Abstract
Neurobehavioral disinhibition (ND) is a complex condition reflecting a wide range of problems involving difficulties with emotion regulation and behavior control. Respiratory sinus arrhythmia (RSA) is a physiological correlate of emotion regulation that has been studied in a variety of at-risk populations; however, there are no studies of RSA in children with ND. Data were drawn from a prospective longitudinal study of prenatal substance exposure that included 1,073 participants. Baseline RSA and RSA reactivity to an attention-demanding task were assessed at 3, 4, 5, and 6 years. ND was assessed at ages 8/9, 11, and 13/14 years via behavioral dysregulation and executive dysfunction composite measures. Greater exposure to early adversity was related to less RSA reactivity at 3 years, increases in RSA reactivity from ages 3 to 6 years, and increased behavioral dysregulation from ages 8/9 to 13/14. RSA reactivity was examined as a moderator of the association between early adversity and changes in ND. A significant Early Adversity × RSA Reactivity quadratic interaction revealed that children with decelerations in RSA reactivity exhibited increases in behavioral dysregulation, regardless of their exposure to early adversity. However, greater exposure to early adversity was related to greater increases in behavioral dysregulation, but only if children exhibited accelerations in RSA reactivity from ages 3 to 6 years. The results contribute to our understanding of how interactions across multiple levels of analysis contribute to the development of ND.
The identification of factors that contribute to the development of psychological disorders across behavioral, environmental, and biological levels of analysis is of central importance to the field of developmental psychopathology. One example that holds promise is neurobehavioral disinhibition (ND), a complex condition of emotional and behavioral dysregulation reflecting a wide range of problems including oppositional defiant disorder (ODD), conduct disorder, attention-deficit/hyperactivity disorder (ADHD), major depressive disorder, and the initiation of substance use (Habeych, Charles, Sclabassi, Kirisci, & Tarter, 2005; Lester et al., 2012; McNamee et al., 2008; Tarter et al., 2003). Children with ND appear to follow fairly consistent negative longitudinal trajectories that include peer rejection, academic difficulties, delinquency, and high rates of mental health, special education, residential care, and juvenile justice system involvement (Clausen, Landsverk, Ganger, Chadwick, & Litrownik, 1998; Harden, 2004). Key features of ND include difficulties with emotion regulation, impulse control (Iacono, Carlson, Taylor, Elkins, & McGue, 1999), and executive functioning (Tarter et al., 2003). Emotion regulation is critical for adaptive responding in social situations and social affiliation, key constructs that are impaired among youths with externalizing behavior (Hill, Degnan, Calkins, & Keane, 2006; Vasilev, Crowell, Beauchaine, Mead, & Gatzke-Kopp, 2009), conduct disorder and ODD (Beauchaine, Gartner, & Hagen, 2000; Beauchaine, Gatzke-Kopp, & Mead, 2007; Beauchaine, Hinshaw, & Pang, 2010; Beauchaine, Hong, & Marsh, 2008), major depressive disorder (Rottenberg, Gross, & Gotlib, 2005), and ADHD (Musser et al., 2011), most of which are included on the spectrum of ND (Iacono et al., 1999).
Children exposed to substances prenatally and who have faced significant early life adversity may be particularly likely to develop ND (Chapman, Tarter, Kirisci, & Cornelius, 2007; Fisher et al., 2011), perhaps in part because such early life stress is known to affect neural systems associated with behavior regulation and modulation (Kishiyama, Boyce, Jimenez, Perry, & Knight, 2009). Respiratory sinus arrhythmia (RSA) is a physiological correlate of emotion regulation that has been studied in a variety of typically developing and at-risk populations; however, there are no studies of RSA in children with ND. RSA is a phenomenon whereby heart rate shows high frequency variability in time with respiration (Beauchaine, 2001; Porges, 2007). There is likely considerable equifinality, or the process by which different etiological pathways lead to the same disorder, to the development of ND that includes transactions across genetic, physiologic, and contextual levels (Fisher et al., 2011). Incorporating measures of RSA into longitudinal studies of ND may help us to identify children who are most susceptible to the development of ND by virtue of their profile of RSA reactivity across early childhood and their exposure to adverse events early in life.
RSA and ND
RSA is typically measured in two ways: during baseline and in response to task demands, termed RSA reactivity. High baseline RSA reflects the functional relationship between the central nervous system and the heart as mediated by the vagus (Berntson et al., 1997; Porges, 2007). High baseline RSA is thought to reflect a baseline of neural integrity and a readiness to respond to environmental stressors (Beauchaine, 2001). Change in RSA in response to acute stress is termed RSA reactivity. We use the term RSA reactivity to reflect decreases in RSA in response to task demands. In typically developing children, RSA reliably decreases in response to challenge and increases once the challenge has resolved (Beauchaine, 2001). Moderate RSA withdrawal in response to attention-demanding tasks is functional and may reflect “optimal” engagement with the environment (Beauchaine, 2001; Marcovitch et al., 2010). In contrast, greater RSA withdrawal may instead be a form of emotional lability suggestive of fight/flight responding (Beauchaine, 2001).
It may be particularly important to study changes in RSA during early childhood. Alterations in RSA associated with later externalizing psychopathology, a key component of the ND construct, appear to develop sometime between preschool and middle childhood (Beauchaine et al., 2007). Given the presumed plasticity of the parasympathetic nervous system during early childhood, changes in RSA across this time period because of early adverse experiences and/or prenatal substance exposure may be prognostic of later externalizing behavior and behavior dysregulation (Beauchaine, 2001).
Previous work has focused on the parasympathetic nervous system and the behavior dysregulation component of ND. Although there are exceptions (Musser et al., 2011), youths prone to ND, including preschoolers with ADHD and ODD (Crowell et al., 2006) and adolescents (Beauchaine et al., 2000), and boys with conduct problems (Beauchaine, Hong, et al., 2008) exhibit lower baseline RSA. Children (Beauchaine et al., 2007) and adolescents (Beauchaine et al., 2000) with clinical levels of externalizing behavior, and boys with conduct problems (Beauchaine, Hong, et al., 2008) also exhibit attenuated baseline RSA. In addition, boys (but not girls) with lower initial levels of baseline RSA had externalizing behavior that increased across adolescence (El-Sheikh & Hinnant, 2011).
Some studies have found no significant association between RSA reactivity and externalizing behavior in clinical samples (Beauchaine et al., 2000, 2007), bit others found significant relations in community samples (Keller & El-Sheikh, 2009) and in children with ADHD (Musser et al., 2011). For instance, children with reduced autonomic functioning in the form of lower RSA reactivity (Keller & El-Sheikh, 2009) and the combination of both low baseline RSA and lower RSA reactivity (Hinnant & El-Sheikh, 2009) exhibited the greatest levels of externalizing behavior. In contrast, others (Calkins, Graziano, & Keane, 2007) found no differences in baseline RSA among 5-year-old children at risk for behavior problems. However, children at risk for both externalizing and internalizing problems exhibited the greatest RSA reactivity compared to children with low behavior problems and children at risk for externalizing problems only.
Although youths at risk for the development of externalizing disorder may exhibit a profile of reduced autonomic functioning, a second plausible pathway to the development of ND exists. The theory of diathesis stress suggests that a “risk” factor in combination with an adverse or stressful environment leads to greater risk for the development of problem behavior (Monroe & Simons, 1991). Children who are more physiologically reactive may be more likely to exhibit ND if they are also raised in adverse environments. For instance, in a community sample of children, Obradović, Bush, Stamperdahl, Adler, and Boyce (2010) found that children with greater RSA reactivity exhibited less prosocial behavior and school engagement, but only if they were exposed to greater environmental adversity (operationalized as a cumulative index of six measures of family stress). Thus, RSA reactivity may moderate the effect of early adversity and/or prenatal substance exposure such that children who are more reactive will be more likely to exhibit growth in ND if exposed to more substances in utero or if reared in particularly adverse environments.
There is comparatively less information about RSA and executive dysfunction, a second component of ND. Children with higher baseline RSA perform better on tasks of attention and working memory (Hansen, Johnsen, & Thayer, 2003; Marcovitch et al., 2010; Staton, El-Sheikh, & Buckhalt, 2009), perhaps because these children are better able to engage with environmental demands and also self-regulate during both cognitive and emotional challenges. Moderate decreases in RSA appear to be related to improved executive functioning, including greater on-task behavior, behavioral inhibition, and set shifting (Blair, 2003; Marcovitch et al., 2010), though null findings with RSA reactivity and executive functions have also been found (Staton et al., 2009). Thus, high baseline RSA and moderate decreases in RSA in response to challenge may be prognostic of better executive functioning compared to low baseline RSA and an absence of RSA reactivity.
Prenatal Substance Exposure, Early Adversity, and RSA
The purpose of many prenatal drug exposure studies is to examine the effects of a single substance (such as cocaine), while controlling for the effects of all other substances (such as alcohol, tobacco, and marijuana). A complementary approach is to take into account recent work suggesting that prenatal substance exposure is a stressor (Lester & Padbury, 2009), and as such, cumulative prenatal stress models may provide an alternative way of modeling the contribution of prenatal substance exposure to relevant developmental processes. Specifically, in addition to its teratogenic properties, prenatal substance exposure can alter the infant's physiological response to the postnatal environment (Lester, Marsit, Conradt, Bromer, & Padbury, in press; Lester & Padbury, 2009). That is, exposure to substances prenatally acts as a stressor that may alter the expression of specific genes important to placental function in late gestation (Lester & Padbury, 2009), which may lead to fetal exposure of high levels of maternal cortisol (Lester & Padbury, 2009). The effects of prenatal substance exposure as an intrauterine stressor that alters physiological response systems (Lester & Padbury, 2009) could result in disrupted parasympathetic responding, leading to the development of ND. A similar process is thought to occur in response to prenatal alcohol (Hellemans, Sliwowska, Verma, & Weinberg, 2010) and tobacco (Heim, Plotsky, & Nemeroff, 2004) exposure. Furthermore, women who use substances prenatally typically use other substances; therefore, polydrug use could be conceptualized as a cumulative prenatal stressor (Lester & Padbury, 2009). Support for this view comes from the work of Fisher et al. (2011), who found that a summative index of prenatal substance exposure predicted blunted hypothalamus–pituitary–adrenal axis reactivity among children in foster care. The literature linking prenatal substance exposure to RSA is small, and no study that we know of has examined the effects of polysubstance exposure. Thus, we focused on polysubstance exposure, with the caveat that different substances may impact RSA via different mechanisms that are unknown thus far.
Studies examining the effects of prenatal substance exposure on RSA are mixed, and they are largely limited to infants. Infants with prenatal substance exposure have lower levels of baseline RSA at 1 and 7 months than do nonexposed infants (Schuetze & Eiden, 2006; Schuetze, Eiden, & Edwards, 2009), and an absence of RSA reactivity at 7 months (Schuetze, Eiden, & Coles, 2007). Other groups found no significant associations with either baseline RSA (DiPietro, Suess, Wheeler, Smouse, & Newlin, 1995) or RSA reactivity (DiPietro et al., 1995; Sheinkopf et al., 2007) compared to non-exposed children. Increased baseline RSA (Mehta et al., 1993) has also been reported in infants with prenatal cocaine exposure, which may be due to the need to utilize greater neurobiological resources in order to meet environmental demands.
