Abstract
Complications related to preterm birth (PTB) and low birth weight (LBW) are leading causes of infant morbidity and mortality. Prenatal depression is a hypothesized psychosocial risk factor for both birth outcomes. The purpose of this systematic review was to examine evidence published between 1977 and 2013 on prenatal depression and risks of these primary adverse birth outcomes. A systematic search of the PUBMED and PsycINFO databases was conducted to identify studies testing the associations between prenatal depressive symptoms, or diagnoses of depression, and risk of PTB or LBW. We systematically selected 50 published reports on PTB and length of gestation, and 33 reports on LBW and BW. Results were reviewed by two independent reviewers and we evaluated the quality of the evidence with an established systematic review method, the Newcastle Ottawa Scale. We then undertook a narrative synthesis of the results following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Less than a quarter of 50 published reports found that prenatal depression was significantly associated with PTB or gestational age. In contrast, slightly more than half of the 33 reports found that prenatal depression was associated with LBW or BW. When weighing methodological features, we determined that the effects of prenatal depression on LBW are more consistent than effects on length of gestation or PTB. Although the evidence may not be strong enough to support routine depression screening for risk of adverse outcomes, screening to enable detection and timely treatment to reduce risk of postpartum depression is warranted. Further rigorous research on prenatal depression and adverse birth outcomes is needed.
Keywords: Preterm birth, Prenatal depression, Low birth weight, Mental health, Pregnancy
Introduction
Preterm birth (PTB) is a global public health problem [1]. Approximately 15 million babies are born preterm each year world-wide, and the prevalence of PTB in the United States is approximately 13 %. Furthermore, approximately 8.2 % of infants in the U.S. in 2009 were born low birth weight (LBW), weighing less than 2,500 g [2]. The consequences include increased risk of mortality, health and developmental problems for infants and children, and emotional and economic costs for families [3]. Understanding the etiology and pathways to these two key adverse birth outcomes is of utmost importance [4]. Established risk factors for PTB include previous PTB, multiple gestation, chronic illnesses, smoking, infections, high or low pre-pregnancy weight, and early or advanced maternal age [5]. In the past three decades, research has also identified some psychosocial risk factors, particularly some forms of stress and prenatal anxiety [6]. However, the evidence is not yet definitive regarding whether prenatal depression is a clear risk factor for either PTB or LBW, which is the focus of this review.
The prevalence of depression during the second and third trimesters has been documented to be twice that as in the general female population [7]. Andersson et al. [8] determined that major depression was present in approximately 3 % and minor depression in 7 % of 1,795 pregnant women, and the majority were found to be undiagnosed and untreated. The trajectory of prenatal depression in 357 pregnant women was characterized by a U-shaped curve decreasing from first trimester (22.1 %) to second trimester (18.9 %) and then increasing again in the third trimester (21.6 %) [9]. More recently, McDonald et al. [10] reported that prenatal depressive symptoms (using the EPDS ≥13 cutoff) were present in 12 % of 3,024 women in the All Our Babies cohort. Major depression is associated with considerable suffering, disability, and lost productivity, and has been ranked by the World Health Organization as the single most burdensome disease in the world in terms of total disability-adjusted life years [11]. Depression during pregnancy has been associated with poorer maternal health behavior [12] and an increased risk of postpartum depression [13].
Authors of prior literature reviews have remarked on the “inconclusive and inconsistent” evidence regarding links between prenatal depression and adverse birth outcomes [14–20]. We suspected that inconsistencies might be due to differences in methodology, sample size or composition, measurement and timing of depression assessment, and variation in whether studies accounted for potential confounds. Meta-analyses of this relatively small literature cannot easily take all of these design features into account. The specification of the birth outcome is also pertinent; that is, the most precise analyses distinguish spontaneous PTB (SPTB) from medically-indicated birth, which prior reviews and meta-analyses have not generally highlighted. A previous meta-analysis of 29 studies found small though significant associations between prenatal depressive symptoms and PTB, LBW, or intrauterine growth restriction (IUGR) [14]. In this meta-analysis, studies were categorized into those using a continuous depression measure versus those with categorical variables in which researchers compare groups with little or no risk to groups at high-risk of depressive disorder. In studies examining no/low versus high-risk groups, effect sizes appear to be larger (pooled RRs: PTB = 1.39; LBW = 1.49; IUGR = 1.45) than in studies using a continuous depression measure (pooled RRs: PTB = 1.03; LBW = 1.04; IUGR = 1.02). Also, higher risks of adverse birth outcomes were evident in depressed women from developing countries and among depressed women of low SES in the U.S. However, this meta-analysis did not take into account critical design and methodological features in drawing conclusions about birth outcomes.
The present systematic review therefore addressed an important gap in the literature by qualitatively examining each study with respect to study design and methodological criteria using a formal system. Taking into account study quality, we seek to determine if prenatal depression predicts PTB or LBW and to identify specific methodological reasons for inconsistencies.
Methods
This systematic review utilized state-of-the-art methods per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21] and performed quality assessments using the Newcastle Ottawa Scale (NOS) [22].
Search Strategy
We conducted a systematic review of the PubMed and PsycINFO electronic databases for English language publications testing associations between depression and birth outcomes between April 1977 when the first publication appeared, and April 2013 (when we completed data collection and began the systematic review process). Keywords included depression, depressive disorder, prenatal, preterm, premature, prematurity, birth weight, low birth weight, small-for-gestational age, gestational age, fetal maturity, fetal growth retardation/restriction, and intrauterine growth retardation/restriction (see Appendix S1 for keyword combinations). Additional studies were identified by reviewing reference sections of retrieved articles.
Inclusion and Exclusion Criteria
Published observational studies were included if they used validated self-report screening tools to measure depressive symptoms during pregnancy, structured psychiatric interviews during pregnancy, or medical record chart review for current unipolar depression diagnoses. A published article had to include sufficient details on results on depressive symptoms/diagnosis and at least one birth outcome (PTB or GA, LBW or BW, small for gestational age, SGA, or IUGR) in order to be considered for inclusion. Some studies were not designed with the primary goal of testing prenatal depression and birth outcomes, but if relevant results were sufficiently described, they were included e.g. [23–26]. Studies were excluded if they: (1) Measured prenatal depression after the birth of a child (retrospectively) [27–45]; (2) Reported pre-pregnancy/postpartum depression [42–47]; (3) Did not use a reliable and/or valid measure of depression [48–55]; (4) Did not separate depression in analyses from antidepressant use [56–58]; (5) Combined unipolar with bipolar depression (or other psychiatric diagnoses) [59–67]; or (6) Reported the same data as a previous article [68–72]. Bipolar disorder and other psychiatric conditions were excluded from this systematic review due to their differing etiologies, treatments, and potential relationship to adverse birth outcomes compared to depression.
Study Selection and Data Extraction
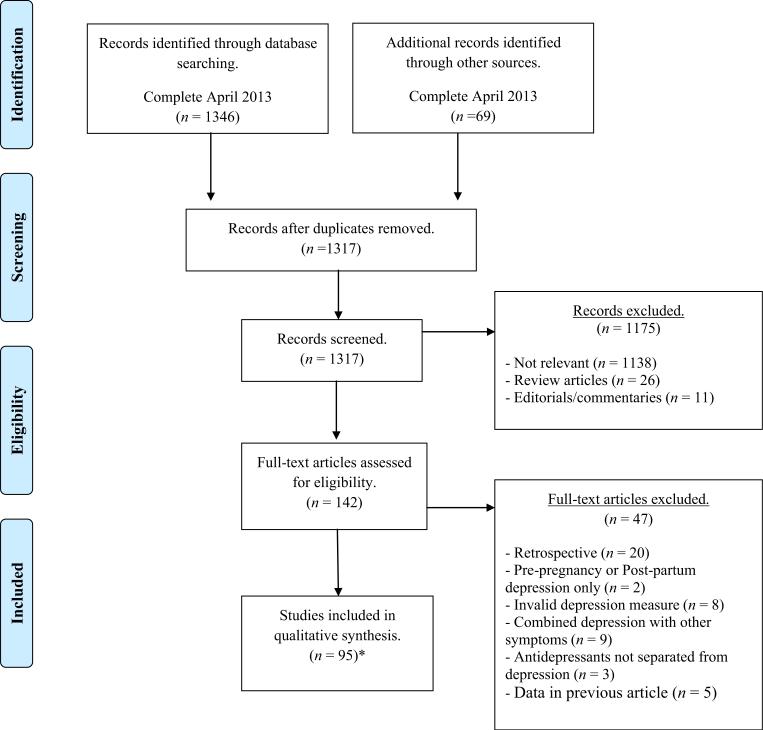
Figure 1 provides an overview of the study selection and data extraction process per PRISMA guidelines [21]. Over 1,300 records were identified, and 142 full-text articles met sufficient criteria for detailed examination. Ninety-five full-length articles met the full inclusion criteria for this systematic review, and 108 published findings were available in the 95 articles. The total number of findings is greater than the number of articles because a number of studies tested associations of depression with both LBW/BW and PTB/GA. In total, this review includes 50 published findings on PTB/GA from 47 articles, 33 findings on LBW/BW from 29 articles, and 25 findings on SGA/IUGR from 19 articles.
Fig. 1.
PRISMA Flow diagram. *This total includes 50 published findings on PTB/GA from 47 articles, 33 findings on LBW/BW from 29 articles, and 25 findings on SGA/IUGR from 19 articles
Study characteristics regarding design, sample, covariates, and timing and method of depression measurement were extracted (see Tables 1, 2, 3, 4). In addition, we extracted information regarding whether the outcome was categorical (PTB, LBW) or continuous (GA, BW), and whether analyses were conducted for SPTB as a subset of all PTBs. One author conducted data extraction (EEA) and another verified it (AC). Discrepancies occurred in less than one quarter of results and were resolved through discussion with all authors.
Table 1.
Prenatal depression and PTB/GA—12 significant associations in chronological order
| Nos. | References | Participants (details) | Study design, timing of assessment and measures | Control variables (NOS guidelines: 0-2 stars) | SPTB? | Primary results | Quality assessment (NOS 5-9 stars; mean = 7) |
|---|---|---|---|---|---|---|---|
| 1. | Steer et al. [129] | N = 389 low SES adults from the U.S.: 28.7% Puerto Rican, 61.8% African American, 9.6 % Caucasian. Total N = 712 inner city adults and adolescents |
Prospective cohort study. Assessed once in 3rd trimester (28 weeks) with the BDI |
2 stars Medical: parity, prior LBW, prior PTD, BMI, adequate weight gain. Excluded if histories of non-obstetric, chronic disease Socio-demographic: Ethnicity, marital status, Medicaid Behavioral: smoking, marijuana, alcohol abuse, or a history of psychiatric illness |
No | OR = 1.06 for PTB when BDI used as a continuous variable OR 3.39 for PTB when depression cutoff score used Significant association found in adults only, none with any birth outcomes in adolescents |
6 |
| 2. | Orr et al. [130] | N = 1,399 low income African American women | Prospective cohort study. Assessed once during 1st and 2nd trimester. The median number of weeks of gestation for CESD was 17 | 2 stars Medical: chronic disease, bleeding, low pre-pregnancy BMI, previous poor pregnancy outcome Socio-demographic: race Behavioral: smoking, drug use |
Yes | Women in top 10 % CESD at greater risk of SPTB (adj. OR 1.96). | 8 |
| 3. | Rondo et al. [127] | N = 865 low SES Brazilian women | Regional cohort study with 17 sites; Assessed 3 times: <16; 20-26, and 30-36 weeks with GHQ-12 | 2 stars Medical: pre-pregnancy BMI, age Socio-demographic: education, marital status Behavioral: smoking, alcohol Excluded: chronic infectious diseases, metabolic diseases, cardiopathy, mental diseases, hypertension, preeclampsia, eclampsia, vaginal bleeding and multiple deliveries |
No | GHQ associated with PTB OR 2.32 | 7 |
| 4. | Drewett et al. [126] | N = 12,391 in the UK | Population-based cohort study. Assessed 4 times: 18 and 32 weeks gestation; 8 weeks and 8 months postpartum with the EPDS |
No stars Medical: None Socio-demographic: None. A “range of social variables” were accounted for, but only specifically mentions home ownership, use of a car, and #kids in regression analyses Behavioral: None |
No | Associated with PTB and failure to thrive. After adjustments, the relative risk for PTB was 1.6 | 5 |
| 5. | Dayan et al. [125], Same cohort as Dayan et al. [72] | N = 641 Caucasian French women | Prospective Cohort Study. Assessed once in 2nd trimester, between 20-28 weeks with the EPDS |
2 stars Medical: maternal age, previous PTB, parity, pre-pregnancy BMI, complications of the current pregnancy: vaginal bleeding, urinary tract infection, cervical or vaginal infection, polyhydramnios, preeclampsia, or gestational hypertension Socio-demographic: occupation Behavioral: smoking |
Yes | Associated with PTB: OR 4.90 (1.60-14.90). The association was stronger with depression when psychotropic users were excluded. Adjusted OR of 4.9. Rate of SPTB was higher for women with higher depression scores than non-depressed. OR 3.3 | 7 |
| 6. | Field et al. [96] | N = 430 USA | Regional; case-control study with multiple sites. Assessed at 22 weeks and again at 32 weeks with SCID and CESD |
No stars Medical: None Socio-demographic: None Behavioral: Women weren't on drugs, alcohol, antidepressants or smoking |
NA GA (no PTB) outcome |
The depressed group had newborns with significantly lower GA and BW | 5 |
| 7. | Kabir et al. [131] | N = 1,684 total Aged 13-21; 32.6 % Caucasian, 31.6 % Black, 32.6 % Hispanic, and 3.2 % Native American/Pacific Islander/Asian |
Cohort study. Assessed 1 or 2 times: N = 687 1st trimester and N = 415 again in 3rd tri N = 667 2nd tri. and 361 again in 3rd tri. N = 330 with 3rd tri. only. CESD full scale and Non-Somatic CESD Subscale | 2 stars Medical: age, chronic medical conditions excluded Socio-demographic: education Behavioral: support |
Yes | Adolescent mothers who were depressed in the 2nd and 3rd trimesters were at increased risk for inadequate weight gain and both small for gestational age fetuses and preterm delivery (ORs 1.6-1.8). Held up with CES-D variation | 7 |
| 8. | Li et al. [91] | N = 791 Ethnically diverse Americans | Population-based prospective cohort study. Assessed once during 1st or 2nd trimester: 10 weeks of gestation on average (6-18 weeks) with the CESD. | 2 stars Medical: maternal age, gravidity, history of miscarriage, preterm delivery or LBW Socio-demographic: education, race/ethnicity Behavioral: vitamin use, vomiting and smoking during pregnancy Findings maintained after removing women on antidepressants (only 1.5 % of sample) |
No | Dose-response relationship of risk of PTB associated with depressive symptoms (CESD >16) during early pregnancy. Compared with women CESD <16 women with a CESD >22 had a greater than twofold increased risk of PTB [adjusted hazard ratio (aHR) = 2.2], whereas women with a CESD score of 16-21 had about 60 % increased risk (aHR = 1.6) | 7 |
| 9. | Van Dijk et al. [87] | N = 4,044 Amsterdam | Large population-based cohort study. Assessed between 14 and 18 weeks with the CESD |
2 stars Medical: maternal age, pre-pregnancy BMI, primiparity, hypertension, onset of delivery Socio-demographic: education after primary school, ethnicity. Behavioral: smoking, alcohol consumption |
NA GA (no PTB) outcome |
Significant association between major depressive Sx and GA (–0.2 weeks; 95 % confidence interval –0.4 to 0.0). Mild and major depressive Sx, as well as the lowest serum folate quintile, were sig associated with LBW in the univariate model but not after multivariate adjustment | 8 |
| 10. | Fransson et al. [132] | N = 2,904 Swedish | A prospective national study. The average length of gestation at assessment time was 16 weeks (SD 3.4) with the EPDS | 2 stars Medical: maternal age, parity, previous miscarriage, pregnancy after assisted reproductive technology, and previous infertility ≥1 year Socio-demographic: education, employment, marital status, born outside Sweden Behavioral: smoking |
No | EPDS >12 associated with PTB OR 1.56 | 8 |
| 11. | Nylen et al. [97] | N = 235 86 % married, 94 % Caucasian, 75 % working mothers Over half 58 % were primiparous USA |
Cohort study: 104 were enrolled in 1st trimester and 131 were enrolled in the 2nd trimester SCID interviews were completed after enrollment (M 17.71 weeks, SD 6.68) | 2 stars Medical: age, parity, indices were created by summing number of risk factors based on obstetric history and medical conditions Socio-demographic: education, ethnicity, income Behavioral: smoking. |
NA GA (no PTB) outcome |
Relative to non-depressed, depressed had babies who weighed less, p < .001, were born earlier p < .001 After adjusting for controls, major depression was a significant predictor of GA. The interaction of major depression and partner support adequacy also predicted GA |
9 |
| 12. | Straub et al. [104] | N = 14,175 pregnant women in USA 70.8 % Caucasian, 7.8 % African American, 13.7 % Hispanic |
National case-control study with multiple sites. Assessed between 24 and 28 weeks gestation with the EPDS |
1 star Medical: Maternal age, history of PTB Socio-demographic: race, insurance status Behavioral: None |
No | EPDS associated with PTB adjusted OR 1.3 | 7 |
Control variables: SPTB addressed adequately
NOS Star system allows for ratings of adequate controls: A study that controls for any 3+ variables from two categories (1) medical risk factors (e.g. maternal age, parity, previous PTB, gestational diabetes, chronic hypertension, infections, pre-pregnancy BMI; (2) sociodemographic factors (e.g. Race/ethnicity, education, employment, SES, marital status etc.) and (3) behavioral factors (e.g. Smoking, alcohol, drugs (incl. antidepressants), physical activity etc.) receives 1 star. A study that controls for any 4+ variables in all three categories above receives 2 stars
Table 2.
