Abstract
Although coverage rates and health outcomes are improving, many poor people around the world still do not benefit from essential health products. An estimated two-thirds of child deaths could be prevented with increased coverage of products such as vaccines, point-of-use water treatment, iron fortification, and insecticide-treated bednets. What limits the flow of products from the producer's laboratory bench to the end users, and what can be done about it? Recent empirical research suggests a crucial role for heavy subsidies.
The great majority of households in the developing world cannot afford essential health products at their retail price. This suggests that such products have to be subsidized if coverage is to expand rapidly. There are a number of theoretical reasons why such subsidies are warranted. First, many of the diseases affecting the developing world are communicable, and therefore both prevention and prompt treatment have social benefits (they reduce transmission risk) in addition to private benefits. Second, subsidizing experimentation with products and services can help households learn how valuable these products are.
However, there has been substantial debate about how to implement subsidies. Controversy has been particularly spirited on the question of cost sharing: What share of the cost should be borne by the end user? If this share is too low, some subsidy takers will generate no health gains, either because they do not need the subsidized product or would not use it. Conversely, if the share is too high, some people who would use the product and become healthier do not take it up because they cannot afford it. These conditions are known as overinclusion and overexclusion, respectively. The pricing debate grew out of the prevailing thought that, for most relevant products, subsidies to reduce overexclusion would necessarily create a lot of overinclusion. With bednets, for example, it was thought that when given away for free, many are wasted on people who do not value them enough as health products and instead misuse them—for example, as fishing nets or wedding veils.
Very large subsidies are necessary to increase usage in the short run
A number of recent experimental studies randomized the price at which households or communities could access a preventive health product. Their results suggest that while overexclusion is indeed a concern in the absence of subsidies, the risk of overinclusion when subsidies are introduced is much lower than previously thought.
Demand for many products appears to drop rapidly as the price increases (1). In Ghana, take-up of water filters worth $14 (U.S.) fell from 89 to 21% when the price increased from $1.40 to $4.20 (2) (Fig. 1). In Kenya, take-up of bednets worth $7 was below 20% for any price above $2.50 (3) (Fig. 1). Providing health information about the product typically did not reduce price sensitivity (4–6).
Fig. 1. Price sensitivity of take-up and usage.
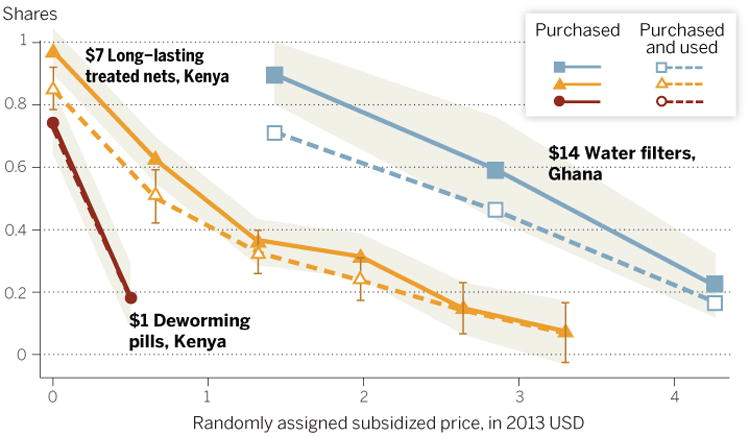
Usage of water filters was measured after 1 month (2). Usage of bednets was measured after 1 year (3). Usage of deworming pills is identical to take-up because the pills were placed in children's mouths by teachers (5). Shaded areas correspond to 95% confidence intervals for purchase rates. For purchase and usage of bednets, 95% confidence intervals are indicated with capped bars.
Because demand falls quickly as the price increases, only heavy subsidies yield high demand. But does this subsidized demand translate into high usage? The second key finding of randomized pricing studies is that it does, because many of those enticed to acquire a product only at low prices actually use it. In Ghana, close to 80% of heavily subsidized water filter owners were using their filter 1 month after they received the subsidy (2). In Kenya, 90% of free bednet beneficiaries were sleeping under the subsidized net 1 year later (3). Thus, whereas overexclusion is important in the absence of large subsidies, overinclusion under heavy subsidies appears limited (Fig. 1). For each product, the gap between the two ends of the dashed line is a measure of overexclusion at the highest price; the gap between solid and hollow markers at any price point is a measure of overinclusion.
