Abstract
The objective of this study was to characterize and compare individual and sexual network characteristics of Black, White, and Latino YMSM as potential drivers of racial disparities in HIV. Egocentric network interviews were conducted with 175 diverse YMSM who described 837 sex partners within 167 sexual-active egos. Sexual partner alter attributes were summarized by ego. Descriptives of ego demographics, sexual partner demographics, and network characteristics were calculated by race of the ego and compared. No racial differences were found in individual engagement in HIV risk behaviors or concurrent sexual partnership. Racial differences were found in partner characteristics, including female gender, non-gay sexual orientations, older age, and residence in a high HIV prevalence neighborhood. Racial differences in relationship characteristics included type of relationships (i.e., main partner) and strength of relationships. Network characteristics also showed differences, including sexual network density and assortativity by race. Most racial differences were in the direction of effects that would tend to increase HIV incidence among Black YMSM. These data suggest that racial disparities in HIV may be driven and/or maintained by a combination of racial differences in partner characteristics, assortativity by race, and increased sexual network density, rather than differences in individual’s HIV risk behaviors.
Keywords: Minority health, Homosexuality, male, social networking, young adult, HIV seroprevalence
Introduction
Young men who have sex with men (YMSM) are disproportionately infected with HIV/AIDS in the U.S.1. Unlike other groups where the number of new infections has been declining or stable, from 2008 to 2010 the number of new HIV infections increased by 22% among MSM aged 13–24 years2. In 2010 the greatest number of new infections among MSM occurred in Black MSM aged 13–24 years, who accounted for 45% of new infections among Black MSM and 55% of infections among YMSM overall2. Data from 18–24 year old MSM in the CDC’s 2008 National HIV Behavioral Surveillance system (NHBS) study conducted in 21 U.S. cities produced estimates of HIV prevalence and incidence among Black YMSM of 16.5% and 5.1%, respectively, compared to 6.2% and 1.6% for White YMSM 3.
Paradoxically, Black YMSM have not been found to engage in more HIV risk behaviors; compared to other racial groups they report similar or higher rates of condom use, fewer sexual partners, and less substance use4–8, paralleling results among adult MSM9–11. As such, disparities in HIV prevalence cannot be explained by individual risk behaviors and instead have been hypothesized to be attributed to sexual network structural and geospatial factors, although published data directly examining these questions are limited, particularly among YMSM1,4,12–15.
Empirical and modeling studies have identified features of networks that create conditions for rapid spread of infections and are therefore candidates for either creating and/or maintaining racial disparities among YMSM. First, modeling studies have shown that very small differences in rates of concurrent relationships (i.e., multiple sexual partnerships that overlap in time) in a population have exponential impacts on population STI prevalence16,17. The exact operationalization of concurrency has varied somewhat across studies in terms of the required proximity of sexual encounters to be classified as concurrent (e.g., date of first sex with one partner preceded the date of last sex with a different partner18, both partnerships occurred within 3 weeks19). Studies of MSM have associated concurrency with STI diagnoses20,21, but tests for racial differences in concurrent sexual partnerships have produced inconsistent results19,22.
A second key feature of networks is assortative mixing—or the tendency to have sex partners from one’s own group. Assortative mixing by race—or the tendency to have sex partners from one’s own racial group—can amplify and sustain long-term prevalence differentials that arise from other social, behavior, or biological differences between racial groups16,23. When assortative mixing is high, particularly in a relatively small population with high HIV prevalence, HIV can be rapidly transmitted to a large proportion of that population, thereby magnifying and sustaining disparities in incidence24. Studies have found the highest levels of racial assortativity among Black MSM in both adults13,25,26 and youth4,5,27. Assortativity by race has been tested using a number of statistical procedures depending on the design of the particular study, including the odds ratio of a partner being of the same race relative to another race4, a coefficient of assortativity based on the matrix of partnerships among racial groups28, or the percentage of sexual partners who are of the same race calculated for each racial group25. The latter approach may consider an adjustment for the background racial distribution in the community to more clearly test if partnering is random or assortative (i.e., if 30% of men in a community are Black then random partner selection would mean 30% of partners in all racial groups would be Black). Assortative mixing by age is also important to HIV dynamics. For example, in African girls, having older male partners increases the odds of being HIV infected by as much as 60%29–31. One study found sex between young and older Black MSM was more likely to be unprotected compared to other race and age pairings5. Since adult Black MSM have the highest domestic HIV prevalence (estimated at 28%32), such couplings potentiate HIV transmission to Black YMSM5,11,27,33. Essentially these dyadic and network phenomena set up a dynamic where high prevalence in adults increases incidence in youths34. Of course it is important to recognize that the average age difference between partners in a full census of a population will be zero, as the difference in age in a couple with an older and younger member will be canceled out when both are part of the population being studied. The absolute value of the age differences can also be examined, with important implications for disease transmission—wider gaps can create more contact across ages with different HIV prevalence, and thus facilitates transmission to the group with lower prevalence—in this case, younger MSM. With the current study’s focus on YMSM, by design we do not have a population sample of MSM of all ages. Therefore, positive differences in the mean age difference with partners would reflect a tendency of these YMSM to have partners older than themselves.
A third important aspect is network topology, the overall structure of the network connections, which has been shown to heavily influence disease spread15,35. One aspect of network topology is sexual network density, which assesses overall network connectedness, and is operationalized as the proportion of actual sexual ties among people from all possible sexual ties. Where sexual networks are denser there are more opportunities for transmission36. Social network density has been examined among drug using adults and found to be associated with increased injection drug use37, but to our knowledge there are no published reports of sexual network density among YMSM. Multiplexity represents the overlap in types of relationships (i.e., sex with friends or drug use with sex partners). Having sex with friends could increase risk due to the perception of familiarity and trust associated with less condom use among YMSM38 or could impact other aspects of the structure of sexual networks (e.g., density)39,40. Alternatively, multiplexity could decrease risk by diffusing safe-sex norms through social networks41, however prior studies of social network composition and HIV risk behaviors have produced mixed results41. Groups with greater tendencies towards overlap among sex and drug partners are likely to be at higher risk for HIV given the greater likelihood of unprotected sex during drug use 42,43.
