Abstract
Patellofemoral pain syndrome causes significant discomfort and disability among much of the general population. Despite recent breakthroughs in dynamic three-dimensional imaging technologies to assess pathological patellofemoral motion, such tools remain costly for clinical diagnostics applications. Thus, this study investigated whether three-dimensional patellofemoral kinematics could be predicted from routine two-dimensional static measures of patellofemoral joint alignment quantified from magnetic resonance imaging (MRI) data acquired in full knee extension. Twenty-six volunteers clinically diagnosed with patellofemoral pain (19F/7M, 25.9±11.1 years) and twenty-six control subjects (19F/7M, 25.3±7.7 years) were included in this IRB-approved study. Static three-dimensional sagittal T1-weighted gradient recall echo and dynamic MRI scans were acquired. For the dynamic image acquisition, subjects cyclically flexed and extended their knee (at 30 cycles/minute) while a full cine-phase contrast MRI set (24 times frames of anatomic images and x, y, and z-velocity images) was acquired. From these data, static measures of patellofemoral alignment and three-dimensional patellofemoral kinematics were derived. Single and multiple regressions between static and kinematic variables were evaluated. Although shown reliable, the static MRI measures could only partially predict patellofemoral kinematics, with r2-values ranging from 16%-77%. This makes it imperitave that the current precise, accurate, 3D, dynamic imaging techniques be translated into clinical tools.
INTRODUCTION
Patellofemoral pain syndrome (PFPS), defined as long-term idiopathic anterior knee pain, affects approximately 14-17% of the young active population1. It is theorized to be caused by a force imbalance at the knee2 and/or abnormal bone shape3,4 that results in pathological patellofemoral (PF) kinematics (pathomechanics)5,6. It is believed that such pathomechanics ultimately lead to increased PF joint stress and pain7,8. Although PFPS is typically exacerbated by dynamic activities requiring active quadriceps loading, clinical evaluation of the knee relies primarily on 2D static imaging-based alignment measures and other clinical markers, because in vivo 3D dynamic PF kinematic measures, quantified during activities requiring active muscle control, are not yet clinically available.
Imaging technologies have continuously evolved in order to more accurately and quantitatively evaluate the PF joint (as well as other joints) under loaded dynamic conditions. The first imaging studies evaluating PF alignment9,10 were limited to 2D static imaging of the anterior aspect of the PF joint. The required flexed knee posture of roentgenographic imaging resulted in high false negative rates9,11. In the late 1980s, computed tomography (CT) and magnetic resonance imaging (MRI) became available to study PF alignment in a fully-extended position12-14. These technologies confirmed that the femoral influence on the patella is lessened as the knee enters terminal extension11,,[chk] making malalignment most evident in this range15. Thus, for interventional decisions, particularly invasive ones, CT and MRI are often favored over x-ray11,16,17. Later, cine-MRI was used to quantify 2D PF kinematics during volitional leg extension exercises6. The ability to image the PF joint during an activity requiring muscle control7 allowed PF pathomechanics to be diagnosed that would have otherwise “been overlooked with static examination techniques”6. Advances in imaging technologies have enabled the 3D PF kinematics contractions to be quantified during either dynamic exercise requiring quadriceps activity18,19 or statically with active quadriceps20. These 3D studies added to previous findings by documenting kinematic differences beyond the classic axial-plane measures. For example, the results from the Sheehan et al.18 study supported the long standing association between patella alta and PFPS21-23, as well as introduced other kinematic variables that may be key components in the development of PFPS, such as pathological PF valgus and flexion19. A recent 3D study24 demonstrated that PF flexion (measured during active extension) could discriminate with 100% accuracy the presence of idiopathic long-term anterior knee pain in a cohort of individuals diagnosed with cerebral palsy.
Many of these novel dynamic imaging methodologies have remained research tools, leaving the simpler static 2D imaging-based measures as the primary methods for diagnosing PF joint pathology9,10,25; even though PF pain is typically experienced during dynamic events requiring high quadriceps loading. The validity of predicting 3D PF kinematics from static, 2D, imaging-based measures remains unestablished. Quantifying the relationship between the static and dynamic states of the PF joint may offer improved diagnostics and eventual treatment of suspected patellar maltracking26. Thus, the purpose of this study was to determine if 3D PF kinematics, acquired in vivo during a volitional leg extension exercise, could be predicted from 2D, static, image-based measures of PF alignment. A secondary aim was to evaluate the reliability of these static measures.
