Abstract
Suboptimal regimen adherence among youth with type 1 diabetes (T1D) is a common challenge for patients, families, and providers. Motivational interviewing (MI) is a brief communication style designed to elicit intrinsic motivation and strengthen commitment to behavior change goals. As pediatric MI research expands, a critical review of its evidence base and applicability to promote adherence behaviors for youth with T1D is needed. This review introduces the core tenets of MI and clinical applications in T1D, synthesizes the existing MI research in T1D, and discusses the next steps in MI research. Overall, mixed results for MI interventions in T1D reflect variations in research study design and clinical implementation. Targeting adherence rather than glycemic outcomes typically demonstrates greater results, highlighting the promise of MI to facilitate meaningful and enduring improvements in youths’ T1D adherence behaviors.
Keywords: Type 1 diabetes, Adherence, Motivational interviewing, Behavioral Intervention, Health care providers, Pediatrics
Introduction
Despite rapid advances in medical regimens and health technology designed to optimize glycemic control, suboptimal diabetes adherence continues to place youth with type 1 diabetes (T1D) at risk for acute and chronic complications. Health care providers play a major role in helping patients and families integrate complex and multidimensional diabetes care behaviors into daily life. Well-intentioned, experienced providers may respond to youths’ adherence difficulties by giving advice on simple steps to improve glycemic control or by emphasizing how repeated high or low blood sugars can lead to serious health consequences. When patients are motivated and ready to make changes, such traditional interventions may lead to successful behavior change.
However, instead of accepting and implementing these thoughtful suggestions, many times, patients respond to such approaches with “yes, but….” The more the provider argues for behavior change (e.g., “If you started checking your blood glucose before you go to bed, you could prevent overnight lows and feel better in the morning”), the stronger the patient argues against change (e.g., “Yes, but I’m too exhausted to remember to check before I fall asleep”), leaving both parties feeling “stuck.” Whether the scenario relates to challenges with blood glucose monitoring, insulin bolusing, carbohydrate counting, or physical activity, most health care providers have felt at one time or another that they have tried all of the tools in their toolbox, yet they still cannot help certain patients change their behavior. On the one hand, the provider may feel frustrated, helpless, and burned-out; and on the other hand, he or she may be interested in learning new approaches to promote diabetes adherence. Motivational interviewing (MI) is one approach designed specifically to help providers facilitate health behavior change [1••].
Over three decades of research have demonstrated that MI is an effective approach to improve a range of health behaviors [2]. With roots in alcohol abuse and addiction treatment [3], MI has been implemented with adults to improve adherence to medical regimens, increase physical activity and improve dietary intake, and has resulted in improvements in medical/ biological outcomes (e.g., reductions in weight/BMI among adults with obesity and in A1c among adults with type 2 diabetes) [2, 4•, 5–7].
More recently, MI has emerged in work with pediatric populations. The first and only meta-analysis of MI to promote health behavior change for multiple pediatric populations to date reported a small yet significant effect size across pediatric chronic conditions (g=0.282) [8••]. Reviews of this growing literature [4•, 9–11] present mixed evidence of the benefits of MI to promote pediatric health behaviors including smoking cessation [12, 13], reductions in substance use [14, 15] and high-risk sexual behavior [16], and improvements in overweight and obesity-related behaviors relating to nutrition and physical activity [17–21] as well as adherence to medical regimens for HIV [22, 23] and asthma [24, 25]. There is also preliminary support for MI to promote youths’ management of T1D [26, 27, 28•, 29].
As integration of MI into clinical and research endeavors continues, there remains a need to evaluate its relevance to the care of youth with T1D. Thus, the goals for the current review are to (1) describe MI and demonstrate clinical applications for treatment of youth with T1D, (2) review the evidence base of MI interventions promoting behavior change among youth with T1D, and (3) discuss “lessons learned” from previous MI research with other pediatric chronic conditions to inform future directions for MI with T1D populations.