The development of children with prenatal substance exposure is also complicated by a host of additional risk factors. Early adverse experiences among children with prenatal substance exposure tend to co-occur and include exposure to parental psychopathology, neighborhood violence, chaotic home environments, and lack of monetary resources (Dong et al., 2004; Propper, 2012), making it extremely difficult to separate the effect of one adverse experience from the other. Many researchers therefore take a cumulative risk approach to studying the impact of co-occurring risk factors on physiological functioning (Eiden, Granger, Schuetze, & Veira, 2011; Fisher et al., 2011; Sameroff, Seifer, Baldwin, & Baldwin, 1993). Cumulative risk models have also been shown to be a more powerful predictor of externalizing and internalizing behavior among children with prenatal substance exposure than risks examined in isolation (Yumoto, Jacobson, & Jacobson, 2008).
Early adverse experiences have been related to the sympathetic and hypothalamus–pituitary–adrenal systems (Blair et al., 2011; Gunnar & Fisher, 2006; Heim et al., 2004; Lupien, King, Meaney, & McEwen, 2001; Saridjan et al., 2010), though evidence of how these adverse experiences impact the parasympathetic system is scarce (Propper, 2012), despite known associations between early adversity and emotion regulation (Pechtel & Pizzagalli, 2011; Tottenham et al., 2011). Though there are exceptions, low income (Propper, 2012), exposure to domestic violence (Rigterink, Fainsilber Katz, & Hessler, 2010), and marital conflict (El-Sheikh & Hinnant, 2011) have been associated with altered RSA either in the form of lower baseline RSA (Field, Pickens, Fox, Nawrocki, & Gonzalez, 1995; Pickens & Field, 1995; Schuetze & Eiden, 2006; Schuetze et al., 2009) or less growth in baseline RSA (Rigterink et al., 2010). El-Sheikh and Hinnant (2011) found that boys with greater RSA reactivity who experienced higher marital conflict at age 8 or increasing marital conflict from ages 8 to 11 exhibited decreases in baseline RSA across early adolescence, suggesting “wear and tear” on the parasympathetic system. Exposure to adverse conditions among children with prenatal substance exposure could exacerbate an already sensitive physiological stress system (Lester & Padbury, 2009), contributing to difficulties with emotion regulation and risk for the development of ND. In other words, children with prenatal substance exposure may be at more of a disadvantage by virtue of the increased likelihood of exposure to adverse conditions postnatally.
Study Aims and Hypotheses
Data from this study come from a prospective longitudinal investigation of children with prenatal substance exposure and from whom extensive measures of early adversity and ND were assessed. Across early childhood, assessments of RSA at baseline and in response to challenge were conducted. We thus have the unique opportunity to examine the effects of prenatal substance exposure and early adversity on growth in baseline RSA and RSA reactivity when these physiological systems are in the process of maturing and are arguably quite vulnerable to environmental influence (Beauchaine, Neuhaus, Brenner, & Gatzke-Kopp, 2008). We focused on RSA as a possible physiological correlate of ND owing to its association with emotion regulation.
There are inconsistencies regarding which disorders are included as components of ND. Tarter et al. (2003) include both internalizing and externalizing problems because both are related to problems with emotional and behavioral dysregulation and frequently co-occur, whereas others (Krueger et al., 2002; Krueger & South, 2009) include only externalizing symptoms. Tarter et al. also include executive function deficits in their model of ND while others do not (Iacono, Malone, & McGue, 2008; Krueger & South, 2009). Furthermore, adolescents whose parents have substance use disorders are frequently included in studies by Tarter. Based on careful consideration of these inconsistencies in the literature, and because of the similarities in our two samples, we decided to follow Tarter et al.'s approach to modeling ND, which includes both internalizing and externalizing symptoms as well as executive dysfunction. We focused on the construct of ND, rather than its component parts, based on observations that psychiatric disorders rarely occur in isolation but often occur in clusters (Lilienfeld, 2003).
We examined growth in ND using a measure of ND validated with the current sample from middle childhood to adolescence (Fisher et al., 2011; Lester et al., 2012). ND was assessed during the transition to adolescence because it is during this time that extensive development in prefrontal areas are associated with the self-regulatory and executive function components of ND. We employed longitudinal growth modeling to better understand both normative and problematic growth trajectories of ND, as well as the impact of prenatal substance exposure, early adversity, RSA, and their interaction on this growth.
Our first goal was to describe the unconditional growth trajectories of baseline RSA and RSA reactivity at ages 3, 4, 5, and 6 years. On the basis of prior evidence, we expected that baseline RSA would increase with age (Schuetze et al., 2009), whereas the magnitude of RSA reactivity would decrease (Blandon, Calkins, Keane, & O'Brien, 2010; Propper et al., 2008). Our second goal was to examine the main effects of prenatal substance exposure, early adversity, and RSA on the development of the behavior dysregulation and executive dysfunction components of ND. We hypothesized that decreases in baseline RSA and increases in RSA reactivity would be associated with increases in behavior dysregulation. Following prior research, we expected that greater increases in baseline RSA and moderate decreases in RSA reactivity over time would be associated with lower levels of executive dysfunction. Based on prior evidence with this sample, we expected that greater levels of prenatal substance exposure and early adversity (Fisher et al., 2011) would be related to increases in both behavior dysregulation and executive dysfunction over time, even when including measures of RSA in our models. Motivated by theories suggesting that interactions across multiple levels of analysis contribute to the development of psychopathology, our third goal was to test interactions between our stress variables (prenatal substance exposure and early adversity) and RSA on growth in ND. Based on the theory of diathesis stress, we expected that greater early adversity and prenatal substance exposure, combined with increased RSA reactivity or decreased baseline RSA (in separate models), would be related to increases in ND (both the behavior dysregulation and executive dysfunction constructs) in adolescence.
Method
Participants
We used data collected from 1,387 participants in the Maternal Lifestyle Study (MLS), a multisite (Detroit, MI; Memphis, TN; Miami, FL; and Providence, RI) investigation of the effects of prenatal substance exposure in a longitudinal follow-up from ages 1 month to 16 years. Details on the enrollment and exclusion criteria are described elsewhere (Lester et al., 2002). In brief, families were selected to be in the exposed group (i.e., maternal report of cocaine or opiate use during pregnancy and gas chromatography–mass spectrometry confirmation of presumptive positive meconium screens for cocaine or opiate metabolites) or the comparison group (i.e., maternal denial of cocaine or opiate use during the pregnancy and a negative enzyme multiplied immunoassay meconium screen for cocaine and opiate metabolites). The exposed and comparison youths were group matched on race, sex, and gestational age within each study site. Other substances associated with cocaine use (e.g., alcohol, tobacco, and marijuana) were present in both groups so that group differences could be attributed to cocaine. Thus, most participants were polysubstance exposed.
The study was approved by the institutional review board at each study site, and written informed consent (caregivers) was obtained from all participants. Each site had a certificate of confidentiality from the National Institute on Drug Abuse. For this study, we used data from visits to the hospital clinic at ages 3, 4, 5, 6, 9, 11, and 13 years. The MLS sample includes children in the following racial and ethnic categories: African American (77%), Caucasian (16%), Hispanic (6%), and children whose parents identified other racial or ethnic backgrounds (1%).
Measures
RSA
Baseline RSA and RSA reactivity were measured at 3, 4, 5, and 6 years. RSA was derived from the R-R time series collected from digitized electrocardiogram (ECG) recordings using the Porges algorithm from MXEdit (Delta-Biometrics Inc., 1988–1993). ECGs were recorded via three electrodes placed on the child's chest and abdomen. The ECG signal was sampled at 1 kHz and stored on a computer for later scoring. Interbeat intervals were defined by detection of R-waves to the nearest millisecond.
Postprocessing of the data took place off-line by using a series of automated algorithms. R-R intervals outside of expected values were identified. Missed or spurious R-waves were flagged and corrected by linear interpolation. A 21-point moving polynomial was then applied to remove low frequency trends in the heart rate signal. Next, a bandpass filter extracted the variance in heart period within the frequency band of spontaneous respiration in young children (0.24–1.04 Hz). This process removes periodicities in the ECG signal that are outside the frequency range of the respiratory cycle. The resulting measure of RSA is in the frequency range of respiration. RSA was computed as the natural logarithm of heart period variance in milliseconds squared [ln(ms)2]. This method was described initially by Porges (1985) and is one of several acceptable approaches for calculating RSA (Berntson et al., 1997). RSA data were calculated in 30-s overlapping windows and then averaged within each episode (baseline and attention task). The RSA data for an individual was used as long as there was a 30-s segment, with less than 20% of segments identified with artifact (Jennings et al., 1981), which is the shortest duration recommended when calculating RSA with children. Thirty-second epochs are frequently sampled in studies of young children (Blandon et al., 2010; Buss, Goldsmith, & Davidson, 2005; Huffman, 1998; Moore & Calkins, 2004). In addition, small amounts of artifact can be expected to have a minimal effect on measures of heart rate variability such as RSA (Berntson, Cacioppo, & Quigley, 1993).
Baseline RSA was assessed while the children were waiting for a mastery motivation procedure (described below) to begin. Because RSA can be activated by psychomotor activity (Bazhenova & Porges, 1997), like others (Obradovic et al., 2010), we assessed baseline RSA during a nonchallenge “control” task that paralleled the motor demands of our challenge task. Specifically, children played with a toy alone or with an experimenter for an average of 164.8 s (range = 135.6–199.3 s) while sitting at a table. Although this baseline required some attention, which may evoke vagal withdrawal (Suess, Porges, & Plude, 1994), the toy with which the child played was simple, and no task demands were placed on the child during this time. Our estimates of baseline RSA are similar (within 1 SD) to other studies of young children of similar ages (Alkon et al., 2003; Buss et al., 2005; Calkins et al., 2007; Calkins & Keane, 2004; Doussard-Roosevelt, Montgomery, & Porges, 2003), who have also calculated RSA based on the Porges technique. Furthermore, the sample as a whole had RSA levels that decreased from this baseline to the attention demanding task at each age assessed (Table 1), indicating that our baseline measure was perceived as less stressful than the attention-demanding task.