Geographic factors are also important considerations when considering racial disparities in HIV44. Neighborhoods often differ greatly with regard to the socioeconomic status and race/ethnicity of their residents, but also can have very different HIV prevalence44,45. In Chicago, HIV prevalence varies by as much as 30 times across community areas, with the highest prevalence in neighborhoods traditionally gay-identified and with high concentrations of Black residents46. The association between neighborhoods and HIV has been linked to general neighborhood factors like disadvantage, disorder, and collective efficacy as well as more HIV-specific neighborhood factors like the number of HIV testing programs and gay acceptance12,44.
Despite being frequently hypothesized as drivers of racial disparities in HIV among YMSM, geographic and sexual network characteristics have received very little empirical investigation. Moreover, most prior studies of networks among MSM have focused on social networks rather than sexual networks, and to our knowledge no prior study has examined sexual, social, and drug networks simultaneously along with geographic residency of sexual partners. We conducted an egocentric network interview with YMSM to characterize these network characteristics and examine their possible role in racial disparities in HIV by comparing the network characteristics of Black, White, and Latino YMSM.
Methods
Participants
Participants (N=175) from Crew 450, an ongoing longitudinal study of syndemic development YMSM, were selected based on the timing of their study visits to participate in this network substudy. Baseline eligibility criteria for Crew 450 included: 16–20 years old, born male, spoke English, had a sexual encounter with a male or identify as gay/bisexual, and available for follow-up for 2 years. Participation for this network study occurred during the 12- or 24-month follow-up visits of Crew 450 (June 2011 – October 2012). A total of 204 parent study participants were contacted about partaking in the network substudy, of which 179 (88%) agreed to participate. However, two participants never showed up for their scheduled appointment and two enrolled, but subsequently withdrew. Eight participants reported never having a sex partner and thus were excluded from these analyses. The demographic characteristics of egos (n=167) and sex partners (n=837) can be found in Table 1. The study protocol was approved by the Institutional Review Board and participants were compensated $25.
Table 1.
Demographic Characteristics of YMSM Egos and Alters Who Were Sex Partners
| Egos (n=167) | Alters (n=837) | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age | 20.1 | 1.4 | 22.4 | 4.5 |
| N | % | N | % | |
| Gender | ||||
| Male | 167 | 100.0 | 767 | 91.6 |
| Female | 0 | 0.0 | 63 | 7.5 |
| Transgender | - | - | 7 | 0.8 |
| Race/Ethnicity | ||||
| Black | 91 | 54.5 | 410 | 49.0 |
| Latino | 37 | 22.2 | 176 | 21.0 |
| White | 22 | 13.2 | 189 | 22.6 |
| Other | 17 | 10.2 | 61 | 7.3 |
| Missing | 0 | 0.0 | 1 | 0.1 |
| Sexual Orientation | ||||
| Gay/Lesbian | 140 | 83.9 | 629 | 75.1 |
| Bisexual | 21 | 12.6 | 128 | 15.3 |
| Heterosexual | 3 | 1.8 | 65 | 7.8 |
| Other | 3 | 1.8 | 7 | 0.8 |
| Missing | 0 | 0.0 | 8 | 1.0 |
| Living Situation* | ||||
| Stable housing | 159 | 95.2 | - | - |
| Unstable housing | 7 | 4.2 | - | - |
| Missing | 1 | 0.6 | - | - |
| Highest Education Level | ||||
| High school grad or less | 69 | 41.3 | - | - |
| Post high school | 97 | 58.1 | - | - |
| Missing | 1 | 0.6 | - | - |
| Employed | ||||
| No | 89 | 53.3 | - | - |
| Yes | 77 | 46.1 | - | - |
| Missing | 1 | 0.6 | - | - |
| HIV-positive | 19 | 11.4 | - | - |
| STI-positive | 12 | 7.2 | - | - |
Living in an apartment, dorm, or house is considered stable housing. Unstable housing is defined by a person living in a shelter, group home, residential treatment facility or is homeless.
Procedures
An egocentric interview gathered information on respondents’ relationships with their alters—persons with whom they had a social, sexual, or substance using connection. Participants were asked to: enumerate all alters, describe characteristics of alters, and portray connections between alters. Adapted from the work of Hogan 47, interviewers utilized a two-step approach of completing a pre-numbered list to enumerate alters and to capture alter characteristics, and then a participant-aided sociogram to elicit respondents’ reported connections between alters. Detailed information on procedures can be found elsewhere48.
Measures and Estimation of Network Parameters
Name Generator
We first elicited a list of the first and last names of individuals with whom participants had supportive relationships via five name generating items. Participants were then asked which individuals on that list they had ever “used drugs or alcohol with” or “had sex with.” Then participants were asked to name anyone else that they had not yet listed that they had ever “used drugs or alcohol with” or “had sex with.” Finally, participants were asked if there was anyone that they had not yet listed who had “used drugs or alcohol” or “had sex with” two or more of the people on their list. After the list of names of alters was generated, demographic characteristics (age, race [mutually exclusive], gender, perceived sexual identity, cross-streets or neighborhood of residence), characteristics of the relationship (frequency of contact, strength of relationship, and relationship type), and behaviors with that person (first and last dates of sexual contact) were obtained. Detailed sexual behavior (type of sexual contact, frequency of sexual contact, condom use) was only obtained about sexual partners from the prior six months. In addition to the above measures, HIV and STI (gonorrhea and Chlamydia) test results were drawn from the Crew 450 parent study. For these analyses, only alters who were indicated to have had sex with the participant were deemed to be part of the sexual network (n = 837).