Overview of Motivational Interviewing
Motivational interviewing (MI) is defined as a collaborative conversation style that elicits intrinsic motivation and strengthens commitment to behavior change goals [1••]. The following description of MI is illustrated by examples relating to the case of Jack, an adolescent male with T1D presented in Fig 1. Feelings of ambivalence, or having strong reasons for and against change, often precede one’s decision to make behavior changes [1••]. This approach is described as “patient-centered,” in that providers guide patients to explore and resolve ambivalence about behavior change by evaluating the patient’s own perceived pros and cons of change in relation to their current lifestyle. For instance, Jack’s provider may ask, “What are the good things about your current routine of not checking your blood glucose before you go to bed?” After reflecting and validating his responses, his provider may then ask, “What are the downsides of missing your bedtime blood glucose check?” or “What would be the benefits, if any, to start checking your blood glucose before bed?” This approach enables Jack to verbalize his current ambivalence about nighttime blood glucose checks as well as argue for his own reasons for change. For example, Jack may respond to the provider’s prompts in the following ways relating to cons, “It’s really hard to remember because I’m so tired by the time I get ready for bed” and pros, “My mom may stop nagging me if I started checking before bed.” Importantly, a key tenet of MI is that the provider does not assert his or her own reasons for Jack to make a behavior change or emphasize the reasons voiced by Jack’s parents. Rather, the provider’s role is to evoke Jack’s intrinsic reasons for change and eventually, once Jack is ready, his own ideas for goal setting and planning [30••].
Fig. 1.
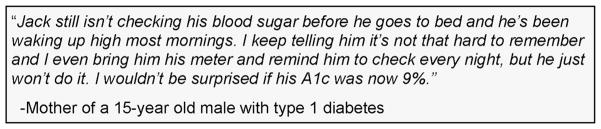
Case example
The collaborative partnership between patient and provider in MI represents a paradigm shift away from authoritative and educational styles traditionally used to improve health behavior in health care settings. Instead, MI asserts that the patient has the ability and responsibility for choosing to change his or her own behavior and the provider supports the patient’s autonomy in this decision [1••]. For instance, Jack’s provider may say, “Ultimately, it’s up to you whether or not you choose to check your blood glucose before you go to bed.” Providers use universal communication skills such as open-ended questions and reflective listening to empathize with the patient’s current experiences and affirm the patient’s strengths, resources, or achievements. For instance, “Jack, you’ve told me how busy you are and it’s tough to remember one more thing like checking your blood glucose before you go to sleep” or “Your health is important to you and you already do so many things to take care of your diabetes during the day.”
The four core processes of MI are engaging, focusing, evoking, and planning [1••]. First, “engaging,” or developing the therapeutic alliance, is used to communicate understanding and acceptance of the patient’s experience. Second, “focusing” is a process where the provider collaborates with the patient to set an agenda and concentrate on a target behavior change goal selected by the patient. Jack’s provider may ask, “Jack, there are lots of topics we could talk about today, such as checking your blood glucose more at bedtime, taking your insulin 30 min before school lunch, or making sure you have the diabetes supplies you need before soccer practice. Which would you like to start with?” The provider guides Jack towards specific targets while giving him a choice of where to begin. Third, the provider evokes or elicits patient-identified arguments for change through prompting such as, “Let’s look three months down the road and imagine that you were checking your blood glucose before bed regularly. What might be different?” When the provider pushes for behavior change without exploring the patient’s ambivalence, the patient naturally pushes back by defending their current behavior. In contrast, the MI approach acknowledges the patient’s “sustain talk” or reasons for not changing (e.g., “I’ve already tried everything to help me remember to check my blood sugar before bed, but I just can’t do it”), while eliciting and strengthening “change talk” or statements of reasons and commitment to change (e.g., “I guess it would be nice not to argue with my mom first thing every morning when she realizes I forgot to check before I fell asleep”). During the “planning” process, the provider helps the patient negotiate a plan for change by setting goals, helping the patient consider various options for change, deciding on a plan, and eliciting commitment to follow through with behavior change. Importantly, the MI process of planning may resemble other goal setting and problem-solving techniques widely used in patient counseling. Once Jack is ready, his provider may transition into planning with comments such as, “What is your next step?” or “Tell me about some strategies you have used in the past that have helped you to check your blood glucose before bed.” Of note, the planning process from the MI approach differs from other approaches in that the decision to initiate planning is contingent upon the patient’s readiness to make behavior changes [1••]. In MI, providers constantly evaluate the patient’s readiness to change to guide the movement between these four core processes.
MI Behavior Change Targets for Type 1 Diabetes
Consistent with the principles of MI, this approach is implemented to promote specific, targeted health behavior change [1••], yet significant effects have also been detected for medical/biological outcomes as well among diabetes populations (e.g., decreased A1c, weight loss) [2, 4•, 5, 6]. Given the complexity of T1D regimens, it may not be feasible or effective to address multiple health behaviors in a single interaction. Agenda setting is a common MI strategy especially when working with children and adolescents, to empower the patient to pick which target(s) he or she wants to focus on during a clinic visit [30••]. As described earlier, Jack’s provider may provide or elicit several options of potential behavioral change goals based on clinically relevant topics, while supporting Jack’s autonomy in selecting a starting point. Setting goals from an MI approach differs from traditional approaches as the process begins when the patient demonstrates readiness and focuses on eliciting the patient’s ideas for behavior change. Prior to providing helpful suggestions, the provider may ask, “Jack, what ideas do you have, if any, that may help you reach your goal of checking more consistently before you go to sleep?” Table 1 presents examples of common diabetes-related behavior goals for which MI may be a useful approach to help facilitate patients’ behavior change.