Prenatal depression and PTB/GA—35 non-significant associations in chronological order
| Nos. | References | Participants (details) | Study design, timing of assessment and measures | Control variablesa (NOS guidelines: 0-2 stars) | SPTB? | Primary results | Quality assessment (NOS 5-9 stars; Mean = 7.2) |
|---|---|---|---|---|---|---|---|
| 1. | Kumar and Robson [93] | N = 108 first-time pregnant women in central London | Regional cohort study with one site. Depression assessed before 14 weeks gestation with GHQ-30 |
0 stars Medical: None Socio-demographic: None Behavioral: None |
No | Maternal prenatal depression not significantly associated with PTB | 5 |
| 2. | Perkin et al. [88] | N = 1,515 Caucasian women in London. | Prospective cohort study. Assessed at Booking, 28, & 36 weeks with the GHQ depression subscale. |
2 stars Medical: age, parity. Socio-demographic: education, employment, marital status. Behavioral: alcohol use. |
Yes PTB separated into 5 different outcomes. |
No significant association of depression or anxiety with PTB. | 7 |
| 3. | Copper et al. [120] | N = 2,593 (63 % African American, 35 % Caucasian) Single, low educated USA |
National sample with multiple sites (10); depression assessed at 25-29 weeks gestation with Abbreviated Scale for the Assessment of Psychosocial Status in Pregnancy (incl. CESD) | 2 stars Medical: maternal age Socio-demographic: race, marital, and educational status, insurance Behavioral: smoking, alcohol, and drugs Excluded: multiple gestation, cerclage, placenta previa, or major fetal anomaly |
Yes SPTB only |
No significant associations found for CESD with PTB or LBW Stress was significantly associated with LBW after demographic controls |
7 |
| 4. | Goldenberg et al. [83] | N = 1,491 women who had previously given birth (69 % African American) USA—Alabama |
Prospective cohort study. Assessed at 24-26 weeks with CESD | 2 stars Medical: maternal BMI, height, hypertension and diabetes, infant sex Socio-demographic: race Behavioral: smoking, alcohol, drugs |
No for PTB GA also assessed |
No association of CESD with PTB Only hypertension and not having a car were significant predictors among African American women; low positive life events and poor paint were predictive among Caucasian women |
7 |
| 5. | Nordentoft et al. [124] | N = 2,432 Caucasian Women from Denmark | Cohort Study. Assessed once during 2nd trimester (week 20) in clinic with the GHQ-12 | 2 stars Medical: maternal age Socio-demographic: education, frequency of seeing family and friends, cohabitating, support, reaction to pregnancy Behavioral: smoking and alcohol, tranquilizers |
No | No significant association of GHQ-12 depression with PTB | 8 |
| 6. | Hoffman & Hatch [90] 2000 | N = 666 USA 98 % Caucasian. |
Community-based prospective cohort study. Assessed during 2nd & 3rd trimesters with CESD: Mailed at 28 and 36 weeks. |
2 stars Medical: maternal age, parity, pre-pregnancy weight, pregnancy hypertension. Socio-demographic: social support, marital events. Behavioral: smoking. Excluded multiparious & 2nd trimester spontaneous abortions & stillbirths. |
No for PTB. GA also assessed. |
No significant association for depression and gestational duration. | 8 |
| 7. | Anders son et al. [86] | N = 1,465 Sweden | Cohort study with 2 sites; depression assessed before ultrasound at 16-18 weeks gestation with PRIME-MD | 2 stars Medical: age, chronic disease, BMI, parity Socio-demographic: marital status, socioeconomic status Behavioral: smoking, tobacco use (other than cigarette smoking), alcohol consumption |
Yes | No significant association of depressive disorders and PTB | 9 |
| 8. | Dole et al. [133] Same cohort as Dole et al. [70] |
N = 1,898 mixed race (USA) | Prospective cohort study. Assessed once during 2nd or 3rd trimester with the CESD | 2 stars Medical: maternal age, parity, pre-pregnancy BMI, bacterial vaginosis Socio-demographic: marital, educational and economic status, and SES Behavioral: alcohol and smoking |
Yes | No association of CESD with PTB, same as Dole 2003. Note: Dole 2004 found significant associations with pregnancy anxiety |
8 |
| 9. | Suri et al. [98] | N = 62 USA |
Prospective cohort study. Assessed depression with the CESD in each trimester. SCID once |
No stars Medical: None. Socio-demographic: None Behavioral: Excluded psychotic symptoms, use of meds known to adversely affect the fetus, other psychotropic medications, presence of suicidality, alcohol, cigarettes, or substances |
No for PTB GA also assessed. |
No significant association of CESD or SCID with GA or BW | 6 |
| 10. | Berle et al. [119] | N = 680 Women from Norway | National cohort study; depression assessed during 1st, 2nd and 3rd trimesters of pregnancy with HADS |
1 stara Medical: maternal age Socio-demographic: education Behavioral: smoking, alcohol, and psych medications aBecause controls only included in first step of analyses |
No | No significant association of HADS-D with PTB or LBW | 7 |
| 11. | Engel et al. [25] | N = 52 women near World Trade Center, NYC, USA | Prospective cohort study. Assessment timing in pregnancy not clear. BDI was used |
No stars Medical: maternal age All birth weight and head circumference models were adjusted for length of gestation |
No for PTB GA also assessed |
Depression not associated with LBW or SGA PTSD associated with longer GA and smaller head circumference |
6 |
| 12. | Haas et al. [134] | N = 1,619 Mixed race Americans | Prospective cohort study. Assessed twice during 2nd and 3rd trimesters with the CESD. Depressive Sx if CESD >10 |
2 stars Medical: maternal age, parity, BMI, medical conditions Socio-demographic: race/ethnicity, education Behavioral: smoking, drugs, exercise |
No | Depressive symptoms were not associated with PTB in any model | 7 |
| 13. | Messer et al. [135] | N = 1,908 USA—North Carolina |
Prospective cohort study. Assessed at 24-29 weeks by mail with the CESD. Higher cutpoints than are commonly used for the CES-D (≥25, 17 through <25 and <17) |
1 star Medical: age Socio-demographic: race, education, and marital status Behavioral: Measured smoking and alcohol, but don't seem to include in analyses |
No | Medium and high levels of depression were not associated with PTB | 7 |
| 14. | Neggers et al. [102] | N = 3,149 low-income women in Jefferson County, AL; 81 % African American | Regional cohort study with multiple sites. Assessed once during 2nd trimester (22-23 weeks) with CESD—incorporated into a 28 item Psychosocial Scale |
2 stars Medical: maternal age, parity, pre-pregnancy BMI, hypertension, diabetes, and infant gender Socio-demographic: education Behavioral: smoking and alcohol |
Yes | Negative affect alone was not significant for SPTB Psychosocial distress (larger scale), which includes trait anxiety, stress etc., was significantly associated with PTB, OR 1.30 |
6 |
| 15. | Rogal et al. [95] | N = 1,100 USA 87 % non-Caucasian | Regional cohort study with multiple sites; depression assessed at any point during pregnancy with the PRIME-MD BHQ |
2 stars Medical: maternal age Socio-demographic: race, language Behavioral: tobacco, alcohol, and illicit drug use in pregnancy |
No | No significant association of prenatal depression with PTB | 7 |
| 16. | Suri et al. [85] Not the same cohort as Suri et al. [98] |
N = 90 USA |
Prospective naturalistic study. Diagnosed with depression (SCID), and assessed (49 Tx for MDD, 22 MDD no Tx, 19 comparisons) depression monthly Ham-D and BDI |
No stars GA confounds controlled for: Medical: maternal age, number of prior pregnancies, hypertension, pre-eclampsia, maternal weight gain |
No for PTB GA also assessed. |
No significant association of depression with PTB or LBW. Antidepressant status has a significant effect on GA at birth, beyond the impact of depression and maternal risk factors | 7 |
| 17. | Xiong et al. [122] | N = 301 women pregnant during or immediately after Hurricane Katrina | Regional cohort study with two sites; depression assessed once at any point in pregnancy with EPDS |
2 stars Medical: age, parity, LBW history Socio-demographic: education, race, marital status, family income Behavioral: smoking, alcohol use |
No | Depression and PTSD were associated with a non-significant decreased risk of PTB and increased risk of LBW Note: High hurricane exposure was associated with increased risk of LBW (OR 3.3) and PTB (OR 2.3) |
7 |
| 18. | Diego et al. [100] | N = 79 mixed race (USA) 59 % Hispanic, 32 % African American, 9 % Caucasian |
Regional case-control study; depression assessed at enrollment at 18-20 weeks gestation with CES-D; SCID used for categorization |
2 stars Medical: maternal age Socio-demographic: marital status and SES Behavioral: See exclusions Excluded: hypertensive disorders, anemia, vaginal bleeding; IUGR; pregnancy complication; HIV, abnormal pre-pregnancy BMI, metabolic or any psychiatric condition other than depression, smoking, alcohol, drugs, antidepressants or other psych medications |
No for PTB GA also assessed. |
No statistically significant association of depression and GA | 8 |
| 19. | Gavin et al. [46] | N = 3,019 Americans The cohort was 65 % non-Hispanic Caucasian, 25 % African American, and 10 % other |
Prospective multicenter (5) cohort study. Assessed once during 2nd trimester (15-27 weeks) with CESD |
2 Stars Medical: maternal age, parity, BMI Socio-demographic: race, Medicaid Behavioral: smoking Mediators: smoking, pre-pregnancy BMI, alcohol use, caffeine use, and illicit drug/substance use |
Yes | Depressive symptoms and use of psych meds were not significantly related to PTB | 8 |
| 20. | Kramer et al. [89] | N = 5,337 Canadian Women | Combines features of a prospective cohort and a nested case-control design. Assessed at 24-26 weeks with CESD >16, 4 item CDS pregnancy-anxiety, etc. |
2 Stars Medical: maternal age and height, parity, pre-pregnancy BMI, and medical/obstetric risk Socio-demographic: education, living arrangement, birthplace, language spoken, family income Behavioral: smoking at the time of the 2nd-trimester interview |
Yes | No significant association with prenatal depression over and above anxiety Note: Pregnancy-related anxiety was significantly associated with the risk of SPTB |
8 |
| 21. | Bae et al. [118] | N = 114 South Korean | Regional case-control study with one site. Depression assessed during 1st, 2nd, 3rd trimesters with BDI; BDI <10: low depression, BDI >10: high depression |
No stars Medical: pre-pregnancy BMI Socio-demographic: None Behavioral: alcohol |
No | No significant differences in BW or GA were observed between two groups Note: PTB cutoff was 38.5, so examined for GA results only, although the findings were consistent |
5 |
| 22. | Benute et al. [94] | N = 326 Brazilian women with medical disorders in pregnancy | Regional case-control study with one site; depression assessed at mean gestational age 28.2 weeks with PRIME-MD |
No stars Sample was specifically recruited for medical disorders i.e. pre-eclampsia or chronic hypertension, heart disease, diabetes mellitus, anemia, collagenosis, and risk for preterm delivery. 22 (6.8 %) women had two associated disorders |
No | Comparison between women who presented with major depression and those who did not revealed no significant differences in preterm delivery, birth weight or low Agpar scores | 5 |
| 23. | Goedhart et al. [136] | N = 8,050 Women in Amsterdam | Prospective, community-based, multicenter, cohort study. Assessed after 1st prenatal visit (12 weeks) with mailed CESD. Used cutoff of >16 for depressed |
2 stars Medical: maternal age, parity, pre-pregnancy BMI, hypertension Socio-demographic: education, ethnicity Behavioral: alcohol and drug use Found a small mediation effect of maternal smoking |
No | No association of CESD with PTB | 8 |
| 24. | Wang and Chen [123] | N = 431 Taiwan, mod-high SES |
Cohort study with multiple sites; depression assessed at 17-38 weeks gestation with EPDS |
0 stars Medical: None Socio-demographic: None Behavioral: None. |
No | Prenatal depression was not significantly associated with any obstetric outcomes studied | 7 |
| 25. | Bodecs et al. [92] | N = 261 Hungarian women | Cohort study with multiple sites; depression assessed at enrollment at average of 8.13 weeks gestation with 9-item BDI |
2 stars Medical: maternal age, parity Socio-demographic: marital, educational and socioeconomic status Behavioral: smoking, alcohol, and vitamins |
No for PTB GA also assessed. |
Maternal depression had no association with birth outcomes | 8 |
| 26. | Shaikh et al. [137] | N = 132 Pakistani | Prospective cohort study. Assessed at 28-30 weeks with the CESD |
1 star Medical: Excluded diabetes mellitus, thyroid disorder, chronic renal or heart disease, or uterine and cervical abnormality Socio-demographic: None Behavioral: Excluded antidepressants or other psychotropic drugs |