Households do value heavily subsidized products
The third finding from recent pricing studies is that people need not have paid for something to value it. Households are as likely to use their bednet when they get it for free as when they have to pay for it (4, 7–9). People are as likely to use their water filter if they paid a lower price for it (2). This is surprising for two reasons. First, standard economic theory suggests that charging nontrivial user fees should help target products to those who need them the most—and thus those most likely to put them to appropriate use. But this reasoning breaks down when people face credit constraints and their ability to pay is lower than their willingness to pay. When those who could use a product the most are too poor to pay cash for it, higher prices screen out the poor, not just those with lower health returns from using the product (9). Second, it is often thought that the act of paying itself makes people value a product or service more; the feeling of “guilt” from having spent money on something that is left unused would make people more diligent users. However, experimental studies designed to test the importance of this psychological phenomenon suggest that this consideration is not important when it comes to essential health (2, 7,10). The cost of poor health seems a good enough incentive to put products to good use.
When overinclusion becomes a concern
The finding that the risk of overinclusion is limited does not apply to medical treatment. Overtreatment with antimalarials is common, and so is overtreatment with antibiotics, with resulting drug resistance concerns. Heavy subsidies can exacerbate this problem. A pricing experiment with artemisinin combination therapy, a drug to treat malaria, found that 64% of adults ingesting the drug when offered at the heavily subsidized price proposed by Kenya under the Affordable Medicine Facility for malaria did not have malaria (11). Overtreatment is driven in great part by the lack of access to reliable diagnostic services and the nonenforceability of prescription-only schemes. The next generation of studies should attempt to solve the problems of how to improve access to accurate diagnostic services in rural areas of the developing world, and how to change the incentives of informal drug outlets—the ubiquitous source of medical treatment in these areas.
Are subsidies good in the long run?
Even for preventive products, where overinclusion is less problematic, it still does not follow that high subsidies are good policies. An important concern that has been raised is that heavy subsidies, by keeping prices artificially low, may create expectations that prices should remain low. This would lower households' willingness to accept price increases and limit take-up once subsidies are lifted, creating a dependency trap. The evidence to date mitigates this concern. A pricing experiment in Kenya found that households randomly sampled to receive a free or highly subsidized bednet were significantly more likely to pay for a similar bednet a year later, despite already owning one (3). It appears that the subsidized bednet trial allowed households to learn the benefits of owning one, which increased their willingness to pay for another one in the future. Moreover, there was no effect of having received a free bednet on the willingness to pay for a water treatment product, which suggests that respondents had no expectation of free health product trials becoming the new norm.
Quality concerns
Low demand sometimes reflects poor quality of service. Health providers often operate as a local monopoly, be it the sole prenatal clinic or the sole drug shop, and may not be subject to regular quality controls. This leaves room for agency problems such as corruption and shirking that can undermine the effectiveness of subsidy programs.
One might worry that health workers could be corrupt, delivering subsidized products to the ineligible for a bribe or extorting illegal payments from the eligible. Overexclusion of targeted households because of such corruption is assumed to be deep and wide, but a recent audit study of bednet distribution programs by nurses at prenatal clinics in Ghana, Kenya, and Uganda found limited corruption among prenatal nurses and, as a result, very high coverage rates among targeted beneficiaries (12). Corruption may be rife in other distribution programs, however. More research is needed on this issue.
Health workers may shirk, by not showing up to work or by making no effort. Empirical studies from a number of countries have shown alarmingly high levels of provider absenteeism (13), as well as low quality for health services in both the private and public sectors (14). These can limit the effectiveness of subsidies at reducing overexclusion. Although effort levels were high in the aforementioned bednet distribution programs (12), provider absence has been shown to affect take-up of other free services such as immunization and HIV prevention (15,16).
Concerns over low provider effort have spurred recent research on the effectiveness of incentive schemes for health providers (17–19), an important topic beyond the scope of this perspective.
Incentives for end users
Sometimes demand remains recalcitrantly low even when the product is free, of good quality, and widely available. This may call for demand-side incentives, which can be thought of as negative prices. In a randomized controlled study in India, where reliable immunization camps were set up in villages, some parents were given a kilogram of lentils per immunization, along with a set of plates per fully immunized child. This incentive scheme led to an increase in full immunization rates from 18% in the control group to 39% in the incentivized group; the cost per shot (including the cost of the incentives) ended up being lower in the incentivized villages, thanks to economies of scale (15). Such “conditional” transfers, in cash or in kind, are increasingly common. Many of these programs, primarily antipoverty programs, give mothers cash if they or their children attend regular health checkups. The evidence to date suggests that such cash incentives are effective at increasing take-up of health services and are sometimes effective at improving health outcomes (20–22). Of course, the health impacts of these incentive schemes depend on the quality of the services and products offered.
Conclusion
A low-hanging fruit for improving health outcomes in the developing world is to increase the coverage of already existing and proven health products and services. Recent field experiments by economists find that for products with large social benefits, free distribution is the most cost-effective strategy for increasing coverage of essential health products and services. It is not always enough, however. In India, child immunization rates remain low despite full subsidies. Additional incentives can make an important difference in this case.