Table 1.
Examples of diabetes behavior targets for MI intervention
| Health domain | Specific behavior goal |
|---|---|
| Diabetes adherence | Increase blood glucose monitoring at specific times (e.g., weekend mornings) or challenging situations (e.g., out with friends) Keep blood glucose logs or download blood glucose information regularly and bring logs to clinic for review Administer insulin 30 min prior to meals Count carbohydrates for accurate insulin dosages |
| Regimen changes | Decide whether to start using an insulin pump or a continuous glucose monitor |
| Nutrition | Make healthier food choices Increase fruits and vegetables Plan ahead for holidays or events (e.g., Halloween, birthday parties, sleepovers) |
| Physical activity | Carry fast acting carbs when exercising Tell a coach or team members about diabetes Increase daily physical activity |
| Diabetes responsibility | Transfer and uptake of developmentally appropriate responsibility for specific diabetes task from parent to youth (e.g., pump site changes, ordering diabetes supplies, scheduling clinic appointments) |
Developmental Considerations of MI for Youth with T1D
To date, the majority of MI interventions for youth with T1D have targeted adolescents, due perhaps to well-established declines in adherence and glycemic control [31–33]. MI is especially appropriate during adolescence, a period characterized by establishing independence and autonomy and by pushing away or resisting authority figures [11, 30••]. Feelings of ambivalence often accompany this transition from childhood into adolescence [34]; thus, MI may be an effective approach to improve self-efficacy and address youths’ ambivalence towards self-care behaviors in the process of improving overall diabetes adherence. Because change is often preceded by ambivalence [1••], integrating MI early in such transitions may be most effective.
In addition to adolescence, MI may be an appropriate approach to promote adherence behaviors during the transition into young adulthood. Young adults take on increasing responsibility and independence and are faced with decisions regarding their lifestyle and related health behaviors, often with less daily involvement of family members [35]. This is also a period of documented risk for suboptimal adherence and glycemic control, and extended gaps between clinic visits are common [36, 37]. MI may be a helpful approach to resolve ambivalence about taking on greater diabetes responsibility amidst changes in many life domains, including the transition to the adult health care setting. Further, MI may facilitate patient-centered discussions to help identify how patients prioritize diabetes care in the context of multiple competing demands and interests.
Evidence Base of MI Interventions for Pediatric T1D
Although there are few randomized controlled trials (RCTs) of MI which target diabetes adherence in youth with T1D, research suggests the potential of this approach to facilitate positive behavior change [26, 27, 28•, 29]. The recent meta-analysis reported MI interventions with pediatric T1D populations yielded greater effect sizes (g=0.914, large) compared to MI interventions across pediatric populations (g=0.282, small) [8••]. MI interventions to promote behavior change across pediatric populations were most effective when completed with youth and parents together (g=0.586, moderate), reflecting the value of intervening on the family rather than individual level (g=0.257, small) [8••], although supporting youth autonomy while eliciting family engagement appropriately may be challenging [38]. The number of sessions was not related to behavior and medical/biological outcomes, suggesting brief MI interventions (one to four sessions) with youth and families yield adequate effects on behavior change. The following sections describe results and lessons learned from previous MI studies in T1D, including those with mixed or null results.
Stand-Alone MI Interventions for T1D Adherence
One early pilot study and corresponding RCT compared an MI intervention (four to six sessions over 12 months) with non-directive educational support [26, 27]. Participant-driven MI sessions were comprised of a menu of strategies, exploration of ambivalence, discussion of costs and benefits of behavior change, and collaborative goal setting. The mean A1c for MI participants was significantly lower than control participants upon completion and 12 months post-treatment when controlling for baseline A1c. Specifically, MI participants’ mean A1c declined 0.6 % from baseline to intervention completion and maintained this decline 12 months post-treatment, whereas control participants’ mean A1c increased 0.2 % at intervention completion and decreased 0.1 % 12 months later. MI participants reported increased levels of life satisfaction and positive well-being and decreased anxiety levels and disease burden. Additionally, the MI group reported stronger beliefs that their own participation in diabetes management would lead to prevention of complications. Consistent with what MI practitioners refer to as the “spirit of MI” [1••], Channon and colleagues [27] supported youths’ autonomy and self-efficacy both within session and in the study design by empowering youth to select the frequency and location of MI sessions. Although they reported improvements in constructs traditionally related to agents of change in MI such as self-efficacy, these were not related to improvements in A1c. Thus, it remains unclear whether or how the core components of MI (e.g., supporting autonomy and self-efficacy) impact glycemic control. A plausible mechanism of this link would be improvements in adherence behaviors, yet these intermediary diabetes care behaviors were not reported in initial MI studies for youth with T1D.