Relationship Type
Relationship type was coded from an item which listed 28 different categories (e.g., Mother, Boyfriend, Teacher). Participants were able to assign up to two relationship types and to choose “Other” and provide their own description. Sex partners that were labeled as either boyfriend, girlfriend, partner, ex-boyfriend, ex-girlfriend, or another similar term such as “my boo” were coded as Main Partners. Sex Partners that were not coded as Main Partners and were labeled as a friend were coded as Friend. Sex Partners that met neither of these criteria were labeled as Non-Main/Non-Friend.
Concurrency
For each partner, the ego indicated the start and end dates of sexual contact. Using those dates, concurrency was defined when a partner’s sexual relationship overlapped with another sexual partner.
High HIV Prevalence Neighborhood
Using 2011 data from the Chicago Department of Public Health, neighborhood HIV rates were calculated by determining the number of males aged 15 to 24 who are currently living with HIV infection per 100,000 for each of Chicago’s 77 neighborhoods49. Neighborhoods were then ordered in lowest to highest prevalence rate, and neighborhoods in the top 25% were considered high prevalence (over 628.9 per 100,000 males aged 15–24) and alters were coded accordingly. Sex partners who lived outside of Chicago (33.0%) or had missing locations (11.9%) were coded missing.
Density
The density of a network is the proportion of possible ties that are present. Following other studies for the assessment of local network density50,51, density of each sexual network was calculated by summing the number of sexual connections observed between the ego/alter and alter/alter pairs, and then dividing by the total number of possible pairs given the number of support, sex, and substance connections that were reported by each ego.
Multiplexity
Multiplexity was calculated by determining the extent of overlap between multiple networks (e.g., sex, support, and drug)50. Correlations between the sexual network and both the drug network and support networks were calculated by utilizing QAP correlation function within UCINET51, which estimates the association between the observed matrices and uses quadratic assignment procedures to estimate standard errors51,52.
Assortativity by race
Newman’s Assortativity Coefficient (AC) was calculated from the racial mixing matrix, a matrix comprised of the proportion of sexual relationships between Black, White, Hispanic, and Other Egos and Alters53. AC ranges from 1.0 to −1.0, with 1.0 indicating that Egos only have sexual partnerships with individuals of their same race, −1.0 that Egos only have sexual partners of a different race, and 0 indicating that sexual partnerships are not influenced by race. In order to consider the influence of differing proportions of racial/ethnic groups within Chicago in our estimation of assortativity, we also calculated a ratio of racial concordance to census proportion (RCR) by racial group by dividing the observed proportion of sexual partners by race by the census proportion of that group. The census proportion was derived from the racial/ethnic breakdown of 18–24 year olds from the 2010 census data for Chicago54.
Analyses
To describe network differences by race, continuous demographic variables were analyzed using t-tests and categorical variables using chi-square tests. To test the significance of differences among means for multiple groups, analyses of variance (ANOVAs) were used.
Results
Alter characteristics by ego race are shown in Table 2. Black YMSM were significantly more likely to have sex partners whom they identified as a main partner and to report strong relationships with their sex partners, while White and Hispanic YMSM were more likely to report weak relationships with their sexual partners. Our analysis found that, although no age differences by race were found within our YMSM participants (p = .86), Black and Latino YMSM on average had sexual partners who were approximately two and a half years older than them, whereas White youth tended to have partners who were on average approximately one year older. There were no significant racial/ethnic differences in having concurrent sexual relationships. Black YMSM had a significantly greater proportion of their sexual partners from high HIV prevalence neighborhoods than Latino, White, and Other YMSM.
Table 2.
Sex Partner Characteristics Stratified by Ego Race/Ethnicity
| Sex Partner Characteristics |
Black n (%) | Latino n (%) | White n (%) | Other n (%) | Chi-Square | |
|---|---|---|---|---|---|---|
| χ2 | p | |||||
| Gender | ||||||
| Male a,b,c,e,f | 394 (90.0) | 190 (96.9) | 112 (96.6) | 71 (81.6) | 23.88 | <.001 |
| Female a,b,c,e,f | 39 (8.9) | 5 (2.6) | 3 (2.6) | 16 (18.4) | 26.97 | <.001 |
| Transgender | 5 (1.1) | 1 (0.5) | 1 (0.9) | 0 | 1.48 | 0.69 |
| Sexual orientation | ||||||
| Gay a,b,e,f | 306 (69.9) | 166 (84.7) | 100 (86.2) | 57 (65.5) | 30.62 | <.001 |
| Bisexual a,b,e,f | 87 (19.9) | 18 (9.2) | 7 (6.0) | 16 (18.4) | 20.83 | <.001 |
| Heterosexual c,e,f | 36 (8.2) | 9 (4.6) | 6 (5.2) | 14 (16.1) | 12.12 | 0.01 |
| Queer | 5 (1.1) | 1 (0.5) | 1 (0.9) | 0 | 1.48 | 0.69 |
| Missing | 4 (0.9) | 2 (1.0) | 2 (1.7) | 0 | 1.58 | 0.66 |
| Type of Relationship | ||||||
| Main Partner a,e | 179 (40.9) | 48 (24.5) | 43 (37.1) | 36 (41.4) | 16.7 | <.001 |
| Friend | 138 (31.5) | 76 (38.8) | 34 (29.3) | 31 (35.6) | 4.32 | <0.23 |
| Non-Main/Non-Friend a,e | 121 (27.6) | 72 (36.7) | 39 (33.6) | 20 (23.0) | 15.67 | 0.001 |
| Strength of relationship | ||||||
| Very Close b,e,f | 118 (26.9) | 40 (20.4) | 16 (13.8) | 28 (32.2) | 13.22 | <.01 |
| Somewhat Close a | 143 (32.6) | 46 (23.5) | 27 (23.3) | 23 (26.4) | 7.86 | .04 |
| Not Close a,b,e,f | 177 (40.4) | 110 (56.1) | 73 (62.9) | 36 (41.4) | 27.05 | <.001 |
| Concurrent Partner | 260 (59.4) | 108 (55.1) | 70 (60.3) | 57 (65.5) | 2.87 | 0.41 |
| Sex Partner from a high HIV prevalence neighborhood a,b,c,e,f | 99 (39.4) | 9 (8.5) | 3 (5.4) | 8 (16.7) | 55.3 | <.001 |
|
| ||||||
| Mean (SD) | F | p | ||||
| Age Difference in Years (Alter Age – Ego Age) b,d | 2.8 (4.6) | 2.9 (3.8) | 1.5 (3.6) | 2.3 (4.5) | 3.29 | 0.02* |
Sex partners who lived outside the city of Chicago, or at an unknown location, were coded as missing.
