: 10.1016/j.acap.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 68.Rofey DL, Kolko RP, Iosif AM, et al. A Longitudinal Study of Childhood Depression and Anxiety in Relation to Weight Gain. Child Psychiatry & Human Development. 2009 Dec;40(4):517–526. doi: 10.1007/s10578-009-0141-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anderson SE, Cohen P, Naumova EN, Must A. Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Archives of Pediatrics & Adolescent Medicine. 2006 Mar;160(3):285–291. doi: 10.1001/archpedi.160.3.285. [DOI] [PubMed] [Google Scholar]
- 70.Epstein LH, Wisniewski L, Weng R. Child and parent psychological problems influence child weight control. Obesity research. 1994;2(6):509–515. doi: 10.1002/j.1550-8528.1994.tb00099.x. [DOI] [PubMed] [Google Scholar]
- 71.Wang L, Anderson JL, Dalton WT, et al. Maternal Depressive Symptoms and the Risk of Overweight in Their Children. Maternal and Child Health Journal. 2013 Jul;17(5):940–948. doi: 10.1007/s10995-012-1080-1. [DOI] [PubMed] [Google Scholar]
- 72.Ramasubramanian L, Lane S, Rahman A. The association between maternal serious psychological distress and child obesity at 3 years: a cross-sectional analysis of the UK Millennium Cohort Data. Child Care Health and Development. 2013 Jan;39(1):134–140. doi: 10.1111/j.1365-2214.2011.01325.x. [DOI] [PubMed] [Google Scholar]
- 73.Jun HJ, Corliss HL, Boynton-Jarrett R, Spiegelman D, Austin SB, Wright RJ. Growing up in a domestic violence environment: relationship with developmental trajectories of body mass index during adolescence into young adulthood. Journal of Epidemiology and Community Health. 2012 Jul;66(7):629–635. doi: 10.1136/jech.2010.110932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Topham GL, Page MC, Hubbs-Tait L, et al. Maternal depression and socio-economic status moderate the parenting style/child obesity association. Public Health Nutrition. 2010 Aug;13(8):1237–1244. doi: 10.1017/S1368980009992163. [DOI] [PubMed] [Google Scholar]
- 75.Phipps SA, Burton PS, Osberg LS, Lethbridge LN. Poverty and the extent of child obesity in Canada, Norway and the United States. Obesity Reviews. 2006 Feb;7(1):5–12. doi: 10.1111/j.1467-789X.2006.00217.x. [DOI] [PubMed] [Google Scholar]
- 76.O'Dougherty M, Story M, Stang J. Observations of parent-child co-shoppers in supermarkets: Children's involvement in food selections, parental yielding, and refusal strategies. Journal of Nutrition Education and Behavior. 2006 May-Jun;38(3):183–188. doi: 10.1016/j.jneb.2005.11.034. [DOI] [PubMed] [Google Scholar]
- 77.Dunton GF, Liao Y, Intille SS, Spruijt-Metz D, Pentz M. Investigating Children's Physical Activity and Sedentary Behavior Using Ecological Momentary Assessment With Mobile Phones. Obesity. 2011 Jun;19(6):1205–1212. doi: 10.1038/oby.2010.302. [DOI] [PubMed] [Google Scholar]
- 78.Campbell J, Ehlert U. Acute psychosocial stress: Does the emotional stress response correspond with physiological responses? Psychoneuroendocrinology. 2012 Aug;37(8):1111–1134. doi: 10.1016/j.psyneuen.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 79.Savva SC, Tornaritis M, Savva ME, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity. 2000;24(11):1453–1458. doi: 10.1038/sj.ijo.0801401. [DOI] [PubMed] [Google Scholar]
- 80.Breithaupt P, Colley RC, Adamo KB. Body composition measured by dual?energy X?ray absorptiometry half?body scans in obese children. Acta Paediatrica. 2011;100(12):e260–e266. doi: 10.1111/j.1651-2227.2011.02378.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.