MI within Multicomponent Treatments for T1D Adherence
Literature suggests MI is effective when integrated into existing treatment programs or combined with other evidence-based approaches [7, 39]. Yet, there remains a need for implementation guidelines to inform the process of integration with other approaches. The recent meta-analysis of MI interventions with pediatric populations determined no significant difference between stand-alone (g=0.324, small) compared with integrated MI interventions (g=0.224, small), although the effect size for stand-alone MI intervention was larger [8••]. While this may suggest that MI for pediatric health behavior change is more effective when delivered independent of other treatments, this finding may also emphasize the lack of guidelines and need for further examination of how to successfully integrate treatment with pediatric populations. One perspective from Naar-King and Suarez [30••] is, “MI provides the platform for a good therapy process regardless of the specific intervention framework you may be using” (pp 77).
An early study by Viner and colleagues [29] piloted a non-randomized multicomponent motivational intervention targeting youth with A1c >8.5 %. Self-selected participants completed 6 weekly group sessions which incorporated components of externalization of diabetes, addressing ambivalence and commitment to change, solution-focused goal setting, and cognitive-behavioral problem-solving strategies. Intervention participants demonstrated significant declines in A1c of 1.5 % 4 to 6 months post-treatment relative to no significant changes in control participants’ mean A1c. Overall improvements in glycemic control were partly maintained, yet group differences were no longer significant 1 year post-treatment. Unique to this pilot study, participants’ readiness to change was evaluated prior to treatment, although no relation was detected with changes in A1c. Future intervention programs with larger samples may implement a similar evaluation to determine how an individual’s readiness to change may moderate timing and utility of MI interventions for behavior change outcomes.
Stanger and colleagues [28•] integrated MI with cognitive-behavioral therapy (CBT) and family-based contingency management strategies for youth with A1c ≥8.0 %. Fourteen weekly family sessions were comprised of a menu of MI intervention components, CBT functional analysis of adherence behaviors, and coping skills to improve decision making. Parent-directed contingency management components included immediate positive or negative consequences for blood glucose monitoring behaviors. Although not randomized, results revealed significant decreases in A1c from 11.6 to 9.1 % upon completion of treatment. Importantly, they detected significant improvements in diabetes care behaviors via parent and youth report and electronic download of blood glucose meters. The use of MI with patients with a history of adherence challenges and related elevated glycemic control demonstrates the potential benefits of implementing MI to address specific behavior targets.
MI Interventions Delivered by Health Care Providers
Earlier MI research across health populations often involved mental health practitioners providing MI interventions [26, 27, 28•]. However, MI clinical and research trends have shifted towards training health care providers in MI to empower their patients to make health behavior changes. One RCT delivered by diabetes educators compared MI with structured diabetes education (SDE) for youth with non-optimal glycemic control (A1c ≥9 %) [40]. Diabetes educators demonstrated adequate MI fidelity after brief MI training. In contrast to hypotheses, A1c was significantly lower among participants in the SDE group 6 months post-treatment compared with those in the MI group. No differences in self-reported diabetes care behaviors, depressive symptoms, or quality of life were detected for either group post-treatment. Wang and colleagues [40] concluded that brief MI without educational content does not necessarily lead to improved glycemic control. Such results reinforce recommendations that MI may be most useful as a way to enhance other behavioral interventions, rather than to serve as a stand-alone intervention. As noted by the authors, level of motivation and diabetes knowledge were not evaluated pre-post treatment, and thus, it remains unclear how additional educational content delivered to the SDE group related to changes in A1c.
An important component of MI interventions is the training of providers to effectively and appropriately use MI in their clinical care. Robling and colleagues [41] examined both provider training and fidelity to MI in relation to patient outcomes. This study evaluated the effectiveness of training pediatric endocrinology health care teams in an MI-informed consulting approach supporting youth self-efficacy for diabetes management. Contrary to hypotheses, training health care teams had no effect on A1c outcomes 1 year post-training. This study presents evidence of feasibility for large-scale MI training of a range of providers including physicians, nurses, and dieticians. Null results for patient outcomes indicate the need to further refine the MI training process in order to provide ongoing evaluation and support to health care providers as they use MI in practice. Given the early stages of MI training specifically with endocrinology teams [42], continued work is needed in this area to improve training approaches and eventually patient outcomes. The literature of training health care providers in MI within a clinical context may provide insight into ways to improve provider fidelity and patient outcomes for future MI research studies [43–45].