No | In the univariable logistic regression analysis depression was not associated with PTB | 7 |
| 27. | El Marroun et al. [82] | N = 7,696 Netherlands | Regional case-control study; depression assessed at mean gestational age 20.6 weeks with BSI |
2 stars Medical: maternal age, body mass index, parity, sex of child Socio-demographic: maternal education, ethnicity Behavioral: smoking and drinking habits, and benzodiazepine use |
No for PTB GA also assessed. |
SSRI-exposed were at higher risk for PTB (OR 2.14). No sig association of PTB and depression in women not using SSRI Results were consistent, whether using GA or PTB, but only in those not treated with SSRI |
8 |
| 28. | Hayes et al. [23] | N = 228,876 USA—Tennessee |
Retrospective cohort study. Collected ICD9 codes for depression (included if diagnosed DURING pregnancy only) and antidepressant prescription and fillings in Medicaid database |
2 stars Medical: maternal age, parity, infant sex, adequacy of prenatal care Socio-demographic: race, education Behavioral: smoking, comorbid anxiety, substance abuse Dx, coexisting Psych Dx, and antidepressants b4 LMP |
No | Second trimester anti-depressant use, not depression diagnosis, was associated with PTB | 9 |
| 29. | Ibanez et al. [84] | N = 1,624 in models French women (N = 2,002 entire sample) |
Case-control study in two regions in France. Assessed between 24 and 28 weeks with CESD |
2 stars Medical: maternal age, parity, pre-pregnancy BMI, hypertension, and infant sex. Excluded Hx diabetes Socio-demographic: level of education, and center Behavioral: smoking |
Yes GA also assessed |
No association for women who were just depressed (CESD >16) and not also anxious | 8 |
| 30. | Okun et al. [26] | N = 217 USA | Prospective Observational Study Assessed at 20, 30, and 36 weeks gestation with the SCID |
No stars (for relevant analyses) For sleep analyses Medical: maternal age and history of PTB Socio-demographic: employment, marital status Behavioral: MDD and SSRI |
No | There were no overall differences in the number of PTBs between depressed and non-depressed women PTB occurred more often among women who were using SSRI medications at 20 and 30 weeks gestation |
7 |
| 31. | Ruiz et al. [138] | N = 470 Hispanic USA |
Cross-sectional study. Assessed at 22-24 weeks with the CESD |
2 stars Medical: history of PTB, preeclampsia, infections during pregnancy, age, BMI Socio-demographic: marital status Behavioral: those using antidepressants were excluded |
No | Depressive symptoms did not directly predict PTB in the model; however, the combination of depressive symptoms with progesterone and E3 predicted PTB, indicating that the combined impact of these factors produced the greatest risk | 6 |
| 32. | Savitz et al. [128] | N = 4,251 USA PIN Study |
Prospective cohort study. Assessed during 24-29 weeks with the CESD and Medical Outcomes Study Social Support Survey |
2 stars Medical: age, parity, BMI Socio-demographic: race and education Behavioral: exercise, smoking, social support |
Yes | CESD alone was not significantly associated with PTB In high risk group (including depression, smoking, exercise etc.) they did find a significant association with PTB |
8 |
| 33. | Subramanian et al. [121] | N = 970 low income African American women | Regional case-control intervention study; depression assessed at enrollment, 2nd trimester, 3rd trimester, and postpartum with 7-item BDI and HSCL-D |
2 stars Medical: age, previous birth outcomes, diabetes, hypertension Socio-demographic: education, marital status, employment, Medicaid/WIC status Behavioral: drug and alcohol use |
No | No significant associations between depression and any birth outcomes (not PTB, LBW, or SGA) | 8 |
| 34. | Yonkers et al. [24] | N = 2,793 USA |
Prospective cohort study. Assessed at 3 time points (±17 weeks gestation; 28 ± 2 weeks gestation; 8 ± 4 weeks postpartum) Depression module of World Mental Health Composite Int'l Diagnostic Interview |
2 stars Medical: mother's age, history of PTB. Excluded if suffered from insulin-dependent diabetes Socio-demographic: education, race Behavioral: smoking, illicit drug Further adjusted for # lifetime hospitalizations, age of depressive onset, # of prior depressive episodes, PTSD, GAD, panic disorder in pregnancy, and suicidal thoughts in pregnancy |
Yes | SRI use (separate from illness) is a clear risk factor for PTB Uncertain risk of PTB associated with depression. Ns are small for SPTB (MDD + SRI N = 2; MDD-SRI N = 6) |
9 |
| 35. | Gawlik et al. [99] | N = 273 German | Prospective case-control study. Assessed late 2nd or 3rd trimester (>24 weeks), mean 32 weeks, with EPDS (phone SCID for those screened >12 on EPDS) |
1 star Medical: Maternal age and infant sex Excluded if serious medical condition. No antidepressants |
No for PTB GA also assessed |
There was no significant influence of depression or state anxiety on GA or BW Note: Of the 14 women above EPDS cutoff, 10 met SCID criteria for anxiety disorders and only 4 for depression |
7 |
Control variables: SPTB addressed adequately
NOS Star system allows for ratings of adequate controls: A study that controls for any 3+ variables from two categories (1) medical risk factors (e.g. maternal age, parity, previous PTB, gestational diabetes, chronic hypertension, infections, pre-pregnancy BMI; (2) sociodemographic factors (e.g. Race/ethnicity, education, employment, SES, marital status etc.) and (3) behavioral factors (e.g. Smoking, alcohol, drugs (incl. antidepressants), physical activity etc.) receives 1 star. A study that controls for any 4+ variables in all three categories above receives 2 stars
Table 3.
Prenatal depression and LBW/BW—11 significant associations in chronological order
| Nos. | References | Participants (details) | Study design, timing of assessment and measures | Control variables (NOS guidelines: 0-2 stars)a | GA | Primary results | Quality assessment (NOS 5-9 stars; Mean = 6.5) |
|---|---|---|---|---|---|---|---|
| 1. | Rondo et al. [127] | N = 865 pregnant women in Jundiai, Brazil | Regional cohort study with 17 sites; depression assessed at 16, 20-26, and 30-36 weeks with GHQ-12 | 2 stars Medical: age, parity, prior history of LBW Socio-demographic: SES, marital status, education, per capita income Behavioral: smoking, alcohol use, coffee use |
No | Mothers with GHQ scores higher than 3 at the second interview (20-26 weeks) were more likely to have LBW infant (RR 1.97, p = 0.019) | 7 |
| 2. | Rahman et al. [103] Same cohort as Rahman et al. [71] |
N = 143 depressed pregnant women and 147 non-depressed pregnant women in rural Pakistan | Regional case-control study; depression assessed during 3rd trimester with SCAN |
2004: 1 star Medical: age, maternal BMI Socio-demographic: social support, age of other children Behavioral: None Excluded: premature births, smokers, physical illness treatment, 'eventful' pregnancies |
No | 2004: Depressed mothers more likely to have LBW infant than non-depressed mothers (RR 2.1) 2007: Infants of depressed mothers had lower BW than those of non-depressed mothers (OR 2.2) |
8 |
|
2007: 1 star Medical: low BMI, firstborn Socio-demographic: relative poverty, nuclear family, maternal empowerment, antenatal consultation Behavioral: None |
|||||||
| 3. | Neggers et al. [102] | N = 3,149 pregnant U.S. low-income women in Jefferson County, AL; 81 % African American | Regional cohort study with multiple sites; depression assessed at 22-23 weeks gestation with the Abbreviated Scale for Assessment of Psychosocial Status in Pregnancy |
2 stars Medical: pre-pregnancy BMI, PTB history, parity, history of hypertension and diabetes, infant gender Socio-demographic: race, education Behavioral: alcohol and tobacco use. Excluded: multiple pregnancies |
No | Negative affect was significantly associated with BW and LBW (AOR 1.4); Association only persistent for low-BMI women | 6 |
| 4. | Patel and Prince [139] | N = 245 pregnant women in Mapusa, Goa, India | Cohort study with one site; depression assessed at more than 30 weeks (mean = 34) with GHQ-12 |
1 star Medical: age Socio-demographic: income, antenatal IPV, maternal and paternal education Behavioral: None Excluded: premature births |
No | Depression associated with LBW (OR 1.53 for each quartile increase in GHQ score) | 6 |
| 5. | Rogal et al. [95] | N = 1,100 pregnant U.S. women in CT; 87 % non-Caucasian | Regional cohort study with multiple sites; depression assessed at any point during pregnancy with the PRIME-MD BHQ |
2 stars Medical: age, panic disorder, PTSD Socio-demographic: race Behavioral: tobacco, alcohol, illicit drug |
No | Mothers with minor depression more likely to have LBW infant (OR 1.91; OR 1.82 in final model) | 7 |
| 6. | Field et al. [96] | N = 430 U.S. pregnant women; 55 % Hispanic, 23 % African American, 22 % non-Hispanic White | Regional; case-control study with multiple sites; depression assessed at 20-24 weeks (mean = 2), 32 weeks, after delivery with CES-D; SCID used to categorize |
0 stars Medical: None Socio-demographic: None Behavioral: None Excluded: smoking, alcohol or drugs during pregnancy or antidepressants |
No | Depressed group had newborns with lower birth weight (3332.3 vs. 3093.3 g; p < .05) | 5 |
| 7. | Diego et al. [100] | N = 79 U.S. women in Miami, FL; 59 % Hispanic, 32 % African American, 9 % Caucasian | Regional case-control study; depression assessed at enrollment at 18-20 weeks gestation with CES-D; SCID used for categorization | 2 stars Medical: age, see exclusions Socio-demographic: SES, marital status Behavioral: See exclusions Excluded: hypertensive disorders, anemia, vaginal bleeding, IUGR; pregnancy complication; HIV or infectious disease; abnormal pre-pregnancy BMI, metabolic disorders or any psychiatric condition other than depression; smoking, alcohol, drugs, antidepressants or other psychotropic medications |
Yes | Prenatal depression was significantly associated with BW Depressed women had 15 % greater incidence of LBW than non-depressed women (89.1 vs. 81.4 g/gestational week; p = .008) |
8 |
| 8. | Nasreen et al. [140] | N = 583 pregnant women in Bangladesh; 50 % below poverty level | Cohort study with multiple sites; depression assessed during 3rd trimester with EPDS |
1 star Medical: maternal malnutrition Socio-demographic: household economic status, emotional support, joint family status, anxiety Behavioral: None Excluded: multiple pregnancies |
No | Depressive symptoms were significantly associated with LBW (OR 2.24) | 6 |
| 9. | Liu et al. [106] | N = 755 U.S. pregnant women in Durham NC; 56 % African American, 44 % Caucasian | Regional cohort study with five sites; depression assessed at enrollment at 4-32.5 weeks (mean = 12) with CES-D |
2 stars Medical: pre-pregnancy/early prenatal BMI, delivery mode, parity, PTB history Socio-demographic: education Behavioral: smoking, folic acid use, psychotropic medication use during pregnancy |
No | Severe depressed mood associated with higher risk of LBW (OR 3.6); association limited to black women (OR 7.2) and more pronounced for female infants (OR 7.5) | 6 |
| 10. | Straub et al. [104] | N = 14,175 pregnant U.S. women; 70.8 % Caucasian, 7.8 % African American, 13.7 % Hispanic | National case-control study with multiple sites; depression assessed at 24-28 weeks with EPDS; EPDS ≥12 or yes to self-harm question considered at risk |
1 star Medical: age, preterm delivery history Socio-demographic: race/ethnicity, insurance status Behavioral: None Excluded: multiple pregnancies |
No | Women at risk for depression had infants with lower birth weight than those not at risk (p = 0.019) | 7 |
| 11. | Earnshaw et al. [101] | N = 420 U.S. women aged 14-21 in NYC; 62 % Latina, 38 % African American; 28 % foreign born | Regional cohort study with multiple sites; depression assessed at 14-24, 32-42 weeks, 6-12 months postpartum with CES-D with somatic symptoms dropped |
0 stars Medical: None Socio-demographic: None Behavioral: None Excluded: medical problems requiring individual care, multiple pregnancies |
Yes | Depressive symptoms associated with decreased BW (correlation –.15b; –.13b in final path model). Also associated with LBW | 6 |
Control variables: NOS Star system allows for ratings of adequate controls: A study that controls for any 3+ variables from two categories (1) medical risk factors (e.g. maternal age, parity, previous PTB, gestational diabetes, chronic hypertension, infections, pre-pregnancy BMI; (2) sociodemographic factors (e.g. Race/ethnicity, education, employment, SES, marital status etc.) and (3) behavioral factors (e.g. Smoking, alcohol, drugs (incl. antidepressants), physical activity etc.) receives 1 star. A study that controls for any 4+ variables in all three categories above receives 2 stars
Table 4.