Table 1. Means and standard deviations for RSA and neurobehavioral disinhibition over time.
| Age | M | SD | Data Present | M | SD | Data Present |
|---|---|---|---|---|---|---|
|
| ||||||
| Baseline RSA | RSA Reactivity | |||||
| 3 years | 5.64 | 1.29 | 53.4% | 0.60 | 0.56 | 51.6% |
| 4 years | 5.78 | 1.26 | 51.6% | 0.29 | 0.55 | 50.6% |
| 5 years | 6.06 | 1.23 | 48.1% | 0.27 | 0.55 | 47.6% |
| 6 years | 6.27 | 1.23 | 51.9% | 0.57 | 0.58 | 51.4% |
|
| ||||||
| Behavioral Dysregulation | Executive Dsyfunction | |||||
|
| ||||||
| Age 8/9 | 0.24 | 0.12 | 77.4% | 0.48 | 0.10 | 68.4% |
| Age 11 | 0.23 | 0.13 | 69.8% | 0.40 | 0.12 | 67.6% |
| Age 13/14 | 0.24 | 0.13 | 71.0% | 0.33 | 0.12 | 66.4% |
Note: RSA, respiratory sinus arrhythmia. Neurobehavioral disinhibition indicators (behavioral dysregulation and executive function difficulties) were rescaled on a continuous 0–1 metric and averaged to compute the behavioral dysregulation and executive dysfunction constructs.
RSA reactivity was assessed in response to a mastery motivation procedure (Dwek, 1991). The attention-demanding task comprised the first 3 min of the procedure. Children transitioned from supportive play with an experimenter to play with a moderately challenging toy just above the developmental level of the child without the aid of the experimenter or caregiver, though the experimenter was present during the task. Toys included a pathfinder (3 years), tinker toys (4 and 5 years), and a puzzle (6 years). Performance during mastery motivation tasks is positively related to emotion regulation (Heckhausen & Dweck, 1998); therefore, it was expected that this challenge should also tax emotion systems. RSA reactivity was calculated using a difference score (RSAbaseline – RSAtask). Positive values reflect greater RSA reactivity (i.e. greater decrease of RSA). Our estimates of RSA reactivity are similar (within 1 SD) to other studies of young children of similar ages using attention-demanding tasks and the Porges technique (Alkon et al., 2003; Buss et al., 2005; Calkins et al., 2007; Calkins & Keane, 2004).
ND
Two longitudinal construct scores were employed to assess growth in ND over three assessment periods during early adolescence using a strategy previously employed in studies involving the same sample (Fisher et al., 2011; Lester et al., 2012). The construct scores for behavioral dysregulation and executive dysfunction were computed from multimethod, multiagent, validated, well-established measures. The ND construct has good predictive validity, particularly its ability to predict substance-use onset, and good construct, discriminative, and concurrent validity, as well as good test–retest and internal reliability (Mezzich et al., 2007).
The behavioral dysregulation construct was a composite score of six measures of internalizing and externalizing problems: (a) problem behaviors reported by caregivers on the Child Behavior Checklist (Achenbach, 1992) using the standardized T scores for total problem behaviors at ages 9, 11, and 13 (we used T scores rather than raw scores because we were interested in comparing children's behavior relative to same-aged peers and normed by sex; in contrast, raw scores cannot be used to compare children's behavior against population norms of other children of the same age and sex, and the use of Child Behavior Checklist T scores is therefore common in longitudinal research in which trajectories of symptoms are assessed; e.g., see Milan & Pinderhughes, 2006); (b) ODD, (c) conduct disorder, (d) ADHD, (e) and major depression symptom counts reported by the parent from the Diagnostic Interview Schedule for Children—IV (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) at ages 8, 11, and 14; and (f) delinquency summary scores for the number of self-reported crimes against people and acts of general delinquency and school delinquency from the Things That You Have Done measure (Elliott, Huizinga, & Ageton, 1985; Ingoldsby, Kohl, McMahon, Lengua, & Group, 2006) at ages 9, 11, and 13. This measure is commonly used as an outcome variable in studies examining predictors of delinquent behavior (Bierman et al., 2004; Kaplow, Curran, & Dodge, 2002; Lamis, Malone, Lansford, & Lochman, 2012). Because the Diagnostic Interview Schedule for Children—IV was administered at years 8 and 14, we computed construct scores and have labeled the assessment periods as years 8/9, 11, and 13/14 throughout the text.
To evaluate comparable means over time, the composite growth score necessitates rescaling the original range of indicators to a common metric ranging from 0 to 1 as a continuous level scale. The composite is computed as the average of the three indicators. Cronbach a values were 0.73, 0.80, and 0.80, respectively, over time for the composite score of behavioral dysregulation. Using principal components factor analyses, we obtained a single-factor solution at each time point: eigenvalues of 2.98, 3.27, and 3.25, respectively, explained over 50% of the variance.
Executive dysfunction was measured with two computerized tests from the Cambridge Neuropsychological Test Automated Batteries (Luciana, 2003) at ages 9, 11, and 13. There is variability in the indicators researchers use to measure executive dysfunction as a component of ND. We chose tasks that assess spatial working memory, thinking time, and planning, all of which have been shown to be related to brain areas related to deficiencies among children exposed prenatally to drugs (Sheinkopf et al., 2009). The spatial working-memory task is self-ordered and requires the respondent to find a “token” in an array of colored boxes; we measured the total number of errors on the task. The Stockings of Cambridge task involves spatial planning, and the respondents must use “balls” in one display to copy the pattern shown in another display. Thinking time includes two trials measuring the time to select the initial stimulus. Shorter times have been related to impulsivity. We measured the total number of correct solutions in the minimal number of moves (reverse scored to indicate executive dysfunction). The composite growth score was the average of the two indicators rescaled to 0–1.
Key predictors
Prenatal substance exposure was measured as a summative index ranging from 0 to 5 for mother-reported (or gas chromatography–mass spectrometry confirmation of presumptive positive meconium screens for cocaine or opiate metabolites) use of cocaine, opiates, marijuana, alcohol, and tobacco during pregnancy. Maternal report/meconium screen of drug use (1 = yes, 0 = no) prenatally was computed. One point was assigned for each substance used. Dichotomous measures are frequently used in testing prenatal substance exposure effects (Fisher et al., 2011; Smith, Johnson, Pears, Fisher, & DeGarmo, 2007).
Early adversity was a summative risk index from birth to the age 3 assessments and included nine risk factors. Each risk factor was either a continuous scale or a count score and was dichotomized to create an overall risk index (0 = no/none, 1 = yes/one or more): (a) annual assessments of postnatal substance use of cocaine, opiates, tobacco, alcohol, or marijuana up to the Year 3 assessment; (b) chronic poverty status calculated as income below $10,000 over annual visits; (c) low social status scored from the Hollingshead Index of Social Position (Hollingshead, 1975) using education and occupation averaged over annual visits and scored as 1 SD or more below the mean; (d) primary caretaker changes; (e) sexual or physical abuse of the child as reported by caregivers; caregiver depression of 1 SD or greater above the mean for averaged depressive symptoms on the caregiver reported Beck Depression Inventory (Beck, Steer, & Brown, 1996); caretaker psychological distress of 1 SD or greater above the mean for averaged psychological symptoms above clinical cutoff on the Brief Symptom Inventory (Derogatis & Coons, 1993); (h) poor quality home environment of 1 SD or more below the mean on the Home Observation Measurement of the Environment (Caldwell & Bradley, 1984); and (i) any history of Child Protective Services Involvement assessed annually until the Year 3 assessment.
Missing data
Participants from the current study come from the sample used in Fisher et al. (2011), which included 1,073 MLS families in which the mothers had prenatal substance exposure scores and the youths had outcome data by the adolescent follow-up period. The MLS study originally enrolled 1,388 mothers with prenatal substance exposure scores. By the age 8/9 assessment, 81% of mothers had data on the youths enrolled in the study. Attrition analyses are described in detail in Fisher et al (2011). In brief, there were no differences on prenatal substance exposure when comparing mothers with youth data at follow-up and those without. Significant differences were observed for early adversity, with mothers and youths in follow-up exhibiting more risk compared to mothers whose children were lost to follow-up (M = 1.80, SD = 1.14, and M = 1.56, SD = 1.07, respectively, p < .01). There were no significant differences in prenatal substance exposure or early adversity between children with and without baseline RSA and RSA reactivity data within each age (all p > .14). Children with missing RSA data at 3 and 4 years had significantly higher behavior dysregulation and executive dysfunction scores at age 8/9 compared to children without missing RSA data at 3 and 4 years (ps < .02). Children with missing RSA data at 4 years also had less growth in behavior dysregulation (b = –0.24, p= .02). There were no other differences in ND (assessed via the behavior dysregulation and executive dysfunction growth factors) between children with and without baseline RSA and RSA reactivity data within each age (all ps > .19).
Analytic strategy
We employed structural equation modeling (SEM) to understand whether prenatal substance exposure and early adversity were related to the level and change over time in RSA and ND. Within this SEM framework, we used latent variable growth modeling to test the hypothesis that change in RSA is related to change in ND. Change in RSA and change in ND were characterized by scale-specific intercepts and slopes that were allowed to randomly vary across people.
Within-person variation in RSA and ND over time was modeled with individual-specific growth parameters (i.e., intercept, linear slope, and, when appropriate, quadratic slope). The two components that comprise ND, behavior dysregulation and executive dysfunction, were modeled separately. We tested two overarching models. In the first, latent growth curves were used to test a series of models examining the level and shape of children's baseline RSA from 3 to 6 years of age and ND (behavior dysregulation and executive dysfunction modeled separately) from ages 8/9 to 13/14. The four chronometric time weights for baseline RSA were specified at 0, 1, 2, and 3. In the second, we examined the level and shape of children's RSA reactivity from 3 to 6 years and ND (behavior dysregulation and executive dysfunction modeled separately) from ages 8/9 to 13/14. RSA reactivity was therefore modeled as a developmental process using a flexible approach to the structure of the SEM model. We specified the four chronometric time weights for the RSA reactivity linear slope factor at 0, 1, 2, and 3, and the quadratic slope as 0, 1, 4, and 9. We specified three chronometric time weights for the ND slope factor at 0, 1, and 2. This model allowed us to test the hypothesis that growth in RSA predicts growth in ND.
We used an SEM approach to test the interaction between growth in RSA and prenatal substance exposure/early adversity on growth in ND (Klein & Moosbrugger, 2000). SEM uses maximum likelihood estimation of model parameters, and when latent variable interactions are included in the model, it does not yield chi-square and related model fit statistics because means, variances, and covariances are not sufficient for model estimation. Instead, nested models were compared using the sample-size adjusted Bayesian information criterion (Sclove, 1987) and the Akaike information criterion (AIC; Akaike, 1987) to determine whether the interaction model resulted in better model fit compared to the main effects model. Lower sample-size adjusted Bayesian information criterion and AIC values indicated better model fit. All analyses were conducted using Mplus 5.1 (Muthén & Muthén, 2007).
Results
Preliminary analyses
The mean of the prenatal substance exposure index was 1.89 substances (SD = 1.38, range = 0–5). Forty-three percent of the sample was cocaine exposed, 8.3% opiate exposed, 58.5% alcohol exposed, 53.0% tobacco exposed, and 23.0% marijuana exposed. The mean number of early adversity factors was 2.35 (SD = 1.43, range = 0–8). As expected, there was a steady increase in baseline RSA from 3 to 6 years (see Table 1). RSA reactivity showed a curvilinear trend, with greater RSA reactivity at 3 years, decreasing RSA reactivity at 4 and 5 years, and increasing RSA reactivity again at 6 years. The mean composite growth construct score for behavioral dysregulation was largely stable over time (see Table 1). The mean composite score for executive function difficulties decreased over time.