Future Directions of MI Interventions to Promote T1D Adherence
Although MI interventions to promote pediatric health behaviors are in the early stages, approaches and treatment targets from other pediatric populations may inform future directions of MI for youth with T1D. Specifically, we present innovative applications of MI drawn from intervention literature of youth with obesity and HIV, and discuss the relevance to future MI interventions in T1D.
Pre-treatment MI for Engagement and Retention
Emerging research of MI interventions with pediatric obesity populations has demonstrated benefits in improving several health behaviors relating to nutrition and physical activity [17–21, 46]. Yet, across treatment approaches, few obesity interventions of any type detect significant long-term reductions in BMI relative to control groups [47], due in part to high attrition rates for comprehensive obesity treatment programs [48]. To address engagement and attrition problems in treatment for obesity, Bean et al. [49•] investigated the efficacy of a two-session MI intervention within a multidisciplinary adolescent treatment program at weeks 1 and 10, time points associated with high rates of attrition. Compared to controls, MI participants remained in treatment 8 weeks longer and had greater overall adherence to treatment visits (e.g., dietician and behavioral support visits) 3 and 6 months after enrollment.
Bean et al. [50] describe further innovative applications of MI to enhance participation in existing obesity treatment programs for parents of children with obesity. They implemented two MI sessions (one via telephone and one in person) upon completion of a telephone eligibility screening and after program orientation to determine if preparation and addressing pre-treatment ambivalence about behavior change may enhance treatment engagement and outcomes. Results from this RCT will be published upon study completion. Collectively, the use of MI pre-treatment or at enrollment may enhance participation in existing comprehensive treatment programs for youth with T1D with both clinical and research contexts [7, 51].
MI and mHealth
Youth living with HIV is another pediatric population in which MI interventions are emerging. Suboptimal adherence to antiretroviral treatment (ART) places youth with HIV at risk for significant long-term consequences of viral suppression and fewer effective treatment options; thus, innovative MI applications target initiation of ART. Naar-King and colleagues have evaluated both in-person and computer-based MI interventions for youth with HIV [22, 23]. First, a four-session in-person MI intervention demonstrated improvements in viral load 6 months post-treatment relative to a control group [22]. Recently, Naar-King and colleagues piloted a two-session computerized MI intervention to promote adherence with youth recently initiating ART, which also yielded promising effects for decreased viral load and improvements in self-reported medication adherence [23]. The use of MI at initiation of new medical regimens and the use of computer-based intervention approaches are two components that may inform further MI interventions with T1D populations.
Advances in medical technologies such as continuous glucose monitors or insulin-bolusing software for insulin pumps are promising, yet underutilized tools among youth with T1D [52, 53]. Thus, using MI while introducing or discussing possibilities of such devices with patients may promote greater implementation and long-term use compared with traditional, information-based approaches. Further, MI interventions may enhance patients’ use of existing text message programs and smartphone applications designed to improve daily adherence behaviors by supporting youths’ self-efficacy and autonomy in individualizing mHealth programs to their daily life.
Conclusions
The body of evidence continues to grow for using MI to promote adherence behaviors in youth with T1D across multiple developmental transitions. Given that MI is guided by youths’ personal characteristics, motivations, and perspectives, MI is particularly well suited for use during periods of shifts in diabetes management behaviors, such as adolescence and young adulthood or during changes in the diabetes management regimen. Previous literature has yielded mixed results for MI’s efficacy, so the future of MI research in T1D will need to focus on targeting health behaviors rather than medical/biological outcomes and on standardizing methods of MI training and fidelity. Moreover, in the value-driven economic climate of today’s health care system, cost-effectiveness studies to demonstrate the clinical and ultimately fiscal benefits of brief MI interventions will be necessary. As the clinical delivery of MI interventions becomes increasingly focused on health care providers, it may be beneficial to incorporate MI training into standard medical, nursing, or certified diabetes education curricula. Whether in a research or clinical context, ultimately, it is up to individual providers to choose whether or not to integrate MI into their daily care of patients.