Prenatal depression and LBW/BW—18 non-significant associations in chronological order
| Nos. | References | Participants (details) | Study design, timing of assessment and measures | Control variables (NOS guidelines: 0-2 stars)a | GA | Primary results | Quality assessment (NOS 5-9 stars; Mean = 7.2) |
|---|---|---|---|---|---|---|---|
| 1. | Copper et al. [120] | N = 2,593 pregnant U.S. women; 63 % Black, 35 % Caucasian, 1 % Hispanic | National sample with multiple sites; depression assessed at 25-29 weeks gestation with Abbreviated Scale for the Assessment of Psychosocial Status in Pregnancy (incl. CESD) |
2 stars Medical: age Socio-demographic: race, marital status, government insurance status, education Behavioral: tobacco, alcohol, drug use during pregnancy Excluded: multiple pregnancies, pregnancy complications |
Nob | Depression was not significantly associated with LBW | 7 |
| 2. | Goldenberg et al. [83] | N = 1,491 pregnant U.S. low-income, women; 69 % Black, 31 % Caucasian | Prospective cohort study. Assessed depression at 24-26 weeks gestation with CESD |
2 stars Medical: Maternal BMI, height, hypertension and diabetes, infant sex Socio-demographic: race Behavioral: smoking, alcohol, drugs |
Noa | No significant associations with BW or LBW | 7 |
| 3. | Shiono et al. [141] | N = 1,150 pregnant U.S. women in Chicago and NYC; 30 % African American, 13 % Chinese, 13 % Dominican, 15 % Mexican, 11 % Puerto Rican, 19 % Caucasian | Cohort study with six sites in two regions; depression assessed at 16-28, 32 weeks with CES-D |
2 stars Medical: age, BMI Socio-demographic: ethnicity, marital status, education, poverty, insurance type Behavioral: smoking Excluded: women using medications for diabetes, heart disease, kidney disease or hypertension |
Noa | Depression not significantly associated with birth weight | 7 |
| 4. | Lundy et al. [142] | N = 63, USA 46 % Hispanic, 41 % African American, 13 % non-Hispanic White |
Case-control study with one-site; depression assessed during 3rd trimester (mean = 32.3 weeks gestation) with CES-D and DIS |
0 stars Medical: None Socio-demographic: None Behavioral: None |
No | No significant differences in BW between depressed and non-depressed mothers | 6 |
| 5. | Andersson et al. [86] | N = 1,465 pregnant women in Sweden | Cohort study with two sites. Depression assessed before ultrasound at 16-18 weeks gestation with PRIME-MD |
2 stars Medical: age, parity, 1st trimester BMI, chronic disease Socio-demographic: marital status, occupation Behavioral: smoking, oral tobacco use |
Nob | No significant differences in LBW rates between women with prenatal depressive disorders and healthy subjects | 9 |
| 6. | Berle et al. [119] | N = 680 pregnant women in Norway | National cohort study; depression assessed during 1st, 2nd and 3rd trimesters of pregnancy with HADS |
1 stara Medical: age Socio-demographic: education Behavioral: smoking, alcohol, psychotropic medication use aBecause ctrls only included in first step of analyses |
No | No significant differences in LBW rates between women who presented major depression and those that did not | 7 |
| 7. | Elsenbruch et al. [143] | N = 896 pregnant women in Germany | Cohort study; depression assessed in 1st trimester with ADS-K (German version of CES-D) |
2 stars Medical: age, BMI, chronic disease Socio-demographic: education, employment Behavioral: smoking |
No | Depression did not significantly predict BW | 7 |
| 8. | Xiong et al. [122] | N = 301 pregnant U.S. women in LA; 43.8 % non-hispanic White, 41.6 % Black | Regional cohort study with two sites; depression assessed once at any point in pregnancy with EPDS |
2 stars Medical: age, parity, LBW history Socio-demographic: education, race, marital status, family income Behavioral: smoking, alcohol use |
No | Depression not significantly associated with an increased LBW risk | 7 |
| 9. | Bae et al. [118] | N = 114 pregnant women in Seoul, Korea | Regional case-control study with one site; depression assessed during 1st, 2nd, 3rd trimesters with BDI; BDI <10: low depression, BDI >10: high depression |
0 stars Medical: age Socio-demographic: None Behavioral: annual alcohol use, frequency of coffee intake Excluded: multiple pregnancies |
No | No significant differences in BW between high and low depression groups | 5 |
| 10. | Benute et al. [94] | N = 326 pregnant women with a medical disorder in Sao Paulo, Brazil | Regional case-control study with one site; depression assessed at mean gestational age 28.2 weeks with PRIME-MD |
0 stars Medical: None Socio-demographic: None Behavioral: None |
No | No significant differences in BW between women who presented with depression and those who did not | 5 |
| 11. | Field et al. [69] | N = 911 pregnant U.S. women; 59 % Hispanic, 32 % Black, 9 % Caucasian | Regional case-control study with one site; depression assessed at 20 weeks gestation with CES-D; SCID used to categorize |
0 stars Medical: None Socio-demographic: None Behavioral: None |
? | No significant differences in BW between depressed and non-depressed mothers | 5 |
| 12. | Wang and Chen [123] | N = 431 pregnant women in Taiwan | Cohort study with multiple sites; depression assessed at 17-38 weeks gestation with EPDS |
0 stars Medical: None Socio-demographic: None Behavioral: None |
No | Depression not significantly associated with birth weight | 7 |
| 13. | Bodecs et al. [92] | N = 261 pregnant women in Hungary | Cohort study with multiple sites; depression assessed at enrollment at average of 8.13 weeks gestation with 9-item BDI |
2 stars Medical: maternal age, parity Socio-demographic: marital, educational and socioeconomic status Behavioral: smoking, alcohol, and vitamins |
No | Depression not significantly associated with BW | 8 |
| 14. | El Marroun et al. [82] | N = 7,696 pregnant women in the Netherlands; 52 % Dutch, 40 % non-Dutch/non-Western | Regional case-control study; depression assessed at mean gestational age 20.6 weeks with BSI |
2 stars Medical: age, enrollment BMI, obstetric information Socio-demographic: ethnicity, education Behavioral: smoking, alcohol, marijuana use Excluded: SSRI use before pregnancy, multiple pregnancies |
No | No significant differences in BW or LBW rates between mothers with depressive symptoms not using SSRIs, mothers using SSRIs, and mothers without depressive symptoms not using SSRIs | 8 |
| 15. | Ibanez et al. [84] | N = 1,719 pregnant women in France | Case-control study in two regions in France. Assessed at 24-28 weeks gestation with CES-D |
2 stars Medical: age, parity, pre-pregnancy BMI, infant sex, hypertension Socio-demographic: education Behavioral: smoking Excluded: multiple pregnancies, history of diabetes |
Nob | No significant differences in BW between women | 8 |
| 16. | Nylen et al. [97] | N = 211 pregnant U.S. women in IA 86 % married, 94 % Caucasian, 75 % working mothers Over half 58 % were primiparous |
Cohort study; depression assessed in 1st [104] or 2nd [131] trimester using the SCID-I |
2 stars Medical: age, previous pregnancy complications, medical condition (kidney disease, epilepsy, diabetes, hypertension, anemia, HIV or infectious disease, etc.) Socio-demographic: income, ethnic minority status, social support, number of children, planned pregnancy Behavioral: smoking Excluded: multiple pregnancies |
Yes | No significant main effects of depression on birth weight | 9 |
| 17. | Subramanian et al. [121] | N = 1,044 pregnant U.S. low income African American women in Washington, DC | Regional case-control intervention study; depression assessed at enrollment, 2nd trimester, 3rd trimester, and postpartum with BDI and HSCL-D |
2 stars Medical: age, previous birth outcomes, diabetes, hypertension Socio-demographic: education, marital status, employment, Medicaid/WIC status Behavioral: drug and alcohol use |
Nob | Depression not significantly associated with LBW or VLBW | 8 |
| 18. | Wisner et al. [143] | N = 238 pregnant U.S. women in OH and PA; 80 % Caucasian, 18 % African American, 2 % other | Cohort study with two sites in two regions; depression assessed 20, 30, 36 weeks gestation with the SCID |
2 stars Medical: age, exposure to FDA class D or X agents Socio-demographic: race Behavioral: diagnosed alcohol abuse, positive urine drug screens Excluded: multiple gestations, chronic diseases, psychosis, bipolar disorder |
Yes | No significant differences in birth weight between women classified into three groups: no SSRI/no depression, SSRI, MDD | 9 |
Control variables: NOS Star system allows for ratings of adequate controls: A study that controls for any 3+ variables from two categories (1) medical risk factors (e.g. maternal age, parity, previous PTB, gestational diabetes, chronic hypertension, infections, pre-pregnancy BMI; (2) sociodemographic factors (e.g. Race/ethnicity, education, employment, SES, marital status etc.) and (3) behavioral factors (e.g. Smoking, alcohol, drugs (incl. antidepressants), physical activity etc.) receives 1 star. A study that controls for any 4+ variables in all three categories above receives 2 stars
Study did include GA in some analyses or as part of another outcome (i.e. small for gestational age, intrauterine growth restriction), but did not control for GA in the relevant analyses
Quality Assessment of Included Studies
Studies were also evaluated for methodological quality by two authors using the Newcastle-Ottawa Scale for Quality Assessment [22]. The NOS guidelines judge each study on three broad predefined criteria, some of which require further specification for the specific review: (1) the selection of the study groups (0–4 stars possible); (2) the comparability of the groups (0–2 stars possible); and (3) the ascertainment of either the exposure or outcome of interest for case–control or cohort studies respectively (0–3 stars possible). Study ratings then range from 0 to 9 stars.
First, quality of selection refers to sample representativeness; selection and definition of control groups; and type of depression assessment. Second, quality of comparability refers to comparability of cases and controls on the basis of the design or analysis. For example, a study received one star for limiting the sample (e.g. excluding smokers), treating a key variable as an effect measure modifier (e.g. race/ethnicity), or statistically controlling for three or more key variables from at least two categories out of three. The categories of possible control variables were: (1) Medical risk factors (maternal age, parity, previous PTB, etc.); (2) Socio-demographic factors (race/ethnicity, education, etc.); and (3) Behavioral factors (smoking, alcohol, etc.). A study received one additional star if it controlled for at least one variable from each category and a total of four or more variables. Finally, quality of outcome refers to whether information on birth outcome variables were obtained from medical records or patient self report; when it was obtained; and the degree of follow-up of cases for birth outcomes data. For example, stars were given for use of medical records, birth weight obtained by scale measurements at time of birth, and better than 80 % follow up with description of those lost.
Disagreement between authors involved differences in interpretations of methods or results with consensus easily achieved in all cases through discussion. Studies with scores ranging from 1 to 3 were considered to be of low quality, those with scores of 4–6 of moderate quality, and studies with scores from 7 to 9 of high quality. Finally, although the NOS does not take sample size into account for quality ratings, we provide sample size information for the benefit of readers.
Definition of Exposure Variable
We included studies of diagnosed depression during pregnancy using criteria from the American Psychiatric Association's (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM) or International Statistical Classification of Diseases (ICD-9 or ICD-10), both of which are widely used classification systems for mental disorders. Validated depression screening tools used in this literature included the Center for Epidemiological Studies Depression Scale (CES-D) [73], Beck Depression Inventory (BDI) [74], Edinburgh Postnatal Depression Scale (EPDS) [75], General Health Questionnaire (GHQ) [76], Hospital Anxiety and Depression Scale—Subset D (HADS-D) [77], and the Brief Symptom Inventory (BSI) [78]. Two studies using a brief version of one screening tool (SCL-5), in which a majority of items address anxiety, were excluded [52, 53]. Although the EPDS and GHQ also include anxiety items, the majority of items are not anxiety-related and these screening tools are commonly used as to assess prenatal depression, thus they were not excluded.
Definition of Outcome Variables
PTB was defined according to convention as birth before the 37th week of gestation. Approximately half of PTBs can be categorized as the result of spontaneous preterm labor (SPTB), 30 % result from premature rupture of the membranes (PROM), and 20 % due to medically-induced births which have not been proposed to be associated with maternal depression and no literature on this category exists [79]. GA was defined as weeks of gestation at time of delivery and BW in grams. PTB and GA were determined by various methods including calculation from last menstrual period (LMP), ultrasound, and size by dates. Conventional definitions of LBW and SGA were used (2,500 g or less and weight below the 10th percentile for GA).
The most common definition of SGA refers to a weight below the 10th percentile for gestational age [80]. However, this definition does not make a distinction between infants constitutionally small versus growth-restricted, although a baby can be one or both. IUGR is defined as a condition in the third trimester when the baby is not gaining adequate weight. Fetal growth restriction (FGR), a synonym for IUGR, is the term used to designate a fetus that has not reached its growth potential because of genetic or environmental factors; FGR results in the birth of an infant who is small for gestational age (SGA) [81].