Significant differences (p<.05) between Black and Latino
Significant differences (p<.05) between Black and White
Significant differences (p<.05) between Black and Other
Significant differences (p<.05) between Latino and White
Significant differences (p<.05) between Latino and Other
Significant differences (p<.05) between White and Other
No significant differences by race were found in the number of sex partners in the past 6 months, number of unprotected vaginal or anal sex partners, or the percent of egos having any unprotected sex (Table 3). Sexual network density was then examined by race and significant differences were found (p < 0.01) across all groups. Tamhane posthoc comparisons indicated that Black YMSM (p < 0.001) and Latino YMSM (p < .05) had significantly denser sexual networks than White YMSM. Based on conventional criteria for Cohen’s d (differences in means divided by standard deviation), these density differences are medium effect sizes55. YMSM were likely to show multiplexity in their sexual relationships (i.e., overlapping sex/drugs and sex/support networks). On average both sex and drug networks (r = 0.38) and sex and support networks (r = 0.13) were significantly associated (ps < .01). Sex partners were more likely than non-sex partners to be either drug partners or to be support network members. However, no significant racial differences were found for either sex and drug or sex and support multiplexity.
Table 3.
Ego Characteristics Stratified by Ego Race
| Sex Partner Characteristics | Black (n=94) | Latino (n=37) | White (n=24) | Other (n=19) | F, p-value | |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | F | P | |
| Number of Sex Partners last 6 mos | 2.07 (2.01) | 2.27 (2.40) | 1.79 (2.15) | 2.32 (2.63) | 0.29 | 0.83 |
| Num Unprotected Vaginal or Anal Sex Partners in the last6 months | 0.59 (0.81) | 0.95 (1.88) | 0.58 (0.88) | 1.32 (2.24) | 2.05 | 0.11 |
| Percent Reported Unprotected Sex in last 6 months* | 41 (43.6) | 14 (37.8) | 10 (41.6) | 11 (57.9) | 2.11 | 0.55 |
| Average Density of Ego/Alter a Sexual Networks | 0.051 (0.028) | 0.049 (0.037) | 0.026 (0.018) | 0.059 (0.063) | 3.996 | <0.01 |
| Multiplexity (Sex by Drug) | 0.38 (0.21) | 0.36 (0.24) | 0.36 (0.18) | 0.46 (0.19) | 0.75 | 0.52 |
| Multiplexity (Sex by Social) | 0.13 (0.17) | 0.13 (0.20) | 0.11 (0.07) | 0.15 (0.18) | 0.11 | 0.96 |
Proportion, standard deviation, and Chi-Square results reported a Significant differences between Black and White, (p < .001), and Latino and White (p = 0.03) using Tamhane post hoc comparisons
Racial mixing was assortative (AC = 0.58), with most egos reporting sexual relationships with individuals of the same race. Patterns of mixing by race/ethnicity are shown in two ways in Table 4: the percentage of participants’ (rows) sexual partners (columns) that were the same race and also the ratio of racial concordance to census proportion (RCR). For example, Black egos reported that 82% of their sexual partners were Black while only 4.3% were White. Latinos had the lowest concordance for race/ethnicity of sexual partners (56.1%). The RCR statistics similarly showed that all racial/ethnic groups were significantly more likely to have partners of their own race compared to census distributions for that racial group (e.g., 82% of Black participants partners were also Black relative to 29.9% of young men in Chicago are Black). While the percentages suggest the lowest concordance for Latino YMSM, the RCR, which accounts for group distribution in the populations, produces different results; relative to the number of Latino young men in Chicago, Latino YMSM are most likely to assort by race/ethnicity.
Table 4.
Assortativity by race
| Sexual Partner Race | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Black | Latino | White | Other | Chi-Sq | P-Value | |||||
|
| ||||||||||
| Ego Race | % | RCR | % | RCR | % | RCR | % | RCR | ||
| Black (n=91) | 82.0 | 2.74 | 5.7 | 0.43 | 4.3 | 0.14 | 7.8 | 0.29 | 248.44 | <0.001 |
| Latino (n=37) | 7.7 | 0.26 | 56.1 | 4.19 | 30.6 | 1.01 | 5.6 | 0.21 | 104.35 | <0.001 |
| White (n=22) | 2.6 | 0.09 | 14.7 | 0.95 | 75.0 | 2.48 | 7.8 | 0.29 | 61.07 | <0.001 |
| Other (n=17) | 37.9 | 1.27 | 27.6 | 2.06 | 26.4 | 0.87 | 8.0 | 0.30 | 14.01 | <0.01 |
| 18–24 Year Old Census Proportion by Race | 29.9% | 13.4% | 30.2% | 26.6% | ||||||
Note: RCR = ratio of racial concordance to census proportion for that racial group. Chi-squares test if sexual partner race is independent of ego race.