Correlations
Correlations between baseline RSA, RSA reactivity, prenatal substance exposure, early adversity, behavioral dysregulation, and executive dysfunction are presented in Table 2. The intercorrelations between baseline RSA at 3, 4, 5, and 6 years were positively and strongly correlated. Intercorrelations among RSA reactivity measures were less strong, though also positive. Greater exposure to early adversity, and less exposure to substances prenatally, was related to less RSA reactivity at 3 years, but greater exposure to early adversity and drugs prenatally was associated with greater RSA reactivity at 6 years. Prenatal substance exposure was also significantly and positively associated with early adversity. Greater levels of behavioral dysregulation at all ages were associated with greater levels of prenatal substance exposure and early adversity, whereas greater levels of executive function difficulties were only significantly associated with greater levels of early adversity. Behavioral dysregulation and executive function difficulties were positively and moderately correlated (rs = .11–.26, ps < .001). In addition, behavioral dysregulation constructs at all ages were positively and strongly correlated (rs =.49–.62), as were the executive function difficulties constructs (rs = .44–.59).
Table 2. Correlations among study measures.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. RSA 36 months | |||||||||||||||
| 2. RSA 48 months | 49*** | — | |||||||||||||
| 3. RSA 60 months | 43*** | 46*** | — | ||||||||||||
| 4. RSA 72 months | 51 *** | 49*** | 49*** | — | |||||||||||
| 5. RSA-R 36 months | .26*** | .04 | −.03 | 17*** | — | ||||||||||
| 6. RSA-R 48 months | .004 | 34*** | .05 | .08 | .07 | — | |||||||||
| 7. RSA-R 60 months | −.01 | .06 | 27*** | 11** | .04 | 19*** | — | ||||||||
| 8. RSA-R 72 months | .004 | .01 | .09 | 23*** | .13** | .11* | 25*** | — | |||||||
| 9. Early adversity | −.003 | −.004 | .08* | 11** | −.09** | −.02 | .08* | .10** | — | ||||||
| 10. Prenatal substance exposure | .08* | .08* | .09* | 13*** | .09* | −.01 | .04 | .08* | 40*** | — | |||||
| 11. BD age 8/9 | −.03 | .01 | −.09* | .04 | −.08 | .01 | .03 | −.02 | 22*** | 11*** | — | ||||
| 12. BD age 11 | .03 | .05 | −.02 | .02 | −.01 | −.02 | .06 | −.04 | 25*** | .16*** | .58*** | — | |||
| 13. BD age 13/14 | −.02 | .05 | .05 | −.04 | −.05 | .05 | .05 | −.07 | 24*** | 20*** | 49*** | .62*** | — | ||
| 14. EF age 8/9 | −.03 | <.001 | .03 | .06 | −.04 | −.01 | −.07 | −.04 | 12*** | .04 | 17*** | 11*** | 11** | — | |
| 15. EFage 11 | .002 | 11** | .05 | .13** | −.09* | .02 | −.04 | −.03 | 15*** | .06 | .26*** | 19*** | 20*** | 49*** | — |
| 16. EF age 13/14 | −.02 | .06 | −.04 | .06 | −.08 | .06 | −.02 | −.11** | 12*** | .05 | 25*** | 19*** | 20*** | 44*** | 59*** |
Note: RSA, baseline respiratory sinus arrhythmia; RSA-R, RSA reactivity; BD, behavioral dysregulation; EF, executive dysfunction. Higher levels of RSA-R reflect greater RSA reactivity.
p < .05.
p < .01.
p < .001.
Unconditional growth models
Baseline RSA
Models were tested examining the level and shape of children's RSA trajectories during the baseline episode. Individual, within-person variation in RSA over time was allowed to vary across persons. On average, children showed a significant linear increase in baseline RSA over time. Children's baseline RSA at 3 years was 5.63 ln(ms)2, and the average rate of change in baseline RSA was 0.19 ln(ms)2. Significant variability was found for children's intercepts (σ2 = 0.79, p < .001), but not slopes (σ2 = 0.003, p = .86). This suggests that the initial level for baseline RSA varied across children, but the rate of change was relatively constant. The model fit the data well, χ2 (4) = 4.40, p = .35; comparative fit index (CFI; Bentler, 1990) = 1.00, root mean square error of approximation (RMSEA; Browne & Cudeck, 1993) = 0.01.
RSA reactivity
Identical models also tested RSA reactivity in response to the attention-demanding task. A model that included a curvilinear growth term (quadratic) provided excellent fit to the data, χ2 (4) = 4.45, p = .35; CFI = 0.99, RMSEA = 0.01 (Bentler, 1990; Browne & Cudeck, 1993), with reactivity highest at 3 years, decreasing at 4 and 5 years, and then increasing again at 6 years. Children's average linear slope was decreasing, suggesting that children were becoming less reactive over time (Mlinear slope = −1.24, p < .001), from an intercept of 2.12 ln(ms)2 at age 3 years. Significant variability in these parameters demonstrated that these patterns differed across children ( , p < .001; , p = .03). Children, on average, also exhibited a significant quadratic trend representing the decreases at ages 4 and 5 and the increase at age 6 (Mquadratic = 0.15, p < .001) with significant variability suggesting differences across children in this pattern over time ( , p = .05).
ND
Details regarding the unconditional model of ND can be found in Fisher et al (2011). In brief, there were significant individual differences in the trajectories of adolescent behavioral dysregulation and executive function difficulties. There was nonsignificant mean growth in behavioral dysregulation, whereas executive function difficulties decreased over time.
Effects of prenatal substance exposure and early adversity on growth in baseline RSA and ND
We next entered the main effects of prenatal substance exposure and early adversity on growth in baseline RSA on the behavioral dysregulation and executive dysfunction components of ND. Child sex was entered as a covariate in all models. The factor variance for the baseline RSA slope was fixed at 0 owing to its very low and nonsignificant value. We therefore did not include any predictors of growth in baseline RSA nor was growth in baseline RSA included as a predictor of behavioral dysregulation or executive dysfunction. This constraint did not affect model fit and improved the estimation of the overall model.
The main effect model for behavioral dysregulation showed acceptable fit (CFI = 0.98, RMSEA = 0.03), χ2 (33) = 70.98, p < .001. The findings indicate that greater prenatal substance exposure was associated with greater baseline RSA at age 3 (b = 0.14, p < .001) and greater increases in behavioral dysregulation over time (b = 0.15, p = .01). Greater levels of early adversity were related to higher initial levels of behavioral dyregulation at age 8/9 (b = 0.27, p < .001). Males had greater levels of behavioral dysregulation at age 8/9 than did females (b = −0.15, p < .001). There were no significant effects of RSA on initial status or growth in behavioral dysregulation.
The main effect model for the executive dysfunction outcome also demonstrated acceptable fit (CFI = 0.98, RMSEA = 0.02), χ2 (33) = 54.37, p = .01. Greater levels of prenatal substance exposure were related to greater baseline RSA at 3 years (b = 0.14, p < .001). There was only one significant association between the substantive covariates and the executive function difficulties construct. Greater levels of early adversity were associated with greater executive function difficulties at age 8/9 (b = 0.18, p < .001). There were no significant effects of RSA on initial levels or growth in executive dysfunction.
We then examined interactions between cumulative substance and baseline RSA at 3 years on initial status and growth in behavioral dysregulation, and the interaction between early adversity and baseline RSA at 3 years on initial status and growth in behavioral dysregulation (in separate models). No significant interaction effects emerged. We also examined these interactions on initial status and growth in executive dysfunction. As with behavioral dysregulation, there were no significant interaction effects.
Effects of prenatal substance exposure and early adversity on growth in RSA reactivity and ND
We repeated the above analyses with RSA reactivity, prenatal substance exposure, and early adversity as predictors of growth in the behavioral dysregulation and executive dysfunction components of ND. The main effect model for behavioral dysregulation showed acceptable fit (CFI = 0.98, RMSEA = 0.03), χ2 (20) = 40.28, p = .05. Greater exposure to early adversity was related to less RSA reactivity at 3 years (b = −0.32, p < .001), increased linear growth in RSA reactivity from 3 to 6 years (b = 0.29, p = .01), but not quadratic growth (b = −18, p = .10). In contrast, greater prenatal substance exposure was associated with greater RSA reactivity at 3 years (b = 0.30, p < .001), less linear growth in RSA reactivity (b = −0.27, p = .01), and greater quadratic growth (e.g., greater accelerations) of RSA reactivity from 3 to 6 years (b = 0.25, p = .03). Higher drug exposure was associated with less RSA reactivity at 4 and 5 years, followed by a steeper increase in RSA reactivity at age 6. Males exhibited more behavioral dysregulation at age 8/9 (b = −0.16, p < .001). Higher levels of early adversity were associated with greater behavioral dysregulation at age 8/9 (b = 0.24, p = .002). There were no main effects of RSA reactivity on initial levels or growth in behavioral dysregulation.
The main effect model for executive dysfunction showed good fit (CFI = 0.99, RMSEA = 0.02), χ2 (20) = 27.22, p > .05. Greater exposure to early adversity was related to less RSA reactivity at 3 years (b = −0.32, p < .001), increased linear growth in RSA reactivity from 3 to 6 years (b = 0.28, p = .01), but not quadratic growth (b = −0.18, p = .09). In contrast, greater prenatal substance exposure was associated with greater RSA reactivity at 3 years (b = 0.30, p < .001), less linear growth in RSA reactivity (b = −0.26, p = .01), and greater quadratic growth (e.g., greater accelerations) of RSA reactivity from 3 to 6 years, b = 0.24, p = .03. Higher drug exposure was associated with less RSA reactivity at 4 and 5 years followed by a steeper increase in RSA reactivity at age 6. There was only one significant association between the substantive covariates and the executive function difficulties construct. Greater levels of early adversity were associated with greater executive function difficulties at age 8/9 (b = 0.18, p = .02).
In separate models, we then examined the interaction between growth in RSA reactivity and prenatal substance exposure and early adversity on initial status and growth in behavioral dysregulation. There were no significant interactions between prenatal substance exposure and linear growth, or prenatal substance exposure and quadratic growth in RSA reactivity, on behavioral dysregulation intercept or linear slope. We next examined interactions between early adversity and linear and quadratic growth in RSA reactivity on initial status and growth in behavioral dysregulation. There was a significant interaction between early adversity and quadratic growth in RSA reactivity (but not with initial status or linear growth; see Figure 1). The inclusion of this interaction resulted in a significantly better model fit (Table 3). We probed this interaction by plotting RSA reactivity scores one standard deviation above and below the mean (Figure 2). The effect of early adversity on growth in behavioral dysregulation depended on quadratic growth in RSA reactivity. Children with decelerations in RSA reactivity exhibited growth in behavioral dysregulation regardless of whether they were exposed to early adversity. Children who exhibited accelerations in RSA reactivity, however, showed increases in behavioral dysregulation, but only if they were also raised in environments of high early life adversity. Children who exhibited accelerations in RSA reactivity and who were raised in environments of less early adversity exhibited no significant growth in behavioral dysregulation. We calculated the effect size as the proportion of explained variance using the following formula (Feingold, 2009):
Figure 1.