Results
A total of 95 studies published between 1977 and 2013 met inclusion criteria. Among these were 76 studies on PTB/GA and LBW/BW, including a total of 83 distinct findings that were extracted. Another 25 findings in 19 published articles were identified on prenatal depression in relation to SGA or IUGR. However, this set of studies was of substantially lower methodological quality compared to studies on PTB/LBW. For this reason, and to narrow the scope of the review, we excluded SGA and IUGR from our analysis (see Appendix S1), concentrating on the remaining 76 studies which are outlined in Tables 1, 2, 3 and 4.
Design
A total of 63 of the 76 articles were observational studies and 13 were case–control design. As can be seen in Tables 1, 2, 3 and 4, many of the investigations fulfilled criteria for moderate to high methodological quality (median NOS score = 7, range of 5–9). Studies with lower scores typically did not treat confounding variables extensively and/or had unclear information regarding attrition or depression assessment. Results were evaluated as significant if results of the key tests were p < 0.05.
PTB and GA Outcomes
Fifty sets of findings related to PTB and/or GA were identified from 47 published studies. Tables 1 and 2 list the depression measures, timing of assessments, summary of findings, and NOS ratings for each study. Thirty-six of 50 reports targeted PTB as the outcome and exactly one-quarter of the 36 (n = 9) report statistically significant associations with prenatal depression and PTB. For example, odds ratios range from 1.06 to 3.3 as can be seen in Table 1. Of the 14 studies on GA, three reported statistically significant associations between prenatal depression whereas a majority did not. Additionally, four studies with high methodological quality [82–85] analyzed both PTB and GA, two of which were case–control studies and two were prospective observational studies. Notably, none reported significant associations with prenatal depression. Because inconsistencies in previous reviews may be due to methodological differences, further results of the systematic review are organized into sections regarding the specific features of concern.
| Important features: the following design elements from the studies are systematically reviewed in each section below |
| 1. Sample size |
| 2. Spontaneous PTB |
| 3. Control variables (socio-demographic, medical, psychological) |
| 4. Timing of depression assessment |
| 5. Diagnostics versus self-reported symptoms |
Sample Size
Although it is important to consider, the NOS does not take sample size into account. The minimum sample size based on simple power analyses for a test of associations of depression and GA or BW would be about 400 to detect a small effect size with a minimum of 500 for analyses with multiple predictors. We therefore refer for our purposes to sample sizes <500 as ‘small’ and >500 as ‘large.’ Of the nine reports of significant associations between PTB and depression, a total of eight had samples over 500 (NOS scores from 5 to 8). Odds ratios ranged from 1.3 to 1.96. Similarly, the large majority of the 27 studies reporting null findings had samples over 500 (20 of 27; NOS scores from 6 to 9). Overall, it appears that studies with large samples and better NOS ratings were more likely to report non-significant results. For example, a methodologically rigorous antidepressant study with the largest sample (n = 228,876) found that second trimester anti-depressant use, not depression diagnosis, predicted PTB [23]. The authors, however, did not conduct separate analyses for SPTB. Two additional studies with large samples and strong methodological quality [24, 86] did address SPTB, measured depressive symptoms using standardized methods, and conducted well-controlled analyses. However, neither found significant associations between prenatal depression and SPTB.
Of the three studies reporting significant associations between prenatal depression and GA, two had sample sizes less than 500. One additional high quality study [87] had a larger sample of 4,044 women. When adjusted for potential confounders, the association between major depressive symptoms (CES-D >23) and GA remained significant with a small effect size (−0.2 weeks) but there were no effects for PTB [87]. Of the 11 non-significant results for prenatal depression and GA (see Tables 1, 2), most had relatively small samples. The largest sample of 7,697 was higher rated on quality, used the BSI screening tool, but yielded null results for both GA and PTB [82].
SPTB
Of 13 published results, ten did not find an association between prenatal depression and SPTB (NOS scores from 6 to 9). Perkin et al. [88], for instance, tested separate models for five different obstetric outcomes in a large sample of 1,515 pregnant women, and found no statistically signifi-cant associations between prenatal depression and either spontaneous or medically induced PTB.
Well-Controlled Studies
Of the 36 PTB reports, 26 included adequate or good control for known PTB risk factors. Of these, only 23 % (n = 6) found significant results whereas the majority (77 %, n = 20) did not. For example, Kramer et al. [89] controlled for 14 medical, socio-demographic and behavioral factors, and excluded women with major medical problems. They found that only pregnancy-specific anxiety independently predicted SPTB. The adjusted odds ratio for depression (CES-D ≥16) was 1.4 (95 % CI 1.0, 2.1), whereas the adjusted odds ratio was 1.8 (95 % CI 1.3, 2.4) for pregnancy-specific anxiety. Although pregnancy-specific anxiety, perception of high pregnancy risk, and depression remained significantly associated with spontaneous PTB in separate multiple logistic regression analyses, only pregnancy-related anxiety retained its association in logistic models containing all 3 measures [89].
Of the 14 reports on prenatal depression and GA, eight included adequate controls. Of those eight, only two found significant associations, whereas six did not. Notably, in one of the rare studies to examine moderators, the authors reported a significant association of prenatal depression with fetal growth. Although they did not find a statistically significant association between prenatal depression and GA, they did find a significant association of prenatal depression and fetal growth in trimester-specific regression analyses in a subsample of over 200 women from lower occupational status households [90].
Timing of Depression Assessment
Of the 50 PTB/GA reports, a majority (n = 37) assessed depression during the second and/or third trimesters, and another 13 assessed depression more than once including the first trimester. Of the 13 with early pregnancy data, only three compared trimesters. Of these, one found that first trimester depression was associated significantly with PTB [91] and two did not [92, 93]. Of the remaining ten that did not compare trimesters, most found that prenatal depression at an unspecified time in first to third trimester was not significantly associated with PTB/GA.
Diagnosed Depression
Of the 36 PTB reports, seven examined depression diagnoses. Notably, none of these studies found that diagnosed depression significantly predicted PTB [23, 24, 26, 85, 86, 94, 95]. Of the 14 reports on GA, six included depression diagnoses. Two of the 6 found that clinically diagnosed prenatal depression significantly predicted GA, although both had relatively small samples and one lacked adequate controls [96, 97]. Of the four that reported null results [85, 98–100], three had small samples (<100), and only one adequately controlled for covariates.
Summary of PTB/GA Studies
In sum, individual PTB or GA studies that met most of the important methodological criteria were rare. Only two investigations with strong methodologies (one on PTB and one on GA) found significant results of depression, and another two PTB articles with strong methodologies reported no significant results. Thus, taking into account the methodological quality of studies, research on depression and PTB/GA is inconclusive at best.
LBW and BW Outcomes
Thirty-three published findings related to LBW and/or BW were identified from 29 studies (see Tables 3, 4). Fifteen of 33 reports targeted LBW of which about half (53 %, n = 8 of 15) found that prenatal depression significantly predicted LBW. For example, odds ratios range from 1.4 to 3.6, as can be seen in Table 3. Another 18 targeted BW in grams, and of these, one-third (n = 6 of 18) reported statistically significant inverse associations between prenatal depression and BW. Additionally, five of the 29 LBW studies reported results for both BW and LBW. Of these, three studies found that depression was significantly associated with both LBW and BW [101–103], whereas two studies found no effects on either variable [82, 83].
Sample Size
A majority of the studies on depression and LBW had larger samples sizes. Five of the eight studies that reported that prenatal depression significantly predicted LBW and six of the seven studies that did not find significant associations had samples over 500. The largest sample was composed of 14,175 racially-diverse pregnant women and results revealed significant associations between prenatal depression (measured by the EPDS) and incidence of LBW [104]. Although sample size was a major strength of this study, there were also weaknesses including the lack of key controls, namely pre-pregnancy BMI, antidepressant use, smoking and substance use [105].
Well-Controlled Studies
The majority of the LBW reports (n = 11 of 15) included adequate controls for risk factors, yet only four of the 11 obtained significant results. The two highest quality studies, however, did report that women with prenatal depression were more likely to have LBW infants, and both involved depression diagnoses and adequately controlled for confounders [95, 103]. For example, in a sample of 1,100 racially diverse pregnant women, Rogal et al. [95] reported that women diagnosed with minor depression were more likely to give birth to an LBW infant (OR 1.82, 95 % CI 1.01, 3.29). Of the 18 studies on continuous BW scores, 8 included adequate controls, but only two of eight found significant associations. Furthermore, eighteen studies predicted both LBW/BW and PTB/GA outcomes and were therefore capable of statistically controlling for gestational age in testing LBW. However, only 4 of the 18 studies did so. Two of the four were of highest quality (NOS = 9), [97, 106] but neither found that prenatal depression was associated with BW when controlling for GA. The other two studies that controlled for GA [100, 101] reported that prenatal depression significantly predicted both BW and LBW and, of note, they both used a more racially diverse sample. Earnshaw et al. [101] had the largest sample of the four studies (n = 420), but did not control for any other important risk factors (NOS = 6). Although Diego et al. [100] was high quality (NOS = 8), their sample was quite small (n = 79) and was not truly representative of the average pregnant community-dwelling resident. Unfortunately, close examination of all four studies does not clarify whether well-controlled studies with high quality methods are likely to find effects.
Timing of Depression Assessment
Of the 33 LBW/BW reports, a large majority (n = 25) assessed depression during the second and/or third trimester/s. Less than a third of these (n = 9 of 25) found significant results. Two more studies (of the 33) assessed depression at an unspecified time over all three trimesters and found that prenatal depression significantly predicted LBW [95, 107]. For example, Liu et al. [107] found that compared to women with no depressed mood (CES-D), infants born to women with severe depressed mood were more likely to be LBW (OR 3.6, 95 % CI 1.1,11.4). There were no effects, however, of moderate depressed mood. Furthermore, they found that this association was limited to infants born to African American women (OR 7.2, 95 % CI 1.8, 28.7) and was more pronounced in female infants (OR 7.5, 95 % CI 1.5, 38.9) [107]. The remaining 6 of the 33 studies with first trimester assessments reported no significant results.
Diagnosed Depression
Of the 15 LBW reports, only three involved diagnosed depression but two of three found that prenatal depression predicted incidence of LBW [95, 103], whereas the other did not. Another seven of 18 studies examined diagnosed depression and infant BW continuously, and three of the seven found significant associations between prenatal depression and BW [96, 100, 101] whereas four did not (see Table 3, 4).
Summary of LBW/BW Studies
Approximately half of the LBW and BW studies reported significant associations or odds ratios with prenatal depression. Of the four most precise and highest quality LBW studies controlling for GA, half report significant effects. However, on the whole, very few met most of the desirable methodological criteria. Indeed, only one LBW article had excellent methodology (large sample size and NOS = 9) and it reported no significant effects.
Discussion
Main Findings
Overall, in this systematic review, there were more published reports on PTB/GA than on LBW/BW. After dissection by study features, a clear pattern emerged showing that prenatal depression is rarely associated with PTB or GA in larger, well-controlled studies. Specifically, 75 % of published PTB findings from 1977 to 2013 did not obtain statistically significant associations with prenatal depression, no matter how it was measured. Significant associations were least likely for SPTB or for clinically-diagnosed depression. Many studies used relatively short screening tools to evaluate levels of depressive symptoms and cutoff scores for identifying clinically significant depressive symptoms. Although this practice is common, it does not equate with a clinical diagnosis by a structured interview. It is also important to note that screening tools that include many somatic symptoms characteristic of depression may produce artificially high scores in pregnancy due to somatic symptoms typical of pregnancy such as fatigue. Screening tools designed for the pregnancy period (like the EPDS) do not include such symptoms.
In contrast to the literature on PTB and GA, the LBW/BW literature is characterized by fewer studies as a whole with “small” sample sizes, less well-controlled analyses, and fewer studies using validated clinical interviews. Nonetheless, we found that about half (53 %) of published LBW findings reported statistically significant associations with prenatal depression. Additionally, of the four most precise and highest quality LBW studies controlling for GA, again half report significant effects. This makes it hard to know if the “glass is half full or half empty” but it provides a clear sense of what evidence we now have and of what quality. With few exceptions, researchers have failed to control for time of delivery (GA) when predicting LBW which confounds length of gestation with fetal growth rate. The advantage of analyses that control for gestational age in testing LBW is to clarify mechanisms. If a baby is LBW and it is not due to shorter gestational length, then slower or impaired fetal growth was likely to be involved. Depressive symptoms in pregnancy were associated with birth weight controlling for timing of delivery in two of the four methodologically strong studies, but much less often with GA or PTB (25 % of studies). Furthermore, when examined by race/ethnicity of the participants, the results become more consistent for depression predicting LBW/BW. Specifically, three studies with samples of mostly non-Caucasian women all found significant inverse associations of prenatal depression and LBW/BW and no significant associations for PTB/GA [95, 100, 102].
Interpretation
In contrast to some prior reviews, we used systematic methods (i.e. PRISMA guidelines and NOS ratings) and covered a longer time period and more recent published studies. This systematic review also excluded all studies which used retrospective assessment of prenatal depression (n = 20), studies using measures of depression that were clearly confounded with anxiety or stress, and studies that did not use a reliable or valid measure of depression. By excluding the large number of retrospective studies, this review helps to clarify inconsistencies in the literature further. We also refined our review by excluding studies that combined unipolar with bipolar depression (or other psychiatric diagnoses), and that grouped depression along with other “high risk” symptoms and behaviors. Thus, this review focused specifically on the very best evidence available, and finds that the evidence slightly favors an association between prenatal depression and LBW, and is much less clear for spontaneous PTB, let alone SGA which did not have as many, or as strong, a set of studies to review.