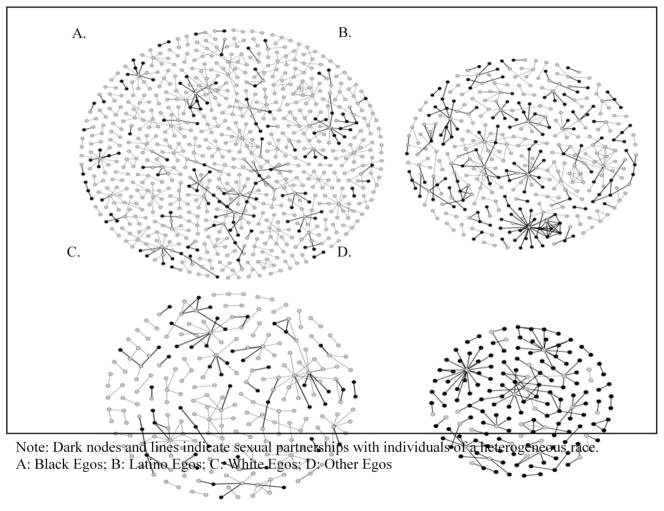
To help visualize these racial/ethnic differences in sex networks, Figure 1 displays all egocentric networks by race/ethnicity of participants. The race/ethnicity of sexual partners is indicated by the shape of the node.
Figure 1.
Sexual networks of sample, split by Ego’s race and indicating homophily.
Discussion
This study presents a novel examination of racial/ethnic differences in sexual network characteristics among YMSM that have previously been found in modeling and empirical studies to create or maintain STI disparities between groups. We examined these differences as putative drivers of racial disparities in HIV among YMSM—disparities that have previously been unexplainable by studying individual behaviors4–11. Consistent with prior studies that found Black MSM report the same or lower levels of engagement in HIV risk behaviors compared to other racial/ethnic groups4–11, we found no significant racial/ethnic differences in engagement in HIV risk behaviors (i.e., number of sex partners, number of unprotected sex partners, engagement in unprotected sex). This null finding further confirmed the need to test hypotheses that the increased incidence in HIV among Black YMSM is driven by sexual network factors and/or partner characteristics rather than individual behavior1,4,12,13.
Increased engagement in sex with older partners has been hypothesized to be a driver of elevated HIV incidence among Black YMSM5,27,34,56. Black and Latino YMSM had sex partners that were significantly older than partners of White YMSM. Given that HIV prevalence escalates with age among MSM32, having an older partner increases the per partner risk of HIV exposure. Studies have also shown that for YMSM, having older partners increases the odds that sex will be unprotected, and the effect is largest for Black YMSM relative to other racial/ethic groups5,27,38. One study also found that the increase in condomless sex was when the older partner was in the insertive rather than receptive role6—the sexual positioning that produces the greatest risk for transmission to YMSM. Taken together, these findings indicate a dynamic that has been referred to as an “intergenerational chain of transmission” where a high prevalence cohort of older males infects a newly sexually active cohort of young men, who may eventually transmit to other younger men16. The causes for these racial/ethnic difference in partner age are poorly understood, although one study suggests they may be partially driven by increased need for emotional, social, and instrumental support provided by older men among youth of color57. Alternatively, it could be driven by lack of accessible same-age partners in the social settings where they are primarily embedded58. For example, schools may have few out gay/bisexually identified young men and individuals under age 21 cannot access bars/clubs that serve as in person venues for meeting other MSM. This may be changing with the increased use of geospatial sociosexual networking apps, but at the time these data were collected such apps were just beginning to be used.
HIV prevalence among young men varies dramatically by neighorhood in Chicago46 and therefore on a population-level, sexual contact with a partner from a high prevalence neighborhood will tend to increase the odds of HIV exposure during unprotexted sex relative to a partner from a low prevalence neighborhood. In this study, we matched each sex partner’s neighborhood of residence to the HIV rates for young men in that neighborhood and compared the percentage of partners from high prevalence areas by race/ethnicity. We found a dramatic difference, with 39.4% of partners of Black YMSM living in the highest HIV prevalence areas, whereas for White and Latino YMSM it was 5.4% and 8.5% respectively. This association is unsurprising, as HIV rates are higher in Chicago neighborhoods with higher concentrations of Black residents46, and given assortativity by race we would expect Black YMSM to have more partners from these neighborhoods. This illustrates the tautology or circularity that is often present in attempts to identify factors that create racial disparities among young people when long-standing patterns of discrimination and segregation are critical, yet difficult to measure with these designs and incoporate in these analyses. Yet the magnitude of these differences starkly demonstrate the need for focused socio-geographic interventions to reduce HIV transmission and improve HIV medical care44,59. Additionally, while decomposing this complex problem into several distinct analyses of hypothesized mechanisms may detect some limited results, we are unable to parse out the entangled effects of race and neighborhood from each other. However, empirical observations such as these gathered within our study may inform systems science approaches which are better able to disentangle these complex phenemon60.
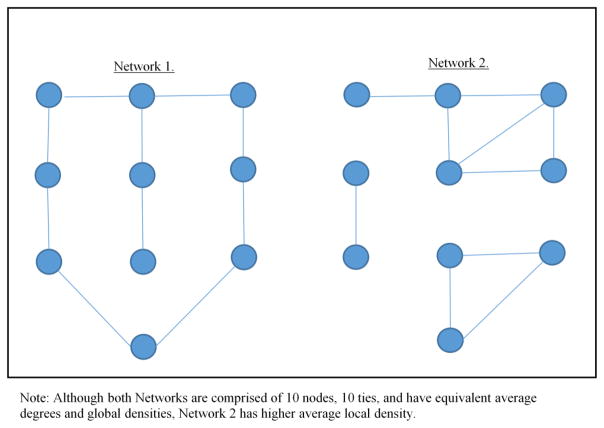
Local sexual network density was another factor that differed by race/ethnicity and according to conventional effect size standards, the difference between racial/ethnic minorities and White YMSM were medium in size. Although Black YMSM do not form more sexual ties on average, our results indicate that the ties that are made are more likely to “close the triangles” or to be transitive. Said another way, Black individuals may be more likely to have local clustering of their sexual partners. To better illustrate this, we are including two example network figures (See Figure 2). Despite similar numbers of nodes and ties, Network 1 displays very little local clustering (no triangles), while Network 2 displays strong network clustering (3 triangles). With the number of overall sexual partnerships constant, denser sexual networks indicate that individuals in a network are reachable by fewer numbers of sexual ties, which facilitates efficient communicable disease transmission. Additionally, local clustering concentrates the likelihood of successful HIV transmission within short distances, while making it less likely that HIV transmission will occur over long distances36,61. As such, the higher density of sexual networks among minority YMSM will tend to increase HIV transmission rates even in the presence of similar norms for unprotected sex. While this is a risk for HIV transmission, it may also present an opportunity for efficient dissemination of prevention methods through Black YMSM sexual networks.