METHODS
For this retrospective, IRB-approved study two cohorts were established from an existing database (controls [n=90] and subjects diagnosed with PFPS [n=54]). Each subject signed informed consent at the time of enrollment. To be included within the PFPS cohort the subject had to be diagnosed with idiopathic anterior knee pain (> 6 months duration), have no history of lower limb surgery, and have positive clinical signs of patellar maltracking5. Subjects included within the control cohort had no current or past history of lower leg pain, injury, surgery, or pathology. All included subjects had a previously acquired dynamic cine phase contrast (CPC) MRI dataset and a 3D static sagittal-plane MRI acquisition with the knee in full extension. Static full extension was defined using visual inspection of the clinical knee angle (created by lines connecting the hip, knee, and ankle joint centers in the sagittal plane). As a check on this visual alignment, the knee was only considered to be in static full extension if the knee angle, as measured in the sagittal GRE images (Fig 1: the 2D acute angle between ty and fy), was within two standard deviations a previous control cohort. For this previous cohort, subjects were placed in full extension, using the same visual alignment procedure, prior to acquiring a sagittal plane 3D GRE image of the knee. If both knees qualified for the study, a single knee was randomly selected (control) or the more impaired knee (PFPS cohort) was selected for inclusion. The final study cohort consisted of 26 controls (19F/7M, 25.3±7.7 years, 166.1±9.3cm, 61.1±11.6kg) and 26 subjects diagnosed with PFPS (19F/7M, 25.9±11.1 years, 165.4±9.1cm, 62.2±10.6kg).
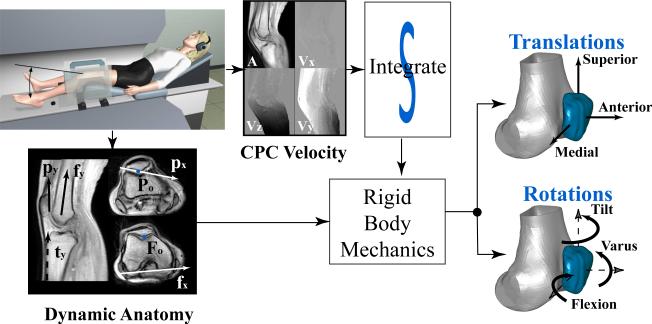
Figure 1. Flow chart for analysis of the dynamic data.
The patellar and femoral medial directions (px, fx) were parallel to the patellar lateral-posterior edge and the femoral posterior edge. In the mid-patellar sagittal image, the patellar posterior edge and the vector bisecting the distal femoral shaft defined the patellar and femoral superior direction (~py, ~fy). The 3D coordinate system was defined such that pz = px X ~py and py = pz X px. The knee angle was the acute angle between fy and ty (parallel to the tibial anterior edge, in a sagittal image just medial to the tibial tuberosity). The static coordinate system and knee angle used identical definitions. Abbreviations: A: anatomic image; Vx, Vy, and Vz: velocity in the x, y, and z directions, respectively; CPC: Cine Phase Contrast; Po and Fo: Origin of the patellar and femoral coordinate systems, respectively.
Subjects lay supine in an MRI scanner (1.5 T; GE Medical Systems, Milwaukee, WI; or 3.0 T; Philips Electronics, Eindhoven, The Netherlands) during static and dynamic image acquisition. For static scanning, the knee and hip were fully extended with the mid-patella at the center of a knee coil. The ankle was held in the anatomical neutral position using cushion blocks. Subjects were instructed to keep their muscles relaxed while static 3D sagittal T1-weighted high resolution (1mm3) gradient recall echo (GRE) images were acquired (TR=11, TE=5.1, 70-84 slices, Flip Angle = 15°). Image acquisition ranged from just distal to the tibial tuberosity to just superior to the quadriceps’ tendon insertion into the rectus femoris (RF). During dynamic scanning (Fig 1) the subject's knee was placed over a cushioned wedge, slightly flexing the hip and knee. Coupled-phased array coils were supported medial and lateral to the knee using a custom-built coil holder. Subjects cyclically flexed and extended their knee (30 cycles/minute, to the beat of an auditory metronome) while a full CPC image set (anatomic and x-, y-, and z-velocity images over 24 times frames) was acquired in a single sagittal plane. The CPC scanning parameters varied slightly between the 3.0T27 and 1.5T28 scanners, but the overall temporal resolution (61.2 msec on the 3T and 73.6msec on the 1.5T) was kept similar. Although the images were acquired in a single plane, the 3D velocity enabled tracking of musculoskeletal points of interest in all three dimensions. A 3-plane axial cine image set (anatomical images only, 24 time frames) was acquired in order to establish anatomic coordinate systems28.