Among adequately controlled analyses reporting significant associations between prenatal depression and PTB, many were lower in methodological quality due to smaller sample size and lack of attention to whether the onset of labor was spontaneous or not. Additionally, the timing of depression diagnosis or screening differed between studies. We observed that studies including depression assessment during the first trimester resulted in fewer significant adverse outcomes (PTB or LBW) than depression assessed at later times in pregnancy, which may suggest that enduring or mid to late pregnancy depression has the greatest effects on fetal development. Vulnerable windows across gestation for adverse effects of prenatal depression may indicate that different mechanisms are operating at different times [108]. Mechanisms whereby depression in mid to late pregnancy affects fetal growth and ultimately BW are likely to involve health behaviors such as diet or physical activity [109]. Those affecting PTB via anxiety are frequently attributed to changes in the hypothalamic– pituitary–adrenal (HPA) axis [110]. Inflammatory mechanisms may also be involved in both pathways as these mechanisms interact with one another and are not independent. These issues require further research.
Several recent reviews and meta-analyses have mentioned that untreated prenatal depression may have more detrimental effects on birth outcomes than antidepressant use [16] whereas others found antidepressants to be harmful [18]. Some of the most methodologically rigorous studies that we reviewed (NOS = 9) were antidepressant studies, most of which found that anti-depressant use—not depression—was associated with PTB e.g. [23, 24]. This fact underlines the importance of attending to medication use in any study of depression or depressive symptoms in pregnancy.
Strengths, Limitations and Research Directions
A strength of this systematic review is full attention to the methodological quality and characteristics of research designs. Because a majority of studies reported null findings, we are not as concerned with publication bias but it cannot be ruled out. Additionally, the studies reviewed here included women from countries other than North America and Europe and women of many races and ethnicities other than Caucasian. Some limitations include the paucity of randomized controlled trials (RCT) in this literature. Although several RCTs attempting to address prenatal depression have been published, only one recent study focused on preventing adverse birth outcomes by reducing depressive symptoms [111]. To do so, this study provided yoga and massage therapies and found decreases in depression and anxiety and longer gestational lengths and higher birth weight in the therapy groups than the no intervention control group. Therefore, future studies applying psychosocial and complementary treatments of depression to reduce PTB and LBW might clarify the picture if designed with state of the art RCT methods. Finally, an updated meta-analysis would be worthwhile as this literature continues to grow.
Implications for Practice
On the basis of the evidence reviewed here, depression screening with instruments that have been validated for use during pregnancy is merited at multiple time points throughout pregnancy—not just in the first trimester. Such a practice may enable detection and timely treatment to potentially reduce risk for adverse birth outcomes and certainly reduce risk of postpartum depression. Non-pharmacological treatments for depression, such as cognitive behavioral therapy [112, 113] and complementary treatments [111] can produce symptom relief with minimal side-effects, although pharmacological treatments should not be ruled out where evidence suggests they are safe and if prescribed and monitored carefully. However, if referral and treatment systems are not in place and well-functioning, such screening is potentially unethical [114]. In the future, high quality prenatal care systems worldwide will develop the capacity for depression risk assessment and treatment in the context of monitoring pregnancies to successful birth.
Conclusion
In conclusion, the evidence on depression and birth outcomes is equivocal despite considerable attention to the topic. When considering only the highest quality studies, prenatal depression was implicated slightly more as a risk factor for LBW/BW than in spontaneous early labor and delivery, length of gestation, and PTB, and especially in racially diverse samples. In fact, other psychosocial factors such as stress and pregnancy anxiety have been documented more consistently as contributors in the complex etiology of PTB [110]. Of note, depression, anxiety, and stress are not synonymous phenomena and cannot be treated as such by researchers. Indeed, stress is usually defined in the literature in ways that are quite distinct from definitions of depression or anxiety [115, 116]. Furthermore, depressive and anxiety symptoms can occur independently of stress exposures, although they are known to be exacerbated by stressors. For example, in the stress diathesis model, high levels of stressors such as major negative life events are posited to contribute to the onset of affective disorders [117]. Also, the term “distress” is often confused with stress but it refers to negative affect in general, including anxiety, depression, and other negative mood states in the literature, and not to stress per se. Finally, the symptoms of anxiety and depression are not measured in the same ways as stress. Therefore, we suggest that future studies should be designed specifically to examine the links between prenatal depression and anxiety (distinct from stress) and adverse birth outcomes.
When studying depression, which was the focus of this review, future work must include validated screening tools for prenatal depression—not retrospectively assessed symptoms and not instruments designed to study depression in the postpartum period—and should control in the research design for the timing of depression assessments during pregnancy. Researchers are also advised to collect complete medical histories for preconception, prenatal medical risks, and obtain full information on health behaviors associated with risk for PTB or LBW. We recommend sampling ethnically diverse samples of at least 500 women in such studies. Finally, the most useful studies will control for gestational age when predicting LBW, and distinguish SPTB from medically-induced PTB when this is the primary outcome. The next generation of studies on prenatal depression and birth can help inform practice with respect to screening and interventions that are designed to increase the quality of life in pregnant women suffering with depression, and perhaps may help to reduce the likelihood of adverse birth outcomes and the effects on offspring.
Supplementary Material
Acknowledgments
The authors wish to thank Lisa Federer, MLIS, MA, AHIP, Research Informationist at the UCLA Biomedical Library, for assistance with the literature search. We also thank Calvin Hobel, M.D., Cedars Sinai Hospital, and Christine Guardino, Ph.D., for their comments and suggestions on a draft of this paper. Finally, we thank Jessica Pham and Kate Pearson, for administrative assistance. This research was supported by training grant fellowships from the National Institutes of Mental Health (T32MHI5750) to the first and second authors.
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s10995-014-1637-2) contains supplementary material, which is available to authorized users.
Conflict of interest
The authors have no conflict of interest to report.
Ethical standard
This study involved published data, and so did not require ethics approval.
References
- 1.Blencowe H, Cousens S, Oestergaard M, Chou D, Moller AB, Narwal R, et al. National, regional and worldwide estimates of preterm birth in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. The Lancet. 2012;379(9832):2162–2170. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 2.Low Birth Weight (LBW) by Rural/Urban Residence Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2009 http://mchb.hrsa.gov/chusa12/rud/downloads/pdf/lbwpb.pdf. [Google Scholar]
- 3.Institute of Medicine . Preterm birth: Causes, consequences, and prevention. National Academies Press; Washington, DC: 2007. [PubMed] [Google Scholar]
- 4.Muglia LJ, Katz M. The enigma of spontaneous preterm birth. New England Journal of Medicine. 2010;362(6):529–535. doi: 10.1056/NEJMra0904308. [DOI] [PubMed] [Google Scholar]
- 5.Behrman RE, Butler AS, editors. Preterm birth: Causes, consequences, and prevention. National Academies Press; Washington, DC: 2006. [PubMed] [Google Scholar]
- 6.Dunkel Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- 7.Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: Systematic review. Obstetrics and Gynecology. 2004;103(4):698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- 8.Andersson L, Sundström-Poromaa I, Bixo M, Wulff M, Bondestam K, Åström M. Point prevalence of psychiatric disorders during the second trimester of pregnancy: A population-based study. American Journal of Obstetrics and Gynecology. 2003;189(1):148–154. doi: 10.1067/mob.2003.336. [DOI] [PubMed] [Google Scholar]
- 9.Lee AM, Lam SK, Lau SMSM, Chong CSY, Chui HW, Fong DYT. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstetrics and Gynecology. 2007;110(5):1102–1112. doi: 10.1097/01.AOG.0000287065.59491.70. [DOI] [PubMed] [Google Scholar]
- 10.McDonald SW, Lyon AW, Benzies KM, McNeil DA, Lye SJ, Dolan SM, Tough SC. The All Our Babies pregnancy cohort: Design, methods, and participant characteristics. BMC Pregnancy and Childbirth. 2013;13(Suppl 1):S2. doi: 10.1186/1471-2393-13-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gotlib IH, Hammen CL, editors. Handbook of depression. Guilford Press; New York: 2008. [Google Scholar]
- 12.Zuckerman B, Amaro H, Bauchner H, Cabral H. Depressive symptoms during pregnancy: Relationship to poor health behaviors. American Journal of Obstetrics and Gynecology. 1989;160:1107–1111. doi: 10.1016/0002-9378(89)90170-1. [DOI] [PubMed] [Google Scholar]
- 13.Burt VK, Stein K. Epidemiology of depression throughout the female life cycle. Journal of Clinical Psychiatry. 2002;63:9–15. [PubMed] [Google Scholar]
- 14.Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Archives of General Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W. Depression and anxiety during pregnancy: A risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. Journal of Maternal-Fetal and Neonatal Medicine. 2007;20(3):189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- 16.Bonari L, Pinto N, Ahn E, Einarson A, Steiner M, Koren G. Perinatal risks of untreated depression during pregnancy. Canadian Journal Psychiatry. 2004;49(11):726–735. doi: 10.1177/070674370404901103. [DOI] [PubMed] [Google Scholar]
- 17.Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: A review. Archives of Women's Mental Health. 2012;15(1):1–14. doi: 10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- 18.Ross LE, Grigoriadis S, Mamisashvili L, VonderPorten EH, Roerecke M, Rehm J, et al. Selected pregnancy and delivery outcomes after exposure to antidepressant medication: A systematic review and meta-analysis. Outcomes after antidepressant use in pregnancy. JAMA Psychiatry. 2013;70(4):436–443. doi: 10.1001/jamapsychiatry.2013.684. [DOI] [PubMed] [Google Scholar]
- 19.Szegda K, Markenson G, Bertone-Johnson ER, Chasan-Taber L. Depression during pregnancy: A risk factor for adverse neonatal outcomes? A critical review of the literature. Journal of Maternal-Fetal and Neonatal Medicine. 2014;27(9):960–967. doi: 10.3109/14767058.2013.845157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stewart RC. Maternal depression and infant growth— A review of recent evidence. Maternal & Child Nutrition. 2007;3(2):94–107. doi: 10.1111/j.1740-8709.2007.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 22.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. [September 3, 2013];The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Retrieved from http://www.ohri.ca/programs/clinical_epide miology/oxford.htm.
- 23.Hayes RM, Wu P, Shelton RC, Cooper WO, Dupont WD, Mitchel E, et al. Maternal antidepressant use and adverse outcomes: A cohort study of 228,876 pregnancies. American Journal of Obstetrics Gynecology. 2012;207(1):49.e1–49.e9. doi: 10.1016/j.ajog.2012.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yonkers KA, Norwitz ER, Smith MV, Lockwood CJ, Gotman N, Luchansky E, et al. Depression and serotonin reuptake inhibitor treatment as risk factors for preterm birth. Epidemiology. 2012;23(5):677–685. doi: 10.1097/EDE.0b013e31825838e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Engel SM, Berkowitz GS, Wolff MS, Yehuda R. Psychological trauma associated with the World Trade Center attacks and its effect on pregnancy outcome. Pediatric and Perinatal Epidemiology. 2005;19(5):334–341. doi: 10.1111/j.1365-3016.2005.00676.x. [DOI] [PubMed] [Google Scholar]
- 26.Okun ML, Luther JF, Wisniewski SR, Sit D, Prairie BA, Wisner KL. Disturbed sleep, a novel risk factor for preterm birth? Journal of Women's Health. 2012;21(1):54–60. doi: 10.1089/jwh.2010.2670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker L, Kim M. Psychosocial thriving during late pregnancy: Relationship to ethnicity, gestational weight gain, and birth weight. Journal of Obstetric Gynecology Neonatal Nursing. 2002;31:263–274. doi: 10.1111/j.1552-6909.2002.tb00048.x. [DOI] [PubMed] [Google Scholar]