Figure 2.
An illustration of local clustering.
The mechanisms that might cause these racial differences in density are still very much unknown. Greater sexual network density among Latino YMSM may be explained by the relatively smaller number of Latino young people in Chicago, however this explanation is unsatisfactory for Black YMSM as there are roughly the same number of Black and White young people in Chicago. These differences may also be driven by preferences for racial homophily, geographic proximity, or other partner selection preferences which are impacted by race, culture, and life circumstances. Future research is needed to tease apart these mechanisms.
There was significant assortativity by race, and our AC estimates were higher than the mean reported in a review of 15 prior network studies (0.58 versus 0.45, respectively)15. The vast majority of the partners of Black and White YMSM were of the same race (82% and 75% respectively), whereas Latino YMSM had a significantly lower proportion. However, once these proportions were set relative to racial/ethnic population distributions in Chicago, Latinos actually showed a higher in-group coefficent than Black and White YMSM. In terms of implications for HIV transmission, because race/ethnicity is associated with a number of factors related to HIV risk exposure, such as poor healthcare access, racial segregation of sexual networks will tend to increase racial differentials disfavoring underserved groups. High assortativity will also sustain differentials as HIV is less likely to be transmitted between groups. As such, the patterns of assortativity we found will tend to maintain or increase HIV disparities that already exist among YMSM.
In terms of relationships with sex partners, Black YMSM had a higher proportion reported as main partners than White and Latino YMSM. They were also significantly more likely to describe the strength of the relationship as “very close” than White YMSM. Prior studies of YMSM have repeatedly demonstrated that substantially more unprotected sex occurs with partners considered “serious” versus “casual”6,36,58, which may be in part driven by a sense of familiarity and safety of partners who are interpersonally close59. Nevertheless, Black YMSM did not have higher rates of condomless sex, so any role this may play on racial disparities must be independent of individual behavior. One possibility is that it may lead to dynamic changes in the network structure. For example, friendship may lead to increased sexual network linkages, which may increase local density and speed transmission within the network.
There were several important null results. No significant differences in rates of sexual concurrency were found. Prior modeling studies have shown that even small differences in concurrency can result in large group differences in STI prevalence 16,17,60, but in our sample the White YMSM had a slightly (but non-significantly so) higher level of concurrency than the minority youth. Other studies of MSM have also not found differences in concurrency by race20,21. Another null result was that while overall there was multiplexity in relationships, there were no significant differences in muliplexity for sex-drug or sex-social networks by race/ethnicity, although future work would benefit from examining how multiplexity may impact local sexual network structure and risk behaviors within sexual partnerships37,38.
Results must be interpreted in the context of study limitations. Most importantly, all data was self-report, including characteristics of alters and associations between alters. Incorrectly reporting of this information would have introduced error into our models and if there were racial differences in reporting it could bias our estimation of group differences. While collecting data from all individuals in the network would eliminate some of this bias, it is infesible to do so as the bounds of this population and the identities of all of its members cannot be ascertained.
In summary, we found signficiant differences in network characteristics that may help explain racial disparities in HIV among YMSM, which have previously been poorly understood through the study of individual behavior. Black YMSM were more likely to have older partners, partners from high prevalence neighborhoods, locally denser sexual networks, and had generally closed sexual networks as indicated by high assortativity by race. Our findings suggest that to eliminate racial inequities in HIV we may need to consider how network and geographic factors can be addressed through structural interventions in concert with prevention at the individual level. For example, our findings regarding the density of Black YMSM sexual networks, coupled with increased sexual partnerships with individuals from high prevalence neighborhoods, suggest that intensive interventions highly targeted to these networks and neighborhoods may have a larger impact on reducing new infections than more generalized and less intensive interventions.
Acknowledgments
This grant was supported by a grant from the National Institute of Drug Abuse (R01DA025548-02S1; PI: Mustanski), which was a competitive revision award to a parent grant (R01DA025548: Dual PIs: Mustanski and Garofalo). We acknowledge the role of Dr. Robert Garofalo as the dual-PI of the parent grant and thank the participants for their involvement in the study. We thank the Chicago Department of Public Health for providing geographic HIV data.
Footnotes
There are no conflicts of interest to declare.