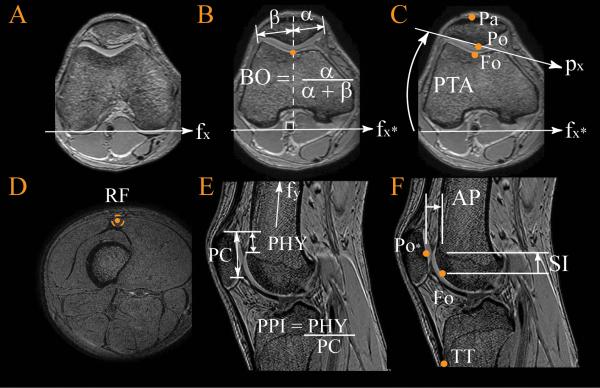
Seven static measures of interest (Fig 2: patellar tilt angle (PTA), lateral patellar displacement (LPD), anterior/posterior displacement (APS), inferior/superior displacement (SIS), bisect offset (BO), patellophyseal index (PPI), and the RF-Q-angle ) were quantified from the 3D GRE images. The subscript “S” denotes static. To quantify these measures, the 3D sagittal GRE images were reconstructed into axial images. Femoral vectors and points of interest were located in axial image at the level of the femoral epicondyle. Likewise, patellar vectors and points of interest were located in mid-patellar axial image. The PTA was quantified as the acute angle between the vectors defining the patellar posterior-lateral border and the femoral posterior edge (Fig 2C). Next, the lateral, anterior, and superior distance from the patellar origin (Po, the most posterior patellar point) to the femoral origin (Fo, the deepest point in the femoral sulcus) was defined as the LPD, APS, and SIS displacement (Fig 2C,F). For the purpose of this study medial, anterior, and superior were considered positive directions. The BO6 and the PPI22 were also measured (Fig 2B, E). Lastly, the RF-Q-angle was quantified as the acute angle between two vectors defined by three points (the tibial tuberosity, the anterior-mid-patellar, and the center of RF just superior to the myo-tendinous junction, Fig 2C,D,F). This measure was created previously to be a more precise measure of the clinical Q-angle. The 2D PF alignment measures were redefined relative to the static femoral coordinate system (Fig 2). This effectively rotated all images such that the posterior edge of the femoral condyles (at the level of the epicondylar width) and the vector bisecting the femoral shaft (in the sagittal plane) were aligned with the image right-left and inferior-superior directions, respectively. This was done to reduce errors from slight variations in subject alignment relative to the magnet25. To account for size variations across subjects, LPD, APS, and SIS were scaled by the ratio of the average epicondylar width from a previous control cohort, 76.9 mm28, to the subject-specific epicondylar width.
Figure 2. Static Magnetic Resonance Imaging-based Measures of Patellofemoral Alignment.
A) fx = the femoral medial direction, which was defined by the most posterior points on the medial and lateral condyles at the level of the epicondylar width. B) BO = bisect offset; fx* a representation of the femoral medial axis as defined in A; α and β = the shortest distance from the most medial and lateral patellar points, respectively, to a line perpendicular to fx that passes through Fo, propagated to the mid-patellar plane. C) PTA = patellar tilt angle; Po and Fo = origin of the patellar and femoral coordinate systems; px = the patellar medial direction; Pa = anterior patella. D) RF = rectus femoris. E) PPI = patellophyseal index; PC = length of patellar articular cartilage; PHY = height of patella above anterior physeal line. F) AP = anterior/posterior distance; SI = superior/inferior distance; Po* - a representation of Po, which is defined in C; TT= tibial tuberosity.
PF translation (MLK, APK, SIK) and rotation (tilt, flexion, and varus rotation) during active extension, was analytically tracked through integration of the CPC data (Fig 1). The accuracy of tracking skeletal kinematics using CPC data is less than 0.5 mm27,29 (average absolute error). These six kinematic variables were expressed relative to the dynamic femoral anatomical coordinate system (Fig 1)28, which was defined similiary to its static counterpart. PF orientation (Fig 1) was calculated using a body-fixed xyz-Cardan rotation sequence (flexion, tilt, and varus)30. All translations were scaled in an identical manner to the static measures.