But is spending on individual subsidies and incentives the best use of typically limited government and international funding for public health? The biggest strides in the history of the reduction of child mortality in the United States came from infrastructural investments—in particular, investments in safe water (23). Malaria was eradicated from the southern United States and southern Europe, obviating the need to identify optimal pricing policies for individual malaria prevention and treatment products. Institutional pushes are needed for such infrastructural investments to take place in the two dozen countries that account for three-quarters of today's child mortality burden. Until these investments are made, micro-level subsidies and incentives appear necessary.
Fig. 2. Villagers looking at new mosquito nets donated in an effort to fight malaria in Matongo, Zambia, in April 2008.

[Photo: Kim Ludbrook/EPA]
Acknowledgments
Supported by NIH grant P01HD061315-01 and NSF grant 1254167.
References and Notes
- 1.JPAL. The Price Is Wrong. JPAL Bulletin. 2011 Apr; www.povertyactionlab.org/publication/the-price-is-wrong.
- 2.Berry J, Fischer G, Guiteras R. Cornell University; Apr, 2012. Eliciting and utilizing willingness to pay: Evidence from field trials in northern Ghana. http://econweb.arts.cornell.edu/jwb295/BFG-BDM-April-2012.pdf. [Google Scholar]
- 3.Dupas P. Econometrica. 2014;82:197–228. doi: 10.3982/ECTA9508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dupas P. Am Econ Rev. 2009;99:224–230. doi: 10.1257/aer.99.2.224. [DOI] [PubMed] [Google Scholar]
- 5.Kremer M, Miguel E. Q J Econ. 2007;122:1007–1065. [Google Scholar]
- 6.Meredith J, Robinson J, Walker S, Wydick B. J Dev Econ. 2013;105:196–210. [Google Scholar]
- 7.Cohen J, Dupas P. Q J Econ. 2010;125:1–45. [Google Scholar]
- 8.Hoffmann V. Am Econ Rev. 2009;99:236–241. [Google Scholar]
- 9.Tarozzi A, et al. Am Econ Rev. 2014;104:1909–1941. doi: 10.1257/aer.104.7.1909. [DOI] [PubMed] [Google Scholar]
- 10.Ashraf N, Berry J, Shapiro J. Am Econ Rev. 2010;100:2383–2413. [Google Scholar]
- 11.Cohen J, Dupas P, Schaner S. Price subsidies, diagnostic tests, and targeting of malaria treatment. 2014 www.nber.org/papers/w17943.pdf.
- 12.Dizon-Ross R, Dupas P, Robinson J. Governance and effectiveness of health subsidies. 2013 doi: 10.1016/j.jpubeco.2017.09.005. www. povertyactionlab.org/publication/governance-and-effectiveness-public-health-subsidies. [DOI] [PMC free article] [PubMed]
- 13.Chaudhury N, Hammer J, Kremer M, Muralidharan K, Rogers FH. J Econ Perspect. 2006;20:91–116. doi: 10.1257/089533006776526058. [DOI] [PubMed] [Google Scholar]
- 14.Das J, Hammer J. Annu Rev Econ. 2014;6:525–553. [Google Scholar]
- 15.Banerjee AV, Duflo E, Glennerster R, Kothari D. BMJ. 2010;340:c2220. doi: 10.1136/bmj.c2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldstein M, Zivin JG, Habyarimana J, Pop-Eleches C, Thirumurthy H. Am Econ J Appl Econ. 2013;5:58–85. doi: 10.1257/app.5.2.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller G, Babiarz KS. Pay-for-performance incentives in low- and middle-income country health programs. In: Culyer AJ, editor. Encyclopedia of Health Economics. Vol. 2. Elsevier; San Diego, CA: 2014. pp. 457–483. [Google Scholar]
- 18.Olken B, Onishi J, Wong S. Should aid reward performance? Evidence from a field experiment on health and education in Indonesia. 2013 doi: 10.1257/app.6.4.1. www. povertyactionlab.org/publication/should-aid-reward-performance-evidence-field-experiment-health-and-education-indonesia. [DOI] [PMC free article] [PubMed]
- 19.Banerjee AV, Duflo E, Glennerster R. J Eur Econ Assoc. 2008;6:487–500. doi: 10.1162/JEEA.2008.6.2-3.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barber SL, Gertler PJ. J Dev Effect. 2010;2:51–73. [Google Scholar]
- 21.Barham T. J Dev Econ. 2011;94:74–85. [Google Scholar]
- 22.Attanasio O, Oppedisano V, Vera-Hernández M. Should cash transfers be conditional? Conditionality, preventative care and health outcomes. 2014 www.homepages.ucl.ac.uk/∼uctpamv/papers/conditionality.pdf.
- 23.Cutler D, Miller G. Demography. 2005;42:1–22. doi: 10.1353/dem.2005.0002. [DOI] [PubMed] [Google Scholar]