References
- 1.Mustanski B, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: A review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012:17. [Google Scholar]
- 3.Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM, Group NS. High HIV incidence and prevalence and associated factors among young MSM, 2008. AIDS. 2013;27:269–278. doi: 10.1097/QAD.0b013e32835ad489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clerkin EM, Newcomb ME, Mustanski B. Unpacking the racial disparity in HIV rates: the effect of race on risky sexual behavior among Black young men who have sex with men (YMSM) J Behav Med. 2011;34:237–243. doi: 10.1007/s10865-010-9306-4. [DOI] [PubMed] [Google Scholar]
- 5.Newcomb ME, Mustanski B. Racial differences in same-race partnering and the effects of sexual partnership characteristics on HIV Risk in MSM: a prospective sexual diary study. J Acquir Immune Defic Syndr. 2013;62:329–333. doi: 10.1097/QAI.0b013e31827e5f8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newcomb ME, Ryan DT, Garofalo R, Mustanski B. The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Arch Sex Behav. 2014;43:61–72. doi: 10.1007/s10508-013-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garofalo R, Mustanski B, Johnson A, Emerson E. Exploring factors that underlie racial/ethnic disparities in HIV risk among young men who have sex with men. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2010;87:318–323. doi: 10.1007/s11524-009-9430-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feldman MB. A critical literature review to identify possible causes of higher rates of HIV infection among young black and Latino men who have sex with men. J Natl Med Assoc. 2010;102:1206–1221. doi: 10.1016/s0027-9684(15)30776-8. [DOI] [PubMed] [Google Scholar]
- 9.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 10.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380:341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 11.Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96:1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amirkhanian YA. Social Networks, Sexual Networks and HIV Risk in Men Who Have Sex with Men. Curr HIV/AIDS Rep. 2014 doi: 10.1007/s11904-013-0194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sudhinaraset M, Raymond HF, McFarland W. Convergence of HIV prevalence and interracial sexual mixing among men who have sex with men, San Francisco, 2004–2011. AIDS Behav. 2013;17:1550–1556. doi: 10.1007/s10461-012-0370-3. [DOI] [PubMed] [Google Scholar]
- 14.Potterat J. Socio-geographic space and sexually transmissible diseases. Australian Microbiologist. 1992;4:366. [Google Scholar]
- 15.Rothenberg R, Muth SQ. Large-network concepts and small-network characteristics: Fixed and variable factors. Sex Transm Dis. 2007;34:604–612. doi: 10.1097/01.olq.0000258358.13825.a8. [DOI] [PubMed] [Google Scholar]
- 16.Morris M, Goodreau SM, Moody J. Sexual networks, concurrency, and STD/HIV. In: Holmes KK, Sparling PF, Stamm WE, et al., editors. Sexually transmitted diseases. 4. New York: McGraw-Hill; 2007. pp. 109–125. [Google Scholar]
- 17.Morris M, Kretzschmar M. Concurrent partnerships and the spread of HIV. AIDS. 1997;11:641–648. doi: 10.1097/00002030-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Doherty IA, Minnis A, Auerswald CL, Adimora AA, Padian NS. Concurrent partnerships among adolescents in a Latino community: the Mission District of San Francisco, California. Sex Transm Dis. 2007;34:437–443. doi: 10.1097/01.olq.0000251198.31056.7d. [DOI] [PubMed] [Google Scholar]
- 19.Bohl DD, Raymond HF, Arnold M, McFarland W. Concurrent sexual partnerships and racial disparities in HIV infection among men who have sex with men. Sex Transm Infect. 2009;85:367–369. doi: 10.1136/sti.2009.036723. [DOI] [PubMed] [Google Scholar]
- 20.Lyons A, Hosking W. Prevalence and Correlates of Sexual Partner Concurrency Among Australian Gay Men Aged 18–39 Years. AIDS Behav. 2013 doi: 10.1007/s10461-013-0613-y. [DOI] [PubMed] [Google Scholar]
- 21.Garofalo R, Hotton A, Kuhns L, Gratzer B, Mustanski B. Incidence of HIV infection and Sexually Transmitted Infections and related factors among young men who have sex with men. 2014. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenberg ES, Khosropour CM, Sullivan PS. High prevalence of sexual concurrency and concurrent unprotected anal intercourse across racial/ethnic groups among a national, Web-based study of men who have sex with men in the United States. Sex Transm Dis. 2012;39:741–746. doi: 10.1097/OLQ.0b013e31825ec09b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aral SO. Patterns of sexual mixing: mechanisms for or limits to the spread of STIs? Sex Transm Infect. 2000;76:415–416. doi: 10.1136/sti.76.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson RM, Gupta S, Ng W. The significance of sexual partner contact networks for the transmission dynamics of HIV. J Acquir Immune Defic Syndr. 1990;3:417–429. [PubMed] [Google Scholar]
- 25.Raymond HF, McFarland W. Racial mixing and HIV risk among men who have sex with men. AIDS Behav. 2009;13:630–637. doi: 10.1007/s10461-009-9574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berry M, Raymond HF, McFarland W. Same race and older partner selection may explain higher HIV prevalence among black men who have sex with men. AIDS. 2007;21:2349–2350. doi: 10.1097/QAD.0b013e3282f12f41. [DOI] [PubMed] [Google Scholar]
- 27.Bingham TA, Harawa NT, Johnson DF, Secura GM, MacKellar DA, Valleroy LA. The effect of partner characteristics on HIV infection among African American men who have sex with men in the Young Men's Survey, Los Angeles, 1999–2000. AIDS Educ Prev. 2003;15:39–52. doi: 10.1521/aeap.15.1.5.39.23613. [DOI] [PubMed] [Google Scholar]
- 28.Bohl DD, McFarland W, Raymond HF. Improved measures of racial mixing among men who have sex with men using Newman's assortativity coefficient. Sex Transm Infect. 2011;87:616–620. doi: 10.1136/sextrans-2011-050103. [DOI] [PubMed] [Google Scholar]
- 29.Pettifor AE, Rees HV, Kleinschmidt I, et al. Young people's sexual health in South Africa: HIV prevalence and sexual behaviors from a nationally representative household survey. AIDS. 2005;19:1525–1534. doi: 10.1097/01.aids.0000183129.16830.06. [DOI] [PubMed] [Google Scholar]
- 30.Kelly RJ, Gray RH, Sewankambo NK, et al. Age differences in sexual partners and risk of HIV-1 infection in rural Uganda. J Acquir Immune Defic Syndr. 2003;32:446–451. doi: 10.1097/00126334-200304010-00016. [DOI] [PubMed] [Google Scholar]