Multiple regression analyses were used to establish predictive models for the PF kinematics. To determine which static variables were appropriate as input to the multiple regression analyses, individual linear regressions between each static and each dynamic variable were evaluated. This was followed by a multiple regression analysis (Enter method, SPSS Inc, Chicago, IL, v19), if multiple static variables demonstrated significant linear regressions to a single dynamic variable. The multiple regression model used only those variables. Based on guidelines for correlations31, a model with an r2 value of greater than 0.60 was defined as being strongly predictive. The numerous regression models were susceptible to type I error. Therefore, regressions were reported only if they remained significant after their p-values were adjusted using a Bonferroni-type false discovery rate procedure32. Although the PF kinematics were determined over a large range of motion, the regressions were focused on the PF kinematics from two knee angles (10°, matching the static position, and 20°), both of which could capture the more unstable PF kinematics near full extension. An a priori power analysis determined that 26 subjects per cohort were required to determine significant regression between the RF-Q-angle and MLK (α= 0.05 and β=0.80), based on a previous study5. Intraclass correlation coefficients (ICCs), using a two-way mixed effects model, were computed to evaluate intra- and inter-rater repeatability of the static PF alignment measures across 25 knees (randomly selected from both cohorts). The two raters were blinded to each others measures, as well as their original measures. A p-value < 0.05 was considered as significant.
RESULTS
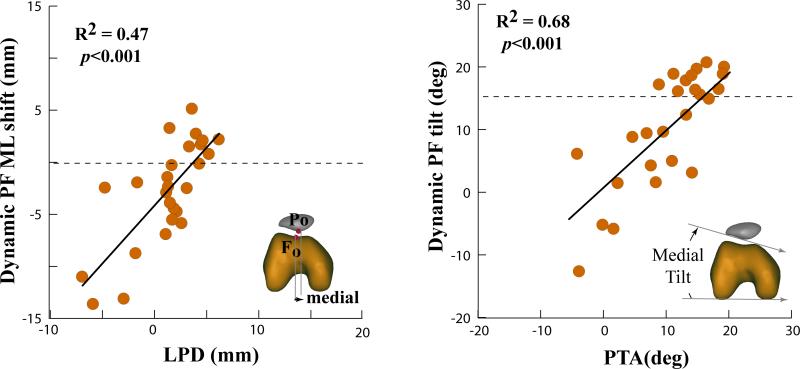
The majority of 3D PF kinematics could be predicted from static MRI measures, but static lateral patellar tilt best predicted its dynamic counterpart (r2-value ranged from 0.59 to 0.69, Fig 3 and Table 2). Multiple regression analyses tended to increase the r2-values (Table 3). This was particularly true for SIK in the PFPS cohort, where r2 increased from 0.38 to 0.77 by adding LPD and RF-Q-angle into the regression. LPD alone could explain 47% (p < 0.001) of the variability (PFPS cohort) in MLK (dynamic lateral shift). This improved to 62% (p<0.001) upon advancing to a multiple regression analysis using both LPD and RF-Q-angle. Varus rotation (PFPS and control cohorts) along with MLK and APK (control cohort) could not be predicted by a single or multiple static variables.
Figure 3. Example Linear Regression Plots for the Patellofemoral Pain Syndrome Cohort.
Control averages for the dynamic variables are provided with a dotted line. Abbreviations: PTA: patellar tilt angle; ML= the medial-lateral location of the patellar origin relative to the femoral origin; LPD= lateral patellar displacement; deg= degree; mm= millimeter; r2= coefficients of determination.
Table 2.
Coefficients of determination (r2) for the control (C), patellofemoral pain syndrome (PFPS), and combined (All) cohorts
| All | C | PFPS | All | C | PFPS | All | C | PFPS | |
|---|---|---|---|---|---|---|---|---|---|
| Translations | MLK | SIK | APK | ||||||
| BO | 0.27** | 0.32 | |||||||
| LPD | 0.32** | 0.47** | 0.22** | 0.43** | |||||
| APS | 0.18 | ||||||||
| SIS | 0.43** | 0.48** | 0.38** | ||||||
| PPI | 0.28** | 0.36** | 0.26** | ||||||
| PTA | 0.23** | 0.31 | |||||||
| RF-Q | 0.19 | 0.35 | 0.30 | ||||||
| Rotations | Flexion | Tilt | Varus | ||||||
| BO | 0.49** | 0.27 | 0.54** | ||||||
| LPD | 0.23** | 0.29 | |||||||
| APS | |||||||||
| SIS | 0.26** | 0.42** | |||||||
| PPI | 0.23** | 0.41** | |||||||
| PTA | 0.69** | 0.59** | 0.68** | 0.17 | |||||
| RF-Q | 0.16 | 0.37 | |||||||
Indicates p < 0.001, otherwise p < 0.05.
Nonsignificant regressions are not shown. For the full regression equations, see supplemental material.
Abbreviations: BO = Bisect Offset; LPD, APS, and SIS = The static medial-lateral, anterior-posterior, and superior-inferior location of the patellar origin relative to the femoral origin (static); PPI = patellophyseal index; PTA = patellar tilt angle; RF-Q angle = The rectus femoris quadriceps angle; MLK, SIK, APK = The medial-lateral, superior-inferior, and anterior posterior location of the patellar origin relative to the femoral origin, measured during active extension at 10° knee angle.