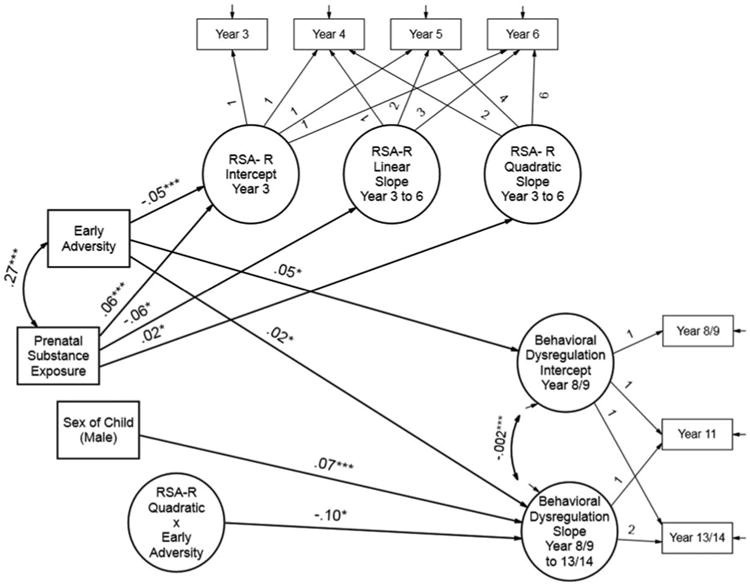
The effects of prenatal substance exposure, early adversity, growth in respiratory sinus arrhythmia (RSA) reactivity, and their interaction on growth in behavioral dysregulation across childhood and adolescence. Paths are beta coefficients. All associations between covariates and growth factors were modeled. We only include the significant pathways for ease of presentation. RSA-R, RSA reactivity; BD, behavioral dysregulation; EA, early adversity. *p < .05, **p < .001.
Table 3. Model fit indices for latent factor main and interaction effects.
| RSA-R | ||
|---|---|---|
|
| ||
| Model | SSABIC | AIC |
| Main effect of behavioral dysregulation | 9577.36 | 9497.09 |
| Main and interaction effects: EA×RSA-R | 9094.38 | 9014.35 |
Note: Only the main and interaction effects as predictors of growth in behavioral dysregulation are reported. RSA-R, respiratory sinus arrhythmia reactivity; SSABIC, sample size adjusted Bayesian information criterion; AIC, Akaike information criterion; EA, early adversity.
Figure 2.
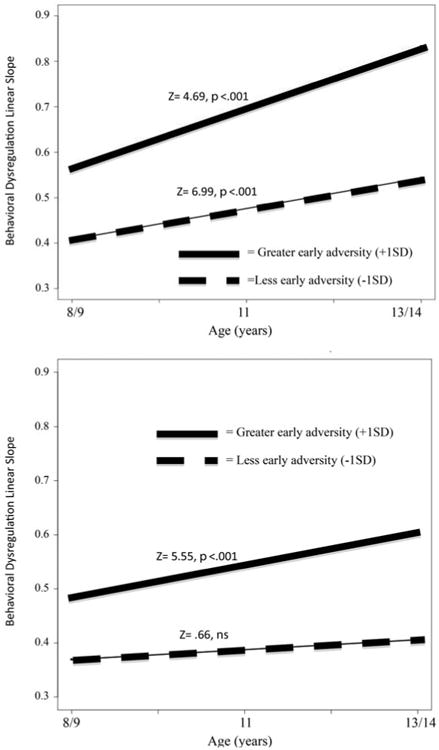
The interaction of change in respiratory sinus arrhythmia (RSA) reactivity and early adversity on change in behavioral dysregulation (a component of neurobehavioral disinhibition) across childhood and adolescence. The top panel represents the effect of early adversity on change in behavioral dysregulation for children with the decelerations in RSA reactivity (1 SD below the mean for quadratic growth in RSA reactivity). The bottom panel represents the effect of early adversity on change in behavioral dysregualtion for children with accelerations in RSA reactivity (1 SD above the mean for quadratic growth in RSA reactivity). Simple slopes of early adversity were modeled at 1 SD above and below the mean for early adversity.
The effect size (R2) was .40, indicating that the interaction explained approximately 40% of the variance in growth in behavior dysregulation.
Next, we examined whether there were interaction effects on executive function difficulties. The first model included the interaction between prenatal substance exposure and change in RSA reactivity on initial status and change in executive function difficulties. The second included the interaction between early adversity and change in RSA reactivity on initial status and change in executive function difficulties. Neither of the interaction effects was significant.
Discussion
The overarching goal of this study was to examine whether a biological marker of emotion regulation would aid in the identification of children who are most susceptible to the development of ND. We also added to the current literature by examining how interactions across environmental and physiological levels of analysis contribute to the development of ND. RSA reactivity moderated the relation between early adversity and trajectories of behavior dysregulation, a component of ND, suggesting that one pathway to the development of behavior dysregulation involves exposure to early adversity and accelerated growth in RSA reactivity across early childhood. In addition, we added to the ND literature by assessing how RSA growth trajectories contribute to growth in ND components. In our main effects models, we found that increases in prenatal substance exposure were associated with greater baseline RSA and RSA reactivity at age 3, linear growth in behavioral dysregulation, and quadratic growth in RSA reactivity that reflected a more rapid increase in RSA reactivity at 5 and 6 years compared with children with lower levels of prenatal substance exposure. Greater exposure to early adversity was related to decreased RSA reactivity at age 3, linear increases in RSA reactivity from ages 3 to 6 years, and increased behavioral dysregulation and executive function difficulties at age 8/9. Below we discuss additional contributions of this study.
Greater prenatal substance exposure and less early adversity were related to greater RSA reactivity at 3 years and less linear growth in RSA reactivity from 3 to 6 years. In typically developing populations, moderate withdrawal of RSA is considered functional (Beauchaine, 2001). That children with prenatal substance exposure exhibited less linear growth in RSA reactivity suggests the possibility that these children may be developing a profile of reduced autonomic functioning that is typically seen among children with externalizing disorders (Beauchaine, 2001; Crowell et al., 2006). Compared to children with less prenatal substance exposure, another possibility is that this pattern of less RSA reactivity over time reflects difficulties prenatally exposed children may have with exhibiting the expected withdrawal of RSA in response to an acute stressor, which may be a risk factor for the development of problem behavior (Calkins & Dedmon, 2000; Gentzler, Santucci, Kovacs, & Fox, 2009; Porges, Doussard-Roosevelt, Portales, & Greenspan, 1996).
It was surprising to us that the effects of prenatal substance exposure and early adversity on growth in RSA reactivity manifested in opposite ways. When examining correlations, these prenatal substance exposure and early adversity exhibit opposite effects on RSA reactivity at age 3, but by age 6 the direction of effect is the same. These findings highlight the importance of examining RSA across multiple developmental periods, as patterns change with development. With greater exposure to adverse experiences over time, there may be a reorganization that occurs in the parasympathetic system. These results support the hypothesis that the effect of early adversity may be latent owing to its impact on specific areas of the brain that are not online until childhood when the child must organize resources to respond to more complex demands (Lester et al., 2002; Shonkoff, Boyce, & McEwen, 2009). As children develop, they face more demands at home, school, and with peers, and it is important that they learn to organize neurobiological resources in order to achieve competence in multiple settings (Lester, LaGasse, & Seifer, 1998).
It is interesting that there were no main effects of RSA on the ND components, though RSA reactivity interacted with early adversity to predict individual differences in growth of behavior dysregulation. RSA reactivity may have stronger links with emotion regulation compared to baseline RSA, because RSA reactivity is related to the organism's ability to engage and disengage with the environment (Beauchaine, 2001; Doussard-Roosevelt et al., 2003). Therefore, it is less surprising that RSA reactivity, compared to baseline RSA, would have a stronger relation with behavior dysregulation because emotion dysregulation is one component of ND. Furthermore, although there was significant variability in baseline RSA at age 3, the lack of variability of growth in baseline RSA precluded our ability to estimate whether it was a predictor of individual differences in the ND components.
It was only through examining growth in RSA reactivity that the relation between early adversity and behavior dysregulation became clear. Decelerated growth in RSA reactivity was related to increases in behavior dysregulation, regardless of the child's exposure to early adversity. This finding highlights the importance of understanding how rates of physiological maturation over time may be associated with increased risk for the development of behavioral dysregulation. Although a faster maturation of the stress response system is thought to be impacted by processes of allostatic load (McEwen, 1998), it appears as though decelerations could also be problematic. Decelerations in RSA reactivity manifest as a flat, or blunted, response from age 3 to age 6. The correlates of this “blunted” RSA response may be similar to that of the neuroendocrine system. A blunted cortisol response to stress is associated with greater exposure to early adversity (Fisher, Stoolmiller, Gunnar, & Burraston, 2007) and prenatal substance exposure (Lester et al., 2010), presumably because of wear and tear on the neuroendocrine system. This is the first study that we know of suggesting that a blunted RSA response may also be problematic. In addition to the effects of early adversity and prenatal substance exposure on this pattern of responding, there may be as yet unmeasured environmental or epigenetic influences. By epigenetic we mean the inheritance of information based on gene expression control rather than gene sequence (Lester et al., 2012). For instance, the theory of biological sensitivity to context (Boyce & Ellis, 2005) suggests that it is through prenatal programming that stress response systems are formed, with the fetus “learning” to upregulate a response to stress if the intrauterine environment forecasts a particularly positive or negative postnatal environment, as a way to adapt to this environment. Perhaps this blunted RSA response was adaptive earlier in life or even in utero. We may also have identified a group of children who are chronically physiologically underaroused and thus may be more sensation seeking or aggressive (Raine, Lencz, Bihrle, Lacasse, & Colletti, 2000).
Children who exhibited accelerated growth in RSA reactivity over time and who had greater exposure to early adversity exhibited increases in behavioral dysregulation. Perhaps the combination of accelerated growth in RSA reactivity and experiencing adversity early in life reflects a “double jeopardy” that places the child at increased risk for the development of behavioral dysregulation. The theory of biological sensitivity to context suggests that greater reactivity may allow the child to be more hypervigilant and aware of his/her surroundings, which may be an adaptive response to a chaotic or unpredictable environment. Because we only measured a negative environment in this study, we cannot also test whether accelerations in RSA reactivity are related to positive outcomes in supportive environments.
However, there were no significant associations with RSA and executive dysfunction. Previous reports measured RSA and executive functions concurrently or RSA measured at one point in time. No studies that we know of examined developmental trajectories of RSA in early childhood and executive dysfunction in middle childhood. RSA may not be as accurate a predictor of executive dysfunction compared to behavior dysregulation. RSA may be more strongly tied to emotion systems and emotion regulation than it is to cognitive control systems per se.