- 31.Gregson S, Nyamukapa CA, Garnett GP, et al. Sexual mixing patterns and sex-differentials in teenage exposure to HIV infection in rural Zimbabwe. Lancet. 2002;359:1896–1903. doi: 10.1016/S0140-6736(02)08780-9. [DOI] [PubMed] [Google Scholar]
- 32.CDC. Prevalence and awareness of HIV infection among men who have sex with men --- 21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59:1201–1207. [PubMed] [Google Scholar]
- 33.Joseph HA, Marks G, Belcher L, et al. Older partner selection, sexual risk behaviour and unrecognised HIV infection among black and Latino men who have sex with men. Sex Transm Infect. 2011;87:442–447. doi: 10.1136/sextrans-2011-050010. [DOI] [PubMed] [Google Scholar]
- 34.Mustanski B, Newcomb ME. Older Sexual Partners May Contribute to Racial Disparities in HIV Among Young Men Who Have Sex With Men. J Adolesc Health. 2013;52:666–667. doi: 10.1016/j.jadohealth.2013.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shirley MDF, Rushton SP. The impacts of network topology on disease spread. Ecol Complex. 2005;2:287–299. [Google Scholar]
- 36.Doherty IA, Padian NS, Marlow C, Aral SO. Determinants and consequences of sexual networks as they affect the spread of sexually transmitted infections. J Infect Dis. 2005;191 (Suppl 1):S42–54. doi: 10.1086/425277. [DOI] [PubMed] [Google Scholar]
- 37.Latkin C, Mandell W, Oziemkowska M, et al. Using social network analysis to study patterns of drug use among urban drug users at high risk for HIV/AIDS. Drug Alcohol Depend. 1995;38:1–9. doi: 10.1016/0376-8716(94)01082-v. [DOI] [PubMed] [Google Scholar]
- 38.Mustanski B, Newcomb ME, Clerkin EM. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychol. 2011;30:597–605. doi: 10.1037/a0023858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Michael Szell RL, Thurnera Stefan. Multirelational organization of large-scale social networks in an online world. Proceedings of the National Academy of Sciences. 2010;107:13636–13641. doi: 10.1073/pnas.1004008107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kyu-Min Lee JYK, Cho Won-kuk, Goh1 K-I, Kim I-M. Correlated multiplexity and connectivity of multiplex random networks. New Journal of Physics. 2012:14. [Google Scholar]
- 41.Drumright LN, Frost SD. Rapid social network assessment for predicting HIV and STI risk among men attending bars and clubs in San Diego, California. Sex Transm Infect. 2010;86(Suppl 3):iii17–23. doi: 10.1136/sti.2010.045914. [DOI] [PubMed] [Google Scholar]
- 42.Celentano DD, Valleroy LA, Sifakis F, et al. Associations between substance use and sexual risk among very young men who have sex with men. Sex Transm Dis. 2006;33:265–271. doi: 10.1097/01.olq.0000187207.10992.4e. [DOI] [PubMed] [Google Scholar]
- 43.Koblin BA, Husnik MJ, Colfax G, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- 44.Latkin CA, German D, Vlahov D, Galea S. Neighborhoods and HIV: A social ecological approach to prevention and care. Am Psychol. 2013;68:210–224. doi: 10.1037/a0032704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raymond HF, Chen YH, Syme SL, Catalano R, Hutson MA, McFarland W. The Role of Individual and Neighborhood Factors: HIV Acquisition Risk Among High-Risk Populations in San Francisco. AIDS Behav. 2013 doi: 10.1007/s10461-013-0508-y. [DOI] [PubMed] [Google Scholar]
- 46.Chicago Department of Public Health. STI/HIV Surveillance Report. Chicago, IL: City of Chicago; 2011. [Google Scholar]
- 47.Hogan B, Carrasco JA, Wellman B. Visualizing personal networks: Working with participant-aided sociograms. Field Methods. 2007;19:116–144. [Google Scholar]
- 48.Kuhns L, Birkett M, Muth SQ, et al. Modifying and adapting participant-aided sociograms for a study of social, sexual and substance-using networks among young men who have sex with men. Connections. 2014 doi: 10.17266/35.1.1. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Youm Y, Mackesy-Amiti ME, Williams CT, Ouellet LJ. Identifying hidden sexual bridging communities in Chicago. J Urban Health. 2009;86 (Suppl 1):107–120. doi: 10.1007/s11524-009-9371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wasserman S, Faust K. Social network analysis: Methods and applications. Cambridge ; New York: Cambridge University Press; 1994. [Google Scholar]
- 51.Borgatti SP. Analyzing social networks. Thousand Oaks, CA: Sage Publications; 2013. [Google Scholar]
- 52.Weeks MR, Clair S, Borgatti SP, Radda K, Schensul JJ. Social Networks of Drug Users in High-Risk Sites: Finding the Connections. AIDS Behav. 2002;6:193–206. [Google Scholar]
- 53.Newman ME. Mixing patterns in networks. Phys Rev E Stat Nonlin Soft Matter Phys. 2003;67:026126. doi: 10.1103/PhysRevE.67.026126. [DOI] [PubMed] [Google Scholar]
- 54.U.S. Census Bureau. American FactFinder. 2010 http://factfinder.census.gov.
- 55.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, New Jersey: Erlbaum; 1988. [Google Scholar]
- 56.Hurt CB, Matthews DD, Calabria MS, et al. Sex with older partners is associated with primary HIV infection among men who have sex with men in North Carolina. J Acquir Immune Defic Syndr. 2010;54:185–190. doi: 10.1097/QAI.0b013e3181c99114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arrington-Sanders R, Leonard L, Brooks D, Celentano D, Ellen J. Older partner selection in young African-American men who have sex with men. J Adolesc Health. 2013 doi: 10.1016/j.jadohealth.2012.12.011. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mustanski B, Birkett M, Greene GJ, Hatzenbuehler ML, Newcomb ME. Envisioning an America without sexual orientation inequities in adolescent health. Am J Public Health. 2014;104:218–225. doi: 10.2105/AJPH.2013.301625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Potterat J. Socio-geographic space and focal condom use. Bathesda, MA: Center For Population Research, National Institute of Health; 1993. [Google Scholar]
- 60.Maglio PP, Sepulveda M-J, Mabry PL. Mainstreaming Modeling and Simulation to Accelerate Public Health Innovation. Am J Public Health. 2014;104:1181–1186. doi: 10.2105/AJPH.2014.301873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jimi Adams JM, Morris Martina. Sex, Drugs, and Race: How Behaviors Differentially Contribute to the Sexually Transmitted Infection Risk Network Structure. Am J Public Health. 2012;103:322–329. doi: 10.2105/AJPH.2012.300908. [DOI] [PMC free article] [PubMed] [Google Scholar]