Table 3.
Multiple Regression Equations.
| Dynamic Variable | Multiple Regressions | R2 | p- value |
|---|---|---|---|
| All | |||
| MLK | = −4.61 + 0.61*LPD −0.15*PTA | 0.38 | <0.001 |
| SIK | = 13.48 −0.62*SIS −0.38*LPD-0.14*RF_Q | 0.53 | <0.001 |
| Flexion | = 8.435 −0.40*SIS −0.57*PAS | 0.36 | <0.001 |
| PFPS Cohort | |||
| MLK | = −4.14 + 1.52*LPD −0.13*RF_Q | 0.62 | <0.000 |
| APK | = 2.34 −0.50*APS −0.001*RF_Q | 0.38 | 0.001 |
| SIK | = 16.80 + 0.51*SIS −1.45*LPD +0.15*RF_Q | 0.77 | <0.001 |
| Flexion | = 7.553 −0.307*SIS −0.540*APS | 0.32 | 0.003 |
| Control Cohort | |||
| Flexion | = 20.816 −0.514*SIS −0.383*PTA | 0.65 | <0.001 |
Multiple Regressions listed if it increased the predictability more than 5 percentage points from the linear regression.
Abbreviations: MLK, SIK, APK = The medial-lateral, superior-inferior, and anterior-posterior location of the patellar origin relative to the femoral origin measured during active extension at 10° knee angle; LPD, APS, and SIS = the static medial-lateral, anterior-posterior, and superior-inferior location of the patellar origin relative to the femoral origin; PTA = patellar tilt angle; RF-Q angle = The rectus femoris quadriceps angle.
The regressions at 20° were typically weaker than at 10° and, thus were not reported. This leads to the likley conclusion that the predictive values worsen with increasing variance between the static and dynamic knee angles.
All static MRI measures showed excellent intra- and inter-rater repeatability, with ICCs ranging from 0.95-0.99 (Table 1). The two cohorts were, on average, very well matched with no significant differences in demographics found between cohorts. The MR based knee angle (10.6°± 3.3° and 10.8° ± 4.2° in the control and PFPS cohorts, respectively) tended to overestimate the clinical knee angle.
Table 1.
Intraclass Correlation Coefficients for static Magnetic Resonance Imaging-based Surrogates.
| Parameter | PTA | BO | LPD | SIS | APS | RF Q-angle |
|---|---|---|---|---|---|---|
| Inter | 0.995 | 0.985 | 0.979 | 0.990 | 0.948 | 0.985 |
| Intra | 0.993 | 0.980 | 0.968 | 0.992 | 0.953 | 0.989 |
Abbreviations: PTA= patellar tilt angle; BO= Bisect Offset; LPD, APS and SIS= The medial-lateral, anterior-posterior, and superior-inferior location of the patellar origin relative to the femoral origin (static); RF-Q angle= The rectus femoris quadriceps angle.
DISCUSSION
Recent breakthroughs in 3D dynamic imaging technologies19,29 have enabled the evaluation of more subtle cases of maltracking6 and the testing of numerous underlying assumptions governing modern PFPS diagnostics and interventions19; 28. As these 3D dynamic imaging technologies have not been clinically available, an often unstated assumption has been that static imaging can be used as a surrogate for quantifying the dynamic state of the joint under active quadriceps control. The current findings demonstrate that static measures of PF alignment, quantified in 2D images acquired with the knee in full extension, can only predict a portion of the 3D PF kinematics during a loaded volitional task.
Although significant linear regressions existed for most kinematic variables, the majority of their variability could not be explained by a single static surrogate. This low predictability is likely due to the fact that the forces on the patella from femoral sulcus begin to lessen as the knee moves into terminal extension. This allows the overall dynamic state of the joint to be more strongly influenced by passive soft tissue and active quadriceps forces in terminal extension6,14,33. The interaction between the contact, passive soft-tissue, and active quadriceps forces varies across subjects, further reducing the predictability of the dynamic state. For example, a large portion of the unexplained variance in SIK may be attributed to its dependence on the nominal lengths and material properties of the patellar and quadriceps tendons, which can vary greatly across subjects, particularly in PFPS18,34.