The results from this study raise interesting questions regarding the bottom-up and/or top-down processes involved in the development of ND (Lester et al., 2012). Altered executive control systems, thought to reflect a higher order cognitive process, may result in problems with emotion regulation (i.e., problems with inhibitory control and impulsivity) and subsequently individual differences in RSA, reflecting a top-down process in the development of ND. Children who exhibit more symptoms of ND exhibit greater activation in these frontal regions (McNamee et al., 2008), suggesting that more activation of these executive control systems is needed to negotiate changing environmental demands. In contrast, children with less control over their emotions (i.e., those who exhibit excessive RSA reactivity), may, through interactions over time with exposure to environmental adversity, develop problems with executive control systems (i.e., poor inhibitory control and planning), thereby impacting the development of ND, suggesting a bottom-up process might also be involved. Although we cannot infer direction of effect with these data, results from this study provide preliminary support for the hypothesis that accelerated growth in RSA reactivity in combination with exposure to early adversity is involved in the development of ND. Early adversity may affect frontal regions associated with emotion regulation (Kishiyama et al., 2009), thereby impacting individual differences in RSA reactivity and increasing the likelihood for the development of ND (e.g., a bottom-up process). These effects might also be bidirectional, with exposure to early adversity impacting frontal cortex inhibitory processes (Kishiyama et al., 2009), thereby compromising behavioral control of emotion and subsequently physiological systems of regulation (a “top-down”) process. Although we did not measure neurological control in this study, future prospective studies are needed to elucidate these potential mechanisms to vulnerability of ND through neurological pathways.
These results also raise important questions regarding the context in which RSA is assessed and how this context may or may not relate to the separate ND components of behavioral dysregulation and executive dysfunction. In some studies, RSA reactivity to emotionally evocative tasks was related to aspects of behavior dysregulation involving externalizing behavior (El-Sheikh, 2001; El-Sheikh, Harger, & Whitson, 2001), whereas in others only RSA reactivity to attention-demanding tasks were related to behavior dysregulation (Calkins & Keane, 2004; Hinnant & El-Sheikh, 2009). It appears as though stressors perceived as attention demanding may also tax emotion systems in addition to cognitive or attention systems, perhaps even more so than tasks that researchers judge to be emotionally evocative. In contrast, behavior dysregulation can be an amorphous and at times all-encompassing construct, and without measures of this dysregulation from multiple informants, we will have difficulty finding relevant physiological predictors or correlates of dysregulation. Although at this point the literature is equivocal, it is important in future work to validate paradigms researchers hypothesize as stressful and to incorporate multiple stressors that tax emotion, cognitive, and attention systems (see Alkon et al., 2003, as an example of such work).
An important limitation of the current study is our assessment of one measure of physiology. Multiple measures of biological processes should be used in future studies to test relevant developmental models (Granger & Kivlighan, 2003). In addition, although most of our physiological measures were evaluated before symptom assessments, we still cannot infer causality with these data. Future studies using a cross-lagged approach will be helpful in understanding whether a physiological process at one point in time influences behavior later in development. We also did not isolate the effects of a single substance, such as cocaine, on RSA, and instead used a summary score approach, which may be a more ecologically valid indicator of prenatal substance use (Mayet et al., 2008). We acknowledge that the mechanism of action of these drugs is different, and we cannot study the relative impact of one drug over another. Future studies could also examine prenatal substance exposure using a latent factor approach as a way to reduce measurement error. However, our interest was in polydrug exposure as used previously (Fisher et al., 2011) as a marker for cumulative intrauterine stress (Lester & Padbury, 2009), which is why we used a summary score approach. Another limitation includes our measurement of baseline RSA. We did not assess RSA while the child was at “rest,” but we instead chose to compare RSA activity during an attention-demanding task with RSA activity when a child was playing with a simple toy and experimental demands were minimal. Although our estimates of baseline RSA converge with other studies using the Porges method, we nonetheless note that our baseline measurement did not measure parasympathetic activity at rest. We also did not include a measure of movement as a covariate in our physiological analyses, which may have impacted heart rate and in turn RSA. In addition, we chose measures of executive dysfunction that have been shown to be related to brain areas related to deficiencies among children exposed prenatally to drugs (Sheinkopf et al., 2009); however, there may have been others (such as inhibitory control) that could have been assessed. Furthermore, although we have added breadth to our understanding of the development of ND, it came at the expense of depth. We are unable to ascertain, for instance, whether growth in RSA reactivity at earlier ages is a stronger contributor to ND than growth at later ages. Likewise, we do not know whether growth in RSA reactivity more strongly influences ND at a particular time point (for instance, during preschool) more so than at later ages. Microlevel approaches are needed if we are to understand when in development a child may be most at risk for a dysregualted physiological profile (Beauchaine, Neuhaus, et al., 2008). Nevertheless, this study has added specificity to our understanding of how Biology × Environment interactions contribute to disease risk.
In sum, we extended our understanding of how transactions between physiology and environmental context contribute to the development of ND. We used a multifaceted model taking into account the dynamic interactions that occur among physiological functioning, early adverse experiences, and prenatal substance exposure to predict the development of ND across preschool, childhood, and adolescence. This study builds on previous work by incorporating how RSA, early adversity, prenatal substance exposure, and their interactions predict the development of ND. The results from this study have illuminated some interesting pathways to the development of ND among a sample of children heterogeneous for exposure to substances prenatally and early adverse experiences. Longitudinal studies such as the one presented in this investigation are needed to elucidate transactional pathways leading to adverse outcomes. This Biology × Environment interaction is of critical importance to early interventionists because it suggests that the child most in need of intervention is one with greater RSA reactivity who is reared in a risky early environment. We hope this work has opened new avenues of research as well as clarified who might be most at risk for the development of a disinhibited profile. This information may then be used to add specificity and therefore cost-effectiveness to sorely needed preventative interventions for this group of underserved children.
Acknowledgments
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network and an interinstitute agreement with the National Institute on Drug Abuse (NIDA) through cooperative agreements U10-DA-024117-01 and U10-HD-21385 (to S.S.), I10-DA-024128-06 and U10-HD-2786 (to H.S.B.), U10-DA-024119-01 and U10-HD-27904 (to B.M.L.), and U10-DA-024118-01 and U10-HD-21397 (to C.R.B.); NICHD contract N01-HD-2-3159 (to B.M.L.); a National Research Service Award from the NIDA, F32DA032175 (to E.C.); and partial support from NIDA Grants P20 DA17952 and P50 DA035763 (to D.D.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDA, the Eunice Kennedy Shriver NICHD, or the National Institutes of Health. Support for the Maternal Lifestyle Study was provided by the National Institutes of Health through the NIDA and the Eunice Kennedy Shriver NICHD, with supplemental funding from the National Institute of Mental Health, the Administration on Children, Youth, and Families, and the Center for Substance Abuse and Treatment, US Department of Health and Human Services. We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study. In addition to those listed as authors, the following individuals and federal funding grants contributed to this study: Brown University, Warren Alpert Medical School Women & Infants Hospital of Rhode Island (U10 HD27904, N01 HD23159) to Cynthia Miller-Loncar, Jean Twomey, Laura Dietz, and Melissa Kupchak; NIDA to Vincent L. Smeriglio and Nicolette Borek; RTI International (U10 HD36790) to W. Kenneth Poole, Abhik Das, and Debra Fleischmann; University of Miami Holtz Children's Hospital (GCRC M01 RR16587, U10 HD21397) to Ann L. Graziotti, Tonya Barriere-Perez, Janine Closius, Diedre Gallop, Edgar Garcia, Susan Gauthier, Wendy Griffin, Elizabeth Jacque, Jennifer Lewis, Daniel A. Messinger, and Yamille Valdez; University of Tennessee (U10 HD42638) to Charlotte Bursi, Deloris Lee, and Lillie Hughey; and Wayne State University Hutzel Women's Hospital and Children's Hospital of Michigan (U10 HD21385) to Eunice Woldt, Jay Ann Nelson, Catherine Bartholomay, Lisa Sulkowski, and Nicole Walker.