Acknowledgments
For those who are interested or may be considering learning more about MI, self-study resources [1••, 30••, 43, 44, 54] and introductory training workshops (www.motivationalinterviewing.org) are widely available. The authors have received grant support from a K12 Career Development Award from NIH/NIDDK 1K12 DK097696.
Footnotes
Conflict of Interest Priscilla W. Powell, Marisa E. Hilliard, and Barbara J. Anderson declare that they have no conflict of interest.
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
This article is part of the Topical Collection on Psychosocial Aspects
Contributor Information
Priscilla W. Powell, Email: priscilp@bcm.edu, Baylor College of Medicine, Texas Children’s Hospital, 1102 Bates St. Suite 940.37, Houston, TX 77030, USA
Marisa E. Hilliard, Email: mehillia@bcm.edu, Baylor College of Medicine, Texas Children’s Hospital, 1102 Bates St. Suite 940.35A, Houston, TX 77030, USA
Barbara J. Anderson, Email: bjanders@texaschildrens.org, Baylor College of Medicine, Texas Children’s Hospital, 1102 Bates St. Suite 940.36, Houston, TX 77030, USA
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1••.Miller WR, Rollnick S. Motivational interviewing: helping people change. 3. New York: Guilford Press; 2013. Miller and Rollnick are the founders of Motivational Interviewing. Recently updated, this seminal work presents the Spirit of MI, the core processes of MI and several vignettes to demonstrate clinical implementation of the MI approach. [Google Scholar]
- 2.Lundahl B, Moleni T, Burke BL, et al. Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns. 2013;93:157–68. doi: 10.1016/j.pec.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Miller W. Motivational interviewing with problem drinkers. Beh Psychother. 1983;11:147–72. [Google Scholar]
- 4•.Christie D, Channon S. The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: a clinical review. Diabetes Obes Metab. 2013 doi: 10.1111/dom.12195. This recent paper reviews MI intervention research for individuals across the lifespan with type 1 and type 2 diabetes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke B. A meta-analysis of motivational interviewing: twenty-five years of research of empirical studies. Res Soc Work Pract. 2010;20:137–60. [Google Scholar]
- 6.Martins RK, McNeil Review of motivational interviewing in promoting health behaviors. Clin Psychol Rev. 2009;29:283–93. doi: 10.1016/j.cpr.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 8••.Gayes LA, Steele RG. A meta-analysis of motivational interviewing interventions for pediatric health behavior change. J Consult Clin Psych. 2014 doi: 10.1037/a0035917. This paper is the first and only meta-analysis of MI interventions to promote health behaviors for multiple pediatric populations to date. [DOI] [PubMed] [Google Scholar]
- 9.Erickson SJ, Gerstle M, Feldstein SW. Brief interventions and motivational interviewing with children, adolescents, and their parents in pediatric health care settings. Arch Pediatr Adolesc Med. 2005;159:1173–80. doi: 10.1001/archpedi.159.12.1173. [DOI] [PubMed] [Google Scholar]
- 10.Suarez M, Mullins S. Motivational interviewing and pediatric health behavior interventions. J Dev Behav Pediatr. 2008;29:417–28. doi: 10.1097/DBP.0b013e31818888b4. [DOI] [PubMed] [Google Scholar]
- 11.Sindelar HA, Abrantes AM, Hart C, Lewander W, Spirito A. Motivational interviewing in pediatric practice. Curr Probl Pediatr Adolesc Health Care. 2004 Oct;:322–339. doi: 10.1016/j.cppeds.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Horn K, Dino G, Hamilton C, Noerachmanto N. Efficacy of an emergency department-based motivational teenage smoking intervention. Prev Chronic Dis. 2007;4:A08. [PMC free article] [PubMed] [Google Scholar]
- 13.Colby SM, Monti PM, Barnett NP, et al. Brief motivational interviewing in a hospital setting for adolescent smoking: a preliminary study. J Consult Clin Psych. 1998;66:574–8. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- 14.McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results form a multi-site cluster randomized trial. Addiction. 2004;99:39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- 15.Grenard JL, Ames SL, Pentz MA, Sussman S. Motivational interviewing with adolescents and young adults for drug-related problems. Int J Adolesc Med Health. 2006;18:53–67. doi: 10.1515/ijamh.2006.18.1.53. [DOI] [PubMed] [Google Scholar]
- 16.Chen X, Murphy DA, Naar-King S, Parsons JT. Adolescent medicine trials network for HIV/AIDS interventions a clinic-based motivational intervention improves condom use among subgroups of youth living with HIV. J Adolesc Health. 2011;49:193–8. doi: 10.1016/j.jadohealth.2010.11.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: conceptual issues and evidence review. J Am Diet Assoc. 2006;106:2024–33. doi: 10.1016/j.jada.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 18.Berg-Smith SM, Stevens VJ, Brown KM, et al. A brief motivational intervention to improve dietary adherence in adolescents. Health Educ Res. 1999;14:399–410. doi: 10.1093/her/14.3.399. [DOI] [PubMed] [Google Scholar]