- 28.Borders AEB, Grobman W, Amsden L, Holl J. Chronic stress and low birth weight neonates in a low-income population of women. Obstetrics and Gynecology. 2007;109:331–338. doi: 10.1097/01.AOG.0000250535.97920.b5. [DOI] [PubMed] [Google Scholar]
- 29.Sanchez SE, Puente GC, Atencio G, Qiu C, Yanez D, Gelaye B, et al. Risk of spontaneous preterm birth in relation to maternal depressive, anxiety, and stress symptoms. Journal of Reproductive Medicine. 2013;58(1):25–33. [PMC free article] [PubMed] [Google Scholar]
- 30.Uguz F, Sahingoz M, Sonmez EO, Karsidag C, Yuksel G, Annagur BB, et al. The effects of maternal major depression, generalized anxiety disorder, and panic disorder on birth weight and gestational age: A comparative study. Journal of Psychosomatic Research. 2013;75(1):87–89. doi: 10.1016/j.jpsychores.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 31.Fransson E, Dubicke A, Bystrom B, Ekman-Ordeberg G, Hjelmstedt A, Lekander M. Negative emotions and cytokines in maternal and cord serum at preterm birth. American Journal of Reproductive Immunology. 2012;67(6):506–514. doi: 10.1111/j.1600-0897.2011.01081.x. [DOI] [PubMed] [Google Scholar]
- 32.Urquia ML, O'Campo PJ, Heaman MI, Janssen PA, Thiessen KR. Experiences of violence before and during pregnancy and adverse pregnancy outcomes: An analysis of the Canadian Maternity Experiences Survey. BMC Pregnancy and Childbirth. 2011;11:42. doi: 10.1186/1471-2393-11-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen CH, Lin HC. Prenatal care and adverse pregnancy outcomes among women with depression: A nationwide population-based study. Canadian Journal of Psychiatry. 2011;56(5):273–280. doi: 10.1177/070674371105600506. [DOI] [PubMed] [Google Scholar]
- 34.Gudmundsson P, Andersson S, Gustafson D, Waern M, Ostling S, Hallstrom T, Hulthen L. Depression in Swedish women: Relationship to factors at birth. European Journal of Epidemiology. 2011;26(1):55–60. doi: 10.1007/s10654-010-9508-7. [DOI] [PubMed] [Google Scholar]
- 35.Smith MV, Shao L, Howell H, Lin H, Yonkers KA. Perinatal depression and birth outcomes in a Healthy Start project. Maternal Child Health Journal. 2011;15(3):401–409. doi: 10.1007/s10995-010-0595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Misra D, Strobino D, Trabert B. Effects of social and psychosocial factors on risk of preterm birth in black women. Pediatric and Perinatal Epidemiology. 2010;24(6):546–554. doi: 10.1111/j.1365-3016.2010.01148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Phillips GS, Wise LA, Rich-Edwards JW, Stampfer MJ, Rosenberg L. Prepregnancy depressive symptoms and preterm birth in the Black Women's Health Study. Annals of Epidemiology. 2010;20(1):8–15. doi: 10.1016/j.annepidem.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferri CP, Mitsuhiro SS, Barros MC, Chalem E, Guinsburg R, Patel V, et al. The impact of maternal experience of violence and common mental disorders on neonatal outcomes: A survey of adolescent mothers in Sao Paulo. 1. Vol. 7. BMC Public Health; Brazil: 2007. p. 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black–White differences in preterm and low-birthweight deliveries: The CARDIA Study. American Journal of Public Health. 2004;94(12):2125–2131. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Walker LO, Kim M. Psychosocial thriving during late pregnancy: Relationship to ethnicity, gestational weight gain, and birth weight. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2002;31(3):263–274. doi: 10.1111/j.1552-6909.2002.tb00048.x. [DOI] [PubMed] [Google Scholar]
- 41.O'Callaghan MJ, Harvey JM, Tudehope DI, Gray PH. Aetiology and classification of small for gestational age infants. Journal of Pediatrics and Child Health. 1997;33(3):213–218. doi: 10.1111/j.1440-1754.1997.tb01582.x. [DOI] [PubMed] [Google Scholar]
- 42.Gungor I, Oskay U, Beji NK. Biopsychosocial risk factors for preterm birth and postpartum emotional well-being: A case–control study on Turkish women without chronic illnesses. Journal of Clinical Nursing. 2011;20(5–6):653–665. doi: 10.1111/j.1365-2702.2010.03532.x. [DOI] [PubMed] [Google Scholar]
- 43.Bansil P, Kuklina EV, Meikle SF, Posner SF, Kourtis AP, Ellington SR, et al. Maternal and fetal outcomes among women with depression. Journal of Women's Health. 2010;19(2):329–334. doi: 10.1089/jwh.2009.1387. [DOI] [PubMed] [Google Scholar]
- 44.Miceli PJ, Goeke-Morey MC, Whitman TL, Kolberg KS, Miller-Loncar C, White RD. Brief report: Birth status, medical complications, and social environment: Individual differences in development of preterm, very low birth weight infants. Journal of Pediatric Psychology. 2000;25(5):353–358. doi: 10.1093/jpepsy/25.5.353. [DOI] [PubMed] [Google Scholar]
- 45.Turner RJ, Grindstaff CF, Phillips N. Social support and outcome in teenage pregnancy. Journal of Health and Social Behavior. 1990;31:43–57. [PubMed] [Google Scholar]
- 46.Gavin AR, Holzman C, Siefert K, Tian Y. Maternal depressive symptoms, depression, and psychiatric medication use in relation to risk of preterm delivery. Women's Health Issues. 2009;19(5):325–334. doi: 10.1016/j.whi.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Heaman M, Kingston D, Chalmers B, Sauve R, Lee L, Young D. Risk factors for preterm birth and small-forgestational-age births among Canadian women. Pediatric Peri-natal Epidemiology. 2013;27(1):54–61. doi: 10.1111/ppe.12016. [DOI] [PubMed] [Google Scholar]
- 48.Cripe SM, Frederick IO, Qiu C, Williams MA. Risk of preterm delivery and hypertensive disorders of pregnancy in relation to maternal co-morbid mood and migraine disorders during pregnancy. Paediatric Perinatal Epidemiology. 2011;25(2):116–123. doi: 10.1111/j.1365-3016.2010.01182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.El-Mohandes AA, Kiely M, Gantz MG, El-Khorazaty MN. Very preterm birth is reduced in women receiving an integrated behavioral intervention: A randomized controlled trial. Maternal Child Health Journal. 2011;15(1):19–28. doi: 10.1007/s10995-009-0557-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C. Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data. Archives of General Psychiatry. 2006;63(8):898. doi: 10.1001/archpsyc.63.8.898. [DOI] [PubMed] [Google Scholar]
- 51.Jesse DE, Seaver W, Wallace DC. Maternal psychosocial risks predict preterm birth in a group of women from Appalachia. Journal of Midwifery & Women's Health. 2003;19(3):191–202. doi: 10.1016/s0266-6138(03)00031-7. [DOI] [PubMed] [Google Scholar]
- 52.Kiely M, El-Mohandes AA, Gantz MG, Chowdhury D, Thornberry JS, El-Khorazaty MN. Understandingthe association of biomedical, psychosocial and behavioral risks with adverse pregnancy outcomes among African-Americans in Washington, DC. Maternal Child Health Journal. 2011;15(1):S85–S95. doi: 10.1007/s10995-011-0856-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nordeng H, van Gelder MM, Spigset O, Koren G, Ein-arson A, Eberhard-Gran M. Pregnancy outcome after exposure to antidepressants and the role of maternal depression: Results from the Norwegian Mother and Child Cohort Study. Journal of Clinical Psychopharmacology. 2012;32(2):186–194. doi: 10.1097/JCP.0b013e3182490eaf. [DOI] [PubMed] [Google Scholar]
- 54.Gonzalez-Calvo J, Jackson J, Hansford C, Woodman C. Psychosocial factors and birth outcome: African American women in case management. Journal of Health Care Poor Underserved. 1998;9:395–419. doi: 10.1353/hpu.2010.0409. [DOI] [PubMed] [Google Scholar]
- 55.Hodgkinson S, Colantuoni E, Roberts D, et al. Depressive symptoms and birth outcomes among pregnant teenagers. Journal of Pediatric Adolescent Gynecology. 2010;23:16–22. doi: 10.1016/j.jpag.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Klieger-Grossmann C, Weitzner B, Panchaud A, Pistelli A, Einarson T, Koren G, Einarson A. Pregnancy outcomes following use of escitalopram: A prospective comparative cohort study. Journal of Clinical Pharmacology. 2012;52(5):766–770. doi: 10.1177/0091270011405524. [DOI] [PubMed] [Google Scholar]
- 57.Sit D, Perel JM, Wisniewski SR, Helsel JC, Luther JF, Wisner KL. Mother–infant antidepressant levels, maternal depression and perinatal events. The Journal of Clinical Psychiatry. 2011;72(7):994. doi: 10.4088/JCP.10m06461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Latendresse G, Ruiz RJ. Maternal corticotropin-releasing hormone and the use of selective serotonin reuptake inhibitors independently predict the occurrence of preterm birth. Journal of Midwifery & Women's Health. 2011;56(2):118–126. doi: 10.1111/j.1542-2011.2010.00023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Loomans EM, Van Dijk AE, Vrijkotte TG, van Eijsden M, Stronks K, Gemke RJ, et al. Psychosocial stress during pregnancy is related to adverse birth outcomes: Results from a large multi-ethnic community-based birth cohort. European Journal of Public Health. 2013;23(3):485–491. doi: 10.1093/eurpub/cks097. [DOI] [PubMed] [Google Scholar]
- 60.Maina G, Saracco P, Giolito MR, Danelon D, Bogetto F, Todros T. Impact of maternal psychological distress on fetal weight, prematurity and intrauterine growth retardation. Journal of Affect Disorders. 2008;111(2–3):214–220. doi: 10.1016/j.jad.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 61.Schneid-Kofman N, Sheiner E, Levy A. Psychiatric illness and adverse pregnancy outcome. International Journal of Gynecology & Obstetrics. 2008;101(1):53–56. doi: 10.1016/j.ijgo.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 62.Jablensky AV, Morgan V, Zubrick SR, Bower C, Yellachich LA. Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. American Journal of Psychiatry. 2005;162(1):79–91. doi: 10.1176/appi.ajp.162.1.79. [DOI] [PubMed] [Google Scholar]
- 63.Ponirakis A, Susman EJ, Stifter CA. Negative emotionality and cortisol during adolescent pregnancy and its effects on infant health and autonomic nervous system reactivity. Developmental Psychobiology. 1998;33(2):163–174. [PubMed] [Google Scholar]
- 64.Zimmer-Gembeck MJ, Helfand M. Low birth-weight in a public prenatal care program: Behavioral and psychosocial risk factors and psychosocial intervention. Social Science and Medicine. 1996;43(2):187–197. doi: 10.1016/0277-9536(95)00361-4. [DOI] [PubMed] [Google Scholar]
- 65.Stevens-Simon C, McAnarney ER. Childhood victimization: Relationship to adolescent pregnancy outcome. Child Abuse and Neglect. 1994;18(7):569–575. doi: 10.1016/0145-2134(94)90083-3. [DOI] [PubMed] [Google Scholar]
- 66.Fogel CI. Pregnant inmates. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 1993;22(1):33–39. doi: 10.1111/j.1552-6909.1993.tb01780.x. [DOI] [PubMed] [Google Scholar]
- 67.MacDonald LD, Peacock JL, Anderson HR. Marital status: Association with social and economic circumstances, psychological state and outcomes of pregnancy. Journal of Public Health. 1992;14(1):26–34. [PubMed] [Google Scholar]
- 68.Field T, Diego M, Hernandez-Reif M. Prenatal dysthymia versus major depression effects on the neonate. Infant Behavior & Development. 2008;31(2):190–193. doi: 10.1016/j.infbeh.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Field T, Diego M, Hernandez-Reif M, Figueiredo B, Deeds O, Ascencio A, et al. Comorbid depression and anxiety effects on pregnancy and neonatal outcome. Infant Behavior & Development. 2010;33(1):23–29. doi: 10.1016/j.infbeh.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. American Journal of Epidemiology. 2003;157(1):14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 71.Rahman A, Bunn J, Lovel H, Creed F. Association between antenatal depression and low birthweight in a developing country. Acta Psychiatrica Scandinavica. 2007;115(6):481–486. doi: 10.1111/j.1600-0447.2006.00950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dayan J, Creveuil C, Herlicoviez M, Herbel C, Baranger E, Savoye C, et al. Role of anxiety and depression in the onset of spontaneous preterm labor. American Journal of Epidemiology. 2002;155(4):293–301. doi: 10.1093/aje/155.4.293. [DOI] [PubMed] [Google Scholar]
- 73.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 74.Beck AT, Ward C, Mendelson M. Beck depression inventory (BDI). Archives of General Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 75.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry. 1987;150(6):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 76.Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychological Medicine. 1979;9:139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 77.Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry. 1988;45(8):742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- 78.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;3:595–605. [PubMed] [Google Scholar]
- 79.Dunkel Schetter C, Glynn LM. Stress in pregnancy: Empirical evidence and theoretical issues to guide interdisciplinary research. In: Contrada R, Baum A, editors. The Handbook of Stress Science: Biology, Psychology, and Health. Springer; New York, NY: 2011. pp. 321–343. [Google Scholar]
- 80.Battaglia FC, Lubchenco LO. A practical classification of newborn infants by weight and gestational age. The Journal of pediatrics. 1967;71(2):159–163. doi: 10.1016/s0022-3476(67)80066-0. [DOI] [PubMed] [Google Scholar]
- 81.Divon MY. Lockwood CJ, Barss VA, editors. Fetal growth restriction: Causes and risk factors. UpToDate. 2014 Retrieved from http://www.uptodate.com/home/index.html.