References
- Achenbach TM. Manual for the Child Behavior Checklist/2–3 and 1992 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1992. [Google Scholar]
- Akaike H. Factor analysis and the AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- Alkon A, Goldstein LH, Smider N, Essex MJ, Kupfer DJ, Boyce WT. Developmental and contextual influences on autonomic reactivity in young children. Developmental Psychobiology. 2003;42:64–78. doi: 10.1002/dev.10082. [DOI] [PubMed] [Google Scholar]
- Bazhenova OV, Porges S. The integrative neurobiology of affiliation. Annals of the New York Academy of Science. 1997;807:469. doi: 10.1111/j.1749-6632.1997.tb51940.x. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP. Vagal tone, development, and Gray's motivational theory: Toward an integrated model of autonomic nervous system functioning in psychopathology. Development and Psychopathology. 2001;13:183–214. doi: 10.1017/s0954579401002012. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Gardner J, Hagen B. Comorbid depression and heart rate variability as predictors of aggressive and hyperactive symptom responsiveness during inpatient treatment of conduct-disordered, ADHD boys. Aggressive Behavior. 2000;26:425–441. doi: 10.1002/1098-2337(200011)26:6<425∷aid-ab2>3.0.co;2-i. [DOI] [Google Scholar]
- Beauchaine TP, Gatzeke-Kapp L, Mead HK. Polyvagal theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology. 2007;74:174–184. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Hinshaw SP, Pang KL. Comorbidity of attention-deficit/hyperactivity disorder and early-onset conduct disorder: Biological, environmental, and developmental mechanisms. Clinical Psychology: Science and Practice. 2010;17:327–336. doi: 10.1111/j.1468-2850.2010.01224.x. [DOI] [Google Scholar]
- Beauchaine TP, Hong J, Marsh P. Sex differences in autonomic correlates of conduct problems and aggression. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:788–796. doi: 10.1097/CHI.Ob013e318172ef4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Neuhaus E, Brenner SL, Gatzke-Kopp L. Ten good reasons to consider biological processes in prevention and intervention research. Development and Psychopathology. 2008;20:745–774. doi: 10.1017/S0954579408000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory—II. New York: Psychological Corporation; 1996. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:885–908. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berntson GG, Bigger JT, Jr, Eckberg DL, Grossman P, Kaufmann PG, Malik M, et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623–648. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]
- Berntson GG, Cacioppo JT, Quigley KS. Respiratory sinus arrhythmia: Autonomic origins, physiological mechanisms, and psychophysiological implications. Psychophysiology. 1993;30:183–196. doi: 10.1111/j.1469-8986.1993.tb01731.x. [DOI] [PubMed] [Google Scholar]
- Bierman KL, Coie JD, Dodge KA, Foster ME, Greenberg MT, Lochman JE, et al. The effects of the Fast Track program on serious problem outcomes at the end of elementary school. Journal of Clinical Child and Adolescent Psychology. 2004;33:650–661. doi: 10.1207/s15374424jccp3304_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair C. Behavioral inhibition and behavioral activation in young children: Relations with self-regulation and adaptation to preschool in children attending Head Start. Developmental Psychobiology. 2003;42:301–311. doi: 10.1002/dev.10103. [DOI] [PubMed] [Google Scholar]
- Blair C, Granger DA, Willoughby M, Mills-Koonce R, Cox M, Greenberg MT, et al. Salivary cortisol mediates effects of poverty and parenting on executive functions in early childhood. Child Development. 2011;82:1970–1984. doi: 10.1111/j.1467-8624.2011.01643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blandon AY, Calkins SD, Keane SP, O'Brien M. Contributions of child's physiology and maternal behavior to children's trajectories of temperamental reactivity. Developmental Psychology. 2010;46:1089–1102. doi: 10.1037/a0020678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce WT, Ellis BJ. Biological sensitivity to context: I. An evolutionary-developmental theory of the origins and functions of stress reactivity. Development and Psychopathology. 2005;17:271–301. doi: 10.1017/s0954579405050145. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods & Research. 1993;21:230–258. [Google Scholar]
- Buss KA, Goldsmith HH, Davidson RJ. Cardiac reactivity is associated with changes in negative emotion in 24-month-olds. Developmental Psychobiology. 2005;46:118–132. doi: 10.1002/dev.20048. [DOI] [PubMed] [Google Scholar]
- Caldwell BM, Bradley RH. Home observation for measurement of the environment. Little Rock, AR: University of Arkansas at Little Rock Press; 1984. [Google Scholar]
- Calkins SD, Dedmon SE. Physiological and behavioral regulation in two-year-old children with aggressive/destructive behavior problems. Journal of Abnormal Child Psychology. 2000;28:103–118. doi: 10.1023/a:1005112912906. [DOI] [PubMed] [Google Scholar]
- Calkins SD, Graziano PA, Keane SP. Cardiac vagal regulation differentiates among children at risk for behavior problems. Biological Psychology. 2007;74:144–153. doi: 10.1016/j.biopsycho.2006.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins SD, Keane SP. Cardiac vagal regulation across the preschool period: Stability, continuity, and implications for childhood adjustment. Developmental Psychobiology. 2004;45:101–112. doi: 10.1002/dev.20020. [DOI] [PubMed] [Google Scholar]
- Chapman K, Tarter RE, Kirisci L, Cornelius MD. Childhood neurobehavior disinhibition amplifies the risk of substance use disorder: Interaction of parental history and prenatal alcohol exposure. Journal of Developmental & Behavioral Pediatrics. 2007;28:219. doi: 10.1097/DBP.0b013e3180327907. [DOI] [PubMed] [Google Scholar]
- Clausen JM, Landsverk J, Ganger W, Chadwick D, Litrownik A. Mental health problems of children in foster care. Journal of Child and Family Studies. 1998;7:283–296. [Google Scholar]
- Crowell SE, Beauchaine TP, Gatzke-Kopp L, Sylvers P, Mead H, Chipman-Chacon J. Autonomic correlates of attention-deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. Journal of Abnormal Psychology. 2006;115:174–178. doi: 10.1037/0021-843X.115.1.174. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Coons HL. Self-report measures of stress. 2nd. New York: Free Press; 1993. [Google Scholar]
- DiPietro JA, Suess PE, Wheeler JS, Smouse PH, Newlin DB. Reactivity and regulation in cocaine-exposed neonates. Infant Behavior and Development. 1995;18:407–414. doi: 10.1016/0163-6383(95)90030-6. [DOI] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse and Neglect. 2004;28:771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Doussard-Roosevelt JA, Montgomery LA, Porges SW. Short-term stability of physiological measures in kindergarten children: Respiratory sinus arrhythmia, heart period, and cortisol. Developmental Psychobiology. 2003;43:230–242. doi: 10.1002/dev.10136. [DOI] [PubMed] [Google Scholar]
- Dwek CS. Self theories and goals: Their role in motivation, personality and development. In: Dienstbeir RA, editor. Nebraska symposium on motivation. Lincoln, NE: University of Nebraska Press; 1991. pp. 213–221. [PubMed] [Google Scholar]
- Eiden RD, Granger DA, Schuetze P, Veira Y. Child behavior problems among cocaine-exposed toddlers: Indirect and interactive effects. Development and Psychopathology. 2011;23:539–550. doi: 10.1017/S0954579411000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Beverly Hills, CA: Sage; 1985. [Google Scholar]
- El-Sheikh M. Parental drinking problems and children's adjustment: Vagal regulation and emotional reactivity as pathways and moderators of risk. Journal of Abnormal Psychology. 2001;110:499. doi: 10.1037//0021-843x.110.4.499. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Harger J, Whitson SM. Exposure to interparental conflict and children's adjustment and physical health: The moderating role of vagal tone. Child Development. 2001;72:1617–1636. doi: 10.1111/1467-8624.00369. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Hinnant JB. Marital conflict, respiratory sinus arrhythmia, and allostatic load: Interrelations and associations with the development of children's externalizing behavior. Development and Psychopathology. 2011;23:815–829. doi: 10.1017/S0954579411000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Pickens J, Fox NA, Nawrocki T, Gonzalez J. Vagal tone in infants of depressed mothers. Development and Psychopathology. 1995;7:227–231. doi: 10.1017/S0954579400006465. [DOI] [PubMed] [Google Scholar]
- Fisher PA, Lester BM, DeGarmo DS, Lagasse LL, Lin H, Shankaran S, et al. The combined effects of prenatal drug exposure and early adversity on neurobehavioral disinhibition in childhood and adolescence. Development and Psychopathology. 2011;23:777–788. doi: 10.1017/S0954579411000290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher PA, Stoolmiller M, Gunnar MR, Burraston BO. Effects of a therapeutic intervention for foster preschoolers on diurnal cortisol activity. Psychoneuroendocrinology. 2007;32:892–905. doi: 10.1016/j.psyneuen.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentzler AL, Santucci AK, Kovacs M, Fox NA. Respiratory sinus arrhythmia reactivity predicts emotion regulation and depressive symptoms in at-risk and control children. Biological Psychology. 2009;82:156–163. doi: 10.1016/j.biopsycho.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granger DA, Kivlighan KT. Integrating biological, behavioral, and social levels of analysis in early child development: Progress, problems, and prospects. Child Development. 2003;74:1058–1063. doi: 10.1111/1467-8624.00590. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Fisher PA. Early Experience, Stress, and Prevention Network: Bringing basic research on early experience and stress neurobiology to bear on preventive interventions for neglected and maltreated children. Development and Psychopathology. 2006;18:651–677. [PubMed] [Google Scholar]
- Habeych ME, Charles PJ, Sclabassi RJ, Kirisci L, Tarter RE. Direct and mediated associations between P300 amplitude in childhood and substance use disorders outcome in young adulthood. Biological Psychiatry. 2005;57:76–82. doi: 10.1016/j.biopsych.2004.09.028. [DOI] [PubMed] [Google Scholar]
- Hansen AL, Johnsen BH, Thayer JF. Vagal influence on working memory and attention. International Journal of Psychophysiology. 2003;48:263–274. doi: 10.1016/s0167-8760(03)00073-4. [DOI] [PubMed] [Google Scholar]
- Harden BJ. Safety and stability for foster children: A developmental perspective. Children, Families, and Foster Care. 2004;14:31–47. [PubMed] [Google Scholar]
- Heckhausen J, Dweck CS. Motivation and selfregulation across the life span. New York: Cambridge University Press; 1998. [Google Scholar]
- Heim C, Plotsky PM, Nemeroff CB. Importance of studying the contributions of early adverse experience to neurobiological findings in depresion. Neuropsychopharmacology. 2004;29:641–648. doi: 10.1038/sj.npp.1300397. [DOI] [PubMed] [Google Scholar]
- Hellemans KG, Sliwowska JH, Verma P, Weinberg J. Prenatal alcohol exposure: Fetal programming and later life vulnerability to stress, depression and anxiety disorders. Neuroscience & Biobehavioral Reviews. 2010;34:791–807. doi: 10.1016/j.neubiorev.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill AL, Degnan KA, Calkins SD, Keane SP. Profiles of externalizing behavior problems for boys and girls across preschool: The roles of emotion regulation and inattention. Developmental Psychology. 2006;42:913–928. doi: 10.1037/0012-1649.42.5.913. [DOI] [PubMed] [Google Scholar]
- Hinnant JB, El-Sheikh M. Children's externalizing and internalizing symptoms over time: The role of individual differences in patterns of RSA responding. Journal of Abnormal Child Psychology. 2009;37:1049–1061. doi: 10.1007/s10802-009-9341-1. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four-Factor Index of Social Status. New Haven, CT: Yale University Press; 1975. [Google Scholar]
- Huffman LC. Infant temperament and cardiac vagal tone: Assessments at twelve weeks of age. Child Development. 1998;69:624. [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: Findings from the Minnesota Twin Family Study. Development and Psychopathology. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, McGue M. Behavioral disinhibition and the development of early-onset addiction: Common and specific influences. Annual Review of Clinical Psychology. 2008;4:325–348. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Ingoldsby EM, Kohl GO, McMahon RJ, Lengua L, Group CPPR. Conduct problems, depressive symptomatology and their co-occurring presentation in childhood as predictors of adjustment in early adolescence. Journal of Abnormal Child Psychology. 2006;34:603–621. doi: 10.1007/s10802-006-9044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings JR, Berg WK, Hutcheson JS, Obrist P, Porges S, Turpin G. Committee report: Publication guidelines for heart rate studies in man. Psychophysiology. 1981;18:226–231. doi: 10.1111/j.1469-8986.1981.tb03023.x. [DOI] [PubMed] [Google Scholar]