- 19.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity. High Five Kids Study. Arch Pediatr Adolesc Med. 2011;165:714–22. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity. Arch Pediatr Adolesc Med. 2007;161:495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 21.Wong EMY, Cheng MMH. Effects of motivational interviewing to promote weight loss in obese children. J Clin Nurs. 2013;22:2519–30. doi: 10.1111/jocn.12098. [DOI] [PubMed] [Google Scholar]
- 22.Naar-King S, Parsons JT, Murphy DA, Chen X, Harris DR, Belzer ME. Improving health outcomes for youth living with the human immunodeficiency virus: a multisite randomized trial of a motivational intervention targeting multiple risk behaviors. Arch Pediatr Adolesc Med. 2009;163:1092–8. doi: 10.1001/archpediatrics.2009.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naar-King S, Outlaw AY, Saar M, et al. Motivational enhancement system for adherence (MESA): pilot randomized trial of a brief computer-delivered prevention intervention for youth initiating antiretroviral treatment. J Pediatr Psychol. 2013;38:638–48. doi: 10.1093/jpepsy/jss132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Halterman JS, Szilagyi PG, Fisher SG, et al. Randomized controlled trial to improve care for urban children with asthma: results of the school-based asthma therapy trial. Arch Pediatr Adolesc Med. 2011;165:262–8. doi: 10.1001/archpediatrics.2011.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seid M, D’Amico EJ, Varni JW, et al. The in vivo adherence intervention for at risk adolescents with asthma: report of a randomized pilot trial. J Pediatr Psychol. 2012;37:390–403. doi: 10.1093/jpepsy/jsr107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Channon S, Smith VJ, Gregory JW. A pilot study of motivational interviewing in adolescents with diabetes. Arch Dis Child. 2003;88:680–3. doi: 10.1136/adc.88.8.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Channon SJ, Huws-Thomas MV, Rollnick S, et al. A multicenter randomized controlled trial of motivational interviewing in teenagers with diabetes. Diabetes Care. 2007;30:1390–5. doi: 10.2337/dc06-2260. [DOI] [PubMed] [Google Scholar]
- 28•.Stanger C, Ryan SR, Delhey LM, et al. A multicomponent motivational intervention to improve adherence among adolescents with poorly controlled type 1 diabetes: a pilot study. J Pediatr Psychol. 2013;38:629–637. doi: 10.1093/jpepsy/jst032. This recent paper describes one approach for integrating MI within a pilot RCT of a multicomponent intervention program for youth with T1D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Viner RM, Taylor VT, Hey S. Motivational/solution-focused intervention improves HbA1c in adolescents with type 1 diabetes. Diabetic Med. 2003;20:739–42. doi: 10.1046/j.1464-5491.2003.00995.x. [DOI] [PubMed] [Google Scholar]
- 30••.Naar-King S, Suarez M. Motivational interviewing with adolescents and young adults. New York: Guilford Press; 2011. Naar-King and Suarez are both established researchers in MI interventions to promote health behaviors in pediatric populations, as well as training health care providers in MI. This book is comprised of an overview of MI within a developmental context and individual chapters targeting specific pediatric populations, meant to serve as a guide for providers interested in integrating MI into practice with adolescent and young adult populations. [Google Scholar]
- 31.Wang JT, Wiebe DJ, White PC. Developmental trajectories of metabolic control among white, black, and hispanic youth with type 1 diabetes. J Pediatr. 2011;159:571–6. doi: 10.1016/j.jpeds.2011.03.053. [DOI] [PubMed] [Google Scholar]
- 32.Helgeson VS, Snyder PR, Seltman H, Escobar O, Becker D, Siminerio L. Brief report: trajectories of glycemic control over early to middle adolescence. J Pediatr Psychol. 2010;35:1161–7. doi: 10.1093/jpepsy/jsq011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood. Diabetes Care. 2001;24:1536–40. doi: 10.2337/diacare.24.9.1536. [DOI] [PubMed] [Google Scholar]
- 34.Baer JS, Peterson PL. Motivational interviewing for adolescents and young adults. In: Miller WR, Rollnick S, editors. Motivational interviewing: preparing people for change. 2. New York: The Guildford Press; 2002. pp. 320–32. [Google Scholar]