The static PTA was the only variable that strongly predicted its dynamic counterpart. This supports a previous study that found strong agreement between excessive lateral tilt measured using a clinical exam and measured using 2D static MRI.13 The strong relationship between the static PTA and PF dynamic lateral tilt may indicate that quadriceps activity has minimal effect on patellar tilt during terminal extension. Thus, even though the femoral sulcus influence diminishes in terminal extension, it may remain a controlling force for lateral patellar tilt4. The regression was likely further strengthened by the large range of values for lateral tilt across both cohorts. Yet, this range in value is the likely reason why none of the recent 3D PF kinematics/alignment studies with active quadriceps reported significant differences in tilt between the PFPS and control cohorts18-20.
In a previous study McWalter and colleagues35 found that the value of a single measure of PF joint alignment, acquired statically at 30° flexion with active isometric quadriceps contraction, could not predict the slope (rate of change relative to knee angle) of 3D PF alignment measures acquired statically at various knee flexion angles in a cohort of healthy volunteers. This inability to predict the rate of change PF alignment may be due to the low reliability (0.58-0.59) in measuring slope using the static methodology reported by McWalter and colleagues20. Although two previous studies18,20 have demonstrated significant differences in the slope of PF alignment/kinematic variables when comparing cohorts of subjects with PF pain to control cohorts, the clinical utility of evaluating slope has not been established. Thus, clinical diagnosis of maltracking remains focused on the value (not slope) of PF aligment/kinematics in terminal extension, as this is where the restraints of the femoral sulcus on the patella are weakest and pathology is typically most evident6,18,36.
Several studies have investigated static joint alignment measures, yet few studies17,37-41 have reported the reliability of these measures. The reliability measures from the current study (0.94 – 0.99) were better than previous studies and satisfied the guidline for reasonable clinical validity (ICC>0.90)38. Only one previous study evaluating patella alta37,40,41 reported “good” inter-rater reliabilities (ICC > 0.7538). The studies measuring patellar tilt and BO reported good reliabilities for measures acquired during active leg extensions (ICC = 0.9017) and passively (ICC=0.76 for BO and ICC=0.86 for PTA)39.
The primary limitation of this study was that specific static counterparts for dynamic PF flexion and varus rotation were not established, thus the predictability of these dynamic variables remained low. Another possible limitation was that the exercise evaluated was open-chain, whereas PF pain is most often thought to be exacerbated by weight-bearing (closed-chain) activities. Yet, PF pain can be induced during free extension19, as well as during long term stationary sitting with flexed knees42. Also, the exercise used in the current study emphasized the conditions of joint instability by requiring a quadriceps force in terminal extension, where the femoral constraints on the patella are at a minimum and pathomechanics are most evident. Based on the work of Hungeford43, this required quadriceps force in terminal extension was likely greater than that required at or near full extension in previous studies evaluating PF kinematics during free squats19,44. Regardless, this study clearly demonstrated the robustness of using specific static variables, such as the patellar tilt angle, to predict PF joint motion. Future studies should examine additional static surrogates for improved prediction.
In conclusion, static PF joint assessment cannot fully represent the dynamic state of this joint and using such static measures for diagnosis would likely produce false negative diagnoses7,15,17. This makes it imperitave that the current precise, accurate, 3D, dynamic imaging techniques be translated into clinical tools in order to improve the diagnosis of PF pathomechanics 7,17,33,45 by providing accurate and precise quantification of PF kinematics, which expands beyond the axial plane, during a volitional activity requiring quadriceps loading.
ACKNOWLEDGEMENTS
This research was supported by Biomedical Engineering Summer Internship Program (BESIP), the Intramural Research Program of the NIH, and the Clinical Center at the NIH. Special thanks is given to S. Sadeghi, AJ Behnam, C. Zampieri-Gallagher, TJ Brindle, CY Shieh, B. Damaska, and the Diagnostic Radiology Department at the NIH for their support and research time.