- 82.El Marroun H, Jaddoe VW, Hudziak JJ, Roza SJ, Steegers EA, Hofman A, et al. Maternal use of selective serotonin reuptake inhibitors, fetal growth, and risk of adverse birth outcomes. Archives of General Psychiatry. 2012;69(7):706–714. doi: 10.1001/archgenpsychiatry.2011.2333. [DOI] [PubMed] [Google Scholar]
- 83.Goldenberg RL, Cliver SP, Mulvihill FX, Hickey CA, Hoffman HJ, Klerman LV, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. American Journal of Obstetrics and Gynecology. 1996;175(5):1317–1324. doi: 10.1016/s0002-9378(96)70048-0. [DOI] [PubMed] [Google Scholar]
- 84.Ibanez G, Charles MA, Forhan A, Magnin G, Thiebau-georges O, Kaminski M, Eden Mother–Child Cohort Study Depression and anxiety in women during pregnancy and neonatal outcome: Data from the EDEN mother–child cohort. Early Human Development. 2012;88(8):643–649. doi: 10.1016/j.earlhumdev.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 85.Suri R, Altshuler L, Hellemann G, Burt V, Aquino A, Mintz J. Effects of antenatal depression and antidepressant treatment on gestational age at birth and risk of preterm birth. American Journal of Psychiatry. 2007;164(8):1206–1213. doi: 10.1176/appi.ajp.2007.06071172. [DOI] [PubMed] [Google Scholar]
- 86.Andersson L. Neonatal outcome following maternal antenatal depression and anxiety: A population-based study. American Journal of Epidemiology. 2004;159(9):872–881. doi: 10.1093/aje/kwh122. [DOI] [PubMed] [Google Scholar]
- 87.Van Dijk AE, Van Eijsden M, Stronks K, Gemke RJ, Vrijkotte TG. Maternal depressive symptoms, serum folate status, and pregnancy outcome: Results of the Amsterdam Born Children and their Development study. American Journal of Obstetrics & Gynecology. 2010;203(6):563.e1–563.e7. doi: 10.1016/j.ajog.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 88.Perkin MR, Bland JM, Peacock JL, Anderson HR. The effect of anxiety and depression during pregnancy on obstetric complications. BJOG: An International Journal of Obstetrics & Gynecology. 1993;100(7):629–634. doi: 10.1111/j.1471-0528.1993.tb14228.x. [DOI] [PubMed] [Google Scholar]
- 89.Kramer MS, Lydon J, Seguin L, Goulet L, Kahn SR, McNamara H, et al. Stress pathways to spontaneous preterm birth: The role of stressors, psychological distress, and stress hormones. American Journal Epidemiology. 2009;169(11):1319–1326. doi: 10.1093/aje/kwp061. [DOI] [PubMed] [Google Scholar]
- 90.Hoffman S, Hatch MC. Depressive symptom-atology during pregnancy: Evidence for an association with decreased fetal growth in pregnancies of lower social class women. Health Psychology. 2000;19(6):535. [PubMed] [Google Scholar]
- 91.Li D, Liu L, Odouli R. Presence of depressive symptoms during early pregnancy and the risk of preterm delivery: A prospective cohort study. Human Reproduction. 2009;24(1):146–153. doi: 10.1093/humrep/den342. [DOI] [PubMed] [Google Scholar]
- 92.Bodecs T, Horvath B, Szilagyi E, Gonda X, Rihmer Z, Sandor J. Effects of depression, anxiety, self-esteem, and health behaviour on neonatal outcomes in a population-based Hungarian sample. European Journal of Obstetric Gynecological Reproductive Biology. 2011;154(1):45–50. doi: 10.1016/j.ejogrb.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 93.Kumar R, Robson KM. A prospective study of emotional disorders in childbearing women. The British Journal of Psychiatry. 1984;144(1):35–47. doi: 10.1192/bjp.144.1.35. [DOI] [PubMed] [Google Scholar]
- 94.Benute GRG, Nomura RMY, Reis JS, Junior RF, Lucia MCSD, Zugaib M. Depression during pregnancy in women with a medical disorder: Risk factors and perinatal outcomes. Clinics. 2010;65(11):1127–1131. doi: 10.1590/S1807-59322010001100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rogal SS, Poschman K, Belanger K, Howell HB, Smith MV, Medina J, et al. Effects of posttraumatic stress disorder on pregnancy outcomes. Journal Affect Disorders. 2007;102(1–3):137–143. doi: 10.1016/j.jad.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Field T, Diego M, Hernandez-Reif M, Figueiredo B, Schanberg S, Kuhn C, et al. Chronic prenatal depression and neonatal outcome. International Journal of Neuroscience. 2008;118(1):95–103. doi: 10.1080/00207450601042144. [DOI] [PubMed] [Google Scholar]
- 97.Nylen KJ, O'Hara MW, Engeldinger J. Perceived social support interacts with prenatal depression to predict birth outcomes. Journal of Behavioral Medicine. 2012;36(4):427–440. doi: 10.1007/s10865-012-9436-y. [DOI] [PubMed] [Google Scholar]
- 98.Suri R, Altshuler L, Hendrick V, Rasgon N, Lee E, Mintz J. The impact of depression and fluoxetine treatment on obstetrical outcome. Archives of Womens’ Mental Health. 2004;7(3):193–200. doi: 10.1007/s00737-004-0057-5. [DOI] [PubMed] [Google Scholar]
- 99.Gawlik S, Waldeier L, Muller M, Szabo A, Sohn C, Reck C. Subclinical depressive symptoms during pregnancy and birth outcome: A pilot study in a healthy German sample. Archives of Womens’ Mental Health. 2013;16(2):93–100. doi: 10.1007/s00737-012-0320-0. [DOI] [PubMed] [Google Scholar]
- 100.Diego MA, Field T, Hernandez-Reif M, Schanberg S, Kuhn C, Gonzalez-Quintero VH. Prenatal depression restricts fetal growth. Early Human Development. 2009;85(1):65–70. doi: 10.1016/j.earlhumdev.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Earnshaw VA, Rosenthal L, Lewis JB, Stasko EC, Tobin JN, Lewis TT, et al. Maternal experiences with everyday discrimination and infant birth weight: A test of mediators and moderators among young, urban women of color. Annual Behavioral Medicine. 2013;45(1):13–23. doi: 10.1007/s12160-012-9404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Neggers Y, Goldenberg R, Cliver S, Hauth J. The relationship between psychosocial profile, health practices, and pregnancy outcomes. Acta Obstetricia et Gynecologica Scan-dinavica. 2006;85(3):277–285. doi: 10.1080/00016340600566121. [DOI] [PubMed] [Google Scholar]
- 103.Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: A cohort study. Archives of General Psychiatry. 2004;61(9):946. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- 104.Straub H, Adams M, Kim JJ, Silver RK. Antenatal depressive symptoms increase the likelihood of pre-term birth. American Journal of Obstetrics & Gynecology. 2012;207(4):329e1–329e4. doi: 10.1016/j.ajog.2012.06.033. [DOI] [PubMed] [Google Scholar]
- 105.Accortt EE, Schetter CD. Pregnant women screening positive for depressive symptoms at 24–28 weeks may have increased risk of preterm birth but more precise research is needed. Evidence Based Nursing. 2013;17(1):11–12. doi: 10.1136/eb-2012-101164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wisner KL, Bogen DL, Sit D, McShea M, Hughes C, Rizzo D, et al. Does fetal exposure to SSRIs or maternal depression impact infant growth? American Journal of Psychiatry. 2013;170(5):485–493. doi: 10.1176/appi.ajp.2012.11121873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Liu Y, Murphy SK, Murtha AP, Fuemmeler BF, Schildkraut J, Huang Z, Hoyo C. Depression in pregnancy, infant birth weight and DNA methylation of imprint regulatory elements. Epigenetics. 2012;7(7):735–746. doi: 10.4161/epi.20734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: Links and possible mechanisms. A review. Neuroscience & Biobehavioral Reviews. 2005;29(2):237–258. doi: 10.1016/j.neubiorev.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 109.Dunkel Schetter C, Lobel M. Pregnancy and birth: A multilevel analysis of stress and birth weight. In: Revenson T, Baum A, Singer J, editors. Handbook of health psychology. 2nd ed. Lawrence Erlbaum; Mahwah, NJ: 2011. pp. 427–453. [Google Scholar]
- 110.Dunkel Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- 111.Field T, Diego M, Hernandez-Reif M, Medina L, Delgado J, Hernandez A. Yoga and massage therapy reduce prenatal depression and prematurity. Journal of bodywork and movement therapies. 2012;16(2):204–209. doi: 10.1016/j.jbmt.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Burns A, Heather O, Baxter H, Bennert K, Wiles N, Ramchandani P, et al. A pilot randomised controlled trial of cognitive behavioural therapy for antenatal depression. BMC Psychiatry. 2013;13(1):33. doi: 10.1186/1471-244X-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.O'Mahen H, Himle JA, Fedock G, Henshaw E, Flynn H. A pilot randomized controlled trial of cognitive behavioral therapy for perinatal depression adapted for women with low incomes. Depression and Anxiety. 2013;30(7):679–687. doi: 10.1002/da.22050. [DOI] [PubMed] [Google Scholar]
- 114.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Current Opinion in Psychiatry. 2012;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- 116.Cohen S, Kessler R, Gordon LU. Measuring stress: A guide for health and social scientists. Oxford University Press; New York: 1995. [Google Scholar]
- 117.Hammen C. Stress and depression. Annual Review Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 118.Bae HS, Kim SY, Ahnv HS, Cho YK. Comparison of nutrient intake, life style variables, and pregnancy outcomes by the depression degree of pregnant women. Nutrition Research and Practice. 2010;4(4):323–331. doi: 10.4162/nrp.2010.4.4.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Berle JO, Mykletun A, Daltveit AK, Rasmussen S, Holsten F, Dahl AA. Neonatal outcomes in off-spring of women with anxiety and depression during pregnancy. A linkage study from The Nord-Trondelag Health Study (HUNT) and Medical Birth Registry of Norway. Archives of Womens’ Mental Health. 2005;8(3):181–189. doi: 10.1007/s00737-005-0090-z. [DOI] [PubMed] [Google Scholar]
- 120.Copper RL, Goldenberg RL, Das A, Elder N, Swain M, Norman G, et al. The preterm prediction study: Maternal stress is associated with spontaneous preterm birth at less than thirty-five weeks’ gestation. American Journal of Obstetrics and Gynecology. 1996;175(5):1286–1292. doi: 10.1016/s0002-9378(96)70042-x. [DOI] [PubMed] [Google Scholar]
- 121.Subramanian S, Katz KS, Rodan M, Gantz MG, El-Khorazaty NM, Johnson A, et al. An integrated randomized intervention to reduce behavioral and psychosocial risks: Pregnancy and neonatal outcomes. Maternal Child Health Journal. 2012;16(3):545–554. doi: 10.1007/s10995-011-0875-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. Exposure to Hurricane Katrina, post-traumatic stress disorder and birth outcomes. American Journal of the Medical Sciences. 2008;336(2):111–115. doi: 10.1097/MAJ.0b013e318180f21c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang SY, Chen CH. The association between prenatal depression and obstetric outcome in Taiwan: A prospective study. Journal of Women's Health. 2010;19(12):2247–2251. doi: 10.1089/jwh.2010.1988. [DOI] [PubMed] [Google Scholar]
- 124.Nordentoft M, Lou HC, Hansen D, Nim J, Pryds O, Rubin P, et al. Intrauterine growth retardation and premature delivery: The influence of maternal smoking and psychosocial factors. American Journal of Public Health. 1996;86(3):347–354. doi: 10.2105/ajph.86.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dayan J, Creveuil C, Marks MN, Conroy S, Herlicoviez M, Dreyfus M, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: A prospective cohort study among women with early and regular care. Psychosomatic Medicine. 2006;68(6):938–946. doi: 10.1097/01.psy.0000244025.20549.bd. [DOI] [PubMed] [Google Scholar]
- 126.Drewett R, Blair P, Emmett P, Emond A. Failure to thrive in the term and preterm infants of mothers depressed in the postnatal period: A population-based birth cohort study. Journal of Child Psychology and Psychiatry. 2004;45(2):359–366. doi: 10.1111/j.1469-7610.2004.00226.x. [DOI] [PubMed] [Google Scholar]
- 127.Rondo PHC, Ferreira RF, Nogueira F, Ribeiro MCN, Lobert H, Artes R. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. European Journal of Clinical Nutrition. 2003;57(2):266–272. doi: 10.1038/sj.ejcn.1601526. [DOI] [PubMed] [Google Scholar]
- 128.Savitz DA, Harmon Q, Siega-Riz AM, Herring AH, Dole N, Thorp JM., Jr. Behavioral influences on preterm birth: Integrated analysis of the pregnancy, infection, and nutrition study. Maternal and Child Health Journal. 2012;16(6):1151–1163. doi: 10.1007/s10995-011-0895-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Steer RA, Scholl TO, Hediger ML, Fischer RL. Self-reported depression and negative pregnancy outcomes. Journal of Clinical Epidemiology. 1992;45(10):1093–1099. doi: 10.1016/0895-4356(92)90149-h. [DOI] [PubMed] [Google Scholar]
- 130.Orr ST, James SA, Prince CB. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. American Journal of Epidemiology. 2002;156(9):797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- 131.Kabir K, Sheeder J, Stevens-Simon C. Depression, weight gain, and low birth weight adolescent delivery: Do somatic symptoms strengthen or weaken the relationship? Journal of Pediatric and Adolescent Gynecology. 2008;21(6):335–342. doi: 10.1016/j.jpag.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 132.Fransson E, Örtenstrand A, Hjelmstedt A. Ante-natal depressive symptoms and preterm birth: A prospective study of a Swedish national sample. Birth. 2011;38(1):10–16. doi: 10.1111/j.1523-536X.2010.00441.x. [DOI] [PubMed] [Google Scholar]
- 133.Dole N, Savitz DA, Siega-Riz AM, Hertz-Picciotto I, McMahon MJ, Buekens P. Psychosocial factors and preterm birth among African American and White women in central North Carolina. American Journal of Public Health. 2004;94(8):1358–1365. doi: 10.2105/ajph.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Haas JS, Fuentes-Afflick E, Stewart AL, Jackson RA, Dean ML, Brawarsky P, Escobar GJ. Prepregnancy health status and the risk of preterm delivery. Archives of Pediatrics and Adolescent Medicine. 2005;159(1):58. doi: 10.1001/archpedi.159.1.58. [DOI] [PubMed] [Google Scholar]
- 135.Messer LC, Dole N, Kaufman JS, Savitz DA. Pregnancy intendedness, maternal psychosocial factors and preterm birth. Maternal and Child Health Journal. 2005;9(4):403–412. doi: 10.1007/s10995-005-0021-7. [DOI] [PubMed] [Google Scholar]
- 136.Goedhart G, Snijders AC, Hesselink AE, van Poppel MN, Bonsel GJ, Vrijkotte TG. Maternal depressive symptoms in relation to perinatal mortality and morbidity: Results from a large multiethnic cohort study. Psychosomatic Medicine. 2010;72(8):769–776. doi: 10.1097/PSY.0b013e3181ee4a62. [DOI] [PubMed] [Google Scholar]
- 137.Shaikh K, Premji S, Rose M, Kazi A, Khowaja S, Tough S. The association between parity, infant gender, higher level of paternal education and preterm birth in Pakistan: A cohort study. BMC pregnancy and childbirth. 2011;11(1):88. doi: 10.1186/1471-2393-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ruiz RJ, Marti CN, Pickler R, Murphey C, Wommack J, Brown CE. Acculturation, depressive symptoms, estriol, progesterone, and preterm birth in Hispanic women. Archives of Women's Mental Health. 2012;15(1):57–67. doi: 10.1007/s00737-012-0258-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Patel V, Prince M. Maternal psychological morbidity and low birth weight in India. The British Journal of Psychiatry. 2006;188(3):284–285. doi: 10.1192/bjp.bp.105.012096. [DOI] [PubMed] [Google Scholar]
- 140.Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Low birth weight in offspring of women with depressive and anxiety symptoms during pregnancy: Results from a population based study in Bangladesh. BMC public health. 2010;10(1):515. doi: 10.1186/1471-2458-10-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Shiono PH, Rauh VA, Park M, Lederman SA, Zuskar D. Ethnic differences in birthweight: The role of lifestyle and other factors. American Journal of Public Health. 1997;87(5):787–793. doi: 10.2105/ajph.87.5.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lundy BL, Jones NA, Field T, Nearing G, Davalos M, Pietro PA, et al. Prenatal depression effects on neonates. Infant Behavior and Development. 1999;22(1):119–129. [Google Scholar]
- 143.Elsenbruch S, Benson S, Rücke M, Rose M, Dudenhausen J, Pincus-Knackstedt MK, et al. Social support during pregnancy: Effects on maternal depressive symptoms, smoking and pregnancy outcome. Human Reproduction. 2007;22(3):869–877. doi: 10.1093/humrep/del432. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.