- 35.Monaghan M, Hilliard M, Sweenie R, Riekert K. Transition readiness in adolescents and emerging adults with diabetes: the role of patient-provider communication. Curr Diab Rep. 2013;13:900–8. doi: 10.1007/s11892-013-0420-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garvey KC, Wolpert HA, Rhodes ET, et al. Health care transition in patients with type 1 diabetes: young adult experiences and relationship to glycemic control. Diabetes Care. 2012;35:1716–22. doi: 10.2337/dc11-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garvey KC, Markowitz JT, Laffel LMB. Transition to adult care for youth with type 1 diabetes. Curr Diab Rep. 2012;12:533–41. doi: 10.1007/s11892-012-0311-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Channon S, Rubak S. Family-based intervention. In: Naar-King S, Suarez M, editors. Motivational interviewing with adolescents and young adults. New York: Guilford Press; 2011. pp. 165–70. [Google Scholar]
- 39.Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol. 2009;64:527–37. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y, Stewart SM, Mackenzie M, Nakonezny PA, Edwards D, White PC. A randomized controlled trial comparing motivational interviewing in education to structured diabetes education in teens with type 1 diabetes. Diabetes Care. 2010;33:1741–3. doi: 10.2337/dc10-0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Robling M, McNamara R, Bennert K, et al. The effect of the Talking Diabetes consulting skills intervention on glycaemic control and quality of life in children with type 1 diabetes: cluster randomized controlled trial (DEPICTED study) BMJ. 2012 doi: 10.1136/bmj.e2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bean MK, Biskobing D, Francis GL, Wickham E. Motivational interviewing in health care: results of a brief training in endocrinology. J Grad Med Educ. 2012:357–361. doi: 10.4300/JGME-D-11-00166.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berger BA, Villaume WA. Motivational interviewing for health care professionals: a sensible approach. Washington DC: American Pharmacists Association; 2013. [Google Scholar]
- 44.Rollnick S, Miler WR, Butler CC. Motivational interviewing in health care: helping patients change behavior. New York: Guilford Press; 2008. [Google Scholar]
- 45.Sonderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns. 2011;84:16–26. doi: 10.1016/j.pec.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 46.Gourlan M, Sarrazin P, Trouilloud D. Motivational interviewing as a way to promote physical activity in obese adolescents: a randomized-controlled trial using self-determination theory as an explanatory framework. Psychol Health. 2013;28:1265–86. doi: 10.1080/08870446.2013.800518. [DOI] [PubMed] [Google Scholar]
- 47.Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125:e396–418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 48.Skelton JA, Beech BM. Attrition in paediatric weight management: a review of the literature and new directions. Obes Rev. 2011;12:e273–281. doi: 10.1111/j.1467-789X.2010.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49•.Bean MK, Powell P, Quinoy A, Ingersoll K, Wickham EP., III Motivational interviewing targeting diet and physical activity improves adherence to paediatric obesity treatment: results from the MI Values randomized controlled trial. Pediatric Obesity. 2014 doi: 10.1111/j.2047-6310. This recent paper describes innovative applications of MI to improve engagement and retention in comprehensive treatment programs for youth with obesity. Use of MI pretreatment, or at enrollment may enhance participation and outcomes of existing research and clinical programs for youth with T1D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bean MK, Jeffers AJ, Tully CB, Thornton LM, Mazzeo SE. Motivational interviewing with parents of overweight children: study design and methods for the NOURISH+ MI study. Contemp Clin Trials. 2014;37:312–21. doi: 10.1016/j.cct.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.MacDonnell K, Brogan K, Naar-King S, Ellis D, Marshall MD. A pilot study of motivational interviewing targeting weight-related behaviors in overweight or obese African American adolescents. J Adolesc Health. 2012;50:201–3. doi: 10.1016/j.jadohealth.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 52.Harris MA, Hood KK, Mulvaney SA. Pumpers, skypers, surfers and texters: technology to improve the management of diabetes in teenagers. Diabetes Obes Metab. 2012;14:967–72. doi: 10.1111/j.1463-1326.2012.01599.x. [DOI] [PubMed] [Google Scholar]
- 53.Driscoll KA, Johnson JB, Hogan J, Gill E, Wright N, Deeb LC. Insulin bolusing software: the potential to optimize health outcomes in type 1 diabetes. J Diabetes Sci Technol. 2013;7:646–52. doi: 10.1177/193229681300700309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rosengren DB. Building motivational interviewing skills; a practitioner workbook. New York: Guilford Press; 2009. [Google Scholar]