- Kaplow JB, Curran PJ, Dodge KA. Child, parent, and peer predictors of early-onset substance use: A multisite longitudinal study. Journal of Abnormal Child Psychology. 2002;30:199–216. doi: 10.1023/a:1015183927979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller PS, El-Sheikh M. Salivary alpha-amylase as a longitudinal predictor of children's externalizing symptoms: Respiratory sinus arrhythmia as a moderator of effects. Psychoneuroendocrinology. 2009;34:633. doi: 10.1016/j.psyneuen.2008.12.016. [DOI] [PubMed] [Google Scholar]
- Kishiyama MM, Boyce WT, Jimenez AM, Perry LM, Knight RT. Socioeconomic disparities affect prefrontal function in children. Journal of Cognitive Neuroscience. 2009;21:1106–1115. doi: 10.1162/jocn.2009.21101. [DOI] [PubMed] [Google Scholar]
- Klein A, Moosbrugger H. Maximum likelihood estimation of latent interaction effects with the LMS method. Psychometrika. 2000;65:457–474. doi: 10.1007/bf02296338. [DOI] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, South SC. Externalizing disorders: Cluster 5 of the proposed meta-structure for DSM-V and ICD-11. Psychologial Medicine. 2009;39:2061–2070. doi: 10.1017/S0033291709990328. [DOI] [PubMed] [Google Scholar]
- Lamis DA, Malone PS, Lansford JE, Lochman JE. Maternal depressive symptoms as a predictor of alcohol use onset and heavy episodic drinking in youths. Unpublished manuscript. 2012 doi: 10.1037/a0028959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, LaGasse LL, Seifer R. Cocaine exposure and children: The meaning of subtle effects. Science. 1998;282:633–634. doi: 10.1126/science.282.5389.633. [DOI] [PubMed] [Google Scholar]
- Lester BM, Lagasse LL, Shankaran S, Bada HS, Bauer CR, Lin R, et al. Prenatal cocaine exposure related to cortisol stress reactivity in 11-year-old children. Journal of Pediatrics. 2010;157:288–295. doi: 10.1016/j.jpeds.2010.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, Lin H, Degarmo DS, Fisher PA, Lagasse LL, Levine TP, et al. Neurobehavioral disinhibition predicts initiation of substance use in children with prenatal cocaine exposure. Drug and Alcohol Dependence. 2012 doi: 10.1016/j.drugalcdep.2012.04.014. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, Marsit C, Conradt E, Bromer C, Padbury J. Behavioral epigenetics and the developmental origins of child mental health disorders. Journal of Developmental Origins of Health and Disease. 1:1. doi: 10.1017/S2040174412000426. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, Padbury JF. Third pathophysiology of prenatal cocaine exposure. Developmental Neuroscience. 2009;31:23–35. doi: 10.1159/000207491. [DOI] [PubMed] [Google Scholar]
- Lester BM, Tronick EZ, LaGasse L, Seifer R, Bauer CR, Shankaran S, et al. The maternal lifestyle study: Effects of substance exposure during pregnancyon neurodevelopmental outcome in 1-month-old infants. Pediatrics. 2002;110:1182–1192. doi: 10.1542/peds.110.6.1182. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO. Comorbidity between and within childhood externalizing and internalizing disorders: Reflections and directions. Journal of Abnormal Child Psychology. 2003;31:285–291. doi: 10.1023/a:1023229529866. [DOI] [PubMed] [Google Scholar]
- Luciana M. Practitioner review: Computerized assessment of neuropsychological function in children: Clinical and research applications of the Cambridge Neuropsychological Testing Automated Battery (CANTAB) Journal of Child Psychology and Psychiatry. 2003;44:649–663. doi: 10.1111/1469-7610.00152. [DOI] [PubMed] [Google Scholar]
- Lupien SJ, King S, Meaney MJ, McEwen BS. Can poverty get under your skin? Basal cortisol levels and cognitive function in children from low and high socioeconomic status. Development and Psychopathology. 2001;13:653–676. doi: 10.1017/s0954579401003133. [DOI] [PubMed] [Google Scholar]
- Marcovitch S, Leigh J, Calkins SD, Leerks EM, O'Brien M, Blankson AN. Moderate vagal withdrawal in 3.5-year-old children is associated with optimal performance on executive function tasks. Developmental Psychobiology. 2010;52:603–608. doi: 10.1002/dev.20462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayet S, Groshkova T, Morgan L, MacCormack T, Strang J. Drugs and pregnancy—Outcomes of women engaged with a specialist perinatal outreach addictions service. Drug and Alcohol Review. 2008;27:497–503. doi: 10.1080/09595230802245261. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McNamee RL, Dunfee KL, Luna B, Clark DB, Eddy WF, Tarter RE. Brain activation, response inhibition, and increased risk for substance use disorder. Alcohoism: Clinical and Experimental Research. 2008;32:405–413. doi: 10.1111/j.1530-0277.2007.00604.x. [DOI] [PubMed] [Google Scholar]
- Mehta SK, Finkelhor RS, Anderson RL, Harcar-Sevcik RA, Wasser TE, Bahler RC. Transient myocardial ischemia in infants prenatally exposed to cocaine. Journal of Pediatrics. 1993;122:945–949. doi: 10.1016/s0022-3476(09)90025-7. [DOI] [PubMed] [Google Scholar]
- Mezzich AC, Tarter RE, Feske U, Kirisci L, McNamee RL, Day B. Assessment of risk for substance use disorder consequent to consumption of illegal drugs: Psychometric validation of the neurobehavior disinhibition trait. Psychology of Addictive Behaviors. 2007;21:508. doi: 10.1037/0893-164X.21.4.508. [DOI] [PubMed] [Google Scholar]
- Milan S, Pinderhughes EE. Family instability and child maladjustment trajectories during elementary school. Journal of Abnormal Child Psychology. 2006;34:40–53. doi: 10.1007/s10802-005-9007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: Implications for the depressive disorders. Psychological Bulletin. 1991;110:406. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Moore GA, Calkins SD. Infants' vagal regulation in the stillface paradigm is related to dyadic coordination of mother–infant interaction. Developmental Psychology. 2004;40:1068. doi: 10.1037/0012-1649.40.6.1068. [DOI] [PubMed] [Google Scholar]
- Musser ED, Backs RW, Schmitt CF, Ablow JC, Measelle JR, Nigg JT. Emotion regulation via the autonomic nervous system in children with attention-deficit/hyperactivity disorder (ADHD) Journal of Abnormal Child Psychology. 2011;39:841–852. doi: 10.1007/s10802-011-9499-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutheén LK, Mutheén BO. Mplus user's guide. 5th. Los Angeles: Author; 2007. [Google Scholar]
- Obradovic J, Bush NR, Stamperdahl J, Adler NE, Boyce WT. Biological sensitivity to context: the Interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Development. 2010;81:270–289. doi: 10.1111/j.1467-8624.2009.01394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: An integrated review of human literature. Psychopharmacology (Berlin) 2011;214:55–70. doi: 10.1007/s00213-010-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickens JN, Field T. Facial expressions and vagal tone of infants of depressed and non-depressed mothers. Early Development and Parenting. 1995;4:83–89. [Google Scholar]
- Porges SW. US Patent No. 4,510,944 Method and apparatus for evaluating rhythmic oscillations in aperiodic physiological response systems. 1985
- Porges SW. The polyvagal perspective. Biological Psychology. 2007;74:116–143. doi: 10.1016/j.biopsycho.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porges SW, Doussard-Roosevelt JA, Portales AL, Greenspan SI. Infant regulation of the vagal “brake” predicts child behavior problems: A psychobiological model of social behavior. Developmental Psychobiology. 1996;29:697–712. doi: 10.1002/(SICI)1098-2302(199612)29:8<697∷AID-DEV5>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Propper C. The early development of vagal tone: Effects of poverty and elevated contextual risk. New York: Oxford University Press; 2012. [Google Scholar]
- Propper C, Moore GA, Mills-Koonce WR, Halpern CT, Hill-Soderlund AL, Calkins SD, et al. Gene–environment contributions to the development of infant vagal reactivity: The interactionof dopamine and maternal sensitivity. Child Development. 2008;79:1377–1394. doi: 10.1111/j.1467-8624.2008.01194.x. [DOI] [PubMed] [Google Scholar]
- Raine A, Lencz T, Bihrle S, Lacasse L, Colletti P. Reduced prefrontal gray matter volume and reduced autonomic activity inantisocial personality disorder. Archives of General Psychiatry. 2000;57:119–127. doi: 10.1001/archpsyc.57.2.119. [DOI] [PubMed] [Google Scholar]
- Rigterink T, Fainsilber Katz L, Hessler DM. Domestic violence and longitudinal associations with children's physiological regulation abilities. Journal of Interpersonal Violence. 2010;25:1669–1683. doi: 10.1177/0886260509354589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rottenberg J, Gross JJ, Gotlib IH. Emotion context insensitivity in major depressive disorder. Journal of Abnormal Psychology. 2005;114:627–639. doi: 10.1037/0021-843X.114.4.627. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Development. 1993;64:80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Saridjan NS, Huizink AC, Koetsier JA, Jaddoe VW, Mackenbach JP, Hofman A, et al. Do social disadvantage and early family adversity affect the diurnal cortisol rhythm in infants? The Generation R Study. Hormones and Behavior. 2010;57:247–254. doi: 10.1016/j.yhbeh.2009.12.001. [DOI] [PubMed] [Google Scholar]
- Schuetze P, Eiden RD. The association between maternal cocaine use during pregnancy and physiological regulation in 4- to 8-week-old infants: An examination of possible mediators and moderators. Journal of Pediatric Psychology. 2006;31:15–26. doi: 10.1093/jpepsy/jsj022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuetze P, Eiden RD, Coles CD. Prenatal cocaine and other substance exposure: Effects on infant autonomic regulation at 7 months of age. Developmental Psychobiology. 2007;49:276–289. doi: 10.1002/dev.20215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuetze P, Eiden RD, Edwards EP. A longitudinal examination of physiological regulation in cocaine-exposed infants across the first 7 months of life. Infancy. 2009;14:19–43. doi: 10.1080/15250000802569660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sheinkopf SJ, Lagasse LL, Lester BM, Liu J, Seifer R, Bauer CR, et al. Vagal tone as a resilience factor in children with prenatal cocaine exposure. Development and Psychopathology. 2007;19:649–673. doi: 10.1017/S0954579407000338. [DOI] [PubMed] [Google Scholar]
- Sheinkopf SJ, Lester BM, Sanes JN, Eliassen JC, Hutchison ER, Seifer R, et al. Functional MRI and response inhibition in children exposed to cocaine in utero: Preliminary findings. Developmental Neuroscience. 2009;31:159–166. doi: 10.1159/000207503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. Journal of the American Medical Association. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Smith DK, Johnson AB, Pears KC, Fisher PA, DeGarmo DS. Child maltreatment and foster care: Unpacking the effects of prenatal and postnatal parental substance use. Child Maltreatment. 2007;12:150–160. doi: 10.1177/1077559507300129. [DOI] [PubMed] [Google Scholar]
- Staton L, El-Sheikh M, Buckhalt JA. Respiratory sinus arrhythmia and cognitive functioning in children. Developmental Psychobiology. 2009;51:249–258. doi: 10.1002/dev.20361. [DOI] [PubMed] [Google Scholar]
- Suess PE, Porges SW, Plude DJ. Cardiac vagal tone and sustained attention in school-age children. Psychophysiology. 1994;31:17–22. doi: 10.1111/j.1469-8986.1994.tb01020.x. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, et al. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. American Journal of Psychiatry. 2003;160:1078–1085. doi: 10.1176/appi.ajp.160.6.1078. [DOI] [PubMed] [Google Scholar]
- Tottenham N, Hare TA, Millner A, Gilhooly T, Zevin JD, Casey BJ. Elevated amygdala response to faces following early deprivation. Developmental Science. 2011;14:190–204. doi: 10.1111/j.1467-7687.2010.00971.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, GatzkeKopp LM. Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry. 2009;50:1357–1364. doi: 10.1111/j.1469-7610.2009.02172.x. [DOI] [PubMed] [Google Scholar]
- Yumoto C, Jacobson SW, Jacobson JL. Fetal substance exposure and cumulative environmental risk in an African American cohort. Child Development. 2008;79:1761–1776. doi: 10.1111/j.1467-8624.2008.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