REFERENCES
- 1.Boling M, Padua D, Marshall S, et al. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2009 doi: 10.1111/j.1600-0838.2009.00996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amis AA. Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc. 2007;15:48–56. doi: 10.1097/JSA.0b013e318053eb74. [DOI] [PubMed] [Google Scholar]
- 3.Keser S, Savranlar A, Bayar A, et al. Is there a relationship between anterior knee pain and femoral trochlear dysplasia? Assessment of lateral trochlear inclination by magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2008;16:911–915. doi: 10.1007/s00167-008-0571-5. [DOI] [PubMed] [Google Scholar]
- 4.Harbaugh CM, Wilson NA, Sheehan FT. Correlating femoral shape with patellar kinematics in patients with patellofemoral pain. J Orthop Res. 2010;28:865–872. doi: 10.1002/jor.21101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheehan FT, Derasari A, Fine KM, et al. Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res. 2010;468:266–275. doi: 10.1007/s11999-009-0880-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brossmann J, Muhle C, Schroder C, et al. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology. 1993;187:205–212. doi: 10.1148/radiology.187.1.8451415. [DOI] [PubMed] [Google Scholar]
- 7.Biedert RM, Sanchis-Alfonso V. Sources of anterior knee pain. Clin Sports Med. 2002;21:335–347, vii.. doi: 10.1016/s0278-5919(02)00026-1. [DOI] [PubMed] [Google Scholar]
- 8.Farrokhi S, Keyak JH, Powers CM. Individuals with patellofemoral pain exhibit greater patellofemoral joint stress: a finite element analysis study. Osteoarthritis Cartilage. 2011;19:287–294. doi: 10.1016/j.joca.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laurin CA, Levesque HP, Dussault R, et al. The abnormal lateral patellofemoral angle: a diagnostic roentgenographic sign of recurrent patellar subluxation. J Bone Joint Surg Am. 1978;60:55–60. [PubMed] [Google Scholar]
- 10.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 11.Walker C, Cassar-Pullicino VN, Vaisha R, McCall IW. The patello-femoral joint--a critical appraisal of its geometric assessment utilizing conventional axial radiography and computed arthro-tomography. Br J Radiol. 1993;66:755–761. doi: 10.1259/0007-1285-66-789-755. [DOI] [PubMed] [Google Scholar]
- 12.Hunter DJ, Zhang YQ, Niu JB, et al. Patella malalignment, pain and patellofemoral progression: the Health ABC Study. Osteoarthritis Cartilage. 2007;15:1120–1127. doi: 10.1016/j.joca.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grelsamer RP, Weinstein CH, Gould J, Dubey A. Patellar tilt: the physical examination correlates with MR imaging. Knee. 2008;15:3–8. doi: 10.1016/j.knee.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 14.Sasaki T, Yagi T. Subluxation of the patella. Investigation by computerized tomography. Int Orthop. 1986;10:115–120. [PubMed] [Google Scholar]
- 15.Conway WF, Hayes CW, Loughran T, et al. Cross-sectional imaging of the patellofemoral joint and surrounding structures. Radiographics. 1991;11:195–217. doi: 10.1148/radiographics.11.2.2028059. [DOI] [PubMed] [Google Scholar]
- 16.Stanford W, Phelan J, Kathol MH, et al. Patellofemoral joint motion: evaluation by ultrafast computed tomography. Skeletal Radiol. 1988;17:487–492. doi: 10.1007/BF00364042. [DOI] [PubMed] [Google Scholar]
- 17.Ward SR, Shellock FG, Terk MR, et al. Assessment of patellofemoral relationships using kinematic MRI: comparison between qualitative and quantitative methods. J Magn Reson Imaging. 2002;16:69–74. doi: 10.1002/jmri.10124. [DOI] [PubMed] [Google Scholar]
- 18.Sheehan FT, Derasari A, Brindle TJ, Alter KE. Understanding patellofemoral pain with maltracking in the presence of joint laxity: complete 3D in vivo patellofemoral and tibiofemoral kinematics. J Orthop Res. 2009;27:561–570. doi: 10.1002/jor.20783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson NA, Press JM, Koh JL, et al. In vivo noninvasive evaluation of abnormal patellar tracking during squatting in patients with patellofemoral pain. J Bone Joint Surg Am. 2009;91:558–566. doi: 10.2106/JBJS.G.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacIntyre NJ, Hill NA, Fellows RA, et al. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg Am. 2006;88:2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- 21.Insall J, Goldberg V, Salvati E. Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res. 1972;88:67–69. doi: 10.1097/00003086-197210000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Ali SA, Helmer R, Terk MR. Patella alta: lack of correlation between patellotrochlear cartilage congruence and commonly used patellar height ratios. AJR Am J Roentgenol. 2009;193:1361–1366. doi: 10.2214/AJR.09.2729. [DOI] [PubMed] [Google Scholar]
- 23.Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am. 2007;89:1749–1755. doi: 10.2106/JBJS.F.00508. [DOI] [PubMed] [Google Scholar]
- 24.Sheehan FT, Babushkina A, Alter KE. Kinematic determinants of anterior knee pain in cerebral palsy: a case-control study. Arch Phys Med Rehabil. 2012;93:1431–1440. doi: 10.1016/j.apmr.2012.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shibanuma N, Sheehan FT, Stanhope SJ. Limb positioning is critical for defining patellofemoral alignment and femoral shape. Clin Orthop Relat Res. 2005:198–206. doi: 10.1097/01.blo.0000155078.52475.63. [DOI] [PubMed] [Google Scholar]
- 26.Powers CM, Bolgla LA, Callaghan M, et al. Patellofemoral pain: proximal, distal, and local factors, 2nd international research retreat. J Orthop Sports Phys Ther. 2012;42:A1–A54. doi: 10.2519/jospt.2012.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Behnam AJ, Herzka DA, Sheehan FT. Assessing the accuracy and precision of musculoskeletal motion tracking using cine-PC MRI on a 3.0T platform. J Biomech. 2011;44:193–197. doi: 10.1016/j.jbiomech.2010.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seisler AR, Sheehan FT. Normative three-dimensional patellofemoral and tibiofemoral kinematics: a dynamic, in vivo study. IEEE Trans Biomed Eng. 2007;54:1333–1341. doi: 10.1109/TBME.2007.890735. [DOI] [PubMed] [Google Scholar]
- 29.Sheehan FT, Zajac FE, Drace JE. Using cine phase contrast magnetic resonance imaging to non-invasively study in vivo knee dynamics. J Biomech. 1998;31:21–26. doi: 10.1016/s0021-9290(97)00109-7. [DOI] [PubMed] [Google Scholar]
- 30.Sheehan FT, Mitiguy P. In regards to the “ISB recommendations for standardization in the reporting of kinematic data”. J Biomech. 1999;32:1135–1136. doi: 10.1016/s0021-9290(99)00077-9. [DOI] [PubMed] [Google Scholar]
- 31.Hebel JR, McCarter RJ. A study guide to epidemiology and biostatistics. 7th ed. Jones & Bartlett Learning; Sudbury, Mass: 2012. Correlations. p. 90. [Google Scholar]
- 32.Benjamini Y, Hochber Y. Controlling the False Discovery Rate: a Practical and Powerful Approach to Mulitple Testing. 1995;57:289–300. [Google Scholar]
- 33.Guzzanti V, Gigante A, Di Lazzaro A, Fabbriciani C. Patellofemoral malalignment in adolescents. Computerized tomographic assessment with or without quadriceps contraction. Am J Sports Med. 1994;22:55–60. doi: 10.1177/036354659402200110. [DOI] [PubMed] [Google Scholar]
- 34.Witvrouw E, Lysens R, Bellemans J, et al. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000;28:480–489. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- 35.McWalter EJ, Macintyre NJ, Cibere J, Wilson DR. A single measure of patellar kinematics is an inadequate surrogate marker for patterns of three-dimensional kinematics in healthy knees. Knee. 2010;17:135–140. doi: 10.1016/j.knee.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 36.Heegaard J, Leyvraz PF, Van Kampen A, et al. Influence of soft structures on patellar three-dimensional tracking. Clin Orthop Relat Res. 1994:235–243. [PubMed] [Google Scholar]
- 37.Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006;14:707–712. doi: 10.1007/s00167-005-0015-4. [DOI] [PubMed] [Google Scholar]
- 38.Portney L, Watkins M. Statistical Measures of Reliability. Foundations of Clinical Research Applications to Practice. 2009 [Google Scholar]
- 39.Jan MH, Lin DH, Lin CH, et al. The effects of quadriceps contraction on different patellofemoral alignment subtypes: an axial computed tomography study. J Orthop Sports Phys Ther. 2009;39:264–269. doi: 10.2519/jospt.2009.2873. [DOI] [PubMed] [Google Scholar]
- 40.Davies AP, Costa ML, Shepstone L, et al. The sulcus angle and malalignment of the extensor mechanism of the knee. J Bone Joint Surg Br. 2000;82:1162–1166. doi: 10.1302/0301-620x.82b8.10833. [DOI] [PubMed] [Google Scholar]
- 41.Seil R, Muller B, Georg T, et al. Reliability and interobserver variability in radiological patellar height ratios. Knee Surg Sports Traumatol Arthrosc. 2000;8:231–236. doi: 10.1007/s001670000121. [DOI] [PubMed] [Google Scholar]
- 42.Kujala UM, Jaakkola LH, Koskinen SK, et al. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 43.Hungerford DS, Barry M. Biomechanics of the patellofemoral joint. Clin Orthop Relat Res. 1979;144:9–15. [PubMed] [Google Scholar]
- 44.Powers CM, Ward SR, Fredericson M, et al. Patellofemoral kinematics during weight- bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. J Orthop Sports Phys Ther. 2003;33:677–685. doi: 10.2519/jospt.2003.33.11.677. [DOI] [PubMed] [Google Scholar]
- 45.Schutzer SF, Ramsby GR, Fulkerson JP. Computed tomographic classification of patellofemoral pain patients. Orthop Clin North Am. 1986;17:235–248. [PubMed] [Google Scholar]